- 1Hebei Key Laboratory of Clinical Pharmacy, Department of Cardiology, Hebei General Hospital, Shijiazhuang, Hebei, China
- 2Department of Cardiology, The Second People's Hospital of Hengshui, Hengshui, Hebei, China
- 3Department of Cardiology, Affiliated Hospital of Hebei University of Engineering, Handan, Hebei, China
- 4Nursing Department, BAO DING NO1 General Hospital Baoding, Hebei, China
Aim: This study aimed to evaluate the benefit of a home-based cardiac rehabilitation (CR) programme with telemonitoring guidance on kinesiophobia in patients with percutaneous coronary intervention (PCI) discharged from hospital. It also aimed to explore the effectiveness of this programme on self-efficacy and cardiorespiratory endurance using a randomised controlled trial.
Design: This study was a single-blind, prospective randomised controlled trial.
Methods: Patients who underwent PCI at our hospital were enrolled. The intervention group (IG) performed WeChat-based brisk walking and the control group (CG) received the usual care, including advice to remain physically active. All patients underwent cardiopulmonary exercise testing to assess their peak oxygen uptake (peak VO2) at baseline and after a 12-week intervention period. The main outcome indicator was kinesiophobia. Secondary outcomes included exercise self-efficacy, cardiorespiratory endurance (i.e., peak VO2), and major adverse cardiovascular events.
Results: A total of 137 patients were enrolled in this study between 1 February 2023 and 31 October 2023. Of them, 130 patients successfully completed a 12-week WeChat-based brisk walking CR programme. After 12 weeks of intervention, the Tampa Scale for Kinesiophobia Heart scores in the IG decreased significantly more than in the CG and pre-IG. The IG's Self-Efficacy for Exercise scores were higher than those of the CG and pre-IG. In addition, the increase in peak VO2 was larger in the IG than in the CG.
Conclusion: The WeChat-based brisk walking programme is beneficial for reducing kinesiophobia by increasing exercise self-efficacy in patients after PCI; it also helps to improve cardiopulmonary endurance. WeChat-based brisk walking is feasible and acceptable.
1 Introduction
Coronary heart disease (CHD) is the most prevalent cardiovascular disease. It is a common condition and is the leading cause of mortality and disability in adults (1). This burden disproportionately affects low- and middle-income countries, contributing to approximately 7 million deaths and 129 million disability-adjusted life years annually (2). The primary medical treatment for CHD is percutaneous coronary intervention (PCI) (3), with 10,142,266 patient cases reported in China in 2021 (4, 5). Cardiac rehabilitation (CR) (6) is an important therapeutic principle for secondary prevention in patients with CHD, which reduces all-cause mortality caused by various coronary events (7–9). Cardiac rehabilitation reduces hospitalisations and increases the quality of life in PCI (10). In addition, exercise-based CR can improve physical capacity and peak oxygen consumption in patients with CHD (11). However, studies show that <20% of patients participate in CR, and the compliance is low. Kinesiophobia is an important obstacle to taking part in CR and one of the main reasons for those who fail to carry on exercising.
Regular physical activity plays a significant role in reducing mortality rates among patients with CHD. For patients who undergo postoperative PCI, non-compliance with exercise therapy after discharge increases the likelihood of a poor prognosis and readmission. Several national and international clinical guidelines recommend that post-PCI patients participate in exercise rehabilitation to improve functional status, exercise capacity, and quality of life.
Kinesiophobia was first identified by Kori, and it was mostly applied to research on agoraphobia in people with chronic pain. Reports on the incidence of kinesiophobia in patients with CHD are in the range of 20%–70% at home and abroad. A Chinese cross-sectional study (12) showed that 41.76% of 376 patients with CHD experienced kinesiophobia. According to a Polish study (13), >70% of people with CHD experience kinesiophobia. Kinesiophobia affects 45% of individuals with CR and dramatically lowers the rate of CR visits (14). In CR, the identification and treatment of kinesiophobia should be a top priority, in addition to boosting exercise self-efficacy.
An early measurement tool developed to assess kinesiophobia is the Tampa Scale of Kinesiophobia (TSK) (15, 16). In 2012, Bäck et al. developed a specific scale suitable for assessing the level of kinesiophobia in patients with CHD based on the original TSK scale, known as the Tampa Scale for Kinesiophobia Heart (TSK-SV Heart) (17). In recent years, Chinese scholar Lei and his colleagues translated it into Chinese and validated it in CHD. The Chinese version of the TSK-SV Heart scale has strong reliability and validity, with a split-half reliability of 0.792 and a Cronbach's alpha coefficient of 0.859, and has been popularised in the study of kinesiophobia (18). A cross-sectional study conducted by Ding utilised the TSK-SV Heart to investigate kinesiophobia in 400 patients with heart disease and achieved more significant results (19). Knapik et al. created the Kinesiophobia Causes Scale (KCS) to examine the root causes of passive movement in adults, highlighting that kinesiophobia arises because of a mix of physiological and psychological variables. In 2020, Zhu et al. (20) “Chinese-ised” it and tested its reliability in patients with chronic low back pain, proving that the scale can be used as a valid tool for evaluating the causes of kinesiophobia in China. However, the KCS scale has not yet been validated in patients with heart disease. Therefore, the Chinese version of the TSK-SV Heart scale is selected in the current study to measure the severity of kinesiophobia in post-PCI patients.
Kinesiophobia can be effectively treated in patients with low back pain by a technique called “graded exposure,” which refers to a gradual acceptance of exercise to gradually remove fear (21). The idea of graded exercise has been partially used in exercise-based CR programmes in patients with cardiac infarction (22). According to most guidelines, a regular exercise rehabilitation workout is necessary for patients after PCI. A psychological and behavioural intervention technique, known as cognitive behavioural intervention, is inspired by cognitive behavioural theory. Interventions guided by this theory include assessment of kinesiophobia, education on kinesiophobia, progressive training, and staged rehabilitation. However, these interventions may not be appropriate for patients in phase II of CR (which is typically carried out within 1–6 months of hospital discharge, when patients are at home). With the application of telemedicine, research has found that home-based CR has the same cardiovascular benefits as CR in hospital (23), which can be used as a prominent supplement or alternative. Nurse-led home-based rehabilitation, which improves adherence to rehabilitation, is supposed to help the patients overcome their fears with professional support (24). Furthermore, it has low intervention costs and addresses the fact that most patients do not go to hospital because of time and financial reasons.
Brisk walking is the simplest and most controlled form of CR recommended by national and international guidelines (25, 26). WeChat-based brisk walking refers to the use of a social networking platform by medical experts to direct participants in their continuous rehabilitation to boost their exercise self-efficacy, reduce kinesiophobia, and improve illness prognosis. Research (27) has shown that multidisciplinary or exercise-based cardiac telerehabilitation is a safe and cost-effective alternative to centre-based CR in patients with CHD or chronic heart failure.
Network-based brisk walking has the following advantages. First, professional guidance from medical staff provides authority and safety. Moreover, the simplicity of brisk walking is expected to encourage participation and patient compliance. Finally, and importantly, WeChat is the most popular social software in China and its use is widespread. The current study has three aims: first, to investigate whether a WeChat-based intervention could alleviate kinesiophobia; second, to establish whether the path of alleviation is through improving patients’ exercise self-efficacy; and third, to test whether professionally guided brisk walking could help patients’ cardiorespiratory endurance after PCI.
2 The study
2.1 Participants
This study involved a single-blind, prospective, randomised controlled trial. Initially, 137 patients who underwent PCI in our hospital between 1 February 2023 and 31 October 2023 were enrolled (Figure 1). They were divided into an intervention group (IG) and a control group (CG) using the random number table method.
2.1.1 Inclusion criteria
The inclusion criteria were as follows: (1) participants followed the Chinese Guidelines for Percutaneous Coronary Intervention (28) and received elective PCI for the first time (29); (2) patients were aged 30–75 years; (3) patients had at least one stent implanted postoperatively with postoperative residual stenosis of 30% (30); and (4) patients (or their primary caregivers) used a smartphone.
2.1.2 Exclusion criteria
The exclusion criteria were as follows: (1) individuals who had >3 vascular lesions in the coronary arteries; (2) individuals with different causes of limb movement abnormalities; or (3) individuals who were currently enrolled in another study.
2.1.3 Shedding standards
Patients were removed from the study if they (1) had a health condition that made it hard to continue exercising or (2) withdrew for personal reasons.
A total of 137 patients who met the inclusion criteria between 1 February 2023 and 31 October 2023 were included in the study. The sample size is usually calculated based on 5–10 times the number of survey questionnaire items; therefore, the sample size required for this study was 105–170. A total of 130 patients successfully completed a 12-week WeChat-based brisk walking CR programme. There were no statistically significant differences between the two groups of patients with regard to general information (p > 0.05).
2.2 Method
The home-based rehabilitation team consisted of a chief nurse, a CR physician, a CR therapist, three CR specialist nurses, and two research assistants. All team members had a bachelor's degree or higher, ≥5 years of cardiology healthcare experience, and ≥3 years of CR expertise.
The chief nurse was the team leader and was responsible for team management, coordination, and quality control. The CR physician was responsible for screening patients into groups, formulating exercise prescriptions, and dynamically assessing changes in participants’ conditions. The therapist was responsible for implementing training prescriptions and guiding participants to walk remotely using the Internet. The CR nurse expert was in charge of creating a WeChat group, interacting with participants, scheduling follow-up visits, and constantly documenting the rehabilitation state. The research assistant was responsible for collecting and organising data. All team members underwent rigorous and uniform training before the study.
2.2.1 The intervention group
2.2.1.1 Pre-discharge rehabilitation guidance
Before discharge, the participants’ heart function was assessed using a cardiopulmonary exercise test (CPET) and non-invasive cardiac output. They were then given the TSK-SV Heart scale, Self-Efficacy for Exercise (SEE) scale, and general information questionnaire to complete. After that, the CR physician explained in detail the essentials and precautions for brisk walking, and the CR nurse established a WeChat group and showed them how to utilise the exercise training record sheets. Then, the participants were given the exercise training record sheets and were shown how to record and upload images to the WeChat group with specific information, including resting heart rate, blood pressure, maximum heart rate during exercise, exercise time, and blood pressure monitoring after exercise. Participants’ self-exercise logbooks and telecommunication through WeChat were used to track and maintain their engagement with the exercise programme.
2.2.1.2 Home-based rehabilitation guidance
All IG participants joined the WeChat group, which was hosted by a CR nurse. First, the CR nurse consistently posted the five main CR prescriptions, namely, assistance with exercise, medicine, food, psychological counselling, and quitting smoking. Second, brisk walking was scheduled together with participants. The brisk-walking-at-moderate-intensity training sessions each lasted 30 min and were conducted 3 days a week for the first 4 weeks. Subsequently, exercise intensity was adjusted by increasing the frequency of brisk walking to 5 days a week for the next 8 weeks. Participants followed the CR physician’s walking instructions. For those who had low compliance, the CR nurse would instruct and supervise them via WeChat. Participants uploaded the exercise training record as required. Participants could use a heart rate monitoring application named Physical Examination Treasure (Beijing Aikangkang Jianbao Health Technology Co., Ltd, Beijing, China) on their smartphones to track their heart rate while exercising and upload the information in the WeChat group. The participants measured their blood pressure using calibrated electronic blood pressure monitors (OMRON Corporation, Kyoto City, Japan) provided by the research team (all electronic blood pressure monitors were of the same brand and calibrated before use). Timely feedback and guidance from the team were offered in the WeChat group.
2.2.2 The control group
Participants in the CG completed the CPET, the general information questionnaire, the TSK-Heart test, and the SEE test on the day of discharge. The CR physician assessed the participant's condition based on the test results. A personalised exercise plan was prescribed, and the importance of adherence was emphasised (see Figure 2, intervention framework diagram).
2.2.3 Evaluation
After 12 weeks of intervention, participants returned to the CR centre and the research assistant performed the data collection. Four patients in the CG and three in the IG dropped out for various reasons, leaving 130 patients (65 in the CG and 65 in the IG). No adverse cardiac events were reported during the intervention period.
2.3 Evaluation means
2.3.1 Tampa Scale for Kinesiophobia Heart
The TSK-SV Heart is a specialised scale designed to assess kinesiophobia in patients with CHD. It has four dimensions and 17 items: perception of danger (four items), avoidance of movement (four items), fear of movement (five items), and dysfunction (four items). The items were rated on a 4-point Likert scale in the range of 1–4, with items 4, 8, 12, and 16 having reversed scores, going from “strongly disagree” to “strongly agree.” A high degree of kinesiophobia is indicated by a score of ≥37. This study used a translated Chinese version of the scale, with an overall Cronbach's alpha coefficient of 0.859, a split-half reliability of 0.792, and test–retest reliability of 0.792, demonstrating good reliability and validity (31).
2.3.2 Self-Efficacy for Exercise scale
The SEE scale, developed by Resnick and Jenkins, was used to quantify and reflect participants’ self-evaluation of exercise capacity. The study used the Chinese version, which had nine items and was translated and “Chinese-ised” by Lee et al. (32). A 10-point Likert scale was applied, with a maximum score of 90 points and a range of “no confidence” to “very confident.” The higher the score, the higher the patient's confidence in overcoming obstacles and maintaining a regular exercise regimen. A strong sense of self-efficacy was defined as having a SEE score of ≥50. The scale has a content validity of 0.90 and a Cronbach's alpha of 0.75.
2.3.3 Cardiopulmonary exercise testing and peak oxygen uptake
As an objective evaluation of cardiac function, CPET is frequently used to guide exercise rehabilitation, predict prognosis, and assess rehabilitation outcomes. It can also serve as a foundation for creating exercise prescriptions (33). Peak VO2 (the peak kilogram oxygen uptake) is the gold standard for assessing aerobic exercise capacity and predicting prognosis because it shows the cardiac output and reserve function of the heart (34). Peak VO2 was the primary CPET indicator used in this study: higher scores denote stronger cardiovascular endurance and reserve function in the patients. Before the test, a MasterScreen CPX device (Jaegar, Bavaria, Germany) was used to measure the participants’ height and weight while they were wearing sportswear and barefoot. Then, participants were seated on a power bicycle with a no-load warm-up for 3 min, and the exercise load was incremented during the test. The CR physician instructed the participants to maintain a bicycle speed of 60–70 rpm until they were exhausted. The test was stopped right away if participants experienced dyspnoea, chest pain, or any other uncomfortable symptoms.
2.4 Patient and public involvement
Patients are the main consideration in trial design, subject recruiting, and data exchange and were prioritised as far as possible. A patient involvement group was established at the outset of the study. During the meeting, the patient–public involvement group was informed about how the study would be conducted. Ample time was spent communicating with patients about constructing the intervention programme. After that, a pre-trial was conducted by randomly selecting several patients to gather their opinions and feelings. The research findings will be shared with participants and the public through various channels, including hospital social media accounts and academic lectures.
2.5 Statistical analysis
The SPSS 26.0 statistical software package was used for statistical analyses of the data. All data were expressed as mean ± SD or median or percentages (for categorical variables). The Shapiro–Wilk test was used to assess normality. At baseline, the groups were compared using the independent two-sample t-test or chi-square test. To compare groups in the follow-up data, the dependent two-sample t-test was employed. The matched samples t-test was used for within-group comparisons, provided normality was met. If not, the Mann–Whitney U-test was used. An intention-to-treat analysis was performed on the primary outcome (kinesiophobia). Pearson correlation coefficients (P) were calculated between kinesiophobia and exercise self-efficacy at 12 weeks. A probability level of p ≤ 0.05 was considered significant.
3 Results
3.1 General information
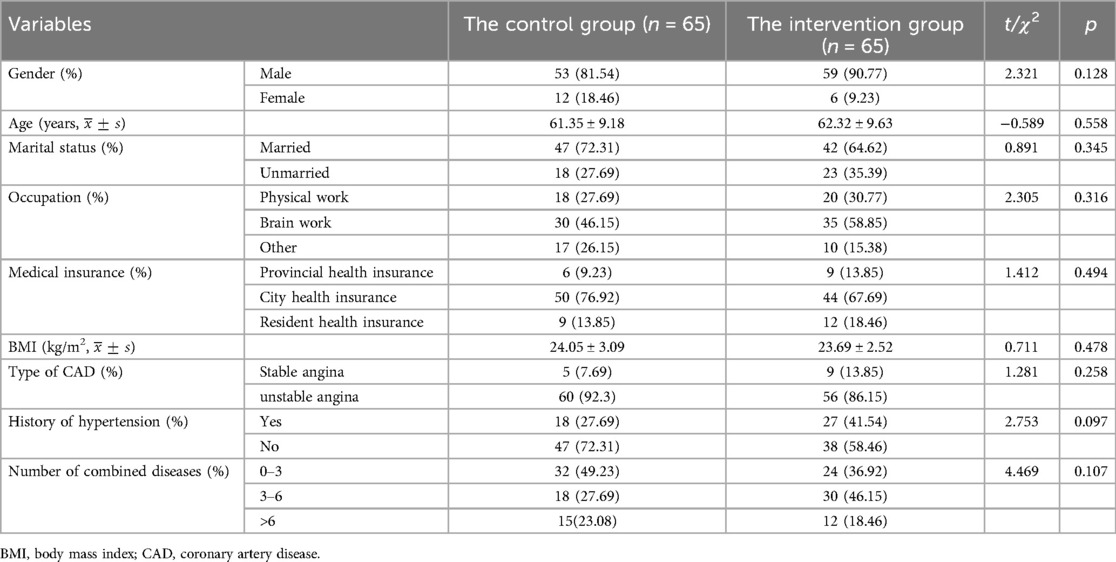
Table 1 shows that there were no significant changes (p > 0.05) in any of the following variables between the two groups: gender, age, marital status, occupation, body mass index (BMI), health insurance type, history of coronary hypertension, or co-morbidity. Most of the patients in the population were aged >60 years (mean age 61.42 ± 0.78 years), with unstable angina as their primary ailment (116/130, 89.23%). They had higher body mass indices (mean BMI 23.57 ± 2.80 kg/m2) and worked in the brain sciences (65/130, 50.0%). Baseline characteristics were comparable between the groups.
3.2 The Tampa Scale for Kinesiophobia Heart score and Self-Efficacy for Exercise score before and after the intervention
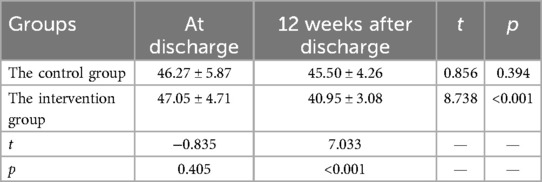
The results showed that the two groups of TSK-SV Heart scores did not differ significantly before the intervention (t = −0.835, p > 0.05). However, after 12 weeks of intervention, the TSK-SV cardiac function scores in both groups decreased, and the intervention group scored lower than the CG, with a large difference (t = 7.033, p < 0.001) (Table 2).
The results showed no significant change in SEE scores in both groups before the intervention (t = −1.337, p > 0.05). There was no significant change in SEE score before and after intervention in the control group. After 12 weeks of intervention, the mean SEE score (43.77 ± 4.62) was significantly higher than the mean score before the intervention (36.95 ± 5.13; t = −7.964, p < 0.001). The SEE score of the intervention group was higher than that of the control group after 12 weeks of intervention. (t = −9.186, p < 0.001) (Table 3).
There was no significant correlation of change in SEE with change in TSK-SV Heart (Pearson P = −0.007, p = 0.934). However, a significant correlation of SEE with TSK-SV Heart (P = −0.449, p < 0.001) at 12 weeks was found.
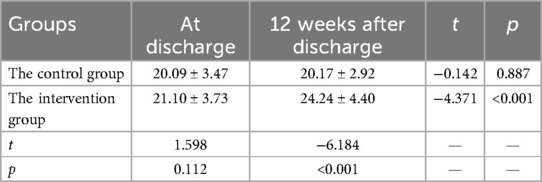
The results showed no difference between the two groups before the intervention (t = 1.598, p = 0.112). In the intervention group, after 12 weeks of intervention, the mean peak VO2 (24.24 ± 4.43) was significantly higher than that before the intervention (21.10 ± 3.73; t = −4.371, p < 0.001). The peak VO2 of the IG was higher than that of the CG after 12 weeks of intervention (t = −6.184, p < 0.001) (Table 4).
3.3 Report on the test safety
The fact that no adverse cardiovascular events happened throughout the entire intervention indicates that the trial was safe. To protect the participants’ safety, a very thorough adverse event protocol was created.
4 Discussion
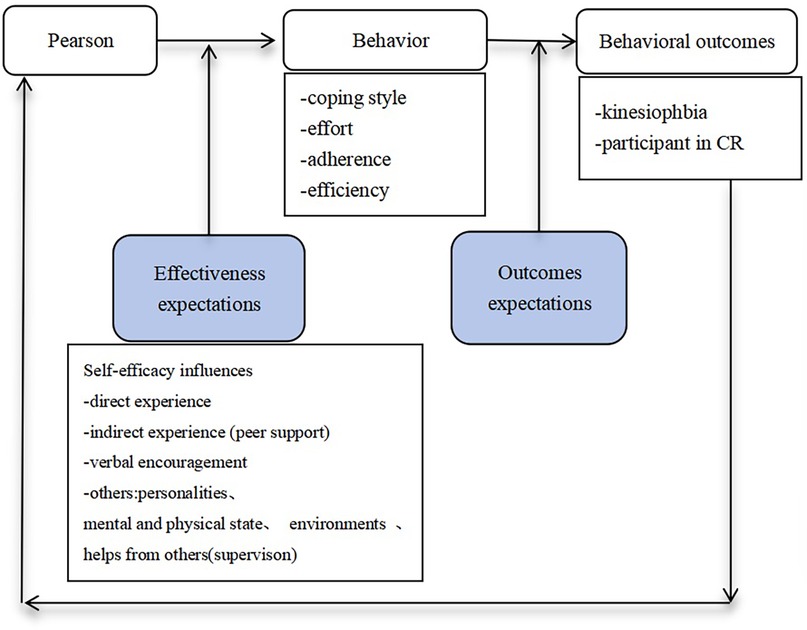
Kinesiophobia may contribute to less physical involvement in a considerable portion of patients with CHD. After 12 weeks of intervention, the kinesiophobia scale scores of the IG reduced considerably, demonstrating the benefit of the WeChat intervention (35). Through WeChat, participants received positive comments and encouragement from health workers as well as moral support from their peers. Health workers are individuals they trust, and peers are those with whom they jointly fight the ailment. According to Bandura's theory, positive feedback and encouragement are necessary to increase self-efficacy (36); the theoretical framework is shown in Figure 2. We supposed that the WeChat-based intervention significantly reduced kinesiophobia by enhancing self-efficacy. Self-efficacy is defined as the patients’ conviction in their own ability to carry out or sustain a habit, which is an important indication of exercise adherence (37). The primary theoretical component elements of self-efficacy are direct experience (e.g., performance achievement), indirect experience, verbal encouragement, and others (e.g., physiological and physical conditions). The verbal encouragement intervention to improve self-efficacy is characterised by growing one's confidence via positive feedback and persuasion, whereas indirect experience is characterised by support from peers. The IG participants exhibited a substantial increase in exercise self-efficacy after the intervention, which is similar to the study by Wang et al. (38). Domestic studies have shown that patients with higher levels of self-efficacy have better exercise compliance (39, 40). Patients with stronger self-efficacy are more enthusiastic about exercising and are less likely to quit, which is the final purpose of any intervention to encourage patients to take CR after PCI.
Brisk walking plays a positive role in improving athletic ability after PCI (41, 42). It is also the most accepted form of exercise for elderly people in China because of its convenience, low cost, and home-based nature. A study has shown that brisk walking for 30 min per day for approximately 3 months improved exercise endurance in patients with CHD (43). Previous studies have focused on the overall interventions and outcomes (44, 45); however, there remains a concern that brisk walking cannot improve patient compliance. The results of the present study showed that after 12 weeks of intervention, peak VO2 in the IG significantly increased compared with the CG and pre-IG, which is consistent with most studies in China and abroad (46, 47). In our study, with the use of WeChat, the home-based CR intervention successfully raised cardiopulmonary endurance in patients after PCI. These outcomes demonstrated that WeChat-based brisk walking improved participants’ adherence because it did not have commuting difficulties and scheduling issues compared with conventional brisk walking, thus raising their cardiopulmonary endurance. In addition, older patients who lack social support and are in worse physical condition are more likely to quit the rehabilitation (27); however, WeChat-based brisk walking plays a crucial role in monitoring their exercise. Through professional guidance, it helps patients develop a daily exercise habit in a way that is both effective and comfortable for them, as expected. Moreover, the WeChat-based brisk walking for post-PCI patients is holistic and continuous. Nurses oversee the entire process, monitoring participants’ conditions and providing guidance on maintaining an optimal heart rate. They also issue alerts when a participant’s heart rate approaches its maximum during exercise. Ensuring safety is crucial to the successful implementation of WeChat-based brisk walking post-PCI patients. In this study, no patient trials involved significant safety risks.
The WeChat-based brisk walking rehabilitation programme provides greater convenience for patients facing financial difficulties or living in remote areas. It may offer more significant benefits and a better cost–benefit ratio than conventional methods (48). In addition, this novel intervention may help patients sustain long-term healthy behaviours.
However, our study has some. First, it included only patients from the cardiology department of a single hospital, resulting in limited sample representativeness. Future research should expand the scope by conducting a multicentre randomised controlled trial. Second, because of limited funding and personnel resources, the intervention only lasted 12 weeks, preventing an assessment of its long-term effects.
5 Conclusion
The WeChat-based brisk walking CR management programme enhances exercise self-efficacy and reduces kinesiophobia through three modalities: medical staff support, positive feedback, and encouragement. It also improves patients’ adherence to exercise, leading to better cardiorespiratory endurance. The WeChat-based brisk walking intervention is both feasible and acceptable, overcoming time and space limitations to support disease management in post-PCI patients. By leveraging established online social media platforms, nurses can share health education materials and engage with patients remotely, which will accelerate the development of e-health.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee of Hebei General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
B-YW: Writing – original draft, Writing – review & editing. CZ: Writing – original draft, Writing – review & editing. XS: Writing – original draft, Writing – review & editing. F-MY: Writing – original draft, Writing – review & editing. M-XL: Writing – original draft, Writing – review & editing. J-YZ: Writing – original draft, Writing – review & editing. QL: Writing – original draft, Writing – review & editing. LZ: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The effect of social network-based brisk walking on rehabilitation self-efficacy of patients with coronary heart disease after PCI No. 20220895.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chepeleva EV. Cell therapy in the treatment of coronary heart disease. Int J Mol Sci. (2023) 24(23):16844. doi: 10.3390/ijms242316844
2. Shahjehan RD, Sharma S, Bhutta BS. Coronary artery disease. In: StatPearls. Treasure Island, FL: StatPearls Publishing (2024).
3. Tao S, Tang X, Yu L, Li L, Zhang G, Zhang L, et al. Prognosis of coronary heart disease after percutaneous coronary intervention: a bibliometric analysis over the period 2004–2022. Eur J Med Res. (2023) 28(1):311. doi: 10.1186/s40001-023-01220-5
4. The WCOTROCHADIC. Report on cardiovascular health and diseases in China 2022: an updated summary. Biomed Environ Sci. (2023) 36(8):669–701. doi: 10.3967/bes2023.106
5. Kohsaka S. To the future and beyond: recent advances in the application of percutaneous coronary intervention. J Clin Med. (2021) 10(2):177. doi: 10.3390/jcm10020177
6. McGregor G, Powell R, Begg B, Birkett ST, Nichols S, Ennis S, et al. High-intensity interval training in cardiac rehabilitation: a multi-centre randomized controlled trial. Eur J Prev Cardiol. (2023) 30(9):745–55. doi: 10.1093/eurjpc/zwad039
7. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. (2022) 29(1):5–115. doi: 10.1093/eurjpc/zwab154
8. Li J, Li Y, Gong F, Huang R, Zhang Q, Liu Z, et al. Effect of cardiac rehabilitation training on patients with coronary heart disease: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10(11):11901–9. doi: 10.21037/apm-21-3136
9. Shea MG, Farris SG, Hutchinson J, Headley S, Schilling P, Pack QR. Effects of exercise testing and cardiac rehabilitation in patients with coronary heart disease on fear and self-efficacy of exercise: a pilot study. Int J Behav Med. (2024) 31(5):659–68. doi: 10.1007/s12529-023-10207-9
10. Hoffmann JM, Hellwig S, Brandenburg VM, Spaderna H. Measuring fear of physical activity in patients with heart failure. Int J Behav Med. (2018) 25(3):294–303. doi: 10.1007/s12529-017-9704-x
11. Dibben GO, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur Heart J. (2023) 44(6):452–69. doi: 10.1093/eurheartj/ehac747
12. Sun MM. Study on the Relationship between Fear of Action, Self-Perceived Burden and Quality of Life in Young and Middle-Aged Patients with Coronary Heart Disease. Yan'an City, Shaanxi Province: Yanan University (2019).
13. Knapik A, Dąbek J, Brzęk A. Kinesiophobia as a problem in adherence to physical activity recommendations in elderly Polish patients with coronary artery disease. Patient Prefer Adherence. (2019) 13:2129–35. doi: 10.2147/PPA.S216196
14. Keessen P, den Uijl I, Visser B, van den Berg-Emons H, Latour CHM, Sunamura M, et al. Fear of movement in patients attending cardiac rehabilitation: a validation study [published correction appears in J Rehabil Med. 2020 Oct 19;52(10):jrm00114]. J Rehabil Med. (2020) 52(2):jrm00021. doi: 10.2340/16501977-2653
15. Han JY, Liu FL, Zhang HM, Li RL, Li R. Status and influencing factors of physical activity among patients after percutaneouscoronary intervention. Modern Prev Med. (2020) 47(14):2677–84. doi: 10.20043/j.cnki.mpm.2020.14.044
16. Zhang HW, Lei MR, Liu P, Liu J, Luan XR. Progress of kinesiophobia in patients with heart diseases. Chin Nurs Manag. (2021) 21(5):785–8. doi: 10.3969/j.issn.1672-1756.2021.05.030
17. Bäck M, Jansson B, Cider A, Herlitz J, Lundberg M. Validation of a questionnaire to detect kinesiophobia (fear of movement) in patients with coronary artery disease. J Rehabil Med. (2012) 44(4):363–9. doi: 10.2340/16501977-0942
18. Lei MJ, Liu TT, Xiong SQ, Sang M, Jin CD. Reliability and validity test of Chinese version of the Tampa scale for kinesiophobia heart. Chin Nurs Manag. (2019) 19(11):1637–42. doi: 10.3969/j.issn.1672-1756.2019.11.009
19. Ding Y, Pan Y, Wang M, Cao L, Xu H, Wei L, et al. Factors influencing kinesiophobia during the “blanking period” after radiofrequency catheter ablation in patients with atrial fibrillation by the fear-avoidance model. Int J Cardiol. (2022) 363:49–55. doi: 10.1016/j.ijcard.2022.06.021
20. Zhu H, Zhang DN, Jin KJ, Chen XM. The reliability and validity of the Chinese version of kinesiophobia causes scale. Nurs J Chin Peoples Liberation Army. (2020) 37(1):1–4. doi: 10.3969/j.issn.1008-9993.2020.01.001
21. Keessen P, Latour CHM, van Duijvenbode ICD, Visser B, Proosdij A, Reen D, et al. Factors related to fear of movement after acute cardiac hospitalization. BMC Cardiovasc Disord. (2020) 20(1):495. doi: 10.1186/s12872-020-01783-9
22. Bäck M, Caldenius V, Svensson L, Lundberg M. Perceptions of kinesiophobia in relation to physical activity and exercise after myocardial infarction: a qualitative study. Phys Ther. (2020) 100(12):2110–9. doi: 10.1093/ptj/pzaa159
23. Avila A, Claes J, Goetschalckx K, Buys R, Azzawi M, Vanhees L, et al. Home-based rehabilitation with telemonitoring guidance for patients with coronary artery disease (short-term results of the TRiCH study): randomized controlled trial. J Med Internet Res. (2018) 20(6):e225. doi: 10.2196/jmir.9943
24. Dai ZJ, Zhou JY, Xu ST, Zhang JF, Zhuang CF, Gu PH. Application of continuous nursing care based on hierarchical diagnosis and treatment mode in stage II cardiac rehabilitation of patients after percutaneous coronary intervention. Front Cardiovasc Med. (2022) 9:922449. doi: 10.3389/fcvm.2022.922449
25. Harriss DJ, MacSween A, Atkinson G. Ethical standards in sport and exercise science research: 2020 update. Int J Sports Med. (2019) 40(13):813–7. doi: 10.1055/a-1015-3123
26. Li Y, Chen KY, Zhou LH. Application of walking exercise method based on timing theory in elderly patients with chronic heart failure. Nurs J Chin Peoples Liberation Army. (2021) 38(6):72–5. doi: 10.3969/j.issn.1008-9993.2021.06.019
27. Brouwers RWM, van Exel HJ, van Hal JMC, Jorstad HT, de Kluiver EP, Kraaijenhagen RA, et al. Cardiac telerehabilitation as an alternative to centre-based cardiac rehabilitation. Neth Heart J. (2020) 28(9):443–51. doi: 10.1007/s12471-020-01432-y
28. The Chinese guidelines for percutaneous coronary interventional therapy (2016) have been officially released. Chin J Interv Cardiol. (2016) 24(06):315. https://kns.cnki.net/kcms2/article/abstract?v=hW9FdoQEeroZ5lUS1N4CDmrn3R-ycgfIpjNmLMcJpwY192RadZXeT4g70yaLMVrBFV-82jjEqbedbhl1IUML9A0pK6mbqFmVTt96LKo5-y1Immc151j2UvPY279M-4uDDSbmzfgd8PFbHkckDjiaM3igiuWwZrzOKy9rR5q6lfF2a0QDIm5rbrKDhNX5rET&uniplatform=NZKPT&language=CHS
29. Shen Y, Wang WM, Zhang Q, Zhou YJ, Shen YF. Clinical research update on percutaneous coronary intervention in 2022. Chin J Interv Cardiol. (2023) 31(1):25–32. doi: 10.3969/j.issn.1004-8812.2023.01.005
30. Hou WX, Hou WC. Effect analysis of percutaneous coronary intervention on the treatment of coronary heart disease. Clin Res. (2024) 32(3):34–7. doi: 10.12385/j.issn.2096-1278(2024)03-0034-04
31. Lei MJ, Liu TT, Xiong SQ, Sang M, Jin CD. The sinicization and reliability validity testing of the exercise fear scale for heart disease patients. Nurs Manag China. (2019) 19(11):6. CNKI:SUN:GLHL.0.2019-11-013
32. Lee LL, Perng SJ, Ho CC, Hsu HM, Lau SC, Arthur A. A preliminary reliability and validity study of the Chinese version of the self-efficacy for exercise scale for older adults. Int J Nurs Stud. (2009) 46(2):230–8. doi: 10.1016/j.ijnurstu.2008.09.003
33. Dun Y, Olson TP, Ripley-Gonzalez JW, Xie K, Zhang W, Cai Y, et al. Safety of exercise testing in the clinical Chinese population. Front Cardiovasc Med. (2021) 8:638682. doi: 10.3389/fcvm.2021.638682
34. Li SJ, Hou SX, Tong SM. Exercise tolerance and its associated factors of coronary heart disease patients at different years after percutaneous coronary intervention. Chin J Rehabil Med. (2022) 37(12):1622–9. doi: 10.3969/j.issn.1001-1242.2022.12.006
35. Zhou SH, Huang ST, Xu N, Chen LW, Chen Q. Application of the WeChat platform to implement continuous nursing for patients after percutaneous coronary intervention. Med Sci Monit. (2020) 26:e925444. doi: 10.12659/MSM.925444
36. Islam KF, Awal A, Mazumder H, Munni UR, Majumder K, Afroz K, et al. Social cognitive theory-based health promotion in primary care practice: a scoping review. Heliyon. (2023) 9(4):e14889. doi: 10.1016/j.heliyon.2023.e14889
37. Picha KJ, Howell DM. A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self-efficacy. Musculoskeletal Care. (2018) 16(1):233–7. doi: 10.1002/msc.1194
38. Wang Z, Zhang Y, Wang Y, Liu L, Zhang J. Kinesiophobia and its associated factors in patients with coronary heart disease: a cross-sectional study based on latent feature analysis. BMJ Open. (2023) 13(7):e072170. doi: 10.1136/bmjopen-2023-072170
39. Ding R, Smith JR, Medina-Inojosa JR, Zhang S, Supervia M, Fischer KM, et al. Cardiac rehabilitation referral and participation rates for heart failure with reduced ejection fraction. J Cardiopulm Rehabil Prev. (2021) 41(2):126–7. doi: 10.1097/HCR.0000000000000589
40. Tang L, Liu CX, Li Y, Ma J. Correlation of awareness on cardiac rehabilitation with exercise compliance in middle-aged and aged coronary heart disease patients after percutaneous coronary intervention. Chin J Multiple Organ Dis Elderly. (2018) 17(1):66–9. doi: 10.11915/j.issn.1671-5403.2018.01.014
41. Nakayama A, Nagayama M, Morita H, Kawahara T, Komuro I, Isobe M. The use of geographical analysis in assessing the impact of patients’ home addresses on their participation in outpatient cardiac rehabilitation: a prospective cohort study. Environ Health Prev Med. (2020) 25(1):76. doi: 10.1186/s12199-020-00917-x
42. Borg S, Öberg B, Leosdottir M, Lindolm D, Nilsson L, Bäck M. Factors associated with non-attendance at exercise-based cardiac rehabilitation [published correction appears in BMC Sports Sci Med Rehabil. 2019 Oct 17;11:24]. BMC Sports Sci Med Rehabil. (2019) 11:13. doi: 10.1186/s13102-019-0125-9
43. Scherrenberg M, Janssen J, Lauwers A, Schreurs I, Swinnen M, Dendale P. Is there an optimal dose of cardiac rehabilitation in coronary artery disease patients? Int J Cardiol. (2021) 330:7–11. doi: 10.1016/j.ijcard.2021.01.065
44. Stefanakis M, Batalik L, Antoniou V, Pepera G. Safety of home-based cardiac rehabilitation: a systematic review. Heart Lung. (2022) 55:117–26. doi: 10.1016/j.hrtlng.2022.04.016
45. Thomas RJ, Petersen CE, Olson TP, Beatty AL, Ding R, Supervia M. Asynchronous and synchronous delivery models for home-based cardiac rehabilitation: a SCIENTIFIC REVIEW. J Cardiopulm Rehabil Prev. (2021) 41(6):407–12. doi: 10.1097/HCR.0000000000000656
46. Duscha BD, Piner LW, Patel MP, Craig KP, Brady M, McGarrah RW, et al. Effects of a 12-week mHealth program on peak VO2 and physical activity patterns after completing cardiac rehabilitation: a randomized controlled trial. Am Heart J. (2018) 199:105–14. doi: 10.1016/j.ahj.2018.02.001
47. Snoek JA, Prescott EI, van der Velde AE, Eijsvogels TMH, Mikkelsen N, Prins LF, et al. Effectiveness of home-based mobile guided cardiac rehabilitation as alternative strategy for nonparticipation in clinic-based cardiac rehabilitation among elderly patients in Europe: a randomized clinical trial. JAMA Cardiol. (2021) 6(4):463–8. doi: 10.1001/jamacardio.2020.5218
Keywords: cardiac rehabilitation, WeChat, brisk walking, kinesiophobia, nursing
Citation: Wan B-Y, Zhou C, Sun X, Yu F-M, Liu M-X, Zhang J-Y, Li Q and Zhang L (2025) The effect of WeChat-based brisk walking on kinesiophobia in patients after percutaneous coronary intervention: a randomised controlled trial. Front. Cardiovasc. Med. 12:1416356. doi: 10.3389/fcvm.2025.1416356
Received: 17 May 2024; Accepted: 24 February 2025;
Published: 29 April 2025.
Edited by:
Kaizheng Gong, Affiliated Hospital of Yangzhou University, ChinaReviewed by:
Yuan Yuan, Yangzhou University, ChinaJuanjuan Xiong, The First Affiliated Hospital of Nanchang University, China
Copyright: © 2025 Wan, Zhou, Sun, Yu, Liu, Zhang, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qi Li, bGlxaXM4bjJ2aDAyQDIxY24uY29t; Li Zhang, emhhbmczbGk1X2gycW96MUB5ZWFoLm5ldA==
 Bo-Ya Wan1
Bo-Ya Wan1 Li Zhang
Li Zhang