Abstract
Objective:
Tai Chi is a form of physical and mental exercise. Hypertension, characterized by persistently elevated blood pressure, is a prevalent cardiovascular condition. At present, the effect of Tai Chi exercise cycle on improving the prognosis of patients with essential hypertension, as well as its impact on patients at different stages of hypertension, has not yet been demonstrated. Through meta-analysis, this study systematically evaluated the effects of Tai Chi on hypertensive patients, as well as the roles played by different practice duration, so as to provide evidence-based guidance for future clinical application.
Methods:
This meta-analysis, registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42024538168), reviewed RCTs involving Tai Chi interventions for hypertension. Studies were sourced from PubMed, the Cochrane Library, CBM, CNKI, WANFANG, and Embase. Mean differences (MD) and 95% confidence intervals (CI) were calculated using a random-effects model. The sources of heterogeneity were explored using the elimination method one by one and subgroup analysis, supplemented by sensitivity analysis and publication bias assessment.
Results:
Seventeen studies were included in the analysis. No adverse events were reported in all the included studies. Tai Chi significantly reduced Systolic Blood Pressure (SBP) (WMD = −9.12; 95% CI = −12.35 to −5.90), Diastolic Blood Pressure (DBP) (WMD = −5.43; 95% CI = −7.22 to −3.64), Total Cholesterol (TC) (WMD = −0.37; 95% CI = −0.62 to −0.12), Triglycerides (TG) (WMD = −0.53; 95% CI = −0.89 to −0.16), and Low-Density Lipoprotein (LDL) levels (WMD = −0.70; 95% CI = −1.12 to −0.28) compared to control groups. Waist circumference (WC) also improved. Subgroup analyses showed that short-term Tai Chi (3 months) was most effective for improving essential hypertension, with a greater impact in grade I hypertension patients compared to those with grade II. No obvious publication bias was found through funnel plots and Egger's test.
Conclusion:
The results demonstrated that Tai Chi effectively reduced SBP, DBP, TC, TG, and LDL levels, with the most significant improvements observed at 12 weeks. These findings support the use of Tai Chi as a scientifically validated exercise rehabilitation tool in clinical settings and suggest avenues for further research.
Systematic Review Registration:
identifier, PROSPERO [CRD42024538168].
1 Introduction
Cardiovascular diseases (CVDs) pose a significant threat to global health, driven by numerous risk factors contributing to their increasing prevalence (1, 2). Recognized traditional risk factors for cardiovascular disease include obesity, hypertension, dyslipidemia, hyperglycemia, poor diet, family history of cardiovascular disease, physical inactivity, and smoking (3, 4). Hypertension affects approximately 275 million individuals in China, with 95% of whom suffer from essential hypertension (EH), making it a major CVD risk factor (5, 6). Left untreated or poorly managed, accelerates EH progression and increases mortality risk.
Lack of physical activity is a major behavioral risk factor for cardiovascular diseases and is often associated with elevated blood pressure, blood lipids, blood sugar, and overweight or obesity (7). Guidelines for cardiovascular disease prevention state that lifestyle changes (including smoking cessation, physical activity and dietary modification) are the first step in primary prevention (4). Regular moderate-intensity exercise helps lower blood pressure, blood lipids, and reduce the risk of heart attack and stroke. The “Chinese Guidelines for Hypertension Prevention and Treatment (2018 Revision)” recommends 120 min of moderate-intensity aerobic exercise per week (8).
In recent years, more studies have shown that appropriate aerobic exercise can effectively regulate the physiological and psychological aspects of patients with EH. Tai Chi, as an aerobic exercise, combines strength and flexibility with a balance of movement and stillness (9). The coordination of breathing, consciousness, and physical movements during Tai Chi enhances patient concentration, reduces sympathetic nervous tension, improves nervous system function, regulates blood pressure, and promotes sleep (10–12). Tai Chi, through its unique mechanisms of mind-quieting, body-relaxation, regulated breathing, and dantian cultivation, offers comprehensive benefits to cardiovascular health. It improves blood pressure and lipid levels through various pathways, including anti-oxidative stress (13), anti-inflammation (14), modulation of the autonomic nervous system (15), and enhancement of endothelial function (16). Existing research indicates that Tai Chi is more economical and safer compared to drug treatment, and it is the most effective method among all non-drug interventions (17, 18). Previous meta-analyses of Tai Chi on patients with essential hypertension generally focused only on its impact on blood pressure values (SBP, DBP), and there were few reports on blood lipids and body morphology (19, 20), different stages of hypertension, and intervention cycles. Dyslipidemia is another significant factor contributing to essential hypertension (EH) (21). The impact of different intervention cycles on the effect is huge.
To comprehensively evaluate the effects of Tai Chi on blood pressure and blood lipids in hypertensive patients, this study conducts a meta-analysis of RCTs involving Tai Chi interventions in hypertensive patients. This study will focus on examining the varying effects of Tai Chi interventions across different stages of hypertension, investigating the impacts of different intervention cycles on essential hypertension, then assessing its feasibility as a non-pharmacological treatment.
2 Methods
2.1 Protocol and registration
This systematic review was conducted according to the guidelines provided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The study protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO), under the registration number CRD42024538168.
2.2 Search strategy
We conducted comprehensive searches of three English-language databases (PubMed, Embase, Cochrane Library) and three Chinese-language databases (CNKI, Wan Fang, CBM) up to April 9, 2024. For PubMed, the search strategy included variations of “Tai Ji” such as “Tai Chi,” “taiji,” and “taijiquan,” combined with terms like “Hypertension,” “Blood Pressure,” or “High Blood Pressure.” The specific search strategy can be found in the Supplementary Materials.
2.3 Inclusion criteria
We employed the PICOS (Participants, Interventions, Comparisons, Outcomes, and Study design) framework to define our inclusion criteria (Table 1). Participants of all nationalities and genders were eligible, provided their average age was 40 years or above. The participants needed to meet the diagnostic criteria for hypertension (SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg) or prehypertension (SBP of 130–139 mm Hg and/or DBP of 80–89 mm Hg). The experimental group performed Tai Chi, either as a stand-alone intervention or combined with Medication treatment, such as oral nifedipine sustained-release tablets. The comparison group were those undergoing standard Western medical treatments, engaging in other forms of exercise, or served as controls. Additionally, studies had to be published with complete data.
Table 1
| PICOS components |
Detail |
|---|---|
| Participants | 40 ≤ Adults average age; hypertensive patient [The participants needed to meet the diagnostic criteria for hypertension (SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg) or prehypertension (SBP of 130 to 139 mm Hg and/or DBP of 80 to 89 mm Hg)]. |
| Interventions | Taichi routine (common form) |
| Comparisons | Standardised western medical, sporting and non-sporting groups |
| Outcomes | Blood pressure (SBP, DBP); TC; TG; LDL; HDL; BMI; WC |
| Study designs | RCT |
The inclusion criteria of PICOS.
SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; TG, triglycerides; LDL, low-density lipoprotein; HDL, high-density lipoprotein; BMI, body mass index; WC, waist circumference; RCT, randomized controlled trial.
2.4 Exclusion criteria
The exclusion criteria were as follows: (1) lack of a control group; (2) duplicate studies, with preference given to the most comprehensive version; (3) non-original sources such as reviews or conference abstracts; (4) studies involving animal models; (5) participants with a history of myocardial infarction, chronic heart failure, arrhythmias, or other cardiovascular disorders; (6) experimental subgroups with fewer than 20 participants per group; (7) inadequate randomization methods; (8) studies classified as low quality.
2.5 Data extraction
The researchers systematically extracted data from all eligible publications. The extracted information included study authors, publication year, participant characteristics (health status, total sample size, mean age, and gender ratio), details of the intervention (frequency and duration), control measures, randomization and blinding methods, and reported outcomes. For studies with multiple observation points, only the final outcome data were considered.
2.6 Quality assessment
We assessed the methodological quality of the included studies using the Cochrane risk-of-bias tool (22). Two researchers independently evaluated each study, resolving any disagreements with a third reviewer. Seven domains were considered: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other potential sources of bias (23). Studies were classified as low risk (five or more domains rated as low risk), moderate risk (three to four domains rated as low risk), or high risk (fewer than three domains rated as low risk) (24).
2.7 Statistical analysis
RevMan 5.3 was used to plot the quality assessment and the forest plots for all indicators, and Stata 14.0 was used for bias tests, sensitivity analyses, and funnel plots. The meta-analyses evaluated various participant parameters, including SBP, DBP, TC, TG, HDL, LDL, BMI, and WC. Mean effects and standard deviations (SD) were calculated using Stata 14.0, with 95% confidence intervals (CIs) were applied to all studies. Statistical significance was defined as P < 0.05. Effect sizes (ES) were used to evaluate the summary estimates. When there was no heterogeneity among the included studies (P > 0.05), a fixed-effects model was chosen for the Meta-analysis, and a random-effects model was applied when there was heterogeneity among the studies. Publication bias was assessed using Egger's test (25, 26), with significance set at P < 0.05.
3 Results
3.1 Study selection
We searched Chinese and English databases and retrieved a total of 1,780 documents. First, NoteExpress literature management software was used to remove duplicates, literature reviews, meta-analyses, animal studies, and conference registrations. Titles, authors, publication years, and journals were then manually screened. Machine-based screening identified and excluded 513 duplicate papers. Further review of the remaining 1,267 abstracts led to the exclusion of studies for the following reasons: (1) not being randomized controlled trials, (2) participants not having hypertension, (3) interventions not involving Tai Chi, (4) being conference abstracts or registration papers, and (5) incomplete or unconvertible data. After a full-text review of 151 studies, 17 articles were deemed eligible for inclusion (Figure 1).
Figure 1
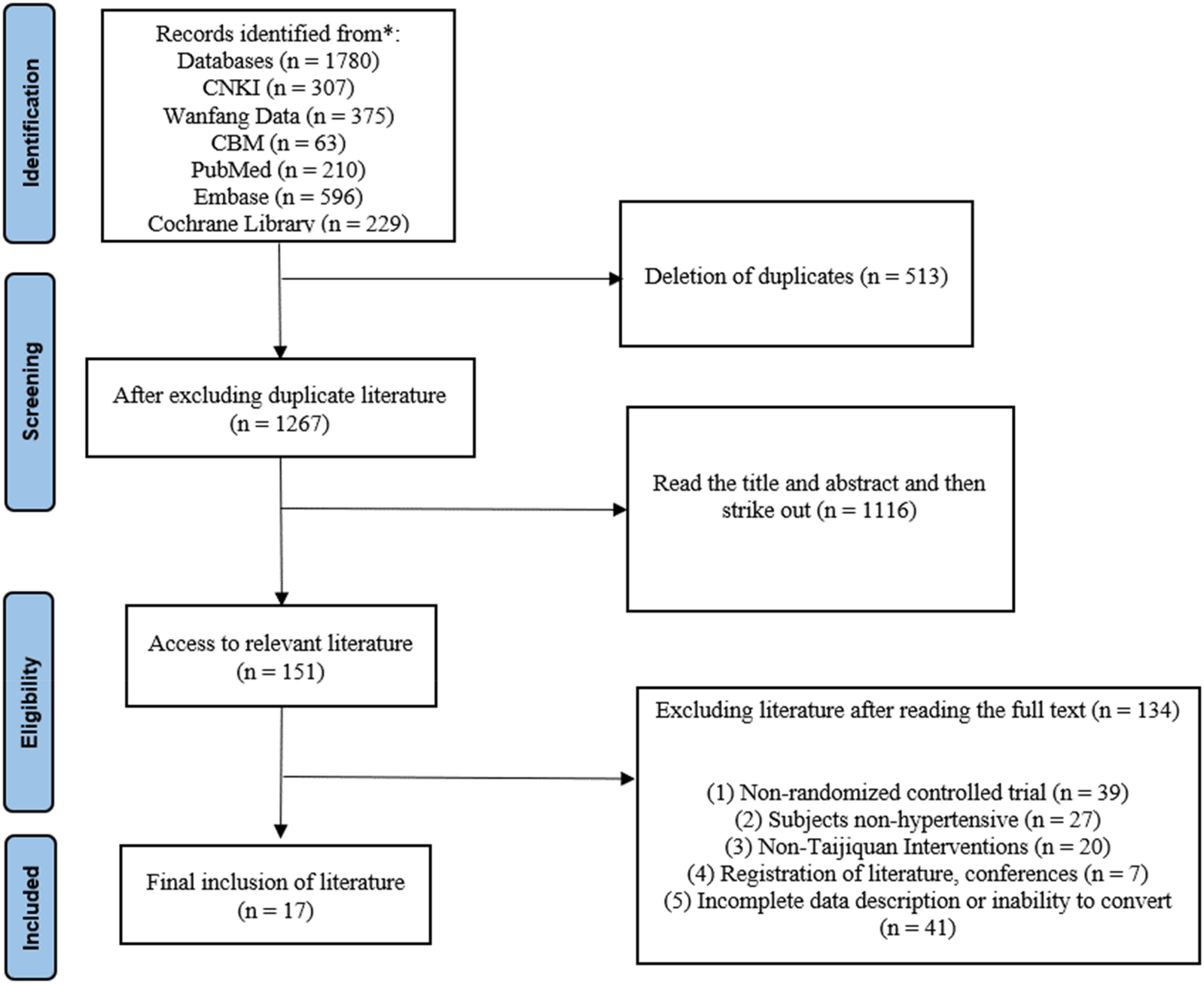
A PRISMA flow chart.
3.2 Characteristics of the included studies
Seventeen studies included Tai Chi as an independent intervention. Most studies were double-arm RCTs, although four studies used a three-arm RCT design. Of the double-arm trials, 11 compared the Tai Chi group to a blank control group, while the other two compared Tai Chi to alternative exercise programs, such as walking or aerobic exercise. Table 2 displays the detailed characteristics of the included studies. Among three-arm pilot studies, three included both blank control groups and groups engaging in other forms of exercise. Another study compared Tai Chi participants to a healthy population without involving additional exercise groups. In all the studies, the interventions spanned a minimum of 12 weeks, with session frequencies ranging from 1 to 10 times per week and session durations varying from 0.5 to 3 h. The most common intervention period was 12 weeks (observed in 12 studies), with a typical session frequency of 3–5 times per week.
Table 2
| Trial | Sample size | Age | Intervention | Treatment | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|
| Experimental group |
Control group | Experimental group |
Control group | Experimental group |
Control group | Period (W) |
Frequency | ||
| Xiaobin Wang 2019 (27) | 50(S) 20/30(M/W) | 50(S) 22/28(M/W) | 67.6 ± 4.5 | 67.4 ± 4.2 | Twenty-four Patterns of Taijiquan | Routine treatment and care of hypertension | 12 | 40–60 min, 3/w | ①②③④⑤⑥ |
| Lijuan Feng 2018 (28) | 36(S) 19/17(M/W) | 37(S) 14/23(M/W) | 66.33 ± 4.74 | 67.51 ± 4.09 | Taijiquan | 1 h routine walk | 12 | 1 h, 3/w | ①②③④⑤⑥ |
| Yongcai Zheng 2015 (29) | 49(S) 20/29(M/W) | 48(S) 19/29(M/W) | 54.71 ± 5.43 | 55.77 ± 6.24 | Twenty-four Patterns of Taijiquan | Nifedipine Sustained-release Tablets | 12 | 40–60 min, 4–8/w | ①②③④⑤⑥ |
| Huijuan Xie 2014 (30) | 25(S) 11/14(M/W) | 25(S) 14/11(M/W) | 60–70 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 1 h, 5/w | ①② | |
| Yami Cao 2024 (31) | 40(S) 21/19(M/W) | 40(S) 22/18(M/W) | 66.98 ± 5.48 | 67.02 ± 5.46 | Twenty-four Patterns of Taijiquan | Levoamlodipine Maleate Tablets | 12 | 60 min, 1/d | ①② |
| Shouxiao Ling 2018 (32) | 98(S) 48/50(M/W) | 100(S) 55/45(M/W) | 52.35 ± 3.26 | 51.35 ± 4.21 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 45–60 min, 1–2/d | ①② |
| Qiaoying Han 2010 (33) | 30 | 28 | 62.12 ± 10.51 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 240 | 45–60 min, 1–2/d | ①② | |
| Xiaojun Wang 2011 (34) | 30 | 30 | 50–70 | Taijiquan Exercise Prescription | General daily lifestyle interventions | 16 | 60 min, 5/w | ①② | |
| Zibo Shi 2017 (35) | 30(S) 17/13(M/W) | 30(S) 18/12(M/W) | 43.26 ± 9.76 | 41.58 ± 9.12 | Taijiquan | Low-salt, low-fat diet education | 12 | 30 min, 4–5/w | ①② |
| Jing Sun 2015 (11) | 136(S) 19/117(M/W) | 130(S) 29/101(M/W) | 45–80 | Taijiquan | Non-motor activity | 48 | Group activities 3 h/week and individual family exercises 2 h/week | ①②③④⑤⑥⑦⑧ | |
| Xiao-Ling Shou 2019 (36) | 98(S) 48/50(M/W) | 100(S) 55/45(M/W) | 52 ± 6.46(M), 51 ± 7.09(W) | 52 ± 8.98(M) 51 ± 7.54(W) | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 40–90 min, 1–2/d | ①②③④⑤⑥⑦ |
| Aileen Wai Kiu Chan 2018 (37) | 82(S) 32/50(M/W) | 82(S) 38/44(M/W) | 64.70 ± 7.59 | 65.13 ± 10.22 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 60 min, 2/w | ①②③④⑤⑥⑦⑧ |
| JEN-CHEN TSAI 2003 (10) | 37(S) 19/18(M/W) | 39(S) 19/20(M/W) | 51.6 ± 16.3 | 50.5 ± 9.8 | Taijiquan | General daily lifestyle interventions | 12 | 50 min, 3/w | ①② |
| Chunhua Ma 2018 (38) | 79(S) 54/25(M/W) | 79(S) 55/24(M/W) | 70.24 ± 10.25 | 69.71 ± 10.84 | Twenty-four Patterns of Taijiquan | Routine nursing of hypertension | 24 | 60 min, 3–5/w | ①②⑦⑧ |
| Xinye Li 2024 (39) | 173(S) 86/87(M/W) | 169(S) 80/89(M/W) | 48.4 ± 12.4 | 50.1 ± 11.4 | Twenty-four Patterns of Taijiquan | Aerobic exercise | 48 | 60 min, 4/w | ①②③④⑤⑥⑦⑧ |
| Zhi-Wei Yan 2022 (40) | 49(S) 17/32(M/W) | 47(S) 17/30(M/W) | 59.31 ± 7.52 | 60.78 ± 7.21 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 60 min, 5/w | ①②⑦ |
| Bo Lin 2021 (41) | 60(S) 36/24(M/W) | 50(S) 29/21(M/W) | 64.20 ± 4.04 | 63.80 ± 4.40 | Twenty-four Patterns of Taijiquan | General daily lifestyle interventions | 12 | 60 min, 3/w | ①② |
Characteristics of the included trials.
① SBP; ② DBP; ③ TC; ④ TG; ⑤ HDL; ⑥ LDL; ⑦ BMI; ⑧ (WC).
S, sum; M, male; W, female; W, week; d, day.
All 17 RCTS included were from China. With a total of 2,186 participants: 1,102 in the intervention group and 1,084 in the control group. Sample sizes ranged from 50 to 342 participants, with an average age exceeding 40 years. Two studies did not provide separate data for male and female participants; and all studies analyzed combined data for both sexes. None specifically investigated gender differences in the effects of Tai Chi. Two studies focused on working individuals with hypertension, and only one examined participants in a pre-hypertensive state.
Hypertension is primarily assessed through blood pressure measurements. All 17 articles included in this study evaluated blood pressure measurements (10, 11, 27–41). Dyslipidemia and hypertension are both risk factors for cardiovascular disease (42), and their co-occurrence may exacerbate arterial damage, with dyslipidemia influencing blood pressure. Seven studies specifically investigated lipid levels in hypertensive patients (11, 27–29, 36, 37, 39). BMI and WC are widely used to assess central obesity, a recognized risk factor for hypertension that can increase blood pressure through mechanisms such as insulin resistance and activation of the renin-angiotensin-aldosterone system (RAAS) (5). Six articles assessed participants' body composition and BMI levels (11, 36–40), while WC values were reported in four studies (11, 37–39).
3.3 Risk-of-bias assessment
All 17 full papers were assessed for risk of bias using the Cochrane tool, with the quality evaluation results illustrated in Figures 2, 3. While all studies (100%) mentioned random allocation, only 13 (71%) studies provided details of specific random methods, such as the random number table method or computer-generated random numbers. The remaining four studies did not describe the allocation process. In Figure 3, five or more out of the seven dimensions indicate high quality, while fewer than five indicate medium to low quality. Twelve studies were classified as high quality. Five studies were rated as moderate quality due to unclear descriptions of allocation methods and participant blinding. Given the active participation required for Tai Chi, blinding of participants was not possible, leading to a high risk of performance bias in all studies. Sensitivity analysis and bias tests for all high-quality studies showed an Egger's test result of P = 0.441, which is greater than 0.05. This aligns with the overall findings, indicating the conclusions are reliable (details of the sensitivity analyses can be found in the Supplementary Material).
Figure 2
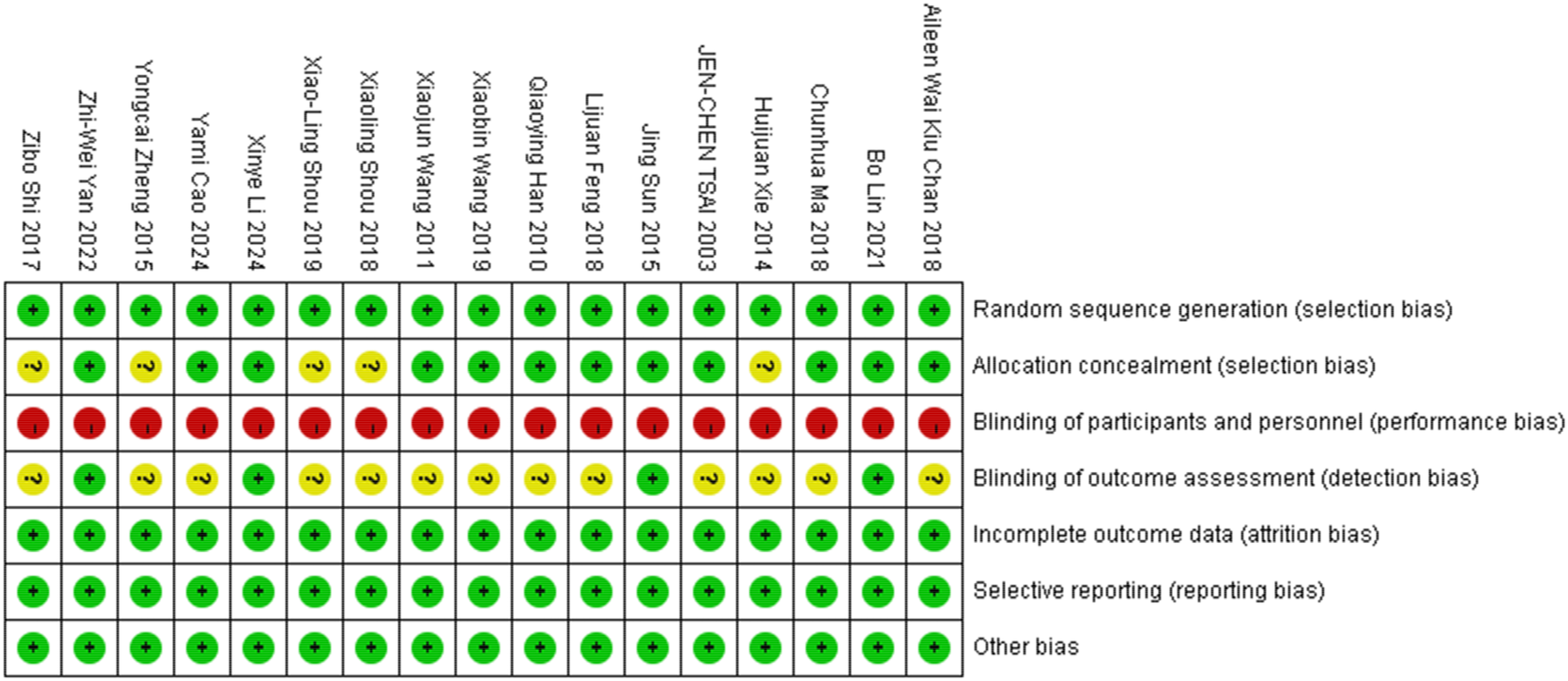
Biases of the included studies.
Figure 3
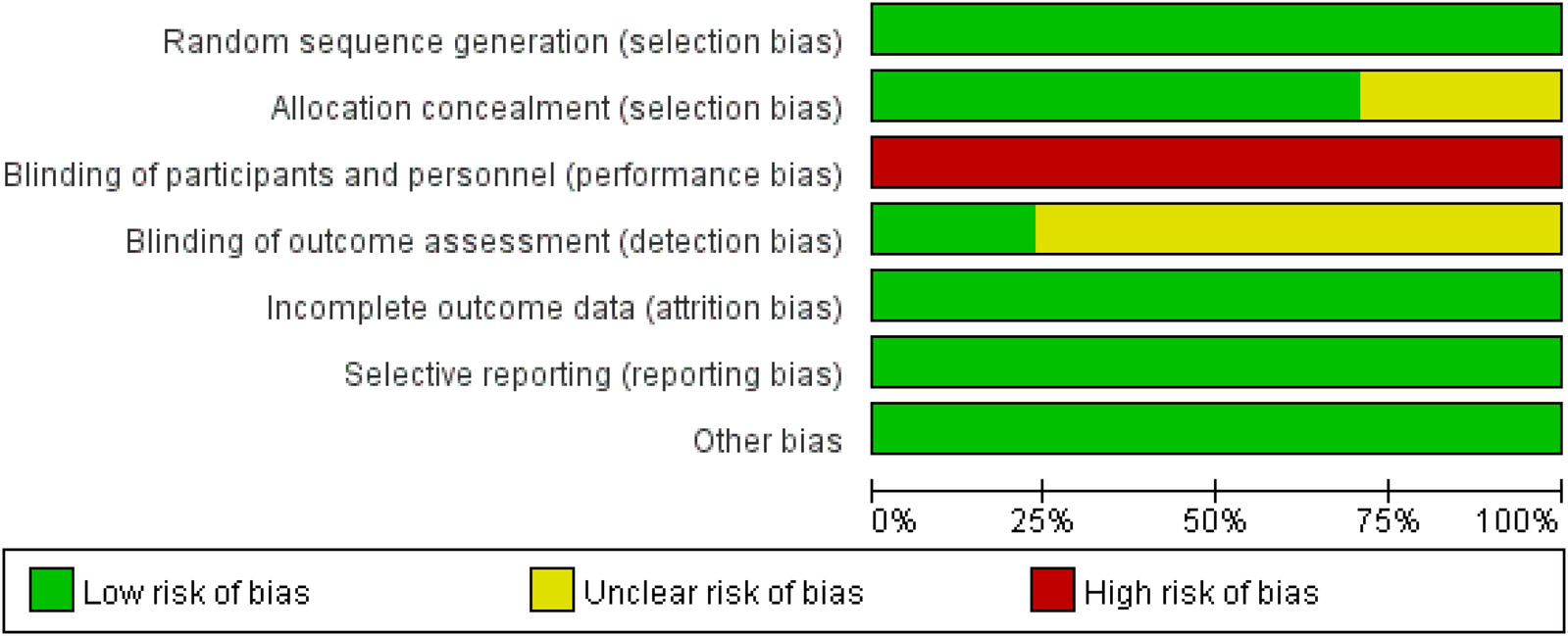
A summary of biases.
4 Effectiveness of Tai Chi
4.1 Tai Chi effect on SBP
The meta-analysis focused on studies that used SBP as the primary outcome measure. Sixteen studies reported a significant decrease in SBP following the Tai Chi intervention (p < 0.05) (10, 11, 28–41), despite some studies showing contradictory results (27). Overall, the meta-analysis revealed that the decrease in SBP was notably higher in the Tai Chi group compared to control groups, although substantial heterogeneity was present (WMD = −9.12; 95% CI = −12.35 to −5.90; Z = 5.54, P = 0.000 < 0.05; I2 = 94%; Egger's test P = 0.685 > 0.05) (Figure 4). Full details of sensitivity analyses and bias assessments are provided in the Supplementary Appendix.
Figure 4
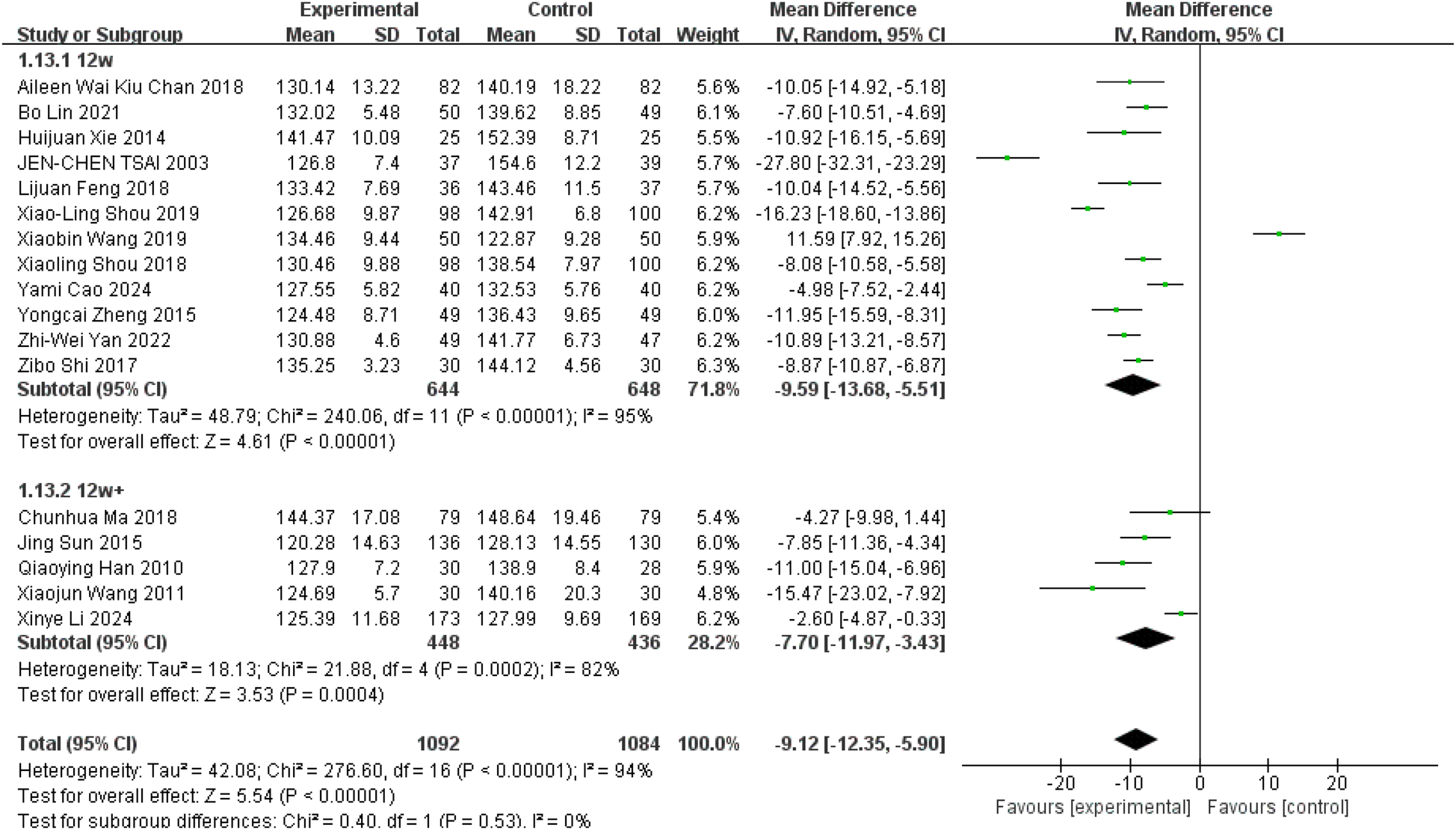
Effect of Tai Chi exercise on SBP levels in hypertensive patients (duration of intervention).
Tai Chi exercise is divided into long-term and short-term intervention cycles, defined as more than three months for long-term and less than three months for short-term interventions. To investigate potential differences in the effects of these intervention cycles on blood pressure in hypertensive patients, time was utilized as a subgroup variable. To further explore the effects of Tai Chi on SBP in hypertensive patients, studies were sub-grouped based on intervention duration: short-term (12 weeks) and long-term (more than 12 weeks). Twelve studies with a short-term intervention demonstrated a significant SBP reduction with Tai Chi (Figure 4, WMD = −9.59; 95% CI = −13.68 to −5.51; Z = 4.61, P = 0.00001 < 0.05; I2 = 95%; Egger's test P = 0.921 > 0.05) (10, 27–32, 35–37, 40, 41), Similarly, five studies with long-term intervention also showed a significant decrease in SBP (Figure 4, WMD = −7.70; 95% CI = −11.97 to −3.43; Z = 3.53, P = 0.0004 < 0.05; I2 = 82%; Egger's test, P = 0.153 > 0.05) (11, 33, 34, 38, 39).
Hypertension is classified into three types: Grade I, Grade II, and Grade III. Grade I hypertension is defined as a systolic blood pressure (SBP) between 140 and 159 mmHg, or a diastolic blood pressure (DBP) between 90 and 99 mmHg. Grade II hypertension is defined as a SBP between 160 and 179 mmHg, or a DBP between 100 and 109 mmHg. Grade III hypertension is defined as a SBP of 180 mmHg or higher, or a DBP of 110 mmHg or higher (1). In studies examining the effects of Tai Chi on hypertension, these subtypes were used as grouping variables, classifying participants into Grade I and Grade II categories. Fourteen studies focused on Grade I hypertension showed that Tai Chi significantly reduced systolic blood pressure (SBP) (Figure 5, WMD = −10.23; 95% CI = −13.10 to −7.35; Z = 6.96, P = 0.00001 < 0.05; I2 = 92%; Egger's test P = 0.375 > 0.05) (10, 11, 28, 30–32, 34–41). Interestingly, three studies targeting Grade II hypertension indicated that while Tai Chi was able to reduce SBP, the difference was not statistically significant (Figure 5, WMD = −3.78; 95% CI = −19.12 to 11.56; Z = 0.48, P = 0.63 > 0.05; I2 = 98%; Egger's test P = 0.754 > 0.05) (27, 29, 33). There was no significant difference between the two groups. Through the one-by-one elimination method, it is found that Wang's (27) study in the Grade 2 hypertension group may be the source of its heterogeneity. After removing it, the analysis results of the Grade 2 hypertension group show that (WMD = −11.52; 95% CI = −14.23 to −8.82; Z = 8.35, P = 0.00001 < 0.05; I2 = 0%) (The figure is in the Supplementary Material).
Figure 5
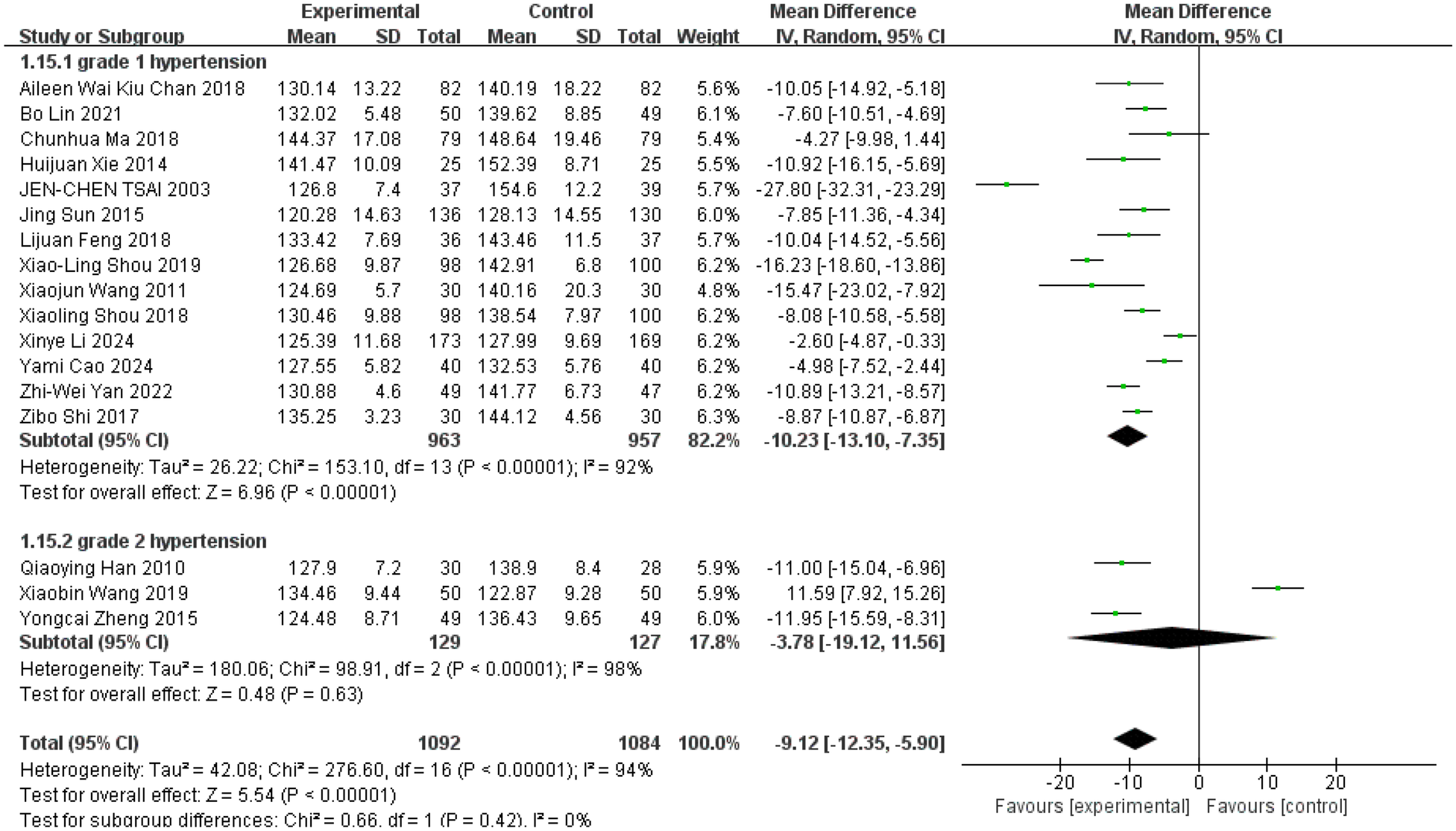
Effect of Tai Chi exercise on SBP levels in hypertensive patients (grade).
4.2 Tai Chi effect on DBP
The meta-analysis included DBP values from all studies (10, 11, 27–41), with 16 studies reported a reduction in DBP following Tai Chi interventions lasting between 12 and 48 weeks (10, 11, 28–41), though some studies reported opposite effects (27). Overall, Tai Chi exercise significantly reduced participants' DBP levels compared to controls (Figure 6, WMD = −5.43; 95% CI = −7.22 to −3.64; Z = 5.94, P = 0.000 < 0.05; I2 = 88%; Egger's test P = 0.67 > 0.05).
Figure 6
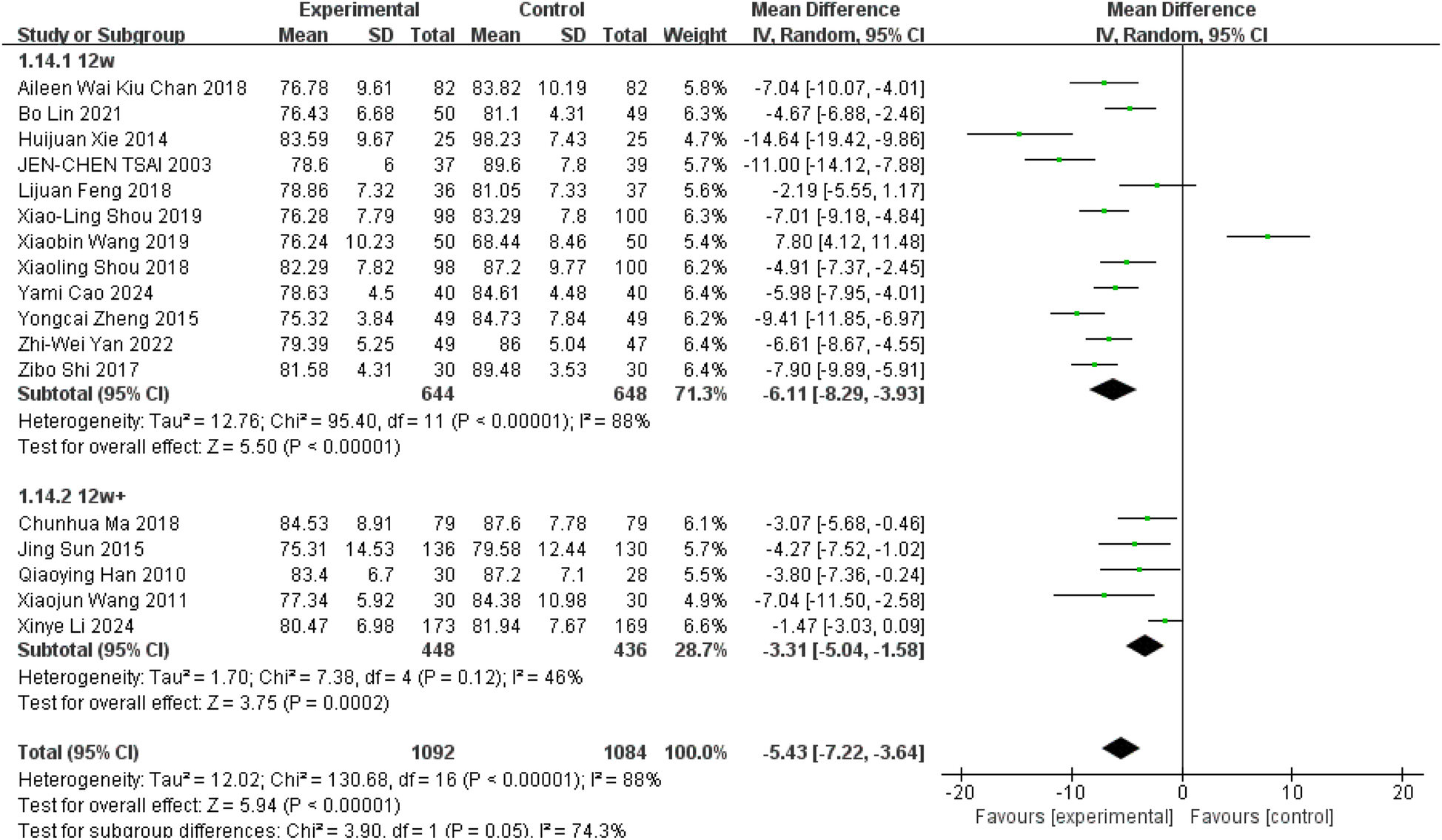
Effect of Tai Chi exercise on DBP levels in hypertensive patients (duration of intervention).
Subgroup analyses revealed a highly significant reduction in DBP among participants engaged in Tai Chi for 12 weeks compared to controls (Figure 6, WMD = −6.11; 95% CI = −8.29 to −3.93; Z = 5.50, P = 0.00001 < 0.05; I2 = 88%; Egger's test, P = 0.689 > 0.05). Additionally, Tai Chi participants demonstrated significantly lower DBP levels compared to controls over intervention durations exceeding 12 weeks (Figure 6, WMD = −3.31; 95% CI = −5.04 to −1.58; Z = 3.75, P = 0.0002 < 0.05; I2 = 46%; Egger's test, P = 0.005).
In studies examining the effects of Tai Chi on hypertension, these subtypes were used as grouping variables, classifying participants into Grade I and Grade II categories. Fourteen studies focused on Grade I hypertension showed that Tai Chi significantly reduced diastolic blood pressure (DBP) (Figure 7, WMD = −6.03; 95% CI = −7.59 to −4.46; Z = 7.53, P = 0.00001 < 0.05; I2 = 82%; Egger's test P = 0.092 > 0.05) (10, 11, 28, 30–32, 34–41). Similarly, three studies of class II hypertension showed that although Tai Chi was able to reduce diastolic blood pressure, the difference was not statistically significant (Figure 7, WMD = −1.87; 95% CI = −11.83 to 8.09; Z = 0.37, p = 0.71 > 0.05; I2 = 97%; Egger's test p = 0.35 > 0.05) (27, 29, 33).
Figure 7
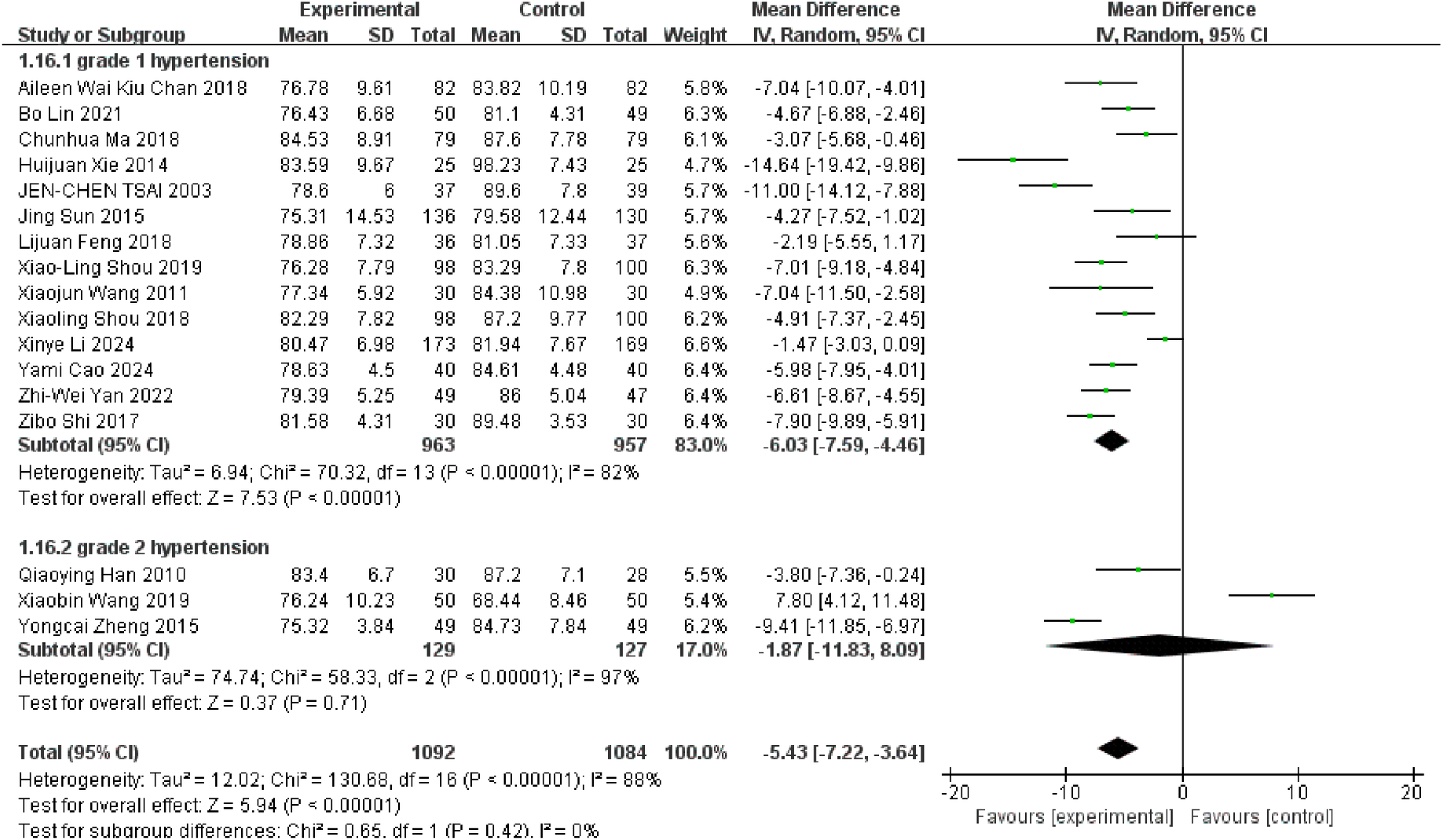
Effect of Tai Chi exercise on DBP levels in hypertensive patients (grade).
4.3 Tai Chi effects on TC
Six studies evaluated the effect of Tai Chi on TC levels (11, 27–29, 36, 37). The meta-analysis demonstrated that Tai Chi exercise significantly reduced TC levels compared to the control groups (WMD = −0.37; 95% CI = −0.62 to −0.12; Z = 2.91, P = 0.004 < 0.05; I2 = 76%; Egger's test, P = 0.213 > 0.05) (The chart is attached to the Supplementary Material). Using one-by-one elimination method, it is found that the source of heterogeneity is Aileen's research (37) (Figure 8, WMD = −0.51; 95% CI = −0.63 to −0.38; Z = 7.8, P = 0.00001 < 0.05; I2 = 36%; Egger's test, P = 0.377 > 0.05).
Figure 8
![Forest plot illustrating mean differences between experimental and control groups across six studies. Each study's mean difference is represented by a square, with lines indicating confidence intervals. The diamond at the bottom shows the overall effect size, favoring the experimental group with a mean difference of -0.51 and a 95% confidence interval of [-0.63, -0.38]. Heterogeneity is moderate, with I² at 36%.](https://www.frontiersin.org/files/Articles/1506912/xml-images/fcvm-12-1506912-g008.webp)
Forest plot comparing TC in Tai Chi and all controls.
4.4 Tai Chi effects on TG
These six studies reported participants' TG levels (11, 27–29, 36, 37). The meta-analysis revealed a notable decrease in TG levels among Tai Chi participants in comparison to the control group (Figure 9, WMD = −0.53; 95% CI = −0.89 to −0.16; Z = 2.83, P = 0.005 < 0.05; I2 = 94%; Egger's test, P = 0.606 > 0.05).
Figure 9
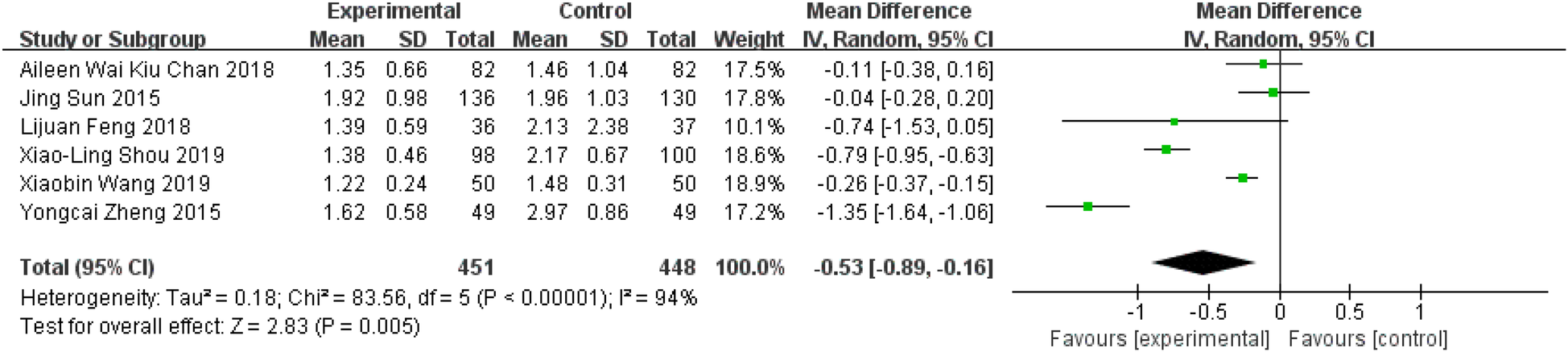
Forest plot comparing TG in TC and all controls.
4.5 Tai Chi effects on LDL
Six studies reported data on participants' LDL levels (11, 27–29, 36, 37). The meta-analysis showed that Tai Chi exercise had a highly significant effect on reducing LDL levels compared to the control group (Figure 10, WMD = −0.70; 95% CI = −1.12 to −0.28; Z = 3.24, P = 0.001 < 0.05; I2 = 97%; Egger's test, P = 0.522 > 0.05).
Figure 10
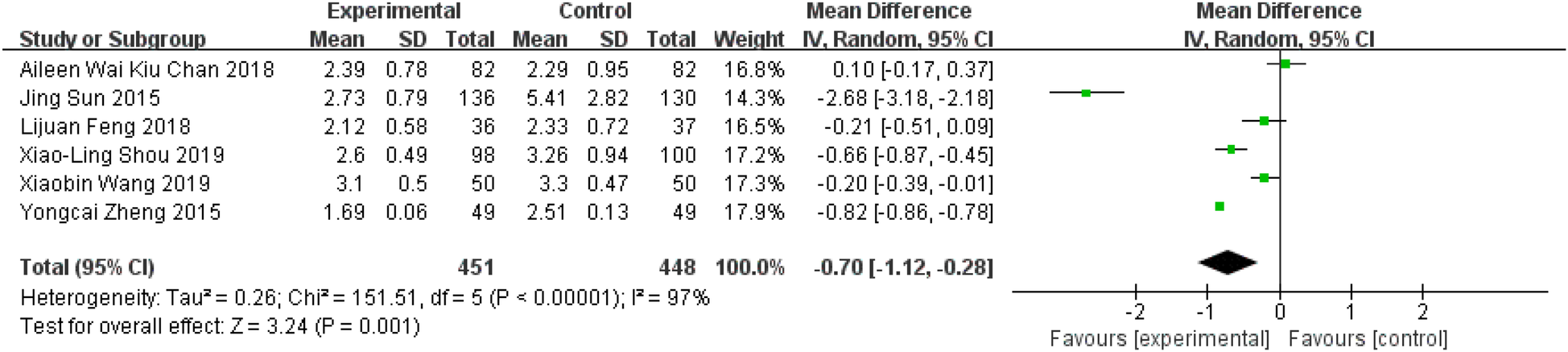
Forest plot comparing LDL in TC and all controls.
4.6 Tai Chi effects on HDL
Six studies reported data on participants' HDL levels (11, 27–29, 36, 37). The meta-analysis showed that participants in the Tai Chi exercise group exhibited non-significant improvements in HDL levels compared to the control group (Figure 11, WMD = −0.76; 95% CI = −1.84 to 0.32; Z = 1.38, P = 0.17 > 0.05; I2 = 100%; Egger's test, P = 0.089 > 0.05).
Figure 11
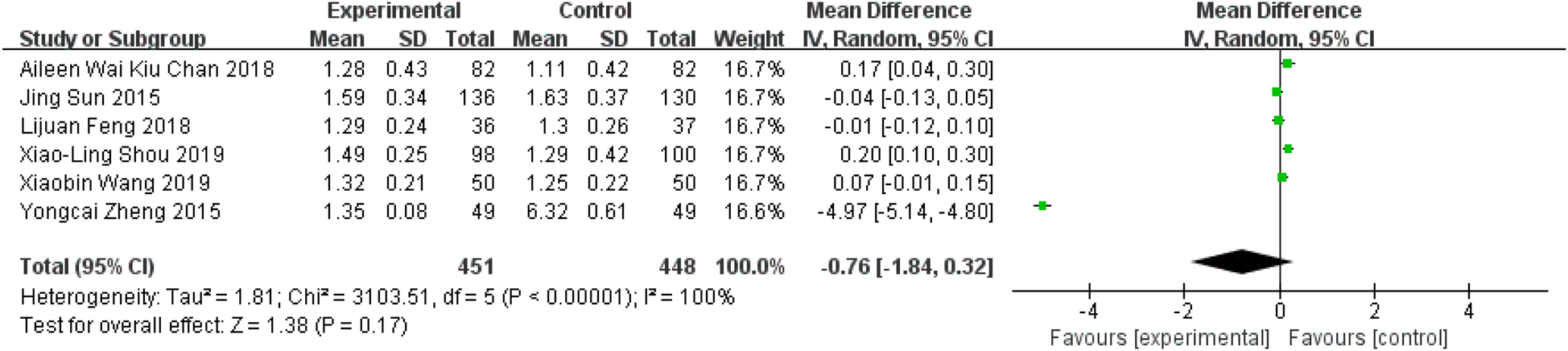
Forest plot comparing HDL in TC and all controls.
4.7 Tai Chi effects on BMI
A total of seven studies reported data on participants' BMI (10, 11, 36–40). The meta-analysis revealed that Tai Chi exercise did not have a statistically significant effect on BMI levels compared to the control group (Figure 12, WMD = 0.13; 95% CI = −0.65 to 0.90; Z = 0.32, P = 0.75 > 0.05; I2 = 86%; Egger's test, P = 0.626 > 0.05).
Figure 12
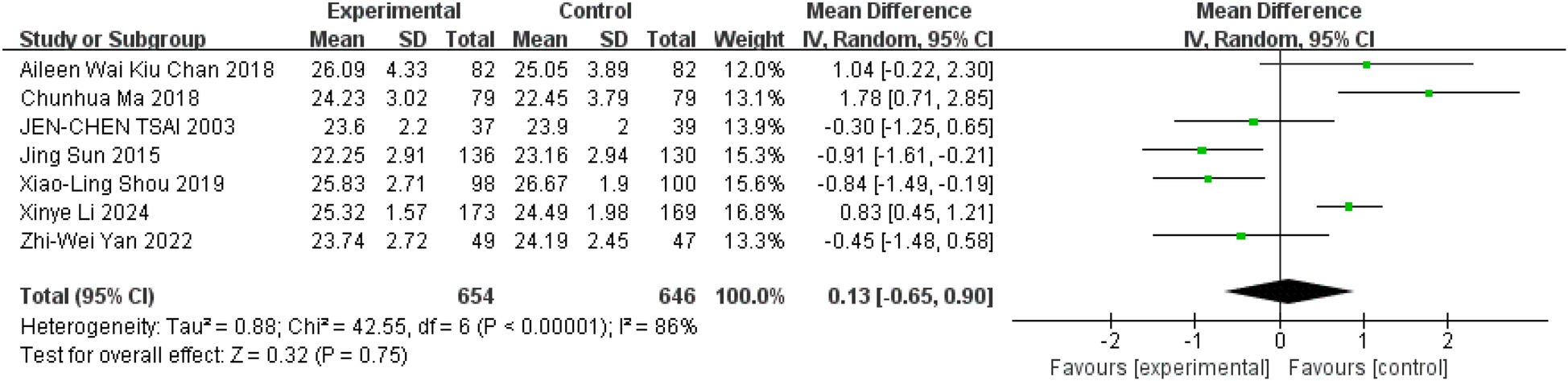
Forest plot comparing BMI in TC and all controls.
4.8 Tai Chi effects on WC
Four studies reported data on participants' WC levels (11, 37–39). The meta-analysis revealed that Tai Chi exercise did not significantly improve WC levels compared to the control group (WMD = −0.16; 95% CI = −2.88 to 2.57; Z = 0.11, P = 0.91 > 0.05; I2 = 87%; Egger's test, P = 0.656 > 0.05) (The chart is attached to the Supplementary Material). By means of one-by-one elimination method, it is found that the source of heterogeneity is Sun's research (11) (Figure 13, WMD = 1.43; 95% CI = 0.38 to 2.48; Z = 2.67, P = 0.008 < 0.05; I2 = 0%; Egger's test, P = 0.246 > 0.05).
Figure 13
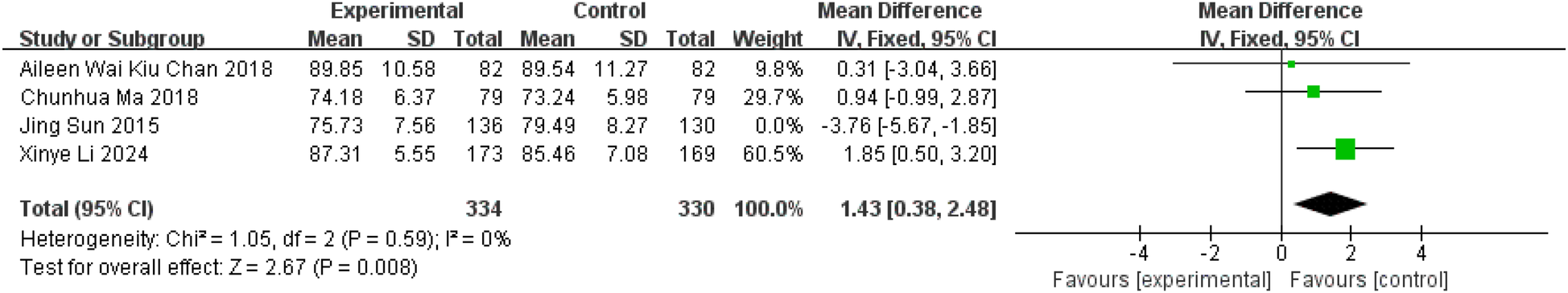
Forest plot comparing WC in TC and all controls.
5 Discussion
This systematic review examined randomized controlled trials (RCTs) investigating the effects of Tai Chi exercise on patients with essential hypertension, with separate subgroup analyses based on the duration of the intervention and the type of hypertension. The results indicated that practicing Tai Chi significantly reduced participants' blood pressure (SBP, DBP), and blood lipids (TC, TG, LDL). However, high density lipoprotein (HDL) and body mass index (BMI) did not change significantly, and waist circumference (WC) showed an increasing trend.
Hypertension is classified into essential and secondary types. Secondary hypertension arises due to specific underlying conditions and accounts for only a small percentage of hypertensive patients, while the majority of individuals with hypertension have primary hypertension (1). The pathogenesis of essential hypertension involves a complex interaction of genetic, environmental, and aging factors (43–45), which contribute to the development of the condition by disrupting the cardiovascular regulatory system. This disruption leads to increased vascular resistance (46), often accompanied by alterations in the renin-angiotensin-aldosterone system (RAAS) and the endothelin system (46–48). It is currently believed that nitric oxide (NO), synthesized and released by vascular endothelial cells, plays an important protective role in the cardiovascular system. NO helps maintain blood pressure, prevents endothelial damage, reduces blood viscosity, and decreases the formation of pathological blood clots and atherosclerotic plaques (49). The imbalance between NO and endothelin-1 (ET-1), along with the dysfunction of endothelium-dependent vasodilation caused by endothelial dysfunction, is a key mechanism in the development of hypertension (50, 51). Beyond these direct contributors, hypertension is also associated with other risk factors such as dyslipidemia, impaired glucose tolerance, and type 2 diabetes mellitus, which further elevate cardiovascular risk (52). The research reported a decrease in blood pressure values after Tai Chi intervention, which is consistent with the results of previous studies (53). Moreover, Subgroup analysis of different control measures (other exercise and medication) revealed that Tai Chi resulted in an average reduction of 4.51 mmHg in SBP compared to other exercises and 9.46 mmHg compared to medications (Supplementary Figure S16). Regarding DBP, Tai Chi led to an average reduction of 5.05 mmHg compared to other exercises and 5.61 mmHg compared to medications (Supplementary Figure S17). When patients with essential hypertension (EH) practice Tai Chi, its mechanisms of mind-quieting and body-relaxing, breathing and exhaling, and dantian drumming help one enter an alpha-wave state, achieve relaxation of the whole body and brain, reduce the patient's state of stress (54), regulate the autonomic nervous system, especially promote the dilatation of small arteries throughout the body, alleviate the sclerosis of the arterial walls by enhancing the activity of the parasympathetic nerves and decreasing sympathetic nervous tension, and increasing the release of NO, thereby reducing blood pressure (10, 54, 55). In addition, Tai Chi, as a group exercise, reduces stress and enhances emotional well-being through social support, which further contributes to the reduction of blood pressure (56).
Dyslipidemia are independent risk factors for hypertension, with studies showing that increased levels of TC, low-density lipoprotein cholesterol (LDL-C), and TG significantly increase the risk of hypertension (57, 58). Elevated levels of TC and TG contribute to atherosclerosis, a condition that leads to the hardening and thickening of the vessel walls, narrowing the lumen, and increasing peripheral resistance, ultimately resulting in elevated blood pressure (58). This study reports the decline of partial blood lipids function (TC, TG, LDL) after Tai Chi intervention. However, in contrast to previous studies (59), the impact of Tai Chi on HDL levels was not statistically significant. There was considerable variation in HDL outcomes across studies, with Zheng et al. reporting a decrease of 4.97 mmol/L in HDL levels (29). After excluding this outlier, the remaining studies showed an average increase of 0.235 mmol/L in HDL levels, though the change was not statistically significant. Overweight or obesity is directly linked to hypertension (60). Individuals with abdominal obesity are at a heightened risk of developing hypertension (61). BMI and WC are correlated with the prevalence of hypertension and can effectively predict its occurrence (62). The results of this study revealed that the effects of Tai Chi intervention on BMI and WC were contrary to those of previous studies (63, 64). Initially, the results of this study showed a slight decrease in WC levels, but the heterogeneity was relatively high. There may be considerable heterogeneity in the study by Sun et al. (11), which demonstrated a greater effect of Tai Chi exercise on WC compared to the other studies included in the analysis. After excluding this study, there was a general trend of elevated WC levels in hypertensive patients following Tai Chi intervention. Our findings show that Tai Chi practice has little effect on this, which could be due to not having good control of the diet (65), individual differences (66), or measurement bias (67).
Notably, the effect of Tai Chi practice was more pronounced at 12 weeks compared to long-term practice, though long-term practice still showed significant benefits when compared to the control group. This finding aligns with the minimum intervention duration (12 weeks) suggested by the 8th Joint National Committee study (68), and, in conjunction with our findings, underscores the importance of 12 weeks as a benchmark for the duration of effective Tai Chi intervention in patients with essential hypertension. It might because the 12-week intervention cycle brought the practice effect of Tai Chi to its peak. However, the effect of cycles over 12 weeks was still more effective than blank control group, but it was lower than the peak. This provides a basis for the fact that Tai Chi intervention for essential hypertension can take effect after 12 weeks. In addition, Tai Chi intervention was found to be more effective in patients with Grade 1 hypertension (P < 0.05) than in those with Grade 2 hypertension (P > 0.05), although the difference between the two groups was not statistically significant. The underlying mechanism may be related to the fact that Grade 1 hypertension can typically be managed through lifestyle changes, whereas Grade 2 hypertension often requires a combination of medications to effectively control blood pressure. In this study, participants continued their usual medication regimen, and the effect of Tai Chi on Grade 1 essential hypertension was more pronounced. However, while the intervention appeared to have a slight downward effect on Grade 2 hypertension, the result was not statistically significant and warrants further investigation in future studies. Wang's research showed opposite results to the other two studies. When Wang's study was excluded (27), Tai Chi showed similar effectiveness in both groups, with no significant difference between them. This may be due to the limited number of studies in the Grade 2 hypertension subgroup and the small sample size. This study demonstrated strong heterogeneity in several indicators such as SBP and DBP. After analyzing the original literature, it was found that this might be due to the duration, frequency, cycle of the intervention and the age of participants. The longest intervention period was as long as 5 years, and the shortest was 12 weeks. Each intervention lasted 30–90 min. The frequency was as high as 1–2 times a day and at least 3 times a week. The age range varied from 40 to 80 years old. Although these intervention level classifications have enriched our results to some extent, they inevitably have a certain impact on the reliability of the results. We have tried our best to eliminate this impact by using random effects models, sensitivity analysis and other methods. Therefore, it is suggested that a unified and standardized Tai Chi intervention plan should be established in future research. To enhance the validity and applicability of science.
Tai Chi may serve as both a physical and mental exercise. Through its unique mechanism of calming the mind and relaxing the body, it can stimulate the functions of internal organs, regulate qi, blood, and bodily fluids, and help the body achieve a state of relaxation and calmness. Additionally, it has been shown to reduce markers of oxidative stress (69), improve psychological well-being (70), lower blood lipid levels (71), and promote lipid metabolism (72), thereby stabilising blood pressure (73). However, the specific underlying mechanisms require further investigation.
6 Limitation
There exist several limitations in our investigation. Firstly, our meta-analysis revealed substantial heterogeneity across studies for several outcomes (I2 > 80%). We used the stepwise exclusion method and found that the heterogeneity was not caused by any single study. Furthermore, the randomisation procedures used in some of the studies were not publicly available, which may have led to selection bias. Third, because of the unique format of the Tai Chi exercise intervention, it was not possible to blind the assessors, which may have led to the presence of performance bias. Forth, the level of quality of the five studies included in the analysis could be considered “acceptable”, which may have influenced the results to some extent (Supplementary Figures S14, S15). Finally, the studies included were limited to English and Chinese literature, potentially introducing bias by excluding other languages. There were variations in the form, style, frequency, and duration of Tai Chi across the studies. It is suggested that a unified and standardized Tai Chi intervention plan should be established in future research. To enhance the validity and applicability of science.
7 Conclusion
This study systematically evaluated the effects of Tai Chi on blood pressure, blood lipids, and body composition in patients with essential hypertension, exploring its feasibility as a non-pharmacological treatment. The findings revealed that Tai Chi effectively lowers levels of SBP, DBP, TC, TG, and LDL. Its efficacy surpasses that of other exercise modalities, with the most pronounced improvements observed at the 12-week mark. In addition, it was observed that Tai Chi has a better blood pressure-lowering effect on grade 1 hypertension than on grade 2 hypertension. These findings support the use of Tai Chi as a scientifically validated exercise rehabilitation tool in clinical settings and suggest avenues for further research. Future research should address several priorities. Firstly, it is important to explore why three-month interventions are the most effective. Additionally, further research is needed to explore the effects of Tai Chi intervention on different stages of hypertension. This will help validate the findings and address potential bias in the results due to the limited literature on type 2 hypertension in this study. Secondly, large-scale randomized controlled trials should be conducted to develop standardized protocols, eliminating potential bias from variations in Tai Chi forms, styles, frequency, and duration. Thirdly, research should evaluate Tai Chi 's effectiveness across different populations and health conditions, with particular attention to cultural adaptation and acceptance for global implementation. Finally, more detailed studies are needed to explore whether the benefits of Tai Chi vary by gender and age group.
Statements
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Author contributions
JX: Data curation, Writing – original draft, Writing – review & editing, Software, Visualization. YH: Data curation, Software, Writing – review & editing, Writing – original draft. LL: Software, Validation, Writing – review & editing. JZ: Funding acquisition, Methodology, Writing – review & editing. CL: Supervision, Writing – review & editing. ML: Data curation, Visualization, Writing – review & editing. YM: Software, Writing – review & editing. JD: Project administration, Supervision, Writing – review & editing. SL: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was financially supported by the “Beijing Natural Science Foundation (7244482)” of JianweiZhang and the 2023 National General Administration of Sport Science and Technology Innovation Project “Research on the Development of a Tai Chi Health Intervention Programme and Its Mechanistic Effects on the Clinical Efficacy for Coronary Heart Disease Patients” of Shaojun Lyu.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1506912/full#supplementary-material
References
1.
Mancia G Kreutz R Brunström M Burnier M Grassi G Januszewicz A et al 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. (2023) 41(12):1874–2071. 10.1097/hjh.0000000000003480
2.
Mills KT Bundy JD Kelly TN Reed JE Kearney PM Reynolds K et al Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134(6):441–50. 10.1161/CIRCULATIONAHA.115.018912
3.
Arnett DK Blumenthal RS Albert MA Buroker AB Goldberger ZD Hahn EJ et al 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. (2019) 140(11):e596–646. 10.1161/CIR.0000000000000678
4.
Barkas F Sener YZ Golforoush PA Kheirkhah A Rodriguez-Sanchez E Novak J et al Advancements in risk stratification and management strategies in primary cardiovascular prevention. Atherosclerosis. (2024) 395:117579. 10.1016/j.atherosclerosis.2024.117579
5.
Wang Z Chen Z Zhang L Wang X Hao G Zhang Z et al Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. (2018) 137(22):2344–56. 10.1161/CIRCULATIONAHA.117.032380
6.
Zhang M Shi Y Zhou B Huang Z Zhao Z Li C et al Prevalence, awareness, treatment, and control of hypertension in China, 2004–18: findings from six rounds of a national survey. Br Med J. (2023) 380:e071952. 10.1136/bmj-2022-071952
7.
Lear SA Hu W Rangarajan S Gasevic D Leong D Iqbal R et al The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet (London, England). (2017) 390(10113):2643–54. 10.1016/S0140-6736(17)31634-3
8.
Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension-A report of the revision committee of Chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16(3):182–241. 10.11909/j.issn.1671-5411.2019.03.014
9.
Bu B Haijun H Yong L Chaohui Z Xiaoyuan Y Singh MF . Effects of martial arts on health status: a systematic review. J Evid Based Med. (2010) 3(4):205–19. 10.1111/j.1756-5391.2010.01107.x
10.
Tsai JC Wang WH Chan P Lin LJ Wang CH Tomlinson B et al The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. (2003) 9(5):747–54. 10.1089/107555303322524599
11.
Sun J Buys N . Community-based mind-body meditative Tai Chi program and its effects on improvement of blood pressure, weight, renal function, Serum lipoprotein, and quality of life in Chinese adults with hypertension. Am J Cardiol. (2015) 116(7):1076–81. 10.1016/j.amjcard.2015.07.012
12.
Zhang Q Xu X Wu Q Zhang J Huang S Wu L et al Effects of different traditional Chinese exercise in the treatment of essential hypertension: a systematic review and network meta-analysis. Front Cardiovasc Med. (2024) 11:1300319. 10.3389/fcvm.2024.1300319
13.
Rosado-Pérez J Ortiz R Santiago-Osorio E Mendoza-Núñez VM . Effect of Tai Chi versus walking on oxidative stress in Mexican older adults. Oxid Med Cell Longev. (2013);2013:298590. 10.1155/2013/298590
14.
Morawin B Tylutka A Chmielowiec J Zembron-Lacny A . Circulating mediators of apoptosis and inflammation in aging; physical exercise intervention. Int J Environ Res Public Health. (2021) 18(6):3165. 10.3390/ijerph18063165
15.
Lu WA Kuo CD . The effect of Tai Chi Chuan on the autonomic nervous modulation in older persons. Med Sci Sports Exerc. (2003) 35(12):1972–6. 10.1249/01.MSS.0000099242.10669.F7
16.
Pan X Zhang Y Tao S . Effects of Tai Chi exercise on blood pressure and plasma levels of nitric oxide, carbon monoxide and hydrogen sulfide in real-world patients with essential hypertension. Clin Exp Hypertens. (2015) 37(1):8–14. 10.3109/10641963.2014.881838
17.
Song Y Li J István B Xuan R Wei S Zhong G et al Current evidence on traditional Chinese exercises for quality of life in patients with essential hypertension: a systematic review and meta-analysis. Front Cardiovasc Med. (2021) 7:627518. 10.3389/fcvm.2020.627518
18.
Chen Z Li Q Xu T Zhou X Shu Y Guo T et al An updated network meta-analysis of non-pharmacological interventions for primary hypertension in adults: insights from recent studies. Syst Rev. (2024) 13(1):318. 10.1186/s13643-024-02744-5
19.
Zhang W Wang H Xiong Z Li C . Efficacy of Tai Chi exercise in patients with hypertension: systematic review and meta-analysis. Curr Probl Cardiol. (2024) 49(11):102798. 10.1016/j.cpcardiol.2024.102798
20.
Wang J Feng B Yang X Liu W Teng F Li S et al Tai Chi for essential hypertension. Evid Based Complement Alternat Med. (2013) 2013:215254. 10.1155/2013/215254
21.
Halperin RO Sesso HD Ma J Buring JE Stampfer MJ Gaziano JM . Dyslipidemia and the risk of incident hypertension in men. Hypertension. (2006) 47(1):45–50. 10.1161/01.HYP.0000196306.42418.0e
22.
Higgins JP Altman DG Gøtzsche PC Jüni P Moher D Oxman AD et al The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. 10.1136/bmj.d5928
23.
Sterne JAC Savovíc J Page MJ Elbers RG Blencowe NS Boutron I et al Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. 10.1136/bmj.l4898
24.
Qi F Soh KG Nasiruddin NJM Leong OS He S Liu H . Effect of Taichi Chuan on health-related physical fitness in adults: a systematic review with meta-analysis. Complement Ther Med. (2023) 77:102971. 10.1016/j.ctim.2023.102971
25.
Borenstein M Hedges LV Higgins JP Rothstein HR . A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1(2):97–111. 10.1002/jrsm.12
26.
Egger M Smith GD Schneider M Minder C . Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34. 10.1136/bmj.315.7109.629
27.
Wang X Ye L . The effect of 24-form simplified taijiquan on primary hypertension with mild anxiety state in the elderly. Fujian Tradit Chin Med. (2019) 50(4):73–5. 10.13260/j.cnki.jfjtcm.011881
28.
Feng L Li G Zhang D Ling Z Li M Jin R . Clinical effect assessment of 24-Simplified Taijiquan exercise on the antihypertensive effect of elderly patients with essential hypertension and on their blood lipid level. China Conv Med. (2018) 27(10):1009–13. 10.13517/j.cnki.ccm.2018.10.001
29.
Zheng Y Chen L Yang J . Taijiquan systematic reviews of primary effects on blood pressure and quality of life of patients with hypertension. J Liaoning Univ Tradit Chin Med. (2015) 17(04):143–6. 10.13194/j.issn.1673-842x.2015.04.050
30.
Huijuan X Caiqin B . Gaseous signal molecular mechanism of Taijiquan's intervention in aged essential hypertension. J Wuhan Sports Univ. (2014) 48(02):51–4. 10.15930/j.cnki.wtxb.2014.02.001
31.
Cao Y Mu R Zhou X Wang Q Wang F Wang J et al Clinical efficacy of Taichi Boxing on elderly patients with primary hypertension. Hebei Tradit Chin Med. (2024) 46(01):69–72. 10.3969/j.issn.1002-2619.2024.01.016
32.
Shou X Wang L Zhu L Ren A Wu W Xin S et al Effect of tai chi chuan on emotion and heart rate variability of in-service hypertension patients. China Modern Doctor. (2018) 56(29):95–9.
33.
Han QY Huang XF Li L Chen LQ . The effect of shadow boxing exercise on the long-term quality of life in middle-aged and elderly patients with primary hypertension. Chin J Mod Nurs. (2010) 16(14):1617–9. 10.3760/cma.j.issn.1674-2907.2010.14.002
34.
Wang XJ Li YJ Liu NN . Empirical study of Taijiquan interventions on the prevention and cure of Hypertension. J Beijing Sport Univ. (2011) 34(09):75–7. 10.19582/j.cnki.11-3785/g8.2011.09.020
35.
Shi Z Miao Z . Research on the treatment of grade 1 hypertension by traditional Chinese medicine sports therapy. Massage Rehabil Med. (2017) 8(20):51–2. 10.19787/j.issn.1008-1879.2017.20.026
36.
Shou XL Wang L Jin XQ Zhu LY Ren AH Wang QN . Effect of T'ai Chi exercise on hypertension in young and middle-aged in-service staff. J Altern Complement Med. (2019) 25(1):73–8. 10.1089/acm.2018.0011
37.
Chan AWK Chair SY Lee DTF Leung DYP Sit JWH Cheng HY et al Tai Chi exercise is more effective than brisk walking in reducing cardiovascular disease risk factors among adults with hypertension: a randomised controlled trial. Int J Nurs Stud. (2018) 88:44–52. 10.1016/j.ijnurstu.2018.08.009
38.
Ma C Zhou W Tang Q Huang S . The impact of group-based Tai Chi on health-status outcomes among community-dwelling older adults with hypertension. Heart Lung. (2018) 47(4):337–44. 10.1016/j.hrtlng.2018.04.007
39.
Li X Chang P Wu M Jiang Y Gao Y Chen H et al Effect of Tai Chi vs aerobic exercise on blood pressure in patients with prehypertension: a randomized clinical trial. JAMA Netw Open. (2024) 7(2):e2354937. 10.1001/jamanetworkopen.2023.54937
40.
Yan ZW Yang Z Yang JH Song CL Zhao Z Gao Y . Comparison between Tai Chi and square dance on the antihypertensive effect and cardiovascular disease risk factors in patients with essential hypertension: a 12-week randomized controlled trial. J Sports Med Phys Fitness. (2022) 62(11):1568–75. 10.23736/s0022-4707.22.13424-9
41.
Lin B Jin Q Liu C Zhao W Ji R . Effect and mechanism of Tai Chi on blood pressure of patients with essential hypertension: a randomized controlled study. J Sports Med Phys Fitness. (2022) 62(9):1272–7. 10.23736/s0022-4707.21.13394-8
42.
Boo S Yoon YJ Oh H . Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: a cross-sectional analysis. Medicine (Baltimore). (2018) 97(51):e13713. 10.1097/MD.0000000000013713
43.
Titze J Luft FC . Speculations on salt and the genesis of arterial hypertension. Kidney Int. (2017) 91(6):1324–35. 10.1016/j.kint.2017.02.034
44.
Kelly TN Sun X He KY Brown MR Taliun SAG Hellwege JN et al Insights from a large-scale whole-genome sequencing study of systolic blood pressure, diastolic blood pressure, and hypertension. Hypertension. (2022) 79(8):1656–67. 10.1161/hypertensionaha.122.19324
45.
Padmanabhan S Dominiczak AF . Genomics of hypertension: the road to precision medicine. Nat Rev Cardiol. (2021) 18(4):235–50. 10.1038/s41569-020-00466-4
46.
Oparil S Acelajado MC Bakris GL Berlowitz DR Cífková R Dominiczak AF et al Hypertension. Nat Rev Dis Primers. (2018) 4:18014. 10.1038/nrdp.2018.14
47.
Mancia G Grassi G . The autonomic nervous system and hypertension. Circ Res. (2014) 114(11):1804–14. 10.1161/CIRCRESAHA.114.302524
48.
Panza JA Casino PR Badar DM Quyyumi AA . Effect of increased availability of endothelium-derived nitric oxide precursor on endothelium-dependent vascular relaxation in normal subjects and in patients with essential hypertension. Circulation. (1993) 87(5):1475–81. 10.1161/01.cir.87.5.1475
49.
Wu Y Ding Y Ramprasath T Zou MH . Oxidative stress, GTPCH1, and endothelial nitric oxide synthase uncoupling in hypertension. Antioxid Redox Signal. (2021) 34(9):750–64. 10.1089/ars.2020.8112
50.
Ignarro LJ Cirino G Casini A Napoli C . Nitric oxide as a signaling molecule in the vascular system: an overview. J Cardiovasc Pharmacol. (1999) 34(6):879–86. 10.1097/00005344-199912000-00016
51.
Kohan DE . Endothelin-1 and hypertension: from bench to bedside. Curr Hypertens Rep. (2008) 10(1):65–9. 10.1007/s11906-008-0013-2
52.
Lu S Bao MY Miao SM Zhang X Jia Q-Q Jing S-Q et al Prevalence of hypertension, diabetes, and dyslipidemia, and their additive effects on myocardial infarction and stroke: a cross-sectional study in Nanjing, China. Ann Transl Med. (2019) 7(18):436. 10.21037/atm.2019.09.04
53.
Zhang P Zhang D Lu D . The efficacy of Tai Chi for essential hypertension: a systematic review and meta-analysis. Int J Nurs Pract. (2024) 30(2):e13211. 10.1111/ijn.13211
54.
Liu D Yi L Sheng M Wang G Zou Y . The efficacy of Tai Chi and Qigong exercises on blood pressure and blood levels of nitric oxide and endothelin-1 in patients with essential hypertension: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med. (2020) 2020:3267971. 10.1155/2020/3267971
55.
Korsager Larsen M Matchkov VV . Hypertension and physical exercise: the role of oxidative stress. Medicina (Kaunas). (2016) 52(1):19–27. 10.1016/j.medici.2016.01.005
56.
Liao SJ Tan MP Chong MC Chua YP . The impact of combined music and Tai Chi on depressive symptoms among community-dwelling older persons: a cluster randomized controlled trial. Issues Ment Health Nurs. (2018) 39(5):398–402. 10.1080/01612840.2017.1417519
57.
Otsuka T Takada H Nishiyama Y Kodani E Saiki Y Kato K et al Dyslipidemia and the risk of developing hypertension in a working-age male population. J Am Heart Assoc. (2016) 5(3):e003053. 10.1161/JAHA.115.003053
58.
Ruixing Y Jinzhen W Weixiong L Yuming C Dezhai Y Shangling P . The environmental and genetic evidence for the association of hyperlipidemia and hypertension. J Hypertens. (2009) 27(2):251–8. 10.1097/HJH.0b013e32831bc74d
59.
Alenazi AM Alshehri MM Hoover JC Yabroudi MA Kachanathu SJ Liu W . The effect of T'ai Chi exercise on lipid profiles: a systematic review and meta-analysis of randomized clinical trials. J Altern Complement Med. (2018) 24(3):220–30. 10.1089/acm.2017.0104
60.
Harsha DW Bray GA . Weight loss and blood pressure control (Pro). Hypertension. (2008) 51(6):1420–5. 10.1161/HYPERTENSIONAHA.107.094011
61.
Wang S Liu Y Li F Jia H Liu L Xue F . A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health. (2015) 15:7. 10.1186/s12889-014-1334-5
62.
Krakauer NY Krakauer JC . A new body shape index predicts mortality hazard independently of body mass index. PLoS One. (2012) 7(7):e39504. 10.1371/journal.pone.0039504
63.
Liu X Miller YD Burton NW Brown WJ . A preliminary study of the effects of Tai Chi and Qigong medical exercise on indicators of metabolic syndrome, glycaemic control, health-related quality of life, and psychological health in adults with elevated blood glucose. Br J Sports Med. (2010) 44(10):704–9. 10.1136/bjsm.2008.051144
64.
Chau JPC Leung LYL Liu X Lo SHS Choi KC Zhao J et al Effects of Tai Chi on health outcomes among community-dwelling adults with or at risk of metabolic syndrome: a systematic review. Complement Ther Clin Pract. (2021) 44:101445. 10.1016/j.ctcp.2021.101445
65.
Verheggen RJ Maessen MF Green DJ Hermus ARMM Hopman MTE Thijssen DHT . A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes Rev. (2016) 17(8):664–90. 10.1111/obr.12406
66.
Hui SS Xie YJ Woo J Kwok TC . Effects of Tai Chi and walking exercises on weight loss, metabolic syndrome parameters, and bone mineral density: a cluster randomized controlled trial. Evid Based Complement Alternat Med. (2015) 2015:976123. 10.1155/2015/976123
67.
Verweij LM Terwee CB Proper KI Hulshof CT van Mechelen W . Measurement error of waist circumference: gaps in knowledge. Public Health Nutr. (2013) 16(2):281–8. 10.1017/S1368980012002741
68.
James PA Oparil S Carter BL Cushman WC Dennison-Himmelfarb C Handler J et al 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) [published correction appears in JAMA. 2014 May 7;311(17):1809]. JAMA. (2014) 311(5):507–20. 10.1001/jama.2013.284427
69.
Chen SC Ueng KC Lee SH Sun KT Lee MC . Effect of T'ai Chi exercise on biochemical profiles and oxidative stress indicators in obese patients with type 2 diabetes. J Altern Complement Med. (2010) 16(11):1153–9. 10.1089/acm.2009.0560
70.
Wang C Bannuru R Ramel J Kupelnick B Scott T Schmid CH . Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Complement Altern Med. (2010) 10:23. 10.1186/1472-6882-10-23
71.
Lan C Chen SY Wong MK Lai JS . Tai Chi chuan exercise for patients with cardiovascular disease. Evid Based Complement Alternat Med. (2013) 2013:983208. 10.1155/2013/983208
72.
Yeh GY Wang C Wayne PM Phillips RS . The effect of Tai Chi exercise on blood pressure: a systematic review. Prev Cardiol. (2008) 11(2):82–9. 10.1111/j.1751-7141.2008.07565.x
73.
Guo Y Shi H Yu D Qiu P . Health benefits of traditional Chinese sports and physical activity for older adults: a systematic review of evidence. J Sport Health Sci. (2016) 5(3):270–80. 10.1016/j.jshs.2016.07.002
Summary
Keywords
Tai Chi, blood pressure, meta-analysis, exercise, public health, hypertension
Citation
Xu J, Huang Y, Li L, Zhang J, Li C, Liu M, Ma Y, Du J and Lyu S (2025) An RCT META analysis based on the efficacy of Tai Chi exercise therapy on blood pressure and blood lipids in patients with essential hypertension. Front. Cardiovasc. Med. 12:1506912. doi: 10.3389/fcvm.2025.1506912
Received
09 October 2024
Accepted
28 July 2025
Published
12 August 2025
Volume
12 - 2025
Edited by
Lanfranco D'Elia, University of Naples Federico II, Italy
Reviewed by
Alexandr Ceasovschih, Grigore T. Popa University of Medicine and Pharmacy, Romania
Qingguang Zhu, Shanghai University of Traditional Chinese Medicine, China
Updates
Copyright
© 2025 Xu, Huang, Li, Zhang, Li, Liu, Ma, Du and Lyu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Junming Du dujunming@pku.edu.cn Shaojun Lyu l13121860699@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.