Abstract
Introduction:
Inclusion Health (IH) encompasses individuals facing social exclusion, presenting a myriad of risk factors leading to compromised health. IH populations, including homeless individuals, substance abusers, and vulnerable migrants, have higher disease prevalence, earlier mortality, and more barriers to healthcare access, with increased risks of developing cardiovascular diseases. While QRISK3 is a validated tool for predicting ten-year cardiovascular risks in the general population in primary care, its application in secondary care or IH populations remains underexplored.
Methods:
This prospective study, conducted at University College London Hospital (UCLH) between December 2021 and December 2023, evaluated IH patients using a locally-developed Collaborative Holistic Inclusion Health Patient Assessment (CHIPA) tool, incorporating clinical scoring systems including QRISK3. QRISK3 scores and corresponding Q ages were calculated independently using its online platform, based on patient demographics, cardiovascular histories, and cholesterol levels. The CHIPA was a detailed medical and social history questionnaire used to evaluate the IH patients referred to IHT in a consistent manner, including the incorporation of questions related to QRISK3 and other scoring systems.
Results:
A total of 217 IH individuals were included in this study (median: 48 years; range: 25-81 years). Our IH patient cohort exhibited significantly higher QRISK3 scores compared to the general population (p < 0.001, paired Wilcoxon test), ranging from 0.1% to 81.7%, with an average increase of 8.6%. The corresponding Q age was, on average, 13 years older than patients' actual age, with a median of 62 years, and 35% of patients had a positive cardiovascular history. The relative risk ranged from 0.5 to 78.0, with an average of 4.0. Compared with the general population, IH patients demonstrated elevated cardiovascular risk.
Discussion:
We highlight the utility of QRISK3 and CHIPA tools in early cardiovascular risk identification within the Inclusion Health cohort of patients, facilitating timely interventions. Integrating clinical risk scores into holistic assessments can improve referral practices, potentially enhancing overall health outcomes and reducing mortality in IH patients.
1 Introduction
Inclusion Health (IH) is a comprehensive term denoting individuals subjected to social exclusion, often encountering a convergence of diverse risk factors contributing to compromised health, including economic deprivation, exposure to violence, stigma, and complex trauma (1). IH pertains to various marginalised groups, such as those facing homelessness, substance use, vulnerable migrants, Romani people and Traveller communities, sex workers, and individuals within the criminal justice system (2). These individuals exhibit significantly raised disease prevalence, spanning cardiovascular and respiratory conditions as well as infections and mental health disorders (3, 4). Their increased vulnerability to physical, mental health, and substance misuse is recognised as tri-morbidity, which is associated with markedly poorer health outcomes (5).
Conversely the IH population tend to encounter suboptimal healthcare with a lack of adherence to standard screening pathways. Barriers to healthcare include a combination of stigma, negative previous experiences of healthcare, a lack of flexibility from specialist services, mainstream services being unaware of or unable to meet Inclusion Health patient needs, Inclusion Health groups experiencing competing needs and priorities, and service fragmentation (6). Access to all community services necessitates proof of connection to a chosen locality, rendering it unattainable for individuals experiencing homelessness (6, 7). Barriers to primary and preventive care contribute to an increased frequency of medical emergencies and Emergency Departments (ED) attendances: Homeless individuals in England attend emergency departments three times more frequently than those without homelessness experiences, resulting in a four-fold risk of unplanned hospital admission and three times longer hospital stays (7–9).
A combination of increased health needs and reduced access to healthcare results in IH patients having markedly inferior health outcomes and higher mortality rates compared to the general population. In the UK, where the average life expectancy was 81.77 years in 2023, individuals experiencing homelessness and rough sleeping faced an average age of death as low as 43 years old for women and 45 years of age for men (1). The all-cause mortality was twelve times higher in females in IH groups and eight times higher in males, highlighting pronounced health disparities (3).
As a growing field IH medicine aims to address the social and health inequities that disproportionately affect marginalised populations. Its main goals are to draw emphasis to the extent and effects of extreme inequality, advocate for preventive and early intervention strategies, enhance access to essential services for individuals adversely affected by social exclusion, and make efforts to include the patients in the planning and implementation of their medical and social care (1).
In 2021 University College London Hospital (UCLH) launched the Inclusion Health Team (IHT), led by a consultant physician with a background in Infectious Diseases (ID) and General Internal Medicine (GIM). This was an initiative to provide comprehensive clinical assessments of IH inpatients and address the unmet health and social needs of the admitted IH patient population. The Collaborative Holistic Inclusion Health Patient Assessment (CHIPA) tool was developed to evaluate patients referred to the team. As part of this tool, the team incorporated existing frameworks and validated clinical scoring systems [QRISK3, FRAX, and the Malnutrition Universal Scoring Tool (MUST)] related to morbidity and mortality for comparative analysis with literature on the general population.
Given the challenges with arranging access to General Practice, scores like QRISK3 and FRAX were adopted to try and evaluate the chronic risks of common health problems, such as cardiovascular disease, in this population. The QRISK3 risk calculator is the standard care of risk tool for prediction of ten-year risk for cardiovascular events in England (10) and is validated in primary care among the general population. While individuals facing homelessness have an approximately three times greater risk of developing cardiovascular disease and heightened cardiovascular mortality (11), the use of QRISK3 in secondary care or in IH populations is poorly investigated.
This study aims to use the QRISK3 score to assess the cardiovascular risk in IH populations admitted to UCLH, compared to the general population. The objective is to contribute to the ongoing progress of IH medicine by highlighting the significance of cardiovascular risk assessment as a risk factor for early mortality. The study also aims to provide insights for the future enhancement of integrated treatment approaches tailored for IH groups, thereby addressing the unique healthcare needs of this population.
2 Materials and methods
This prospective single-centre study was conducted on IH patients referred to and seen by IHT at UCLH in London between December 2021 and December 2023. All patients had been admitted via the Emergency Department or Ambulatory Care Unit and were inpatients within UCLH. The study utilised the CHIPA framework developed within the multidisciplinary team, incorporating various history taking elements alongside clinical scoring systems. These included cognitive assessments (Abbreviated Mental Test Score – AMTS) and established tools such as QRISK3, FRAX, and MUST as surrogates for risk of morbidity and mortality. All patients provided consent for data collection. The only exclusions were based on age, the QRISK3 is not validated in patients less than 25 years of age for example, or lack of data (such as height and weight), as per the requirements to complete the QRISK3. As such we do not anticipate any bias from the perspective of the authors.
The QRISK3 scores utilised in our study were independently computed via the online tool available at https://qrisk.org/ and was not modified in anyway. Data was inserted into the QRISK3 calculator using components of each patient's past medical history, such as history of smoking, incorporated as standard into the CHIPA, up-to-date cholesterol to high density lipoprotein testing, acute blood pressure monitoring, and the patient's height and weight, along with their postcode if they had accommodation. The QRISK3 risk calculator was able to generate a percentage estimate of ten-year risk of heart attack or stroke, the equivalent percentage estimate of ten-year risk for a healthy person (defined as no adverse clinical indicators and a cholesterol ratio of 4.0, a stable systolic blood pressure of 125, and body mass index of 25) of the same age, sex, and ethnicity, a relative risk between the two percentage risks, and an estimated “healthy heart age” for the patient. The “healthy heart age”, or “Q age”, is defined as the age at which a healthy person of the same sex and ethnicity as an individual would be expected to have their equivalent 10-year QRISK3 score.
2.1 Patient and public involvement
Patients were not involved in the design and conduct of this research. During the feasibility stage priority of the research question, choice of outcome measures, and methods of recruitment were informed by discussions with patients during their admission with the IHT.
2.2 Statistical analysis
The estimated QRISK3 scores in the IH cohort and the expected QRISK3 scores from the general population were compared using paired t-tests and paired Wilcoxon test. A significance level of p < 0.05 was applied throughout.
3 Results
A total of 223 patients were identified and underwent a CHIPA consultation (Table 1). QRISK3 scores were successfully computed for 217 patients, with 1 patient excluded due to an absence of vital basic details such as height and weight and 5 patients excluded due to age below 25. Initial IH assessments were primarily conducted by IH consultants (72%), IH specialist nurses (24%), and doctors on consultant supervised “taster day” experiences (3.2%). The majority of patients were male (78%), with a median age at admission of 48 years and a mean age of 49 years (range from 25 to 84 years). The predominant ethnicity was UK born Caucasian (60%), and 98% of patients had no prior consultations with the IH physicians.
Table 1
| Age | Median: 48 years; range: 25–84 years | ||
|---|---|---|---|
| Gender | Male | 170 | 78% |
| Female | 47 | 22% | |
| Ethnicity | White United Kingdom | 131 | 60% |
| White Irish | 16 | 7% | |
| White Gypsy, Irish Traveller, or Roma | 3 | 1% | |
| Any other white background | 18 | 8% | |
| White and black Caribbean | 2 | 1% | |
| White and black African | 1 | 0% | |
| White and Asian | 2 | 1% | |
| Any other mixed or multiple ethnic background | 0 | 0% | |
| Indian | 3 | 1% | |
| Pakistani | 1 | 0% | |
| Bangladeshi | 1 | 0% | |
| Chinese | 3 | 1% | |
| Black African | 10 | 5% | |
| Black Caribbean | 2 | 1% | |
| Any other black, black British, or Caribbean | 10 | 5% | |
| Arab | 10 | 5% | |
| Any other | 4 | 2% | |
| IVDU | No | 204 | 94% |
| Active use | 11 | 5% | |
| Ex-user | 1 | 0% | |
| Skin-popping | 1 | 0% | |
| CADU | No | 181 | 83% |
| Yes | 36 | 17% | |
| Alcohol misuse | No | 177 | 82% |
| Yes | 40 | 18% | |
| Alcohol/Other withdrawal | No | 193 | 89% |
| Yes | 14 | 6% | |
| Suspected | 6 | 3% | |
| Previous/risk | 4 | 2% | |
| Seen by IHT before | No | 212 | 98% |
| Yes | 5 | 2% | |
Patient demographics and clinical details upon referral.
IHT, Inclusion Health team; IVDU, intravenous drug user; CADU, crack cocaine users.
77 patients were identified as having a history of cardiovascular disease, with 34% having hypertension, 14% ischemic heart disease, and 9% atrial fibrillation (Table 2). The median QRISK3 score was 8.5%, with a mean of 13.7% ± 13.7% (standard deviation) (Figure 2). When compared to the general population, the expected QRISK3 scores at equivalent ages ranged from 0% to 33%, indicating statistically significant differences (p < 0.001, Wilcoxon signed rank test). Corresponding Q ages, based on observed QRISK3 scores in our patient cohort, were significantly higher than patients' actual ages (p < 0.001, Wilcoxon signed rank test) (Figure 1). The relative risk ranged from 1 to 78, with an average of 4 (Table 3; Figure 2).
Table 2
| Cardiovascular condition | Past medical history count (n = 77) | Presenting complaint count (n = 49) | |
|---|---|---|---|
| Atrial fibrillation | 7 | Arrythmia: 8 | |
| Bradyarrhythmia | 2 | ||
| Palpitations unknown cause | 1 | ||
| Tachyarrhythmia | 1 | ||
| Postural Tachycardia syndrome | 0 | ||
| Unspecified arrythmia | 1 | ||
| Congestive/left heart failure | 4 | Heart failure: Acute: 2 Acute on chronic: 3 |
|
| Right ventricular failure | 2 | ||
| Heart failure excluded on previous echocardiogram | 1 | ||
| Cardiomegaly | 1 | N/A | |
| Hypotension, including postural | 2 | ||
| Hypertension, including secondary causes | 26 | ||
| Complications of hypertension | 3 | ||
| Angina | 3 | 1 | |
| Ischemic heart disease | 11 | N/A | |
| Congenital heart disease | 2 | ||
| Previous cardiac arrest | 2 | ||
| Previous percutaneous coronary intervention | 1 | ||
| Previous valve surgery | 0 | ||
| Permanent pacemaker | 1 | ||
| Implantable cardioverter-defibrillator including removed as malfunctioning | 2 | ||
| Reveal device | 1 | ||
| Infective endocarditis (IE) | 1 (resolved) | 2 | |
| Septic emboli | 1 | N/A | |
| Pleural effusion | n/a | 4 | |
| Electrocardiogram (ECG) abnormalities | Prolonged QTc | 21 | |
| T wave inversion | 1 | ||
| Right bundle branch block | 2 | ||
| Possible acute coronary syndrome | 1 | ||
| Non-specific | 2 | ||
| Abnormal but unchanged from previous | 1 | ||
| Abnormal but likely spurious | 1 | ||
Cardiovascular history and presenting complaint.
QTc, QT corrected for heart rate.
Figure 1
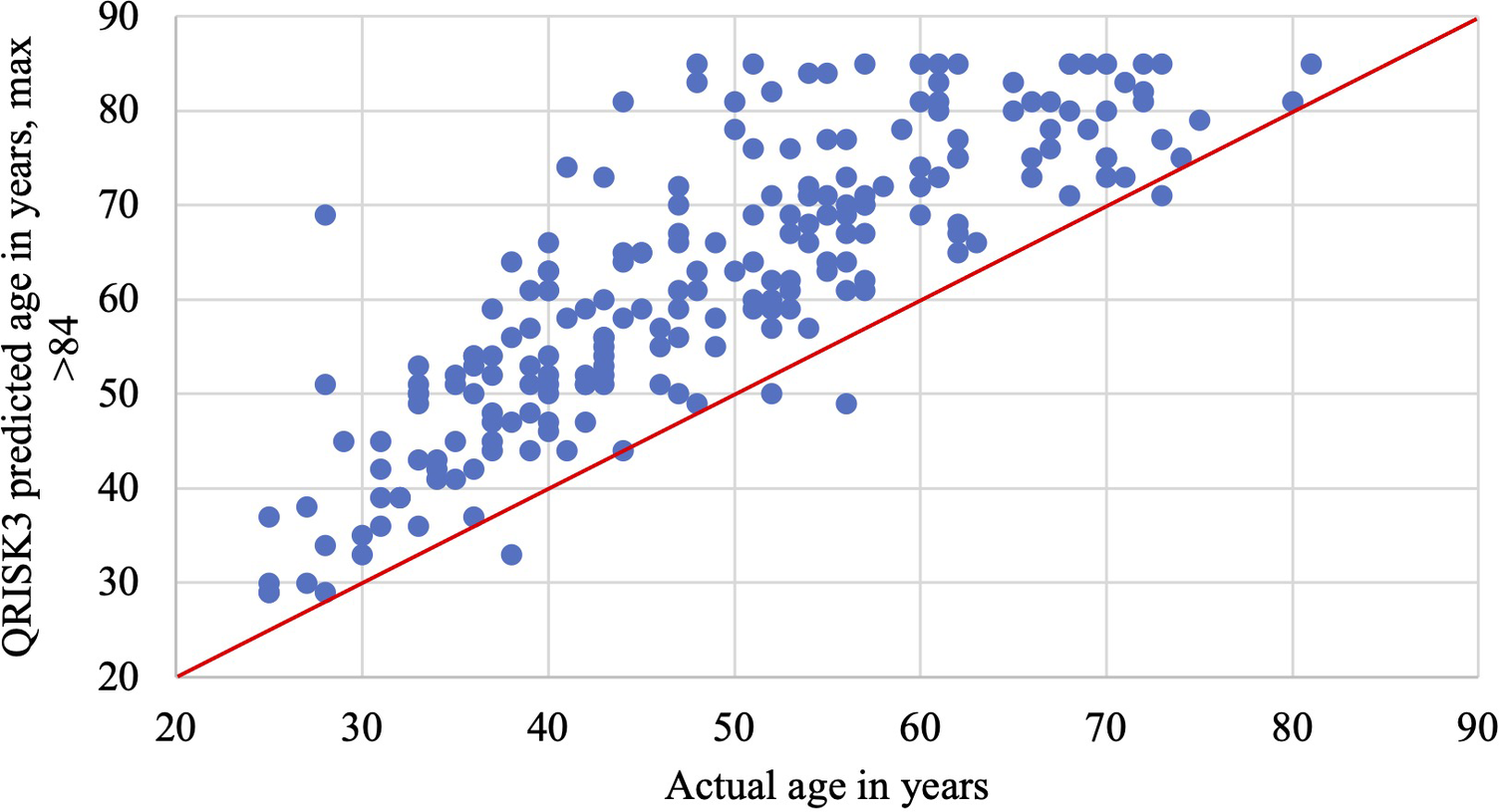
Age versus QRISK3 predicted age in years: the maximum QRISK3 predicted age is >84 years, which was recorded as 85 years on this graph.
Figure 2
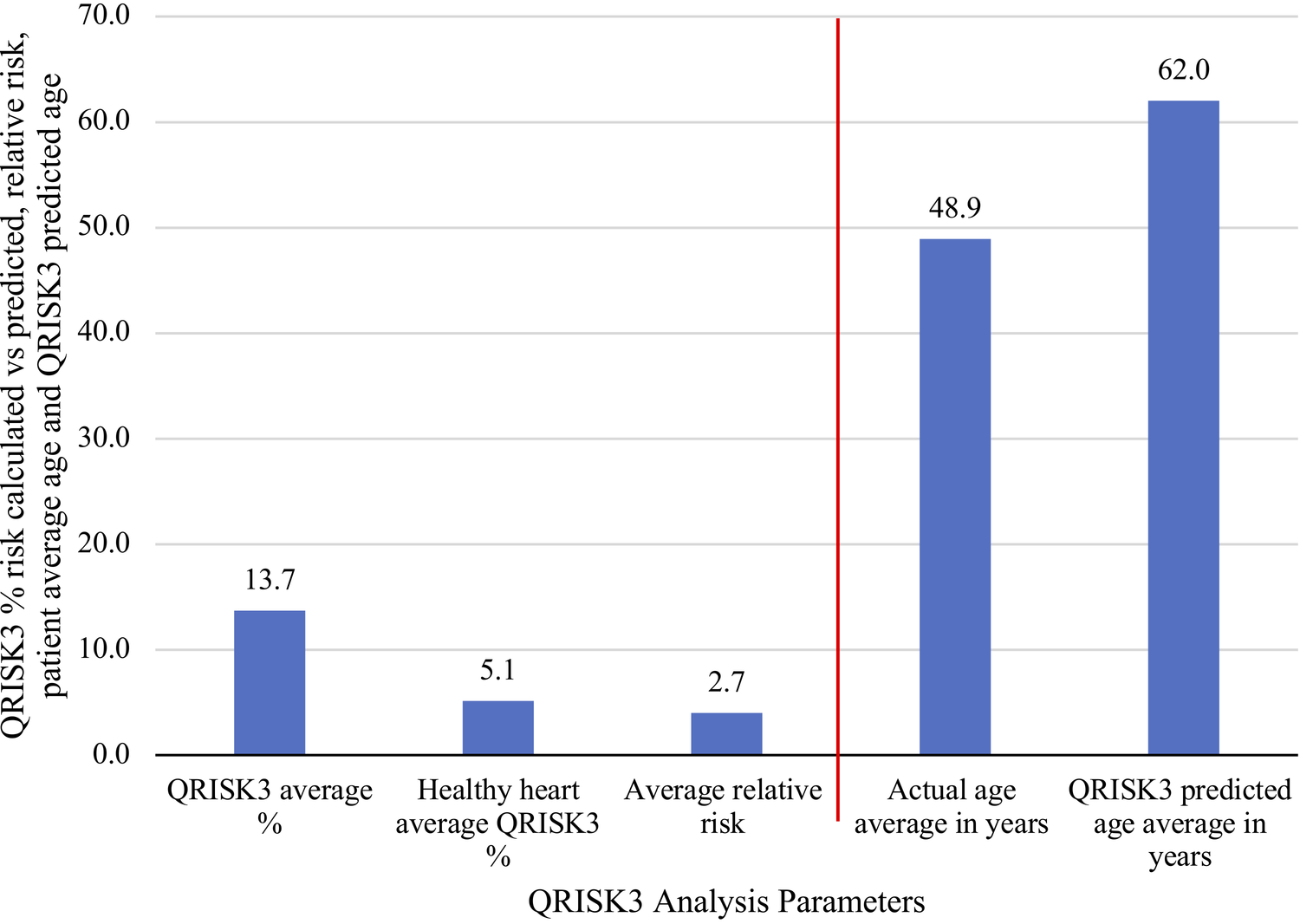
Comparing average results for QRISK3 analysis, including relative risk, versus patients’ average actual and predicted ages.
Table 3
| Metric | QRISK3% score | QRISK3 “healthy person” % risk | Actual age | QRISK3 ‘healthy heart’ age | Relative risk |
|---|---|---|---|---|---|
| Min | 0.1 | 0.1 | 25.0 | 29.0 | 0.5 |
| Max | 81.7 | 33.4 | 81.0 | 85.0 | 78.0 |
| Median | 8.5 | 2.9 | 48.0 | 63.0 | 2.7 |
| Mean | 13.7 | 5.1 | 49.1 | 62.0 | 4.0 |
| QRISK3% score thresholda | ≥7.5 | ≥10 | ≥20 |
| Count (%) | 117 (54%) | 96 (44%) | 55 (25%) |
QRISK3, Q age and relative risk.
aQRISK3% score thresholds indicate the percentage of patients with a 10-year cardiovascular risk at or above the specified cutoff (≥7.5%, ≥10%, ≥20%), calculated from the QRISK3 online tool: https://qrisk.org/. Higher thresholds reflect greater predicted cardiovascular risk.
Same admission follow-up with the IHT was conducted for 125 patients, and 31 patients passed away within the timeframe of the study, including 5 deaths during their admission when seen by IHT. The duration from the initial IHT review to death varied from 6 to 599 days, with an average of 274 days. The causes of death were predominantly unknown, although one patient experienced an out-of-hospital cardiac arrest. Within our patient cohort the mean age of death was 57 and the median was 59 (range 29–81). These findings underscore the diverse age range and complexities associated with mortality within the studied population. A single patient was identified as having had an inpatient non-ST elevation myocardial infarction (NSTEMI), a diagnosis made by the IHT. This patient was managed with percutaneous coronary intervention (PCI) at UCH's local tertiary referral centre, with a good outcome.
4 Discussion
Our study conducted a direct quantitative comparison of the cardiovascular risk within our IH patient cohort in relation to the general population, employing the QRISK3 score. Figure 2 summarises our primary take-home messages of this study. Notably IH patients seen by UCH IHT between December 2021 and 2023 demonstrated a median relative risk of 2.7 in developing cardiovascular events in the next ten years according to their QRISK3 scores, with a significant cardiovascular age discrepancy of 13 years when compared to the general population (Figure 2).
In the UK, where the average life expectancy was 81.77 years in 2023, individuals experiencing homelessness and rough sleeping faced an average age of death as low as 43 years for women and 45 years for men (1). Our study revealed a comparable mean age of death at 57 years for our cohort of IH patients admitted to UCH within the timeframe of the study. Despite the small size of the death cohort and the predominantly unclear causes of death, this observed heightened cardiovascular risk within the IH population raises concerns about its potential contribution to premature mortality. Indeed, other studies have found cardiovascular disease as an important contributor to excess morbidity and mortality in Inclusion Health populations, including homeless populations, incarcerated populations, and people who use drugs (3, 12–14).
QRISK3 scoring provides a relative risk score that is benchmarked against the general population's heart disease risk and it is independent of current presenting complaint of the patient. It is worth considering its universal application for Inclusion Health patients during admission, given their known difficulties accessing and attending scheduled appointments in primary and secondary care. This approach may provide valuable insights into cardiovascular risk profiles, enabling proactive and targeted interventions to address the cardiovascular risks in this vulnerable population, from screening and preventive measures to acute and chronic management, incorporating early medical interventions and lifestyle modifications.
Data about individual types of cardiovascular disease (CVD) within the IH population remain limited. Our study demonstrated that one-third of our IH cohort had a cardiovascular history of hypertension, a condition which is typically managed in primary care settings to which many of these patients have limited access. For instance, homeless individuals and those with substance use disorders are less likely to engage with primary care services, leading to underdiagnosis and undertreatment of chronic conditions (15).
This lack of access to preventive care exacerbates the progression of modifiable risk factors such as hypertension and hyperlipidaemia, particularly when poorly controlled, compounding the overall risk burned in IH populations. This underscores the need for further observational and interventional studies on CVD in the IH population to inform the development of dedicated IH teams, mobile healthcare units, and tailored care pathways and programmes (11, 16), especially in the community.
Further research is also required to determine whether specific CVD types are disproportionately prevalent in IH populations and whether social determinants of health further modify their risk profiles. For example there is limited data on the effects of lifestyle associated with IH populations, particularly related to diet and street drug use, and the effects these might have on long term cardiac and other risk factors. Using these current data as a benchmark, with ongoing review of the selected patients going forwards, we hope to cast some light on this area in the future. We also look at a broader IH population, compared to other studies that are focussed exclusively on homeless patients, for example.
Our study had also identified prolonged QTc intervals as the most common ECG abnormality observed in our IH patient cohort. Prolonged QTc is a known risk factor for ventricular arrhythmias and sudden cardiac death, and studies suggest that it may serve as an independent predictive marker for cardiovascular mortality (17, 18), particularly in vulnerable populations with underlying risk factors such as illicit drug use and electrolyte imbalances. Given that nearly all ED patients undergo ECG upon admission, further research is warranted to determine whether QTc prolongation represents an independent, early cardiovascular risk marker in the IH population. Monitoring of these patients QTc is also important given many patients will be started on methadone during their admission, which is known to prolong the Q interval (19).
Our study is subject to limitations. The QRISK3 score is validated for the general population in primary care settings (10) whereas the study group is an inpatient population who are therefore more likely to have cardiovascular diseases regardless of their IH health status. Therefore we are limited in the interferences we can make from this data. Additionally, while the QRISK3 score accounts for several risk factors, potential confounding variables such as socioeconomic status, access to healthcare and lifestyle behaviours, for example smoking, alcohol use and substance misuse, likely contribute to the observed elevated cardiovascular risk scores (20) and are not part of the QRISK3 scoring. Previous studies have illustrated that social determinants of health, including unstable housing, fuel poverty and financial insecurity, significantly influence cardiovascular outcomes (20, 21). This is reflected in the wide range of our relative risk (0.5–78), highlighting the heterogeneity of cardiovascular risk profiles among IH patients. Clinicians interpreting such broad relative risk ranges should consider both clinical risk factors and individual social circumstances when tailoring interventions.
Follow-up data was obtained for just over half of our patients and the follow-up period has been short. Achieving continuity in care is particularly challenging within the IH patient cohort, as primarily due to their challenges to accessing healthcare and common status of homelessness, preventing access to causes of death and further comprehensive cardiovascular risk assessment. Despite insights from reattendance data at our centre, undisclosed new admissions in other hospitals may introduce unexplored variables into our study. On top of this nonattendance, difficulty accessing healthcare, and a lower level of education among the participants may contribute to the masking of conditions such as diabetes, atrial fibrillation, silent myocardial infarction, and mental health problems. These factors could lead to an underestimation of our QRISK3 results, as these conditions may go unrecognised due to patient lifestyles and lack of awareness.
Notwithstanding these limitations our study has provided preliminary evidence affirming the significantly raised cardiovascular risks in IH patients, in keeping with previous literature. This underscores the utility of the QRISK3 and CHIPA tools in the assessment of IH patients upon admission, providing a holistic perspective. This proactive approach can enable clinicians to identify cardiovascular risks in IH patients at an earlier stage, presenting opportunities for timely and preventive interventions, for example antihypertensives or lipid-lowering therapies, as well as referrals to preventive cardiology services. This has the potential to save both time and costs associated with managing more complex medical issues that may otherwise arise at later stages. Furthermore, the incorporation of clinical risk scores, including QRISK3, within the CHIPA tool, could prompt and facilitate improved referral and engagement with appropriate community services for IH patients at an earlier stage, thereby increasing patient awareness. Such considerations may contribute to enhancing overall health outcomes and potentially reducing mortality in IH patients. Further research should explore the long-term effectiveness of such interventions in reducing cardiovascular events and mortality in IH populations with larger sample size. Additionally, alternative cardiovascuarl risk stratification tools, such as the Framingham risk score (22), Systematic COronary Risk Evaluation 2 (SCORE2) (23), Revised Pooled Cohort Equations (RPCE) (24), and World Health Organization cardiovascular disease (WHO CVD) (25) models may also be used in parallel to optimise risk assessment strategies in this high-risk population.
5 Conclusion
In conclusion our study has demonstrated that the IH patient cohort exhibits significantly higher QRISK3 scores, suggesting an advanced cardiovascular age compared to the general population, with a markedly elevated risk of detrimental cardiac events. The use of QRISK3 and CHIPA tools has the potential to facilitate improved referral practices and early interventions, offering opportunities for enhancing overall health outcomes in IH patients.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval was not required for the studies involving humans because our study is a prospective quality improvement project, therefore ethical approval from a board or committee was not required. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YG: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. JN: Conceptualization, Data curation, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
A national framework for NHS – action on inclusion health. NHS England accessed 26 October, 2023. Available at:https://www.england.nhs.uk/long-read/a-national-framework-for-nhs-action-on-inclusion-health/(Accessed January 29, 2024).
2.
Core20PLUS5 (adults) – an approach to reducing healthcare inequalities. NHS England. https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/(Accessed January 26, 2024).
3.
Aldridge RW Story A Hwang SW Nordentoft M Luchenski SA Hartwell G et al Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. (2018) 391(10117):241–50. 10.1016/S0140-6736(17)31869-X
4.
Lewer D Aldridge RW Menezes D Sawyer C Zaninotto P Dedicoat M et al Health-related quality of life and prevalence of six chronic diseases in homeless and housed people: a cross-sectional study in London and Birmingham, England. BMJ Open. (2019) 9(4):e025192. 10.1136/bmjopen-2018-025192
5.
Stringfellow EJ Kim TW Pollio DE Kertesz SG . Primary care provider experience and social support among homeless-experienced persons with tri-morbidity. Addict Sci Clin Pract. (2015) 10(1):A64. 10.1186/1940-0640-10-S1-A64
6.
Davies A Wood LJ . Homeless health care: meeting the challenges of providing primary care. Med J Aust. (2018) 209(5):230–4. 10.5694/mja17.01264
7.
Himsworth C Paudyal P Sargeant C . Risk factors for unplanned hospital admission in a specialist homeless general practice population: case-control study to investigate the relationship with tri-morbidity. Br J Gen Pract. (2020) 70(695):e406–11. 10.3399/bjgp20X710141
8.
Field H Hudson B Hewett N Khan Z . Secondary care usage and characteristics of hospital inpatients referred to a UK homeless health team: a retrospective service evaluation. BMC Health Serv Res. (2019) 19(1):857. 10.1186/s12913-019-4620-1
9.
Boobis DHaS. Unhealthy State of Homelessness 2022: Findings from the Homeless Health Needs Audit. Homeless Link. Available at:https://homeless.org.uk/knowledge-hub/unhealthy-state-of-homelessness-2022-findings-from-the-homeless-health-needs-audit/(Accessed April 18, 2024).
10.
Hippisley-Cox J Coupland C Brindle P . Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. Br Med J. (2017) 357:j2099. 10.1136/bmj.j2099
11.
Al-Shakarchi NJ Evans H Luchenski SA Story A Banerjee A . Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. (2020) 106(19):1483–8. 10.1136/heartjnl-2020-316706
12.
Wang EA Redmond N Dennison Himmelfarb CR Pettit B Stern M Chen J et al Cardiovascular disease in incarcerated populations. J Am Coll Cardiol. (2017) 69(24):2967–76. 10.1016/j.jacc.2017.04.040
13.
Lewer D Tweed EJ Aldridge RW Morley KI . Causes of hospital admission and mortality among 6683 people who use heroin: a cohort study comparing relative and absolute risks. Drug Alcohol Depend. (2019) 204:107525. 10.1016/j.drugalcdep.2019.06.027
14.
Aldridge RW Menezes D Lewer D Cornes M Evans H Blackburn RM et al Causes of death among homeless people: a population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Res. (2019) 4:49. 10.12688/wellcomeopenres.15151.1
15.
Fazel S Geddes JR Kushel M . The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. (2014) 384(9953):1529–40. 10.1016/S0140-6736(14)61132-6
16.
Luchenski S Maguire N Aldridge RW Hayward A Story A Perri P et al What works in inclusion health: overview of effective interventions for marginalised and excluded populations. Lancet. (2018) 391(10117):266–80. 10.1016/s0140-6736(17)31959-1
17.
Zhang Y Post WS Blasco-Colmenares E Dalal D Tomaselli GF Guallar E . Electrocardiographic QT interval and mortality: a meta-analysis. Epidemiology. (2011) 22(5):660–70. 10.1097/EDE.0b013e318225768b
18.
Straus SM Kors JA De Bruin ML van der Hooft CS Hofman A Heeringa J et al Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol. (2006) 47(2):362–7. 10.1016/j.jacc.2005.08.067
19.
Methadone: Interactions. National Institute for Health and Care Excellence. Available at:https://bnf.nice.org.uk/interactions/methadone/#:∼:text=Both%20Methadone%20and%20Amiodarone%20prolong,hypokalaemia)%20predispose%20to%20QT%20prolongation(Accessed April 11, 2025).
20.
Sorcha Daly JA . Voluntary Sector Action on the Social Determinants of Health - evidence review. Institute of Health Equity. Available at:https://www.instituteofhealthequity.org/resources-reports/voluntary-sector-action-on-the-social-determinants-of-health/voluntary-sector-action-on-the-sdoh-evidence-review.pdf(Accessed April 1, 2025).
21.
Marmot MAJ Boyce T Goldblatt P Morrison J . Health Equity in England: The Marmot Review 10 Years On. Institute of Health Equity. Available at:https://www.instituteofhealthequity.org/resources-reports/marmot-review-10-years-on/the-marmot-review-10-years-on-full-report.pdf(Accessed April 1, 2025).
22.
D'Agostino RB Sr Vasan RS Pencina MJ Wolf PA Cobain M Massaro JM et al General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation. (2008) 117(6):743–53. 10.1161/circulationaha.107.699579
23.
SCORE2 Risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. (2021) 42(25):2439–54. 10.1093/eurheartj/ehab309
24.
Yadlowsky S Hayward RA Sussman JB McClelland RL Min YI Basu S . Clinical implications of revised pooled cohort equations for estimating atherosclerotic cardiovascular disease risk. Ann Intern Med. (2018) 169(1):20–9. 10.7326/M17-3011
25.
Stephen K Lisa P Dirk DB Marie TC Maryam K Gretchen S et al World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health. (2019) 7(10):e1332–45. 10.1016/S2214-109X(19)30318-3
Summary
Keywords
Inclusion Health, QRISK3 scores, cardiovascular risk, CHIPA, marginalised populations
Citation
Gao Y and Norman J (2025) Evaluating cardiovascular risk in an Inclusion Health population admitted to secondary care. Front. Cardiovasc. Med. 12:1507029. doi: 10.3389/fcvm.2025.1507029
Received
14 October 2024
Accepted
05 May 2025
Published
16 May 2025
Volume
12 - 2025
Edited by
Rajeev Gupta, Spectrum Medical Center, United Arab Emirates
Reviewed by
Binaya Basyal, MedStar Washington Hospital Center, United States
Deepanjan Bhattacharya, All India Institute of Medical Sciences, India
TIa Bimal, Mount Sinai Hospital, United States
Updates
Copyright
© 2025 Gao and Norman.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yujia Gao yujia.gao.19@ucl.ac.uk
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.