- 1College of Social Work, The Ohio State University, Columbus, OH, United States
- 2Higher Education Center for Alcohol and Drug Misuse Prevention and Recovery, The Ohio State University, Columbus, OH, United States
- 3School of Social Work, University at Buffalo, Buffalo, NY, United States
- 4Center for the Study of Drugs, Alcohol, Smoking, and Health, University of Michigan, Ann Arbor, MI, United States
- 5Health & Wellness, Wayne State University, Detroit, MI, United States
- 6School of Social Work, Wayne State University, Detroit, MI, United States
- 7Counseling and Psychological Services, Wayne State University, Detroit, MI, United States
- 8Merrill Palmer Skillman Institute, Wayne State University, Detroit, MI, United States
Introduction: Recovery capital is important to substance use recovery among general populations and among college students in recovery. Demographic factors and various psychosocial variables have been associated with recovery capital in studies including adults in the general population. However, recovery capital has received limited research attention in the context of collegiate recovery, and there has been little empirical evaluation of factors that might be linked with recovery capital among college students. As more collegiate recovery programs are developed to support students in recovery, these programs should implement features to augment students’ recovery capital.
Methods: We conducted a needs assessment on a campus with a newly developing collegiate recovery program. Students in recovery (n = 86) were asked to complete the 28-item Multidimensional Inventory of Recovery Capital (MIRC). They were also asked about sociodemographic and recovery-related factors including length of time in recovery, recovery pathway, perceived discrimination, mental health challenges, quality of relationships, and financial well-being. A multiple regression analysis was conducted to assess relationships between these variables and recovery capital.
Results: Students reported a moderate level of recovery capital (M = 82.55, SD = 13.64). Students who reported fewer mental health challenges in the past 30 days (β = −.25, t = −2.79, p = .006), better quality of relationships in the past week (β = .27, t = 3.41, p = .001), and greater financial well-being (β = .38, t = 4.69, p < .001) had greater recovery capital. Sociodemographic variables, recovery length, recovery pathway, and perceived discrimination were not associated with recovery capital.
Discussion: To our knowledge, this is the first study to identify associations between recovery capital as measured by the MIRC and various sociodemographic and recovery-related factors among a sample of college students in recovery. As such, this study extends previous work with updated knowledge of how students can be supported in their efforts to increase recovery capital. Future research can build on this study by utilizing the MIRC on various types of campuses and by assessing recovery capital among college students longitudinally.
1 Introduction
The U.S. Substance Abuse and Mental Health Services Administration (1) defines recovery as a “process of change through which people improve their health and wellness, live self-directed lives, and strive to reach their full potential”. Recovery Capital (RC) was introduced by Granfield and Cloud to describe how people who had ceased substance use without any form of treatment (i.e., unassisted recovery) drew upon various internal and external resources to initiate and sustain recovery from addiction (2). RC is divided into four main domains (3). Social capital encompasses the support and relationships provided by family, friends, and recovery communities, fostering a sense of belonging and connectedness that serves as a critical foundation for both emotional and practical support during recovery. Physical capital includes tangible assets such as housing, financial stability, access to transportation, and other material resources that create a stable and supportive recovery environment. Human capital refers to individual attributes such as education, skills, physical health, and mental health, which enhance personal resilience and the ability to maintain long-term recovery. Cultural capital represents the values, beliefs, and norms that shape recovery behaviors, including societal attitudes toward addiction and recovery. This domain underscores the importance of aligning recovery efforts with culturally sensitive practices (3, 4).
While positive recovery capital supports recovery efforts, barriers to recovery are captured by the concept of negative recovery capital (5). Negative recovery capital includes strained family relationships, economic hardship, homelessness, untreated mental health conditions, and stigma, all of which can significantly hinder an individual's recovery journey (3, 4). Such barriers are particularly detrimental when individuals lack access to supportive environments or resources to offset these challenges. White and Cloud (3) emphasize that effective interventions should not only focus on building positive recovery capital but also work to mitigate the effects of these barriers. By addressing these obstacles, recovery efforts can foster a recovery-friendly ecosystem.
Over the past decades since the concept was introduced, knowledge of RC has expanded, with a growing body of scholarship examining its various facets (6). Recent studies have documented associations between RC and a variety of outcomes, including greater likelihood of completing treatment (7, 8), decreases in substance use for individuals in opioid outpatient treatment (9) and opioid intervention courts (10), and maintaining recovery during the COVID-19 pandemic (11). Other research has examined changes in recovery capital over time, finding that RC typically increases over length of stay in recovery residences and is associated with greater quality of life (12, 13).
Additionally, scholars have introduced the concept of institutional justice capital, originally focused on how the legal system can support individuals' efforts to gain social and community recovery capital by making resources available (14). In turn, these institutional supports can foster the development of personal capital (14). Howard et al. (15) found that among a sample of justice-involved people, access to housing, peer recovery supports, and culturally responsive care predicted positive outcomes, including higher personal capital. These findings suggest that structural conditions within institutions shape recovery outcomes. Similarly, Martel et al. (16) found that among drug court-involved individuals, access to a peer recovery support program was associated with a sixfold increase in high recovery capital at the six-month follow-up. This lens can be extended to college campuses, because they are another setting in which institutional efforts to help students build social and community capital are likely to also impact personal capital. For example, the presence of a CRP and the college or university's commitment to making it visible might be a form of institutional justice capital.
There is a need for examining RC among specific populations that face challenges in addiction recovery (17). One such population is emerging adults, as the rate of substance use disorders is highest among people ages 18 to 25 (18). Recent data from Monitoring the Future shows that in the past 30 days, 64.9% of individuals aged 19 to 30 reported alcohol use and 28.7% reported marijuana use (19). Elswick et al. (20) explored recovery capital among emerging adults ages 18–25, finding that residential and financial instability are hindrances, while spirituality, family support, and visible recovery role models are facilitators. In a study of emerging adults ages 18–21 undergoing residential treatment in Australia, Mawson et al. (21) found that lower levels of substance use within social networks were significantly associated with higher recovery capital and improved environmental quality of life.
To date, relatively little work has addressed recovery capital among college students specifically, while rates of substance use remain high. The Spring 2024 National College Health Assessment (22) found that in the past 30 days, 54.8% of students reported alcohol use and 20% reported marijuana use. In college, substance use is typically normalized and viewed as a harmless rite of passage (23, 24), while recovery is often stigmatized (25–27). Qualitative work that has utilized the recovery capital framework provides clues as to how recovery capital benefits college students in recovery. For example, internal resources like personal strengths and coping strategies (28, 29) build human capital, as do new educational and career opportunities (27). Peer networks built in mutual aid recovery programs or in recovery-supportive activities increase social capital (27–29). Supportive family members, when available, also build social capital (28). Furthermore, professors who support the student's recovery, and access to services like the university's counseling center add to cultural capital (28, 29).
Evidence from a longitudinal study of students across 43 collegiate recovery programs (CRPs) found high levels of recovery capital and recovery-related functioning despite experiencing high levels of adversity (i.e., polysubstance use, substance use disorder severity, mental health challenges, and criminal legal system involvement) (30). CRPs offer promise for increasing recovery capital because they provide dedicated physical spaces on campus, a community of peers who share similar recovery journeys, and are staffed by professionals who can link students to needed services (31). CRPs are associated with positive outcomes such as sustained abstinence from substances (32), and participants achieving higher grades and graduation rates than the general student population (33). There are fewer than 200 CRPs among the 3,931 higher education institutions in the United States and fewer than ten other CRPs worldwide (25, 34, 35), suggesting an opportunity to create additional programs with an eye on augmenting students' recovery capital.
Prior research provides clues as to what variables might be associated with improved recovery capital among the general adult population. Regarding sociodemographic variables, prior research indicates that being part of a racially minoritized population is associated with greater barriers to recovery and to building recovery capital, though members of minoritized groups also demonstrate resilience at individual and community levels (36–39). People who are women, gender minorities, and sexual minorities also experience greater obstacles to building recovery capital (40–42).
Recovery-related variables are also important to consider. Greater length of time in recovery has been associated with high levels of recovery capital in prior research (7, 12, 43, 44). Furthermore, individuals in unassisted recovery (i.e., not utilizing any treatment services or mutual aid groups) may have less severe histories of substance use and mental health (45), but may also have above-average variability in levels of recovery capital (44). Perceived discrimination based on substance use history is also associated with lower levels of recovery capital (46). Notably, research on the relationships between these variables and recovery capital has been conducted primarily among adults in the general population, leaving gaps in knowledge regarding how sociodemographic and recovery-related factors may be linked with recovery capital in college students (28).
Lastly, several social-contextual variables may facilitate or impede recovery capital development. Although factors such as mental health challenges, problems in interpersonal relationships, and financial strain can be hypothesized to be negatively associated with recovery capital (4, 5, 20), little research has empirically evaluated these associations, particularly in college students. To address these gaps in the recovery capital research literature and to inform CRP programming, the aim of this analysis was to assess factors associated with recovery capital among college students on a campus that was preparing to implement a CRP. Based on the prior literature, we asked: what sociodemographic, recovery-related, and social-contextual variables are associated with recovery capital cross-sectionally among a sample of college students on a campus preparing to implement a CRP? To answer this research question, we analyzed the results of a needs assessment at a campus that had recently established a collegiate recovery program, analyzing the associations between sociodemographic, recovery-related, and social-contextual variables and recovery capital for college students.
2 Materials and methods
A sample of students at a Midwestern university who identified as being in recovery or as being a recovery ally were recruited to complete a needs assessment to support the development of a collegiate recovery program (N = 178). We limited the analysis that follows to those participants who identified as being in recovery (n = 86). Of note, recovery was self-defined as previously having a problem with alcohol or other drugs, but already resolving that problem or being in the process of resolving the problem (45). In other words, a participant did not need to be abstinent to be eligible to complete the survey. To recruit participants, we utilized flyers posted on the university's web-based announcement platform, on Facebook, and attached to university news articles about the CRP. Author EM also conducted presentations in substance use courses within the School of Social Work to introduce students to the collegiate recovery program. At the end of each presentation, time was provided for students to complete the needs assessment if they chose to participate. Recruitment took place between October 2023 and March 2024.
Participants provided information on their demographics, including racial/ethnic identity, gender identity, age, and sexual orientation. They also responded to questions regarding their participation in assisted recovery pathways (e.g., Alcoholics Anonymous, Narcotics Anonymous), length of time in recovery, perceived discrimination encountered because of having a substance use issue, mental health challenges, quality of relationships, and financial well-being. There were various other topics covered in the needs assessment that were not included in the present study. The survey took approximately 15 min to finish. Participants were offered the chance to enter a drawing for one of five $100 gift cards. To ensure adequate data quality, we followed Pozzar et al.'s (47) approach to combating low-quality data from online surveys, by removing respondents who had unrealistic completion times (<5 min) and nonsensical or duplicate responses to open-ended items from the sample. This resulted in the removal of n = 10 responses of the 178 recorded for the larger study. The [BLINDED] Institutional Review Board approved all study procedures.
2.1 Measures
2.1.1 Demographic variables
Participants were asked to report their age (in years). They were also asked to report their gender identity, choosing all of the following that applied: man, woman, trans man, trans woman, genderqueer/gender non-conforming, or another gender identity, with an open response option. Similarly, participants were asked to report their race/ethnicity, choosing all of the following that were applicable: African American or Black, American Indian or Alaska Native, Arabic or Middle Eastern, Asian American, Hispanic/Latino, Native Hawaiian or Other Pacific Islander, White, or another race/ethnicity with an open response option. Likewise, participants were presented with several options for sexual orientation and asked to mark all that applied: straight/heterosexual, gay/homosexual, bisexual, pansexual, queer, or asexual, with an open-text response option for other sexual orientations.
Because relatively few respondents identified as a gender other than man or woman, we trichotomized gender as woman (=1), man (=2), or trans man, trans woman, genderqueer/gender non-conforming, or another gender identity (=3). Likewise, because relatively few participants identified as a race other than White, we dichotomized race as did not select one or more minoritized racial or ethnic groups (=0) vs. selected one or more minoritized racial or ethnic groups (=1). In terms of sexual orientation, a small fraction of participants chose any besides straight/heterosexual. We therefore dichotomized this variable as selected one or more sexual minority groups (=0) vs. straight/heterosexual (=1). Each of these decisions helped to ensure that we retained the necessary statistical power to detect differences between groups.
2.1.2 Length of time in recovery
Participants were asked to report how long they have been in recovery, in years and months (45), via an open-text response. We then created a variable to express each participant's recovery time numerically, using months and years combined. For example, a response of “8 years, 5 months” would be represented as 8.42.
2.1.3 Recovery pathway
Participants were asked to indicate whether they currently, previously, or never used each of five recovery pathways (45). These included: (1) professionally-assisted recovery support (e.g., outpatient or inpatient treatment), (2) anti-relapse/craving medication (e.g., Suboxone), (3) twelve-step groups (e.g., AA or NA), (4) other mutual aid groups (e.g., SMART Recovery), and (5) other community-based recovery support (e.g., sober living). We condensed this variable to compare participants who reported never using any of these services (unassisted recovery, =0) to those who reported currently or previously using at least one of these services (assisted recovery, =1).
2.1.4 Perceived discrimination
To gauge participants' perceived experiences of discrimination resulting from their history of substance use and recovery, we used the eight-item Micro Discrimination Subscale of the Perceived Discrimination in Addiction Recovery Scale (46). This scale begins by asking, “Since you’ve been in recovery, how frequently have the following occurred because someone knew about your alcohol or other drug use history?” Participants then respond to statements such as “People treated me like a criminal” and “People said I looked like an “alcoholic” or “addict””. Each response was scored on a four-point Likert scale, including never (=1), once or twice (=2), a few times (=3), and often (=4). We then summed the eight items for the total scale, which ranged from 8 to 32 (Cronbach's ɑ = .91).
2.1.5 Mental health challenges
To assess mental health challenges, we used the six-item Kessler Psychological Distress Scale (48). This scale begins with the prompt “During the past 30 days, how often did you feel…” and then asks participants to indicate how often they felt “nervous?” “hopeless?” “restless or fidgety?” “so depressed that nothing could cheer you up?” “that everything was an effort?” and “worthless?” Each response was scored on a five-point Likert scale, including none of the time (=1), a little of the time (=2), some of the time (=3), most of the time (=4), and all of the time (=5). We then summed the six items for the total scale, ranging from 5 to 30 (Cronbach's ɑ = .89).
2.1.6 Quality of relationships
To understand the quality of participants’ interpersonal relationships, we utilized the five-item Interpersonal Relationships Subscale of the BASIS-24 (49). This scale begins with the prompt “During the past week, how often did you…” followed by “get along with people in your family”, “get along with people outside your family?” “get along well in social situations?” “feel close to another person?” and “feel like you had someone to turn to if you needed help?” Each response was scored on a five-point Likert scale, including none of the time (=0), a little of the time (=1), half of the time (=2), most of the time (=3), and all of the time (=4). We then summed the five items for the total scale, ranging from 0 to 20 (Cronbach's ɑ = .78).
2.1.7 Financial well-being
We assessed financial well-being with the five-item Financial Strain Scale (50). This scale presents statements such as “I have enough money to participate in most of the same activities as my peers” and “I worry about being able to pay my current monthly expenses”. Each item was scored on a four-point Likert scale with strongly disagree (=1), disagree (=2), agree (=3), and strongly agree (=4). Three items were reverse-scored so that a higher score indicated greater financial well-being. Lastly, the five items were summed for each participant to create a total scale ranging from 5 to 20 (Cronbach's ɑ = .86).
2.1.8 Recovery capital
Participants completed the Multidimensional Inventory of Recovery Capital (MIRC), a recently developed comprehensive measure of RC (51). The 28-item MIRC assesses RC across four subscales aligning with the constructs of social, physical, human, and cultural capital (4). MIRC items assess both positive and negative recovery capital, with negative capital items being reverse scored so that higher scores indicate greater RC (total score range 28–112; Cronbach's ɑ = .93).
2.2 Data analysis
Data analyses were conducted in IBM SPSS Statistics (Version 29) using multiple imputation with 10 imputations for missing data (52), then using ordinary least squares linear regression to examine associations between recovery capital and other variables. To specify a regression model, we began by selecting several variables that have been associated with recovery capital in previous studies or that might be associated with it among college students, such as undergraduate vs. graduate status, or part-time vs. full-time enrollment in school. We then conducted several regression analyses with combinations of these variables, starting with simple models including sociodemographic variables and one or two other variables at a time. To specify the final model, we retained sociodemographic variables and those that increased the predictive ability of simpler models.
Data were screened for outliers and multicollinearity among independent variables. Cook's Distance was used to test for extreme data points that may distort results, with no cases greater than 0.50 (53). Normal probability plots demonstrated that residuals were normally distributed, scatterplots suggested homoscedasticity, and variance inflation factors showed no evidence of problems with multicollinearity. To assess factors associated with recovery capital among participants, descriptive statistics were calculated for all independent and dependent variables. T-tests and ANOVA were performed to assess the relationship between each categorical predictor and total recovery capital independently. Pearson's correlation analyses were implemented to understand the pairwise relationships between each continuous predictor and total recovery capital. Finally, ordinary least squares linear regression was conducted to determine which independent variables were associated with recovery capital. The significance threshold was set at p < .05.
3 Results
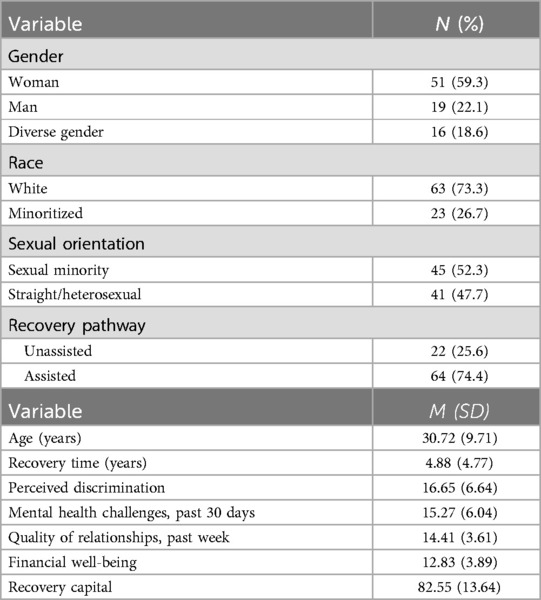
Descriptive statistics are presented in Table 1. Approximately one-quarter of participants (26.7%, n = 23) identified as a member of at least one racial or ethnic minority group. Most of the participants (59.3%, n = 51) identified as women. Nearly half of the sample (47.7%, n = 41) identified as a member of one or more sexual minority groups. Age ranged from 17 to 64 (M = 30.72, SD = 9.71).
Participants reported recovery times anywhere from 0 years, 0 months1 to 19 years, 0 months (M = 4.88, SD = 4.77). Nearly three quarters of participants (74.4%, n = 64) reported currently or previously engaging in an assisted recovery pathway, with 58.1% (n = 50) having used professionally-assisted recovery support, 27.9% (n = 24) having used anti-relapse/craving medication, 65.1% (n = 56) having used twelve-step groups, 27.9% (n = 24) having used other mutual aid groups (e.g., SMART Recovery), and 38.4% (n = 33) having used other community-based recovery support (e.g., sober living). Perceived discrimination scores ranged from 8 to 32 (M = 16.65, SD = 6.64). Mental health challenges ranged from 6 to 30 (M = 15.27, SD = 6.04), relationship quality ranged from 5 to 20 (M = 14.41, SD = 3.61), and financial well-being ranged from 5 to 20 (M = 12.83, SD = 3.89). These indicate a moderate level of mental health challenges, relatively strong relationship quality, and a moderate level of financial well-being among the overall sample. Finally, total scores on recovery capital ranged from 55 to 111, with a mean score of 82.55 (SD = 13.64).
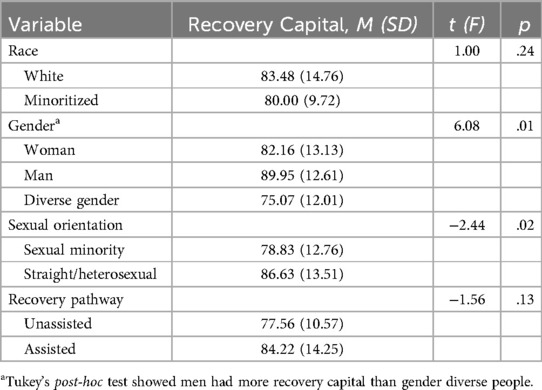
Bivariate associations between categorical predictors and recovery capital are available in Table 2. At the bivariate level, gender was associated with recovery capital (F = 6.08, p = .01). A Tukey's post-hoc test revealed that men had more recovery capital than gender-diverse participants, while there were no significant differences in recovery capital between men and women or women and gender-diverse individuals. Identifying as straight/heterosexual was associated with greater recovery capital in comparison to identifying as a sexual minority (t = −2.44, p = .02). Race and recovery pathway were not associated with recovery capital at the bivariate level.
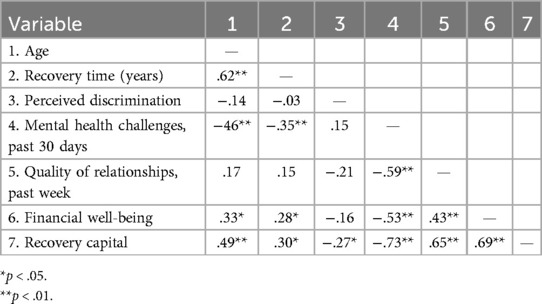
A correlation matrix displaying relationships between continuous predictors, and the relationship of each predictor to recovery capital, is available in Table 3. Older age (r = .49, p < .001), longer time in recovery (r = .30, p = .01), less perceived discrimination (r = −.27, p = .02), fewer mental health challenges in the past 30 days (r = −.73, p < .001), better quality of relationships in the past week (r = .65, p < .001), and greater financial well-being (r = .69, p < .001) were associated with greater recovery capital.
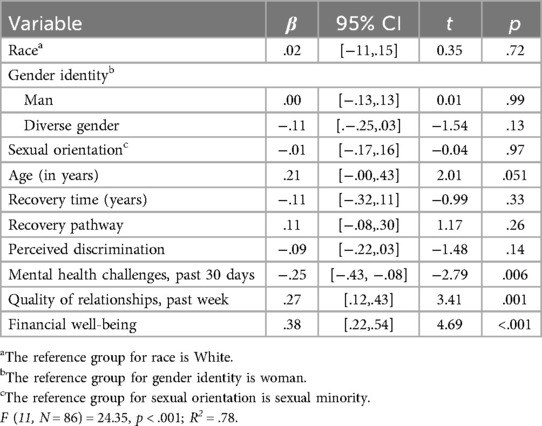
The results of the multiple regression analysis are summarized in Table 4. The overall model was significant [F (11, N = 86) = 24.35, p < .001; R2 = .78]. Those who reported fewer mental health challenges over the past 30 days (β = −.25, t = −2.79, p = .006), better quality of relationships in the past week (β = .27, t = 3.41, p = .001), and greater financial well-being (β = .38, t = 4.69, p < .001) had greater recovery capital. Demographic variables, recovery pathway, perceived discrimination, and recovery time were not associated with recovery capital in this model.
4 Discussion
In this study, we examined factors associated with recovery capital among students (N = 86) who participated in a needs assessment for a newly developing collegiate recovery program. We therefore extend previous, primarily qualitative, work that has examined recovery capital among college students, and provide updated knowledge of how CRPs can plan their activities with the goal to support and increase recovery capital (54). Overall, students reported a moderate level of recovery capital, with considerable variation in recovery capital levels between participants (M = 82.55, SD = 13.64). These results align with those of a prior study using the MIRC with an adult (18+) sample of persons in recovery, which reported M = 77.4, SD = 13.1 (51). Furthermore, compared to a national multisite study of students participating in CRPs at public institutions (55), our sample included a higher proportion of students identifying as female and racial/ethnic minorities. Although it is difficult to directly compare our results with the results of this study in terms of recovery-related characteristics due to differing measures, in both studies the majority of students reported a history of inpatient or outpatient SUD treatment and had been in recovery for at least one year. Thus, our findings help to provide a fuller picture of the characteristics of college students in recovery, suggesting that students in a sample with considerable diversity in terms of gender and race/ethnicity had substantial though variable levels of recovery capital, prior to the implementation of a CRP.
Those who experienced fewer mental health challenges in the past 30 days reported greater recovery capital. Mental health is situated in the human capital subdomain of the MIRC, and better mental health may also make it easier to connect with other people in recovery and potentially supportive people outside of recovery, thereby boosting both social and cultural capital. Additionally, better quality of relationships in the past week was linked with higher recovery capital. The social capital subscale of the MIRC asks about relational support, and better relationships could reinforce other domains of RC. For example, better relationships may promote a sense of meaning and purpose in life (human capital). Finally, greater financial well-being was linked with higher recovery capital. The physical capital subscale of the MIRC asks about finances and, as with mental health and relationship quality, it is likely that financial well-being is also conducive to other aspects of recovery capital. For example, it could make helpful services and resources accessible (cultural capital) and reduce stress (human capital). Although other research has documented associations between measures of recovery capital and assessments of variables such as relationship quality, health and mental health, and financial wellbeing (56), this study is the first–to our knowledge–to do so using the MIRC measure and in a sample of college students self-identifying as in recovery.
4.1 Implications
This study highlights ways collegiate recovery programs can help students boost recovery capital. While the presence of these programs serves as a form of cultural capital, our findings have implications for human, physical, and social capital. Regarding human capital, because fewer past-month mental health challenges may be associated with greater recovery capital, campus-based services should tackle mental health challenges among students in recovery. It may be possible to embed clinical services within the CRP (31) and if not, CRP staff can refer students in need to campus counseling services. This idea is consistent with ARHE's (31) statement that CRPs should recognize the prevalence of co-occurring disorders and be ready to offer needed programming and referrals for impacted students. Moreover, our findings suggest that such resources may be conducive to increased recovery capital, so providing such resources can be a way to incorporate recovery capital within the development of a CRP.
Because greater financial well-being may be associated with greater recovery capital, CRPs could consider offering financial literacy education and even financial support for their members. Workshops could be conducted to assist students with budgeting and other aspects of financial wellness. CRP staff could pool a list of scholarships for which members might be eligible. Additionally, some CRPs offer financial assistance to members (31), and even a small stipend could ease the pressures of paying for college. Many CRPs receive financial support from private donors or CRP alumni who are invested in the members' success (57), and it may be feasible to provide such stipends via these funds. Additional funding to defray the costs of college may reduce students' need to work while also balancing academics and recovery, which previous research has found to be a barrier to recovery (25, 28). Therefore, financial support would boost physical capital and may also assist with human capital by making it easier to maintain recovery and schooling.
In our sample, participants who reported better quality of relationships in the past week also reported greater recovery capital. CRPs are well-positioned to support members' social capital needs. They may offer mutual aid meetings or informal social gatherings and at minimum, they facilitate a peer support network (31). CRPs should ensure that students have opportunities to connect at least weekly, such as a check-in meeting or a weekend activity. These opportunities could help students build and maintain positive relationships. In addition to augmenting social capital, these offerings may also increase cultural capital.
4.2 Limitations and directions for future research
This study had a relatively small sample size. Previous work has documented this as a challenge in collegiate recovery research (32). Although they did not remain significant in the final multiple regression model, several sociodemographic and recovery-related variables were associated with recovery capital in bivariate models. A larger sample would provide the statistical power necessary to detect more potential relationships between sociodemographic and recovery-related factors and recovery capital and in turn, to further direct CRP-building efforts. Likewise, it would allow for subgroup analyses with the potential to reveal recovery capital needs among specific student populations, such as racial, gender, or sexual minorities. This could be accomplished by conducting a multi-campus needs assessment including students from CRPs that are in a similar stage of development.
Additionally, we conducted this needs assessment on a relatively large, urban, primarily commuter campus. Campus characteristics such as urbanicity, proportion of residential vs. commuter students, and overall size of the student population may impact recovery capital, and recovery experiences in general. For example, residential campuses may facilitate social capital by presenting students with more opportunities to build supportive relationships, and also increase the risk of negative recovery capital via more pressure to use substances (28). Future work should therefore consider how recovery capital needs differ on various types of campuses, with an eye towards building tailored support services.
While our study highlights factors associated with recovery capital among a sample of college students, future work could also utilize an institutional justice capital (IJC) lens to focus on how colleges and universities support or impede the growth of recovery capital. For example, future work could examine if presentations by CRP staff to potentially interested students might be a touchpoint that helps students feel supported in their recovery efforts. Such activities may also reduce stigma and enhance resource navigation, thereby helping students to increase their recovery capital. Similarly, future work could investigate how various structural components of campuses, such as the presence or absence of stigma education programs for the general student population or tailored recovery services for multiply-marginalized students (i.e., those who are in recovery and hold at least one other marginalized identity) impact recovery capital. These examples all reflect intentional efforts by a higher education institution to support students' recovery, therefore making them candidates for further study of how institutional justice capital might work in the campus setting.
Because the MIRC is a newer measure (51), there were few studies with which we could directly compare our results in terms of understanding recovery capital levels and variations among college students. Future research using the MIRC in diverse populations and settings, including with college students in recovery, will advance understanding of recovery capital in this population. This research should also examine how recovery capital might differ among students who are utilizing various “assisted” recovery pathways (e.g., students in twelve-step groups vs. those in other mutual aid groups). There is also a remaining need for longitudinal studies investigating how various components of CRPs contribute to desired recovery capital outcomes among CRP members (54). This aim could be accomplished by gathering data on students' demographics and other characteristics when they initiate CRP membership, then measuring students' level of engagement in CRP activities and their relevant outcomes quarterly or semi-annually (54). Moreover, there is currently limited research on how longer-term outcomes like graduation are related to recovery capital changes (58), and longitudinal research could address such questions too.
4.3 Conclusion
This study documents associations between a novel measure of recovery capital, the MIRC, and various sociodemographic and recovery-related factors among college students. There was a moderate level of recovery capital among the overall sample. Factors associated with greater recovery capital in the linear regression model included fewer mental health challenges in the past 30 days, better quality of relationships in the past week, and greater financial well-being. Collegiate recovery programs can utilize these findings to plan programming to augment students' recovery capital. Future research can illuminate factors associated with recovery capital among students on different types of campuses. Moreover, longitudinal study would facilitate understanding of how various aspects of collegiate recovery programming relate to desired changes in recovery capital.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Wayne State University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MB: Writing – review & editing, Methodology, Writing – original draft, Formal analysis, Funding acquisition, Validation, Conceptualization. JA: Writing – original draft, Formal analysis, Writing – review & editing. EB: Writing – original draft, Resources, Writing – review & editing, Methodology. EP: Writing – original draft, Formal analysis, Funding acquisition, Conceptualization, Validation, Writing – review & editing, Methodology. EM: Writing – review & editing, Funding acquisition, Writing – original draft, Formal analysis, Validation, Data curation, Investigation, Conceptualization. JK: Writing – original draft, Writing – review & editing, Funding acquisition. SR: Data curation, Conceptualization, Writing – original draft, Validation, Methodology, Investigation, Writing – review & editing, Formal analysis, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Jamie Daniels Foundation awards R1-2023-54/CB-22-647 and R2-2024-12_CB-24-823. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnote
1. ^Some recorded lengths of recovery appear as zero due to rounding of small values.
References
1. Substance Abuse and Mental Health Services Administration. SAMHSA’s working definition of recovery. (2012). Available online at: https://store.samhsa.gov/sites/default/files/pep12-recdef.pdf (Accessed March 27, 2025).
2. Granfield R, Cloud W. Coming Clean: Overcoming Addiction Without Treatment. New York and London: New York University Press (1999).
3. White W, Cloud W. Recovery capital: a primer for addictions professionals. Counselor. (2008) 9(5):22–7.
4. Cloud W, Granfield R. A life course perspective on recovery capital. In: Kelly JF, White WL, editors. Addiction Recovery Management. New York: Springer (2004). p. 59–75.
5. Patton D, Best D, Brown L. Overcoming the pains of recovery: the management of negative recovery capital during addiction recovery pathways. Addict Res Theory. (2022) 30(5):340–50. doi: 10.1080/16066359.2022.2039912
6. Best D, Hennessy EA. The science of recovery capital: where do we go from here? Addiction. (2022) 117(4):1139–45. doi: 10.1111/add.15732
7. Headid RJ, Doane TC, Cohen BD, Smith EC, Redden D, Stoner AM. Identifying components of recovery capital that support substance use disorder treatment completion. Addict Behav Rep. (2024) 19:100538. doi: 10.1016/j.abrep.2024.100538
8. Sánchez J, Sahker E, Arndt S. The assessment of recovery capital (ARC) predicts substance abuse treatment completion. Addict Behav. (2020) 102:106189. doi: 10.1016/j.addbeh.2019.106189
9. Bormann NL, Weber AN, Arndt S, Lynch A. Improvements in recovery capital are associated with decreased alcohol use in a primary opioid use disorder treatment-seeking cohort. Am J Addict. (2023) 32(6):547–53. doi: 10.1111/ajad.13431
10. Knapp KS, Kulak JA, Homish DL, Granfield R, Homish GG, Kahn LS. Longitudinal trajectories in recovery capital and associations with substance use among adult drug treatment court clients. Drug Alcohol Depend. (2024) 260:111343. doi: 10.1016/j.drugalcdep.2024.111343
11. Gilbert PA, Soweid L, Kersten SK, Brown G, Zemore SE, Mulia N, et al. Maintaining recovery from alcohol use disorder during the COVID-19 pandemic: the importance of recovery capital. Drug Alcohol Depend. (2021) 229:109142. doi: 10.1016/j.drugalcdep.2021.109142
12. Cano I, Best D, Edwards M, Lehman J. Recovery capital pathways: modelling the components of recovery wellbeing. Drug Alcohol Depend. (2017) 181:11–9. doi: 10.1016/j.drugalcdep.2017.09.002
13. Härd S, Best D, Sondhi A, Lehman J, Riccardi R. The growth of recovery capital in clients of recovery residences in Florida, USA: a quantitative pilot study of changes in REC-CAP profile scores. Subst Abuse Treat Prev Policy. (2022) 17(1):58. doi: 10.1186/s13011-022-00488-w
14. Best D, Hamilton S, Hall L, Bartels L. Justice capital: a model for reconciling structural and agentic determinants of desistance. Probat J. (2021) 68(2):206–23. doi: 10.1177/02645505211005018
15. Howard H, Skinner-Osei P, Freeman K, Hulick J. Evaluating recovery capital to promote long-term recovery for justice-involved persons in south Florida. J Addict Offender Couns. (2025) 46(1):53–68. doi: 10.1002/jaoc.12141
16. Martel I, Eubanks R, Hughes E, Micek J, Barrett M. Improvements in recovery capital within the context of adult drug court with parallel peer support services: a 6-month post-enrollment study. J Adv Just. (2024) V:19–40.
17. Bowen E, Hennessy EA. Conceptualizing recovery capital: domains and critical perspectives. In: Best D, Hennessy E, editors. The Addiction and Recovery Capital Reader. Bristol: Bristol University Press (2025). p. 97–119.
18. Substance Abuse and Mental Health Services Administration. Highlights for the 2023 national survey on drug use and health. (2024). SAMHSA Publication No. PEP24-07-020. Available online at: https://www.samhsa.gov/data/sites/default/files/NSDUH%202023%20Annual%20Release/2023-nsduh-main-highlights.pdf (Accessed March 27, 2025).
19. Patrick ME, Miech RA, Johnston LD, O’Malley PM. Monitoring the Future Panel Study Annual Report: National Data on Substance use among Adults Ages 19 to 65, 1976–2023. Ann Arbor, MI: Institute for Social Research, University of Michigan (2024). (Monitoring the Future Monograph Series).
20. Elswick A, Fallin-Bennett A, Ashford K, Werner-Wilson R. Emerging adults and recovery capital: barriers and facilitators to recovery. J Addict Nurs. (2018) 29(2):78–83. doi: 10.1097/JAN.0000000000000218
21. Mawson E, Best D, Beckwith M, Dingle GA, Lubman DI. Social identity, social networks and recovery capital in emerging adulthood: a pilot study. Subst Abuse Treat Prev Policy. (2015) 10:45. doi: 10.1186/s13011-015-0041-2
22. American College Health Association. National College Health Assessment III: Undergraduate Student Reference Group Data Report Spring 2024. Silver Spring, MD: American College Health Association (2024).
23. Perron BE, Grahovac ID, Uppal JS, Granillo TM, Shutter J, Porter CA. Supporting students in recovery on college campuses: opportunities for student affairs professionals. J Stud Aff Res Pract. (2011) 48(1):47–64. doi: 10.2202/1949-6605.6226
24. Scott A, Anderson A, Harper K, Alfonso ML. Experiences of students in recovery on a rural college campus. SAGE Open. (2016) 8:1–8. doi: 10.1177/2158244016674762
25. Burns VF, Strachan T, Sinclair I, Hadad N. Recovery is complicated”: a qualitative exploration of Canadian university students’ diverse recovery experiences. Alcohol Treat Q. (2024) 42(3):359–76. doi: 10.1080/07347324.2024.2347241
26. Kollath-Cattano C, DeMaria AL, Sundstrom B, Kooper A, Manzi H, McInnis SM, et al. Everyone wants a community’: a qualitative investigation of the challenges and service needs among college students in recovery. Addict Res Theory. (2018) 26(5):369–76. doi: 10.1080/16066359.2017.1414199
27. Park M, Fudjack S, Soucie K, LaBelle O. Participant experiences in student recovery programs in Canada: an interpretative phenomenological analysis. Alcohol Treat Q. (2023) 41(3):338–61. doi: 10.1080/07347324.2023.2204819
28. Broman MJ, Pasman E, Brown S, Resko SM. Barriers and facilitators to recovery among college students without access to a collegiate recovery program. Drugs Educ Prev Policy. (2024):1–12. doi: 10.1080/09687637.2024.2415313
29. Terrion JL. The experience of post-secondary education for students in recovery from addiction to drugs or alcohol: relationships and recovery capital. J Soc Pers Relatsh. (2013) 30(1):3–23. doi: 10.1177/0265407512448276
30. Smith RL, Bannard T, McDaniel J, Aliev F, Brown A, Holliday E, et al. Characteristics of students participating in collegiate recovery programs and the impact of COVID-19: an updated national longitudinal study. Addict Res Theory. (2024) 32(1):58–67. doi: 10.1080/16066359.2023.2216459
31. Association of Recovery in Higher Education. Standards & recommendations for collegiate recovery programs. (2024). Available online at: https://collegiaterecovery.org/standards-recommendations/ (Accessed March 27, 2025).
32. Vest N, Reinstra M, Timko C, Kelly J, Humphreys K. College programming for students in addiction recovery: a PRISMA-guided scoping review. Addict Behav. (2021) 121:106992. doi: 10.1016/j.addbeh.2021.106992
33. Laudet AB, Harris K, Kimball T, Winters KC, Moberg DP. Characteristics of students participating in collegiate recovery programs: a national survey. J Subst Abuse Treat. (2015) 51:38–46. doi: 10.1016/j.jsat.2014.11.004
34. National Center for Education Statistics. Fast facts: Educational institutions. (2022). Available online at: https://nces.ed.gov/fastfacts/display.asp?id=1122 (Accessed March 27, 2025).
35. Association of Recovery in Higher Education. CRPs-CRCs. (2025). Available online at: https://collegiaterecovery.org/crps-crcs/ (Accessed March 27, 2025).
36. Blount TN, LaGuardia AC, Fitzpatrick DC. African American women’s substance use recovery experiences: a phenomenological inquiry. Couns Val. (2021) 66(1):92–110. doi: 10.1002/cvj.12146
37. Jason LA, Guerrero M, Bobak T, Light JM, Stoolmiller M. Reducing health disparities among black individuals in the post-treatment environment. J Ethn Subst Abuse. (2022) 21(4):1452–67. doi: 10.1080/15332640.2020.1861497
38. Pouille A, Bellaert L, Vander Laenen F, Vanderplasschen W. Recovery capital among migrants and ethnic minorities in recovery from problem substance use: an analysis of lived experiences. Int J Environ Res Public Health. (2021) 18(24):13025. doi: 10.3390/ijerph182413025
39. Wagner EF, Baldwin JA. Recovery in special emphasis populations. Alcohol Res Curr Rev. (2020) 40(3):05. doi: 10.35946/arcr.v40.3.05
40. Abreu Minero V, Best D, Brown L, Patton D, Vanderplasschen W. Differences in addiction and recovery gains according to gender—gender barriers and specific differences in overall strengths growth. Subst Abuse Treat Prev Policy. (2022) 17(1):21. doi: 10.1186/s13011-022-00444-8
41. Bormann NL, Weber AN, Miskle B, Arndt S, Lynch AC. Sex differences in recovery capital gains post-incarceration. Subst Use Misuse. (2023) 58(14):1839–46. doi: 10.1080/10826084.2023.2257303
42. Haik AK, Greene MC, Bergman BG, Abry AW, Kelly JF. Recovery among sexual minorities in the United States population: prevalence, characteristics, quality of life and functioning compared with heterosexual majority. Drug Alcohol Depend. (2022) 232:109290. doi: 10.1016/j.drugalcdep.2022.109290
43. Kelly JF, Greene MC, Bergman BG. Beyond abstinence: changes in indices of quality of life with time in recovery in a nationally representative sample of U.S. Adults. Alcohol Clin Exp Res. (2018) 42(4):770–80. doi: 10.1111/acer.13604
44. Knapp KS, Knapp JB, Bowen EA. Recovery capital profiles among a heterogeneous sample of individuals in recovery from alcohol problems. Psychol Addict Behav. (2024) 38(8):901–10. doi: 10.1037/adb0001031
45. Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, White WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend. (2017) 181:162–9. doi: 10.1016/j.drugalcdep.2017.09.028
46. Vilsaint CL, Hoffman LA, Kelly JF. Perceived discrimination in addiction recovery: assessing the prevalence, nature, and correlates using a novel measure in a U.S. National sample. Drug Alcohol Depend. (2020) 206:107667. doi: 10.1016/j.drugalcdep.2019.107667
47. Pozzar R, Hammer MJ, Underhill-Blazey M, Wright AA, Tulsky JA, Hong F, et al. Threats of bots and other bad actors to data quality following research participant recruitment through social media: cross-sectional questionnaire. J Med Internet Res. (2020) 22(10):e23021. doi: 10.2196/23021
48. Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. (2002) 32(6):959–76. doi: 10.1017/S0033291702006074
49. Idiculla TB, Eisen SV. The BASIS-24 behavior and symptom identification scale. Integrating Sci Pract. (2012) 2(2):16–9.
50. Rehr TI, Regan EP, Abukar Z, Meshelemiah JCA. Financial wellness of first-generation college students. Coll Stud Aff J. (2022) 40(1):90–105. doi: 10.1353/csj.2022.0007
51. Bowen E, Irish A, Wilding G, LaBarre C, Capozziello N, Nochajski T, et al. Development and psychometric properties of the multidimensional inventory of recovery capital (MIRC). Drug Alcohol Depend. (2023) 247:109875. doi: 10.1016/j.drugalcdep.2023.109875
52. Enders CK. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosom Med. (2006) 68(3):427–36. doi: 10.1097/01.psy.0000221275.75056.d8
53. Cook RD, Weisberg S. Residuals and Influence in Regression. 1st ed. New York: Chapman and Hall (1982).
54. Hennessy EA, Nichols LM, Brown TB, Tanner-Smith EE. Advancing the science of evaluating collegiate recovery program processes and outcomes: a recovery capital perspective. Eval Program Plann. (2022) 91:102057. doi: 10.1016/j.evalprogplan.2022.102057
55. Hennessy EA, Tanner-Smith EE, Nichols LM, Brown TB, Mcculloch BJ. A multi-site study of emerging adults in collegiate recovery programs at public institutions. Soc Sci Med. (2021) 278:113955. doi: 10.1016/j.socscimed.2021.113955
56. Bunaciu A, Bliuc AM, Best D, Hennessy EA, Belanger MJ, Benwell CSY. Measuring recovery capital for people recovering from alcohol and drug addiction: a systematic review. Addict Res Theory. (2024) 32(3):225–36. doi: 10.1080/16066359.2023.2245323
57. Association of Recovery in Higher Education. FAQ. (2025). Available online at: https://collegiaterecovery.org/faq/ (Accessed March 27, 2025).
Keywords: recovery capital, students in recovery, collegiate recovery, substance use recovery, collegiate recovery programs, needs assessment
Citation: Broman MJ, Acharya J, Bowen EA, Pasman E, Marks E, Kuentzel JG and Resko SM (2025) Promoting recovery capital among college students in recovery on a campus developing a collegiate recovery program. Front. Adolesc. Med. 3:1602144. doi: 10.3389/fradm.2025.1602144
Received: 28 March 2025; Accepted: 17 June 2025;
Published: 30 June 2025.
Edited by:
Jo-Hanna H Ivers, Trinity Biomedical Sciences Institute, IrelandReviewed by:
Emily A. Hennessy, Massachusetts General Hospital and Harvard Medical School, United StatesSharynne Hamilton, University of Western Australia, Australia
Copyright: © 2025 Broman, Acharya, Bowen, Pasman, Marks, Kuentzel and Resko. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael J. Broman, YnJvbWFuLjZAb3N1LmVkdQ==
 Michael J. Broman
Michael J. Broman Jhuma Acharya1
Jhuma Acharya1 Jeffrey G. Kuentzel
Jeffrey G. Kuentzel