Abstract
Artificial chordae are increasingly used to repair mitral prolapse. The application of premeasured artificial chordae facilitates the creation of chordae with an appropriate length. Herein, we describe our experience of applying premeasured artificial chordae in 14 cases of mitral prolapse caused by elongated papillary muscles, with an emphasis on the importance of restoring the physiological features of sub-valvular structures during mitral valve repair.
Introduction
Artificial chordae are increasingly used to repair abnormal sub-valvular structures with excellent long-term results (1). The primary challenges of this technique include determining and maintaining correct chordal lengths. Additionally, papillary muscle (PM) variations may influence surgical complexity (2). Von Oppell developed the concept of premeasured loops to allow for the creation of chordae with appropriate lengths (1). This technique can be used to repair mitral valves, especially those that exhibit prolapse due to elongated or ruptured chordae (3). However, few articles have reported the application of premeasured loops in patients with abnormal PMs. Here, we describe our experience of using premeasured artificial chordae in 14 cases of mitral prolapse caused by elongated PMs, highlighting the importance of restoring the physiological features of sub-valvular structures during mitral valve repair.
Description of the cases
We conducted a case series of all patients diagnosed with mitral prolapse caused by PMs elongation through their preoperative echocardiography. According to their echocardiographic images, we measured the length of the chordae and papillary muscles during left ventricular systole (Figure 1). The length of PM was the distance from the endocardial surface at the left ventricular base to the fibrous head of PM. The length of the chord was the distance from the fibrous head of PM to the segment of the leaflet. Besides, we ruled out other heart diseases (such as coronary artery disease, congenital heart diseases, hypertrophic obstructive cardiomyopathy, etc.) based on the patient's echocardiography and laboratory findings. The registry collects comprehensive data on baseline patient characteristics, surgical details, in-hospital outcomes, and annual clinical follow-up.
Figure 1
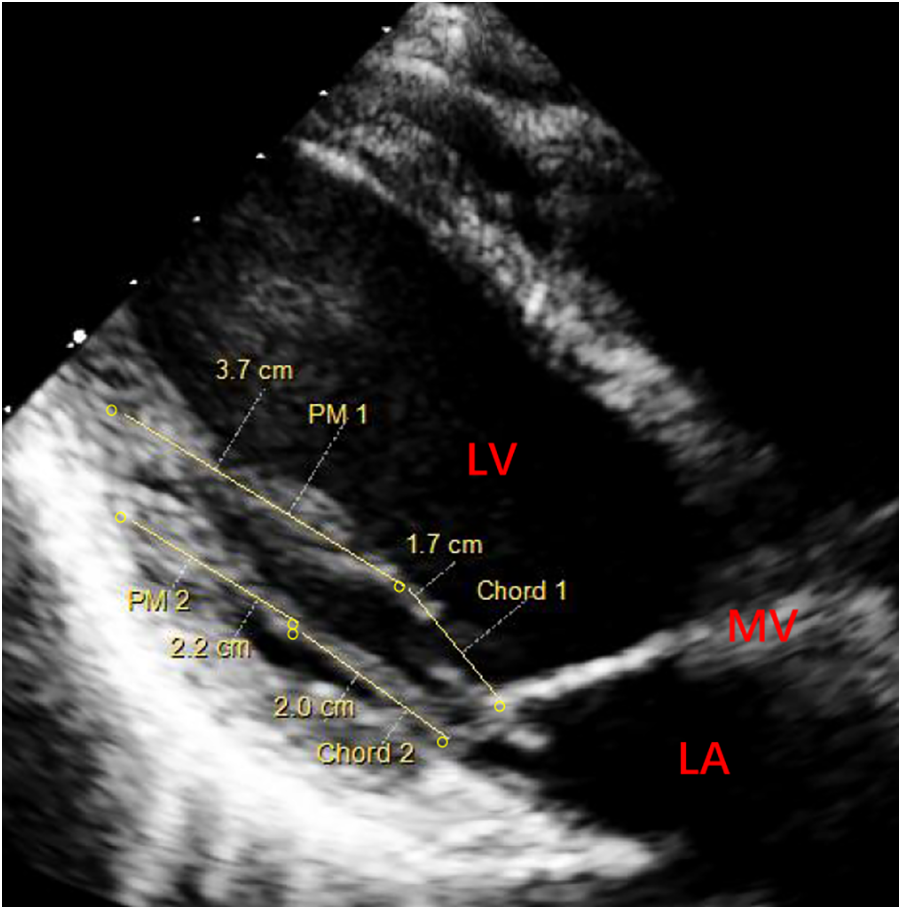
Preoperative echocardiography (parasternal long-axis view) of left ventricular systole for measuring the length of papillary muscles. PM 1 (elongated PM, 3.7 cm) and Chord 1 (the chord of abnormal PM, 1.7 cm). PM 2 (normal PM, 2.2 cm) and Chord 2 (normal chord, 2.0 cm). PM, papillary muscle; MV, mitral valve; LA, left atrium; LV, left ventricle.
Operative details
The patients underwent midline sternotomy and hypothermic cardiopulmonary bypass. The mitral leaflet was then carefully assessed to confirm the prolapsed position and the presence of abnormal sub-valvular structure(s). In all cases, mitral prolapse was caused by the presence of one PM longer than the others in the same group (Figure 2A). In order to measure the length of a normal chord adjacent to the prolapsed area, a sizing caliper was inserted into the ventricle, with which the tip was placed at the PM insertion of the normal chord (Figure 2B). A single ePTFE CV-4 (4-0 GORE-TEX) was threaded around this caliper and ligated four times to create the artificial chordae loop. For diffuse prolapse, the above process should be repeated based on the number of chords, since the anterior leaflet's free edge can be supported by one single chordal loop for up to 5–10 mm (3).
Figure 2
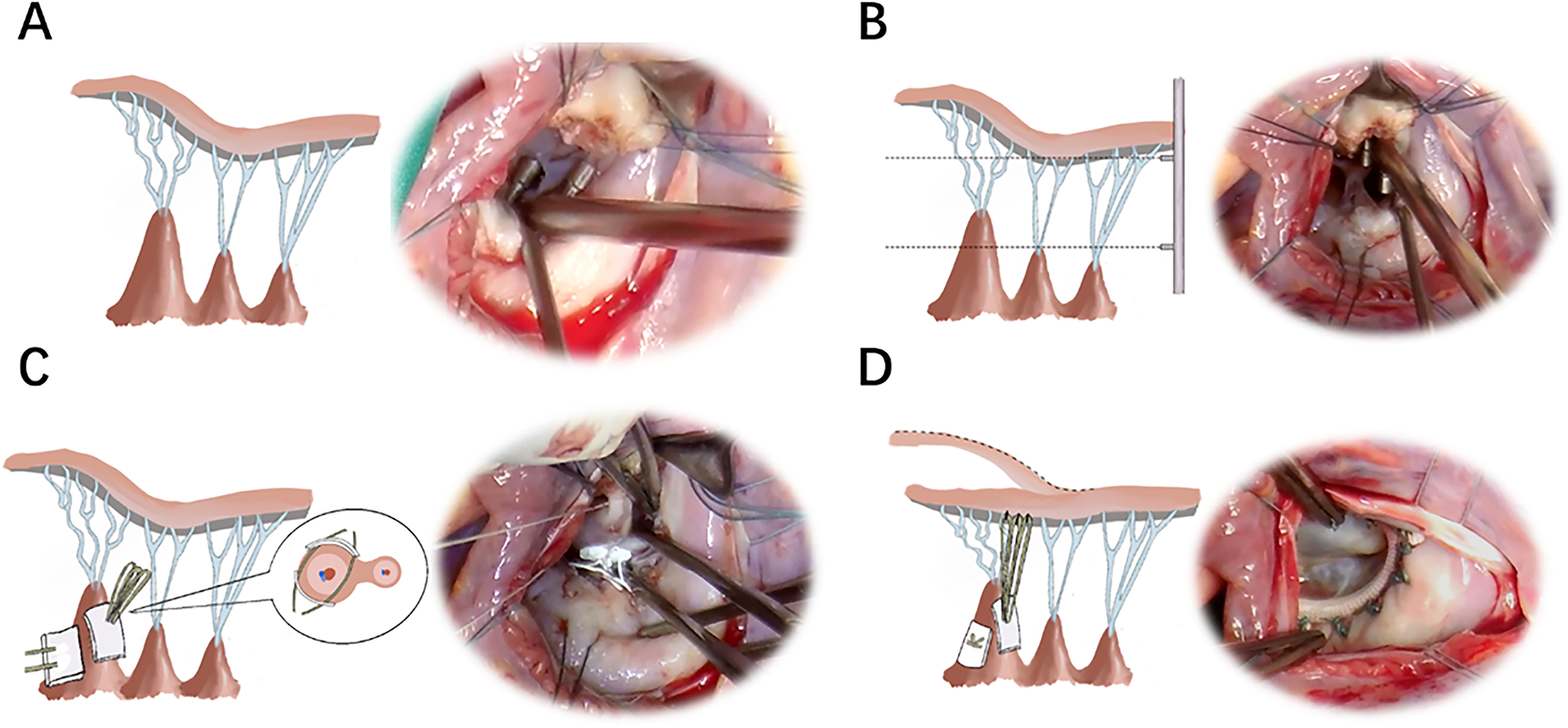
Schematic diagrams and photographs of the operation. (A) The mitral leaflet was assessed to confirm the prolapsed position and abnormal sub-valvular apparatus. (B) A caliper was used to measure the length of the normal chord and PM. (C) The pledget knots were attached to the body of the elongated PM. The sutures were passed through the outer one-third of the PM and carefully tied. (D) The artificial chordae were affixed to the leaflet edge. PM, papillary muscle.
The loop pledgets were attached to the body of the elongated PM by two sutures, which made the pledgets towards the PM base comparable to the adjacent normal PMs (Figure 2C). To reduce injury to the PM, each suture was carefully threaded through the outer one-third of the PM with a second pledget and gently ligated 10 times (Figure 2C). During this process, a back-handed technique was used to pass the needles, in which the chords arose from the portion of the PM facing the surgeon. Each chordal loop was sequentially attached to the prolapsing segment of the leaflet from the ventricular to the atrial side with other ePTFE CV-5 (5-0 GORE-TEX) for reconstructing the artificial chordae (Figure 2D). The loops were attached to the anterior PM for A1 and the lateral half of A2, as well as to the posterior PM for A3 and the medial half of A2 (3). Additionally, an appropriate annular ring was selected to preserve the flexibility of the valve annulus, according to the distance between the two commissures, the surface area of the anterior leaflet, and the coaptation height. Valve function was assessed by injecting saline across the mitral valve under pressure. After completion of de-airing and discontinuation of bypass, valve function was assessed using transesophageal echocardiography.
Results
From July 2017 to June 2022, premeasured artificial chordae were used in 14 patients with moderately severe or severe mitral prolapse caused by elongated PMs. The patients' mean age was 32 ± 14.5 years and nine (64.3%) were male, as shown in Table 1. All patients had A2–A3/A3 prolapse of the anterior mitral leaflet segments caused by elongated posteromedial PMs. The mean cardiopulmonary bypass and aortic cross-clamp times were 95 ± 17.2 min and 138 ± 17.5 min. Short-term postoperative echocardiographic images (Figure 3) showed trivial or no valvular regurgitation. Furthermore, the sutured PMs showed no significant signs of ischemia or rupture. All patients were discharged without any adverse events. At their 1–6-year follow-ups, none of the patients reported needing reoperation, and all survived with New York Heart Association class I or II cardiac function.
Table 1
| Patient characteristics | Diagnosis | Preoperative echocardiography | Operation | Number of implanted loops | CPB (min) | ACC (min) | Size of the annuloplasty ring | Postoperative echocardiography | Follow-up |
|---|---|---|---|---|---|---|---|---|---|
| 48Y, man | Severe mitral insufficiency, NYHA-II | MRA: 7.3 cm2, LVEF: 65%, mitral anterior prolapse (A2-A3) | Mitral valve repair, premeasured artificial chordae | 3 | 136 | 93 | 30 | 6 years after surgery MRA: 3.0 cm2, LVEF: 62% |
Alive at 6 years follow-up with NYHA-II |
| 18Y, woman | Severe mitral insufficiency, NYHA-III | MRA: 8.8 cm2, LVEF: 56%, mitral anterior prolapse (A2-A3) | Mitral valve repair, premeasured artificial chordae, plication of posteromedial commissure | 3 | 145 | 97 | 28 | 1 year after surgery MRA: 1.0 cm2, LVEF: 70% |
Alive at 6 years follow-up with NYHA-I |
| 30Y, woman | Moderately severe mitral insufficiency, NYHA-II | MRA: 7.1 cm2, LVEF: 62%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 3 | 120 | 75 | 26 | 9 months after surgery MRA: 0.0 cm2, LVEF: 60% |
Alive at 6 years follow-up with NYHA-I |
| 35Y, man | Moderately severe mitral insufficiency, NYHA-II | MRA: 6.1 cm2, LVEF: 66%, mitral anterior prolapse (A3) | Mitral valve repair, premeasured artificial chordae, plication of posteromedial commissure | 2 | 156 | 119 | 30 | 4 years after surgery MRA: 4.2 cm2, LVEF: 67% |
Alive at 6 years follow-up with NYHA-I |
| 23Y, man | Severe mitral insufficiency, NYHA-II | MRA: 13.8 cm2, LVEF: 68%, mitral anterior prolapse (A3) | Mitral valve repair, premeasured artificial chordae | 3 | 128 | 106 | 28 | 5 years after surgery MRA: 1.0 cm2, LVEF: 65% |
Alive at 6 years follow-up with NYHA-I |
| 27Y, man | Moderately severe mitral insufficiency, NYHA-II | MRA: 6.6 cm2, LVEF: 65%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 3 | 128 | 82 | 30 | 6 months after surgery MRA: 0.8 cm2, LVEF: 66% |
Alive at 5 years follow-up with NYHA-I |
| 52Y, man | Severe mitral insufficiency, NYHA-II | MRA:8.3 cm2, LVEF: 65%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae, plication of posteromedial commissure | 3 | 166 | 128 | 32 | 1 year after surgery MRA: 0.7 cm2, LVEF: 72% |
Alive at 4 years follow-up with NYHA-I |
| 58Y, man | Severe mitral insufficiency, NYHA-II | MRA:13.5 cm2, LVEF: 61%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 3 | 96 | 74 | 34 | 11 months after surgery MRA: 5.9 cm2, LVEF: 55% |
Alive at 4 years follow-up with NYHA-II |
| 31Y, man | Severe mitral insufficiency, NYHA-II | MRA:16.2 cm2, LVEF: 65%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 2 | 161 | 111 | 26 | 4 years after surgery MRA: 1.7 cm2, LVEF: 60% |
Alive at 4 years follow-up with NYHA-I |
| 55Y, man | Severe mitral insufficiency, NYHA-II | MRA:14.4 cm2, LVEF: 65%, mitral anterior prolapse (A3) | Mitral valve repair, premeasured artificial chordae | 3 | 153 | 86 | 28 | 4 years after surgery MRA: 1.3 cm2, LVEF:62% |
Alive at 4 years follow-up with NYHA-II |
| 16Y, woman | Severe mitral insufficiency, NYHA-I | MRA:8.7 cm2, LVEF: 67%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 3 | 107 | 75 | 30 | 3 years after surgery MRA: 0.0 cm2, LVEF: 51% |
Alive at 3 years follow-up with NYHA-I |
| 15Y, woman | Severe mitral insufficiency, NYHA-IV | MRA:12.5 cm2, LVEF: 66%, mitral anterior prolapse (A2-A3-PC) | Mitral valve repair, premeasured artificial chordae | 3 | 135 | 90 | — | 4 years after surgery MRA: 0.0 cm2, LVEF: 73% |
Alive at 4 years follow-up with NYHA-I |
| 21Y, woman | Severe mitral insufficiency, NYHA-III | MRA:8.4 cm2, LVEF: 63%, mitral anterior prolapse (A2–A3-PC) | Mitral valve repair, premeasured artificial chordae | 3 | 149 | 106 | 26 | 2 years after surgery MRA: 1.3 cm2, LVEF: 70% |
Alive at 2 years follow-up with NYHA-I |
| 26Y, man | Severe mitral insufficiency, NYHA-II | MRA:9.8 cm2, LVEF: 70%, mitral anterior prolapse (A2–A3) | Mitral valve repair, premeasured artificial chordae | 3 | 169 | 115 | 26 | 2 years after surgery MRA: 0.7 cm2, LVEF: 63% |
Alive at 2 years follow-up with NYHA-I |
The clinical characteristics and follow-up results of 14 patients.
NYHA, New York Heart Association functional class; MRA, jet mitral regurgitant area; LVEF, left ventricular ejection fraction; CPB, cardiopulmonary bypass time; ACC, aortic cross-clamp time.
Figure 3
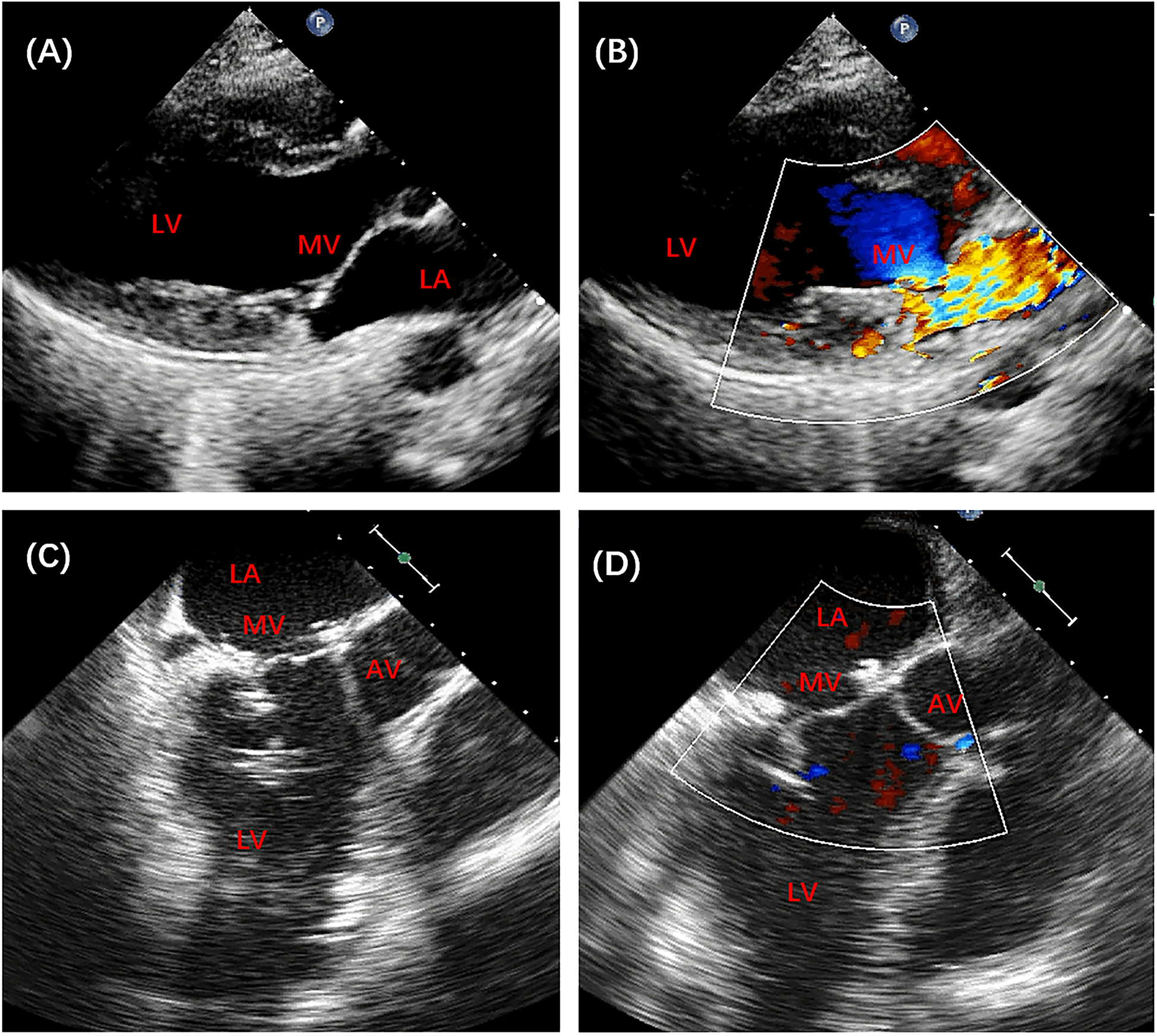
Preoperative and postoperative echocardiography of patient no. 13. (A,B) Preoperative echocardiography revealed severe mitral insufficiency. (C,D) Postoperative echocardiography showed good mitral valve function. AV, aortic valve; MV, mitral valve; LA, left atrium; LV, left ventricle.
Discussion
Since its first description two decades ago (1), the premeasured loops technique has become increasingly popular. Gillinov described and illustrated this surgical technique in detail for repairing mitral prolapse caused by elongated or ruptured chordae (3). However, few articles have reported the application of this technique in patients with abnormal PMs. Here, we introduce our experience of using the premeasured artificial chordae for repairing mitral prolapse caused by elongated PMs.
PMs vary in length and breadth, which may influence the complexity of valve repair surgery (2). Moreover, it is difficult to determine an appropriate chordal length for mitral prolapse caused by elongated PMs. Herein, we describe our experience using premeasured artificial chordae in 14 cases of mitral prolapse caused by elongated PMs, which could be an addition to the surgical indications for this procedure. Methods utilizing premeasured artificial chordae could assist surgeons in determining the loop length and in making chordal replacement less subjective. We adopted a lower attachment position of the loops to maintain the length of the artificial chordae in the case of these special sub-valvular structures (compared to that used for the pledgets, which were attached at the tip of the PMs). During our clinical experience, all cases had anterior leaflet prolapse caused by abnormal posteromedial PMs; however, this technique may also be used in cases of posterior leaflet prolapse.
PM elongation disrupts the normal mitral valve mechanics by altering the force distribution between the PM and chordae tendineae, leading to asymmetric leaflet tethering and eccentric regurgitation. This distinct pathophysiology presents unique challenges in determining chordal length, as traditional reference points become unreliable when elongated sub-valvular structures are present (2). As with Von Oppell's (1), we demonstrated that premeasured artificial chordae provide reliable repair of sub-valvular structures. In patients with mitral prolapse secondary to PM elongation, the artificial chordae were constructed to match the length of adjacent normal chordae, thereby restoring the sub-valvular ratio and facilitating physiological leaflet movement. These results underscore the importance of restoring the physiological characteristics of sub-valvular structures during mitral valve repair, particularly in cases with elongated PMs or chordae. The premeasured artificial chordae technique offers several distinct advantages over conventional approaches for managing PM elongation. When compared with the standard interrupted neochordae (4), this approach facilitates simultaneous implantation of multiple chordae (mean 2.8 ± 0.4 per case), thereby enabling more efficient correction of diffuse prolapse. In comparison with the running technique (5), this method significantly reduces PM trauma through the elimination of repetitive suture penetration. Compared with the standard loop technique (6), our technique provides more physiological length restoration by utilizing adjacent native chordae as reference, thus maintaining sub-valvular geometry more effectively. These technical advantages are particularly relevant for PM elongation cases where maintaining natural force distribution is paramount.
Although we attached the loops to the body of the PM, we did not observe any tearing, ischemic changes, or adverse clinical/echocardiographic outcomes. One may find answers in the follow-up of other mitral valve repair techniques, such as homograft replacement. Hvass et al. (7) observed that while their procedures on PMs may cause damage, there were no cases of PM rupture in follow-up.
Conclusion
Premeasured artificial chordae effectively repaired mitral prolapse caused by elongated PMs, demonstrating stable mid-term outcomes. While limited by sample size, this standardized approach shows promise for focal lesions, warranting further validation in complex pathologies.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Research Ethics Committee of Guangdong Provincial People's Hospital (ethical No: KY-Q-2022-398-01). The study was conducted in accordance with local legislation and institutional requirements. Written informed consent was obtained from all patients for the publication of any potentially identifiable images or data included in this article.
Author contributions
LG: Data curation, Writing – original draft. OC: Methodology, Writing – review & editing. FC: Data curation, Investigation, Writing – review & editing. WW: Methodology, Writing – review & editing. HQ: Investigation, Writing – review & editing. XJ: Funding acquisition, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the National Natural Science Initiating Funds of China (No. 8217020713).
Acknowledgments
The authors thank Miss Liuyun Huang and Miss Yuxin Xie for the schematic diagrams and pictures of the operation (Figure 2).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1543876/full#supplementary-material
Supplementary Video S1Preoperative and postoperative echocardiography of patient no. 13.
Supplementary Video S2Surgical technique.
Abbreviations
PM, papillary muscle.
References
1.
Von Oppell UO Mohr FW . Chordal replacement for both minimally invasive and conventional mitral valve surgery using premeasured gore-tex loops. Ann Thorac Surg. (2000) 70(6):2166–8. 10.1016/s0003-4975(00)02047-6
2.
Gunnal SA Wabale RN Farooqui MS . Morphological variations of papillary muscles in the mitral valve complex in human cadaveric hearts. Singapore Med J. (2013) 54(1):44–8. 10.4103/1995-705X.152994
3.
Gillinov AM Banbury MK . Pre-measured artificial chordae for mitral valve repair. Ann Thorac Surg. (2007) 84(6):2127–9. 10.1016/j.athoracsur.2007.04.046
4.
Perier P . A new paradigm for the repair of posterior leaflet prolapse: respect rather than resect. Oper Tech Thorac Cardiovasc Surg. (2005) 10:180–93. 10.1053/j.optechstcvs.2005.08.003
5.
David TE . Replacement of chordae tendineae with expanded polytetrafluoroethylene sutures. J Card Surg. (1989) 4(4):286–90. 10.1111/j.1540-8191.1989.tb00291.x
6.
Hysi I Rebet O Gautier L Fabre O . A standardized loop technique for mitral valve repair. Ann Thorac Surg. (2017) 103(1):e105–6. 10.1016/j.athoracsur.2016.06.104
7.
Hvass U Juliard JM Assayag P Laperche T Pansard Y Chatel D . Tricuspid autograft for mitral-valve repair. Lancet. (1996) 347(9002):659–61. 10.1016/s0140-6736(96)91206-4
Summary
Keywords
cardiac valve surgery, mitral valve, mitral valve repair, mitral valve prolapse, papillary muscle abnormalities
Citation
Gan L, Chen O, Chen F, Wang W, Qing H and Jian X (2025) Case Report: Surgical repair of mitral prolapse caused by papillary muscle elongation using premeasured artificial chordae: a case series. Front. Cardiovasc. Med. 12:1543876. doi: 10.3389/fcvm.2025.1543876
Received
14 February 2025
Accepted
02 June 2025
Published
08 July 2025
Volume
12 - 2025
Edited by
Giuseppe Gatti, Azienda Sanitaria Universitaria Giuliano Isontina, Italy
Reviewed by
Alessandro Fiocco, University of Pisa, Italy
Tahir Yagdi, EGE University, Türkiye
Updates
Copyright
© 2025 Gan, Chen, Chen, Wang, Qing and Jian.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Xuhua Jian jianxuhuagdgh@126.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.