- Department of Cardiology, Peking Union Medical College Hospital, Peking Union Medical College & Chinese Academy of Medical Science, Beijing, China
In December 2019, Coronavirus Disease 2019 (COVID-19) caused by SARS-CoV-2, occurred in China and has currently led to a global pandemic. In addition to respiratory involvement, COVID-19 was also associated with significant multiple organ dysfunction syndrome (MODS). Cardiovascular impairment has been observed and is now drawing growing attention. Cardiovascular protective strategies are urgent and of great significance to the overall prognosis of COVID-19 patients. Direct viral infection, cytokine storm, and aggravation of existing cardiovascular diseases were recognized as possible mechanisms of cardiovascular impairment in COVID-19. Hyperactivated inflammation plays an important role in all three mechanisms and is considered to be fundamental in the development of cardiovascular impairment and MODS in COVID-19. Therefore, in addition to conventional cardiovascular treatment, anti-inflammatory therapy is a reasonable strategy for severe cases to further enhance cardiovascular protection and potentially mitigate MODS. We reviewed the inflammatory features and current promising treatments of COVID-19 as well as cardiovascular anti-inflammatory therapies that have been verified in previous clinical trials with positive outcomes. We believe that targeting the central pathway (IL-1β, TNF-α, IL-6), balancing the Th1 and Th2 response, and administering long-term anti-inflammatory therapy might be promising prospects to reduce cardiovascular impairment and even MODS during the acute and recovery phases of COVID-19. The cardiovascular anti-inflammatory therapies might be of great application value to the management of COVID-19 patients and we further propose an algorithm for the selection of anti-inflammatory therapy for COVID-19 patients with or at high risk of cardiovascular impairment. We recommend to take the experiences in cardiovascular anti-inflammatory therapy as references in the management of COVID-19 and conduct related clinical trials, while the clinical translation of novel treatments from preclinical studies or in vitro drug screening should proceed with caution due to unguaranteed efficacy and safety profiles.
Introduction
In December 2019, a series of pneumonia cases, now known as Coronavirus Disease 2019 (COVID-19), occurred in Wuhan, Hubei Province, China. A novel coronavirus was later identified as the cause of COVID-19 (1).
By February 11, 2020, a total of 72,314 cases had been reported in mainland China with 44,672 (61.8%) confirmed cases. A total of 1023 patients died, with a case fatality rate of 2.3%, and most of the deaths were in patients over 60 years of age. Among the confirmed cases, severe cases and critical cases accounted for 13.8 and 4.7%, respectively.
The Coronavirus Study Group of the International Committee on Taxonomy of Viruses assessed the novelty of the novel coronavirus and formally recognized it as a sister to severe acute respiratory syndrome coronaviruses (SARS-CoVs), designating it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) based on phylogeny, taxonomy and established practice (2).
However, unlike the SARS that occurred in 2003, SARS-CoV-2 infection not only leads to pneumonia and acute respiratory distress syndrome (ARDS) but is also associated with significant multiple organ dysfunction syndrome (MODS). The name of COVID-19 was chosen recently by the World Health Organization to cover the diverse clinical manifestations and reflect the complexity of the disease. Common complications among COVID-19 patients include shock, ARDS, arrhythmia, and acute cardiac injury (1). Especially for patients who require ICU care, significant cardiovascular impairment has already been observed, characterized by elevation of cardiac biomarkers, abnormalities in electrocardiography and echocardiography, and eventual circulatory failure. Cardiovascular impairment is now drawing growing attention in clinical practice, and the American College of Cardiology has already released a clinical bulletin on Feb 13, 2020, to address the cardiac implications of COVID-19 (3).
Inflammation plays an important role in the development of cardiovascular impairment and even MODS. As a cardiologist and a member of the high-level expert group appointed by the National Health Commission to fight COVID-19, during the clinical practice, I found that the experiences in cardiovascular anti-inflammatory therapy might be instructive in the management of COVID-19, especially those severe cases. Therefore, in this article, we would like to summarize the related available information and share our perspectives.
Mechanism of Cardiovascular Impairment in COVID-19
The main reasons for cardiovascular impairment in COVID-19 patients can be summarized as follows.
Direct Infection
The virus might directly infect the myocardial tissue and lead to cardiac injury. Cardiac injury has been noted as a protruding clinical feature in COVID-19 patients. In a study of 138 patients, 10 patients were diagnosed with cardiac injury and 8 of them required ICU care, accounting for 22% of all the severe cases. Compared with the non-ICU patients, ICU patients had higher level of hypersensitive troponin I and creatine kinase–MB, indicating that cardiac injury is associated with the disease severity (1). SARS-CoV-2 and SARS-CoV share the same functional host-cell receptor, angiotensin-converting enzyme 2 (ACE2) for cell entry (4), but the affinity of ACE2 for SARS-CoV-2 is approximately 10- to 20-fold higher than that for SARS-CoV (5). ACE2 is highly expressed in both the lung and heart (6), and the SARS-CoV viral RNA has been detected in autopsied heart samples from SARS patients (7). However, large-scale autopsy or biopsy studies are still required to further confirm the myocardial infection in COVID-19 by the tissue viral RNA detection or in situ hybridization at heart and endothelium. In addition, it is worth noticing that both blockades of AT1 receptors and inhibition of Ang II synthesis would increase the expression of cardiac ACE2 (8); therefore, for patients with hypertension or congestive heart failure (HF), regular treatment with ACE inhibitors or angiotensin receptor blockers (ARB) could further increase the risk of coronavirus infection (Figure 1). However, the causal relationship between ACEI/ARB intake and increased viral load and deleterious outcomes in COVID-19 is still uncertain. Animal studies even showed a protective effect of ARB in lung injury during SARS-CoV infection (9, 10). Considering the solid evidence of the beneficial effect of ACEI/ARB in cardiovascular diseases, it is currently not recommended to discontinue the RASS inhibition treatment in COVID-19 (11).
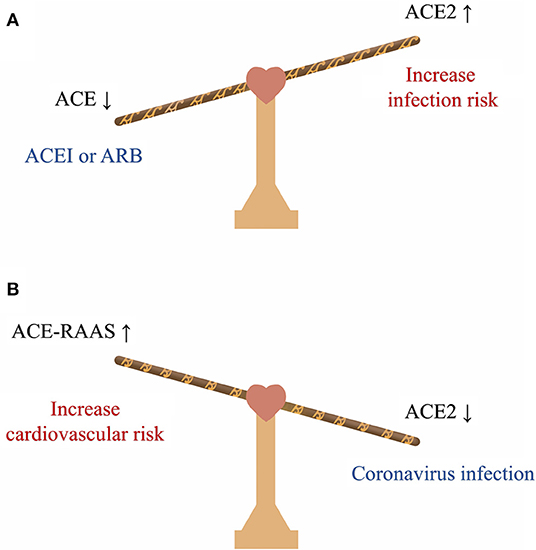
Figure 1. The balance between ACE and ACE2 in COVID-19. (A) Treatment with ACEI or ARB increases the expression of cardiac ACE2 and could further increase the risk of coronavirus infection. (B) Coronavirus infection can downregulate ACE2, further activate the RAAS system and increase the cardiovascular burden. ACE, angiotensin-converting enzyme; ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; RAAS, renin-angiotensin-aldosterone system.
Cytokine Storm
Similar to SARS-CoV and MERS-CoV infection, SARS-CoV-2 infection can also induce excessive and aberrant host immune responses, leading to a cytokine storm (12). Studies have shown increased amounts of cytokines, such as IL-1β, IL-1ra, IL-6, TNF-α, IL-7, IL-8, IL-9, IL-10, FGF basic, G-CSF, GM-CSF, IFN-γ, IP-10, MCP-1, MIP-1a, MIP-1b, in the serum of COVID-19 patients, and the cytokine storm was associated with disease severity (1, 13). An autopsy study of a COVID-19 patient also revealed that there were a few interstitial mononuclear inflammatory infiltrates in the heart tissue; besides, the flow cytometric analysis of peripheral blood found that CD4 and CD8 T cells were hyperactivated and the concentration of highly proinflammatory Th17 cells significantly increased (14). Cytokines play an important role in the immune response to defend against viral infections; however, it has also been recognized that dysregulated and excessive immune responses may cause immunopathology. Inflammation after infection can be progressively amplified through positive feedback and eventually form a cytokine storm, leading to systematic self-attack, which is a well-established explanation for MODS during coronavirus infection (15, 16).
Aggravation of Existing Cardiovascular Diseases
SARS-CoV-2 infection is more likely to affect older patients with underlying cardiovascular comorbidities (17). According to a study, 4.2% of the confirmed cases and 22.7% of deaths have cardiovascular comorbidities (18). The fatality rate of patients with comorbidities was much higher than that of patients without comorbidities, and the fatality rate of patients with cardiovascular diseases (10.5%) was the highest (18). Therefore, COVID-19 patients are at risk of acute cardiovascular events. Secondary infection, disorder of sodium and water homeostasis, hypoxia, tissue hypoperfusion, and shock occurring during COVID-19 can all result in the aggravation of existing cardiovascular diseases and trigger severe events, such as acute coronary syndromes or exacerbation of HF. Additionally, a study has demonstrated that SARS-CoV infection can lead to the downregulation of ACE2 and activate the renin-angiotensin-aldosterone system (RASS), which would further increase the cardiovascular burden and contribute to adverse outcomes (7) (Figure 1).
In addition to the three mechanisms, the treatment with non-steroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, and anti-viral agents, such as lopinavir/ritonavir (LVP/r), interferon-α (IFN-α), ribavirin, and azithromycin, could further increase the cardiovascular risk of COVID-19 patients and bring additional challenges. The harmful effects of NSAIDs and glucocorticoids on the cardiovascular system have been well-demonstrated by numerous studies that they can increase the risk of all cardiovascular events, myocardial infarction (MI), HF, and cerebral infarction (19, 20). LPV/r can induce cardiac conduction alteration and QTc and/or PR interval prolongation, further leading to atrioventricular block and torsade de pointes. LPV/r may also increase the risk of MI (21). Besides, protease inhibitor therapy has been associated with hyperglycemia, hyperlipidemia, and lipodystrophy (22) and such metabolic disturbances were also verified in patients treated with LPV/r (23). IFN-α is associated with hypertension, hypertriglyceridemia, and various cardiovascular adverse reactions and has been given a US boxed warning for its potential risk of ischemic disorders (24). A statement from the American Heart Association has announced that IFN-α can cause numerous direct cardiotoxicities, including arrhythmias, MI, and cardiomyopathy, and can also exacerbate underlying myocardial dysfunction (25). A US boxed warning has been issued for ribavirin that the hemolytic anemia associated with ribavirin may worsen underlying cardiac disease and lead to fatal and non-fatal MI (26). A recent study has shown that azithromycin could reinforce the anti-viral effect of hydroxychloroquine (27); however, its proven risk of severe QT prolongation should also be considered (28), especially when it is combined with hydroxychloroquine to treat the elderly COVID-19 patients (29).
Rationale for Cardiovascular Anti-Inflammatory Therapy in COVID-19
Cardiovascular protective strategies are urgent for the prevention and management of severe adverse cardiovascular events, which is of great significance to the overall prognosis of COVID-19 patients. The clinical bulletin released by the American College of Cardiology has issued several points of clinical guidance regarding cardiac complications (3), and the Chinese Society of Cardiology of Chinese Medical Association also developed an expert consensus on the clinical management of patients with emergent high-risk cardiovascular disease during the epidemic period (30). However, whether the conventional treatment is sufficient to overcome such challenges and whether any additional strategy to further reduce the risk of cardiovascular attack is needed in severe cases of COVID-19 remain unclear.
Excessive inflammation should be considered as a promising target because it plays an important role in all three mechanisms described above. It has already been demonstrated that for myocarditis with or without viral trigger, inflammation is implicated in the development of both acute cardiac injury and subsequent dilated cardiomyopathy (31). There is also abundant evidence that inflammation participates in various cardiovascular diseases, such as coronary artery disease (CAD) and HF. Especially in atherosclerosis, inflammation promotes the formation, destabilization, and rupture of atheromatous plaques and has already been recognized as an independent risk factor and prognostic predictor (32).
Therefore, conventional cardiovascular treatment plus anti-inflammatory therapy is a reasonable enhanced strategy for better management of cardiovascular impairment in severe cases of COVID-19. In addition, as the inflammatory attack on different organs shares numerous similar mechanisms and pathways, such as the inflammatory response under ischemia/reperfusion injury (IRI) of the heart, liver, and kidney (33), suppression of the systematic inflammatory response will not only exert cardiovascular protection effect but also have potential benefits for MODS. Rheumatologists have also focused on the dysregulated inflammation and suggested that there might be a “window of opportunity” for immunosuppressive strategies used to treat rheumatic diseases to serve as strong allies in the fight against COVID-19 (34, 35).
Verified Cardiovascular Anti-Inflammatory Therapies
Many clinical trials have been conducted in the past decade to directly test the feasibility of using different anti-inflammatory agents for cardiovascular protection under various conditions, mainly including CAD, myocardial IRI, HF, myocarditis/dilated cardiomyopathy, and rheumatic diseases [rheumatoid arthritis (RA), psoriatic arthritis, etc.]. Accumulating evidence has supported the efficacy of this novel strategy in improving cardiovascular outcomes. Here, we reviewed the currently available cardiovascular anti-inflammatory therapies that have been verified in clinical trials with positive results (36–47). The detailed information of these trials is listed in Table 1.
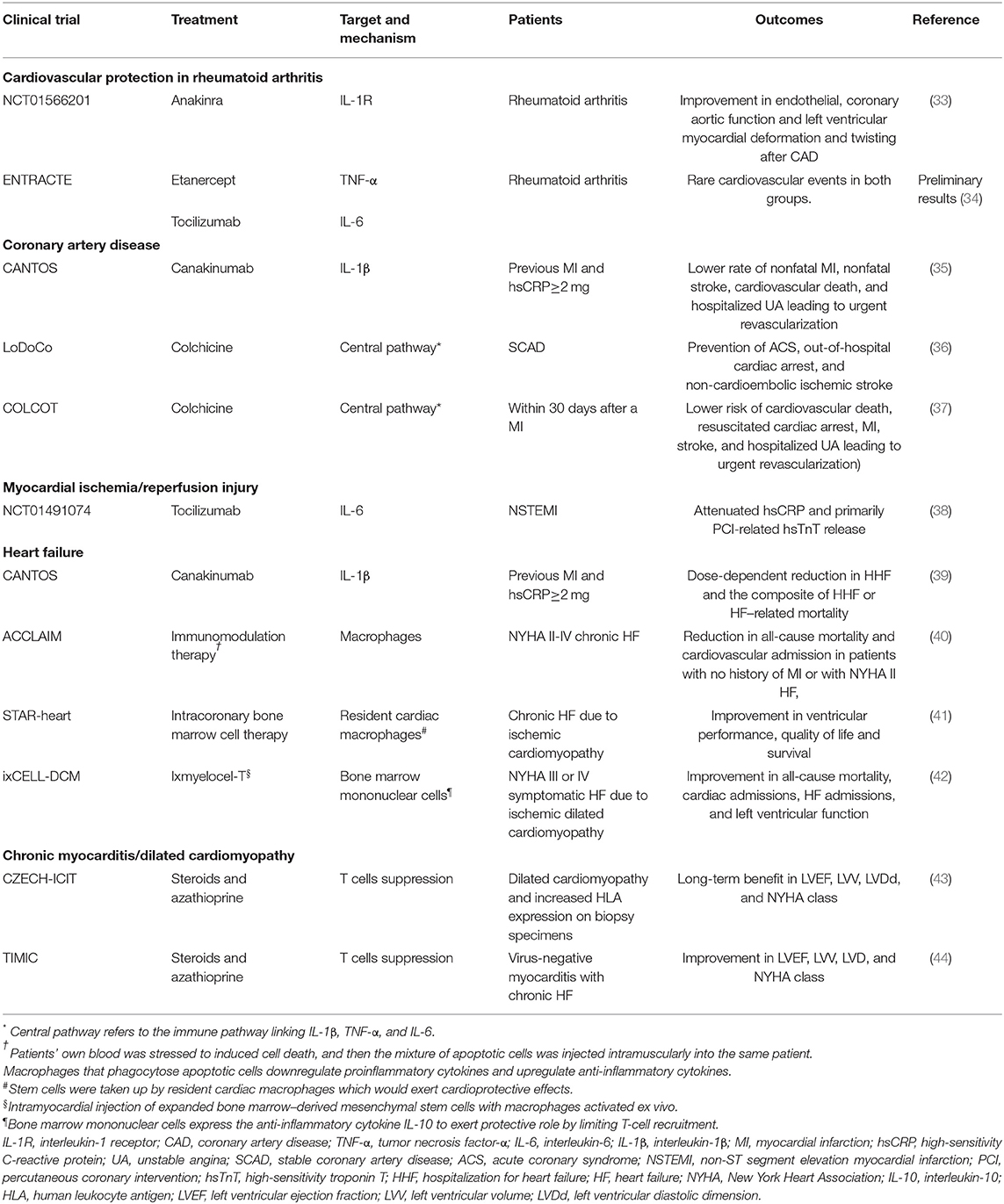
Table 1. Clinical trials of anti-inflammatory therapy for cardiovascular protection with positive outcomes.
Promising Prospects
Based on the above review and summarization, there are several perspectives that we can conclude to possibly guide the selection of anti-inflammatory therapies in COVID-19.
Targeting the Central Pathway (IL-1β, TNF-α, IL-6)
The immune pathway linking IL-1β, TNF-α, and IL-6, known as the central pathway, has long been implicated in atherosclerosis and is considered to play an important role in CAD (48). The significant effect of such a central pathway has also been recognized in many other fields of cardiovascular research (49–52), and a large portion of the clinical trials reviewed above was designed to target this pathway. Activation of the central pathway has already been observed in COVID-19 and should, therefore, be considered as a promising target (13). A multicenter, randomized controlled trial (ChiCTR2000029765) has been registered to evaluate the efficacy and safety of IL-6 blockade using tocilizumab in COVID-19. According to the preliminary treatment results currently released, among the 14 patients recruited (maximum age 82), including 9 severe cases and 2 critical cases, tocilizumab significantly improved the fever symptom and lung function and also accelerated the absorption of lung lesions. In addition to the benefits reviewed above, it is worth mentioning that tocilizumab also has a potential electrophysiological protective effect. Increased IL-6 level has been associated with acquired long QT-syndrome in patients with systemic inflammation, leading to higher risks for arrhythmias such as torsade de pointes (53). In RA patients, tocilizumab treatment led to a rapid and significant QT shortening correlating with the decrease in CRP and cytokine levels, which might benefit the overall mortality (54, 55). Such anti-arrhythmic potential may further support the application of tocilizumab in COVID-19 patients to counteract the risk of adverse QT prolongation and related life-threatening arrhythmias associated with elevated IL-6 and the anti-viral agents. A series of clinical trials on chloroquine in the treatment of COVID-19 are also currently underway and have revealed considerable benefits (27). Chloroquine has now been included in the 6th version of the Diagnosis and Treatment Plan for Novel Coronavirus Pneumonia (56). In addition to its direct antiviral effect (57), chloroquine might also exert anti-inflammatory effects by inhibiting the central pathway (58). Hydroxychloroquine (HCQ) has long been used to reduce inflammation in patients with RA and lupus. In a nationwide cohort study, HCQ use was associated with decreased CAD risk in the RA population (59). Besides, an OXI trial (NCT02648464) is currently underway to study the effect of HCQ on the prevention of recurrent cardiovascular events among MI patients (60). Therefore, we recommend targeting the central pathway by blockade of IL-6 (tocilizumab), IL-1β [canakinumab (IL-1β monoclonal antibody), anakinra (IL-1 receptor antagonist)], and TNF-α (etanercept, infliximab) to control the cytokine storm in the acute phase of COVID-19, thereby reducing cardiovascular impairment and even mitigating MODS.
Balancing the T-helper-1 (Th1) Cell and T-helper-2 (Th2) Cell Response and Promoting the Secretion of Anti-Inflammatory Cytokines
Studies of IRI and myocarditis have revealed that the Th1 response, characterized by the expression of multiple proinflammatory cytokines, is activated in the early disease phase and is associated with acute cardiac injury (61–63), while the Th2 response dominates later, promoting the resolution of acute inflammation and tissue repair. M2 macrophage polarization was found to be a significant change contributing to the transition from the Th1 to Th2 response, and monocyte-derived IL-10 is a well-recognized Th2-related anti-inflammatory cytokine that is highly expressed in the reparative phase and inhibits the Th1 response (64, 65). Early activation of the Th2 response or increased IL-10 expression in IRI and myocarditis could significantly inhibit the secretion of Th1-related proinflammatory cytokines and reduce myocardial necrosis (66–69). Patients with COVID-19 had high amounts of IL-1β, IFN-γ, IP-10, and MCP-1, indicating an activated Th1 response; besides, SARS-CoV-2 could also initiate increased secretion of Th2 cytokines, especially IL-10, which is different from SARS-CoV infection (70). Therefore, the implantation of mesenchymal stromal cells (MSCs) from allogeneic donors with an activated Th2 response or ex vivo bone marrow-derived MSCs after M2 macrophage polarization might increase the level of IL-10 in the acute phase of COVID-19 and serve as a possible solution to inflammation-mediated damage. In addition to the application in cardiovascular diseases reviewed above, cellular therapy using MSCs has also shown efficacy in the management of ARDS and is now being evaluated in phase 1/2 trials (12).
Long-Term Anti-Inflammatory Therapy in the Recovery Phase
Inflammation in the acute phase can lead to extensive injury; however, it should also be noted that after the acute damage, chronic residual inflammation that occurs with fibrosis during the reparatory phase can also result in persistent organ dysfunction. Studies of HF due to ischemic cardiomyopathy and chronic myocarditis have found that chronic residual inflammation is associated with myocardial fibrosis and adverse ventricular remodeling (49, 71–73). In addition, the long-term inflammatory status is also a hazard to atherosclerosis (32). During the follow-up of SARS and MERS patients, it was also observed that in those who survive intensive care, residual immune responses could lead to long-term lung damage and fibrosis, causing functional disability and reduced quality of life (74, 75). Therefore, in addition to the control of acute injury, it is also of great significance to conduct long-term follow-up after admission to monitor residual inflammation in COVID-19 patients, especially those with severe clinical manifestations or intense acute inflammatory responses. After excluding potential contraindications, long-term anti-inflammatory therapy, such as steroids, azathioprine, and canakinumab, should be considered to reduce the residual inflammation and prevent further chronic structural and functional damage.
Discussion
Hyperactivated inflammation is fundamental in the development of cardiovascular impairment and even MODS in COVID-19. In addition to conventional cardiovascular treatment, anti-inflammatory therapy is a reasonable strategy to further enhance cardiovascular protection and potentially mitigate MODS. By reviewing the inflammatory features and current promising treatments of COVID-19 as well as cardiovascular anti-inflammatory therapies that have been verified in clinical trials with positive results, we believed that targeting the central pathway (IL-1β, TNF-α, IL-6), balancing the Th1 and Th2 response, and administering long-term anti-inflammatory therapy should be considered as promising strategies to control cardiovascular impairment or even MODS during the acute and recovery phases of COVID-19. The experiences in cardiovascular anti-inflammatory therapies might be of great value to the management of COVID-19 patients and we recommended to take such experiences as references for clinical practice and conduct related clinical trials. We here propose a possible algorithm regarding the selection of anti-inflammatory therapy for COVID-19 patients with or at high risk of cardiovascular impairment (Figure 2).
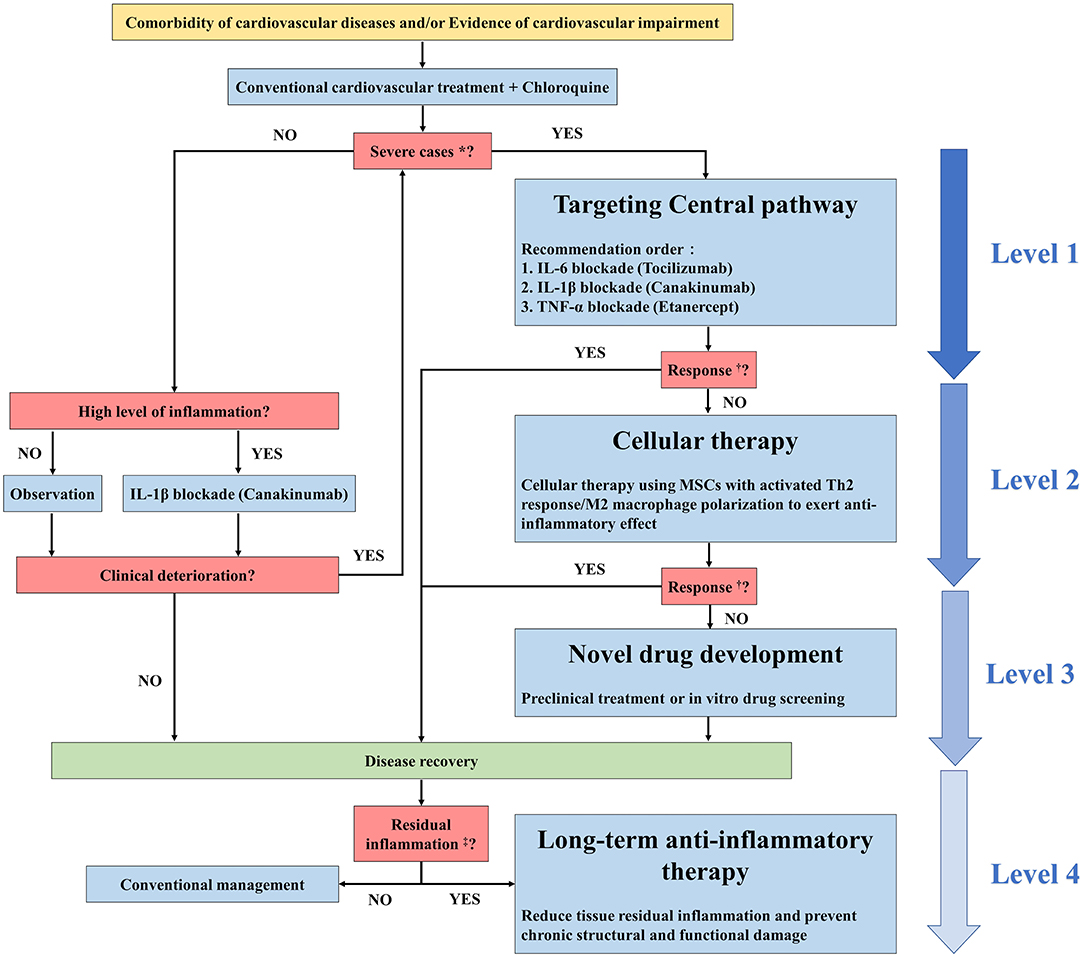
Figure 2. Possible algorithm regarding the selection of anti-inflammatory therapy for COVID-19 patients with cardiovascular impairment. *Severe cases refer to patients with the following conditions according to the 6th version of the Diagnosis and Treatment Plan for Novel Coronavirus Pneumonia: respiratory rate≥30 bpm; SpO2 ≤ 30% at rest; PaO2/FiO2 ≤ 300 mmHg; progression on chest images>50% within 24 to 48 h; respiratory failure that requires mechanical ventilation; shock; organ dysfunction that requires ICU admission. †Response refers to the response to anti-inflammatory therapy. The criteria include but are not limited to decreased white blood cell counts, decreased hsCRP levels, decreased cytokine levels, significant symptom improvement, and significant improvement in chest images. Residual inflammation refers to evidence of a persistent state of high inflammation characterized by high levels of hsCRP and/or serum cytokines.
Despite all the beneficial effects described above, it is also important to pay attention to the potential adverse cardiovascular effects of these drugs. For tocilizumab, hypercholesterolemia and hypertension are both common adverse events, prompting concern about increased cardiovascular risk (76). Especially, tocilizumab was widely noted to induce a proatherogenic lipid profile with increased serum levels of low-density lipoprotein cholesterol and total cholesterol (77–79). However, these changes can be improved by concomitant therapy with statins (80). For TNF inhibitor (TNFi), although not universally acknowledged, it might not be beneficial to HF. Severe HF remains a contraindication to TNFi treatment in RA patients. A clinical trial showed that high-dose infliximab could be harmful to patients with moderate-to-severe HF (81). For RA populations, a cohort study found that TNFi might increase the risk of both first hospitalization and exacerbation of HF in elderly patients with RA (82). Additionally, for hydroxychloroquine, a recent study pointed out that hydroxychloroquine could lead to unwanted QT interval prolongation by blocking the KCNH2-encoded hERG/Kv11.1 potassium channel, thereby increasing the risk of drug-induced torsade de pointes and sudden cardiac death (83). Therefore, biochemical indicators, hemodynamic parameters, and cardiac electrophysiology profiles should be monitored in clinical practice to avoid drug-induced adverse effects on cardiovascular risk factors, cardiac function, or lethal arrhythmias. Besides, corresponding treatment, such as lipid-lowering or antihypertensive medications should be prescribed if necessary.
Currently, a large number of novel therapies from preclinical studies or in vitro drug screening have been registered and accelerated into clinical practice. However, the safety profiles of these therapies have always not been well-characterized, especially for elderly COVID-19 patients with hepatic or renal dysfunction. In addition, as many of the therapies were proven to be effective only by in vitro experiments or poorly designed small-scale clinical studies, the exact benefits were also not guaranteed. Therefore, clinical translation of novel treatments from preclinical studies or in vitro drug screening should proceed with caution due to unguaranteed efficacy and safety profiles. Recently, experts from multiple research institutions in China raised their criticism and announced an urgent call for increasing the scientific rigorousness of clinical trials on COVID-19 (84). Considering timeliness and safety, we suggest prioritizing cardiovascular protective strategies that have been proven by large-scale clinical trials for proof-of-concept studies and clinical application on COVID-19 instead of rushing into new drug research and development.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Author Contributions
LW contributes to the literature search, manuscript preparation, and manuscript editing. YZ contributes to concept, design, manuscript preparation, and manuscript editing. SZ contributes to concept, design, definition of intellectual content, and manuscript review.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank all the members of the high-level expert group appointed by the National Health Commission to fight COVID-19. We also thank the Wuhan assistance medical team of Peking Union Medical College Hospital and the medical team appointed to be in charge of the ICU of Huazhong University of Sciences & Technology, Tongji Hospital, Sino-French new city branch.
References
1. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china. Jama. (2020) 7:e201585. doi: 10.1001/jama.2020.1585
2. Gorbalenya AE, Baker SC, Baric RS, Groot RJd, Drosten C, Gulyaeva AA, et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses – a statement of the coronavirus study group. bioRxiv [Preprint]. (2020). doi: 10.1101/2020.02.07.937862
3. Mohammad Madjid SDS, Vardeny O, Mullen B. Acc Clinical Bulletin: Cardiac Implications of Novel Wuhan Coronavirus (2019-ncov). American College of Cardilogy (2020).
4. Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in china. Nature. (2020) 579:265–9. doi: 10.1038/s41586-020-2008-3
5. Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-em structure of the 2019-ncov spike in the prefusion conformation. Science. (2020) 367:1260–3. doi: 10.1101/2020.02.11.944462
6. Patel VB, Zhong JC, Grant MB, Oudit GY. Role of the ace2/angiotensin 1-7 axis of the renin-angiotensin system in heart failure. Circ Res. (2016) 118:1313–26. doi: 10.1161/CIRCRESAHA.116.307708
7. Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, et al. Sars-coronavirus modulation of myocardial ace2 expression and inflammation in patients with sars. Eur J Clin Invest. (2009) 39:618–25. doi: 10.1111/j.1365-2362.2009.02153.x
8. Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin ii receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. (2005) 111:2605–10. doi: 10.1161/CIRCULATIONAHA.104.510461
9. Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. (2005) 436(7047):112-6. doi: 10.1038/nature03712
10. Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. A crucial role of angiotensin converting enzyme 2 (ace2) in sars coronavirus-induced lung injury. Nat Med. (2005) 11:875–9. doi: 10.1038/nm1267
11. Kuster GM, Pfister O, Burkard T, Zhou Q, Twerenbold R, Haaf P, et al. Sars-cov2: Should inhibitors of the renin-angiotensin system be withdrawn in patients with covid-19? Eur Heart J. (2020) 20:ehaa235. doi: 10.1093/eurheartj/ehaa235
12. Zumla A, Hui DS, Azhar EI, Memish ZA, Maeurer M. Reducing mortality from 2019-ncov: host-directed therapies should be an option. Lancet. (2020) 395:e35–6. doi: 10.1016/S0140-6736(20)30305-6
13. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in wuhan, china. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
14. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of covid-19 associated with acute respiratory distress syndrome. Lancet Respir Med. (2020) 8:420–2. doi: 10.1016/S2213-2600(20)30076-X
15. Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. (2012) 76:16–32. doi: 10.1128/MMBR.05015-11
16. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. (2017) 39:529–39. doi: 10.1007/s00281-017-0629-x
17. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in wuhan, china: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
18. Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. [the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (covid-19) in china]. Zhonghua Liu Xing Bing Xue Za Zhi. (2020) 41:145–51. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003
19. England BR, Thiele GM, Anderson DR, Mikuls TR. Increased cardiovascular risk in rheumatoid arthritis: mechanisms and implications. BMJ. (2018) 361:k1036. doi: 10.1136/bmj.k1036
20. Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, et al. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis. (2015) 74:480–9. doi: 10.1136/annrheumdis-2014-206624
21. Lopinavir, and ritonavir: Drug Information,. Available online at: https://wwwuptodatecom/contents/lopinavir-and-ritonavir-drug-information
22. Tsiodras S, Mantzoros C, Hammer S, Samore M. Effects of protease inhibitors on hyperglycemia, hyperlipidemia, and lipodystrophy: a 5-year cohort study. Arch Intern Med. (2000) 160:2050–6. doi: 10.1001/archinte.160.13.2050
23. Hill A, Sawyer W, Gazzard B. Effects of first-line use of nucleoside analogues, efavirenz, and ritonavir-boosted protease inhibitors on lipid levels. HIV Clin Trials. (2009) 10:1–12. doi: 10.1310/hct1001-1
24. Interferon, alfa-2b: Drug Information,. Available online at: https://wwwuptodatecom/contents/interferon-alfa-2b-drug-information
25. Page RL 2nd, O'Bryant CL, Cheng D, Dow TJ, Ky B, Stein CM, et al. Drugs that may cause or exacerbate heart failure: a scientific statement from the american heart association. Circulation. (2016) 134:e32–69. doi: 10.1161/CIR.0000000000000426
26. Ribavirin (systemic): Drug Information. Available online at: https://wwwuptodatecom/contents/ribavirin-systemic-drug-information?source=see_link
27. Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of covid-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. (2020) 105949. doi: 10.1016/j.ijantimicag.2020.105949
28. Gibson PG, Yang IA, Upham JW, Reynolds PN, Hodge S, James AL, et al. Effect of azithromycin on asthma exacerbations and quality of life in adults with persistent uncontrolled asthma (amazes): a randomised, double-blind, placebo-controlled trial. Lancet. (2017) 390:659–68. doi: 10.1016/S0140-6736(17)31281-3
29. Choi Y, Lim HS, Chung D, Choi JG, Yoon D. Risk evaluation of azithromycin-induced qt prolongation in real-world practice. Biomed Res Int. (2018) 2018:1574806. doi: 10.1155/2018/1574806
30. Chinese Society of Cardiology of Chinese Medical A. Expert consensus on clinical management of patients with emergent high-risk cardiovascular disease during the epidemic period of novel coronavirus pneumonia. Chinese J Cardiol. (2020) 48:E001. doi: 10.3760/cma.j.issn.0253-3758.2020.0001
32. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. (2002) 105:1135–43. doi: 10.1161/hc0902.104353
33. Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Ischemia/reperfusion. Compr Physiol. (2016) 7:113–70. doi: 10.1002/cphy.c160006
34. Ferro F, Elefante E, Baldini C, Bartoloni E, Puxeddu I, Talarico R, et al. Covid-19: the new challenge for rheumatologists. Clin Exp Rheumatol. (2020) 38:175–80.
35. Sarzi-Puttini P, Giorgi V, Sirotti S, Marotto D, Ardizzone S, Rizzardini G, et al. Covid-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. (2020) 38:337–42.
36. Ikonomidis I, Tzortzis S, Andreadou I, Paraskevaidis I, Katseli C, Katsimbri P, et al. Increased benefit of interleukin-1 inhibition on vascular function, myocardial deformation, and twisting in patients with coronary artery disease and coexisting rheumatoid arthritis. Circ Cardiovasc Imaging. (2014) 7:619–28. doi: 10.1161/CIRCIMAGING.113.001193
37. ClinicalTrials.gov. A Study of Tocilizumab in Comparison to Etanercept in Participants With Rheumatoid Arthritis and Cardiovascular Disease Risk Factors. Available online at: https://clinicaltrials.gov/ct2/show/results/nct01331837 (accessed July 13, 2017).
38. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. (2017) 377:1119–31. doi: 10.1056/NEJMoa1707914
39. Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. (2013) 61:404–10. doi: 10.1016/j.jacc.2012.10.027
40. Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. (2019) 381:2497–505. doi: 10.1056/NEJMoa1912388
41. Kleveland O, Kunszt G, Bratlie M, Ueland T, Broch K, Holte E, et al. Effect of a single dose of the interleukin-6 receptor antagonist tocilizumab on inflammation and troponin t release in patients with non-st-elevation myocardial infarction: a double-blind, randomized, placebo-controlled phase 2 trial. Eur Heart J. (2016) 37:2406–13. doi: 10.1093/eurheartj/ehw171
42. Everett BM, Cornel JH, Lainscak M, Anker SD, Abbate A, Thuren T, et al. Anti-inflammatory therapy with canakinumab for the prevention of hospitalization for heart failure. Circulation. (2019) 139:1289–99. doi: 10.1161/CIRCULATIONAHA.118.038010
43. Torre-Amione G, Anker SD, Bourge RC, Colucci WS, Greenberg BH, Hildebrandt P, et al. Results of a non-specific immunomodulation therapy in chronic heart failure (acclaim trial): a placebo-controlled randomised trial. Lancet. (2008) 371:228–36. doi: 10.1016/S0140-6736(08)60134-8
44. Strauer BE, Yousef M, Schannwell CM. The acute and long-term effects of intracoronary stem cell transplantation in 191 patients with chronic heart failure: the star-heart study. Eur J Heart Fail. (2010) 12:721–9. doi: 10.1093/eurjhf/hfq095
45. Patel AN, Henry TD, Quyyumi AA, Schaer GL, Anderson RD, Toma C, et al. Ixmyelocel-t for patients with ischaemic heart failure: A prospective randomised double-blind trial. Lancet. (2016) 387:2412–21. doi: 10.1016/S0140-6736(16)30137-4
46. Wojnicz R, Nowalany-Kozielska E, Wojciechowska C, Glanowska G, Wilczewski P, Niklewski T, et al. Randomized, placebo-controlled study for immunosuppressive treatment of inflammatory dilated cardiomyopathy: two-year follow-up results. Circulation. (2001) 104:39–45. doi: 10.1161/01.CIR.104.1.39
47. Frustaci A, Russo MA, Chimenti C. Randomized study on the efficacy of immunosuppressive therapy in patients with virus-negative inflammatory cardiomyopathy: the timic study. Eur Heart J. (2009) 30:1995–2002. doi: 10.1093/eurheartj/ehp249
48. Ridker PM, Luscher TF. Anti-inflammatory therapies for cardiovascular disease. Eur Heart J. (2014) 35:1782–91. doi: 10.1093/eurheartj/ehu203
49. Dick SA, Epelman S. Chronic heart failure and inflammation: What do we really know? Circ Res. (2016) 119:159–76. doi: 10.1161/CIRCRESAHA.116.308030
50. Westman PC, Lipinski MJ, Luger D, Waksman R, Bonow RO, Wu E, et al. Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol. (2016) 67:2050–60. doi: 10.1016/j.jacc.2016.01.073
51. Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol. (2014) 11:255–65. doi: 10.1038/nrcardio.2014.28
52. Matsumori A. Cytokines in myocarditis and cardiomyopathies. Curr Opin Cardiol. (1996) 11:302–9. doi: 10.1097/00001573-199605000-00011
53. Aromolaran AS, Srivastava U, Ali A, Chahine M, Lazaro D, El-Sherif N, et al. Interleukin-6 inhibition of herg underlies risk for acquired long qt in cardiac and systemic inflammation. PLoS ONE. (2018) 13:e0208321. doi: 10.1371/journal.pone.0208321
54. Lazzerini PE, Acampa M, Capecchi PL, Fineschi I, Selvi E, Moscadelli V, et al. Antiarrhythmic potential of anticytokine therapy in rheumatoid arthritis: Tocilizumab reduces corrected qt interval by controlling systemic inflammation. Arthritis Care Res (Hoboken). (2015) 67:332–9. doi: 10.1002/acr.22455
55. Kobayashi H, Kobayashi Y, Yokoe I, Kitamura N, Nishiwaki A, Takei M, et al. Heart rate-corrected qt interval duration in rheumatoid arthritis and its reduction with treatment with the interleukin 6 inhibitor tocilizumab. J Rheumatol. (2018) 45:1620–7. doi: 10.3899/jrheum.180065
56. National health commission of the people's republic of china. The Diagnosis and Treatment Plan for Novel Coronavirus Pneumonia (6th version). Available online at: http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.Shtml (accessed February, 19, 2020).
57. Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-ncov) in vitro. Cell Res. (2020) 30:269–71. doi: 10.1038/s41422-020-0282-0
58. Monzavi SM, Alirezaei A, Shariati-Sarabi Z, Tavakol Afshari J, Mahmoudi M, Dormanesh B, et al. Efficacy analysis of hydroxychloroquine therapy in systemic lupus erythematosus: a study on disease activity and immunological biomarkers. Inflammopharmacology. (2018) 26:1175–82. doi: 10.1007/s10787-018-0512-y
59. Hung YM, Wang YH, Lin L, Wang PYP, Chiou JY, Wei JC. Hydroxychloroquine may be associated with reduced risk of coronary artery diseases in patients with rheumatoid arthritis: a nationwide population-based cohort study. Int J Clin Pract. (2018) 72:e13095. doi: 10.1111/ijcp.13095
60. Hartman O, Kovanen PT, Lehtonen J, Eklund KK, Sinisalo J. Hydroxychloroquine for the prevention of recurrent cardiovascular events in myocardial infarction patients: Rationale and design of the oxi trial. Eur Heart J Cardiovasc Pharmacother. (2017) 3:92–7. doi: 10.1093/ehjcvp/pvw035
61. Yan X, Anzai A, Katsumata Y, Matsuhashi T, Ito K, Endo J, et al. Temporal dynamics of cardiac immune cell accumulation following acute myocardial infarction. J Mol Cell Cardiol. (2013) 62:24–35. doi: 10.1016/j.yjmcc.2013.04.023
62. Cunningham MW. Cardiac myosin and the th1/th2 paradigm in autoimmune myocarditis. Am J Pathol. (2001) 159:5–12. doi: 10.1016/S0002-9440(10)61665-3
63. Okura Y, Yamamoto T, Goto S, Inomata T, Hirono S, Hanawa H, et al. Characterization of cytokine and inos mrna expression in situ during the course of experimental autoimmune myocarditis in rats. J Mol Cell Cardiol. (1997) 29:491–502. doi: 10.1006/jmcc.1996.0293
64. Shiraishi M, Shintani Y, Shintani Y, Ishida H, Saba R, Yamaguchi A, et al. Alternatively activated macrophages determine repair of the infarcted adult murine heart. J Clin Invest. (2016) 126:2151–66. doi: 10.1172/JCI85782
65. Frangogiannis NG, Mendoza LH, Lindsey ML, Ballantyne CM, Michael LH, Smith CW, et al. Il-10 is induced in the reperfused myocardium and may modulate the reaction to injury. J Immunol. (2000) 165:2798–808. doi: 10.4049/jimmunol.165.5.2798
66. DeBerge M, Yeap XY, Dehn S, Zhang S, Grigoryeva L, Misener S, et al. Mertk cleavage on resident cardiac macrophages compromises repair after myocardial ischemia reperfusion injury. Circ Res. (2017) 121:930–40. doi: 10.1161/CIRCRESAHA.117.311327
67. Yang Z, Zingarelli B, Szabo C. Crucial role of endogenous interleukin-10 production in myocardial ischemia/reperfusion injury. Circulation. (2000) 101:1019–26. doi: 10.1161/01.CIR.101.9.1019
68. Watanabe K, Nakazawa M, Fuse K, Hanawa H, Kodama M, Aizawa Y, et al. Protection against autoimmune myocarditis by gene transfer of interleukin-10 by electroporation. Circulation. (2001) 104:1098–100. doi: 10.1161/hc3501.096190
69. Chen X, Zeng XH, Wang M, Chen L, Zhang N, Rao M, et al. Bcl2-like protein 12 is required for the aberrant t helper-2 polarization in the heart by enhancing interleukin-4 expression and compromising apoptotic machinery in cd4+ t cells. Circulation. (2018) 138:2559–68. doi: 10.1161/CIRCULATIONAHA.118.033890
70. Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. (2004) 136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x
71. Frangogiannis NG. Regulation of the inflammatory response in cardiac repair. Circ Res. (2012) 110:159–73. doi: 10.1161/CIRCRESAHA.111.243162
72. Kuhl U, Noutsias M, Seeberg B, Schultheiss HP. Immunohistological evidence for a chronic intramyocardial inflammatory process in dilated cardiomyopathy. Heart. (1996) 75:295–300. doi: 10.1136/hrt.75.3.295
73. Kawai C. From myocarditis to cardiomyopathy: Mechanisms of inflammation and cell death: Learning from the past for the future. Circulation. (1999) 99:1091–100. doi: 10.1161/01.CIR.99.8.1091
74. Batawi S, Tarazan N, Al-Raddadi R, Al Qasim E, Sindi A, Al Johni S, et al. Quality of life reported by survivors after hospitalization for middle east respiratory syndrome (mers). Health Qual Life Outcomes. (2019) 17:101. doi: 10.1186/s12955-019-1165-2
75. Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS. The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health status. Respirology. (2010) 15:543–50. doi: 10.1111/j.1440-1843.2010.01720.x
76. Tanaka T, Ogata A, Narazaki M. Tocilizumab for the treatment of rheumatoid arthritis. Expert Rev Clin Immunol. (2010) 6:843–54. doi: 10.1586/eci.10.70
77. Bacchiega BC, Bacchiega AB, Usnayo MJ, Bedirian R, Singh G, Pinheiro GD. Interleukin 6 inhibition and coronary artery disease in a high-risk population: a prospective community-based clinical study. J Am Heart Assoc. (2017) 6:1–9. doi: 10.1161/JAHA.116.005038
78. McInnes IB, Thompson L, Giles JT, Bathon JM, Salmon JE, Beaulieu AD, et al. Effect of interleukin-6 receptor blockade on surrogates of vascular risk in rheumatoid arthritis: measure, a randomised, placebo-controlled study. Ann Rheum Dis. (2015) 74:694–702. doi: 10.1136/annrheumdis-2013-204345
79. Gabay C, McInnes IB, Kavanaugh A, Tuckwell K, Klearman M, Pulley J, et al. Comparison of lipid and lipid-associated cardiovascular risk marker changes after treatment with tocilizumab or adalimumab in patients with rheumatoid arthritis. Ann Rheum Dis. (2016) 75:1806–12. doi: 10.1136/annrheumdis-2015-207872
80. Soubrier M, Pei J, Durand F, Gullestad L, John A. Concomitant use of statins in tocilizumab-treated patients with rheumatoid arthritis: a post hoc analysis. Rheumatol Ther. (2017) 4:133–49. doi: 10.1007/s40744-016-0049-8
81. Chung ES, Packer M, Lo KH, Fasanmade AA, Willerson JT. Randomized, double-blind, placebo-controlled, pilot trial of infliximab, a chimeric monoclonal antibody to tumor necrosis factor-alpha, in patients with moderate-to-severe heart failure: Results of the anti-tnf therapy against congestive heart failure (attach) trial. Circulation. (2003) 107:3133–40. doi: 10.1161/01.CIR.0000077913.60364.D2
82. Setoguchi S, Schneeweiss S, Avorn J, Katz JN, Weinblatt ME, Levin R, et al. Tumor necrosis factor-alpha antagonist use and heart failure in elderly patients with rheumatoid arthritis. Am Heart J. (2008) 156:336–41. doi: 10.1016/j.ahj.2008.02.025
83. Giudicessi JR, Noseworthy PA, Friedman PA, Ackerman MJ. Urgent guidance for navigating and circumventing the qtc prolonging and torsadogenic potential of possible pharmacotherapies for covid-19. Mayo Clinic Proc. (2020). doi: 10.1016/j.mayocp.2020.03.024. [Epub ahead of print].
Keywords: Coronavirus Disease 2019, cardiovascular impairment, inflammation, cardiovascular diseases, cardiovascular anti-inflammatory therapy
Citation: Wang L, Zhang Y and Zhang S (2020) Cardiovascular Impairment in COVID-19: Learning From Current Options for Cardiovascular Anti-Inflammatory Therapy. Front. Cardiovasc. Med. 7:78. doi: 10.3389/fcvm.2020.00078
Received: 24 March 2020; Accepted: 15 April 2020;
Published: 30 April 2020.
Edited by:
Pietro Enea Lazzerini, University of Siena, ItalyReviewed by:
Elena Bartoloni, University of Perugia, ItalyBernhard Maisch, University of Marburg, Germany
Copyright © 2020 Wang, Zhang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuyang Zhang, c2h1eWFuZ3poYW5nMTAzQG5yZHJzLm9yZw==
†These authors have contributed equally to this work
 Lun Wang
Lun Wang Yang Zhang
Yang Zhang Shuyang Zhang
Shuyang Zhang