- 1Health Management Center, Affiliated Hospital of Jiangsu University, Zhenjiang, China
- 2Department of Respiratory Medicine, Affiliated Hospital of Jiangsu University, Zhenjiang, China
- 3Cardiovascular Department, Affiliated Hospital of Jiangsu University, Zhenjiang, China
Background: Acute myocardial infarction remains a major contributor to global morbidity and mortality. Cardiac rehabilitation is widely recognized as an essential component of the comprehensive medical management for patients with ST-elevation myocardial infarction, especially among those who have undergone percutaneous coronary intervention. Adherence to cardiac rehabilitation encompasses patient collaboration with a healthcare provider, active involvement in the treatment regimen, and persistence in practice, characterized by self-efficacy and relapse prevention. Outpatient cardiac rehabilitation constitutes the second phase of the continuum of care, bridging the inpatient and long-term maintenance stages. However, adherence to outpatient cardiac rehabilitation programs in China remains suboptimal. The factors influencing outpatient cardiac rehabilitation in patients with ST-elevation myocardial infarction after percutaneous coronary intervention have not yet been fully elucidated.
Aims: To investigate the status and influencing factors of adherence to outpatient cardiac rehabilitation in patients with ST-elevation myocardial infarction after percutaneous coronary intervention one month after discharge in China and gain a deeper understanding of this phenomenon of interest.
Methods: An explanatory sequential mixed-methods design will be employed to conduct this study with three phases. The first phase is a quantitative study with a cross-sectional design to assess the level of adherence to outpatient cardiac rehabilitation and related influences based on the Health Belief Model among 198 patients with ST-elevation myocardial infarction after percutaneous coronary intervention in two tertiary hospitals in Zhenjiang, Jiangsu Province, China. The second phase is followed by a qualitative study to explore the patients’ perceived facilitators and barriers to adherence to outpatient cardiac rehabilitation. Purposive sampling, semi-structured interviews, and conventional content analysis approaches will be used to collect and analyze the data. The final phase links to integrating the data and developing a targeted strategy to improve adherence to outpatient cardiac rehabilitation among patients with ST-elevation myocardial infarction after percutaneous coronary intervention. The nominal group technique and "weaving techniques" will be implemented in accordance with the results of the preceding two phases.
Discussion: A targeted strategy to improve outpatient cardiac rehabilitation adherence would be designed considering the factors affecting adherence to outpatient cardiac rehabilitation in patients with ST-elevation myocardial infarction after percutaneous coronary intervention.
Clinical Trial Registration: This study has been registered in the Chinese Clinical Trial Registry: ChiCTR2400080035.
1 Background
Acute myocardial infarction (AMI) is a leading cause of global morbidity and mortality. In recent years, the incidence and mortality of AMI have steadily increased annually in most countries (1, 2). Traditionally, AMI has been classified into ST-elevation MI (STEMI) and non-ST-elevation MI (NSTEMI) (3). Survivors of AMI in Asian countries have relatively high mortality rates. In China, the mortality rates for hospitalization, 30-day, and 90-day were 4.0%, 5.9%, and 7.6%, respectively (4). AMI also entails a significant financial and social burden, such as missed work, prescription expenses, and hospital stay (5). Percutaneous coronary intervention (PCI) is the preferred treatment for AMI revascularization (6). An increase of 1% in PCI cases was associated with a 0.72% decrease in mortality rate (7). According to data from the Chinese National Center for Cardiovascular Quality Improvement, 86.8% of STEMI patients in tertiary hospitals had reperfusion, with emergency PCI accounting for 98.37% of cases (8). Nonetheless, the hospital mortality rate of patients with STEMI after PCI (STEMI-PCI) reached 5.3% in Shanghai (9, 10) and 26.08% in Hebei (11), and the 30-day mortality rate in Sichuan was 12.7% (12).
The American Heart Association (AHA) underscored the significance of cardiac rehabilitation (CR) in patients with AMI and demanded prompt attention to this worldwide issue (13). CR can be divided into three phases: inpatient, outpatient, and maintenance phase (13). In hospitalized and outpatient patients with recent myocardial infarction (MI), PCI, CABG, stable angina, and similar conditions, the AHA placed a strong emphasis on CR (14). The World Health Organization (WHO) defined “adherence” as “the extent to which a person's behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider” in 2003 (15). After that, scholars proposed a conceptual analysis and delineated “adherence to CR” as “patients' collaboration with a healthcare provider, active involvement in the treatment regimen, and persistence in practice characterized by self-efficacy and relapse-prevention” (16).
Numerous benefits have been empirically supported and thoroughly demonstrated (13, 17, 18). These benefits include cardiac risk prevention (19), reduction of cardiac and all-cause mortality rates by approximately 30% and 15% at 1-year follow-up (14), and improvement of quality of life (QoL) and negative emotions (14, 20). However, hospital-based CR participation rates among eligible outpatient patients globally remain at a low level of 10%–30%, due to obstacles such as low socio-economic position, accessibility, conflicting commitments, and cost (21). As a result, home-based CR has gained popularity in the UK, Canada, and Australia, and the adherence rate of STEMI-PCI patients to OCR has remained between 22% and 80% (22, 23). However, this situation is not optimistic in China. The adherence rate has only reached 7.05%–29.9% (24, 25), although the rate among inpatients was 72.74% (26). Chinese scholars have released a summary of multiple pieces of evidence related to CR (27, 28) and have suggested that patients in stable conditions can more flexibly switch to home-based CR from hospital- or center-based CR to improve adherence with appropriate self-monitoring methods.
Despite the general recognition of the benefits of CR adherence, dropout rates exceed 80% (29, 30). Numerous studies have shown a significant increase in the risk of death and MI when CR programs are not adhered to (13), and the influencing factors are multifactorial and individualistic (31). According to an Australian study, the factors included male sex, employment status, health support, shorter hospital stays, and previous AMI or PCI (23). However, in China, adherence was adversely correlated with age, male sex, hyperlipidemia, and D2B time, but positively connected to educational level and arrhythmia during PCI (25). Additional research has noted that adherence to OCR is statistically influenced by patient recognition (32), depression (33, 34), and self-efficacy (35, 36). Diabetes, smoking, and CR costs (22, 37) were all linked to poor OCR adherence. A qualitative study found that STEMI-PCI patients may not be able to recognize and manage ischemic symptoms immediately, may have psychological problems during the acute and recovery stages (38), as well as often overestimate their level of physical activity after discharged (39). More importantly, few studies have investigated effective strategies for improving the level of adherence to OCR in STEMI-PCI patients. The identification of both facilitators and obstacles to adherence to OCR and the mechanisms involved have not been evaluated.
The Health Belief Model (HBM) (40) is a theoretical framework designed to measure the motivations behind starting and continuing health behaviors. It considers demographic variables, psychological characteristics, patients' beliefs about their health, barriers and benefits for certain health behaviors, self-efficacy, and actions triggered by cues (41). HBM has been widely applied in behavioral prevention (42). Even so, no study has found how STEMI-PCI patients' health beliefs actively initiate health behaviors, how their views matter, or how they adhere to OCR. In addition, there are notable differences in the efficacy of influencing factors in different contexts (e.g., gender and social support) (43). Considering the significance and variances in culture, the economy, and society, an inclusive approach is required to address this issue. A mixed-methods design enables researchers to use a qualitative lens to explain the findings of quantitative results by exploring informants' perceptions in greater detail and, thus, a deeper understanding of the phenomenon than either method alone (44). Therefore, it is important and urgent to determine the level of adherence to OCR in STEMI-PCI patients and related influencing factors based on HBM. This will also serve as a basis for early identification and precise control to improve adherence to OCR, particularly in China.
1.1 Study aim
This study aims to identify the level and factors influencing adherence to home-based OCR in STEMI-PCI patients within one month after discharge and related influencing factors (quantitative phase), then explore the perceived facilitators and barriers of adherence to OCR (qualitative phase), and finally, gain a deeper understanding to develop target strategies to improve adherence to CR in China.
1.2 Specific objectives
1. Determining the level and factors influencing adherence to OCR among STEMI-PCI patients one month after discharge in two tertiary hospitals in Zhenjiang, Jiangsu Province, China.
2. Exploring perceived facilitators and obstacles of adherence to OCR among STEMI-PCI patients one month after discharge from two tertiary hospitals in Zhenjiang, Jiangsu Province, China.
3. Generating a deeper understanding of adherence to OCR in STEMI-PCI patients and developing targeted strategies to improve adherence to OCR.
1.3 Definition of terms for this study
Adherence to CR is the behavior of AMI-PCI patients who are actively involved in the home-based CR program after discharge. It will be measured using the Chinese version of the Adherence to Cardiac Rehabilitation Scale (C-ACRS), developed by Wen Xiaohui (45), which includes five dimensions: physician-prescribed exercise, medication management, nutrition management, cardiac risk factor modification, and psychological management.
2 Methods/design
2.1 Study design
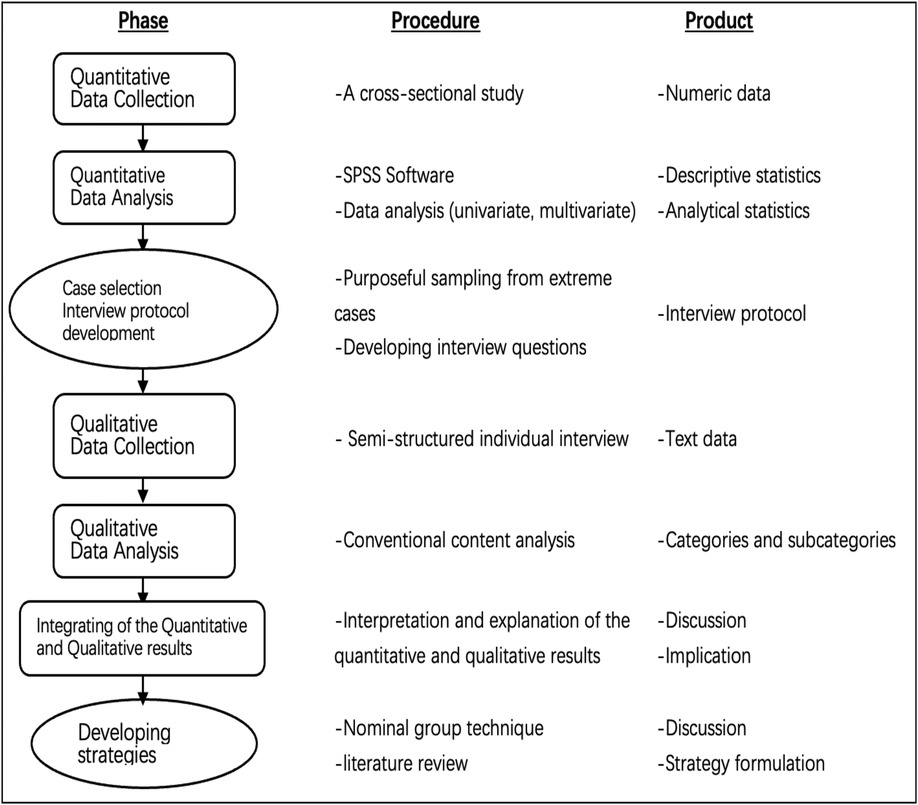
This study uses a sequential explanatory mixed-method approach for data collection, analysis, and integration of the quantitative and qualitative phases (Figure 1). Based on post-positivism, the mixed-method paradigm combines quantitative and qualitative methods to improve our understanding of OCR adherence in patients undergoing STEMI-PCI. Qualitative data will be expanded to quantitative data in the first phase, and both quantitative and qualitative data will be integrated subsequently. These findings will contribute to targeted strategies for improving adherence to OCR.
2.2 Phase one: quantitative study
Phase one is designed as a cross-sectional study that will be carried out to assess the level of adherence to OCR of STEMI-PCI patients one month after discharge from two tertiary hospitals in Zhenjiang, Jiangsu Province, China. Then, the impact of demographic variables, psychological characteristics, health beliefs, and adherence to OCR, as well as the related factors influencing adherence, will be investigated.
2.2.1 Sample size and sampling method
According to the suggestion of Nunnally and Bernstien, selecting 5–10 participants per item is appropriate for multivariate analysis (46) 165 participants will be recruited to unitize the factor analysis for the 33 items of the Scale of Adherence to Cardiac Rehabilitation scale (ACRS). Considering a follow-up attrition rate of 20%, this number will increase to 198.
Following the approval of the research project by the Ethics Committee of the two hospitals, the study will be conducted on 198 participants with AMI after PCI one month after discharge who receive home-based OCR. The researchers will visit two hospitals, identify eligible patients using the hospital information system (HIS) following the proportion (70% and 30%) of the target population in two hospitals, explain the study objectives and brief process to them, and obtain informed consent to participate. Patients will complete the Demographic Data Sheet (DDS).
2.2.2 Inclusion criteria
Patients who (1) are aged ≥18 years; (2) are diagnosed with AMI (I21of ICD-10 standard); (3) have received PCI; (4) participate in the home-based phase 2 CR; (5) can speak, read, and understand Mandarin; and (6) are willing to participate in this survey.
2.2.3 Exclusion criteria
Patients who (1) have complications from PCI and (2) participate in the phase 2 CR program in the hospital as outpatients will be excluded.
2.2.4 Research instrument
2.2.4.1 The demographic data sheet (DDS)
The researcher will develop a DDS, which will include two parts: demographic data, such as age, sex, marital status, educational level, employment status, and smoking status, and history of illness, such as diabetes, dyslipidemia, length of stay, D2B time, and arrhythmia during PCI. The DDS will be a form of open-ended and closed-ended questions.
2.2.4.2 The center for epidemiological studies depression scale (CES-D-S)
Feng et al. (47) developed a Chinese version of the CES-D-S to measure depression. This scale contains four dimensions with 10 items: physical factors, interpersonal relationships, negative emotions, and positive emotions. The I-CVIs ranged from 0.830–1.000, while the S-CVI was 0.86. CFA showed that the structural validity model achieved adaption (RMSEA <0.08, GFI and CFI >0.90, and CMIN/df <3) (47). Each item is rated on a 4 Likert scale from 0 to 3, with a total score range of 0–30 points. The higher the score, the more severe the depression.
2.2.4.3 The multidimensional scale of perceived social support (MSPSS)
The MSPSS evaluates perceived social support and was translated into Chinese by Chen et al. (48). The Chinese Version of the MSPSS has 12 items with three dimensions: family support, friend support, and other important support. The CFA of this scale supported a three-factor first-order model that fit well (RMSEA = 0.070, CFI = 0.941, and χ2/df = 2.753) (48). Each item is rated on a 7 Likert-type scale, where 1 means “strongly disagree,” and 7 means “strongly agree.” The total score ranges from 12 to 84 points. Higher scores represent higher perceived social support.
2.2.4.4 The coronary artery disease health belief scale (HBMS)
The HBMS was developed by Zhang et al. (49) in Chinese based on the HBM to assess patients' health beliefs related to behavior change. It contains five dimensions: perceived susceptibility, perceived seriousness, perceived benefit, perceived barriers, and cues to action. with 27 items. Eight common factors were extracted from the EFA of this scale, and the cumulative variance contribution rate was 60.698%. The correlation between the subscales and the total scale ranged from 0.811 to 0.876 (49). Each item was rated on a 5 Likert–type scale ranging from 1 (strongly disagree) to 5 (strongly agree). The total score ranged from 27 to 135. Higher scores indicate higher health beliefs.
2.2.4.5 The Chinese version of the cardiac self-efficacy scale (C-CSES)
The C-CSES was developed by Zhang et al. (50) and was translated from the CSEQ developed by Sullivan et al. (51) includes 13 items with three dimensions: control illness, control symptoms, and maintain function. The I-CVIs of this scale ranged from 0.81–0.96, while the S-CVI was 0.87. Confirmatory factor analysis (CFA) supported a three-factor high-order structure of the C-CSES with model fit indices: RMSEA = 0.084, CFI = 0.954, NNFI = 0.927, IFI = 0.954 and χ2/df = 2.572 (50). Each item was rated on a 5 Likert–type scale ranging from 0 (not at all) to 4 (completely confident). The total score ranged from 0 to 52 points. Higher scores indicate higher self-efficacy.
2.2.4.6 The scale of adherence to cardiac rehabilitation (ACRS)
The ACRS was developed by Wen, X.H. (52) based on quality interviews and literature reviews to assess adherence to CR in CHD patients. The ACRS contains 33 items with five subscales: exercise, medication, risk factors, nutritional, and psychological management. The I-CVIs of the scale ranged from 0.80–1.00, while the S-CVI was 0.96. The cumulative variance contribution rate was 60.698%, and the CFA showed good structural validity: X2 < 0.001, RMSEA = 0.055, CFI = 0.851 (52). The scale responds “yes” or “no” for each item (yes = 1 point, no = 0 points). The total score range of the scale is 0–33 points. The total score is classified into high and low: 33–25 points indicates high adherence to cardiac rehabilitation and 24–0 indicates low adherence to cardiac rehabilitation (45).
2.2.5 Data collection
This study will collect quantitative data using questionnaires. The following stages will be implemented to complete the data collection process.
(1) After obtaining permission from the directors of each hospital, the researcher will ask one research coordinator from the cardiac clinic of each hospital and a quiet, private room at the cardiac clinic to collect the form and questionnaires.
(2) The researcher will prepare 200 packages, each containing a form and five questionnaires, and explain the data collection process to the research coordinators.
(3) The researcher will obtain a list of STEMI PCI patients for follow-up at the outpatient department. The researcher will screen eligible patients and assign numerical codes to replace the patients' names. Subsequently, the researcher will provide a coded list to the research coordinators for subject selection.
(4) The research coordinator will schedule an appointment in advance for potential patients at the cardiac clinic after they meet the doctor and explain the study's purposes, procedures, duration, and benefits. If the subjects agree to participate, they will be requested to sign a consent form.
(5) The research coordinator distributes the research package to all participants. Each participant will spend 45–60 min completing the questionnaires and will then return the questionnaires and consent form separately in two designated boxes within the room. The research coordinator then checks for the completeness of all documents collected from the boxes and returns them to the researcher every week.
2.2.6 Data analysis
IBM SPSS 22.0 software will be used for data analysis. Statistical significance will be set at p < 0.05. The data analysis process was as follows:
The independent variables, including demographic variables, psychological characteristics, and the six constructs of the HBM, are described using frequency, percentage, mean, and standard deviation.
Dummy coding will be performed for categorical data. The assumption of logistic regression, including linearity, homoscedasticity, and residual normality, will be checked before entering the data into SPSS. Linearity: The partial regression plot between dependent and independent variables should be random. Homoscedasticity: Check the residual plot of the dependent variable; the scatter plot should be random without a curve pattern. Normality of residuals: Check the histogram of the dependent variable and a standard probability plot. Univariate analysis and binary logistic multivariate statistical analysis will be used to calculate the regression coefficient, odds ratio (OR), and 95% confidence interval of each variable using the stepwise entry method, and the independent risk factors related to adherence to home-based phase 2 CR will be analyzed.
2.3 Phase two: qualitative study
This phase consists of an exploratory qualitative study with conventional content analysis. Using this approach, perceived facilitators and obstacles to adherence to OCR will be investigated and explained.
2.3.1 Sampling method
Purposive sampling will be employed to explore patients' perceived facilitators and barriers to adherence to OCR within one month after discharge. Qualitative interviews were conducted after completion of the quantitative phase. Extreme cases on both sides of the overall ACRS score spectrum from phase one (the uppermost and lowermost 10% extreme scores of different subgroups of adherence) will be selected as participants in this phase.
2.3.2 Data collection
(1) Gaining access: The researcher will explain the purpose of the study to the directors of the selected hospitals to gain administrative permission and support.
(2) Recruiting informants: The researcher will communicate and invite potential informants to participate in the interview. Informants who are willing to participate and available for the time will be interviewed by the researcher. Usually, 20–30 patients of them are invited to participate in interviews. Purposive sampling will be used to recruit informants, some from the high-adherence group and others from the low-adherence group. The interview guide will design questions based on the quantitative study findings before the qualitative phase. The time will be set based on the agreement between the patients and the researcher.
(3) Data collection: Digital audio recorders were used during the interviews after obtaining verbal permission. The time for the interview will be 60–90 min.
(4) Establishing rapport and trust:
(a) The research coordinator will receive informants with greetings and help them be seated in a quiet private room for the interview in the cardiac clinic and introduce herself to the patients. The research objectives and research questions will be introduced, and patients will be asked to sign an informed consent form.
(b) Project posters will be placed to ensure that all informants understand the purposes and procedures.
(c) General questions of the informants will be asked before to increase their comfort and level of confidence among them. Then, the interview questions will be gradually raised according to the interview guidelines.
2.3.3 Data analysis
Qualitative data will be analyzed using a conventional content analysis approach, which is typically employed with a study design whose goal is to characterize a phenomenon when there is little current theory or research literature on a topic (53). Using this approach, data analysis begins by reading all the data repeatedly to achieve immersion and obtain a sense of the whole. The data were then read word by word to derive codes by first highlighting the exact words from the text to capture critical thoughts or concepts. Next, the researchers make notes of their first impressions, thoughts, and initial analysis. Following this, code labels appear, which are typically the original coding scheme and are frequently taken straight from the text. The researcher selects preliminary codes after open-coding three to four transcripts, which can then be applied to the remaining transcripts. When data do not fit into an existing code, new codes may be added. Consequently, the codes are grouped into categories that make sense. Based on their distinctions and commonalities, these codes are divided into main categories and subcategories. To interpret the underlying meaning, this method makes it possible to extract both manifest content and implicit context (54). The accuracy of the qualitative data will be assessed in this study using traditional criteria (Credibility, Dependability, Confirmability, Transferability) (55). NVivo software (version 12.0) will be employed to manage the interview data.
The “following a thread” method will be used to analyze the data. It begins by analyzing the data of each component to locate important conclusions and unanswered questions. Researchers refer to this as a thread when they take a category or theme from one component and follow it throughout others (56). “Extreme case analysis” is an additional method that involves identifying extreme cases by continuously analyzing datasets. High- and low-extreme cases will be used to demonstrate a substantial association between patients' health perceptions and adherence to OCR.
2.4 Phase three: integration and development
Conventional content analysis generally yields an interpretation that offers a comprehensive response to research questions while staying more in line with the phenomenon. Researchers must combine content categories to create a relevant panorama and cogent narrative to accomplish this in practice. It is critical to convey the intricacy of the facts within the larger narrative or interpretation. The key conclusions of both quantitative and qualitative data are presented side by side and narratively reported through “weaving techniques” in data integration. Together, these two sets of data can yield new insights and additional information through joint displays, which offer a deeper and more comprehensive explanation of participant responses and research problems (44).
The nominal group technique (NGT) will be used to develop appropriate strategies to promote adherence to OCR in patients undergoing STEMI-PCI. NGT is a structured group-based technique used to establish a consensus (57). Here's an overview:
• Expert session: We will convene a panel of cardiologists, CR specialists, general practitioners, cardiac nurses, nutritionists, and relevant stakeholders.
• Strategy presentation: We will introduce a set of proposed effective strategies derived from earlier research phases.
• Input collection: Participants and their families will be invited to provide feedback aimed at refining and prioritizing these strategies.
• Synthesis and refinement: The strategies will be further refined based on expert input to ensure they are evidence-based and effective.
3 Discussion
The main points of lowering the 30-day mortality rate of AMI-PCI patients after discharge and raising patient quality of life are adhering to CR. The causes of non-adherence or low adherence rates, however, are many and complex.
The level and indicators pertaining to adherence to OCR in STEMI-PCI patients should be determined to achieve this goal. This is the first study to examine the level and relevant factors impacting adherence to OCR in STEMI-PCI patents and to design targeted improvement strategies by exploring adherence to OCR using an explanatory sequential mixed-method. This study's design advances our knowledge of the variables that affect OCR adherence by supporting the integration of various viewpoints, strategies, and techniques in line with the principles of epistemological pluralism. To help STEMI-PCI patients achieve better health outcomes, the strategy suggested in this study may help increase awareness among CR providers and policymakers, particularly those pertaining to medical insurance.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the Affiliated Hospital of Jiangsu University (code number: KY2024K0103). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
WZ: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. HW: Conceptualization, Writing – review & editing. PL: Data curation, Formal analysis, Writing – review & editing. BW: Data curation, Formal analysis, Writing – review & editing. XW: Data curation, Formal analysis, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to acknowledge all participating medical staff of the Affiliated Hospital of Jiangsu University and Zhenjiang First People's Hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
STEMI, ST-segment evaluated myocardial infarction; PCI, percutaneous coronary intervention; ACRS, the adherence to cardiac rehabilitation scale; WHO, world health organization; AHA, American heart association.
References
1. Kim RB, Kim JR, Hwang JY. Epidemiology of myocardial infarction in Korea: hospitalization incidence, prevalence, and mortality. Epidemiol Health. (2022) 44:e2022057. doi: 10.4178/epih.e2022057
2. Sun XH, Duan HP, Yu CQ. Analysis on incidence, mortality and disease burden of acute myocardial infarction in Qingdao, 2014–2020. Chin J Epidemiol. (2023) 44(2):250–6. doi: 10.3760/cma.j.cn112338-20220825-00733
3. Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet. (2017) 389(10065):197–210. doi: 10.1016/S0140-6736(16)30677-8
4. Long Z, Liu W, Zhao Z, Tong S, Wang L, Zhou M, et al. Case fatality rate of patients with acute myocardial infarction in 253 chest pain centers—China, 2019–2020. China CDC Wkly. (2022) 4(24):518–21. doi: 10.46234/ccdcw2022.026
5. Bauersachs R, Zeymer U, Briere JB, Marre C, Bowrin K, Huelsebeck M. Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Ther. (2019) 2019:8295054. doi: 10.1155/2019/8295054
6. Khaled S, Ahmed WE, Shalaby G, Alqasimi H, Ruzaizah RA, Haddad M, et al. Disparities of demographics, clinical characteristics, and hospital outcomes of AMI pilgrims vs non-pilgrims-tertiary center experience. Egypt Heart J. (2020) 72(1):31. doi: 10.1186/s43044-020-00068-y
7. Krumholz HM, Normand ST, Wang Y. Twenty-year trends in outcomes for older adults with acute myocardial infarction in the United States. JAMA Netw Open. (2019) 2(3):e191938. doi: 10.1001/jamanetworkopen.2019.1938
8. Han YL. Clinical performance and quality measures for adults with acute ST-elevation myocardial infarction in China. Chin Circ J. (2020) 35(4):313–25. doi: 10.3969/j.issn.1000-3614.2020.04.001
9. Chen WS. Retrospective Analysis and Follow-up Study of Acute Myocardial Infarction Cases. Shanghai: Naval Medical University (2022).
10. Chen WX, Gu Y, Xiao YC, Zhao XX, Ma LP. Proportion and in-hospital mortality of hospitalized patients with ST-segment elevation myocardial infarction or non-ST-segment elevation myocardial infarction from 2007 to 2018. Acad J Second Mil Med Univ. (2020) 41(10):1053–61.
11. Wang Y, Wang W, Jia S, Gao M, Zheng S, Wang J, et al. Development of a nomogram for the prediction of in-hospital mortality in patients with acute ST-elevation myocardial infarction after primary percutaneous coronary intervention: a multicentre, retrospective, observational study in Hebei province, China. BMJ Open. (2022) 12(2):e056101. doi: 10.1136/bmjopen-2021-056101
12. Mo C, Cheng Y, Pan J, Tan K, Zhang X, Xu J. Association between hospital characteristics and 30-day mortality of patients hospitalized for acute myocardial infarction in Sichuan, China. J Evid Based Med. (2022) 15(3):236–44. doi: 10.1111/jebm.12491
13. Thomas RJ, Balady G, Banka G, Beckie TM, Chiu J, Gokak S, et al. ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association task force on performance measures. Circ Cardiovasc Qual Outcomes. (2018) 11(4):e000037. doi: 10.1161/HCQ.0000000000000037
14. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. (2017) 135(10):e146–603. doi: 10.1161/CIR.0000000000000485
15. Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization (2003).
16. Liu H, Tian X. Adherence—a concept analysis in the context of cardiac rehabilitation. TMR Integr Nurs. (2018) 2(1):12–7.
17. Abreu A, Mendes M, Dores H, Silveira C, Fontes P, Teixeira M, et al. Mandatory criteria for cardiac rehabilitation programs: 2018 guidelines from the Portuguese society of cardiology. Rev Port Cardiol. (2018) 37(5):363–73. doi: 10.1016/j.repce.2018.02.017
18. Ma J, Tai Y, Fan M, Wang Z. Cardiac rehabilitation of patients with acute ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention in a han population in northern China: a prospective cohort study. Int J Gen Med. (2021) 14:4959–65. doi: 10.2147/IJGM.S326725
19. Sjolin I, Back M, Nilsson L, Schiopu A, Leosdottir M. Association between attending exercise-based cardiac rehabilitation and cardiovascular risk factors at one-year post myocardial infarction. PLoS One. (2020) 15(5):e0232772. doi: 10.1371/journal.pone.0232772
20. Zheng X, Zheng Y, Ma J, Zhang M, Zhang Y, Liu X, et al. Effect of exercise-based cardiac rehabilitation on anxiety and depression in patients with myocardial infarction: a systematic review and meta-analysis. Heart Lung. (2019) 48(1):1–7. doi: 10.1016/j.hrtlng.2018.09.011
21. Santiago de Araujo Pio C, Chaves GS, Davies P, Taylor RS, Grace SL. Interventions to promote patient utilisation of cardiac rehabilitation. Cochrane Database Syst Rev. (2019) 2(2):CD007131. doi: 10.1002/14651858.CD007131.pub4
22. Sunamura M, Ter Hoeve N, Geleijnse ML, Steenaard RV, van den Berg-Emons HJG, Boersma H, et al. Cardiac rehabilitation in patients who underwent primary percutaneous coronary intervention for acute myocardial infarction: determinants of programme participation and completion. Neth Heart J. (2017) 25(11):618–28. doi: 10.1007/s12471-017-1039-3
23. Soo Hoo SY, Gallagher R, Elliott D. Predictors of cardiac rehabilitation attendance following primary percutaneous coronary intervention for ST-elevation myocardial infarction in Australia. Nurs Health Sci. (2016) 18(2):230–7. doi: 10.1111/nhs.12258
24. Xu L, Yang Y, Chen HF, Jiang M, Pu J. Study on influencing factors and effect evaluation of patients with acute myocardial infarction in the cardiac rehabilitation center. J Shanghai Jiaotong Univ. (2022) 42(5):646–52. doi: 10.5958/0976-5506.2019.00183.9
25. Ma JR, Yang YH, Zhang GY, Ying S. Current status of rehabilitation for acute ST-segment elevation myocardial infarction patients after percutaneous coronary intervention. J China Med Univ. (2021) 50(9):794–8.
26. Yan FJ, Song WX, Chen GL, Tang LX. The completion rate of phase I cardiac rehabilitation program and influencing factors of emergency PCI patients. Chin Nurs Manag. (2021) 21(11):1617–21.
27. Liu JT, Su H, Qin XJ. Guidelines on cardiac rehabilitation in patients with coronary heart disease: a systematic review. Chin Gen Pract. (2023) 26(19):2323–31. doi: 10.12114/j.issn.1007-9572.2022.0700
28. Tang YF, Huang YL, Gu ZJ, Hu XL, Gao CH, Mei KW. Evidence summary of management of cardiac rehabilitation compliance in patients with ischemic heart disease. Chin Nurs Manage. (2022) 22(8):1221–7. doi: 10.3969/j.issn.1672-1756.2022.08.021
29. Ruano-Ravina A, Pena-Gil C, Abu-Assi E, Raposeiras S, van ‘t Hof A, Meindersma E, et al. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J Cardiol. (2016) 223:436–43. doi: 10.1016/j.ijcard.2016.08.120
30. Armstrong MJ, Martin B-J, Arena R, Hauer TL, Austford LD, Stone JA, et al. Patients with diabetes in cardiac rehabilitation: attendance and exercise capacity. Med Sci Sports Exercise. (2014) 46(5):845–50. doi: 10.1249/MSS.0000000000000189
31. Resurreccion DM, Moreno-Peral P, Gomez-Herranz M, Rubio-Valera M, Pastor L, Caldas de Almeida JM, et al. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: a systematic review of prospective cohort studies. Eur J Cardiovasc Nurs. (2019) 18(1):38–47. doi: 10.1177/1474515118783157
32. Ghisi GL, Britto R, Motamedi N, Grace SL. Disease-related knowledge in cardiac rehabilitation enrollees: correlates and changes. Patient Educ Couns. (2015) 98(4):533–9. doi: 10.1016/j.pec.2014.12.001
33. Gostoli S, Roncuzzi R, Urbinati S, Morisky DE, Rafanelli C. Unhealthy behaviour modification, psychological distress, and 1-year survival in cardiac rehabilitation. Br J Health Psychol. (2016) 21(4):894–916. doi: 10.1111/bjhp.12204
34. Ghaffari S, Kolahdouzan K, Rahimi M, Tajlil A. Predictors of ST depression resolution in STEMI patients undergoing primary PCI and its clinical significance. Int J Gen Med. (2020) 13:271–9. doi: 10.2147/IJGM.S258573
35. Shajrawi AM, Al-Smadi AM, Ashour A, Momani A, Al-Akash HY, Granat M, et al. The impact of type of acute myocardial infarction on cardiac patient self-efficacy after hospitalization. Dimens Crit Care Nurs. (2022) 41(6):295–304. doi: 10.1097/DCC.0000000000000547
36. Shajrawi A, Granat M, Jones I, Astin F. Physical activity and cardiac self-efficacy levels during early recovery after acute myocardial infarction: a Jordanian study. J Nurs Res. (2021) 29(1):e131. doi: 10.1097/JNR.0000000000000408
37. Farah M, Abdallah M, Szalai H, Berry R, Lagu T, Lindenauer PK, et al. Association between patient cost sharing and cardiac rehabilitation adherence. Mayo Clin Proc. (2019) 94(12):2390–8. doi: 10.1016/j.mayocp.2019.07.018
38. Herawati T, Keliat BA, Waluyo A. Perceptions of self-care readiness among STEMI patients following primary PCI. Enfermería Clínica. (2019) 29:820–5. doi: 10.1016/j.enfcli.2019.04.123
39. Serves N, Pazart L, Gabriel D, Mourot L, Ecarnot F. Adherence to rehabilitation and home exercise after myocardial infarction: a qualitative study of expectations, barriers and drivers. BMC Sports Sci Med Rehabil. (2023) 15(1):98. doi: 10.1186/s13102-023-00714-3
40. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. (1974) 2(4):328–35. doi: 10.1177/109019817400200403
41. Abraham C, Sheeran P. The health belief model. Predicting Health Behav Res Pract Soc Cogn Models. (2015) 2:30–55.
42. Horwood H, Williams MJ, Mandic S. Examining motivations and barriers for attending maintenance community-based cardiac rehabilitation using the health-belief model. Heart Lung Circ. (2015) 24(10):980–7. doi: 10.1016/j.hlc.2015.03.023
43. Sun L, Wu T, Zhang M, Huang S, Zeng Z, Wu Y. Investigation on family support system and willingness of patients to participate in cardiac rehabilitation after percutaneous coronary intervention. Evid Based Complement Alternat Med. (2022) 2022:3633188. doi: 10.1155/2022/3633188
44. Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. (2013) 48(6 Pt 2):2134–56. doi: 10.1111/1475-6773.12117
45. Wen XH. Preliminary Construction and Validation of Cardiac Rehabilitation Compliance Prediction Model for Patients with Coronary Heart Disease. Hunan Province: University of South China (2023).
46. Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. (1995) 7(3):286–99. doi: 10.1037/1040-3590.7.3.286
47. Feng X, Guo LN, Liu K. Reliability and construct validity of cut version of center for epidemiological studies depression scale (CES-D) in community elderly population. China J Mod Med. (2016) 26(10):133–7. doi: 10.3969/j.issn.1005-8982.2016.10.029
48. Chen Y, Ma HM, Chen Z, Jia YL, Wang X, Chen JJ. Reiiabiiity and vaIidity of Chinese version of muItidimensionaI ScaIe of perceived sociaI support in eIderIy peopIe with chronic diseases. J Nurs. (2018) 25(18):5–8. doi: 10.16460/j.issn1008-9969.2018.18.005
49. Zhang M, Wang YX, Jin CD. Coronary artery disease health belief scale: develop and testing of reliability and validity. Chin J Prac Nurs. (2014) 30(29):40–3. doi: 10.3760/cma.j.issn.1672-7088.2014.29.013
50. Zhang X, Zhan Y, Liu J, Chai S, Xu L, Lei M, et al. Chinese Translation and psychometric testing of the cardiac self-efficacy scale in patients with coronary heart disease in mainland China. Health Qual Life Outcomes. (2018) 16(1):43. doi: 10.1186/s12955-018-0872-4
51. Sullivan MD, LaCroix AZ, Russo J, Katon WJ. Self-efficacy and self-reported functional status in coronary heart disease: a six-month prospective study. Psychosom Med. (1998) 60(4):473–8. doi: 10.1097/00006842-199807000-00014
52. Wen XH, Zhang Q, Cui X, Tian DD, Liu MQ, Liu YT, et al. Development of an adherence of cardiac rehabintation assessment scale in patients with coronary heart disease based on the delphi method. Chin J Rehab Med. (2023) 38(3):348–55. doi: 10.3969/j.issn.1001-1242.2023.03.011
53. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15(9):1277–88. doi: 10.1177/1049732305276687
54. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. (2004) 24(2):105–12. doi: 10.1016/j.nedt.2003.10.001
55. Holloway G. Qualitative Research in Nursing and Healthcare. 4th edn. United Kingdom: Library of Congress Cataloging-in-Publication Data (2016).
56. O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. Br Med J. (2010) 341:1147–50.
Keywords: adherence, cardiac rehabilitation, health belief model, acute myocardial infarction, percutaneous coronary intervention, mixed-methods study
Citation: Zhang W, Wang H, Li P, Wu B and Wang X (2025) Adherence to outpatient cardiac rehabilitation and related factors in STEMI after PCI in China: a sequential explanatory mixed method study protocol. Front. Cardiovasc. Med. 12:1542942. doi: 10.3389/fcvm.2025.1542942
Received: 15 February 2025; Accepted: 21 July 2025;
Published: 5 August 2025.
Edited by:
Georgios A. Christou, University of Ioannina, GreeceReviewed by:
Simona Minardi, University of L'Aquila, ItalyAndrea Sonaglioni, IRCCS MultiMedica, Italy
Copyright: © 2025 Zhang, Wang, Li, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenjie Zhang, emhhbmd3ajc4NzhAMTYzLmNvbQ==
†ORCID:
Wenjie Zhang
orcid.org/0000-0003-0827-7533
 Wenjie Zhang
Wenjie Zhang Hongjin Wang
Hongjin Wang Peiru Li
Peiru Li Beibei Wu2
Beibei Wu2