- 1Department of Human Development, California State University, Long Beach, CA, United States
- 2School of Social Work, Portland State University, Portland, OR, United States
Background: Though past research has identified links between higher weight status and substance use in young adulthood, prospective studies are scarce and mixed, the role of higher weight status on vaping is less clear, and little empirical work has examined differences between obesity vs. overweight on poly-substance use. The current study assessed the role of weight status on poly-substance use trajectories across young adulthood.
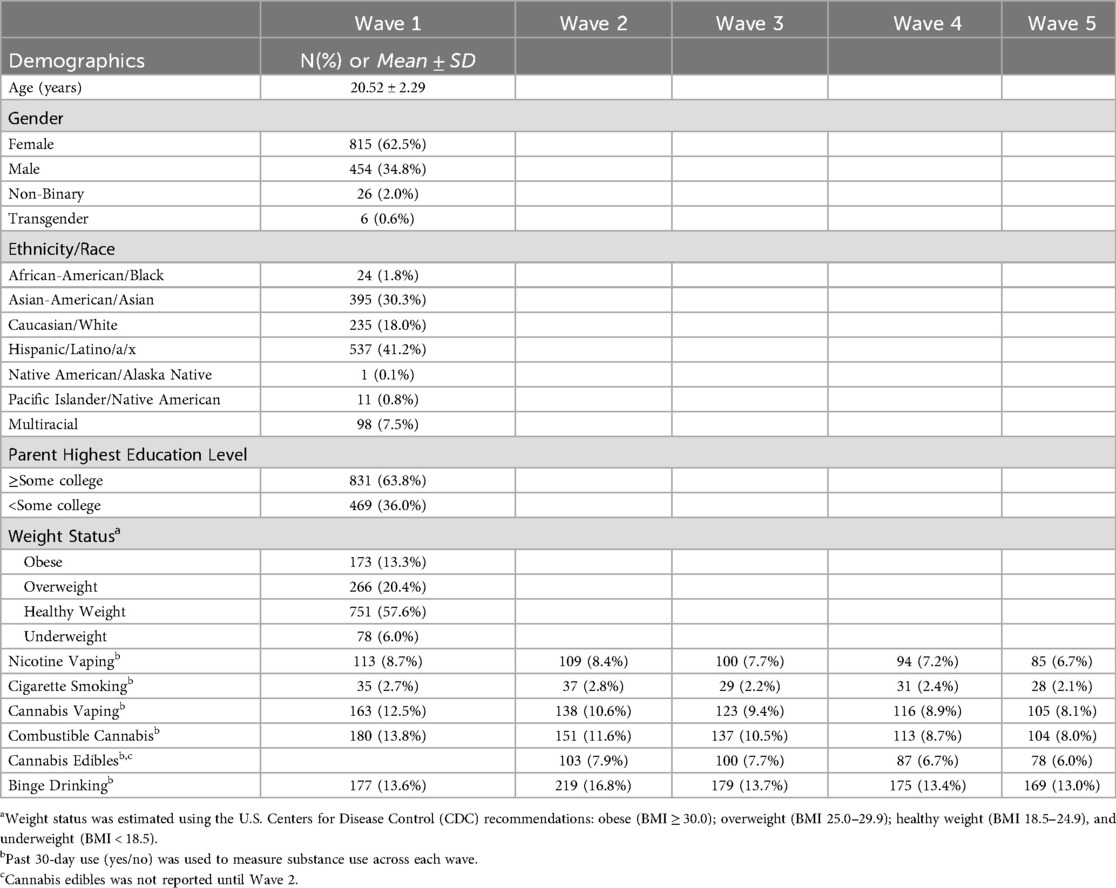
Methods: 1,303 young adults (20.5 ± 2.3 years; 63% female; 41% Latina/o/x, 30% Asian-American/Asian, 18% Caucasian/White) from a public, urban university were surveyed at six-month intervals from spring 2021 (W1) to spring 2023 (W5). Weight status was measured at W1 with body mass index (BMI) and categorized into obese (BMI ≥ 30.0); overweight (BMI 25.0–29.9); healthy weight (BMI 18.5–24.9); and underweight (BMI < 18.5). Past 30-day use of nicotine vaping, cigarette smoking, cannabis vaping, combustible cannabis, cannabis edibles, and binge drinking across waves were used to identify poly-substance use trajectories with parallel growth mixture modeling (PGMM).
Results: Four trajectories were identified: Nicotine/Tobacco Users and Binge Drinkers (7.2%); Poly-Users (9.8%); Moderate Cannabis Users and Binge Drinkers (18.7%); and Non-Users (64.3%). Obese young adults (vs. healthy weight) had lower odds of belonging to the Nicotine/Tobacco Users and Binge Drinkers trajectory [aOR = .24(.06-.99)] vs. Non-Users trajectory. Overweight young adults (vs. healthy weight) had higher odds of belonging to the Moderate Cannabis Users and Binge Drinkers trajectory [aOR = 1.94(1.25–3.03)] vs. Non-Users trajectory.
Conclusions: Overweight young adults' higher odds vs. obese young adults' lower odds of belonging to poly-substance use trajectories suggest overweight young adults may be a key target group for poly-use public health initiatives. Poly-substance use differences between obese and overweight status indicate a greater need for specificity when evaluating relationships between higher weight status and substance use.
1 Introduction
Obesity and poly-substance use are viewed as major public health concerns in young adulthood, as they are both linked to pervasive negative physical health outcomes, including earlier mortality risk, cancers, organ damage/failure, and cardiovascular illnesses (1–4), as well as mental health impairments (5–7). Among U.S. young adults, recent estimates report obesity (body mass index ≥ 30.0) prevalence at 35.5% (8) and overweight (body mass index 25.0–29.9) at 24.8% (9). Substance use among young adults for nicotine/tobacco (8.5% past 30-day cigarette smoking; 17.2% past 30-day nicotine vaping), cannabis (28.8% past 30-day marijuana; 13.9% past 30-day cannabis vaping), and alcohol (30.5% past two-weeks binge drinking) remains problematic (10). In a systematic review evaluating substance use among young adults across 20 studies, de Jonge et al. (11) found that about one-half to two-thirds of young adults were classified into some type of poly-substance use class (often co-occurring alcohol and tobacco use classes measured with lifetime, past 12 months, or past 30-day use). Given the high prevalence in young adulthood and marked negative health outcomes associated with obesity and poly-substance use, a growing literature has sought to examine whether higher weight status and substance use significantly co-occur in young adulthood. Recent studies suggest higher weight status and substance use share underlying mechanisms, such as dysregulation in similar brain reward pathways, depressive symptoms, and socio-contextual factors, which may contribute to their co-occurrence (12–14). Previous empirical work has reported both significant positive and negative associations between higher weight status and substance use (15–17). Significant gaps remain that limit our ability to know whether higher weight status is a predictor of poly-substance use in young adulthood. This study sought to address some of the current limitations of the literature by assessing the role of weight status on poly-substance use (nicotine/tobacco, cannabis, binge drinking) trajectories in young adulthood.
1.1 Prospective studies on higher weight status and poly-substance use
Prospective studies evaluating the role of higher weight status on poly-substance use are scarce. Available studies evaluating associations between higher weight status and different forms of substance use (including nicotine/tobacco, cannabis, and alcohol) have generally indicated positive associations between higher weight status and nicotine/tobacco use but not with cannabis or alcohol use. For example, earlier work using a nationally representative sample reported that obese or overweight vs. non-obese or overweight adolescents had a higher likelihood of belonging to a regular cigarette smoker class in young adulthood, but not to other substance use classes comprised of alcohol or cannabis use (18). Later using a sample of college students, Lanza et al. (19) found that obese vs. non-obese status predicted higher likelihood of belonging to a dual cigarette/e-cigarette latent class, but again not to classes characterized by alcohol or cannabis use. In a community-based sample, Gearhardt et al. (20) indicated that obesity status predicted less problematic alcohol and illicit drug use vs. those in the normal weight category; however, nicotine dependence was significantly higher among obese and normal weight vs. overweight groups. The established relationship between nicotine and appetite suppression (21) may partly explain the positive association between higher weight status and nicotine/tobacco use; both adolescents and young adults frequently report using cigarette smoking and nicotine vaping as a weight management tool (22, 23). Even across different populations (community and college samples), ages (emerging adults <26 years and young adults 18–29 years), substance use indicators (e.g., nicotine dependence vs. past 30-day use), and time between weight status and substance use assessment (six months, adolescence to young adulthood), the link between obesity and nicotine/tobacco vs. other substances in young adulthood is fairly consistent. However, a closer look at differences between higher weight categories (obese vs. overweight) on substance use is less clear, which may be a result of some of these methodological differences.
1.2 Obesity vs. overweight status on substance use
Beyond the limited number of prospective studies assessing the relationship between higher weight status and poly-substance use, the current literature also has paid little attention to evaluating whether belonging to different higher weight status categories (obese vs. overweight) increases or decreases risk of substance use in young adulthood. Using CDC guidelines to classify obese and overweight status based on body mass index (BMI), a person is considered overweight if their BMI is between 25.0 to 29.9 and obese if their BMI is greater than or equal to 30.0 (https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/). Though there is speculation that an inverse U-shaped relationship between BMI and substance use may exist (24), where overweight status may increase the likelihood of substance use compared to obesity status, an U-shaped relationship, particularly between BMI and nicotine/tobacco use, has also shown that obese smokers have greater frequency of use and nicotine dependence than non-obese smokers (25, 26). To add to the complexity of the relationship, most conceptual models on weight status and substance use date prior to the popularity of nicotine and cannabis vaping as well. Currently, only a few prospective studies have compared obese and overweight groups on substance use outcomes. Findings point to significant differential relationships, albeit with mixed results. In a prospective cohort study of college students, Lanza et al. (12) found that overweight status predicted higher likelihood of combustible cannabis use and binge drinking, whereas obese status predicted lower likelihood of nicotine vaping. In a population-based study of adolescents, Lee et al. (27), reported that BMI trajectories characterized by overweight or obesity status (e.g., “overweight early increasing”, “obesity stable”) predicted higher likelihood of cigarette use, but only BMI trajectories characterized by overweight (“overweight late increasing”, “overweight increasing then decreasing”) predicted higher likelihood of e-cigarette use. As noted earlier, Gearhardt's et al.'s (20) study using a community-based sample reported lower likelihood of problematic alcohol and illicit drug use among obese vs. normal weight groups, but a higher likelihood of nicotine dependence (smoking) among obese and normal weight groups compared to the overweight group.
Additional prospective studies are warranted to elucidate the relationship between obese vs. overweight status and substance use in young adulthood. Moreover, a focus on poly-substance use analyses that simultaneously includes nicotine/tobacco (cigarette smoking, nicotine vaping), cannabis (combustible cannabis, cannabis vaping), and alcohol (binge drinking) use is likely to inform previous mixed findings. Along with the utility of using prospective studies to identify differences between weight status categories on poly-substance use, closer consideration to the methods used across these studies may inform why mixed findings exist. The present dearth of research precludes knowing whether obese vs. overweight young adults would benefit from different approaches to substance use prevention and intervention. The implications for identifying overweight status as a predictor of poly-substance use are notable. Though obese status receives greater focus and resources across research, healthcare utilization, and public health policy compared to overweight status (28, 29), overweight status is significantly linked to similar physical [e.g., Type II diabetes, cancers, cardiovascular disease; (30, 31)] and mental (32, 33) health diseases and impairments as obese status. Building on past evidence suggesting overweight status is associated with substance use in ways that are different from obesity may help garner more attention and resources to a significant proportion of young adults.
1.3 The current study
Limitations on our knowledge regarding the role of higher weight status on substance use in young adulthood are three-fold: (1) there are a lack of prospective studies evaluating the risk of weight status on poly-substance use; (2) little empirical work has assessed differences between obese vs. overweight young adults on substance use; and (3) the role of obese vs. overweight status on poly-substance use trajectories is unclear. To address these limitations, the current study used data from a prospective cohort of young adults in college (five assessments across a two-year period; 2021–2023) to identify poly-substance trajectories (including nicotine vaping, cigarette smoking, cannabis vaping, combustible cannabis, and binge drinking) and assess whether weight status categories (obesity, overweight, underweight, healthy weight) predicted poly-substance use trajectories. Given the available evidence on weight status and poly-substance use in young adulthood (18, 20, 19), we expected obese status to predict higher likelihood of belonging to a trajectory class characterized by tobacco/nicotine use, but not cannabis use or binge drinking. The few prospective studies assessing differential associations between obese and overweight groups on substance use (12, 20, 27) led us to hypothesize that there would be differences in poly-substance use trajectory membership between obese and overweight groups, though specific differences were not predicted due to past mixed findings. A greater understanding of the relationship between weight status and poly-substance use in young adulthood will be beneficial for informing public health efforts aimed at combating two of the most critical public health issues facing young adults today—substance use and obesity/overweight.
2 Methods
2.1 Participants and procedure
Participants were 1,303 young adults from a prospective cohort study conducted at a large, urban public university in Southern California. With close to two-thirds (61.4%) of U.S. high school graduates attending college (34), and evidence that undergraduates are at high risk for both poly-substance use and obesity (35, 36), college students are an increasingly valuable population for understanding development of co-occurring health-risk behaviors. During Spring 2021, 93 classes were randomly selected for participant recruitment from all undergraduate classes with meeting times. Of the 93 randomly selected classes, 67 (72.0%) instructors agreed to a 10-minute class recruitment visit. Class visits (which took place online due to COVID-19 restrictions) were conducted by the PI from late January to late April 2021. Following the study presentation, eligible (≥18 years, currently enrolled undergraduate) and interested participants were able to review the informed consent online. Once a student completed and submitted the informed consent form online, the PI individually emailed the participant an online survey link and unique verification code. Participants completed a 15 min health behavior survey that included questions on eating habits, exercise, weight status, substance use, mood, personality, and social relationships; surveys were completed in spring 2021 and then at six-month intervals (fall 2021, spring 2022, fall 2022, and spring 2023). To avoid identifying information being collected within the survey, the unique verification code was used to link a participant's survey with their informed consent. Participants received a $15 Amazon e-giftcard for each survey. All study protocol was approved by the California State University, Long Beach Institutional Review Board.
Of 2,651 students targeted in 67 randomly selected classes, 1,361 students (51.3%) participated in the study. Participants between 18 and 29 years at baseline (spring 2021) were selected for current study analyses (N = 1,303; 95.7% of total sample). Retention rates among the analytic sample were: 1,085 (83.3%) at six-month follow-up; 982 (75.4%) at one-year follow-up; 890 (68.3%) at 18-month follow-up; and 888 (68.2%) at two-year follow-up. The average age of participants was M = 20.52 (SD = 2.29) years. The sample closely aligned with the gender and race/ethnicity composition of the institution's undergraduate population. Participants in the sample included (university 2020–2021 academic year statistics in parentheses): 62.5% (59.4%) female, 34.8% (40.6%) male; 2.5% transgender or gender variant/non-binary/non-conforming; 41.2% (47.9%) Hispanic/Latino/a/x, 30.3% (25.3%) Asian-American/Asian, 18.0% (16.1%) Caucasian/White, 1.8% (3.7%) African-American/Black, 7.5% (4.6%) Multiracial; 0.8% (0.2%) Pacific Islander/Native Hawaiian, and 0.1% (0.1%) Native American/Alaskan Native. About two-thirds (63.8%) reported their parents attended some college or a higher level of education.
3 Measures
3.1 Weight status
Participants self-reported height and weight at baseline (Wave 1), which was used to calculate body mass index (BMI; weight(lbs)/[height(in)2 × 703). Based on U.S. Centers for Disease Control (CDC) recommendations (https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/), participants were categorized into one of four weight status categories: obese (BMI ≥ 30.0); overweight (BMI 25.0–29.9); healthy weight (BMI 18.5–24.9); and underweight (BMI < 18.5). Dummy coding for the multinomial weight status variable was created with healthy weight as the reference category (obese vs. healthy weight, overweight vs. healthy weight, underweight vs. healthy weight).
3.2 Substance use
Past 30-day use of nicotine vaping, cigarette smoking, cannabis vaping, combustible cannabis, cannabis edibles, and binge drinking were assessed with participant self-report at each wave, from spring 2021 (W1) to spring 2023 (W5). The exception was cannabis edibles, which was not measured until fall 2021 (W2). Questions were derived from the National Institute of Drug Abuse (NIDA) Clinical Trials Network Tobacco, Alcohol, Prescription Medications, and Substance Use/Misuse (TAPS) assessment, which validated substance use questions on an adult population-based sample (37), as well as the Health & Happiness Study, a population-based prospective cohort study of adolescents and young adults in Southern California that has published vast studies on youth tobacco/nicotine and cannabis use (38, 39). For each type of substance, participants were first asked about lifetime use: “Have you ever used a vaporizer to vape nicotine (e.g., Puff Bar, JUUL, Box mod)?”; “Have you ever smoked a cigarette?”; “Have you ever used a vaporizer to vape cannabis (e.g., Pax Era, Heavy Hitters, Dosist, Kandypens)?”; “Have you ever smoked cannabis (marijuana, weed, pot)?”; “Have you ever consumed a cannabis (marijuana) edible?”; “Have you ever consumed more than 5 alcoholic drinks in one sitting (if you are a man) or 4 alcoholic drinks in one sitting (if you are a woman)?”. If participants reported lifetime use for a specific substance, they were asked a corresponding question on past 30-day use: (e.g., “In the past 30 days have you vaped nicotine?”; “In the past 30 days have you consumed a cannabis edible?”). Dichotomous variables for past 30-day use (past 30-day use vs. no past 30-day use) were created for each substance use product at each wave.
3.3 Sociodemographic covariates
Age, gender, race/ethnicity, and parent highest education were self-reported at baseline. Participants reported their age (in years), gender (female, male, transgender female, transgender male, gender variant/non-binary/non-conforming), race/ethnicity (African-American/Black, Asian-American/Asian, Caucasian/White, Hispanic/Latino/a/x, Native American/Alaskan Native, Pacific Islander/Native Hawaiian, Multi-racial, and other), and highest parent education (less than some high school, some high school, graduated from high school, some college, graduated from college, earned graduate degree). Gender was recoded as male vs. non-male (instead of male vs. female) to include all participants, including transgender and non-binary, in analyses. Race/ethnicity was recoded into dummy variables (Asian American/Asian vs. non-Asian American/Asian) for racial/ethnic groups representing ≥10% of the sample (89.2% of the total sample was comprised of Hispanic/Latino/a/x: 41.4%, Asian American/Asian: 29.6%; and Caucasian/White: 18.2%). Highest parent education was recoded into a dichotomous variable (≥some college vs. <some college).
3.4 Analysis plan
We used parallel process growth mixture modeling (PGMM) to estimate poly-substance use trajectories. Each substance use product was simultaneously modeled as a unique growth process producing 3 growth factors (i.e., intercept, linear and quadratic slopes [rate of change across the five time points, (40, 41)]. The model estimated trajectory groups based on covariation across the six distinct sets of growth factors (i.e., one set of growth factors—intercept, linear, quadratic—per product, 18 total factors). GMM uses a data-driven approach to estimate trajectory classes; classes are not identified a priori but rather derived from the unobserved heterogeneity in the population. An increasing number of trajectory classes were estimated until an optimal model was identified using statistical fit indices, including the Bayesian Information Criterion [BIC; (42)] and Lo-Mendell Rubin Likelihood Ratio Test [LMR LRT; (43)], as well as class interpretation and parsimony. Full information maximum likelihood was used to account for missing data. Covariates of identified trajectories were evaluated within the PGMM framework using a validated 3-step approach to account for classification error (44). After the best fitting class model was chosen, a most likely latent class variable was created using the latent class posterior probabilities. Logits reflecting the classification uncertainty rate were applied to account for measurement error in the most likely class variable. The most likely class variable was then used to assess covariates of trajectory membership. Analyses were conducted with Mplus 8.11 (45).
4 Results
4.1 Descriptive statistics
Table 1 presents demographic characteristics and weight status at Wave 1, as well as past 30-day substance use prevalence at each wave. Just over a half of participants were classified as healthy weight (57.6%). A third of the sample were obese (13.3%) or overweight (20.4%); 6.0% were underweight. Across all waves, binge drinking had the highest past 30-day prevalence (13.0%-16.8%) while cigarette smoking had the lowest past 30-day prevalence (2.1%–2.8%).
4.2 Substance use trajectories
4.2.1 Model selection
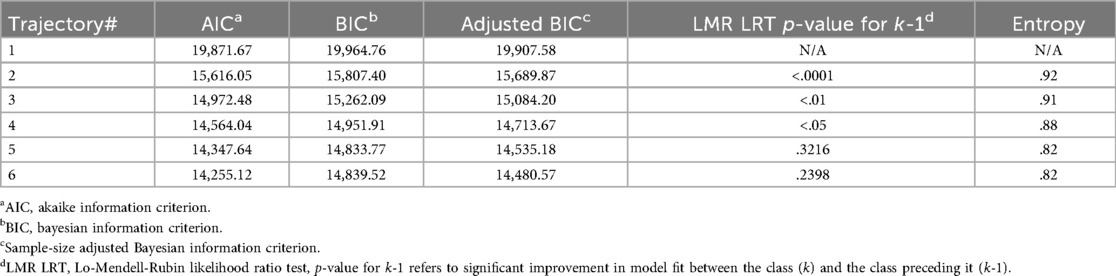
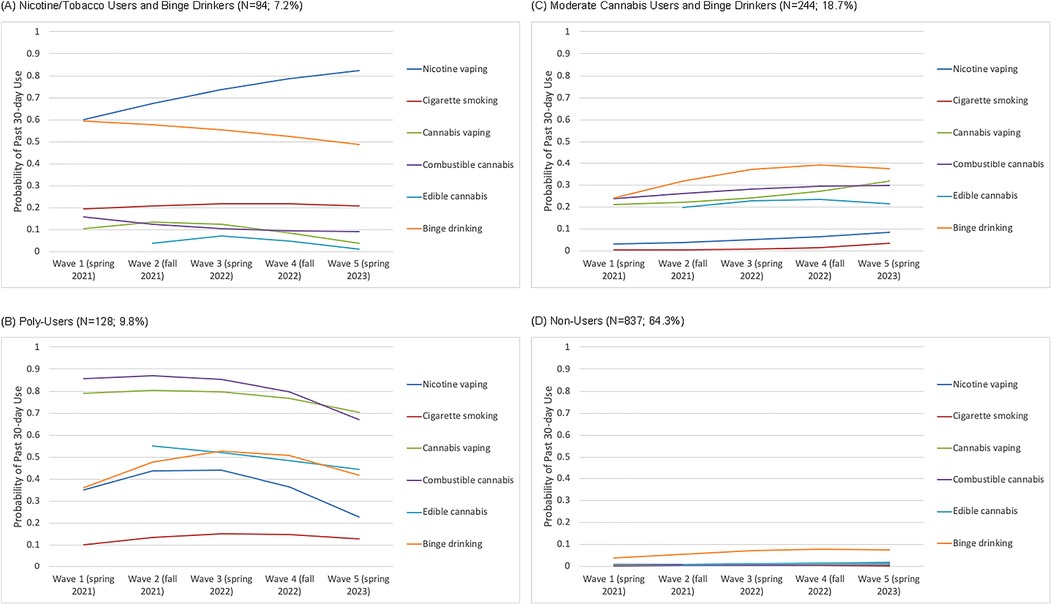
Model fit was evaluated across an increasing number of trajectory classes. Based on statistical indices (Table 2), class interpretability, and parsimony, the four-class model was identified as best-fitting the data. The LMR LRT indicated that the four-class model was ideal; the LMR LRT was not significant past the five-class solution. Although the four-class model did not have the lowest BIC or adjusted-BIC values, the BIC values leveled off between the three- and four-class models. This leveling-off, along with consideration of class interpretation (distinct and homogenous classes) and parsimony, resulted in identifying the four-class model as optimal. Figure 1 presents the probability of past 30-day use of each substance use product for each identified trajectory.
4.2.2 Identified trajectories
The Nicotine/Tobacco Users and Binge Drinkers trajectory (7.2%) was characterized by relatively high probability of nicotine/tobacco use and binge drinking, but low probability of cannabis use (Figure 1A). Nicotine vaping probabilities across waves (60.0%–82.5%), as well as binge drinking (48.7%–59.4%) were prominent. Comparatively, cigarette smoking probabilities were low across waves (19.3%–21.8%), but still higher within this trajectory than any other trajectory class.
The Poly-Users trajectory (9.8%) reflected high probability of use for various tobacco/nicotine and cannabis products, as well as binge drinking across waves (Figure 1B). Probability of use was highest for combustible cannabis (67.1%–86.9%) and cannabis vaping (70.2%–80.5%) across waves. Edible cannabis remained at about 45%–55% across the study period. A significant quadratic decrease was identified for both binge drinking (quadratic = −.14, p < .01) and nicotine vaping (quadratic = −.17, p < .01). Binge drinking increased from Wave 1 (36.2%) to Waves 2 (47.6%) and 3 (52.6%), but then decreased at Waves 4 (50.6%) and 5 (41.8%). Similarly, nicotine vaping increased from Wave 1 (35.0%) to Waves 2 (43.7%) and 3 (44.2%), but then decreased at Waves 4 (36.4%) and 5 (22.6%). Cigarette smoking probability was lower than other substance use products and held stable across waves (10.1%–15.1%).
The Moderate Cannabis Users and Binge Drinkers trajectory (18.7%) was characterized by moderate probability of cannabis use and binge drinking and low probability of tobacco/nicotine use (Figure 1C). Probability of all cannabis products (vaping, combustible, edible) ranged between 20%-32% across waves. Binge drinking probability was slightly higher; a significant rate of change (slope = .46, p < .05) was found for binge drinking across waves (24.0%–39.0%). Probability of nicotine vaping and cigarette smoking was relatively low (<10%) across waves.
Non-Users (64.3%) comprised the largest trajectory class. This trajectory was comprised of no or very low substance use across waves (Figure 1D). Probability of tobacco/nicotine use and cannabis use was negligible across waves (<2%). Binge drinking probability was also low (<8%) across waves; a significant rate of change (slope = .49, p < .05) was found for binge drinking across waves (3.7%–7.6%).
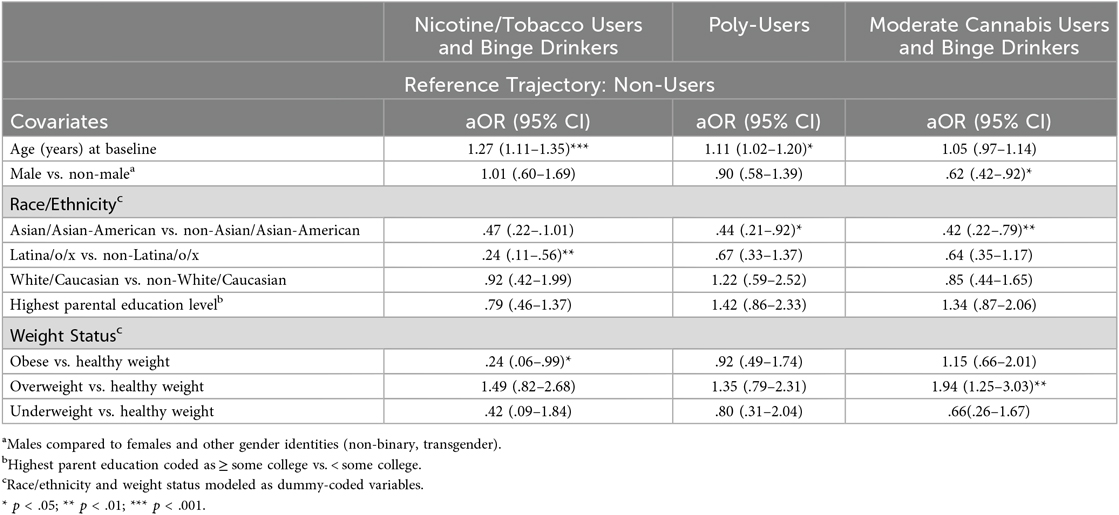
4.3 Correlates of substance use trajectories
Sociodemographic and weight status covariates were added to the parallel process GMM to determine the odds of trajectory membership in each of the three substance-using trajectories vs. the Non-Users trajectory (Table 3). Obese young adults (vs. healthy weight) had lower odds of belonging to the Nicotine/Tobacco Users and Binge Drinkers trajectory [aOR = .24(.06–.99)] vs. Non-Users trajectory. Overweight young adults (vs. healthy weight) had higher odds of belonging to the Moderate Cannabis Users and Binge Drinkers trajectory [aOR = 1.94(1.25–3.03)] vs. Non-Users trajectory. Underweight status was not a significant covariate of any poly-substance use trajectory.
Older participants had higher odds of belonging to the Nicotine/Tobacco Users and Binge Drinkers [aOR = 1.27(1.11–1.35)] and Poly-Users [aOR = 1.11(1.02–1.20)] trajectories vs. the Non-Users trajectory. Males had lower odds of belonging to the Moderate Cannabis Users and Binge Drinkers trajectory [aOR = .62(.42–.92)] vs. the Non-Users trajectory. Asian/Asian-American young adults had lower odds of belonging to the Poly-Users [aOR = .44(.21–.92)] and Moderate Cannabis Users and Binge Drinkers [aOR = .42(.22–.79)] trajectories compared to the Non-Users trajectory. Latina/o/x young adults had lower odds of belonging to the Nicotine/Tobacco Users and Binge Drinkers trajectory [aOR = .24(.11–.56)] vs. the Non-Users trajectory.
5 Discussion
The current study advanced understanding of the relationship between weight status and poly-substance use during young adulthood by identifying trajectories of tobacco/nicotine, cannabis, and alcohol poly-use and assessing the role of weight status on trajectory membership. All three identified substance-using trajectories (Nicotine/Tobacco Users and Binge Drinkers, Poly-users, Moderate Cannabis Users and Binge Drinkers) were characterized by some form of poly-use, highlighting the importance of integrative substance use approaches for prevention and intervention during this critical developmental period for substance use. Compared to healthy weight status, obesity status predicted lower, not higher, odds of belonging to a substance-using trajectory (Nicotine/Tobacco Users and Binge Drinkers). On the other hand, overweight status (vs. healthy weight) predicted higher odds of belonging to a substance-using trajectory (Moderate Cannabis Users and Binge Drinkers). The marked difference between obese and overweight young adults' risk of poly-substance use suggests greater specificity is needed when evaluating the relationship of higher weight status on substance use.
Using a parallel approach to GMM, this study identified four distinct underlying subpopulations of tobacco/nicotine, cannabis, and alcohol use: (1) Non-Users (64.3%); (2) Moderate Cannabis Users and Binge Drinkers (18.7%); (3) Poly-Users (9.8%); and (4) Tobacco/Nicotine Users and Binge Drinkers (7.2%). These developmental patterns indicate a significant proportion of young adults in this study—close to 40%—engaged in some form of poly-substance use. This proportion of poly-substance use is in line with de Jonge et al.'s (11) systematic review that reported one-half to two-thirds of young adults were engaged in poly-use. It is notable that all three poly-substance use trajectories were characterized by a high probability of binge drinking. Though current binge drinking prevalence remains high among young adults [30.5%; (10)], the rise of novelty tobacco/nicotine and cannabis products (nicotine vaping, cannabis vaping, cannabis edibles, etc.) and significant attention paid to ever-evolving tobacco/nicotine and cannabis legislative policies (e.g., e-cigarette flavor bans, cannabis legalization) has potentially undermined public health concerns related to young adult binge drinking. This is concerning as recent studies, including systematic reviews and meta-analyses, show young adult binge drinking is linked to structural and functional abnormalities in brain regions involved in self-regulation and reward processing, which increases the likelihood of risky sexual behavior, poly-substance use, and interpersonal violence (46–49). Overall, the current study finds that focus on poly-substance use vs. single-substance use is warranted to prevent problematic substance use patterns in young adults.
In addition to addressing gaps in the young adult substance use literature related to longitudinal measurement of poly-use involving tobacco/nicotine, cannabis, and binge drinking, a key aim of the study was to add to the small but burgeoning knowledge base on the role weight status plays on substance use in young adulthood. Though our hypothesis that obese vs. healthy weight young adults would have a higher likelihood of belonging to tobacco/nicotine-using trajectories was based on past studies indicating obesity status predicted tobacco/nicotine use in young adulthood (18–20), the lack of prospective studies, especially on nicotine vaping, makes the unexpected finding that obese status (vs. healthy weight) predicted lower likelihood of belonging to the Nicotine/Tobacco Users and Binge Drinkers vs. Non-Users trajectory less surprising. Moreover, the finding that overweight vs. healthy weight young adults had a higher likelihood of belonging to the Moderate Cannabis Users and Binge Drinkers vs. Non-Users trajectory suggests overweight young adults may be a key target group for anti-cannabis and binge drinking public health initiatives. There is already some evidence indicating overweight young adults are vulnerable to combustible cannabis and binge drinking (12). Though this study lends some evidence for the inverse U-shaped relationship between weight status and substance use posited by Amiri and Behnezhad (24), it is important to note underweight vs. healthy weight was not associated with higher or lower risk of poly-substance use. The notable differences between obese and overweight young adults suggest greater specificity is needed when evaluating relationships between weight status and substance use.
Obese and overweight young adults' differential poly-substance use risk suggest obese vs. overweight categories have distinct shared underlying mechanisms with poly-substance use. For example, different socio-environmental contexts between obese and overweight young adults may explain why overweight young adults were at higher risk of poly-substance use vs. healthy weight young adults, but obese young adults were not. Overweight young adults may have an easier time than obese young adults socializing with peers, but their vulnerability to being socially excluded may influence greater risk of poly-substance use to appear cool and engaged in what they believe is the normative peer social context (50). It is also possible that a significant proportion of overweight young adults in this study recently shifted from healthy to unhealthy weight status, as increased weight is a common experience among college students (51). Potentially these overweight young adults may be engaging in poly-substance use as a coping mechanism in response to recent body weight increases (52–54). Conversely, obese young adults' opportunities to engage in poly-substance use, which often take place at social events with peers during the college years (55, 56) may be more limited because obese young adults face greater challenges (e.g., social stigma, marginalization) participating in social and recreational activities compared to overweight young adults (57, 58). Moreover, it is possible that the food-drug competition hypothesis (20, 59, 60) played a role in obese young adults' lower risk of poly-substance use compared to healthy weight peers. Obese individuals' greater vulnerability towards over-eating compared to other weight categories (61) may protect against poly-substance use as the neural reward pathways shared by food and drugs are saturated with over-eating behaviors.
The current study also used a sample that was largely racial/ethnic minority (82.0%) and female (62.5%), which may explain differences with previous studies evaluating race/ethnicity and gender across poly-substance use trajectories. Unlike two recent studies indicating White vs. non-White participants had higher odds of belonging to a poly-substance use vs. a non-users trajectory (62, 78), this study did not find Caucasian/White (vs. non-Caucasian/White) young adults at higher risk of membership in a poly-substance use vs. non-users trajectory. A lower likelihood of Asian/Asian-American vs. non-Asian/Asian-American young adults belonging to the Poly-Users and Moderate Cannabis Users and Binge Drinkers vs. Non-Users trajectory corroborates Cho et al.'s (63) study that showed Asian (vs. Hispanic) adolescents had lower odds of belonging to an early initiation poly-use trajectory (vs. non-users). We also found that Latina/o/x vs. non-Latina/o/x young adults had lower odds of belonging to the Nicotine/Tobacco and Binge Drinkers vs. Non-Users trajectory. Males vs. non-males lower odds of belonging to the Moderate Cannabis Users and Binge Drinkers vs. Non-Users trajectory aligns with a past finding indicating males vs. females had lower odds of belonging to a Young Adult-Onset Poly-Substance/Poly-Product Users vs. non-users trajectory (64), though another poly-substance trajectory study reported males (vs. females) had a higher likelihood of belonging to a poly-substance use trajectory vs. non-users trajectory, as well as earlier vs. later poly-use (65). Potentially the higher risk of overweight and obesity status among Latina/o/xs and females, and lower risk among Asian/Asian-Americans (36, 66, 67) may have contributed to the racial/ethnic and gender differences observed in this sample, which was predominately Asian/Asian-American, Latina/o/x and female.
Of course, limitations of this study need to be considered when drawing conclusions. The use of a sample specific to Southern California limits generalizability of findings to other regions; however, a regionally-specific sample increases the likelihood that participants were exposed to similar tobacco/nicotine, cannabis, and alcohol regulatory policies and trends during assessment. The sample attrition rate grew across timepoints and was close to one-third at the conclusion of the study; however, full information maximum likelihood enabled participants with at least one wave of data to be analyzed. Though the study relied on self-report of past 30-day substance use, self-report remains the most common method of measuring substance use behaviors. In addition, we recognize that measuring substance use with a binary (yes/no) indicator compared to frequency of use did not allow us to determine whether poly-substance use trajectory classes reflect problematic use. The study also relied on self-reported vs. directly measured BMI. Although directly measured vs. self-reported height and weight is ideal, past research has indicated that self-reported BMI has high concordance with directly measured BMI among adolescents and young adults (68–70). That said, we recognize that BMI, whether directly measured or self-reported, is not as accurate an indicator as anthropometric measures (e.g., visceral adiposity, waist circumference, skinfold thickness) for evaluating healthy vs. unhealthy status (70, 79, 80), and additional research on this topic using anthropometric measures is needed. Moreover, only weight status at baseline was included in the analysis; thus, we do not know the impact between acute vs. chronic higher weight status. Additionally, though most prospective studies among adolescent and young adult populations have focused on the pathway from higher weight status to substance use, there is evidence that substance use, specifically cigarette smoking and binge drinking, predict higher BMI, overweight, and obese status in adolescents and young adults (71–74). Future research assessing bidirectional associations between poly-substance use and weight status is warranted to further inform the underlying pathways to co-occurring substance use and weight status health-risks among young adults. We also note that our proxy for SES, parent education, did not allow for more meaningful interpretations of the role SES has on poly-substance use trajectories. Additionally, we did not consider hypothesized underlying mechanisms of both weight status and substance use, such as depressive symptoms, social context, and biobehavioral markers of shared reward pathways (12–14). Though our primary aim in the current study was addressing gaps in the literature related to the use of prospective studies, poly-substance use measures, and comparison of weight status categories, moving forward with the current findings can inform which underlying processes may best explain the significant associations identified.
Despite these limitations, this study advances knowledge on the relationship between weight status and substance use by identifying distinct differences between higher weight status categories' risk of poly-substance use trajectories in young adulthood. Obese and overweight young adults, often viewed as more similar than different in relation to physical and psychosocial consequences, reported unique associations with substance use. Overweight (vs. healthy weight) young adults had a higher likelihood of belonging to a Moderate Cannabis Users and Binge Drinkers vs. Non-users trajectory, whereas obese (vs. healthy weight) young adults unexpectedly had a lower likelihood of belonging to a Tobacco/Nicotine Users and Binge Drinkers vs. Non-users trajectory. The findings highlight a need to better understand the epidemiological distinctions between obese and overweight young adults' poly-substance use. A more nuanced view of the role weight status plays on substance use in young adulthood is likely to improve current efforts to reduce co-occurring health-risks earlier in the lifespan. Though obese status earns significantly more research and clinical attention than overweight status, overweight young adults' greater risk of poly-substance use compared to healthy weight peers suggests they may be a key target group for anti-poly-substance use public health initiatives. Moving forward, identifying underlying risk processes and pathways linking overweight to poly-substance use in young adulthood, which may involve an interaction between peer context and internalizing symptoms different from obese young adults, is warranted. Additionally, the significant proportion of poly-substance use vs. single-substance use observed in this study indicates poly-substance use may be the normative pattern of tobacco/nicotine, cannabis, and binge drinking among young adults. Greater attention to developing comprehensive, integrative approaches to substance use health services that reflect the high prevalence of poly-substance use is critical moving forward, especially as young adults engaged in poly-substance use are at greater risk of deleterious health outcomes compared to single-substance users, including cognitive deficits, mental health impairments, and greater substance dependence (75–77). Further research on the determinants and health consequences of poly-substance use is warranted to not only understand key targets for intervention, but also policy priorities for reducing poly-substance use in young adulthood.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board, California State University, Long Beach. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HL: Visualization, Resources, Formal analysis, Funding acquisition, Project administration, Writing – original draft, Validation, Data curation, Investigation, Supervision, Conceptualization, Methodology, Writing – review & editing. KW: Writing – review & editing, Writing – original draft. LS: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the National Institute of General Medical Sciences of the National Institutes of Health (SC3GM125548). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bendor CD, Bardugo A, Pinhas-Hamiel O, Afek A, Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. (2020) 19:1–14. doi: 10.1186/s12933-020-01052-1
2. Choi K, Inoue-Choi M, McNeel TS, Freedman ND. Mortality risks associated with dual–and poly–tobacco-product use in the United States. Am J Epidemiol. (2022) 191(3):397–401. doi: 10.1093/aje/kwz143
3. Piano MR, Mazzuco A, Kang M, Phillips SA. Cardiovascular consequences of binge drinking: an integrative review with implications for advocacy, policy, and research. Alcohol Clin Exp Res. (2017) 41(3):487–96. doi: 10.1111/acer.13329
4. Preston SH, Vierboom YC, Stokes A. The role of obesity in exceptionally slow US mortality improvement. Proc Natl Acad Sci USA. (2018) 115(5):957–61. doi: 10.1073/pnas.1716802115
5. Baral A, Hanna F, Chimoriya R, Rana K. Cannabis use and its impact on mental health in youth in Australia and the United States: a scoping review. Epidemiologia. (2024) 5(1):106–21. doi: 10.3390/epidemiologia5010007
6. Chu DT, Nguyet NTM, Nga VT, Lien NVT, Vo DD, Lien N, et al. An update on obesity: mental consequences and psychological interventions. Diabetes Metab Syndr Clin Res Rev. (2019) 13(1):155–60. doi: 10.1016/j.dsx.2018.07.015
7. Kang W, Malvaso A. Understanding the longitudinal associations between e- cigarette use and general mental health, social dysfunction and anhedonia, depression and anxiety, and loss of confidence in a sample from the UK: a linear mixed effect examination. J Affect Disord. (2024) 346:200–5. doi: 10.1016/j.jad.2023.11.013
8. Emmerich SD, Fryar CD, Stierman B, Ogden CL. Obesity and Severe Obesity Prevalence in Adults: United States, August 2021–August 2023. Hyattsville, MA: NCHS (2024). (NCHS Data Brief No. 508 September 2024).
9. Ellison-Barnes A, Johnson S, Gudzune K. Trends in obesity prevalence among adults aged 18 through 25 years, 1976–2018. JAMA. (2021) 326(20):2073–4. doi: 10.1001/jama.2021.16685
10. Patrick ME, Miech RA, Johnston LD, O’Malley PM. Monitoring the Future Panel Study Annual Report: National Data on Substance use among Adults Ages 19 to 65, 1976–2023. Ann Arbor, MI: Institute for Social Research, University of Michigan (2024).
11. de Jonge MC, Bukman AJ, van Leeuwen L, Onrust SA, Kleinjan M. Latent classes of substance use in young adults–a systematic review. Subst Use Misuse. (2022) 57(5):769–85. doi: 10.1080/10826084.2022.2040029
12. Lanza HI, Orozco M, Motlagh G. Differential associations between weight status (obesity, overweight, underweight) and substance use in young adulthood. Subst Use Misuse. (2022) 57:1663–72. doi: 10.1080/10826084.2022.2107670
13. Saules KK, Carr MM, Herb KM. Overeating, overweight, and substance use: what is the connection? Curr Addict Rep. (2018) 5(2):232–42. doi: 10.1007/s40429-018-0208-9
14. Volkow N, Wang GJ, Fowler JS, Tomasi D, Baler R. Food and drug reward: overlapping circuits in human obesity and addiction. Brain Imaging Behav Neurosci. (2011) 11:1–24. doi: 10.1007/7854_2011_169
15. Daw J, Margolis R, Wright L. Emerging adulthood, emergent health lifestyles: sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. J Health Soc Behav. (2017) 58(2):181–97. doi: 10.1177/0022146517702421
16. Merrill RM. A national survey of marijuana use among US adults according to obesity status, 2016–2022. Cannabis Cannabinoid Res. (2024). doi: 10.1089/can.2024.0069
17. Smith CE, O’Neil PM. Prevalence of obesity among electronic cigarette and tobacco users in the United States: results from the 2018 wave of the behavioral risk factor surveillance system. Subst Use Misuse. (2024) 59(10):1481–7. doi: 10.1080/10826084.2024.2354787
18. Lanza HI, Grella CE, Chung PJ. Does adolescent weight status predict problematic substance use patterns? Am J Health Behav. (2014) 38(5):708–16. doi: 10.5993/AJHB.38.5.8
19. Lanza HI, Pittman P, Batshoun J. Obesity and cigarette smoking: extending the link to e-cigarette/vaping use. Am J Health Behav. (2017) 41(3):338–47. doi: 10.5993/AJHB.41.3.13
20. Gearhardt AN, Waller R, Jester JM, Hyde LW, Zucker RA. Body mass index across adolescence and substance use problems in early adulthood. Psychol Addict Behav. (2018) 32(3):309. doi: 10.1037/adb0000365
21. Audrain-McGovern J, Benowitz NL. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. (2011) 90(1):164–8. doi: 10.1038/clpt.2011.105
22. Mason TB, Leventhal AM. Weight status and effects of non-tobacco flavors on e- cigarette product appeal. Subst Use Misuse. (2021) 56(6):848–53. doi: 10.1080/10826084.2021.1899229
23. Morean ME, Wedel AV. Vaping to lose weight: predictors of adult e-cigarette use for weight loss or control. Addict Behav. (2017) 66:55–9. doi: 10.1016/j.addbeh.2016.10.022
24. Amiri S, Behnezhad S. Obesity and substance use: a systematic review and meta- analysis. Obesity Medicine. (2018) 11:31–41. doi: 10.1016/j.obmed.2018.06.002
25. Carreras-Torres R, Johansson M, Haycock PC, Relton CL, Smith GD, Brennan P, et al. Role of obesity in smoking behaviour: Mendelian randomization study in UK biobank. Br Med J. (2018) 361:k1767. doi: 10.1136/bmj.k1767
26. Rupprecht LE, Donny EC, Sved AF. Obese smokers as a potential subpopulation of risk in tobacco reduction policy. Yale J Biol Med. (2015) 88(3):289–94. Available online at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4553649/26339212
27. Lee DS, Tackett AP, Naya C, Harlow AF, Mason TB. Trajectories of body mass index and combustible and electronic cigarette use across adolescence: findings from the PATH study. Addict Behav. (2024) 149:107901. doi: 10.1016/j.addbeh.2023.107901
28. Lehnert T, Sonntag D, Konnopka A, Riedel-Heller S, König HH. Economic costs of overweight and obesity. Best Pract Res Clin Endocrinol Metab. (2013) 27(2):105–15. doi: 10.1016/j.beem.2013.01.002
29. Spieker EA, Pyzocha N. Economic impact of obesity. Prim Care Clin Off Pract. (2016) 43(1):83–95. doi: 10.1016/j.pop.2015.08.013
30. Ganz ML, Wintfeld N, Li Q, Alas V, Langer J, Hammer M. The association of body mass index with the risk of type 2 diabetes: a case–control study nested in an electronic health records system in the United States. Diabetol Metab Syndr. (2014) 6(1):50. doi: 10.1186/1758-5996-6-50
31. Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. (2009) 9(1):88. doi: 10.1186/1471-2458-9-88
32. Amiri S, Behnezhad S. Obesity and anxiety symptoms: a systematic review and meta-analysis. Neuropsychiatr. (2019) 33(2):72–89. doi: 10.1007/s40211-019-0302-9
33. Pereira-Miranda E, Costa PR, Queiroz VA, Pereira-Santos M, Santana ML. Overweight and obesity associated with higher depression prevalence in adults: a systematic review and meta-analysis. J Am Coll Nutr. (2017) 36(3):223–33. doi: 10.1080/07315724.2016.1261053
34. U.S. Bureau of Labor Statistics. College Enrollment and Work Activity of Recent High School and College Graduates Summary—2023 (Report no. USDL-24-0742). U.S. Department of Labor (2024). Available online at: https://www.bls.gov/news.release/hsgec.nr0.htm (Accessed June 18, 2025).
35. Willis E, Adams R, Keene J. If everyone is doing it, it must be safe: college students’ development of attitudes toward poly-substance use. Subst Use Misuse. (2019) 54(11):1886–93. doi: 10.1080/10826084.2019.1618334
36. Sa J, Cho BY, Chaput JP, Chung J, Choe S, Gazmararian JA, et al. Sex and racial/ethnic differences in the prevalence of overweight and obesity among US college students, 2011–2015. J Am Coll Health. (2021) 69(4):413–21. doi: 10.1080/07448481.2019.1679814
37. Wu LT, McNeely J, Subramaniam GA, Sharma G, VanVeldhuisen P, Schwartz RP. Design of the NIDA clinical trials network validation study of tobacco, alcohol, prescription medications, and substance use/misuse (TAPS) tool. Contemp Clin Trials. (2016) 50:90–7. doi: 10.1016/j.cct.2016.07.013
38. Han DH, Cho J, Vogel EA, Harlow AF, Tackett AP, Eckel SP, et al. Longitudinal transitions between use of combustible, noncombustible, and multiple cannabis products from adolescence to young adulthood and intersections with nicotine use. Am J Epidemiol. (2024) 193(4):617–25. doi: 10.1093/aje/kwad230
39. Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, et al. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. (2015) 314(7):700–7. doi: 10.1001/jama.2015.8950
40. Muthén BO. Beyond SEM: general latent variable modeling. Behaviormetrika. (2002) 29:81–117. doi: 10.2333/bhmk.29.81
41. Wu J, Witkiewitz K, McMahon RJ, Dodge KA, Conduct Problems Prevention Research Group. A parallel process growth mixture model of conduct problems and substance use with risky sexual behavior. Drug Alcohol Depend. (2010) 111(3):207–14. doi: 10.1016/j.drugalcdep.2010.04.013
42. Schwartz G. Estimating the dimension of the model. Ann Stat. (1978) 6:461–4. Available online at: https://www.jstor.org/stable/2958889
43. Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. (2001) 88:767–78. doi: 10.1093/biomet/88.3.767
44. Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using Mplus. Struct Equ Model. (2014) 21:329–41. doi: 10.1080/10705511.2014.915181
46. Cho HS, Yang Y. Relationship between alcohol consumption and risky sexual behaviors among adolescents and young adults: a meta-analysis. Int J Public Health. (2023) 68:1605669. doi: 10.3389/ijph.2023.1605669
47. Parks MJ, Maggs JL, Patrick ME. Daily fluctuations in drinking intensity: links with vaping and combustible use of nicotine and marijuana. Drug Alcohol Depend. (2022) 233:109347. doi: 10.1016/j.drugalcdep.2022.109347
48. Pérez-García JM, Suárez-Suárez S, Doallo S, Cadaveira F. Effects of binge drinking during adolescence and emerging adulthood on the brain: a systematic review of neuroimaging studies. Neurosci Biobehav Rev. (2022) 137:104637. doi: 10.1016/j.neubiorev.2022.104637
49. Savage J, Rossler M. Binge drinking and violence in the transition to adulthood. Aggress Behav. (2023) 49(5):480–91. doi: 10.1002/ab.22084
50. Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity. (2008) 16(10):2205–11. doi: 10.1038/oby.2008.365
51. Vadeboncoeur C, Townsend N, Foster C. A meta-analysis of weight gain in first year university students: is freshman 15 a myth? BMC Obes. (2015) 2(1):1–9. doi: 10.1186/s40608-015-0051-7
52. Bennett BL, Pokhrel P. Weight concerns and use of cigarettes and e-cigarettes among young adults. Int J Environ Res Public Health. (2018) 15(6):1084. doi: 10.3390/ijerph15061084
53. Espinosa A, Ruglass LM, Conway FN, Jackson KM, White HR. Motives, frequency, and consequences of cannabis use among college students. J Drug Issues. (2022) 53:61–78. doi: 10.1177/00220426221093608
54. Krieger H, Young CM, Anthenien AM, Neighbors C. The epidemiology of binge drinking among college-age individuals in the United States. Alcohol Res Curr Rev. (2018) 39(1):23–30. doi: 10.35946/arcr.v39.1.05
55. Beard SJ, Yoon L, Venticinque JS, Shepherd NE, Guyer AE. The brain in social context: a systematic review of substance use and social processing from adolescence to young adulthood. Dev Cogn Neurosci. (2022) 57:101147. doi: 10.1016/j.dcn.2022.101147
56. Gunn RL, Sokolovsky A, Stevens AK, Hayes K, Fitzpatrick S, White HR, et al. Contextual influences on simultaneous alcohol and cannabis use in a predominately white sample of college students. Psychol Addict Behav. (2021) 35(6):691. doi: 10.1037/adb0000739
57. Cheng HL, Medlow S, Steinbeck K. The health consequences of obesity in young adulthood. Curr Obes Rep. (2016) 5:30–7. doi: 10.1007/s13679-016-0190-2
58. Puhl RM, Lessard LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep. (2020) 9:402–11. doi: 10.1007/s13679-020-00408-8
59. Cummings JR, Ray LA, Tomiyama AJ. Food–alcohol competition: as young females eat more food, do they drink less alcohol? J Health Psychol. (2017) 22(5):674–83. doi: 10.1177/1359105315611955
60. Kleiner KD, Gold MS, Frostpineda K, Lenzbrunsman B, Perri MG, Jacobs WS. Body mass index and alcohol use. J Addict Dis. (2004) 23(3):105–18. doi: 10.1300/J069v23n03_08
61. Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE. Food-related impulsivity in obesity and binge eating disorder–a systematic review. Obes Rev. (2013) 14(6):477–95. doi: 10.1111/obr.12017
62. Tucker JS, Rodriguez A, Dunbar MS, Pedersen ER, Davis JP, Shih RA, et al. Cannabis and tobacco use and co-use: trajectories and correlates from early adolescence to emerging adulthood. Drug Alcohol Depend. (2019) 204:107499. doi: 10.1016/j.drugalcdep.2019.06.004
63. Cho J, Goldenson NI, Kirkpatrick MG, Barrington-Trimis JL, Pang RD, Leventhal AM. Developmental patterns of tobacco product and cannabis use initiation in high school. Addiction. (2021) 116(2):382–93. doi: 10.1111/add.15161
64. Lanza HI. Weighing the risk: developmental pathways and processes underlying obesity to substance use in adolescence. J Res Adolesc. (2022) 32(1):337–54. doi: 10.1111/jora.12610
65. Richmond-Rakerd LS, Fleming KA, Slutske WS. Investigating progression in substance use initiation using a discrete-time multiple event process survival mixture (MEPSUM) approach. Clin Psychol Sci. (2016) 4(2):167–82. doi: 10.1177/2167702615587457
66. Cooper AJ, Gupta SR, Moustafa AF, Chao AM. Sex/gender differences in obesity prevalence, comorbidities, and treatment. Curr Obes Rep. (2021) 10(4):458–66. doi: 10.1007/s13679-021-00453-x
67. Gupta RD, Chakraborty PA, Al Kibria GM. Racial/ethnic disparities in prevalence and trends of obesity, grade 3 obesity, and abdominal obesity among US adults, 2003–18. Obes Med. (2021) 28:100372. doi: 10.1016/j.obmed.2021.100372
68. Davies A, Wellard-Cole L, Rangan A, Allman-Farinelli M. Validity of self-reported weight and height for BMI classification: a cross-sectional study among young adults. Nutrition. (2020) 71:110622. doi: 10.1016/j.nut.2019.110622
69. Lipsky LM, Haynie DL, Hill C, Nansel TR, Li K, Liu D, et al. Accuracy of self-reported height, weight, and BMI over time in emerging adults. Am J Prev Med. (2019) 56(6):860–8. doi: 10.1016/j.amepre.2019.01.004
70. Wu Y, Li D, Vermund SH. Advantages and limitations of the body mass index (BMI) to assess adult obesity. Int J Environ Res Public Health. (2024) 21(6):757. doi: 10.3390/ijerph21060757
71. Fazzino TL, Fleming K, Sher KJ, Sullivan DK, Befort C. Heavy drinking in young adulthood increases risk of transitioning to obesity. Am J Prev Med. (2017) 53(2):169–75. doi: 10.1016/j.amepre.2017.02.007
72. Huang DY, Lanza HI, Anglin MD. Association between adolescent substance use and obesity in young adulthood: a group-based dual trajectory analysis. Addict Behav. (2013) 38(11):2653–60. doi: 10.1016/j.addbeh.2013.06.024
73. McCarty CA, Kosterman R, Mason WA, McCauley E, Hawkins JD, Herrenkohl TI, et al. Longitudinal associations among depression, obesity and alcohol use disorders in young adulthood. Gen Hosp Psychiatry. (2009) 31(5):442–50. doi: 10.1016/j.genhosppsych.2009.05.013
74. Pasch KE, Velazquez CE, Cance JD, Moe SG, Lytle LA. Youth substance use and body composition: does risk in one area predict risk in the other? J Youth Adolesc. (2012) 41:14–26. doi: 10.1007/s10964-011-9706-y
75. Bourgault Z, Rubin-Kahana DS, Hassan AN, Sanches M, Le Foll B. Multiple substance use disorders and self-reported cognitive function in US adults: associations and sex-differences in a nationally representative sample. Front Psychiatry. (2022) 12:797578. doi: 10.3389/fpsyt.2021.797578
76. Connor JP, Gullo MJ, White A, Kelly AB. Polysubstance use: diagnostic challenges, patterns of use and health. Curr Opin Psychiatry. (2014) 27(4):269–75. doi: 10.1097/YCO.0000000000000069
77. Yang Y. Suicidal thoughts and behaviors among US adolescents: the cumulative effects of polysubstance use behaviors. Subst Use Misuse. (2024) 59(13):1930–7. doi: 10.1080/10826084.2024.2392504
78. Lanza HI, Bello MS, Cho J, Barrington-Trimis JL, McConnell R, Braymiller JL, et al. Tobacco and cannabis poly-substance and poly-product use trajectories across adolescence and young adulthood. Prev Med. (2021) 148:106545. doi: 10.1016/j.ypmed.2021.106545
79. Camhi SM, Bray GA, Bouchard C, Greenway FL, Johnson WD, Newton RL, et al. The relationship of waist circumference and BMI to visceral, subcutaneous, and total body fat: sex and race differences. Obesity. (2011) 19(2):402–8. doi: 10.1038/oby.2010.248
Keywords: binge drinking, cannabis/marijuana, obesity, overweight, poly-substance use, tobacco/nicotine, vaping
Citation: Lanza HI, Waller K and Sevillano L (2025) Obesity vs. overweight status: differential predictions to poly-substance use in young adulthood. Front. Adolesc. Med. 3:1657086. doi: 10.3389/fradm.2025.1657086
Received: 30 June 2025; Accepted: 13 October 2025;
Published: 30 October 2025.
Edited by:
Tammy Chung, The State University of New Jersey, United StatesReviewed by:
Jasmina Burdzovic Andreas, Norwegian Institute of Public Health (NIPH), NorwayLogan Fields, Arcadia University, United States
Copyright: © 2025 Lanza, Waller and Sevillano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: H. Isabella Lanza, aXNhYmVsbGEubGFuemFAY3N1bGIuZWR1
 H. Isabella Lanza
H. Isabella Lanza Kailey Waller1
Kailey Waller1 Lalaine Sevillano
Lalaine Sevillano