- Division of Cardiovascular Medicine and Endocrinology and Metabolism, Faculty of Medicine, Tottori University, Yonago, Japan
Background: Acute myocardial infarction (AMI) and acute ischemic stroke (AIS) are the leading causes of death globally. Cardio-cerebral infarction (CCI) is the rare occurrence of AMI and AIS, either simultaneously or one after the other. Treatment recommendations are not clear in case of the occurrence of AMI and AIS simultaneously, especially the strategy of primary percutaneous coronary intervention (PCI).
Case presentation: We report consecutive seven case series of patients with CCI who underwent primary PCI in our institute. Comorbidities, strategy of primary PCI, and outcomes were investigated. All patients presented with the chief complaints associated with stroke. Atrial fibrillation (AF) was complicated in five of CCI patients, and four of AF patients were not anticoagulated. The major causes of stroke were cardiogenic and/or hemodynamic in this case series. All patients showed total occlusion in the culprit lesion, and six patients had other diseased vessels. Thrombus aspiration was mainly chosen as the reperfusion strategy in PCI. However, only two patients were diagnosed as definitive coronary embolism, and stenting was needed in six patients due to severe atherosclerotic lesion in culprit coronary artery. Final thrombolysis in myocardial infarction (TIMI) 3 flow was achieved only in four patients. Hemorrhagic complications occurred in three patients. Two patients died during in-hospital stay, and most had to be transferred for rehabilitation.
Conclusions: CCI was a rare but fatal condition in patients who underwent primary PCI. Although CCI was associated with concomitant atrial fibrillation, organic coronary stenosis requiring stenting for revascularization was present in almost all the cases. Given the complexity of coronary artery lesions and high in-hospital mortality, further investigations are needed to determine the optimal treatment strategy.
1. Introduction
Acute myocardial infarction (AMI) and acute ischemic stroke (AIS) are the leading causes of death globally (1). In ST-segment elevation myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) contributes to high revascularization success rates, less cardiac events, and earlier discharge, and is effective even in patients with cardiogenic shock (2–4). In terms of AIS, thrombolysis has been a standard care, and endovascular thrombectomy has been used more aggressively in recent years, contributing to improved prognosis (5, 6) However, treatment recommendations are not clear in cases combining AMI and AIS. Cardio-cerebral infarction (CCI) is the rare occurrence of AMI and AIS, either at the same time (simultaneous or synchronous) or one after the other (metachronous) (7). It has been reported that the prognosis is poor with high rates of hemorrhagic events and in-hospital mortality, and primary PCI was performed in only 14% of cases of CCI (8). There were few reports on the treatment strategy of CCI, especially the strategy of primary PCI. Therefore, we retrospectively reviewed the records of 808 patients who underwent primary PCI for AMI from April 2012 to March 2022 in Tottori University Hospital. Patients with concurrent AIS during the same hospitalization were included in this case series, and obvious iatrogenic cerebral infarction (catheter induced) was excluded. Here, we report seven patients with CCI who underwent primary PCI in terms of the patient background, coronary angiographic characteristics, strategy of primary PCI, and clinical outcomes.
2. Case series
The ethics committee of Tottori University Hospital permits case reporting without obtaining written consent from each patient in accordance with the Ethical Guidelines for Epidemiological studies established by the Ministry of Health, Labour and Welfare, Japan.
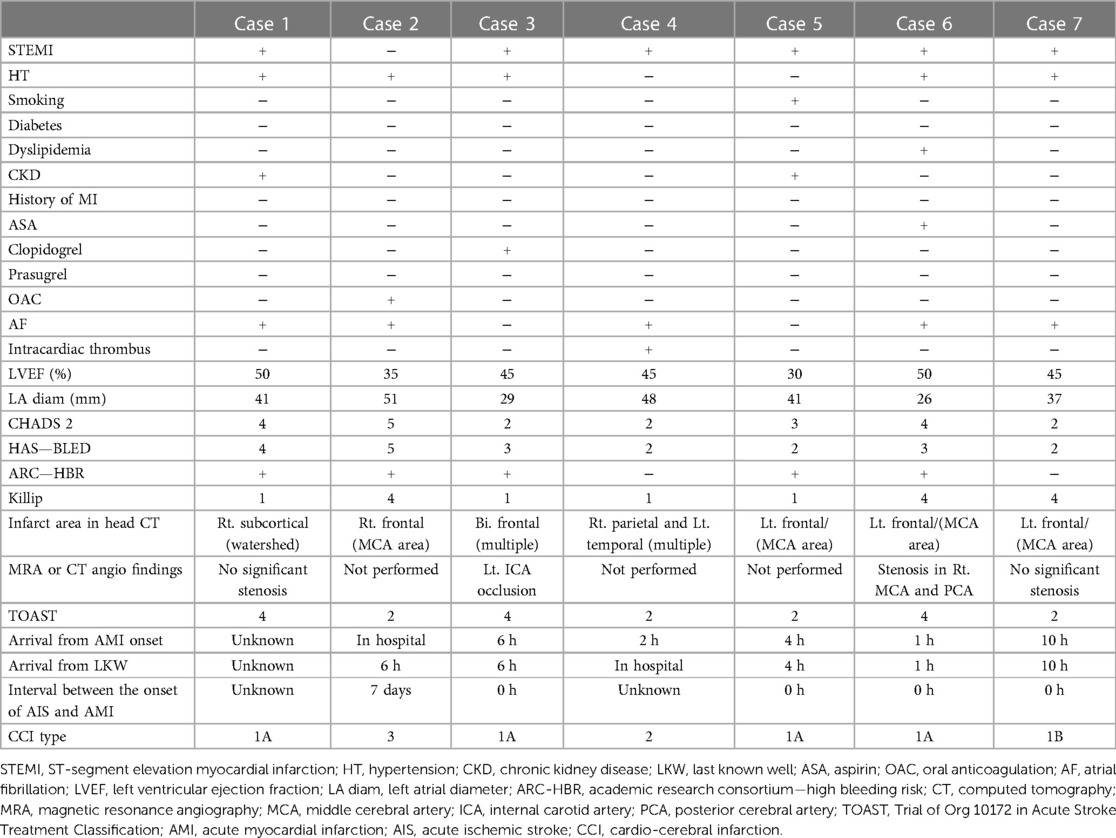
The background of the seven patients is shown in Table 1. The background of the patients comprised age, gender, type of AMI, hypertension, smoking, diabetes, dyslipidemia, chronic kidney disease, history of myocardial infarction, taking aspirin, clopidogrel of prasugrel, oral anticoagulation, history of atrial fibrillation (AF), Killip classification, the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification (9), and CCI type. The type of CCI was classified based on the definitions reported by Habib et al. (10).
Patients ranging in age from 40s to 90s were enrolled in this case series. Four patients were female and have fewer common coronary risk factors. Most patients had high bleeding and embolic risk. AF was highly consistent with CCI patients, and four of five AF patients were not anticoagulated. The cases with untreated AF consisted of elderly patients who had no cerebrovascular events and did not choose anticoagulation before admission. All patients presented with the chief complaints associated with stroke: hemiplegia, dysarthria, ataxia, apraxia, loss of speech, loss of consciousness, and hemispatial neglect on admission. The major causes of stroke were cardiogenic and/or hemodynamic in this case series.
No patient underwent endovascular treatment or thrombolytic therapy for AIS in this case series, because most was unstable or had a long or uncertain time since last known well. Because of unstable condition, adequate neurological assessment with cerebrovascular imaging such as contrast-enhanced computed tomography (CT) or magnetic resonance angiography was not conducted in three cases.
The patients were pretreated with 200 mg aspirin and 300 mg clopidogrel or 20 mg prasugrel as the loading doses, followed by intravenous heparin boluses during the procedure to maintain an activated clotting time of >250 s. Before PCI, coronary angiography was performed, and the thrombolysis in myocardial infarction (TIMI) flow and Rentrop grade were evaluated at the initial angiography. The PCI strategy such as thrombus aspiration, plain old balloon angiography (POBA), and stenting was left to the discretion of each physician. Glycoprotein IIb/IIIa inhibitors are not available in Japan.
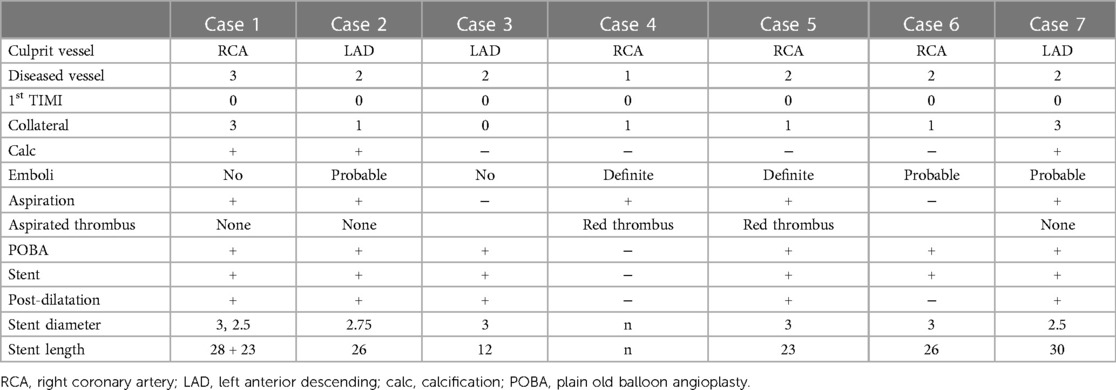
The angiographic and therapeutic characteristics are shown in Table 2. A diseased vessel was defined as numbers of non-culprit vessel that showed over 75% stenosis. Coronary embolism was judged as definite or probable by using the diagnostic criteria previously reported (11).
All the patients showed total occlusion in the culprit lesion, and six patients had other diseased vessels. Only two patients were diagnosed as definitive coronary embolism. Thrombus aspiration was mainly chosen as the reperfusion strategy in PCI. However, retrieved visible thrombus was obtained in only two cases. Stenting was needed in six patients due to severe atherosclerotic lesion in culprit coronary artery, and relatively long stenting and post-dilation also tended to be required. Although one case (case 5) was diagnosed as a definitive coronary artery embolism based on the algorithm described above (11), the patient underwent stenting due to the concomitant atherosclerotic lesion.
Treatments post-PCI and outcomes are shown in Table 3. IABP was used in three patients, but final TIMI 3 flow was achieved in four patients (57.1%). Three patients required intensive antithrombotic therapy including dual antiplatelet and anticoagulation, and hemorrhagic complications occurred in three patients. Despite AF, case 2 was not prescribed anticoagulation therapy because of her advanced age. Conversely, AF was not detected in case 3, but he underwent triple therapy (dual antiplatelet therapy and anticoagulation) because the embolic cause could not be ruled out. In-hospital mortality was 28.6%, and four of five survived patients were transferred to satellite hospitals.
A representative case of CCI requiring stenting for myocardial infarction due to severe atherosclerotic lesions (case 7) is shown in Figure 1. The patient was admitted to the emergency room with a chief complaint of impaired consciousness and right hemiplegia for the past 9 h. She was diagnosed with AIS in the left middle cerebral artery area, and obvious ischemic changes were already detected by head CT (Figure 1A). However, the electro-cardiogram showed AF and ST-segment elevation in the anterior leads (Figure 1B). The chest x-ray showed cardiomegaly and pulmonary congestion (Figure 1C). Primary PCI was performed because of suspected pulmonary edema due to anterior STEMI. Angiography showed total occlusion in the proximal of left anterior descending artery (Figure 1D). Although we strongly suspected coronary embolism because of the concomitant AF and AIS, repeated thrombectomy and balloon angioplasty were ineffective. Intra-vascular ultrasound showed severe calcification and diffuse atherosclerotic lesion in the proximal to the middle of left anterior descending artery (Figure 1E). Stenting was effective to gain the recanalization, and post-dilatation was performed. Anticoagulation and antiplatelet therapy were administered to prevent recurrence, and she was transferred to a satellite hospital 2 months later without hemorrhagic stroke (Figure 1F).
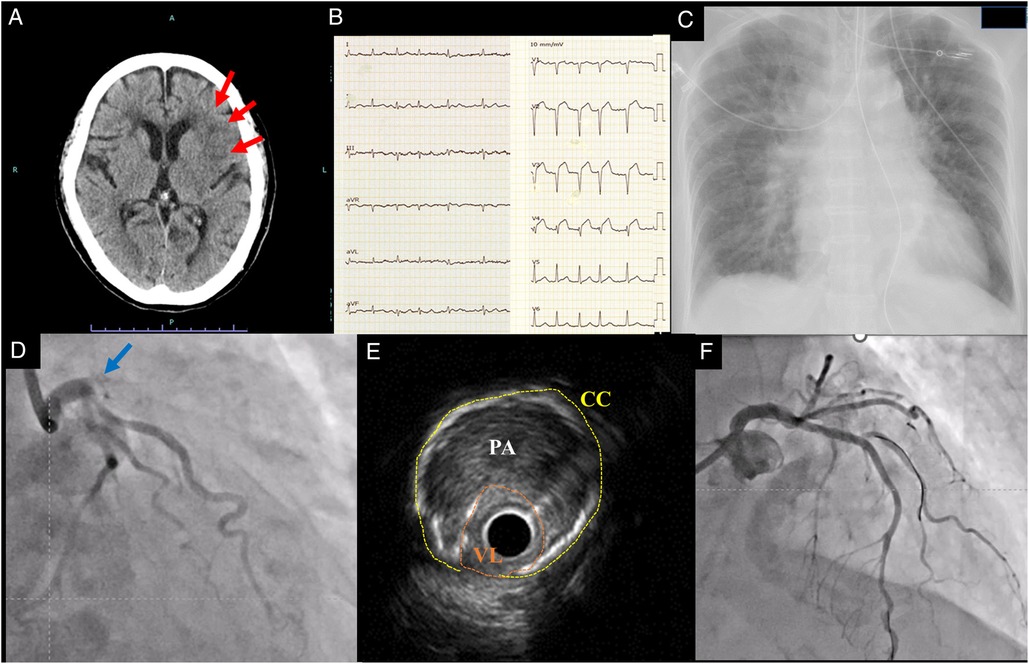
Figure 1. Representative case of cardio-cerebral infarction requiring coronary stenting for myocardial infarction. Head CT showed low density area in left middle cerebral artery area (red allows) at admission (A). Electro-cardiogram showed ST-segment elevation in anterior leads (B). Chest X ray showed pulmonary congestion (C). Coronary angiography showed total occlusion at proximal of left anterior descending artery (blue arrow) (D). Intravascular ultrasound showed that vessel lumen (VL) was narrowed (highlighted in orange) by plaque area (PA) and circumferential calcification (CC) (highlighted in yellow) due to atherosclerotic changes in the culprit lesion (E). TIMI 3 flow was obtained after stenting, and the stented lesion was indicated (F).
3. Discussion
We described seven patients with CCI who underwent primary PCI. AF was highly complicated in CCI patients (71.4%), and thrombus aspiration was mainly selected as the initial reperfusion strategy in PCI. However, stenting was needed in six of seven patients due to severe atherosclerotic lesion in culprit coronary artery. In-hospital mortality was as high as 28.6%, and most of the survived patients required transfer to satellite hospitals.
Considering the current case series, the prevalence of CCI was 0.87% in AMI patients who underwent primary PCI. The prevalence of diabetes was lower and that of AF was higher in CCI patients as compared with typical ACS patients in Japan (12). In this report, the CCI patients were mostly without the prescription of anticoagulant before the admission and were clinically treated as Type 2 (cardio-embolic) of the TOAST classification. However, coronary lesions resisted stentless strategy including aspiration, and finally required stenting. Yeo et al. (13) also reported that three of three CCI patients who underwent PCI required stenting.
The use of PCI with stenting requires peri-procedural heparin infusion, and long-term use of dual antiplatelet therapy. Especially, stenting in AMI patients requires more intense antiplatelet therapy, including loading dose. Previous report suggested that this was the reason for hesitation regarding primary PCI in acute stroke patients, but two of two CCI patients without primary PCI died (14). A small retrospective study by Schmidbauer et al. (15) showed that the incidence of intracerebral hemorrhage in AIS patients was not increased by cardiac catheterization including PCI. Coronary stenting should not be necessarily hesitated in cases of STEMI or obvious hemodynamic instability even in the acute phase of CCI.
Post-PCI antithrombotic therapy should be considered integrated as appropriate antithrombotic therapy with the target of reducing embolic events and bleeding complications in the current guidelines (16). In this case series, three patients were treated with intensive antithrombotic therapy including dual antiplatelet and anticoagulation therapy. This may be due to the inclusion of cases before the current guidelines were disseminated. If treatment is based on this current strategy, de-escalation of antithrombotic therapy may reduce bleeding complications even if stenting is used.
Ideally, comprehensive examinations and simultaneous treatment for infarction of the two organs should be performed. Although intravenous thrombolysis for AIS and AMI seems to be an appropriate approach in this context, there is a dilemma regarding the different indications and dosages of intravenous alteplase in the treatment of AIS and AMI (14). Furthermore, thrombolysis does not always provide a recanalization, and endovascular treatments are increasingly used in AIS (17). Treatment algorithms and concepts including endovascular treatment have been proposed, and further research is needed for the ideal management strategy that provides the best outcomes (13, 18). This case series reported that AMI was mostly attributed to severe arteriosclerotic coronary artery disease rather than to an embolic mechanism in patients with CCI. It suggests that stenting is likely to be necessary in the treatment of CCI even if there is a concomitant embolic event.
CCI is a rare condition in patients who underwent primary PCI. Although CCI was frequently associated with concomitant AF, organic coronary stenosis requiring stenting for revascularization was present in most cases in this study. Given the complexity of coronary artery lesions and high in-hospital mortality, further investigations are needed to determine the optimal treatment strategy.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
We did not take written informed consent for each patient in this case series, because opt-out case reporting is allowed by Tottori University Hospital's Ethics Committee in accordance with Japanese ethical guidelines. The opt-out for case reporting is posted on the hospital's website: https://www2.hosp.med.tottori-u.ac.jp/introduction/privacy-policy.html#houkoku. Personal identifiable information (age, gender) was avoided in accordance with the journal's guidelines.
Author contributions
TW has drafted the work and is also the corresponding author. SK and RA analyzed the patient data. KY had modified version and substantively revised the work. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bacci MR, Santos JA. Stroke and myocardial infarction: a terrible association. BMJ Case Rep. (2012):2012. doi: 10.1136/bcr-2012-007089
2. Ozaki Y, Hara H, Onuma Y, Katagiri Y, Amano T, Kobayashi Y, et al. CVIT Expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) update 2022. Cardiovasc Interv Ther. (2022) 37(1):1–34. doi: 10.1007/s12928-021-00829-9
3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. (2018) 39(2):119–77. doi: 10.1093/eurheartj/ehx393
4. Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. (2016) 67(10):1235–50. doi: 10.1016/J.JACC.2015.10.005
5. Broderick JP, Hill MD. Advances in acute stroke treatment 2020. Stroke. (2021) 52:729–34. doi: 10.1161/STROKEAHA.120.033744
6. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50(12):E344–418. doi: 10.1161/STR.0000000000000211
7. Omar HR, Fathy A, Rashad R, Helal E. Concomitant acute right ventricular infarction and ischemic cerebrovascular stroke; possible explanations. Int Arch Med. (2010) 3(1). doi: 10.1186/1755-7682-3-25
8. de Castillo LLC, Diestro JDB, Tuazon CAM, Sy MCC, Añonuevo JC, San Jose MCZ. Cardiocerebral infarction: a single institutional series. J Stroke Cerebrovasc Dis. (2021) 30(7). doi: 10.1016/j.jstrokecerebrovasdis.2021.105831
9. Love BB, Bendixen BH. Classification of subtype of acute ischemic stroke definitions for use in a multicenter clinical trial. Stroke. (1993) 24(1):35–41. doi: 10.1161/01.str.24.1.35
10. Habib M. Cardio-cerebral infarction syndrome: definition, diagnosis, pathophysiology, and treatment. J Integr Cardiol. (2021) 7(1). doi: 10.15761/JIC.1000308
11. Shibata T, Kawakami S, Noguchi T, Tanaka T, Asaumi Y, Kanaya T, et al. Prevalence, clinical features, and prognosis of acute myocardial infarction attributable to coronary artery embolism. Circulation. (2015) 132(4):241–50. doi: 10.1161/CIRCULATIONAHA.114.015134
12. Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, et al. Management and two-year long-term clinical outcome of acute coronary syndrome in Japan—prevention of atherothrombotic incidents following ischemic coronary attack (PACIFIC) registry. Circ J. (2013) 77(4):934–43. doi: 10.1253/circj.cj-13-0174
13. Yeo LLL, Andersson T, Yee KW, Tan BYQ, Paliwal P, Gopinathan A, et al. Synchronous cardiocerebral infarction in the era of endovascular therapy: which to treat first? J Thromb Thrombolysis. (2017) 44(1):104–11. doi: 10.1007/s11239-017-1484-2
14. Ibekwe E, Kamdar HA, Strohm T. Cardio-cerebral infarction in left MCA strokes: a case series and literature review. Neurol Sci. (2022) 43(4):2413–22. doi: 10.1007/s10072-021-05628-x
15. Schmidbauer ML, Rizas KD, Tiedt S, Dimitriadis K. Low rate of intracerebral hemorrhage after cardiac catheterization in patients with acute ischemic stroke in a large case series. Clin Neurol Neurosurg. (2020) 198. doi: 10.1016/j.clineuro.2020.106159
16. Nakamura M, Kimura K, Kimura T, Ishihara M, Otsuka F, Kozuma K, et al. JCS 2020 Guideline focused update on antithrombotic therapy in patients with coronary artery disease. Circ J. (2020) 84(5):831–65. doi: 10.1253/circj.CJ-19-1109
17. Nardai S, Lanzer P, Abelson M, Baumbach A, Doehner W, Hopkins L, et al. Interdisciplinary management of acute ischaemic stroke: current evidence training requirements for endovascular stroke treatment: position paper from the ESC council on stroke and the European Association for Percutaneous Cardiovascular Interventions with the support of the European Board of Neurointervention. Eur Heart J. (2021) 42(4):298–307. doi: 10.1093/eurheartj/ehaa833
18. Nardai S, Vorobcsuk A, Nagy F, Vajda Z. Successful endovascular treatment of simultaneous acute ischaemic stroke and hyperacute ST-elevation myocardial infarction: the first case report of a single-operator cardio-cerebral intervention. Eur Heart J Case Rep. (2021) 5(11). doi: 10.1093/ehjcr/ytab419
Keywords: acute myocardial infarction, acute ischemic stroke, coronary embolism, primary percutaneous coronary intervention, cardio-cerebral infarction, case report
Citation: Watanabe T, Kobara S, Amisaki R and Yamamoto K (2023) Primary percutaneous coronary intervention for cardio-cerebral infarction: a case report. Front. Cardiovasc. Med. 10:1165735. doi: 10.3389/fcvm.2023.1165735
Received: 14 February 2023; Accepted: 13 July 2023;
Published: 31 July 2023.
Edited by:
Mauro Chiarito, Humanitas University, ItalyReviewed by:
Pradyumna Agasthi, Mayo Clinic, United StatesJaroslaw Zalewski, Jagiellonian University Medical College, Poland
Akihiko Takahashi, Kobe Women’s University, Japan
© 2023 Watanabe, Kobara, Amisaki and Yamamoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tomomi Watanabe dG93YXRhbmFiZS10dHJAdW1pbi5hYy5qcA==
 Tomomi Watanabe
Tomomi Watanabe Satoshi Kobara
Satoshi Kobara Ryosuke Amisaki
Ryosuke Amisaki