Abstract
Background:
Statistics show that approximately 70% of patients with acute ST-segment elevation myocardial infarction (STEMI) experience relief from chest pain symptoms within 48 h post-percutaneous coronary intervention (PCI). However, over 30% of these patients still suffer from angina post-PCI during their hospital stay and after discharge. Although the interrelation between cardiovascular diseases and psychological states, notably anxiety and stress, has been extensively studied and acknowledged, the specific influence of anxiety disorders on post-PCI clinical outcomes for STEMI patients, especially the recurrence of angina, remains undefined.
Methods:
This study included a total of 324 STEMI patients who underwent PCI treatment due to chest pain in our hospital. Baseline and surgical data for all patients were collected. During their hospital stay, patients’ emotional states were assessed using the Hamilton Anxiety Scale, while angina was evaluated using the Seattle Angina Questionnaire. All patients were followed up for 6 months post-discharge to gather clinical data and outcomes, analyzing whether anxiety disorders would affect the recurrence of angina post-PCI in STEMI patients.
Results:
Out of the 324 patients, 82 experienced recurrent angina symptoms within 6 months post-PCI discharge. Compared to the non-recurrence group, the recurrence group showed statistically significant differences in anxiety levels. Other differing factors included the spouse's health status, cardiac Killip classification, severity of coronary lesions, and the state of the coronary microcirculation. After utilizing propensity score matching to eliminate inherent biases between the two groups at a 1:1 ratio, the COX regression analysis indicated that a patient's anxiety status is a risk factor for the occurrence of angina post-PCI in STEMI patients (HR = 2.094, 95% CI = 1.248–3.514, P = 0.005).
Conclusion:
Anxiety is a significant factor for short-term recurrence of angina post-PCI in STEMI patients. This further confirms the crucial impact of mental health on cardiovascular wellness.
1. Introduction
Angina is a clinical syndrome resulting from an imbalance in the myocardial oxygen supply, leading to myocardial ischemia. The primary triggers for its onset are either an increased oxygen demand by the heart or a reduction in the blood flow through the coronary arteries. Clinically, reduced blood flow due to coronary lesions often precipitates angina, with the most severe type being Acute Myocardial Infarction (AMI) (1). Emotional distress, excessive fatigue, and poor lifestyle choices all play significant roles in triggering angina (2). Percutaneous Coronary Intervention (PCI) can quickly restore blood flow in obstructed vessels, effectively alleviating chest pain, reducing AMI mortality, and enhancing patient quality of life. Its efficacy in reducing myocardial ischemia is significantly superior to pharmacotherapy (3). However, not all patients experience complete relief from chest pain post-PCI; some face a recurrence shortly after discharge. Studies indicate (4) that the recurrence of anginal symptoms post-PCI is a risk factor for adverse cardiovascular events. Compared to those without recurrent pain, patients experiencing chest pain recurrence within a year post-PCI face medical costs that are 1.8 times higher (5). This highlights the need to further investigate and understand the myriad factors that may precipitate angina recurrence, to mitigate its impact on patient health and the healthcare system. Anxiety can directly impact cardiac function and potentially increase the risk of angina recurrence indirectly through influencing patient behavior and lifestyle choices. Hence, providing a more accurate risk assessment and management strategy, further optimizing the treatment and recovery of STEMI patients, and exploring the link between anxiety and angina recurrence becomes crucial.
2. Literature review
Through the exploration and review of existing literature, we find that anxiety has a dual impact on human health: on one hand, it can trigger various self-protective mechanisms in the body (such as preventing the recurrence of traumatic memories and enhancing immune responses), while on the other hand, excessive anxiety can lead to a series of severe pathological conditions (such as cytokine storms within the body, post-traumatic stress disorder, and myocardial infarction) (6). A study of notable significance was conducted in 2011 by Swedish scholar Falkstedt D and colleagues (7), which encompassed a sample of 49,321 men. The subjects were assessed for anxiety prior to their conscription and were followed up for 37 years. It was concluded that anxiety disorders are closely related to the onset of cardiovascular diseases and acute myocardial infarctions. A domestic study reflecting the beneficial impact of treating anxiety disorders for better prognosis of coronary heart disease was identified (8). In this study, patients with coronary heart disease and anxiety disorders were divided into two groups. The first group received conventional coronary heart disease drug treatment, while the second group received anti-anxiety medication in addition to the conventional treatment. After a 12-week follow-up, the study results indicated that both drug and exercise therapies can delay the progression of coronary heart disease in patients with anxiety disorders. This implies that addressing anxiety disorders in tandem with the primary disease can be highly beneficial. Rutger W (9) found through patient-centered personalized networks and remote cardiac monitoring that anxiety disorders impact the morbidity of coronary artery disease patients. Improving anxiety disorders can reduce the recurrence rate and mortality of discharged patients with coronary heart disease. There are also domestic and international reports on the impact of anxiety disorders on hypertension, heart failure, and other cardiovascular diseases (10, 11).
The mechanism by which anxiety affects cardiovascular diseases is still not clear. Some scholars propose that anxiety disorders might influence the development of cardiovascular diseases through pathways. The most accepted mechanism is that anxiety leads to hyperactivation of the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system, increased release of plasma catecholamines, and endothelial damage, eventually causing arteriosclerosis, coronary artery disease, and acute coronary events. This can also explain the relationship between anxiety and hypertension. Some scholars believe that the cardiovascular effects of psychological stressors such as anxiety and depression are consistent (12). Acute anxiety and cardiovascular stress lead to increased resting heart rate reactivity, decreased heart rate variability, impaired baroreflex function, and increased ventricular repolarization variability. In summary, the hyperactive sympathetic nervous system and the hypothalamic-pituitary-adrenal axis release nerve impulses that control cardiac activity changes, a process that may increase the risk of cardiovascular diseases, further increasing the risks of cardiac ischemia, arrhythmias, and sudden cardiac death.
Though current theoretical knowledge offers explanations for how anxiety impacts cardiovascular diseases, there's a lack of corresponding clinical research both domestically and internationally to confirm these theories. In our clinical work, designing a scientific research plan to demonstrate how anxiety promotes the progression of cardiovascular diseases, and studying the relationship between post-PCI STEMI patient angina recurrence and anxiety, is a preferred choice within a controllable scope. Due to sample size limitations and the presence of errors, conventional statistics might not produce relatively accurate results. Propensity Score Matching (PSM) is an innovative method to some extent to overcome endogeneity bias and is highly recommended in academic circles. Therefore, this study uses the PSM method to explain the baseline data of the research subjects and further conducts statistical analysis.
3. Materials and methods
3.1. Study subjects
This study included a total of 324 cases from January 2019 to December 2022, who visited our hospital due to chest pain, met the inclusion criteria, and had complete hospitalization records. All patients were admitted with evidence of STEMI based on a 12-lead bedside ECG and exhibited relief from chest pain symptoms upon discharge after undergoing PCI. A 6-month follow-up was conducted for all patients. Based on the follow-up results, patients were divided into two groups: chest pain recurrence group (Group I, n = 82) and non-recurrence group (Group II, n = 242). Inclusion criteria were: (1) Age ≥18 years; (2) Indications met for PCI; (3) Absence of angina symptoms at discharge post-PCI; (4) Clear consciousness. Exclusion criteria included: (1) Chronic heart failure, severe arrhythmias, or other cardiovascular diseases; (2) Infectious diseases; (3) Severe hepatic or renal dysfunction; (4) Malignant tumors; (5) Mental disorders; (6) Poor compliance or lost to follow-up (Figure 1).
Figure 1
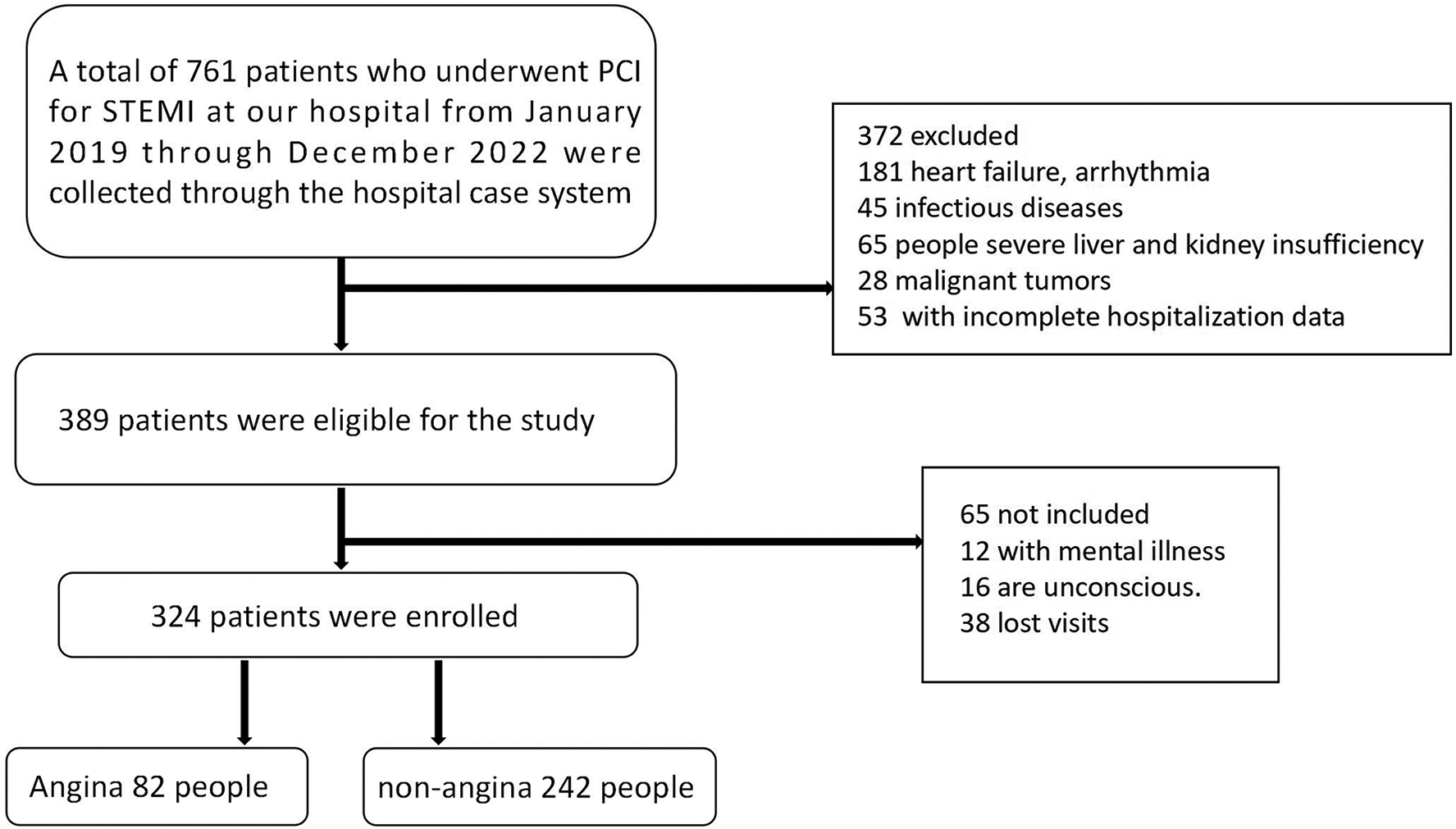
Study flow diagram.
3.2. Variable description
-
(1)
Dependent variable: Recurrence of angina in patients. The Seattle Angina Questionnaire (SAQ) was used to score angina, with the scale consisting of 5 main sections and 19 items. After scoring each item, corresponding formulas were used to convert scores to standard points, ranging from 0 to 100. A higher score suggests milder clinical symptoms (13). In this study, an SAQ score between 75 and 100 was considered as no angina.
-
(2)
Key independent variable: Patient's anxiety level. The Hamilton Anxiety Rating Scale (HAMA) was used to assess anxiety levels in both groups, with HAMA scores ranging from 0 to 56. A higher score indicates severe anxiety (14). In this study, a HAMA score >10 was defined as an anxiety disorder.
-
(3)
Control variables: These primarily included patients’ baseline clinical data, surgical details, and postoperative medications. Data, such as gender, age, Body Mass Index (BMI), economic status, spouse's health condition, smoking history, hypertension, diabetes, and history of hyperlipidemia were retrospectively collected from the hospital's medical records system. Some continuous variables were transformed into categorical ones for statistical convenience. Information was gathered by the nursing department during patients’ hospital admission. Economic status was based on the average annual income of local residents, with those earning below 50% of the average considered poor and above 100% as wealthy. Spousal health status was differentiated based on their activity level, categorized as healthy, ill, or no spouse. Illnesses included stroke, Alzheimer's, arthritis, fractures, vision or mental disorders, heart disease, and chronic pulmonary diseases that limit activity. Before surgery, all patients were given a dual antiplatelet therapy combination of aspirin with either ticagrelor or clopidogrel. The time of preoperative chest pain was noted. During the operation, three experienced coronary intervention surgeons assessed the coronary lesions of the patients. Intraoperative data such as thrombolysis, stent implantation, and circulation status (evaluated by TIMI grading) were recorded. Unless contraindicated, patients were given dual antiplatelet therapy (aspirin with either ticagrelor or clopidogrel) and statins post-operation. Additionally, treatment options such as β-blockers, ACE inhibitors (ACEI)/Angiotensin II receptor blockers (ARB), nitrate vasodilators, etc., were administered as needed. Postoperative relief of chest pain symptoms within 36 h and in-hospital adverse events (excluding chest pain recurrence), such as severe hypotension, acute heart failure, arrhythmia, shock, and puncture site infection, were noted.
3.3. Follow-up details
Researchers followed up with all study participants for 6 months post-discharge through outpatient visits, patient chat groups, phone calls, and text messages. The average follow-up time was 150 days The main focus of the follow-up was the recurrence of angina within 6 months post-discharge and if the SAQ score met the angina criteria, noting the time of angina recurrence.
3.4. Statistical methods
Data were analyzed using SPSS 27.0 and R 4.3.1 software. The Shapiro-Wilk test was employed to check for the normality of continuous variables. Non-normally distributed data were expressed as median (P25, P75) and analyzed using the Mann-Whitney U test. Categorical variables were expressed in percentages and compared using the Chi-square test or Fisher's exact test. COX regression analysis was conducted to identify risk factors for post-PCI angina recurrence, calculating hazard ratios (hr) and 95% CI. The Kaplan-Meier method was used to plot survival curves, and the log-rank test compared differences between patient groups with varying clinical pathologies. The PSM method was employed to match certain baseline data and other significant differences, setting a caliper value of 0.02. Patients were matched in a 1:1 ratio based on closest scores. A P-value of <0.05 was considered statistically significant.
4. Results and analysis
4.1. Comparison of baseline data, surgical information, and postoperative medication between the two groups of patients. A total of 324 subjects were included in this study. Based on follow-up results, 82 individuals experienced recurrent angina within 6 months.
For baseline data, there were no significant differences between the two groups in terms of gender, age, BMI, economic background, and personal history, including smoking, hypertension, diabetes, hyperlipidemia, etc. (P > 0.05). Patients with recurrent angina had a higher prevalence of anxiety disorders and their spouses were in poorer health, primarily reflected in a higher likelihood of their spouses having illnesses. The difference was statistically significant (P < 0.05), as shown in Table 1.
Table 1
| Characteristics | Totality | Group I | Group II | P |
|---|---|---|---|---|
| Sex | 0.442 | |||
| Male | 252 (77.8) | 61 (74.4) | 191 (78.9) | |
| Female | 72 (22.2) | 21 (25.6) | 51 (21.1) | |
| Age | 0.307 | |||
| ≥65 | 160 (49.4) | 46 (56.1) | 118 (48.8) | |
| <65 | 164 (50.6) | 36 (43.9) | 124 (51.2) | |
| BMI | 0.701 | |||
| >24 | 179 (55.2) | 47 (57.3) | 132 (54.2) | |
| ≤24 | 145 (44.8) | 35 (42.7) | 110 (45.5) | |
| Economic situation | 0.931 | |||
| Normal | 243 (75) | 63 (76.8) | 180 (74.4) | |
| Poor | 42 (13) | 10 (12.2) | 32 (13.2) | |
| Rich | 39 (12) | 9 (11.0) | 30 (12.4) | |
| Spouse | <0.001 | |||
| Well | 208 (64.2) | 38 (46.3) | 170 (70.2) | |
| Unwell | 94 (29) | 36 (43.9) | 58 (24.0) | |
| None | 22 (6.8) | 8 (9.8) | 14 (5.8) | |
| Smoking | 0.610 | |||
| Yes | 167 (51.5) | 40 (48.8) | 127 (52.5) | |
| No | 157 (48.5) | 42 (51.2) | 115 (47.5) | |
| Hypertension | 0.121 | |||
| Yes | 184 (56.8) | 53 (64.6) | 131 (54.1) | |
| No | 140 (43.2) | 29 (35.4) | 111 (45.9) | |
| Diabetes | 0.172 | |||
| Yes | 105 (32.4) | 32 (39) | 73 (30.2) | |
| No | 219 (67.6) | 50 (61) | 169 (69.8) | |
| Hyperlipemia | 0.655 | |||
| Yes | 77 (23.8) | 21 (25.6) | 56 (23.1) | |
| No | 247 (76.2) | 61 (74.4) | 186 (76.9) | |
| Anxiety | <0.001 | |||
| Yes | 231 (71.3) | 36 (43.9) | 57 (23.6) | |
| No | 93 (28.7) | 46 (56.1) | 185 (76.4) | |
| Follow-up time | 164 (144–180) | 101.5 (62.5–135) | 172 (158.5–180) | <0.001 |
Comparison of baseline data between the two groups of patients.
Follow-up time in days. Group I (n = 82), Group II (n = 242). Spouse means spouse's health, well means healthy spouse, unwell means unhealthy spouse, none means no spouse.
Regarding surgical information, there were no differences between the two groups in terms of ischemic time before surgery and whether the myocardial infarction site was an anterior wall infarction (P > 0.05). Significant differences were found between the recurrent angina group and the non-recurrent group in terms of Killip classification of myocardial infarction, the number of coronary artery lesions, the number of stents implanted, intraoperative thrombolysis, postoperative revascularization status, TIMI score, and TMBG score (P < 0.05). See Table 2 for details.
Table 2
| Characteristics | Totality | Group I | Group II | P |
|---|---|---|---|---|
| Ischemic time | 0.087 | |||
| 0–6 | 201 (62.0) | 59 (72.0) | 142 (58.7) | |
| 6–12 | 56 (17.3) | 12 (14.6) | 44 (18.2) | |
| >12 | 67 (20.7) | 11 (13.4) | 56 (23.1) | |
| AWMI | 0.203 | |||
| Yes | 150 (46.3) | 43 (52.4) | 107 (44.2) | |
| No | 174 (53.7) | 39 (47.6) | 135 (55.8) | |
| Killip grading | <0.001 | |||
| 1 | 207 (63.9) | 33 (40.2) | 174 (71.9) | |
| 2 | 72 (22.2) | 17 (20.7) | 55 (22.7) | |
| ≥3 | 45 (13.9) | 32 (39.1) | 13 (5.4) | |
| Coronary lesions | <0.001 | |||
| 1 | 170 (52.5) | 30 (36.6) | 140 (57.9) | |
| 2 | 120 (37.0) | 32 (39.0) | 88 (36.4) | |
| ≥3 | 34 (10.5) | 20 (24.4) | 14 (5.8) | |
| Stents implantation | 0.022 | |||
| 1 | 194 (59.9) | 46 (56.1) | 148 (61.2) | |
| 2 | 93 (28.7) | 24 (29.3) | 69 (28.5) | |
| ≥3 | 15 (4.6) | 1 (1.2) | 14 (5.8) | |
| 0 | 22 (6.8) | 11 (13.4) | 11 (4.5) | |
| Thrombolysis | 0.012 | |||
| Yes | 208 (64.2) | 39 (47.6) | 77 (31.8) | |
| No | 116 (35.8) | 43 (53.4) | 165 (38.2) | |
| Revascularization mode | <0.001 | |||
| SCLCR | 170 (52.5) | 30 (36.6) | 140 (57.9) | |
| MCLCR | 47 (14.5) | 11 (13.4) | 36 (14.9) | |
| MCLIR | 107 (33.0) | 41 (50.0) | 66 (27.3) | |
| TIMI | <0.001 | |||
| 1 | 4 (1.2) | 3 (3.7) | 1 (0.4) | |
| 2 | 72 (22.3) | 29 (35.4) | 43 (17.8) | |
| 3 | 248 (76.5) | 50 (61.0) | 198 (81.8) | |
| TMBG | <0.001 | |||
| 1 | 4 (1.2) | 3 (3.7) | 1 (0.4) | |
| 2 | 76 (23.5) | 27 (32.9) | 44 (18.2) | |
| 3 | 244 (75.3) | 52 (63.4) | 197 (81.4) |
Comparison of surgical data between the two groups of patients.
Ischemic time in hours. AWMI: anterior wall myocardial infarction. Coronary lesions: Number of coronary lesions. Stents implantation: Number of coronary stents implanted. Revascularization modalities include the following classifications: SCLCR means complete revascularization of a single vessel, MCLCR means complete revascularization of multiple vessels, MCLIR means incomplete revascularization of multiple vessels.
Concerning postoperative changes and medication, there were no noticeable differences between the two groups in adverse events during hospitalization and medication use (P > 0.05). However, there was a significant difference between the two groups in terms of chest pain relief within 36 h post-surgery. The group with recurrent chest pain had a higher proportion of patients who did not experience chest pain relief than the group without recurrence. The difference was statistically significant (P < 0.05), as illustrated in Table 3.
Table 3
| Characteristics | Totality | Group I | Group II | P |
|---|---|---|---|---|
| Chest pain 36 h after surgery | <0.001 | |||
| Remission | 215 (66.4) | 39 (47.6) | 176 (72.7) | |
| Nonremission | 109 (33.6) | 43 (52.4) | 66 (27.3) | |
| In-hospital adverse events | 0.326 | |||
| Yes | 101 (31.2) | 22 (26.8) | 79 (32.6) | |
| No | 223 (68.8) | 60 (73.2) | 163 (67.4) | |
| Postoperative medication | ||||
| Double anti-plate | 324 (100) | 82 (100) | 242 (100) | — |
| Statins | 324 (100) | 82 (100) | 242 (100) | — |
| ACEI/ARB | 122 (37.7) | 34 (41.5) | 88 (36.4) | 0.431 |
| Beta blockers | 120 (37.0) | 28 (34.1) | 92 (38.0) | 0.597 |
| Nitrates | 155 (47.8) | 37 (45.1) | 118 (48.8) | 0.610 |
Postoperative condition and medication in both groups.
In-hospital adverse events: Including severe hypotension, acute heart failure, cardiac arrhythmia, shock, and infection of the puncture incision. ACEI/ARB: Angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists.
4.2. COX regression analysis
Based on follow-up results, whether angina recurred was taken as the dependent variable, and significant baseline data, as well as some clinical data with differences, were included as independent variables in the COX regression model. The univariate COX regression model indicated that patient anxiety, spouse illness, Killip classification, the number of coronary lesions, stent implants, intraoperative thrombolysis, revascularization method, and TIMI score were all related to recurrent angina. After testing, some variables, including the number of coronary lesions, stent implants, postoperative revascularization status, TIMI score, and TMBG score, demonstrated strong interactivity. To eliminate multicollinearity, some items were excluded, retaining those with less correlation with other research variables. Multivariate COX regression analysis showed that patient anxiety and spouse illness were both risk factors for recurrent angina after discharge. The HR (95% CI) were 1.641 (1.050–2.566) and 2.624 (1.618–4.255), respectively. Refer to Table 4.
Table 4
| Characteristics | Univariate | mnivariate | |||
|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | ||
| Sex | Female | Reference | Reference | ||
| Male | 0.812 (0.494–1.333) | 0.410 | 0.889 (0.526–1.503) | 0.661 | |
| Age | <65 | Reference | Reference | ||
| ≥65 | 1.263 (0.816–1.954) | 0.294 | 1.251 (0.801–1.953) | 0.325 | |
| BMI | ≤24 | Reference | Reference | ||
| >24 | 1.081 (0.698–1.675) | 0.727 | 0.885 (0.565–1.385) | 0.592 | |
| Spouse | Well | Reference | Reference | ||
| Unwell | 2.498 (1.582–3.945) | <0.001 | 2.624 (1.618–4.255) | <0.001 | |
| None | 2.247 (1.048–4.817) | 0.037 | 1.676 (0.753–3.732) | 0.206 | |
| Hypertension | No | Reference | — | ||
| Yes | 1.580 (0.959–3.372) | 0.075 | |||
| Diabetes | No | Reference | — | ||
| Yes | 1.401 (0.899–2.184) | 0.136 | |||
| Hyperlipemia | No | Reference | — | ||
| Yes | 1.120 (0.682–1.839) | 0.654 | |||
| Anxiety | No | Reference | Reference | ||
| Yes | 2.106 (1.361–3.258) | <0.001 | 1.641 (1.050–2.566) | 0.030 | |
| Ischemic time | 0–6 | Reference | – | ||
| 6–12 | 0.689 (0.370–1.282) | 0.240 | |||
| >12 | 0.540 (0.284–1.027) | 0.060 | |||
| Killip grading | 1 | Reference | Reference | ||
| 2 | 1.571 (0.875–2.821) | 0.130 | 1.612 (0.859–2.903) | 0.112 | |
| ≥3 | 6.134 (3.761–10.004) | <0.001 | 4.983 (2.965–8.377) | <0.001 | |
| Coronary lesions | 1 | Reference | – | ||
| 2 | 1.537 (0.934–2.529) | 0.091 | |||
| ≥3 | 4.356 (2.468–7.689) | <0.001 | |||
| Stents implantation | 1 | Reference | Reference | ||
| 2 | 1.099 (0.671–1.800) | 0.709 | 1.055 (0.635–1.755) | 0.835 | |
| ≥3 | 2.587 (1.339–4.998) | 0.005 | 1.432 (0.036–1.943) | 0.192 | |
| 0 | 0.256 (0.035–1.858) | 0.178 | 0.266 (0.682–1.839) | 0.308 | |
| Thrombolysis | No | Reference | Reference | ||
| Yes | 1.739 (1.128–2.683) | 0.012 | 1.429 (0.906–2.254) | 0.125 | |
| Revascularization mode | MCLCR | Reference | – | ||
| SCLCR | 1.737 (0.893–3.380) | 0.104 | |||
| MCLIR | 0.735 (0.368–1.467) | 0.383 | |||
| TIMI | 3 | Reference | – | ||
| 2 | 7.122 (2.216–22.889) | <0.001 | |||
| 1 | 2.170 (1.373–3.430) | <0.001 | |||
COX regression.
Ischemic time in hours. Coronary lesions: Number of coronary lesions. Stents implantation: Number of coronary stents implanted. Revascularization modalities include the following classifications: SCLCR means complete revascularization of a single vessel, MCLCR means complete revascularization of multiple vessels, MCLIR means incomplete revascularization of multiple vessels. Spouse means spouse's health, well means healthy spouse, unwell means unhealthy spouse, none means no spouse.
4.3. Propensity score matching (PSM) results
To eliminate the impact of endogeneity bias and explore the relationship between anxiety and post-discharge recurrent angina, this study used PSM to perform a 1:1 match between the two groups of patients. Matching was done between the anxiety and non-anxiety groups, primarily based on major baseline data and some clinical data with differences. Table 5 provides patient information before and after matching. As shown in Table 5, before matching, there were a total of 324 patients, with 93 having anxiety disorders and 231 without. After matching, the total number of patients was 162, with 81 each in the anxiety and non-anxiety groups. After matching, there were no significant differences in major baseline data and some pre-matching clinical data with differences between the two groups (P > 0.05).
Table 5
| Characteristics | Before PSM | After PSM | |||||
|---|---|---|---|---|---|---|---|
| Anxiety | Anxiety free | P | Anxiety | Anxiety free | P | ||
| Sex | Male | 69 (74.2) | 183 (79.2) | 0.376 | 62 (76.5) | 64 (79.0) | 0.850 |
| Female | 24 (25.8) | 48 (20.8) | 19 (23.5) | 17 (21.0) | |||
| Age | ≥65 | 51 (54.8) | 113 (48.9) | 0.390 | 44 (54.3) | 40 (49.4) | 0.637 |
| <65 | 42 (45.2) | 118 (51.1) | 37 (45.7) | 41 (50.6) | |||
| BMI | >24 | 50 (53.8.) | 129 (55.8) | 0.805 | 46 (56.8) | 48 (59.3) | 0.874 |
| ≤24 | 43 (46.2) | 102 (44.2) | 35 (43.2) | 33 (40.7) | |||
| Spouse | Well | 57 (61.3) | 151 (65.4) | 0.292 | 51 (63.0) | 52 (64.2) | 0.318 |
| Unwell | 32 (34.4) | 82 (26.8) | 28 (34.6) | 23 (28.4) | |||
| No | 4 (4.3) | 18 (7.8) | 2 (2.5) | 6 (7.4) | |||
| Hypertension | Yes | 53 (57.0) | 131 (56.7) | 0.963 | 47 (58.0) | 49 (60.5) | 0.873 |
| No | 40 (43.0) | 100 (43.3) | 34 (42.0) | 32 (39.5) | |||
| Diabetes | Yes | 34 (36.6) | 71 (30.7) | 0.359 | 28 (34.6) | 26 (32.1) | 0.868 |
| No | 59 (63.4) | 160 (69.3) | 53 (65.4) | 55 (67.9) | |||
| Hyperlipemia | Yes | 20 (78.5) | 57 (24.7) | 0.568 | 20 (24.7) | 18 (22.2) | 0.427 |
| No | 73 (21.5) | 174 (75.3) | 61 (75.3) | 63 (77.8) | |||
| Ischemic time | 0–6 | 60 (64.5) | 141 (61.0) | 0.415 | 51 (63.0) | 55 (67.9) | 0.823 |
| 6–12 | 18 (19.4) | 38 (16.5) | 16 (19.8) | 14 (17.3) | |||
| >12 | 15 (16.1) | 52 (22.5) | 14 (17.2) | 12 (14.8) | |||
| Killip grading | 1 | 56 (60.2) | 151 (65.4) | 0.104 | 55 (67.9) | 43 (53.1) | 0.142 |
| 2 | 18 (19.4) | 54 (23.4) | 14 (17.3) | 25 (28.4) | |||
| ≥3 | 19 (20.4) | 26 (11.3) | 12 (14.8) | 15 (18.5) | |||
| Coronary lesions | 1 | 40 (43.0) | 130 (56.3) | 0.035 | 40 (49.4) | 38 (46.9) | 0.595 |
| 2 | 38 (40.9) | 82 (35.5) | 31 (38.3) | 28 (34.6) | |||
| ≥3 | 15 (16.1) | 19 (8.2) | 10 (12.3) | 15 (18.5) | |||
| Stents implantation | 1 | 57 (61.3) | 137 (59.3) | 0.491 | 53 (65.4) | 49 (60.5) | 0.503 |
| 2 | 23 (24.7) | 70 (30.3) | 18 (22.2) | 25 (30.9) | |||
| ≥3 | 9 (9.7) | 13 (5.6) | 7 (8.6) | 6 (7.4) | |||
| 0 | 4 (4.3) | 11 (4.8) | 3 (3.7) | 1 (1.2) | |||
| Thrombolysis | Yes | 55 (59.1) | 153 (66.2) | 0.250 | 32 (39.5) | 32 (39.5) | 1.000 |
| No | 38 (40.9) | 78 (33.8) | 49 (60.5) | 49 (60.5) | |||
| Revascularization mode | SCLCR | 40 (43.0) | 130 (56.3) | 0.087 | 40 (49.4) | 38 (46.9) | 0.905 |
| MCLCR | 15 (40.9) | 32 (13.8) | 11 (13.6) | 10 (12.3) | |||
| MCLIR | 38 (16.1) | 69 (29.9) | 30 (37.0) | 33 (40.8) | |||
| TIMI | 1 | 2 (2.2) | 2 (0.9) | <0.001 | 0 (0) | 1 (1.2) | 0.596 |
| 2 | 34 (36.6) | 38 (16.5) | 24 (29.6) | 20 (24.7) | |||
| 3 | 57 (61.3) | 191 (82.7) | 57 (70.4) | 60 (74.1) | |||
Propensity score matching (PSM).
Ischemic time in hours. Coronary lesions: Number of coronary lesions. Stents implantation: Number of coronary stents implanted. Revascularization modalities include the following classifications: SCLCR means complete revascularization of a single vessel, MCLCR means complete revascularization of multiple vessels, MCLIR means incomplete revascularization of multiple vessels. Spouse means spouse's health, well means healthy spouse, unwell means unhealthy spouse, none means no spouse.
4.4. COX regression analysis after PSM matching
Multivariable regression analysis post-propensity score matching showed that spouse illness, anxiety, and Killip ≥3 were all related to recurrent angina. The effect of anxiety was particularly significant (HR = 2.094, 95% CI = 1.248–3.514, P = 0.005), consistent with the pre-matching results. See Table 6 for details.
Table 6
| Characteristics | N | HR (95% CI) | P | |
|---|---|---|---|---|
| Sex | Female | 36 | Reference | |
| Male | 126 | 0.786 (0.421–1.465) | 0.448 | |
| Age | <65 | 78 | Reference | |
| ≥65 | 84 | 1.245 (0.753–2.059) | 0.393 | |
| BMI | ≤24 | 68 | Reference | |
| >24 | 94 | 1.307 (0.771–2.218) | 0.32 | |
| Spouse | Well | 103 | Reference | |
| Unwell | 51 | 3.148 (1.846–5.367) | <0.001 | |
| None | 8 | 3.042 (1.120–8.261) | 0.029 | |
| Anxiety | No | 81 | Reference | |
| Yes | 81 | 2.094 (1.248–3.514) | 0.005 | |
| Killp rating | 1 | 98 | Reference | |
| 2 | 37 | 0.995 (0.513–1.932) | 0.989 | |
| ≥3 | 27 | 2.981 (1.681–5.284) | <0.001 | |
| Coronary lesions | 1 | 78 | Reference | |
| 2 | 59 | 0.792 (0.446–1.407) | 0.427 | |
| ≥3 | 25 | 0.999 (0.502–1.985) | 0.997 | |
| Thrombolysis | No | 98 | Reference | |
| Yes | 64 | 1.613 (0.976–2.667) | 0.062 | |
| TIMI | 3 | 117 | Reference | |
| 2 | 45 | 1.193 (0.703–2.025) | 0.514 | |
Multifactor COX regression after PSM.
Spouse means spouse's health, well means healthy spouse, unwell means unhealthy spouse, none means no spouse. Coronary lesions: Number of coronary lesions. Stents implantation: Number of coronary stents implanted.
4.5. Subgroup analysis
Comparing baseline data between the two groups, we found a statistically significant difference in postoperative 36-hour chest pain relief among discharged patients (see Table 3). To evaluate whether the lack of short-term postoperative chest pain relief and recurrent chest pain after discharge were related to patient anxiety, we divided the patients matched by PSM into two groups based on whether they experienced chest pain relief within 36 h post-surgery: the chest pain relief group (n = 88) and the no chest pain relief group (n = 74). Subgroup analysis results indicated that anxiety was associated with post-discharge recurrent angina at both the 36-hour post-surgery chest pain relief (HR = 2.810, 95% CI = 1.205–6.552, P = 0.017) and the 36-hour post-surgery no chest pain relief (HR = 1.988, 95% CI = 1.074–3.679, P = 0.029) levels. Details are in Table 7 and Figure 2.
Table 7
| Characteristics | Anxiety | N | HR (95% CI) | P |
|---|---|---|---|---|
| 36 h angina relief | No | 51 | Reference | |
| Yes | 37 | 2.810 (1.205–6.552) | 0.017 | |
| Angina is not relieved in 36 h | No | 30 | Reference | |
| Yes | 44 | 1.988 (1.074–3.679) | 0.029 | |
| Totality | No | 81 | Reference | |
| Yes | 81 | 2.232 (1.344–3.706) | 0.002 |
Subgroup analysis of whether chest pain was relieved at 36 h postoperatively.
Figure 2
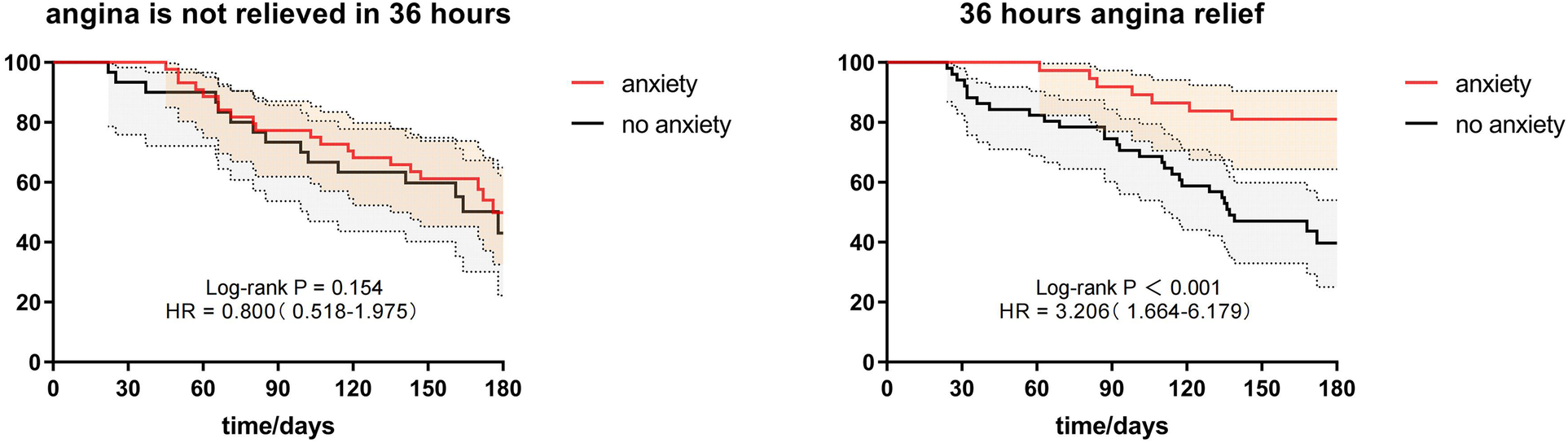
Subgroup analysis of whether chest pain was relieved at 36 h postoperatively.
To explore whether differences in the health status of a patient's spouse might influence recurrent angina and if it is related to patient anxiety, we divided the patients based on their spouse's health status into three groups: spouse healthy, spouse ill, and no spouse. Due to sample size limitations, the no-spouse group, which had a smaller number of patients after PSM matching, was excluded from the discussion. Subgroup analysis suggested that for patients in the spouse healthy group, anxiety might be a factor for recurrent angina within 6 months post-discharge (HR = 2.129, 95% CI = 1.26–4.418, P = 0.042). The recurrence of angina in patients in the spouse ill group was not related to patient anxiety (P > 0.05). Details are in Table 8 and Figure 3.
Table 8
| Characteristics | Anxiety | N | HR (95% CI) | P |
|---|---|---|---|---|
| Spouse well | No | 52 | Reference | |
| Yes | 51 | 2.129 (1.26–4.418) | 0.042 | |
| Spousal illness | No | 23 | Reference | |
| Yes | 28 | 1.638 (0.822–3.264) | 0.160 | |
| Mateless | No | 6 | Reference | |
| Yes | 2 | —— | 0.249 | |
| Totality | No | 81 | Reference | |
| Yes | 81 | 2.055 (1.265–3.341) | 0.004 |
Subgroup analysis of spousal health status.
Figure 3
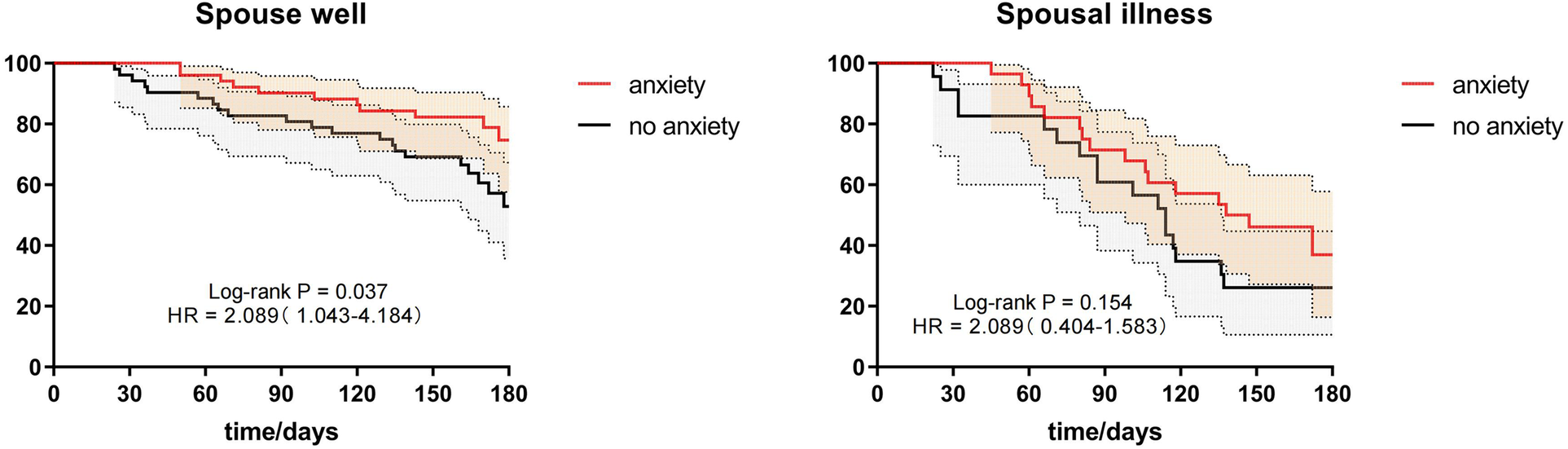
Subgroup analysis of spousal health status.
To study whether the severity of a patient's condition leading to recurrent angina post-discharge was related to anxiety, subgroup analysis was conducted based on the Killip classification to examine whether recurrent angina in patients with different Killip classifications was associated with anxiety. The results showed that, at different Killip classification levels, the recurrence of angina within 6 months post-STEMI PCI was not related to whether the patient was anxious. Refer to Table 9 and Figure 4.
Table 9
| Characteristics | Anxiety | N | HR (95% CI) | P |
|---|---|---|---|---|
| Killp I | No | 43 | Reference | |
| Yes | 55 | 1.590 (0.794–3.184) | 0.191 | |
| Killp II | No | 23 | Reference | |
| Yes | 14 | 4.155 (0.926–18.642) | 0.063 | |
| Killp III | No | 15 | Reference | |
| Yes | 12 | 2.087 (0.949–4.589) | 0.067 | |
| Totality | No | 81 | Reference | |
| Yes | 81 | 1.912 (1.172–3.118) | 0.009 |
Subgroups analysis of different killip grading subgroups.
Figure 4
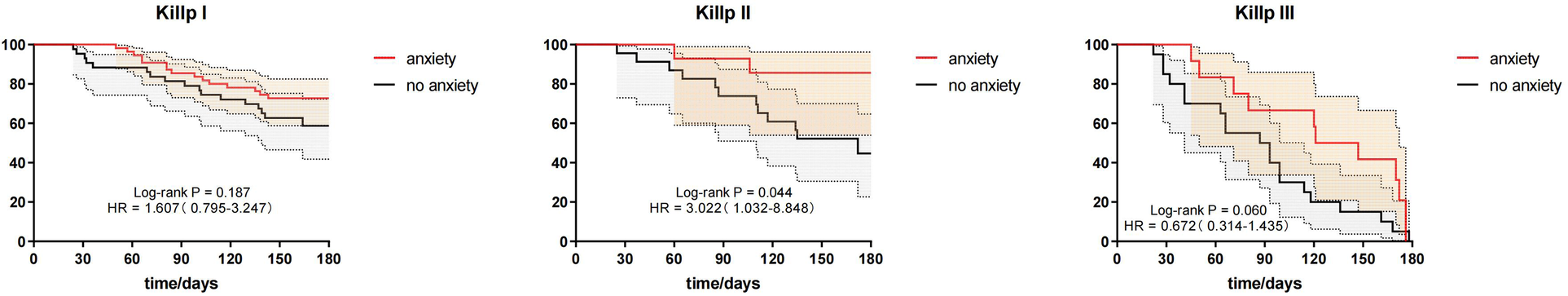
Subgroups analysis of different killip grading subgroups.
5. Discussion
Cardiovascular diseases have consistently been the leading cause of human mortality, with Acute Myocardial Infarction (AMI) being among the most severe types. ST-segment elevation myocardial infarction (STEMI) is the most common type of AMI. The fastest and most effective clinical treatment for STEMI is Percutaneous Coronary Intervention (PCI). However, post-PCI angina recurrence poses a challenge to both STEMI patients and clinicians due to its complex etiology and the sheer number of affected individuals. Despite advancements in medical treatment, many patients can't effectively control its recurrence even with regular medication (15). In this study, we primarily investigated the risk factors of angina recurrence after PCI in STEMI patients and explored the impact of anxiety on post-discharge angina recurrence. Since all participants in this study had undergone PCI following STEMI, no significant differences in baseline data were identified. Factors influencing angina recurrence after discharge mainly included anxiety levels, spouse's health status, and differences in surgical data. To better understand the impact of anxiety on angina recurrence, we treated patient anxiety as an independent variable and angina recurrence as the dependent variable, applying Propensity Score Matching (PSM) to match baseline data and significantly different surgical data to reduce bias. Multivariate COX regression analysis before matching showed that patient anxiety status, spouse's illness, and a Killip classification of ≥3 were factors for post-PCI angina recurrence. Post-matching COX regression results supported these findings. Before including surgical data as control variables in the COX regression model, we conducted an interaction test on some surgical data. Strong multicollinearity was found among variables like TIMI grade, vascular reconstruction methods, the number of coronary lesions, and the number of stents implanted. To ensure the accuracy of the regression model results, we excluded some variables, retaining those with minimal interaction with other variables. During the research, we found that pain relief within 36 h post-surgery was significantly different at the time of discharge. To determine if this was related to the patient's anxiety status, we grouped by pain relief within 36 h post-PCI and carried out a subgroup analysis. The results showed that anxiety was related to post-discharge angina recurrence regardless of pain relief status within 36 h after surgery. Subsequent subgroup analyses based on the COX regression results suggest that among patients with healthy spouses, post-discharge angina recurrence was related to the patient's anxiety status. Contrary to subjective feelings, angina occurrence after discharge in patients with sick spouses and those with various Killip classifications was not related to anxiety. This result might be due to insufficient sample size, but combined with COX regression results, it still reflects that the sickness status of the patient's spouse and a higher Killip classification are independent risk factors for post-discharge angina recurrence after PCI.
The negative impact of anxiety disorders on the cardiovascular system has already been discussed in our literature review. Besides increasing the activity of the sympathetic nervous system, leading to faster heart rates, inducing arrhythmias, elevating blood pressure, causing damage to blood vessel walls, and accelerating the process of arteriosclerosis, anxiety is also linked to poor health behaviors such as smoking, excessive drinking, reduced physical activity, and unhealthy diets. All these increase the risk of cardiovascular diseases (16). The theoretical basis of this study is grounded in the belief that anxiety has detrimental effects on the cardiovascular system. However, existing theories also suggest that having a cardiovascular disease can induce anxiety in patients (17, 18). Given that AMI is one of the most severe cardiovascular diseases, patients inevitably develop fears about mortality and further heart attacks post-diagnosis. Considering the reduced physical capabilities post-surgery and the long-term medications, the financial burden on the family increases. Preventing another heart attack might also require changes to existing lifestyles, possibly limiting social interactions. All these factors could induce anxiety. It's evident that anxiety and cardiovascular diseases have a mutually reinforcing relationship. This mutual impact is unfavorable for clinicians and needs mitigation. By deeply exploring this issue, we hope to see more similar studies providing more precise risk assessment and management strategies, thereby further optimizing the treatment and rehabilitation of STEMI patients.
There are some limitations to our study. Firstly, the insufficient sample size can lead to inadequate test power, increasing the risk of Type II errors. Secondly, gauging emotional status changes post-discharge is challenging. The risk of anxiety disorders may increase after a STEMI episode, and some patients may develop new anxiety symptoms post-discharge, which might be overlooked during the in-hospital Hamilton Anxiety Rating Scale assessment. To address these challenges, more prospective studies with larger sample sizes are needed.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Second People’s Hospital of Hefei. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because this is a retrospective study. As our study was based on the relevant clinical data obtained from the hospital’s previous medical records, all the questionnaire results were routinely investigated by the nursing department of our hospital on the understanding of the condition of the admitted patients, and the follow-up content was the postoperative health follow-up of the discharged patients. Researchers authorized by the Ethics Committee of Hefei Second People’s Hospital are not required to obtain written consent from patients.
Author contributions
ZZ: Conceptualization, Data curation, Formal Analysis, Investigation, Software, Validation, Visualization, Writing – original draft. XW: Data curation, Investigation, Writing – original draft. JW: Data curation, Investigation, Writing – original draft. YW: Data curation, Investigation, Writing – original draft. CL: Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We wish to show our gratitude to all those who were involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
llrich H Olschewski M Münzel T Gori T . Coronary in-stent restenosis: predictors and treatment. Dtsch Arztebl Int. (2021) 118(38):637–44. 10.3238/arztebl.m2021.0254
2.
Radley C Berry C . Definition and epidemiology of coronary microvascular disease. J Nucl Cardiol. (2022) 29(4):1763–75. 10.1007/s12350-022-02974-x
3.
l-Lamee RK Nowbar AN Francis DP . Percutaneous coronary intervention for stable coronary artery disease. Heart. (2019) 105(1):11–9. 10.1136/heartjnl-2017-312755
4.
De Luca L Rosano GMC Spoletini I . Post-percutaneous coronary intervention angina: from physiopathological mechanisms to individualized treatment. Cardiol J. (2022) 29(5):850–7. 10.5603/CJ.a2021.0042
5.
En-Yehuda O Kazi DS Bonafede M Wade SW Machacz SF Stephens LA et al Angina and associated healthcare costs following percutaneous coronary intervention: a real-world analysis from a multi-payer database. Catheter Cardiovasc Interv. (2016) 88(7):1017–24. 10.1002/ccd.26365
6.
Iwaszczuk P Łosiak W Szczeklik W Musiałek P . Patient periprocedural stress in cardiovascular medicine: friend or foe?Adv Interv Cardiol. (2021) 17(3):259–71. 10.5114/aic.2021.109176
7.
Alkstedt D Lundberg I Hemmingsson T . Childhood socio-economic position and risk of coronary heart disease in middle age: a study of 49,321 male conscripts. Eur J Public Health. (2011) 21(6):713–8. 10.1093/eurpub/ckq158
8.
I B Ding X . Observation and analysis of 126 cases of coronary heart disease unstable angina pectoris complicated with anxiety. Medical Food Therapy and Health. (2020) 18(20):62–5.
9.
Brouwers RW Kraal JJ Traa SC . Effects of cardiac telerehabilitation in patients with coronary artery disease using a personalised patient-centred web application: protocol for the SmartCare-CAD randomised controlled trial. BMC Cardiovasc Disord. (2017) 17(1):46. 10.1186/s12872-017-0477-6
10.
Zhang S Zhong Y Wang L . STEP Study Group. Anxiety, home blood pressure monitoring, and cardiovascularevents among older hypertension patients during the COVID-19 pandemic. Hypertens Res. (2022) 45(5):856–65. 10.1038/s41440-022-00852-0
11.
Chialà O Vellone E Klompstra L Jaarsma T . Relationships between exercise capacity and anxiety, depression, and cognition in patients with heart failure. Heart Lung. (2018) 47(5):465–70. 10.1016/j.hrtlng.2018.07.010
12.
Torabizadeh C Rousta S Parvizi MM . Efficacy of education delivery through multimedia and text messaging on the psychological parameters of patients scheduled for coronary angiography: a single-blind randomized controlled clinical trial. BMC Cardiovasc Disord. (2021) 21(1):3. 10.1186/s12872-020-01820-7
13.
Thomas M Jones PG Arnold SV Spertus JA . Interpretation of the Seattle angina questionnaire as an outcome measure in clinical trials and clinical care: a review. JAMA Cardiol. (2021) 6(5):593–9. 10.1001/jamacardio.2020.7478
14.
Zhu C Zhang Y Wang T Zhu DM . Vitamin D supplementation improves anxiety but not depression symptoms in patients with vitamin D deficiency. Brain Behav. (2020) 10(11):e01760. 10.1002/brb3.1760
15.
Peterson BE Bhatt DL Steg PG Ballantyne CM . REDUCE-IT Investigators. Treatment with icosapent ethyl to reduce ischemic events in patients with prior percutaneous coronary intervention: insights from REDUCE-IT PCI. J Am Heart Assoc. (2022) 11(6):e022937. 10.1161/JAHA.121.022937
16.
Broers ER Gavidia G Wetzels M Ribas V Ayoola I Piera-Jimenez J et al Usefulness of a lifestyle intervention in patients with cardiovascular disease. Am J Cardiol. (2020) 125(3):370–5. 10.1016/j.amjcard.2019.10.041
17.
Wen Y Yang Y Shen J Luo S . Anxiety and prognosis of patients with myocardial infarction: a meta-analysis. Clin Cardiol. (2021) 44(6):761–70. 10.1002/clc.23605
18.
Zhou S J Zhang J . Research progress on the relationship between anxiety and depression and its evaluation and cardiovascular diseases. Journal of Cardiovascular Rehabilitation Medicine. (2021) 30(3):335–40. 10.3969/j.issn.1008-0074.2021.03.22
Summary
Keywords
anxiety, STEMI, percutaneous coronary intervention, angina, follow-up
Citation
Zhang Z, Wei X, Wei J, Wang Y and Luo C (2023) Does anxiety cause angina recurrence after percutaneous coronary intervention in patients with STEMI?. Front. Cardiovasc. Med. 10:1283182. doi: 10.3389/fcvm.2023.1283182
Received
28 August 2023
Accepted
16 October 2023
Published
31 October 2023
Volume
10 - 2023
Edited by
Artur Dziewierz, Jagiellonian University Medical College, Poland
Reviewed by
Zbigniew Siudak, Jan Kochanowski University, Poland Łukasz Niewiara, Jagiellonian University Medical College, Poland
Updates
Copyright
© 2023 Zhang, Wei, Wei, Wang and Luo.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Chunmiao Luo 18949874332@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.