- 1PRISMATICS Lab (Predictive Research in Spine/Neuromodulation Management and Thoracic Innovation/Cardiac Surgery), Poitiers University Hospital, Poitiers, France
- 2Association Francophone McKenzie (AFMcK – McKenzie Francophonic Association), Paris, France
- 3Institut Pprime UPR 3346, CNRS – Université de Poitiers – ISAE-ENSMA, Poitiers, France
- 4Centre Européen d’Enseignement en Rééducation et Réadaptation Fonctionnelle (CEERRF – European Center for Education in Rehabilitation and Functional Rehabilitation), Saint Denis, France
- 5Institut d’Ingénierie de la Santé, Université de Picardie Jules Verne, Amiens, France
- 6Department of Spine, Pain and Disability Neurosurgery, Poitiers University Hospital, Poitiers, France
- 7The Sports Clinic, Christchurch, New Zealand
- 8Center for Adaptable MRI Technology, Institute of Medical Sciences, School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, Aberdeen, United Kingdom
Introduction: The dynamic disc model (DDM) is a theoretical framework in spine mechanics that theorizes the behavior of the nucleus pulposus within the intervertebral disc under various loads. The model predicts displacement of the nucleus pulposus away from the bending loads, for example backward displacement of the nucleus pulposus with a flexion load. These predictions are regularly used as a theoretical basis for explaining certain disc pathologies, such as disc herniation.
Methods: We screened seven databases (CENTRAL, Embase, MEDLINE, CINAHL, ScienceDirect, Google Scholar, and HAL) up to July 2024, identifying studies through a PRISMA-guided approach that detailed the mechanical transformation (displacement and deformation) of the nucleus pulposus under bending load on the intervertebral disc. We conducted a double-blind data extraction and quality assessment of the body of evidence. Finally, we performed a meta-analysis of proportions.
Results: From the 9,269 articles screened, 14 studies were included in the systematic review and meta-analysis. Magnetic Resonance Imaging (MRI) was employed in 92.8% of the studies, revealing four strategies for assessing nucleus pulposus transformation. The meta-analysis of asymptomatic subjects’ data demonstrated that the nucleus pulposus behavior aligned with dynamic disc model predictions in 85.4% (95% CI = [79.4–91.4]) across spinal regions and bending directions. However, significant heterogeneity and low study quality were noted. Only one study used discography to assess the DDM in a discogenic pain population, identifying discrepancies in nucleus pulposus transformation and contrast agent leakage.
Conclusion: Evidence for the dynamic disc model for intact discs is of low strength, whereas very limited evidence challenges the dynamic disc model for fissured discs. New multiparametric MRI studies may help guiding future clinical assessment protocols.
Systematic Review Registration: CRD42022331774.
Introduction
With an estimated prevalence of approximately 20%, millions of individuals suffer from low back pain (LBP) worldwide (Hoy et al., 2012). LBP represents a tremendous burden for healthcare systems, costing billions of dollars/euros annually (Vos et al., 2016). In some cases, LBP extends beyond a self-limiting painful condition as it translates into disability (Vos et al., 2016) and impacts the quality of life (Ounajim et al., 2021), as well as the psychological (Pincus et al., 2002) and sociological wellbeing of patients (Naiditch et al., 2021b; Naiditch et al., 2021a). Despite a large number of clinical and experimental studies (McKenzie, 1981) exploring LBP over the past few decades, no consensus has been reached regarding the diagnostic process of the LBP population (Maher et al., 2017). In this context, different pathophysiological hypotheses, such as the dynamic disc model (DDM), have been proposed in the literature.
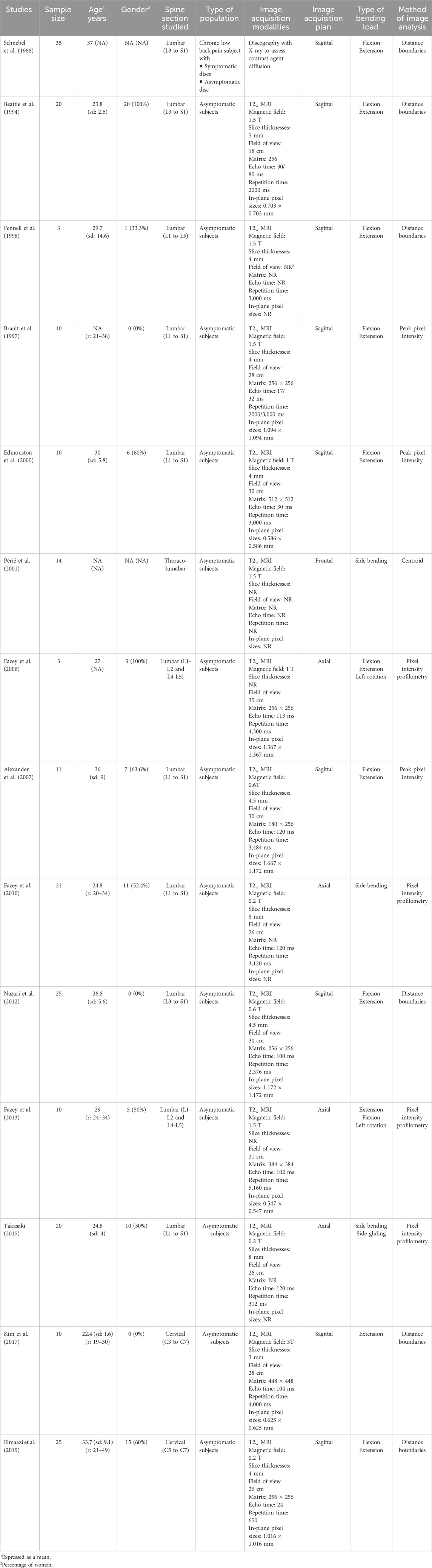
The DDM is based on mechanical transformation, i.e. displacement or strain, of the nucleus pulposus (NP) within the intervertebral disc in the opposite direction from pressure applied by bending load (Figure 1). In a healthy disc, the annulus fibrosus (AF), containing the NP, would limit the deformation or displacement. Consequently, radial fissures of the annulus fibrosus (fissure from the center to the periphery of the AF), may allow the NP to spread into the fissure and stimulate nociceptors localized in the external part of the annulus fibrosus (García-Cosamalón et al., 2010) or surrounding fissure (Lama et al., 2018).
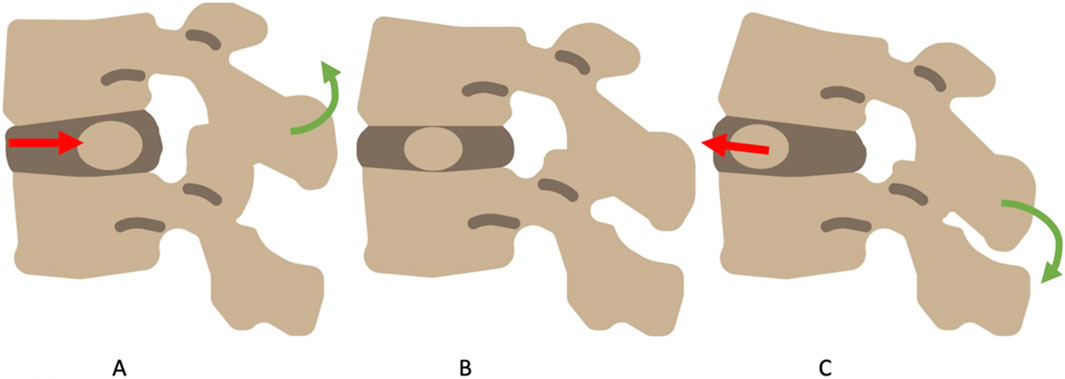
Figure 1. The dynamic disc model, in flexion (A) the NP migrates backward, in extension (C) the NP migrates forward. In neutral (B) the NP is central.
The DDM was used to provide a patho-anatomical explanation for the pain centralization phenomenon (CP) observed in clinical practice (Cyriax, 1950; McKenzie, 1981). CP is defined as the rapid and lasting abolition of distal pain as consequence of spinal bending load, and it occurs in a specific direction, called the directional preference (DP). According to the concept advocated by McKenzie (1981), CP may be the symptomatic expression of migration of the NP material away from the fissure towards the center of the intervertebral disc, while peripherization (opposite to the centralization phenomenon) may reflect the migration of the NP into the fissure.
Fifteen years ago, in a systematic review including 12 studies, Kolber and Hanney (2009) reported that lumbar NP moved opposite to the side of loading in asymptomatic and young subjects for lumbar sagittal bending loads. The authors also reported limited and contradictory results supporting the DDM for older or pathological lumbar discs. In addition, they highlighted a lack of research for the cervical, thoracic, and lumbar spine outside of the sagittal plane. Since then, studies have investigated the NP behavior thanks to new technological advances (Nazari et al., 2012; Fazey et al., 2013; Takasaki, 2015). An updated literature synthesis is now timely for providing new insights into NP mechanical transformation according to the bending load imposed.
This systematic review with meta-analysis aimed to identify and summarize the in vivo evidence of nucleus pulposus behavior with lumbar, thoracic, and cervical intervertebral disc loading. This review covered both the evidence for intact and for radially fissured discs.
Methods
The current systematic review and meta-analysis was performed in line with the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) (Page et al., 2021). The protocol for this systematic review was registered on PROSPERO (number CRD42022331774).
Search strategy
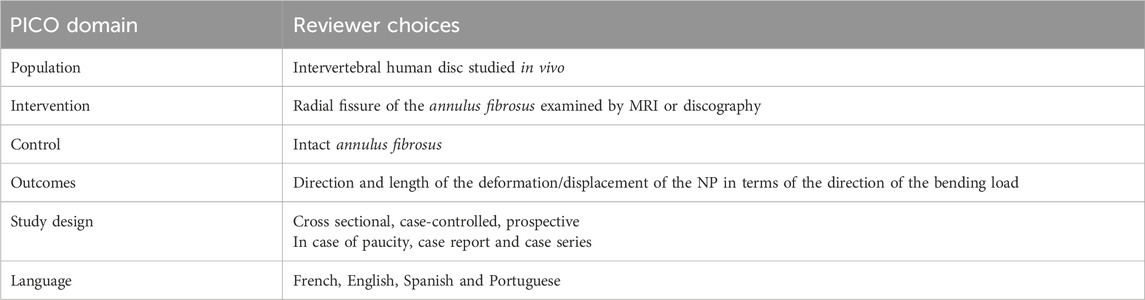
Electronic database MEDLINE, EMBASE, CINAHL, Cochrane Center Register of Controlled Clinical Trials (CENTRAL), ScienceDirect, Google Scholar and Archives Ouvertes HAL were searched until 25 August 2024 with no date limitation no date limitation (see PICO strategy in Table 1). Search results were augmented by direct contact with experts in the field, to identify potential missed references. Search strategies, based on MeSH terms, were developed for MEDLINE, and subsequently adapted for each database. The full search strategy is available in Supplemental Digital Content Section 1.
Study selection
All results were imported to a citation manager (Zotero 6.0.26) and duplicate entries were merged before importing the final list into the Rayyan website for the review process. Each article was screened for eligibility twice, independently, and blindly, by two authors, first by title/abstract, then by full article reading. In case of disagreement, a third reviewer arbitrated the final decision for inclusion/exclusion. The list of excluded articles and the reasons for their exclusion are available in Supplemental Digital Content Section 2 (starting from the full-text review stage).
Eligibility criteria
Every study that assessed and reported the mechanical transformation of NP during or after bending loads was included. We considered cross-sectional, case-controlled, or prospective studies. We considered human intervertebral discs studying in vivo conditions within asymptomatic or low back pain populations. Low back pain patients must have been screened for discogenic pain or radial fissure prior to the DDM assessment. Full scientific articles written in English, French, Spanish or Portuguese were considered.
Intervention/exposition
We considered intervertebral painful disc with radial fissures according to the North American Spine Society (NASS) classification. NASS defined radial fissure as “[…] disruption of annular fibers extending from the nucleus pulposus outward toward the periphery of the annulus fibrosus, usually in the cranial-caudad (vertical) plane, although, at times, with axial horizontal (transverse) components […]”(Fardon et al., 2014).
Data extraction
Data of interest were extracted from eligible articles twice, independently, and blindly. Information from considered studies included authors, year of publication, country, funding, participants characteristics (age, gender, symptomatic/asymptomatic status), MRI characteristics (magnetization, slice thickness, field of view, matrix dimensions, echo and repetition time), image acquisition plan, type of bending load, method of image analysis. Disagreements were resolved through discussion or, if necessary, by a third independent reviewer.
Risk of bias and reporting bias assessment
Risk of bias of each eligible article was rated twice, independently, and blindly, using the Newcastle-Ottawa scale (NOS). Disagreements were resolved through discussion or, if necessary, by a third reviewer. The scale evaluates the following domains: representativeness of sample, sample size justification, non-respondents, ascertainment of the exposure, comparability, assessment of outcome.
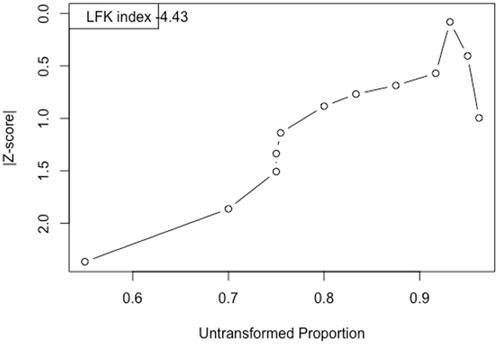
For the meta-analysis, reporting bias was assessed with the LFK index and Doi plot (Furuya-Kanamori et al., 2018). While Egger index and funnel plot (Higgins and Collaboration, 2020) are commonly used, recent evidence demonstrated the superiority of LFK index and Doi plot, especially for proportion meta-analysis (Hunter et al., 2014; Furuya-Kanamori et al., 2018; Cheema et al., 2022).
Certainty assessment
To assess the certainty of evidence, the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) was used (Guyatt et al., 2008). Certainty of evidence was rated as high, moderate, low, or very low according to risk of bias, heterogeneity, and methodological quality of the study.
Quantitative synthesis method
Two proportion meta-analyses were performed, one to assess intact disc among pain-free subjects and a second one to assess fissured disc among discogenic pain population. We used a proportion meta-analysis to determine the proportion of experimental observation in which the disc matches with the DDM, in vivo. We defined a DDM match as the NP moving/deforming away from the direction of the bending load, e.g., NP moving/deforming backward when flexion bending loads were imposed to the disc. We define an experimental observation as an observation in which the disc is bent, e.g., if a study assesses 10 discs in flexion and extension with respect to neutral position, the study includes a total of 20 observations. We conducted proportion meta-analysis for intact and fissured discs independently.
We used a random-effect model for gathering data, considering the potential high variability between studies. Heterogeneity was quantified with I2 statistic and the Cochrane’s Q test. We evaluated heterogeneity graphically using Forest plots. In case of insufficient information report, we contacted the authors of the study to request data sharing. If the requested information was not available, the study was excluded from the meta-analysis.
Analyses were performed using R language (version: R 4.2.2. GUI 1.79; interface: Rstudio 2022.07.2; package: meta, metafor, metasens and dosresmeta; operating system: MacOS Ventura 13.2).
Results
Study selection
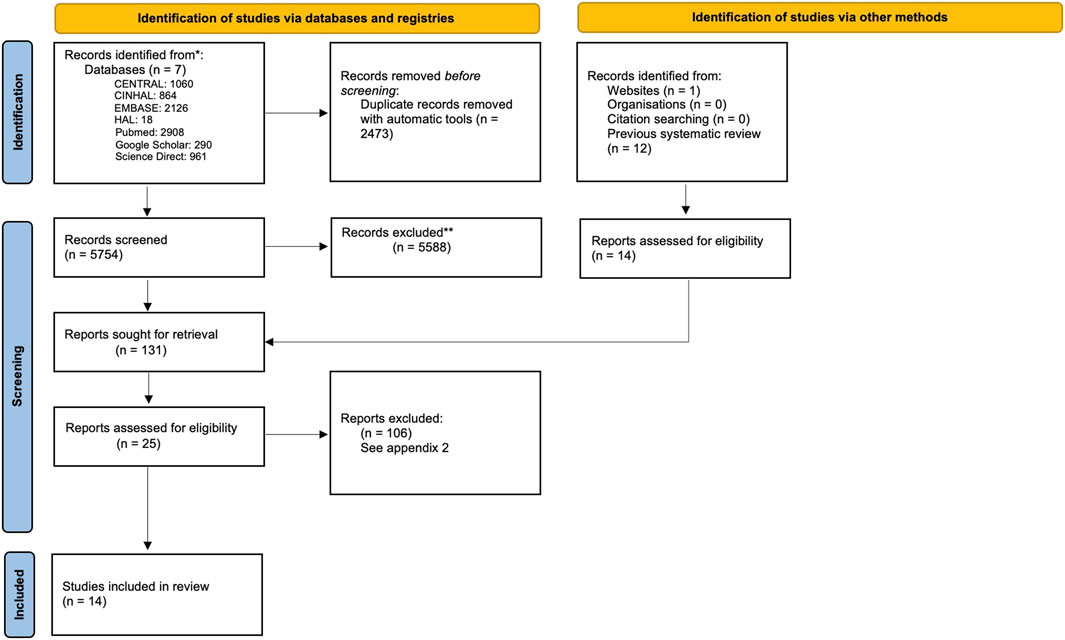
The PRISMA flow chart detailing the screening process is presented in Figure 2. The initial database research identified 9,269 articles. After removing 3,164 duplicates, 6,105 articles were selected for abstract and title assessment, and 25 studies were analyzed as full-text publications. After full-text screening, we included 14 articles in the final systematic review and 10 in the meta-analysis. The reliability of the full inclusion process was good (Cohen’s Kappa = 0.85 CI95% = [0.73–0.96] and %agreement = 0.998) (Landis and Koch, 1977).
Eight studies initially identified in the systematic review by Kolber and Hanney, (2009) were not included in the present review.
Four of these studies were cadaveric studies (Shah et al., 1978; Gill et al., 1987; Krag et al., 1987; Seroussi et al., 1989). The others evaluated the deformation of the annular wall, via MRI, in subjects with or without low back pain, during trunk movements (Zamani et al., 1998; Weishaupt et al., 2000; Fredericson et al., 2001; Parent et al., 2006). Despite the value of annular wall deformation data for understanding the mechanics of the intervertebral disc in a broad sense, they are not direct observation of the NP transformations. Therefore, they did not assess the DDM, hence the decision to exclude these articles. In this regard, we identified several studies conducted after the review by Kolber and Hanney (2009), assessing annular deformation (Zou et al., 2008; 2009), that were not included. Lastly, one additional study was excluded although the methods described were very close to our inclusion criteria (Abdollah et al., 2018). In this study, the authors identified the position of the NP via MRI in subjects with low back pain before and after repeated extension movements. However, these authors considered a population of low back pain patients without first identifying those suffering from discogenic pain or comparing target disc(s) with intact and pain-free ones.
Study characteristics
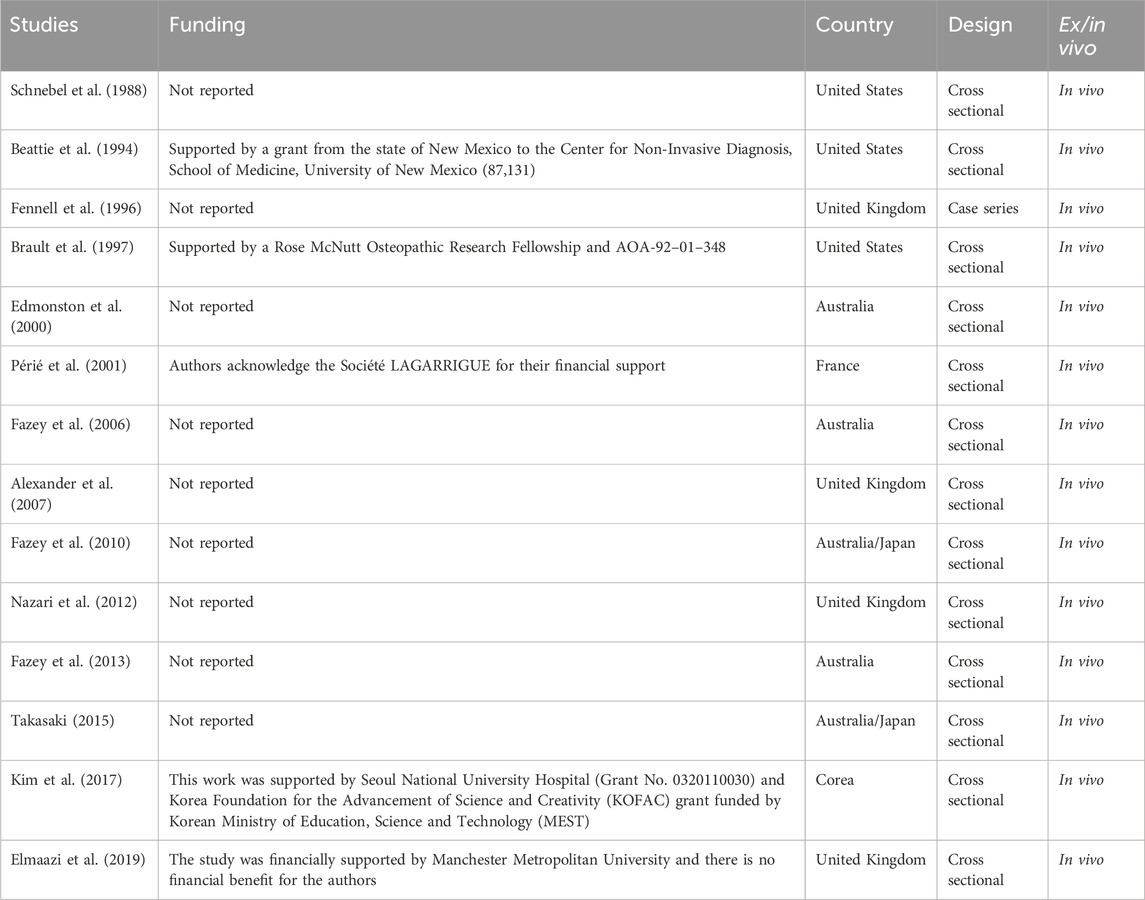
A comprehensive review of study characteristics is reported in Table 2. The earliest study dated from 1988 and latest from 2019.
Thirteen in vivo studies (92.8%) evaluated the dynamic behavior of the NP in young adults with intact discs (ranging in age from 22.4 to 37 years) (Beattie et al., 1994; Fennell et al., 1996; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; 2010; 2013; Alexander et al., 2007; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017), while one study assessed the dynamic behavior of the NP in chronic low back pain population (Schnebel et al., 1988), including subjects eligible for awake discography at three levels (Schnebel et al., 1988).
Thirteen studies (92.8%) used T2-weighted MR images (T2w-MRI) for assessing the dynamic behavior of the NP (Beattie et al., 1994; Fennell et al., 1996; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; 2010; 2013; Alexander et al., 2007; Takasaki H et al., 2010; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017; Elmaazi et al., 2019), while one used discography (Schnebel et al., 1988).
Two studies focused on the NP behavior of cervical discs in the sagittal plane (Kim et al., 2017; Elmaazi et al., 2019)when a sagittal bending load was applied (flexion/extension), while six others focused on lumbar discs (Fennell et al., 1996; Edmondston et al., 2000; Fazey et al., 2006; 2010; 2013; Alexander et al., 2007). Among these six studies, two also assessed the effect of axial rotation (axial plane) on NP transformation in the frontal plane (Fazey et al., 2006; 2013). Additionally, two different studies assessed the effect of frontal plane bending load (side glide and side bending) on the transformation of the lumbar NP in the frontal plane (Périé et al., 2003; Takasaki, 2015).
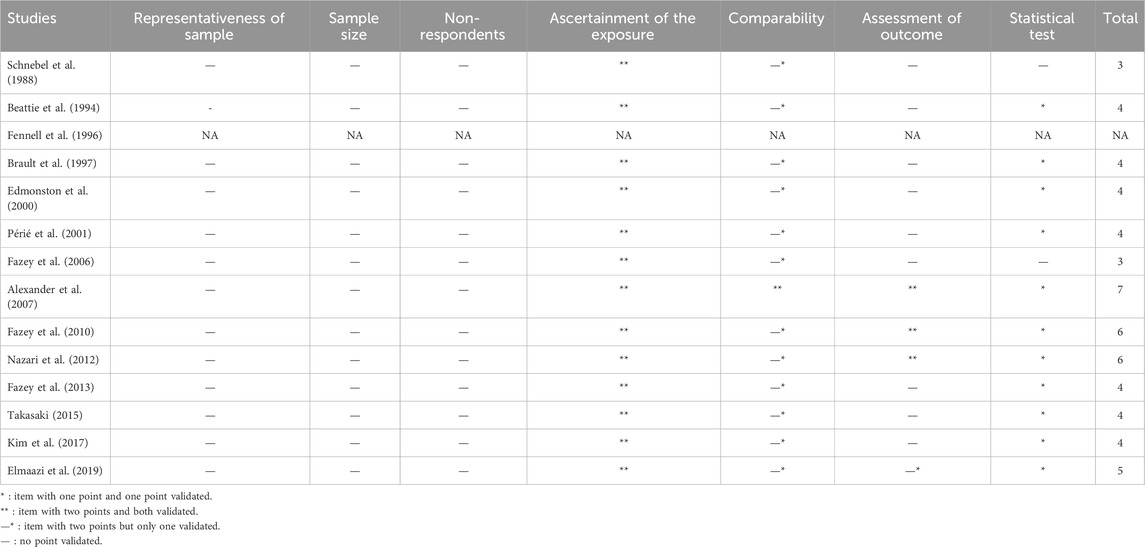
Risk of bias
Methodological quality assessment of the retained studies is reported in Table 3. The overall quality is low to fair, and risk of bias is high (score on the NOS ranging from 3 to 7). Two (14.2%) (Alexander et al., 2007; Fazey et al., 2010; Nazari et al., 2012) scored above six out of 10 and one scored 7 (7.1%) (Alexander et al., 2007). In all studies, we did not find any attempt at a priori sample size justification (Gill et al., 1987; Schnebel et al., 1988; Beattie et al., 1994; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; Fazey et al., 2010; Fazey et al., 2013; Alexander et al., 2007; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017; Elmaazi et al., 2019). In all of the 13 studies including asymptomatic subjects (92.8%), only young people with no sign of disc degeneration or pathologies were included. The 10 (71.4%) lower ranked studies did not properly describe methods used to assess the main outcome (e.g., blind analysis) (Gill et al., 1987; Schnebel et al., 1988; Beattie et al., 1994; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; 2013; Takasaki, 2015; Kim et al., 2017). Nearly all the studies used methods which ascertain the direction of movement imposed to the vertebral unit properly (either with MRI or discography). Finally, 11 studies (78.6%) performed statistical analysis (with confidence intervals) (Beattie et al., 1994; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Alexander et al., 2007; Fazey et al., 2010; 2013; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017; Elmaazi et al., 2019).
Reported bias assessment of the meta-analysis (meta-proportion for objective 1, Figure 3) is high with a LFK index = −4.43 and a left skewed asymmetric Doi plot.
Results of syntheses
Narrative synthesis of the dynamic behavior of the NP assessment
We identify two image acquisition methods (T2w-MRI and discography procedures) and four image analysis methods (distance boundaries, peak pixel intensity, pixel intensity profilometry, centroid method).
Regarding image acquisition, 13 studies utilized MRI (Beattie et al., 1994; Fennell et al., 1996; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; Fazey et al., 2010; Fazey et al., 2013; Alexander et al., 2007; Takasaki H et al., 2010; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017; Elmaazi et al., 2019), with significant heterogeneity in the acquisition methods.
• Magnetic field ranged from 0.2 to 3 T.
• Slice thicknesses ranged from 4 to 8 mm.
• Field of view ranged from 18 to 35 cm.
• Echo time ranged from 16 to 120 milliseconds.
• Repetition time ranged from 312 to 5,160 milliseconds (see Table 4).
• No study reported in-plane pixel sizes.
Only one study utilized discography to obtain the images (Schnebel et al., 1988). The authors described a lateral approach for the contrast agent injection and used X-ray from a lateral plane to observe the diffusion of the contrast agent.
Regarding the four image analysis methods: (i) Five studies (Beattie et al., 1994; Fennell et al., 1996; Nazari et al., 2012; Kim et al., 2017; Elmaazi et al., 2019) utilizing MRI and the one utilizing discography (Schnebel et al., 1988) used distance boundaries. The latter consist in calculating the distance from the margin of the NP to the margin of disc and two of those studies reported (Kim et al., 2017; Elmaazi et al., 2019) appropriate reliability indicators with ICC ranging from 0.77 to 0.94 and SEM from 0.26 to 0.37 mm. (ii) Three studies (Brault et al., 1997; Edmondston et al., 2000; Alexander et al., 2007) used peak pixel intensity consisting in identifying the position of the maximum pixel intensity of the NP on a line which bisects the anterior and posterior limits of the intervertebral disc on a T2w image. The distance from the peak pixel intensity to the anterior limit of the disc was measured. Then the distance was converted from mm to % of the antero-posterior diameter of the intervertebral disc. Two studies reported ICC ranging from 0.71 to 0.97, and one reported SEM of 4.3% (Edmondston et al., 2000; Alexander et al., 2007). (iii) Four studies (Fazey et al., 2006; Fazey et al., 2010; Fazey et al., 2013; Takasaki, 2015) used pixel intensity profilometry, which consists of extracting grayscale intensity values from T2-weighted MRI images across the full diameter of the intervertebral disc. Specifically, the intensity values were sampled along 3 to 55 image matrix lines (i.e., rows or columns of the MRI image matrix) that passed through the nucleus pulposus, spanning from one boundary of the disc to the other (e.g., right to left). Each line was rescaled to a 100-point normalized axis to account for variations in disc size. The intensity values were then plotted as a function of this normalized position, generating a pixel intensity profile. Two main parameters were derived from this curve: (i) the distance between the point of maximum intensity and the nearest disc boundary, and (ii) the centroid of the area under the curve, defined as the point dividing the total area under the intensity curve into two equal halves. One study (Takasaki, 2015) reported an ICC >0.8, the others do not report reliability measurement. (iv) One study (Périé et al., 2003) used the centroid method consisting in determining the centroid by segmenting the NP and the two adjacent vertebrae. After computing the centroids of each vertebra, a midpoint was established between them. The distance from this midpoint to the NP’s centroid was then measured. The study (Périé et al., 2003) did not report ICC or SEM values.
All the MRI studies assessed intact discs, with a NP behavior consistent with the prediction of the DDM. In the discography study, the authors assessed patients with both normal and abnormal discs. Abnormal discs were those in which the injection reproduced the patient’s pain, allowing for a classification as discogenic pain, but the authors did not report more information regarding the morphology of the disc (presence of a fissure, size, orientation). From our results, it is the only study assessing the behavior of the NP in a discogenic pain population. The contrast agent did not move as predicted by the DDM for abnormal discs, whereas it did for the normal disc. They also reported an opposite behavior with the L5-S1 abnormal disc, where the contrast agent was seen to migrate posteriorly with an extension load.
Quantitative synthesis
From the 10 analyzed studies, the global proportion of NP behaving as predicted by the DDM was 85.4% (CI95% = [79.4–91.4]). The NP behavior as predicted by the DDM was 86% (CI95% = [76.8–95.2]) for deformation of the NP in the sagittal plane following lumbar sagittal bending load (flexion/extension), 83.2% (95CI% [73.27–93.2]) for deformation of the NP in the sagittal plane following cervical sagittal bending load (flexion/extension), and 90.4% (95CI% = [81.9–98.9]) for deformation of the NP in the frontal plane following lumbar frontal bending load (side bending or side gliding).
Regarding lumbar axial rotation, the interpretation of NP deformation remains uncertain due to a lack of clarity in the experimental setups described in the two original studies. In particular, one study reported inducing “left trunk rotation” by placing a foam wedge under the left hemipelvis, but without specifying whether the shoulders were constrained or allowed to follow the rotation. As a result, the actual orientation of trunk rotation—clockwise or counterclockwise from a cranio-caudal perspective—cannot be determined with certainty. Because this information is essential to assess whether the nucleus pulposus moved in the same direction as the rotation or in the opposite direction (as predicted by the DDM), these data could not be reliably interpreted. For this reason, the results from these two studies were excluded from the meta-analysis.
Heterogeneity was high with I2 = 81.2% (Figure 4).
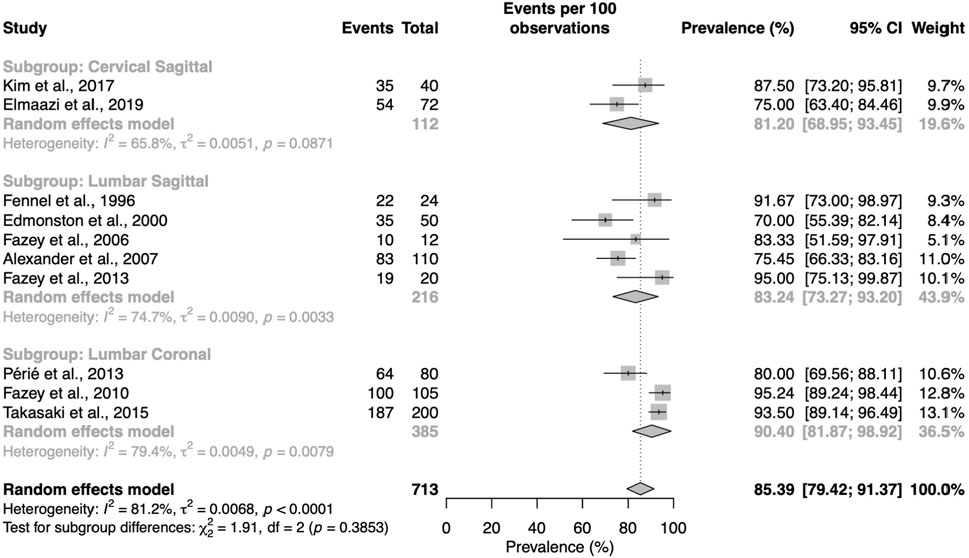
Figure 4. Proportion meta-analysis for intact discs and doi plot. The proportion is the total cases of interest (column Number) representing the number of experimental observations in which the DDM is confirmed. The size of the sample (column Total) represents the total number of observation), e.g., if a study assesses 10 discs in flexion and extension, we have a sample size of 20 observations.
Discussion
Our systematic review included 14 studies. It showed a consistent behavior of the NP across spinal levels and plans of movement among young and asymptomatic subjects with no pathological disc. We identified two different imaging modalities and four image analysis methods to characterize the NP behavior. Our meta-analysis included 10 studies. It showed that the NP behavior supported the dynamic disc model (DDM) in 85.4% of the observations, with 83.2% in the sagittal plane following lumbar sagittal bending load, 81.2% in the sagittal plane following cervical sagittal bending load, and 90.4% in the frontal plane following lumbar frontal bending load. Studies showed low quality evidence for intact discs and high heterogeneity (I2 = 81.2%) (Shah et al., 1978; Beattie et al., 1994; Fennell et al., 1996; Brault et al., 1997; Edmondston et al., 2000; Périé et al., 2003; Fazey et al., 2006; 2010; 2013; Alexander et al., 2007; Nazari et al., 2012; Takasaki, 2015; Kim et al., 2017; Elmaazi et al., 2019).
The dynamic disc model for intact and fissured discs
Our results for lumbar intact intervertebral discs subjected to flexion/extension tend to align with those of the previous systematic review (Kolber and Hanney, 2009). In addition to this trend, we conducted a meta-analysis and determined that 85.4% [79.4–91.4] of the observations were coherent with the prediction of the Disc Displacement Model (DDM). Moreover, in contrast to the previous review, we identified results for the lumbar spine in other planes of movement, with side bending/gliding (90.4% [79.4–98.9]), as well as for the cervical spine in the sagittal plane (81.2% [68.9–93.4]). These meta-analyses and results for other planes of movement and spine regions allow a more precise understanding of the behavior of the nucleus pulposus (NP) when the intervertebral disc is subjected to loads.
Although the DDM provides clear predictions for NP behavior under sagittal and frontal bending loads, its applicability to rotational movements remains uncertain. In this review, two studies investigated the deformation of the NP during axial trunk rotation (Fazey et al., 2006; Fazey et al., 2013). However, due to methodological ambiguities, it is not possible to draw meaningful conclusions from their results. In particular, these two studies described inducing “left trunk rotation” by placing a foam wedge under the left hemipelvis, but did not specify whether the shoulders were fixed or allowed to follow the pelvic movement. This omission makes it impossible to determine the actual orientation of trunk rotation (i.e., clockwise or counterclockwise from a cranio-caudal perspective), which is a critical parameter for interpreting the direction of NP displacement in relation to the DDM.
Furthermore, both studies lacked sufficient detail on the kinematic conditions to distinguish whether the applied loads represented pure axial rotation or were combined with side bending or gliding. As interpretation of NP behavior in the DDM relies on well-defined loading directions, this lack of clarity prevents any reliable comparison. For these reasons, the data from these two studies were excluded from the meta-analysis, and no conclusions can be drawn regarding the effect of axial rotation on NP displacement within the framework of the DDM.
Although promising in most of the different bending planes, the heterogeneity of the results compels caution when interpreting them. Nazari et al. (2012) provided another interpretation of the NP behavior, suggesting an elongation of the nucleus pulposus with flexion. They argued that elongation of the NP with flexion shortens the distance between the posterior wall of the NP and the posterior wall of the annulus fibrosus, inducing a perceptual impression of backward displacement. However, the distance between the anterior wall of the annulus and the nucleus also shortens, demonstrating a global elongation of the NP and not a backward displacement. The opposite phenomenon (contraction of the NP) is observed with extension loads. Whereas the data presented by Nazari et al. (2012) support elongation/contraction (strain) of the NP hypothesis, no extensive literature was available for supporting this. The authors suggested that the illusion of movement measured in the other studies results from the measurement methods limited to only a part of the NP and not the whole NP. Rather than viewing Nazari et al.'s hypothesis as entirely opposing the DDM, we could suggest that both mechanisms (displacement and strain) may coexist. Consequently, the current results suggesting nucleus pulposus displacement could be overestimated due to the concurrent phenomenon of strain. The contraction/elongation phenomenon of the NP, combined with displacement of the NP, makes the transformation of NP following bending loads more complex than expected. This hypothesis should be considered in future research.
The dynamic disc model for fissured discs
One study evaluated the DDM in the context of discogenic pain using provocative discography (Schnebel et al., 1988). In this study, the authors analyzed the behavior of the contrast agent injected into the disc during flexion and extension movements. The contrast agent injected into discs identified as abnormal through discography exhibited erratic and unpredictable behavior. In the case of L5/S1 levels, this behavior was even contrary to the expected behavior. However, several limitations must be considered. Firstly, Schnebel et al. (1988) classified discs as normal or abnormal but did not clearly specify the presence of a radial fissure or its orientation. Radial fissures can be oriented in any direction within the disc (Yu et al., 1988; Saifuddin et al., 1998; Bogduk et al., 2013). To properly test the DDM, the bending load should be oriented in the direction of the fissure. If this condition is not met, erratic results could be obtained. Secondly, the dimensions of the fissure can sufficiently alter the disc to the point of rendering the DDM inoperative. In this scenario, the DDM may not be applicable in all cases of radial fissures but only in those where the fissure exists in certain dimensions. Thirdly, as these data suggested, the disc could behave differently depending on the level of the spine under study, especially noticeable in L5-S1. Lastly, the differences in mechanical properties (Iatridis et al., 1996) between the contrast agent (liquid) and the NP (viscoelastic solid) might cause the unpredictable behavior. This finding aligns with an ex vivo study (not included in this review), suggesting that the DDM is invalid in the context of a fissured disc (Gill et al., 1987). However, no firm conclusion on the invalidity of the DDM in a context of fissured disc could be made due to the paucity of published work in the field as well as the methodological issues raised previously. Future research is necessary.
Methodological considerations for assessing DDM
Two imaging modalities were identified for the evaluation of DDM. On the one hand, discography was used in one study retained in this work and several excluded studies (ex vivo) (Shah et al., 1978; Gill et al., 1987; Schnebel et al., 1988). This method involves the injection of a contrast agent into the patient’s disc. The liquid induces mechanical distension of the inner part of the disc, replicating the primary consultation pain if the disc is to be considered a source of nociception. In healthy discs, participants reported discomfort or atypical pain only. Using X-ray or CT scan, diffusion of the contrast agent within the disc could be observed (Bogduk, 2013), as a component of the criteria for establishing the diagnosis of discogenic pain. To our knowledge, this approach is the only one that provides visualization of the shape, size, and orientation of disc’s radial fissure in vivo. Yet, X-ray/CT scan-based discography presents two major drawbacks in addition to being ionizing. First, discography is invasive and seem to accelerate the degeneration of the disc (Carragee et al., 2009), which could limit its use in future research. Secondly, discography is limited as it provides visualization of the contrast agent only, and not the NP. Therefore, inferences from studies using discography are based on the behavior of the contrast agent rather than that of the NP.
The second approach relies on T2-weighted MR images (T2w) and does not use contrast medium injection, making it not only non-ionizing but also non-invasive as opposed to discography. Additionally, T2w MRI allows for direct visualization of the NP, facilitating direct measurement of mechanical transformations. However, T2w MRI suffers from different limitations. To our knowledge, direct visualization of the radial fissure in the annulus fibrosus in vivo using MRI has never been reported using T2-weighted images. This limitation does not cause concerns regarding DDM research in healthy discs, but leads to major issues when evaluating DDM in the context of a fissured disc. Some authors describe changes in the signal within the AF, called a High-Intensity Zone (HIZ) (Aprill and Bogduk, 1992), that might be wrongly attributed to radial fissure visualization, although it seems to reflect the granulation tissue infiltrating the radial fissure instead (Ross et al., 1990). Finally, contrast in T2w MRI is influenced by the age and tissue degeneration, illustrated by decreased NP signal intensity (Pfirrmann et al., 2001). Therefore, in aging populations, differentiating between the NP and AF is less evident with T2w MRI, making image analysis challenging.
To date, despite their usability, both discography and T2w MRI provide limited information about the complexity of characterizing the NP and its mechanical response to loading in patients presenting with potentially fissured discs.
Future research perspectives and recommendations
Recent imaging developments combine different MRI methods, including quantitative techniques like diffusion (Beattie PF et al., 2009), relaxometry (Deneuville et al., 2021) and spectroscopy (Gornet et al., 2019), to enable a multiparametric approach (Stabile et al., 2020). Relaxometry computes pixel-wise maps of the absolute T1 and T2 relaxation times of the targeted structures, while T2w MRI sequences provide images in shades of gray which contrast highly depending on the acquisition parameters and MRI hardware. Hence, quantitative T1 and T2 relaxometry mapping provides more objective and consistent imaging compared to conventional T2-weighted sequences (Deoni, 2010). In a proof-of-concept study on cadaveric ovine samples, Deneuville et al. (2021), employed quantitative relaxometry mapping to detect radial fissures in the AF and to monitor NP migration under bending loads, both inside and outside the fissure. Diffusion MRI captures the diffusion of water molecules in tissues. Considering the NP’s high-water content, diffusion MRI emerges as a pertinent choice. Beattie et al. (2009) leveraged this feature and measured variations in the NP’s apparent diffusion coefficient following manual therapy loading procedures. Magnetic resonance spectroscopy (MRS) is sensitive to chemical shift differences between molecules and informs on their concentration levels in tissues. Gornet et al. (2019) demonstrated the capability of MRS to distinguish between painful and non-painful discs. Compared to discography, MRS was able to classify 206 painful/non-painful discs with an average 80% sensitivity and 86% in specificity, which increased to 91% and 93% respectively in non-herniated discs. By combining T2w MRI and a deep learning algorithm, Waldenberg et al. (2022) were able to accurately identify radial fissures (100% sensitivity and 97% specificity) compared to discography. However, despite this very good diagnostic performance, their method did not allow for the direct visualization of the fissure itself—as regards its orientation, length, or precise anatomical extent. This recent advance in MRI data processing opens new avenues for radial fissure detection and characterization. Beyond basic research, visualizing radial fissures in the AF, pinpointing NP positioning, and correlating with symptoms and symptom changes could be a new clinical tool. Multiparametric MRI might supersede invasive discography, potentially guiding clinical decisions for surgeons, physiotherapists, and physicians.
For future DDM fissure research, we recommend adopting a test–intervention–retest methodology. This would require a baseline MRI (test), spinal loading via repeated movements (intervention), and a post-intervention MRI (retest). While some researchers have used this design, it has not been applied to a group with identified radial fissures in the AF (Abdollah et al., 2018).
A considerable challenge in the future will consist in managing the duration of multiparametric MRI sequences, considering both patient comfort and equipment availability. To address this, advanced computational techniques—such as finite element analysis and musculoskeletal multibody modeling—can be leveraged. For instance, Remus and colleagues proposed and validated an open-source model based on the ArtiSynth framework, integrating finite element and multibody approaches to create a comprehensive numerical model of the spine (Remus et al., 2021). This model constitutes a solid foundation for the development of more refined and patient-specific simulations. When combined with deep learning algorithms, such modeling techniques offer promising avenues for characterizing the mechanical properties of the nucleus pulposus (NP) under various loading configurations and for tailoring simulations to individual patients using the concept of numerical twins (Asad et al., 2023). Digital twin approaches have already found applications in clinical practice, notably for simulating postoperative risks following knee surgery (Aubert et al., 2021), as well as for modeling vertebroplasty procedures to predict the mechanical response of the treated vertebral body (Ahmadian et al., 2022a; Ahmadian et al., 2022b). Unlike static image-based assessments, numerical models provide a dynamic and integrative mechanical evaluation, enabling the analysis of displacements and deformations across all three anatomical planes and within the full spinal structure.
Limitations
The present study has several acknowledged limitations. The high heterogeneity in the proportional meta-analysis influenced by the non-standardization of measurement protocols provided limited evidence to draw objective conclusions. The paucity and heterogeneity of available literature prevented meta-analyses addressing several secondary aims related to the dose-response relationship between bending load and mechanical transformation of the NP and the association between NP migration into a radial fissure and the centralization phenomenon.
No study meeting our inclusion criteria to address association between centralization phenomenon and NP mechanical behavior could be identified. Three studies have demonstrated the high specificity (from 0.7 to 0.95) of centralization phenomenon for discogenic pain (Donelson et al., 1997; Young et al., 2003; Laslett et al., 2005). Although these studies do not demonstrate the association between the behavior of the NP and pain variation, they indicate that the intervertebral disc is the implicated anatomical source of nociception. Therefore, it seems essential to test various hypotheses that could explain this pain behavior. Additionally, we identified a case study showing the association between symptom variation and changes in the position of the NP (identified by MRI and pixel intensity profilometry) (Takasaki et al., 2010). Although this article does not allow for any definitive conclusions, it may be considered proof-of-concept to be replicated on a larger scale. Future research should be conducted to evaluate the relationship between centralization and NP mechanical behavior.
Conclusion
Based on different methods of image acquisition and analysis to characterize the NP behavior, the DDM was accurate for intact discs in 85.4% of the observations, regardless of the movement plane and the spinal region. Additionally, the DDM was found to be accurate in 81.2% of cases in the sagittal plane for the cervical region and 83.2% for the lumbar region. Accuracy was 90.4% for the lumbar region in frontal plane, respectively. However, based on experimental study results, the relevance of the dynamic disc model (DDM) showed however low evidence quality for intact discs. Whereas data for fissured discs suggested an invalidity of the DDM, no strong conclusion can be reached due to paucity of available data and methodological limitations. Discography and MRI approaches are the most commonly used methods for characterizing NP properties. We recommend exploring new multiparametric MRI approaches in future studies, which may enhance our understanding of disc mechanics as well as inform future clinical assessment and therapeutic pathways.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
J-PD: Conceptualization, Formal Analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review and editing. MB: Project administration, Supervision, Validation, Writing – original draft, Writing – review and editing. AC: Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review and editing. SP: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. MM: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. MK: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. ME: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. MB: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. AP: Data curation, Formal Analysis, Software, Writing – original draft, Writing – review and editing. RD: Methodology, Project administration, Resources, Software, Supervision, Writing – original draft, Writing – review and editing. MR: Project administration, Resources, Validation, Writing – original draft, Writing – review and editing. AO: Formal Analysis, Software, Visualization, Writing – original draft, Writing – review and editing. ML: Supervision, Validation, Writing – original draft, Writing – review and editing. MS: Resources, Validation, Visualization, Writing – original draft, Writing – review and editing. NS: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review and editing. AG: Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review and editing. PR: Conceptualization, Resources, Supervision, Validation, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank Karine Furcy, Catherine Weill, Colin Cidre, Aurélie Morichon, Dr Romain Artico and Prof. Yannick Toussignant Laflamme tor their help us with the literature review equation and research. We also wish to thank Julien Louis for his help with the figure illustration. Finally, we thank Joevin Burnel for his careful reviewing and quality assessment using the AMSTAR-2 scale.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2025.1582438/full#supplementary-material
References
Abdollah, V., Parent, E. C., and Battié, M. C. (2018). MRI evaluation of the effects of extension exercises on the disc fluid content and location of the centroid of the fluid distribution. Musculoskelet. Sci. Pract. 33, 67–70. doi:10.1016/j.msksp.2017.11.008
Ahmadian, H., Mageswaran, P., Walter, B. A., Blakaj, D. M., Bourekas, E. C., Mendel, E., et al. (2022a). A digital twin for simulating the vertebroplasty procedure and its impact on mechanical stability of vertebra in cancer patients. Numer. Methods Biomed. Eng. 38, e3600. doi:10.1002/cnm.3600
Ahmadian, H., Mageswaran, P., Walter, B. A., Blakaj, D. M., Bourekas, E. C., Mendel, E., et al. (2022b). Toward an artificial intelligence -assisted framework for reconstructing the digital twin of vertebra and predicting its fracture response. Numer. Methods Biomed. Eng. 38, e3601. doi:10.1002/cnm.3601
Alexander, L. A., Hancock, E., Agouris, I., Smith, F. W., and MacSween, A. (2007). The response of the nucleus pulposus of the lumbar intervertebral discs to functionally loaded positions. Spine (Phila Pa 1976) 32, 1508–1512. doi:10.1097/BRS.0b013e318067dccb
Aprill, C., and Bogduk, N. (1992). High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. BJR 65, 361–369. doi:10.1259/0007-1285-65-773-361
Asad, U., Khan, M., Khalid, A., and Lughmani, W. A. (2023). Human-centric digital twins in industry: a comprehensive review of enabling technologies and implementation strategies. Sensors 23, 3938. doi:10.3390/s23083938
Aubert, K., Germaneau, A., Rochette, M., Ye, W., Severyns, M., Billot, M., et al. (2021). Development of digital twins to optimize trauma surgery and postoperative management. A case study focusing on tibial plateau fracture. Front. Bioeng. Biotechnol. 9, 722275. doi:10.3389/fbioe.2021.722275
Beattie, P. F., Brooks, W. M., Rothstein, J. M., Sibbitt, W. L., Robergs, R. A., MacLean, T., et al. (1994). Effect of lordosis on the position of the nucleus pulposus in supine subjects: a study using magnetic resonance imaging. Spine 19, 2096–2102. doi:10.1097/00007632-199409150-00017
Beattie, P. F., Donley, J. W., Arnot, C. F., and Miller, R. (2009). The change in the diffusion of water in normal and degenerative lumbar intervertebral discs following joint mobilization compared to prone lying. J. Orthop. and Sports Phys. Ther. 39, 4–11. doi:10.2519/jospt.2009.2994
Bogduk, N. (2013). Practice guidelines for spinal diagnostic and treatment procedures. 2nd Edn. San Francisco, CA: International Spine Intervention Society.
Bogduk, N., Aprill, C., and Derby, R. (2013). Lumbar discogenic pain: state-of-the-art review: lumbar discogenic pain. Pain Med. 14, 813–836. doi:10.1111/pme.12082
Brault, J. S., Driscoll, D. M., Laakso, L. L., Kappler, R. E., Allin, E. F., and Glonek, T. (1997). Quantification of lumbar intradiscal deformation during flexion and extension, by mathematical analysis of magnetic resonance imaging pixel intensity profiles. Spine (03622436) 22, 2066–2072. doi:10.1097/00007632-199709150-00002
Carragee, E. J., Don, A. S., Hurwitz, E. L., Cuellar, J. M., Carrino, J., and Herzog, R. (2009). 2009 issls prize winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine 34, 2338–2345. doi:10.1097/BRS.0b013e3181ab5432
Cheema, H. A., Shahid, A., Ehsan, M., and Ayyan, M. (2022). The misuse of funnel plots in meta-analyses of proportions: are they really useful? Clin. Kidney J. 15, 1209–1210. doi:10.1093/ckj/sfac035
Cyriax, J. (1950). The treatment of lumbar disk lesions. Br. Med. J. 2, 1434–1438. doi:10.1136/bmj.2.4694.1434
Deneuville, J.-P., Yushchenko, M., Vendeuvre, T., Germaneau, A., Billot, M., Roulaud, M., et al. (2021). Quantitative MRI to characterize the nucleus pulposus morphological and biomechanical variation according to sagittal bending load and radial fissure, an ex vivo ovine specimen proof-of-concept study. Front. Bioeng. Biotechnol. 9, 676003. doi:10.3389/fbioe.2021.676003
Deoni, S. C. L. (2010). Quantitative relaxometry of the brain. Top. Magnetic Reson. Imaging 21, 101–113. doi:10.1097/RMR.0b013e31821e56d8
Donelson, R., Aprill, C., Medcalf, R., and Grant, W. (1997). A prospective study of centralization of lumbar and referred pain: a predictor of symptomatic discs and anular competence. Spine 22, 1115–1122. doi:10.1097/00007632-199705150-00011
Edmondston, S. J., Song, S., Bricknell, R. V., Davies, P. A., Fersum, K., Humphries, P., et al. (2000). MRI evaluation of lumbar spine flexion and extension in asymptomatic individuals. Man. Ther. 5, 158–164. doi:10.1054/math.2000.0356
Elmaazi, A., Morse, C. I., Lewis, S., Qureshi, S., and McEwan, I. (2019). The acute response of the nucleus pulposus of the cervical intervertebral disc to three supine postures in an asymptomatic population. Musculoskelet. Sci. Pract. 44, 102038. doi:10.1016/j.msksp.2019.07.002
Fardon, D. F., Williams, A. L., Dohring, E. J., Murtagh, F. R., Gabriel Rothman, S. L., and Sze, G. K. (2014). Lumbar disc nomenclature: version 2.0. Spine J. 14, 2525–2545. doi:10.1016/j.spinee.2014.04.022
Fazey, P. J., Song, S., Mønsås, Å., Johansson, L., Haukalid, T., Price, R. I., et al. (2006). An MRI investigation of intervertebral disc deformation in response to torsion. Clin. Biomech. 21, 538–542. doi:10.1016/j.clinbiomech.2005.12.008
Fazey, P. J., Song, S., Price, R. I., and Singer, K. P. (2013). Nucleus pulposus deformation in response to rotation at L1–2 and L4–5. Clin. Biomech. 28, 586–589. doi:10.1016/j.clinbiomech.2013.03.009
Fazey, P. J., Takasaki, H., and Singer, K. P. (2010). Nucleus pulposus deformation in response to lumbar spine lateral flexion: an in vivo MRI investigation. Eur. Spine J. 19, 1115–1120. doi:10.1007/s00586-010-1339-4
Fennell, A. J., Jones, A. P., and Hukins, D. W. (1996). Migration of the nucleus pulposus within the intervertebral disc during flexion and extension of the spine. Spine (Phila Pa 1976) 21, 2753–2757. doi:10.1097/00007632-199612010-00009
Fredericson, M., Lee, S.-U., Welsh, J., Butts, K., Norbash, A., and Carragee, E. J. (2001). Changes in posterior disc bulging and intervertebral foraminal size associated with flexion-extension movement:. Spine J. 1, 10–17. doi:10.1016/s1529-9430(01)00014-6
Furuya-Kanamori, L., Barendregt, J. J., and Doi, S. A. R. (2018). A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evidence-Based Healthc. 16, 195–203. doi:10.1097/XEB.0000000000000141
García-Cosamalón, J., Del Valle, M. E., Calavia, M. G., García-Suárez, O., López-Muñiz, A., Otero, J., et al. (2010). Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? intervertebral disc, sensory nerves and neurotrophins. J. Anat. 217, 1–15. doi:10.1111/j.1469-7580.2010.01227.x
Gill, K., Videman, T., Shimizu, T., and Mooney, V. (1987). The effect of repeated extensions on the discographic dye patterns in cadaveric lumbar motion segments. Clin. Biomech. 2, 205–210. doi:10.1016/0268-0033(87)90083-0
Gornet, M. G., Peacock, J., Claude, J., Schranck, F. W., Copay, A. G., Eastlack, R. K., et al. (2019). Magnetic resonance spectroscopy (MRS) can identify painful lumbar discs and may facilitate improved clinical outcomes of lumbar surgeries for discogenic pain. Eur. Spine J. 28, 674–687. doi:10.1007/s00586-018-05873-3
Guyatt, G. H., Oxman, A. D., Vist, G. E., Kunz, R., Falck-Ytter, Y., Alonso-Coello, P., et al. (2008). GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926. doi:10.1136/bmj.39489.470347.ad
J. P. T. Higgins, and C. Collaboration (2020). Cochrane handbook for systematic reviews of interventions. Second edition (Hoboken, NJ: Wiley-Blackwell).
Hoy, D., Bain, C., Williams, G., March, L., Brooks, P., Blyth, F., et al. (2012). A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism 64, 2028–2037. doi:10.1002/art.34347
Hunter, J. P., Saratzis, A., Sutton, A. J., Boucher, R. H., Sayers, R. D., and Bown, M. J. (2014). In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 67, 897–903. doi:10.1016/j.jclinepi.2014.03.003
Iatridis, J. C., Weidenbaum, M., Setton, L. A., and Mow, V. C. (1996). Is the nucleus pulposus a solid or a fluid? Mechanical behaviors of the nucleus pulposus of the human intervertebral disc: spine. Spine Phila. pa. 1976. 21, 1174–1184. doi:10.1097/00007632-199605150-00009
Kim, Y.-H., Kim, S.-I., Park, S., Hong, S. H., and Chung, S. G. (2017). Effects of cervical extension on deformation of intervertebral disk and migration of nucleus pulposus. PM&R 9, 329–338. doi:10.1016/j.pmrj.2016.08.027
Kolber, M. J., and Hanney, W. J. (2009). The dynamic disc model: a systematic review of the literature. Phys. Ther. Rev. 14, 181–189. doi:10.1179/174328809x452827
Krag, M. H., Seroussi, R. E., Wilder, D. G., and Pope, M. H. (1987). Internal displacement distribution from in vitro loading of human thoracic and lumbar spinal motion segments: experimental results and theoretical predictions. Spine 12, 1001–1007. doi:10.1097/00007632-198712000-00011
Lama, P., Le Maitre, C. L., Harding, I. J., Dolan, P., and Adams, M. A. (2018). Nerves and blood vessels in degenerated intervertebral discs are confined to physically disrupted tissue. J. Anat. 233, 86–97. doi:10.1111/joa.12817
Landis, J. R., and Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics 33, 159. doi:10.2307/2529310
Laslett, M., Öberg, B., Aprill, C. N., and McDonald, B. (2005). Centralization as a predictor of provocation discography results in chronic low back pain, and the influence of disability and distress on diagnostic power. Spine J. 5, 370–380. doi:10.1016/j.spinee.2004.11.007
Maher, C., Underwood, M., and Buchbinder, R. (2017). Non-specific low back pain. Lancet 389, 736–747. doi:10.1016/S0140-6736(16)30970-9
Naiditch, N., Billot, M., Goudman, L., Cornet, P., Roulaud, M., Ounajim, A., et al. (2021a). Professional status of persistent spinal pain syndrome patients after spinal surgery (PSPS-T2): what really matters? A prospective study introducing the concept of “adapted professional activity” inferred from clinical, psychological and social influence. JCM 10, 5055. doi:10.3390/jcm10215055
Naiditch, N., Billot, M., Moens, M., Goudman, L., Cornet, P., Le Breton, D., et al. (2021b). Persistent spinal pain syndrome type 2 (PSPS-T2), a social pain? Advocacy for a social gradient of health approach to chronic pain. JCM 10, 2817. doi:10.3390/jcm10132817
Nazari, J., Pope, M. H., and Graveling, R. A. (2012). Reality about migration of the nucleus pulposus within the intervertebral disc with changing postures. Clin. Biomech. 27, 213–217. doi:10.1016/j.clinbiomech.2011.09.011
Ounajim, A., Billot, M., Louis, P.-Y., Slaoui, Y., Frasca, D., Goudman, L., et al. (2021). Finite mixture models based on pain intensity, functional disability and psychological distress composite assessment allow identification of two distinct classes of persistent spinal pain syndrome after surgery patients related to their quality of life. JCM 10, 4676. doi:10.3390/jcm10204676
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ n71, n71. doi:10.1136/bmj.n71
Parent, E. C., Videman, T., and Battié, M. C. (2006). “The effect of lumbar flexion and extension on disc contour abnormality measured quantitatively on magnetic resonance imaging: spine,”Spine (Phila. pa. 1976), 31. 2836–2842. doi:10.1097/01.brs.0000245834.30646.aa
Périé, D., Curnier, D., and de Gauzy, J. S. (2003). Correlation between nucleus zone migration within scoliotic intervertebral discs and mechanical properties distribution within scoliotic vertebrae. Magn. Reson Imaging 21, 949–953. doi:10.1016/s0730-725x(03)00216-9
Pfirrmann, C. W. A., Metzdorf, A., Zanetti, M., Hodler, J., and Boos, N. (2001). Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26, 1873–1878. doi:10.1097/00007632-200109010-00011
Pincus, T., Burton, A. K., Vogel, S., and Field, A. P. (2002). A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 27, E109–E120. doi:10.1097/00007632-200203010-00017
Remus, R., Lipphaus, A., Neumann, M., and Bender, B. (2021). Calibration and validation of a novel hybrid model of the lumbosacral spine in ArtiSynth–The passive structures. PLoS ONE 16, e0250456. doi:10.1371/journal.pone.0250456
Ross, J. S., Modic, M. T., and Masaryk, T. J. (1990). Tears of the anulus fibrosus: assessment with Gd-DTPA-enhanced MR imaging. Am. J. Roentgenol. 154, 159–162. doi:10.2214/ajr.154.1.2136783
Saifuddin, A., Emanuel, R., White, J., Renton, P., Braithwaite, I., and Taylor, B. A. (1998). An analysis of radiating pain at lumbar discography. Eur. Spine J. 7, 358–362. doi:10.1007/s005860050090
Schnebel, B. E., Simmons, J. W., Chowning, J., and Davidson, R. (1988). A digitizing technique for the study of movement of intradiscal dye in response to flexion and extension of the lumbar spine. Spine (Phila Pa 1976) 13, 309–312. doi:10.1097/00007632-198803000-00014
Seroussi, R. E., Krag, M. H., Muller, D. L., and Pope, M. H. (1989). Internal deformations of intact and denucleated human lumbar discs subjected to compression, flexion, and extension loads. J. Orthop. Res. 7, 122–131. doi:10.1002/jor.1100070117
Shah, J., Hampson, W., and Jayson, M. (1978). The distribution of surface strain in the cadaveric lumbar spine. J. Bone Jt. Surg. Br. 60-B, 246–251. doi:10.1302/0301-620X.60B2.659474
Stabile, A., Giganti, F., Rosenkrantz, A. B., Taneja, S. S., Villeirs, G., Gill, I. S., et al. (2020). Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nat. Rev. Urol. 17, 41–61. doi:10.1038/s41585-019-0212-4
Takasaki, H. (2015). Comparable effect of simulated side bending and side gliding positions on the direction and magnitude of lumbar disc hydration shift: in vivo MRI mechanistic study. J. Man. and Manip. Ther. 23, 101–108. doi:10.1179/2042618613Y.0000000059
Takasaki, H., May, S., Fazey, P. J., and Hall, T. (2010). Nucleus pulposus deformation following application of mechanical diagnosis and therapy: a single case report with magnetic resonance imaging. J. Man. and Manip. Ther. 18, 153–158. doi:10.1179/106698110X12640740712455
Vos, T., Allen, C., Arora, M., Barber, R. M., Bhutta, Z. A., Brown, A., et al. (2016). Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1545–1602. doi:10.1016/S0140-6736(16)31678-6
Waldenberg, C., Eriksson, S., Brisby, H., Hebelka, H., and Lagerstrand, K. M. (2022). Detection of imperceptible intervertebral disc fissures in conventional MRI—an AI strategy for improved diagnostics. JCM 12, 11. doi:10.3390/jcm12010011
Weishaupt, D., Schmid, M. R., Zanetti, M., Boos, N., Romanowski, B., Kissling, R. O., et al. (2000). Positional MR imaging of the lumbar spine: does it demonstrate nerve root compromise not visible at conventional MR imaging? Radiology 215, 247–253. doi:10.1148/radiology.215.1.r00ap06247
Young, S., Aprill, C., and Laslett, M. (2003). Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J. 3, 460–465. doi:10.1016/S1529-9430(03)00151-7
Yu, S., Sether, L. A., Ho’, P. S. P., Wagner, M., and Haughton’, V. M. (1988). Tears of the anulus fibrosus
Zamani, A. A., Moriarty, T., Hsu, L., Winalski, C. S., Schaffer, J. L., Isbister, H., et al. (1998). Functional MRI of the lumbar spine in erect position in a superconducting open-configuration MR system: preliminary results. J. Magn. Reson. Imaging 8, 1329–1333. doi:10.1002/jmri.1880080622
Zou, J., Yang, H., Miyazaki, M., Morishita, Y., Wei, F., McGovern, S., et al. (2009). Dynamic bulging of intervertebral discs in the degenerative lumbar spine, Dyn. Bulging Intervertebral Discs Degener. Lumbar Spine Spine 34, 2545–2550. doi:10.1097/BRS.0b013e3181b32998
Keywords: dynamic disc model, intervertebral disc biomechanics, systematic review/meta-analysis, low back pain, directional preference
Citation: Deneuville J-P, Billot M, Cervantes A, Peterlongo S, Meyer M, Kolder M, Escande M, Bourgeois M, Pallot A, David R, Roulaud M, Ounajim A, Laslett M, Sarracanie M, Salameh N, Germaneau A and Rigoard P (2025) Dynamic behavior of the nucleus pulposus within the intervertebral disc loading: a systematic review and meta-analysis exploring the concept of dynamic disc model. Front. Bioeng. Biotechnol. 13:1582438. doi: 10.3389/fbioe.2025.1582438
Received: 24 February 2025; Accepted: 01 May 2025;
Published: 06 June 2025.
Edited by:
Marwan El-Rich, Khalifa University, United Arab EmiratesReviewed by:
Nader M. Hebela, Cleveland Clinic Abu Dhabi, United Arab EmiratesJudith Meakin, University of Exeter, United Kingdom
Copyright © 2025 Deneuville, Billot, Cervantes, Peterlongo, Meyer, Kolder, Escande, Bourgeois, Pallot, David, Roulaud, Ounajim, Laslett, Sarracanie, Salameh, Germaneau and Rigoard. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jean-Philippe Deneuville, amVhbi5waGlsaXBwZS5kZW5ldXZpbGxlQHVuaXYtcG9pdGllcnMuZnI=
 Jean-Philippe Deneuville
Jean-Philippe Deneuville Maxime Billot
Maxime Billot Alexandra Cervantes2
Alexandra Cervantes2 Amine Ounajim
Amine Ounajim Mathieu Sarracanie
Mathieu Sarracanie Najat Salameh
Najat Salameh Arnaud Germaneau
Arnaud Germaneau