- 1Department of Pediatrics, The Warren Alpert Medical School of Brown University, Providence, RI, United States
- 2Division of Pediatric Endocrinology and Diabetes, Department of Pediatrics, Hasbro Children's Hospital,, Brown University Health, Providence, RI, United States
- 3Brown University Health BERDI (Biostatistics, Epidemiology, Research Design, Informatics), Providence, RI, United States
- 4Department of Psychiatry and Human Behavior, The Warren Alpert Medical School of Brown University, Providence, RI, United States
- 5Weight Control and Diabetes Research Center, The Miriam Hospital, The Warren Alpert Medical School of Brown University, Providence, RI, United States
- 6Bradley-Hasbro Children’s Research Center, Hasbro Children’s, Brown University Health, Providence, RI, United States
Introduction: Obesity in childhood and adolescence continues to be a major public health challenge. Mindfulness-based interventions (MBIs) can be great adjuvants to multidisciplinary weight management interventions for adolescents. Delivery of MBI via mobile phones can decrease barriers to engagement. Mindfulness increases present-moment awareness, which may promote self-regulation, which is in turn important for weight management. Several studies have shown that delivering mindfulness training for adolescents via mobile devices may be feasible and acceptable, but this is still a growing area of research. The Unified Theory of Acceptance and Use of Technology (UTAUT) is a framework that has been used to understand why individuals choose to use health apps. This study aims to gather adolescent perceptions about an existing mindful eating mobile app designed for adults, via mixed methods research, and to utilize their feedback to design and develop a mindful eating app for adolescents.
Methods: This was a cross-sectional, mixed methods study. Twenty-five adolescents, 13–17 years old, with a BMI ≥ 85th percentile completed a UTAUT-based survey and a semi-structured interview after viewing excerpts from an existing mindful eating mobile app.
Results: Adolescents with overweight/obesity are receptive to using a mindful eating app, with some concerns about Effort Expectancy and Self-Efficacy. Youth endorse that such an app should have reminders, short and colorful videos with captions, and it should be engaging, relatable, and non-judgmental. This information was used to develop a mindful-eating web-based app for adolescents, SAMBA (Study of an Adolescent Mindfulness-Based App).
Conclusions: We developed a mindful eating web-based app for adolescents utilizing feedback from this youth cohort using an existing mobile app as the starting point. Future directions include pilot testing the app and its content.
1 Introduction
Obesity, which affects 1 in 5 children and adolescents in the US, is associated with increased morbidity and mortality (1, 2). Standard treatment for obesity involves Intensive Health Behavior and Lifestyle Treatment. However, weight loss maintenance remains a challenge, with most interventions followed by significant relapse (3, 4). Strategies to improve weight maintenance include interventions that teach maintenance skills such as self-regulation (5) or extending the length of treatment, which is costly and may benefit from using digital tools as a novel strategy (6).
The practice of mindfulness, which promotes purposeful and nonjudgmental awareness of the present moment, was first introduced to the Western medical field in 1985 by Jon Kabat-Zinn (7, 8). Mindfulness-based interventions (MBI) can enhance multidisciplinary pediatric weight management programs (9). MBIs address the underlying behavioral mechanisms for maladaptive eating (10–12); they support self-regulation for weight loss by reducing habitual eating patterns (emotional eating, external eating), and can improve self-awareness and self-acceptance (10). Adolescents are particularly susceptible to self-regulation challenges and are more likely to eat in response to internal (emotional) and/or external (environmental) cues, as opposed to physiologic hunger and satiety cues (11). MBIs have shown to be acceptable and feasible for children and adolescents with or without parental involvement (13, 14). Recent research has found that MBIs may prevent or improve childhood obesity (15, 16), as well as improve eating behaviors and body image acceptance among children and adolescents (17–20). Furthermore, recent meta-analyses have found that MBIs can be effective for improving youth mental health and well-being (21, 22).
Mindful eating is the practice of bringing present moment intentional awareness and acceptance (mindfulness) to eating-related thoughts, emotions, bodily sensations, and behaviors (23, 24). Mindful eating involves several practices including 1) paying attention to the sensory properties of food, 2) paying attention to bodily hunger and satiety cues (which has overlap with intuitive eating), 3) observing and accepting food-related thoughts and cravings in a non-judgmental way, noticing that they are separate from the self, and how they occur in response to internal or external triggers (25). Mindful eating interventions may help patients improve their relationships with food by disrupting habit loops of maladaptive eating behaviors (10, 26). Mindful eating programs may reduce emotional and external eating among patients with overweight or obesity (27). Even a brief mindful eating program has been shown to lead to less impulsive food choices (28). For youth with obesity, these programs have been shown to improve mindful eating, food cravings and weight control (29).
A study of an MBI on mindful eating and resilience found the program to be feasible and acceptable among schoolchildren and their parents (30). Furthermore, research suggests that MBIs specifically focused on eating behaviors, delivered in clinical settings, may be effective for decreasing emotional eating (31). MBIs may improve eating behaviors and promote weight loss among adults with overweight and obesity, with a large effect on eating behaviors and a moderate effect size on psychological outcomes (anxiety) and body weight (12, 32–34). A randomized anti-obesity feasibility study among adolescent females suggested that a satiety-focused mindful eating intervention may reduce BMI among adolescent females with overweight or obesity (35). However, a recent meta-analysis suggested that the effect of MBI on improving BMI among children with overweight and obesity remains inconsistent and further research is needed (36). Digital tools offer innovative approaches to delivering health interventions to adolescents (37), especially as smartphone use is nearly universal within this population (38). Delivering MBIs via mobile phones may increase accessibility by overcoming barriers to accessing traditional interventions (39, 40). A study of a mindful eating intervention found that a family-based mindfulness-based cooking class could be feasible for youth with overweight and obesity, while also highlighting key barriers to participation, such as cost and busy schedules (41). Mobile interventions may be particularly beneficial for patients with financial, socioeconomic, and geographic barriers to participation in traditional mindfulness programs (42). A randomized trial found a mindful eating intervention for adolescents delivered via smartphones was feasible and efficacious (43). For adolescents, the development of successful mobile health apps requires a user-centered design approach that elicits user feedback through a combination of both quantitative and qualitative methods (44–48).
The Unified Theory of Acceptance and Use of Technology (UTAUT) model has been used widely to predict user acceptance and use of technology (49, 50). Semi-structured interviewing is a valuable tool for eliciting nuanced feedback about mobile health interventions (51, 52). Used jointly, the UTAUT and semi-structured interviews can provide important insight into the acceptance and adoption of mobile health apps (50). Recent research employing the UTAUT model and semi-structured interviews suggests that mobile apps can provide communicative support, reduce distress, and improve well-being and self-care in youth with chronic conditions or long-term illnesses (53, 54). The UTAUT model has been shown to explain a large percent of the variance in acceptance of digital health interventions among adults with obesity and to be helpful in designing consumer health technology to manage adolescent obesity (55, 56). Qualitative analysis from semi-structured interviews has been previously utilized to understand adolescent preferences during the development of mobile health applications for mental health (57) and obesity (58).
Research suggests that mobile health apps may benefit youth, including improving healthy eating habits and weight loss (59, 60); mindfulness-based apps, in particular, may improve awareness of weight-related behaviors in adolescents and young adults (61). Despite the success of mindful eating apps for individuals with obesity, many available apps could improve upon the domains of comprehensive information, engagement, and aesthetics (62); furthermore, very few have been specifically designed for adolescents (61). The Eat Right Now app® was developed by Judson Brewer (Mindfulness Center of Brown University), and was shown to reduce craving-related eating and over-eating behaviors and improve weight loss among adults (39, 63).
Given the lack of mindful eating apps for adolescents, and the evidence suggesting positive effects of mindful eating apps in adults and mobile health apps in this population, we aimed to develop a mindful eating app for adolescents. Using the Eat Right Now® app as a starting point, we aimed to understand the acceptability and feasibility of a mindful eating app for adolescents. In this study, we elicited adolescent feedback about this mindful eating app via the UTAUT and semi-structured interviews. Specifically, we used results of the UTAUT survey to gauge adolescent interest in a mindful eating app. Results from the semi-structured interviews, analyzed via Framework Matrix Analysis (FMA), provided real-time feedback for the development of a mindful eating app specifically for adolescents, the Study of an Adolescent Mindfulness-Based App (SAMBA). After creating this initial version of the SAMBA app, we further analyzed the qualitative data via applied thematic analysis (ATA), in order to provide depth to the UTAUT findings, and to identify additional user feedback for guiding future testing and iterations of the app.
2 Methods
2.1 Study design
This study was conducted at Hasbro Children's Hospital (Brown University Health) in Providence, RI from July 2022 to May 2023. Participants were recruited from the Pediatric Endocrinology Clinic and the Primary Care Clinic during their regular clinic appointments, by members of the research staff. A convergent mixed methods design was used, with survey and interview data collected concurrently. Data were analyzed independently, and then integrated to identify areas where qualitative themes explained, or expanded on the quantitative results.
2.2 Participants and eligibility
Participants were recruited from the Pediatric Endocrinology and Primary Care Clinics at Hasbro Children's Hospital. Participants were required to be 13–17 years old, have overweight or obesity (BMI for age/sex ≥ 85th percentile), speak English, and have daily access to a smartphone. Exclusion criteria included medical conditions that would preclude adherence to dietary recommendations (such as inflammatory bowel disease), genetic or endocrine causes of obesity, a diagnosis of type 1 or type 2 diabetes mellitus, severe developmental delay and/or serious cognitive impairment, current use of psychotropic medications which could affect weight, or being non-English-speaking.
Eligibility was determined via chart review by research staff and confirmed by discussion with the participant and their parent. All participants received compensation for their participation in the study.
2.3 Procedure
Informed consent and assent were obtained from all participants prior to the study visit. Each participant met with a member of the research team once over a HIPAA-compliant video platform. Demographic data, including age, school grade, sex, gender identity, race, ethnicity, type of health insurance, BMI (extracted from the Electronic Health Record), and technology use data, was collected in REDCap and de-identified.
Participants reported their current weight-related stage of change by selecting the statement that best described their current weight situation, based on the transtheoretical model for weight management (64): (1) At the moment, I am not doing anything to lose weight, and I have no intention about doing anything over the next 6 months; (2) At the moment, I am not doing anything to lose weight, but I am thinking about doing something over the next 6 months; (3) I have been making an effort to lose weight (by dieting and/or exercising) for less than 6 months; (4) I have been making an effort to maintain my weight (by dieting and/or exercising) for 6 months or more.
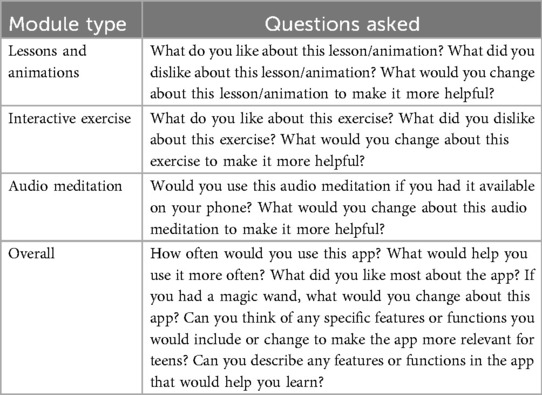
Based on subject enrollment order, participants were assigned to review (via videoconference) one of three different subsets of video lessons, video animations, and mindfulness exercises from a commercially available mindful eating application (Eat Right Now®), which was designed for and tested with adult participants (39). The goal of this grouping was to keep each interview time-limited and engaging. After playing the clip of each video lesson, video animation, or mindfulness exercise to the participant, the researcher conducted a short semi-structured interview to elicit participant opinions about the app, including likes and dislikes about app features, suggestions for change, and how to adapt the app for adolescents (Table 1). Interviews were audio-recorded, transcribed, and then reviewed for accuracy and appropriate deidentification.
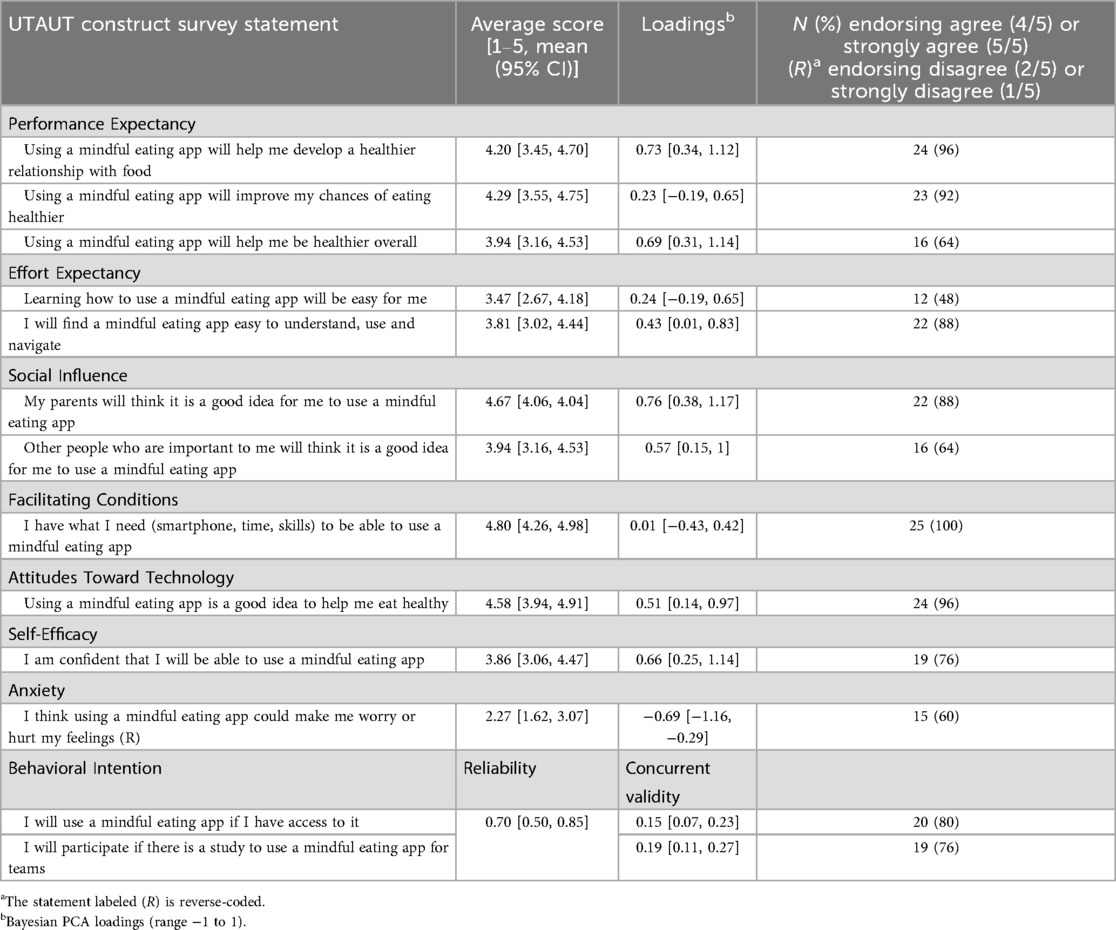
The study visit concluded with a survey that was developed by our group based on the Unified Theory of Acceptance and Use of Technology (UTAUT) constructs. Participants completed the survey online using REDCap electronic data capture tools hosted at Brown University Health (65). The survey included 13 statements, organized in eight constructs assessing Performance Expectancy, Effort Expectancy, Social Influence, Facilitating Conditions, Attitudes toward Technology, Self-Efficacy, Anxiety, and Behavioral Intention. Participants responded to each statement via a 5-point Likert scale (66). We analyzed average scores for each construct to determine participant perceptions of the app. We assessed the percent of participants that provided favorable ratings for each statement, a 4 or 5/5 (agree or strongly agree), or 1 or 2/5 (strongly disagree or disagree) for the Anxiety construct, which is reverse-coded. An a-priori benchmark of 80% of participants reporting favorable ratings was used to gauge acceptability.
Reliability and validity were also estimated for the UTAUT-based survey, using principal components analysis. Scale validation focuses on correlations. If the questions are all valid measures of the same underlying trait, in this case willingness to use technology for managing mindful eating, then participants who endorse high scores on one question should also endorse high scores on other questions as well– a pattern of positive correlations. Principal components analysis summarizes these correlations in a loading, denoted λ, which can be interpreted like a correlation between an individual question and all other questions on the questionnaire. Values close to 1 represent positive correlations with most other questions, values close to −1 represent generally negative correlations with other questions, and values close to 0 represent no association. This can be used to evaluate whether or not all questions are equally relevant to participant attitudes, which reflects internal structure validity. This provides information on how to interpret what scores represent, as well as which questions are most insightful to individual attitudes.
The values of the loadings were used to estimate reliability, interpreted as representing the percentage of total variation in scores that is meaningful. Reliability of 0.70, or 70% meaningful variation, is often considered acceptable. Lastly, the correlation between summed scores on the UTAUT and the two questions about Behavioral Intention was estimated to represent concurrent validity. If the UTAUT validly represents willingness to use a mindful eating app, then participants who endorse higher scores on the questionnaire will also endorse greater willingness to use the app when directly asked, a positive correlation. Using this approach allowed us to investigate this empirically. A Bayesian estimation procedure was used because the sample size is modest (N = 25 participants).
All data was de-identified before analysis.
2.4 Framework matrix & applied thematic analyses
Framework matrix analysis (FMA) and applied thematic analysis (ATA) were used to analyze qualitative data from the interview transcripts. Considering the time-consuming process of ATA in the context of app development (67), we conducted FMA first, as it provided real-time feedback for the design and initial development of our mindful eating web-based app (SAMBA). Together with the results from the UTAUT survey, which gauged adolescent interest in a mindful eating app, the results from the FMA of the interview transcripts informed the development of the initial version of the SAMBA app. Once app development was underway, we again analyzed the interview transcripts, via comprehensive ATA, to gain a more nuanced perspective on the app's successes and potential areas of improvement for future iterations of the app.
First, all 25 audio-recorded participant interviews were transcribed by members of the research team. Full review of the transcripts yielded inductive (based on the researcher's interests) and deductive (based on interview responses) FMA codes. A research assistant entered summaries of participants' comments, relevant quotes, and key decisions regarding app development into the framework matrix. After the framework matrix was built, matrix contents were reviewed by the principal investigator and deemed accurate and complete. Data helped inform app design and development (67).
After FMA was complete, we used the framework matrix to create a second codebook for ATA. Two coders reviewed the ATA codebook and independently coded the first transcripts, then met to review their coding, finalize the codebook and add additional inductive codes. With the finalized codebook, the two coders then independently coded all 25 transcripts. After the initial coding was completed, the two coders met to review 5 (20%) randomly selected transcripts to review codes and resolve discrepancies. The master coded transcripts were entered into NVivo software (version 14.0). Concordance was calculated at 90%, demonstrating a high consistency between the coders.
3 Results
3.1 Participant characteristics
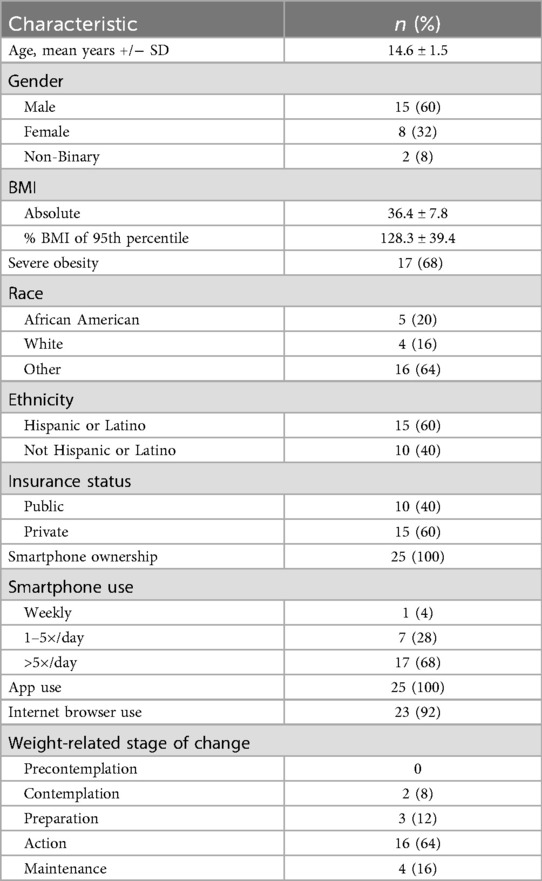
In total, 25 participants completed the research study, including providing demographic and technology use information, and completing the semi-structured interview and UTAUT questionnaire. Fifteen (60%) identified as male. In terms of race and ethnicity, 5 identified as African-American (20%), 4 identified as white (16%), and 15 (60%) identified as Hispanic or Latino. Seventeen (68%) had severe obesity, defined as a BMI percentile at ≥120% of the 95th percentile. All 25 participants reported owning a smartphone and using apps. Detailed demographic information is summarized in Table 2. When asked about their weight-related stage of change, 2 (8%) were contemplating changing their behaviors, 3 (12%) were preparing to change their behaviors, 16 (64%) were actively changing behaviors, and 4 (16%) were in the maintenance stage of behavior change.
3.2 Unified theory of acceptance and use of technology (UTAUT) survey
Findings from the UTAUT survey are summarized in Table 3. The Performance Expectancy, Social Influence, Facilitating Conditions, and Attitudes toward Technology constructs received average scores between 4 and 5/5, indicating that most participants responded “Agree”, or “Strongly Agree” to the questionnaire statements for these constructs. However, the Effort Expectancy and Self-Efficacy constructs had lower average scores, between 3 and 4. Over 80% of participants selected either “Agree” (4/5) or “Strongly Agree” (5/5) with at least one statement from each construct, including Behavioral Intention, with the exception of the Self-Efficacy construct. The Anxiety construct, which was reverse coded, received an average score of 2.27 [1.62, 3.07], indicating that most participants responded “Disagree” (2/5) or “Neither Agree nor Disagree” (3/5) to these statements. These results suggest that adolescents are motivated and think a mindful eating app would be helpful, but they may lack confidence in their ability to use it. Overall, the high levels of agreement for these constructs support the development of a mindful eating app for adolescents.
In terms of internal validity of the survey, the loadings (which range from −1 to 1) representing common association between an individual question and all other questions, were large (λ > 0.5) except for facilitating conditions (λ = 0.01). This is because all teens endorsed this question, which indicates it provides no meaningful information. The association with behavioral intention was positive [correlation > 0.15, 95% CI (0.07, 0.27)], which supports the validity of the survey, meaning that those who endorse the constructs say they would be more likely to use the app. Reliability was appropriate [0.70, 95% CI (0.50, 0.85)], suggesting that similar youth would get similar scores using this questionnaire.
3.3 Framework matrix analysis
FMA supported the findings from the survey in that participants overall were receptive to a mindful eating mobile app. It also pointed to additional app features that adolescents consider important, which were not present in the app that was presented to them during this study, as it was developed for an adult audience (39).
Analysis of inductive codes “attitude and tone” and “user flexibility” found that youth overall found the app relatable and encouraging; however, they disliked content containing moralizing language about food and weight. They also preferred the self-directed exercises that provided many choices.
Analysis of the deductive codes “easy to understand” and “educational” revealed that adolescents found the app educational and easy to understand. Analysis of the deductive codes “engaging” and “visually appealing,” contained mixed responses. While some youth found the app engaging, others wanted shorter videos, captioning, and more visual engagement. Similarly, while some youth found the app visually engaging, others provided suggestions to increase engagement, including text message reminders, introduction videos, gamification features, and teen-specific examples.
3.4 SAMBA app features guided by FMA findings
Given that adolescents disliked moralizing language about food and weight, we avoided the use of such language in the SAMBA app. The SAMBA app was designed to include directions for following certain exercises depending on each person's daily experience, and at their own pace, since adolescents preferred self-directed exercises that provided choices,
Youth preferences highlighted the need for shorter videos, captioning, and more visual engagement; SAMBA's lesson videos include captions, have an abundance of visual aids, and are shorter and more colorful than those in apps designed for adults, such as Eat Right Now®. We followed participants' suggestions to add customizable text reminders, and thus the SAMBA app sends five text reminders per week. We included two introduction videos that must be watched before the video lessons. We also included personalization features, including the opportunity to choose between two different characters who are wearing different clothes, have different gender and different body weight. In terms of gamification, the SAMBA app also allows participants to accrue experience points, XP, for their app use (i.e., completion of audio meditations, video lessons, mindful eating exercises). As their XP increase, youth progress through different experience levels based on their XP accrual: beginner, intermediate, advanced, and pro-mindful eater, and these levels are displayed on the main screen (Figure 1). For the pilot study to test the app, our plan is to offer prizes if participants accrue enough XP reflecting that they have used the app as intended. The app also includes teen-specific examples to increase engagement (i.e., the lesson videos include examples pertinent to school experiences, as opposed to work experiences which would match an adult audience).

Figure 1. Representation of SAMBA mindful eating app personalization features (choice of preferred character, Sam) and gamification features [accrual of XP (experience) points and completion of levels (i.e., Beginner Mindful Eater)]. As shown, SAMBA features colorful and engaging graphics throughout the app.
3.5 Applied thematic analysis
During review of the master coded transcripts, three themes emerged. These themes embodied the participants' opinions about the app's visual engagement and interactivity, ease of use, and the overall tone of the app.
3.5.1 Mindful eating apps should be engaging, interactive, and visually appealing
Many participants described the app's design as an important factor in their willingness to engage with an app. We identified where participants described the app as boring vs. engaging and visually appealing. In particular, participants described the importance of engaging visuals, including colorful animations and backgrounds, instead of direct speech or text.
Well, I did like the way it [was] portrayed– it helped us visualize it. You know, it's better to get shown something rather than told something. [Participant 9, 13 years old]
Furthermore, many participants reported the need for an interactive app with gamification and examples. Participants suggested gamification options including rewards systems (points, badges, prizes), minigames, and pop quizzes.
I'd add certain structures to it, where you're supposed to watch a certain amount of videos at once, just so you don't forget about it. Like the way to check if the person's understanding the video, that would help, because I think the message behind the videos sometimes got a little lost. [Participant 26, 14 years old]
While design and interactivity were common themes described by the majority of participants, participants also expressed that this should be balanced by lessons that are simple with ample explanation.
It was both thorough but simple enough to get the gist of it. And it wasn't too much for people to understand, I guess. So, it still gives you a tidbit of what they expect from the app and what you're going to have, but it doesn't throw too much info at you so you're like, “I don't want this at all.” [Participant 12, 16 years old]
3.5.2 Mindful eating apps should be flexible, adaptable, and easy to use
Several participants suggested that clear instructions were important in encouraging participation. Although they appreciated flexibility and did not want to feel controlled, some expressed that structure and step-by-step directions would prevent users from feeling overwhelmed with options.
…the other ones were more like, “this is what you’re doing wrong. You should be doing this.” but it doesn't really tell you how to get from point A to Point B… It's like, this is what you're doing wrong, and this is what you should be doing, but there's no helpful tips. [The Gears lesson] had more instructions instead of– I don't want to call it criticisms, because they're not really criticisms. It's just showing you two sides of one coin instead of showing you the process of flipping the coin. [Participant 19, 16 years old]
Participants highlighted the importance of an easy-to-understand app that teaches you how to engage in mindfulness training.
…it walks you through everything. Instead of just telling you, “You need to do this, that, and that,” it gives you ways to do that. And kind of guides you through it. [Participant 6, 17 years old]
Similarly, participants wanted an app that was both visually appealing and simple enough to use easily.
Nothing about [the app] was confusing at all. It wasn't an app that's easy to get lost in. [Participant 14, 17 years old]
3.5.3 Mindful eating apps should be relatable, non-judgmental, and helpful
Participants described the importance of an app that is honest and relatable– one that acknowledges the realities and challenges of food cravings.
I like how it doesn't hide from the fact that people crave foods and stuff like that. And he was basically saying it's better to accept [that] than act like it's not there. And he was also saying, like, when you have cravings, you see changes in your body. Your mind and your body change once you have cravings. [Participant 5, 15 years old]
Multiple participants resonated with the lessons' messages about mindful eating, cravings, and the challenges of breaking habit loops related to food.
It made me think of how I used to use food as a stress relief. And I almost relate to how that person felt when… about what they were talking about. I understood personally; it related to a personal experience. [Participant 19, 16 years old]
Participants described the app and the messages, examples, and stories within the lessons as relatable. They described the app as one that acknowledges the challenging nature of improving one's relationship with food and eating.
It kind of just, like, goes through the stages of how people sometimes mess up, and they'll be like, “Well, I can't do it anymore,” and then they'll realize their faults and try again. [Participant 12, 16 years old]
The themes of visual engagement, usability, and positive app tone revealed during ATA supported our findings from the FMA. In particular, findings from the ATA and FMA both highlighted the importance of visual appeal, engagement, usability, and non-judgmental tone in a mindful-eating app. The ATA also revealed the need to include gamification, relatable examples, and thorough explanations. While the FMA informed the development of the SAMBA app, given its rapid turnaround time, the ATA findings are important data that may influence future iterations of the app.
4 Discussion
4.1 Principal results
Results from the UTAUT-based survey showed that a mindful eating app is acceptable to adolescents overall, with high scores for Performance Expectancy, Social Influence, Facilitating Conditions, and Attitudes Toward Technology. However, the survey results also identified potential challenges in terms of Effort Expectancy and Self-Efficacy. Qualitative analysis supported and contextualized the survey findings. Advanced thematic analysis showed adolescents to be receptive to a mindful eating app, and also identified themes pointing to essential features for successful youth engagement.
Similarly to prior work, given that the FMA methodology has a faster turn-around time, it was used in real time to inform app design and development, whereas final insights from ATA were available after app development (67). Importantly, analysis of the semi-structured interviews using FMA and ATA yielded consistent results, an approach for analyzing qualitative data that has been described in past research (67). Specifically, both FMA and ATA codebooks elicited similar themes regarding the importance of an easy-to-use, engaging, and visually appealing app for adolescents.
While the FMA codebook summarized the participants' individual interview responses about the app and shaped the development of the SAMBA app, the ATA codebook identified broader themes. In addition to the major themes elicited by analysis of the semi-structured interviews, participants provided constructive suggestions regarding visual engagement, gamification, and the addition of teen-specific examples.
Participants' answers to the UTAUT survey constructs demonstrated that they believe that a mindful eating app may improve their relationship with food and help them be healthier. Overall, participants agreed that they have the resources and time to use this type of app, and that they (and their parents) would have a positive perception of this technology. However, participants cited lower agreement with the Effort Expectancy and Self-Efficacy constructs, indicating that they may find a mindful eating app confusing or intimidating, or they anticipate potential challenges with learning to use a mindful eating app. Qualitative themes that emerged from thematic analysis suggested several potential features that may mitigate youths' lack of confidence in successfully using such a digital tool. Specifically, youth endorsed that a mindful eating app for adolescents needs to have a specific design, allowing it to be engaging, interactive, and visually appealing; it should also have a specific structure and flow, allowing it to be flexible, adaptable, and easy to use, and finally, it should have content that is relatable, non-judgmental, and helpful.
Pilot testing of health apps, such as the SAMBA app, should include exit interviews to assess for specific barriers to Effort Expectancy and Self-Efficacy that may affect youth engagement with apps and their content. This would inform user feedback-driven iterations of the SAMBA app to optimize adherence and clinical outcomes.
4.2 Future directions
The SAMBA web-based app, a mindful eating app for adolescents, was developed with the incorporation of adolescent feedback from this study. As a next step, we had planned to test the SAMBA app in an NIH-funded pilot randomized controlled trial (RCT), to assess the feasibility of app use by adolescents and its effect on eating behavior. Unfortunately, the web-based app was hacked and due to the high cost of launching it again, plans were halted. Instead, we plan to proceed stepwise, and to first test the core curriculum (didactic video lessons, audio meditations) for acceptability and feasibility. For this, we plan to use either text messaging or e-mail to deliver links to our didactic videos and audios, which are hosted on a streaming platform, or to use one of the existing robust online platforms that are designed to centralize the delivery of educational content. This approach of utilizing text messaging, e-mail, or an existing platform as opposed to a brand-new web-based app would allow for a much lower cost, shorter timeline, and increased robustness against real-world challenges such as hacking.
With the rising clinical use of glucagon-like peptide receptor (GLP-1s) agonist medications for weight management in adolescents, the practice of mindful eating remains highly relevant (68, 69). Recent literature has highlighted the need for a focus on nutritional interventions to optimize GLP-1 efficacy (70–72). GLP-1s slow down gastric emptying and intestinal motility and thus can cause early fullness, and they are frequently associated with side effects including nausea, vomiting, bloating, and abdominal pain (73). Interventions focused on eating practices, such as mindful eating, may be able to promote medication compliance and decrease side effects by encouraging youth to pay attention to their bodily cues of hunger and satiety. Following these body cues can lead to eating smaller, more frequent meals, at a slower pace, and stopping before feeling full, which may be less likely to be associated with gastrointestinal side effects (70, 71). The practice of mindful eating remains highly important, and may be beneficial, when used in conjunction with obesity medications such as GLP-1s. Based on our clinical experience and the literature, the proportion of adolescents with obesity seen in weight management clinics who are eligible and interested in taking GLP-1s as an adjuvant to intensive health behavior and lifestyle treatment has been rapidly increasing (74). Thus, we plan to test the SAMBA app on adolescents who are preparing to start GLP-1s. Other future directions include adapting our mindful eating curriculum for youth with type 1 diabetes mellitus, as this population may also benefit from mindful eating practices given their increased risk for weight gain (75–77) and food-centric management.
4.3 Limitations
The limitations of this preliminary study include a relatively small sample size of 25 participants from a single urban institution, which does not allow us to draw conclusions about app perceptions by gender or severity of obesity, and which may limit generalizability of findings to the general population. We did not include non-English-speaking participants (as the app and its curriculum are only available in English at this time) or older adolescents (greater than 17 years old), as we wanted to focus on middle adolescence, which is different developmentally and socially from late adolescence (18–21 years) (78).
All participants attended a clinical weight management program, and thus may be more motivated than the general adolescent population, as reflected in their answer to the weight-related stages of change questionnaire. Participants viewed excerpts from a mindful eating app and answered a questionnaire endorsing the behavioral intention to use the app, which is different from actually using the app in their daily lives. A future pilot randomized controlled trial (RCT) will seek to address these limitations by assessing the acceptability and feasibility of the core SAMBA curriculum vs. a control, followed by a larger RCT.
4.4 Conclusions
Tailored mindful eating apps should continue to be studied as a potential intervention for adolescents seeking to improve their relationship with food, as an adjunct to multicomponent weight management interventions. Mindful eating apps designed and developed for adolescents, such as SAMBA, should prioritize non-judgmental and relatable features that encourage interactivity with the app.
As technology changes and app use increases among adolescents, prospective studies should continue to assess feasibility of app use within this population. Research measures such as the UTAUT model can help evaluate what influences youth to adopt and use technology, and qualitative analysis can provide depth to those findings. Competing timelines and high costs for app development, unexpected challenges which are becoming more commonplace, such as hacking, and research implementation present challenges to creating and studying health apps including mindful eating apps. Creative solutions are needed to address these challenges to developing and studying digital MBIs for adolescents.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Brown University Health Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
MS-G: Project administration, Writing – review & editing, Funding acquisition, Investigation, Formal analysis, Supervision, Writing – original draft, Data curation, Methodology, Conceptualization, Resources. MT: Writing – review & editing, Project administration, Methodology, Data curation. AM: Writing – review & editing, Methodology, Data curation. JT: Formal analysis, Writing – review & editing. RR: Writing – review & editing. EJ: Writing – review & editing, Supervision. BJ: Writing – review & editing, Supervision, Formal analysis.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by a Children's Miracle Network annual scholar award through Hasbro Children’s Hospital (MS-G) and also partially supported by the National Institutes of Health (NIH) Environmental Influences on Child Health Outcomes (ECHO) Idea States Pediatric Clinical Trials Network (ISPCTN), Rhode Island Clinical Trials Collaborative, UG1OD024951. The project described was supported by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Rhode Island Clinical and Translational Research (Advance RI-CTR). Support from the Biostatistics, Epidemiology, and Research Design Core of Advance-RI CTR was received. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgments
We would like to thank all participants, as well as the adolescents and young adults who contributed to alpha and beta testing of the SAMBA app. Thank you to Drs. Thomas Chun and Philip Gruppuso for their mentorship throughout this project. Support from the Biostatistics, Epidemiology and Research Design Core of Advance RI-CTR was received.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MBI, mindfulness-based intervention; UTAUT, The Unified Theory of Acceptance and Use of Technology; SAMBA, Study of an Adolescent Mindfulness-Based Intervention App; FMA, framework matrix analysis; ATA, applied thematic analysis; RCT, randomized controlled trial.
References
1. Jebeile H, Kelly AS, O'Malley G, Baur LA. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. (2022) 10(5):351–65. doi: 10.1016/S2213-8587(22)00047-X
2. Prevention CfDCa. Childhood Obesity Facts (2024). Available online at: https://www.cdc.gov/obesity/childhood-obesity-facts/childhood-obesity-facts.html#:∼:text=From%202017%20to%20March%202020,percentile%20for%20age%20and%20sex (Accessed December 16, 2024).
3. Epstein LH, Myers MD, Raynor HA, Saelens BE. Treatment of pediatric obesity. Pediatrics. (1998) 101(3 Pt 2):554–70. doi: 10.1542/peds.101.S2.554
4. Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. (1994) 13(5):373–83. doi: 10.1037/0278-6133.13.5.373
5. Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. (2006) 355(15):1563–71. doi: 10.1056/NEJMoa061883
6. Butryn ML, Wadden TA, Rukstalis MR, Bishop-Gilyard C, Xanthopoulos MS, Louden D, et al. Maintenance of weight loss in adolescents: current status and future directions. J Obes. (2010) 2010:789280. doi: 10.1155/2010/789280
7. Kabat-Zinn J, Hanh T. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Random House LLC (2009).
8. Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. (1985) 8(2):163–90. doi: 10.1007/BF00845519
9. Barnes VA, Kristeller JL. Impact of mindfulness-based eating awareness on diet and exercise habits in adolescents. Int J Complement Altern Med. (2016) 3(2):60–7. doi: 10.15406/ijcam.2016.03.00070.
10. Brewer JA, Ruf A, Beccia AL, Essien GI, Finn LM, van Lutterveld R, et al. Can mindfulness address maladaptive eating behaviors? Why traditional diet plans fail and how new mechanistic insights may lead to novel interventions. Front Psychol. (2018) 9:1418. doi: 10.3389/fpsyg.2018.01418
11. Schneider-Worthington CR, Smith KE, Roemmich JN, Salvy SJ. External food cue responsiveness and emotional eating in adolescents: a multimethod study. Appetite. (2022) 168:105789. doi: 10.1016/j.appet.2021.105789
12. Fuentes Artiles R, Staub K, Aldakak L, Eppenberger P, Rühli F, Bender N. Mindful eating and common diet programs lower body weight similarly: systematic review and meta-analysis. Obes Rev. (2019) 20(11):1619–27. doi: 10.1111/obr.12918
13. Kumar S, Croghan IT, Biggs BK, Croghan K, Prissel R, Fuehrer D, et al. Family-based mindful eating intervention in adolescents with obesity: a pilot randomized clinical trial. Children (Basel). (2018) 5(7):93. doi: 10.3390/children5070093
14. Bockmann JO, Yu SY. Using mindfulness-based interventions to support self-regulation in young children: a review of the literature. Early Child Educ J. (2023) 51(4):693–703. doi: 10.1007/s10643-022-01333-2
15. de Lara Perez B, Delgado-Rios M. Mindfulness-based programs for the prevention of childhood obesity: a systematic review. Appetite. (2022) 168:105725. doi: 10.1016/j.appet.2021.105725
16. Shao S, Li L, Zhang Y, Liu Z, Zhang X. Research progress on the role of mindfulness in intervention for adolescent obesity. Front Endocrinol (Lausanne). (2024) 15:1412522. doi: 10.3389/fendo.2024.1412522
17. Bernstein R, Sanchez N, Clark ELM, Conte I, Gulley LD, Legget KT, et al. Mindfulness-based intervention in adolescents at risk for excess weight gain: 1.5-year follow-up of pilot randomized controlled trial. Eat Behav. (2021) 43:101580. doi: 10.1016/j.eatbeh.2021.101580
18. Gayoso L, de Tomas I, Téllez R, Maiz E, Etxeberria U. Mindfulness-based eating intervention in children: effects on food intake and food-related behaviour during a mid-morning snack. Mindfulness (N Y). (2021) 12(5):1185–94. doi: 10.1007/s12671-020-01587-0
19. Omiwole M, Richardson C, Huniewicz P, Dettmer E, Paslakis G. Review of mindfulness-related interventions to modify eating behaviors in adolescents. Nutrients. (2019) 11(12):2917. doi: 10.3390/nu11122917
20. Bacalhau SPOS, Orange LG, Correia Junior MAV, Nunes JV, Almeida CLAS, Coriolano-Marinus MWL. Mindfulness-based interventions and their relationships with body image and eating behavior in adolescents: a scoping review. J Eat Disord. (2025) 13(1):77. doi: 10.1186/s40337-025-01238-6
21. Reangsing C, Punsuwun S, Schneider JK. Effects of mindfulness interventions on depressive symptoms in adolescents: a meta-analysis. Int J Nurs Stud. (2021) 115:103848. doi: 10.1016/j.ijnurstu.2020.103848
22. Dunning DL, Griffiths K, Kuyken W, Crane C, Foulkes L, Parker J, et al. Research review: the effects of mindfulness-based interventions on cognition and mental health in children and adolescents - a meta-analysis of randomized controlled trials. J Child Psychol Psychiatry. (2019) 60(3):244–58. doi: 10.1111/jcpp.12980
23. Knol L, Crowe-White K, Appel S. Mindful eating is related to lower intake of energy and added sugars among overweight, premenopausal women. Curr Dev Nutr. (2020) 4(Suppl 2):1318. doi: 10.1093/cdn/nzaa059_035
24. Tapper K. Mindful eating: what we know so far. Nutr Bull. (2022) 47(2):168–85. doi: 10.1111/nbu.12559
25. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutr Res Rev. (2017) 30(2):272–83. doi: 10.1017/S0954422417000154
26. O'Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. (2014) 15(6):453–61. doi: 10.1111/obr.12156
27. Morillo-Sarto H, López-Del-Hoyo Y, Pérez-Aranda A, Modrego-Alarcón M, Barceló-Soler A, Borao L, et al. Mindful eating’ for reducing emotional eating in patients with overweight or obesity in primary care settings: a randomized controlled trial. Eur Eat Disord Rev. (2023) 31(2):303–19. doi: 10.1002/erv.2958
28. Hendrickson KL, Rasmussen EB. Mindful eating reduces impulsive food choice in adolescents and adults. Health Psychol. (2017) 36(3):226–35. doi: 10.1037/hea0000440
29. Gutiérrez-Domingo T, Vivas S. Mindful eating intervention for preventing obesity in youth: a narrative review of literature. Nutr Res. (2025) 140:116–34. doi: 10.1016/j.nutres.2025.07.001
30. Krebs S, Moak E, Muhammadi S, Forbes D, Yeh MC, Leung MM. Testing the feasibility and potential impact of a mindfulness-based pilot program in urban school youth. Int J Environ Res Public Health. (2022) 19(6):3464. doi: 10.3390/ijerph19063464
31. Kao TA, Ling J, Alanazi M, Atwa A, Liu S. Effects of mindfulness-based interventions on obesogenic eating behaviors: a systematic review and meta-analysis. Obes Rev. (2025) 26(3):e13860. doi: 10.1111/obr.13860
32. Carrière K, Khoury B, Günak MM, Knäuper B. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev. (2018) 19(2):164–77. doi: 10.1111/obr.12623
33. Yu J, Song P, Zhang Y, Wei Z. Effects of mindfulness-based intervention on the treatment of problematic eating behaviors: a systematic review. J Altern Complement Med. (2020) 26(8):666–79. doi: 10.1089/acm.2019.0163
34. Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. (2015) 77(1):59–67. doi: 10.1097/PSY.0000000000000127
35. Daly P, Pace T, Berg J, Menon U, Szalacha LA. A mindful eating intervention: a theory-guided randomized anti-obesity feasibility study with adolescent Latino females. Complement Ther Med. (2016) 28:22–8. doi: 10.1016/j.ctim.2016.07.006
36. Shan R, Shao S, Li LD, Zhang D, Chen J, Xiao W, et al. Mindfulness-based interventions for improvement of lifestyle behaviors and body mass index in children with overweight or obesity: a systematic review and meta-analysis. Eur J Pediatr. (2025) 184(2):132. doi: 10.1007/s00431-024-05958-w
37. Rosa C, Marsch LA, Winstanley EL, Brunner M, Campbell ANC. Using digital technologies in clinical trials: current and future applications. Contemp Clin Trials. (2021) 100:106219. doi: 10.1016/j.cct.2020.106219
38. Atske S. Teens, Social Media and Technology 2022 Pew Research Center (2022). Available online at: https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/ (Accessed December 19, 2024).
39. Mason AE, Jhaveri K, Cohn M, Brewer JA. Testing a mobile mindful eating intervention targeting craving-related eating: feasibility and proof of concept. J Behav Med. (2018) 41(2):160–73. doi: 10.1007/s10865-017-9884-5
40. Carrière K, Siemers N, Thapar S, Knäuper B. Proof-of-concept testing of a mobile application-delivered mindfulness exercise for emotional eaters: RAIN delivered as a step-by-step image sequence. Mhealth. (2024) 10:24. doi: 10.21037/mhealth-23-56
41. Burton ET, Smith WA. Mindful eating and active living: development and implementation of a multidisciplinary pediatric weight management intervention. Nutrients. (2020) 12(5):1425. doi: 10.3390/nu12051425
42. Rung AL, Oral E, Berghammer L, Peters ES. Feasibility and acceptability of a Mobile mindfulness meditation intervention among women: intervention study. JMIR Mhealth Uhealth. (2020) 8(6):e15943. doi: 10.2196/15943
43. Zhang Q, O'Connor DB, Hugh-Jones S. Feasibility of a multiple-component mindfulness intervention for Chinese adolescents living with overweight: a pilot randomized trial. Appl Psychol Health Well Being. (2023) 15(2):516–35. doi: 10.1111/aphw.12393
44. Alqahtani F, Winn A, Orji R. Co-designing a Mobile app to improve mental health and well-being: focus group study. JMIR Form Res. (2021) 5(2):e18172. doi: 10.2196/18172
45. Cushman G, Larsen M, Jandasek B, Kopel S, Esteban C, Rudders S, et al. Friends, family, and food app: improvements in child management self-efficacy and caregiver communication. J Allergy Clin Immunol. (2023) 151:AB38. doi: 10.1016/j.jaci.2022.12.121
46. Raeside R, Todd A, Wardak S, Gardner L, Champion KE, Kang M, et al. Striking the right balance: co-designing the Health4Me healthy lifestyle digital health intervention with adolescents. Res Involv Engagem. (2023) 9(1):114. doi: 10.1186/s40900-023-00524-4
47. Bosworth KT, Ghosh P, Flowers L, Proffitt R, Koopman RJ, Tosh AK, et al. The user-centered design and development of a childhood and adolescent obesity electronic health record tool, a mixed-methods study. Front Digit Health. (2024) 6:1396085. doi: 10.3389/fdgth.2024.1396085
48. Alwashmi MF, Hawboldt J, Davis E, Fetters MD. The iterative convergent design for Mobile health usability testing: mixed methods approach. JMIR Mhealth Uhealth. (2019) 7(4):e11656. doi: 10.2196/11656
49. Ammenwerth E. Technology acceptance models in health informatics: TAM and UTAUT. Stud Health Technol Inform. (2019) 263:64–71. doi: 10.3233/SHTI190111
50. Alsahli S, Hor SY, Lam MK. Physicians’ acceptance and adoption of mobile health applications during the COVID-19 pandemic in Saudi Arabia: extending the unified theory of acceptance and use of technology model. Health Inf Manag. (2024) 54(3):255–67. doi: 10.1177/18333583241300534
51. Wessels NJ, Hulshof L, Loohuis AMM, van Gemert-Pijnen L, Jellema P, van der Worp H, et al. User experiences and preferences regarding an app for the treatment of urinary incontinence in adult women: qualitative study. JMIR Mhealth Uhealth. (2020) 8(6):e17114. doi: 10.2196/17114
52. Chen E, Muessig K, Moracco K. Understanding the acceptability of health apps among adolescents: a qualitative study. ACI Open. (2022) 06:e103–13. doi: 10.1055/s-0042-1758461
53. Salihu EY, Omuya H, Joseph DT, Hassan JH, Ali A, Chewning B. Acceptability and scalability of a meditation app among adolescents with type 1 diabetes mellitus. Cureus. (2024) 16(10):e72700. doi: 10.7759/cureus.72700
54. Wiljén A, Chaplin JE, Crine V, Jobe W, Johnson E, Karlsson K, et al. The development of an mHealth tool for children with long-term illness to enable person-centered communication: user-centered design approach. JMIR Pediatr Parent. (2022) 5(1):e30364. doi: 10.2196/30364
55. LeRouge CM, Hah H, Deckard GJ, Jiang H. Designing for the co-use of consumer health technology in self-management of adolescent overweight and obesity: mixed methods qualitative study. JMIR Mhealth Uhealth. (2020) 8(6):e18391. doi: 10.2196/18391
56. Rentrop V, Damerau M, Schweda A, Steinbach J, Schüren LC, Niedergethmann M, et al. Predicting acceptance of e-mental health interventions in patients with obesity by using an extended unified theory of acceptance model: cross-sectional study. JMIR Form Res. (2022) 6(3):e31229. doi: 10.2196/31229
57. Ribanszki R, Saez Fonseca JA, Barnby JM, Jano K, Osmani F, Almasi S, et al. Preferences for digital smartphone mental health apps among adolescents: qualitative interview study. JMIR Form Res. (2021) 5(8):e14004. doi: 10.2196/14004
58. Bosworth KT, Flowers L, Proffitt R, Ghosh P, Koopman RJ, Wilson G, et al. Mixed-methods study of development and design needs for CommitFit, an adolescent mHealth app. Mhealth. (2023) 9:22. doi: 10.21037/mhealth-22-35
59. Wang JW, Zhu Z, Shuling Z, Fan J, Jin Y, Gao ZL, et al. Effectiveness of mHealth app-based interventions for increasing physical activity and improving physical fitness in children and adolescents: systematic review and meta-analysis. JMIR Mhealth Uhealth. (2024) 12:e51478. doi: 10.2196/51478
60. Langarizadeh M, Sadeghi M, As’habi A, Rahmati P, Sheikhtaheri A. Mobile apps for weight management in children and adolescents; an updated systematic review. Patient Educ Couns. (2021) 104(9):2181–8. doi: 10.1016/j.pec.2021.01.035
61. Turner T, Hingle M. Evaluation of a mindfulness-based Mobile app aimed at promoting awareness of weight-related behaviors in adolescents: a pilot study. JMIR Res Protoc. (2017) 6(4):e67. doi: 10.2196/resprot.6695
62. Lyzwinski LN, Edirippulige S, Caffery L, Bambling M. Mindful eating Mobile health apps. Review and Appraisal. JMIR Ment Health. (2019) 6(8):e12820. doi: 10.2196/12820
63. Sun S, Nardi W, Murphy M, Scott T, Saadeh F, Roy A, et al. Mindfulness-based Mobile health to address unhealthy eating among middle-aged sexual minority women with early life adversity: mixed methods feasibility trial. J Med Internet Res. (2023) 25:e46310. doi: 10.2196/46310
64. de Freitas PP, de Menezes MC, Dos Santos LC, Pimenta AM, Ferreira AVM, Lopes ACS. The transtheoretical model is an effective weight management intervention: a randomized controlled trial. BMC Public Health. (2020) 20(1):652. doi: 10.1186/s12889-020-08796-1
65. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
66. Likert R. A technique for the measurement of attitudes. Archives of Psychology. (1932) 22(140):55.
67. Rosen RK, Gainey M, Nasrin S, Garbern SC, Lantini R, Elshabassi N, et al. Use of framework matrix and thematic coding methods in qualitative analysis for mHealth: the FluidCalc app. Int J Qual Methods. (2023) 22:16094069231184123. doi: 10.1177/16094069231184123
68. Kompaniyets L, Pierce SL, Porter R, Autrey K, Chua KP, Belay B, et al. Prescriptions for obesity medications among adolescents aged 12–17 years with obesity - United States, 2018–2023. MMWR Morb Mortal Wkly Rep. (2025) 74(20):337–44. doi: 10.15585/mmwr.mm7420a1
69. Hannon TS, Arslanian SA. Obesity in adolescents. N Engl J Med. (2023) 389(3):251–61. doi: 10.1056/NEJMcp2102062
70. Mozaffarian D, Agarwal M, Aggarwal M, Alexander L, Apovian CM, Bindlish S, et al. Nutritional priorities to support GLP-1 therapy for obesity: a joint advisory from the American college of lifestyle medicine, the American society for nutrition, the obesity medicine association, and the obesity society. Obesity (Silver Spring). (2025) 33(8):1475–503. doi: 10.1002/oby.24336
71. Almandoz JP, Wadden TA, Tewksbury C, Apovian CM, Fitch A, Ard JD, et al. Nutritional considerations with antiobesity medications. Obesity (Silver Spring). (2024) 32(9):1613–31. doi: 10.1002/oby.24067
72. Wharton S, Davies M, Dicker D, Lingvay I, Mosenzon O, Rubino DM, et al. Managing the gastrointestinal side effects of GLP-1 receptor agonists in obesity: recommendations for clinical practice. Postgrad Med. (2022) 134(1):14–9. doi: 10.1080/00325481.2021.2002616
73. Bellavance D, Chua S, Mashimo H. Gastrointestinal motility effects of GLP-1 receptor agonists. Curr Gastroenterol Rep. (2025) 27(1):49. doi: 10.1007/s11894-025-00995-3
74. Lee JM, Sharifi M, Oshman L, Griauzde DH, Chua KP. Dispensing of glucagon-like peptide-1 receptor agonists to adolescents and young adults, 2020–2023. JAMA. (2024) 331(23):2041–3. doi: 10.1001/jama.2024.7112
75. Marlow AL, Rowe CW, Anderson D, Wynne K, King BR, Howley P, et al. Young children, adolescent girls and women with type 1 diabetes are more overweight and obese than reference populations, and this is associated with increased cardiovascular risk factors. Diabet Med. (2019) 36(11):1487–93. doi: 10.1111/dme.14133
76. Maffeis C, Birkebaek NH, Konstantinova M, Schwandt A, Vazeou A, Casteels K, et al. Prevalence of underweight, overweight, and obesity in children and adolescents with type 1 diabetes: data from the international SWEET registry. Pediatr Diabetes. (2018) 19(7):1211–20. doi: 10.1111/pedi.12730
77. Guo Y, Lin C, Cai X, Wu H, Yan J, Li Z, et al. Regional, age-specific and sex-specific trends in the prevalence of overweight or obesity in type 1 diabetes from 1980 to 2020: a meta-analysis of 78 observational studies with 650,265 participants. Diabetes Res Clin Pract. (2025) 229:112899. doi: 10.1016/j.diabres.2025.112899
Keywords: mHealth, mindful eating, mindfulness training, app development, adolescents, obesity, UTAUT, semi-structured interview
Citation: Serrano-Gonzalez M, Triedman M, Mandapati A, Tanzer JR, Rosen R, Jelalian E and Jandasek B (2025) The development of a mindful eating app for adolescents through mixed-methods feedback from adolescents with overweight or obesity. Front. Adolesc. Med. 3:1667649. doi: 10.3389/fradm.2025.1667649
Received: 16 July 2025; Accepted: 20 October 2025;
Published: 10 November 2025.
Edited by:
Chao Liu, Huaqiao University, ChinaReviewed by:
Catarina I. Reis, Polytechnic Institute of Leiria, PortugalTamara Gutiérrez-Domingo, University of Cordoba, Spain
Copyright: © 2025 Serrano-Gonzalez, Triedman, Mandapati, Tanzer, Rosen, Jelalian and Jandasek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Monica Serrano-Gonzalez, bW9uaWNhX3NlcnJhbm9AYnJvd24uZWR1
 Monica Serrano-Gonzalez
Monica Serrano-Gonzalez Miranda Triedman
Miranda Triedman Amiya Mandapati1
Amiya Mandapati1