- 1Medical School of Chinese PLA, Beijing, China
- 2Department of Stomatology, The First Medical Centre, Chinese PLA General Hospital, Beijing, China
- 3Department of Stomatology, Beijing Friend ship Hospital, Capital Medical University, Beijing, China
- 4Department of Stomatology, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University, Beijing, China
Background: We developed olecranon-type tracheotomy and expansion forceps (OTEF) for emergency tracheotomy in patients experiencing acute airway obstruction. By using OTEF, medical rescue personnel can perform emergency tracheotomy more quickly and accurately on their own, while conventional tracheotomy requires the cooperation of two surgeons.
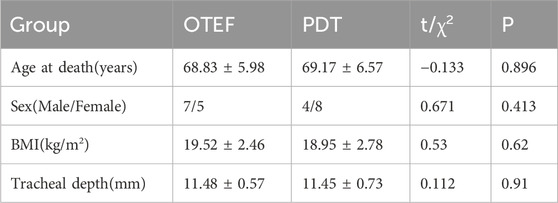
Methods: In this study, 24 adult cadavers that had died within 24 h were randomly assigned to the OTEF or PDT groups. Tracheotomies were performed by the same physician, using the OTEF technique for the OTEF group and the percutaneous dilational tracheotomy technique for the PDT group. The collected data included basic cadaver characteristics, operative time, incision length, and intraoperative tracheal wall injuries.
Results: In the OTEF group, the mean tracheotomy completion time was 96.83 ± 8.82 s, with a mean incision length of 13.67 ± 3.67 mm. In the PDT group, the mean tracheotomy completion time was 566.50 ± 47.14 s, and the mean incision length was 20.67 ± 4.76 mm. Compared with the PDT group, the OTEF group demonstrated significantly shorter operative times (P < 0.05) and smaller incision lengths (P < 0.05).
Conclusion: OTEF enables efficient and minimally traumatic tracheostomies in emergency settings with minimal environmental and positioning requirements. In disaster sites or even on battlefields where medical personnel are in short supply, this device can enhance the battlefield rescue skills and emergency response capabilities of non-medical rescue workers, effectively alleviate rescue pressure and save the lives of the injured.
1 Background
The airway is a vital component of human physiology, and its obstruction represents a critical medical emergency. When conventional airway management techniques are unsuccessful or impractical, tracheotomy serves as a life-saving procedure, offering a direct route for ventilation. Traditionally, this invasive intervention has been performed by medical teams in controlled environments, such as hospitals or operating rooms. However, in specific critical situations—such as prehospital settings, remote areas, or emergencies with limited medical personnel—the availability of a full team cannot be guaranteed.
Current devices and instruments for emergency airway access, including traditional tracheotomy kits and cricothyrotomy tools, are predominantly designed for collaborative use by multiple individuals. Clinicians commonly employ two main types of tracheostomies: surgical tracheotomy and percutaneous dilational tracheotomy (Karlsson et al., 2022). Relevant studies indicate no significant differences in mortality or the incidence of major complications—such as respiratory distress, hemorrhagic shock, or tracheal stenosis—between these two procedures. However, percutaneous tracheotomy is associated with shorter operation times and reduced risks of wound infection (Putensen et al., 2014). Consequently, many clinical guidelines recommend percutaneous dilation tracheotomy when there are no contraindications (Karlsson et al., 2022; Putensen et al., 2014; Ciaglia et al., 1985). To further reduce operation times and complications, various improved surgical techniques have been developed, including guidewire dilating forceps (Griggs et al., 1990), trans laryngeal tracheotomy (Fantoni and Ripamonti, 1997), Ciaglia Blue Rhin (Byhahn et al., 2000), cricoid membrane puncture-directed tracheotomy (Chen et al., 2018; Chen et al., 2015), and quick-response tracheotomy (Graeme, 2016). These techniques often require a team of operators: one to stabilize the patient’s anatomy, another to make the incision, and a third to secure and confirm airway placement. Such multi-operator requirements make these methods unsuitable for single-operator scenarios, where an individual must independently manage every aspect of the procedure. There is evidence to support the argument that advanced airway management can be performed in the prehospital setting without delaying transfer to a trauma center. When performed by skilled emergency medical services providers, advanced airway management is associated with a significant decrease in mortality (Kovacs and Sowers, 2018). This limitation has driven interest in designing instruments specifically tailored for single-person use, enabling safe and efficient emergency tracheotomies even under adverse conditions.
To address these challenges, we developed a novel instrument specifically designed for single-person emergency tracheotomies, focusing on simplicity, precision, and ease of use. The device integrates features that streamline the procedure, minimize error margins, and enhance safety in high-pressure situations. For instance, it allows a single operator to stabilize the patient’s airway, make an incision, and insert a tracheotomy tube in a sequential and controlled manner. This design process was informed by the challenges commonly encountered during emergency airway management and aimed to overcome the limitations of existing methods.
2 Methods
2.1 Materials
The research team independently designed an olecranon-type tracheotomy and expansion forceps, which has been submitted for invention patents (Patent number: ZL202011064693.2). The team aimed to integrate the tracheotomy and distraction instruments into a single device capable of performing both procedures. The team aimed to integrate a tracheotomy and distraction instrument into a single device capable of performing both tracheotomy and distraction procedures (Figure 1). The original design featured a straight tip. However, animal experiments revealed that the straight tip could easily injure the posterior tracheal wall during puncture. Moreover, the sharp tip posed a risk of scratching the tracheal mucosa during distraction. Consequently, the design was refined, resulting in the olecranon-shaped tracheotomy and distraction forceps. The device is fabricated from stainless steel, measures approximately 20 cm in length, and consists of a tip and a forceps handle. The front end of the forceps is sharp and arc-shaped. The inner surface of the arc features a sharp cutting edge, whereas the outer surface remains blunt. Graduated scales are engraved along the lateral aspect of the forceps, starting from the tip. When the forceps handle is closed, the jaws open, allowing the inner cutting edge to incise the trachea, thereby facilitating surgical manipulation. The device, fabricated from stainless steel, is approximately 20 cm in length and consists of a tip and a forceps handle. The front end of the forceps is sharp and arc-shaped. The inner surface of the arc features a sharp cutting edge, while the outer surface is blunt. Scales are engraved from the tip along the side of the forceps body. When the forceps handle is closed, the jaws open, allowing the inner cutting edge to incise the trachea, facilitating easier surgical manipulation.

Figure 1. Olecranon-type tracheotomy and expansion forceps. One side features a sharp cutting edge, with scales marked from the tip to the side of the forceps body.
2.2 Cadaver experiments
In this study, 24 non–formalin-fixed adult cadavers that had died within 24 h were enrolled. The cadavers were provided by the Body Donation Registration and Acceptance Station of the Chinese Academy of Medical Sciences and Peking Union Medical College. Each cadaver was intubated nasotracheally. A second physician conducted tracheal examinations with a fiberoptic bronchoscope to document intraoperative injuries during subsequent procedures.
A coupling agent was applied to the cadavers’ necks, after which a portable ultrasonic diagnostic device was used to visualize the neck structures (Figure 2). This procedure allowed measurement of the distance from the anterior wall of the trachea to the skin surface and identification of the optimal tracheotomy site. The duration of the ultrasound assessment was recorded for each cadaver.
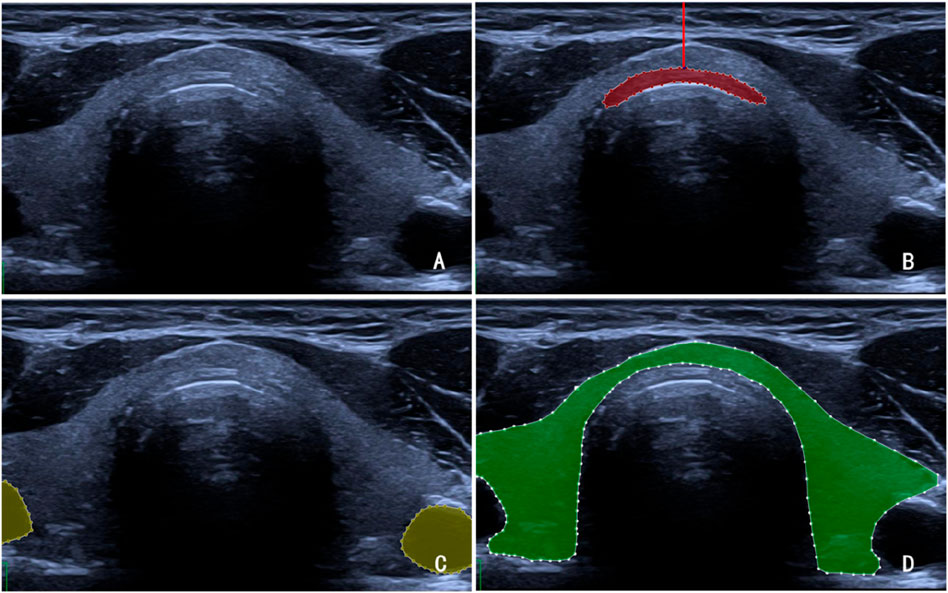
Figure 2. (A) Ultrasound image of a cadaver’s neck. (B) The red-shaded region in the figure denotes the tracheal rings, while the red line indicates the tracheal depth at that site, defined as the vertical distance from the trachea to the cervical skin surface. (C) The yellow-shaded region represents the vascular structures. (D) The green-shaded region represents the thyroid gland.
In the OTEF group, tracheotomy was performed using olecranon-type tracheotomy with expansion forceps, whereas in the PDT group, percutaneous dilational tracheotomy was performed. All procedures were conducted by the same surgeon to minimize operator variability. This experimental design enabled comparison of procedural feasibility, accuracy, and efficiency between the two tracheotomy techniques under controlled cadaveric conditions.
2.3 Tracheotomy procedure
The olecranon-type tracheotomy and expansion forceps were positioned parallel to the trachea’s long axis. The curved jaw tip was aligned perpendicularly to the skin over the trachea and inserted downward. The puncture depth was determined based on the distance measured by ultrasound, with an additional 1 cm added to ensure penetration of the trachea. Upon reaching the predetermined depth, the forceps were gradually rotated perpendicular to the skin so that the jaw tips shifted from vertical to horizontal alignment, minimizing the risk of posterior tracheal wall injury. The jaws were then opened to a length of approximately 2 cm, allowing the sharp inner edge of the arc-shaped jaws to incise the tracheal ring and pretracheal soft tissue longitudinally. An endotracheal tube was inserted between the open jaws and gradually advanced into the trachea. The forceps were then carefully withdrawn, and the inner core of the endotracheal tube was removed. The cuff was inflated, the tube was secured, and it was connected to a ventilator. The time required for the entire procedure was recorded.
After surgery, the endotracheal tube was removed, and a bronchoscope was used to examine postoperative airway damage and measure the incision length.
Fiberoptic bronchoscopy was performed to assess damage to the tracheal wall following the procedure (Figure 3).
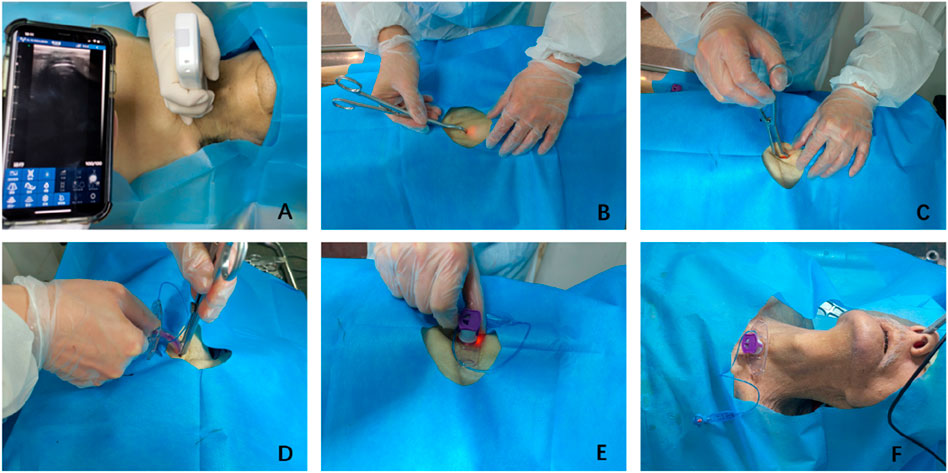
Figure 3. Surgical procedure. (A) Ultrasound examination to determine the puncture point. (B) Puncture into the trachea. (C) Reaching the predetermined depth and opening the forceps. (D) Inserting the tracheostomy tube into the trachea between the jaws. (E) Withdrawing the forceps. (F) Securing the tracheostomy tube.
2.4 Outcome measures
General measures: age at death, sex, Body mass index (BMI), and tracheal depth (the vertical distance from the anterior wall of the trachea to the skin surface).
Surgery-related measures: operative time, incision length, and the time required for tracheal intubation following the incision.
2.5 Statistical analysis
Statistical analyses were performed using SPSS software (IBM Corp., Chicago, IL, United States). P < 0.05 was considered statistically significant. The normality of continuous variables was evaluated using the Shapiro-Wilk test. Data with a normal distribution were expressed as mean ± standard deviation (SD) and compared using the independent-sample t-test, whereas non-normally distributed data were expressed as median (interquartile range) and analyzed using the Mann-Whitney U test. Categorical variables were presented as frequencies and percentages, and intergroup comparisons were performed using the Chi-squared test.
3 Results
Tracheotomy was successfully completed on all 24 cadavers. Fiberoptic bronchoscopy confirmed no damage to the tracheal wall (Figure 4).
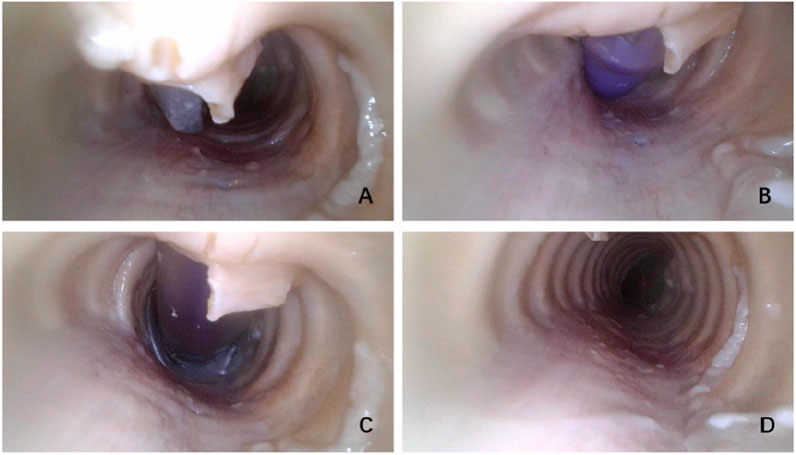
Figure 4. (A) Puncture into the trachea. (B) Tracheotomy tube insertion into the trachea. (C) Completed tracheotomy. (D) Postoperative examination of tracheal wall damage.
No significant differences were observed between the two groups in terms of age at death, sex, BMI, tracheal depth, or the time required for tracheal intubation following the incision (P > 0.05) (Table 1).
In the OTEF group, the mean tracheotomy completion time was 96.83 ± 8.82 s, with a mean incision length of 13.67 ± 3.67 mm. In the PDT group, the mean tracheotomy completion time was 566.50 ± 47.14 s, and the mean incision length was 20.67 ± 4.76 mm. Compared with the PDT group, the OTEF group demonstrated significantly shorter operative times (P < 0.05) and smaller incision lengths (P < 0.05) (Figure 5).
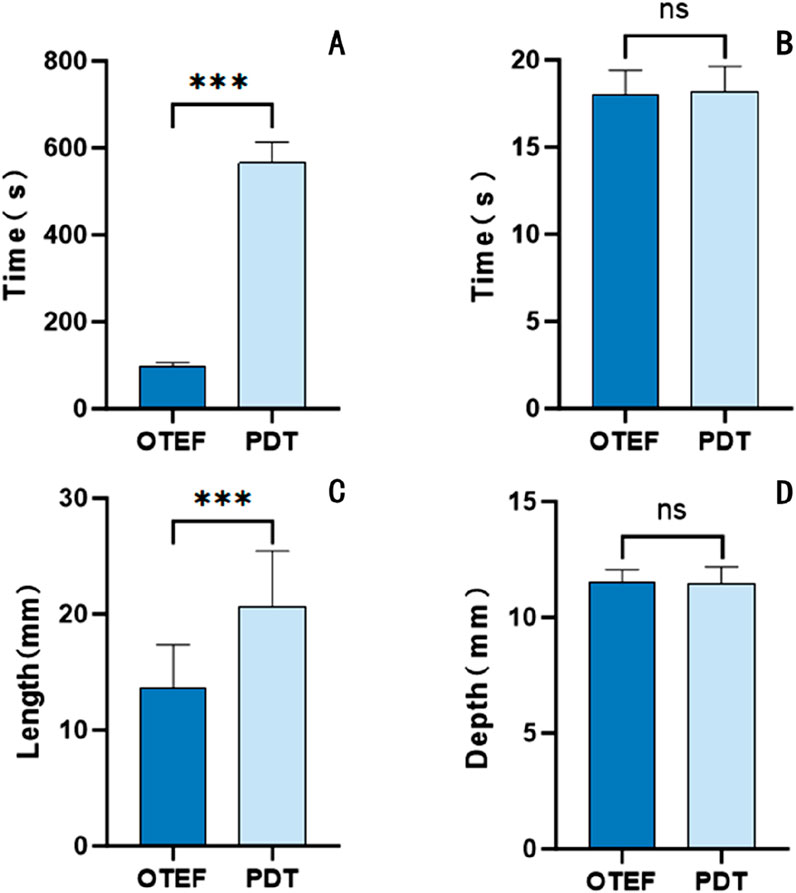
Figure 5. (A) Operation time: The mean operation time was 96.83 ± 8.82 s in the OTEF group and 566.50 ± 47.14 s in the PDT group, with a statistically significant difference (P < 0.001). (B) Time to tracheotomy tube insertion: The mean time was 18.00 ± 1.41 s in the OTEF group and 18.17 ± 1.47 s in the PDT group, with no significant difference (P > 0.05). (C) Incision length: The mean incision length was 13.67 ± 3.67 mm in the OTEF group and 20.67 ± 4.76 mm in the PDT group, showing a significant difference (P < 0.001). (D) Tracheal depth: The mean depth was 11.48 ± 0.57 mm in the OTEF group and 11.45 ± 0.73 mm in the PDT group, with no significant difference (P > 0.05).
4 Discussion
In resource-limited, understaffed, or emergency situations, a single-person tracheotomy represents a crucial option. Emergency tracheotomy performed by a single operator is a straightforward, rapid, and safe procedure to establish an airway in minimal time, potentially saving the patient’s life. Cadaveric experiments investigating single-person emergency tracheostomies provide essential insights into the feasibility, operational challenges, and limitations of this technique.
Olecranon-type tracheotomy and expansion forceps feature sharp anterior ends that efficiently penetrate the trachea with minimal tissue damage. Once the forceps’ tips are inserted vertically into the trachea, tilting the body of the forceps toward the patient’s head naturally directs the tips toward the feet. The device’s scale allows precise puncture depth determination, minimizing the risk of airway injury. The curved inner surface of the forceps includes a blade to cut through skin, muscle, and tracheal rings, while the outer blunt surface prevents damage to adjacent tissues during the procedure, emulating the incision process of a traditional tracheotomy scalpel. After the tracheotomy is completed, the jaw of the forceps guides accurate insertion of the tracheal tube into the trachea, facilitating the operation for healthcare providers.
The forceps tip is divided into two parts, front and back, which do not overlap like scissors. Only the front edge of the front part is sharp. The rear edge of the front part and the front edge of the back part form a smooth curved surface. The tracheotomy tube is inserted into the trachea between these two parts. Care must be taken during the operation to ensure the correct insertion position to minimize the risk of damaging the air cuff.
Traditional emergency tracheotomy methods, such as open surgical tracheotomy and cricothyrotomy, often require multiple operators, advanced training, and numerous instruments. These methods are time-consuming and associated with complications like incorrect incision placement, bleeding, and infection, particularly in suboptimal conditions. Cricothyrotomy is comparatively simpler for non-medical personnel to perform, as it involves fewer vital anatomical structures. Consequently, many military first-aid protocols prioritize cricothyrotomy as an emergency airway intervention on the battlefield. However, cricothyrotomy cannot provide a stable, long-term airway in patients with severe airway injuries, necessitating tracheotomy within 48 h to minimize postoperative complications and enhance recovery (Isabel Araújo et al., 2014; Trouillet et al., 2011; Yue et al., 2012; Rumbak et al., 2004). In contrast, the novel olecranon-type device simplifies the tracheotomy procedure through guided steps, reducing the technical and cognitive burden on operators. Cadaveric studies have shown that this device ensures consistent tracheotomy tube placement, minimizes variability, and enhances procedural safety. In this study, the incision length was 13.67 ± 3.67 mm, and the procedure was completed in 96.83 ± 8.82 s. According to literature, trained operators can perform emergency cricothyroidotomy on cadavers within 50 s (Schaumann et al., 2005). The findings suggest that olecranon-type tracheotomy and expansion forceps could replace emergency cricothyroidotomy in battlefield first aid. Following successful puncture, initial relief from suffocation was achieved.
Suffocation is common during emergencies, often due to trauma. Determining the puncture site can be challenging, particularly in cases involving unclear anatomical structures, such as in morbidly obese patients. Guinot et al. (2012). demonstrated that ultrasound-guided percutaneous dilation tracheotomy effectively resolves these issues by visualizing the trachea and tracheal rings, assisting operators in determining the puncture site and depth, and avoiding injury to blood vessels or the thyroid isthmus (Alan et al., 2015). The usefulness of ultrasonography in percutaneous dilational tracheotomy has been demonstrated in four open randomized studies. Among 275 patients who underwent preoperative ultrasonography, 40 (14.5%) experienced complications. In comparison, 285 patients who did not undergo ultrasonography had a higher complication rate, with 74 (26%) experiencing at least one complication. The use of ultrasonography significantly improved the success rate of first-attempt surgeries (Rudas et al., 2014; Yavuz et al., 2014; Ravi and Vijay, 2015; Gobatto et al., 2016). Additionally, some studies have reported that fiberoptic bronchoscopy can also reduce the occurrence of complications during tracheotomy (Saritas et al., 2016). However, fiberoptic bronchoscopy is challenging to operate, requires significant training, and is prone to damage, limiting its practicality in complex first-line emergency environments. In this study, portable ultrasound exploration was used to assist operators in accurately identifying the trachea before tracheotomy. The time from exploration initiation to operation completion was 96.83 ± 8.82 s. Portable ultrasound devices enhance operator accuracy and reduce complications such as pneumothorax, airway injury, and detubation. Furthermore, their portability and ease of use make them suitable for prehospital settings, remote locations, and emergency situations.
The integration of tracheal ultrasound image recognition and artificial intelligence enables the real-time annotation of anatomical structures like the trachea and thyroid in ultrasound images. This, to a certain degree, alleviates the difficulty of related training. Nevertheless, it is of utmost importance to closely monitor the systemic risks associated with artificial intelligence and guard against the emergence of blind trust.
The olecranon-type device is particularly useful in prehospital care, remote areas, and disaster scenarios where medical teams may be unavailable. It has potential applications in military medical kits and first-aid equipment for extreme environments, mass casualty events, and pandemics. By enabling single operators to perform tracheotomies efficiently, this device may improve survival rates and reduce complications associated with delayed airway management. The integration of portable ultrasound machines with this device further supports accurate tracheal localization and enhances procedural safety.
This study demonstrated the feasibility and safety of the olecranon-type tracheotomy and expansion forceps (OTEF) for single-operator tracheotomy under cadaveric conditions. However, several limitations should be acknowledged. First, the present study was conducted on cadaveric models, which cannot fully replicate the physiological conditions of living subjects, such as tissue elasticity, bleeding, and airway movement. Consequently, the potential risks of vascular or thyroid injury, as well as posterior tracheal wall damage, remain to be verified in future animal and clinical studies.
In addition, although no statistically significant difference in sex distribution was observed between the two groups (p = 0.413), potential anatomical variations related to sex—such as differences in neck circumference, tracheal diameter, and soft tissue thickness—may influence procedural performance. These factors could affect the ease of tracheal identification and puncture accuracy during the tracheotomy procedure. Future studies with larger and more balanced samples are warranted to further investigate the impact of sex-related anatomical differences on procedural outcomes.
Furthermore, operator-related factors such as learning curve, clinical background, and training duration were not analyzed in the present study. We plan to explore these parameters in future work to better define the learning requirements and skill acquisition process for single-operator tracheotomy. The learning curve for using this device must also be considered. While designed for simplicity, effective use requires proper training to ensure operators can confidently and safely perform the procedure under stress. Standardized training protocols, including simulation-based modules, are critical to the device’s widespread adoption.
In future studies, we plan to conduct a systematic investigation of the learning curve associated with single-operator tracheotomy. Although the present study primarily focused on the feasibility and procedural safety of the olecranon-type tracheotomy and expansion forceps (OTEF), the influence of operator experience and training duration on procedural performance remains to be fully elucidated. Understanding the learning curve is essential for defining the minimum training requirements, optimizing teaching strategies, and improving overall procedural safety and efficiency. To achieve this, future work will include quantitative assessment of performance indicators-such as operation time, success rate, and procedural accuracy-cross operators with varying levels of clinical experience. These data will help establish a standardized training protocol for the single-operator tracheotomy technique and provide valuable evidence for its wider clinical implementation.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Basic Medical Sciences Chinese Academy of Medical Sciences (No. 2022125). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
LZ: Writing – original draft, Writing – review and editing. FM: Data curation, Methodology, Writing – review and editing. NJ: Conceptualization, Data curation, Investigation, Methodology, Writing – review and editing. LX: Conceptualization, Data curation, Methodology, Project administration, Resources, Writing – original draft. YW: Data curation, Formal Analysis, Funding acquisition, Methodology, Writing – review and editing. HZ: Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research publication of this article.
Acknowledgements
Tissue provided by: National Human Brain Bank for Development and Function, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. This study was supported by the Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences, Neuroscience Center, and the China Human Brain Banking Consortium. The present study was approved by the Institutional Review Board of the Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences (Approval Number: 009-2014, 031–2017, 2022125).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alansari, M., Alotair, H., Al Aseri, Z., and Elhoseny, M. A. (2015). Use of ultrasound guidance to improve the safety of percutaneous dilatational tracheostomy: a literature review. Crit. Care 19, 229. doi:10.1186/s13054-015-0942-5
Byhahn, C., Wilke, H. J., Halbig, S., Lischke, V., and Westphal, K. (2000). Percutaneous tracheostomy: ciaglia blue rhino versus the basic ciaglia technique of percutaneous dilational tracheostomy. Anesth. Analg. 91, 882–886. doi:10.1097/00000539-200010000-00021
Chen, Y., Zhang, Q., and Zhang, H. (2015). A novel tracheostomy technique for emergency airway: a randomized controlled study in minipigs. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 50 (10), 842–847.
Chen, Y., Han, Y., August, M., Ferraro, N. F., Zhang, Q., and Zhang, H. (2018). Cricothyroid membrane puncture-guided tracheostomy: a new technique for emergency airway access. J. Oral Maxillofac. Surg. 76 (6), 1248–1254. doi:10.1016/j.joms.2017.12.028
Ciaglia, P., Firsching, R., and Syniec, C. (1985). Elective percutaneous dilatational tracheostomy. Chest 87, 715–719. doi:10.1378/chest.87.6.715
Fantoni, A., and Ripamonti, D. (1997). A non-derivative, non-surgical tracheostomy: the translaryngeal method. Int. Care Med. 23, 386–392. doi:10.1007/s001340050345
Gobatto, A. L. N., Besen, B. A. M. P., Tierno, PFGMM, Mendes, P. V., Cadamuro, F., Joelsons, D., et al. (2016). Ultrasound-guided percutaneous dilational tracheostomy versus bronchoscopy-guided percutaneous dilational tracheostomy in critically ill patients (TRACHUS): a randomized noninferiority controlled trial. Intensive Care Med. 42 (3), 342–351. doi:10.1007/s00134-016-4218-6
Graeme, A. B. (2016). Quick response tracheotomy: a novel surgical procedure. J. Intensive Care Med. 31 (4), 276–284. doi:10.1177/0885066615627141
Griggs, W. M., Worthley, L. G., Gilligan, J. E., Thomas, P. D., and Myburg, J. A. (1990). A simple percutaneous tracheostomy technique. Surg. Gynecol. Obstet. 170, 543–545.
Guinot, P. G., Zogheib, E., Petiot, S., Marienne, J. P., Guerin, A. M., Monet, P., et al. (2012). Ultrasound-guided percutaneous tracheostomy in critically ill obese patients. Crit. Care 16, 40. doi:10.1186/cc11233
Isabel Araújo, M. C., Sousa, V., Marques Pinto, L., and Barros, E. (2014). Impact of early elective tracheotomy in critically ill patients. Braz J. Otorhinolaryngol. 80 (5), 428–434. doi:10.1016/j.bjorl.2014.07.008
Karlsson, T., Brännström, A., Gellerfors, M., Gustavsson, J., and Günther, M. (2022). Comparison of emergency surgical cricothyroidotomy and percutaneous cricothyroidotomy by experienced airway providers in an obese, in vivo porcine hemorrhage airway model. Mil. Med. Res. 9 (1), 57. doi:10.1186/s40779-022-00418-8
Kovacs, G., and Sowers, N. (2018). Airway management in trauma. Emerg. Med. Clin. North Am. 36 (1), 61–84. doi:10.1016/j.emc.2017.08.006
Putensen, C., Theuerkauf, N., Guenther, U., Vargas, M., and Pelosi, P. (2014). Percutaneous and surgical tracheostomy in critically ill adult patients: a meta-analysis. Crit. Care Lond Engl. 18 (6), 544. doi:10.1186/s13054-014-0544-7
Ravi, P. R., and Vijay, M. N. (2015). Real time ultrasound-guided percutaneous tracheostomy: is it a better option than bronchoscopic guided percutaneous tracheostomy? Med. J. Armed Forces India 71 (2), 158–164. doi:10.1016/j.mjafi.2015.01.013
Rudas, M., Seppelt, I., Herkes, R., Hislop, R., Rajbhandari, D., and Weisbrodt, L. (2014). Traditional landmark versus ultrasound guided tracheal puncture during percutaneous dilatational tracheostomy in adult intensive care patients: a randomised controlled trial. Crit. Care 18 (5), 514. doi:10.1186/s13054-014-0514-0
Rumbak, M. J., Newton, M., Truncale, T., Schwartz, S. W., Adams, J. W., and Hazard, P. B. (2004). A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit. Care Med. 32 (8), 1689–1694. doi:10.1097/01.ccm.0000134835.05161.b6
Saritas, A., Saritas, P. U., Kurnaz, M. M., Beyaz, S. G., and Ergonenc, T. (2016). The role of fiberoptic bronchoscopy monitoring during percutaneous dilatational tracheostomy and its routine use into tracheotomy practice. JPMA J. Pak Med. Assoc. 66 (1), 83–89.
Schaumann, N., Lorenz, V., Schellongowski, P., Staudinger, T., Locker, G. J., Burgmann, H., et al. (2005). Evaluation of Seldinger technique emergency cricothyroidotomy versus standard surgical cricothyroidotomy in 200 cadavers. Anesthesiology 102 (1), 7–11. doi:10.1097/00000542-200501000-00005
Trouillet, J.-L., Luyt, C. E., Guiguet, M., Ouattara, A., Vaissier, E., Makri, R., et al. (2011). Early percutaneous tracheotomy Versus prolonged intubation of mechanically ventilated patients after cardiac surgery: a randomized trial. Ann. Intern Med. 154 (6), 373–383. doi:10.7326/0003-4819-154-6-201103150-00002
Yavuz, A., Yılmaz, M., Göya, C., and Alimoglu, E. (2014). Advantages of US in percutaneous dilatational tracheostomy: randomized controlled trial and review of the literature. Radiology 273 (3), 927–936. doi:10.1148/radiol.14140088
Keywords: tracheotomy, airway management, emergency treatment, surgical instruments, cadaver
Citation: Zhu L, Meng F, Jin N, Xing L, Wang Y and Zhang H (2025) A novel olecranon-type tracheotomy and expansion forceps for single-person emergency airway access. Front. Bioeng. Biotechnol. 13:1712809. doi: 10.3389/fbioe.2025.1712809
Received: 25 September 2025; Accepted: 06 November 2025;
Published: 19 November 2025.
Edited by:
Yi Sun, University Hospitals Leuven, BelgiumReviewed by:
Berivan Cecen, New Jersey Institute of Technology, United StatesFeng Li, KU Leuven, Belgium
Xiaozhen Lin, People’s Liberation Army General Hospital, China
Copyright © 2025 Zhu, Meng, Jin, Xing, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haizhong Zhang, emhhbmdoYWl6aG9uZ0AzMDFob3NwaXRhbC5jb20uY24=; Yi Wang, d2FuZ3lpMUAzMDFob3NwaXRhbC5jb20uY24=
†These authors have contributed equally to this work
 Liang Zhu1,2†
Liang Zhu1,2† Nenghao Jin
Nenghao Jin Haizhong Zhang
Haizhong Zhang