- 1Department of Geriatrics, The Third People's Hospital of Chengdu, Chengdu, China
- 2Health Management Center, Affiliated Hospital of North Sichuan Medical College, Nanchong, Sichuan, China
Background: The objective of this meta-analysis is to evaluate and compare the effectiveness of various mind-body exercises in the rehabilitation of individuals with chronic cardiopulmonary dyspnoea.
Design: A systematic review and network meta-analysis was conducted on articles from PubMed, EMBASE, Cochrane Library, Web of Science, and China National Knowledge infrastructure which were searched up to November 21, 2024. The methodological quality of the included trials was evaluated using the Cochrane Risk of Bias tool. A network meta-analysis was performed to compare the effects of various mind-body therapies, including Liuzijue, Baduanjin, Yoga, Tai Chi, Wuqinxi, Qigong, Yijinjing, and Buddhist walking meditation.
Results: The analysis included 44 randomized controlled trials involving a total of 2,957 subjects. The network meta-analysis indicated that Yoga might be the most effective exercise intervention for reducing the MLHFQ score (SUCRA: 71.8%). Yoga training demonstrated superior results in increasing the 6-minute walk distance (6MWD) (SUCRA: 99.7%). Qigong was also identified as the most effective exercise intervention for decreasing St. George's Respiratory Questionnaire (SGRQ) (SUCRA: 97.1%). When compared with other treatments, Baduanjin is likely the most appropriate intervention for decreasing COPD Assessment Test (CAT) (SUCRA: 87.1%). Regarding N-terminal pro-B-type natriuretic peptide (NT-proBNP), Yoga might be more advantageous for decreasing the NT-proBNP (SUCRA: 83.4%).
Conclusion: The findings of this study suggest that mind-body exercise may represent a promising intervention for the management of chronic cardiopulmonary dyspnoea. Our findings indicate that Yoga might be the most effective exercise intervention for improving the MLHFQ scores, 6MWD, and NT-proBNP. Qigong is identified as the most effective exercise intervention for decreasing SGRQ. Compared to other treatment methods, Baduanjin may be the most suitable intervention for lowering CAT. This study recommends that patients with chronic cardiopulmonary dyspnoea select appropriate mind-body exercises to achieve effective management of chronic cardiopulmonary dyspnoea.
Systematic Review Registration: https://inplasy.com/inplasy-2024-11-0092/, INPLASY INPLASY2020100052.
1 Introduction
1.1 Background
Chronic cardiopulmonary dyspnoea is a complex and severe clinical syndrome and a heavy burden for patients with a decline in cardiopulmonary function (1–3). The most prevalent types include chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, pulmonary artery hypertension, pulmonary embolism, heart failure (HF), valvular heart disease, and myocardiopathies (4, 5). Dyspnoea is considered chronic if present for more than 1 month (6, 7). Due to its high incidence and mortality rates, chronic cardiopulmonary dyspnoea has become a significant public health issue (8, 9). With the advancement of modern medicine, exercise rehabilitation has emerged as a core element of cardiopulmonary rehabilitation and has become one of its most important aspects, enabling patients to improve their disease status through active exercise (10–12).
Mind-body exercises primarily include Liuzijue, Baduanjin, Yoga, Tai Chi, Wuqinxi, Qigong, Yijinjing, and Buddhist walking meditation (BWM) (13, 14). Mind-body exercises are gentle, require minimal equipment or external assistance, and are not constrained by location or time, making them easy to perform and learn. Therefore, they are suitable for individuals with compromised health, such as those with cardiopulmonary dyspnoea (15, 16). Particularly, mind-body therapies combine physical exercise with breathing and deep relaxation techniques, which can enhance physical function as well as emotional and mental awareness, and therefore may provide greater benefits than other forms of traditional exercise.
However, different mind-body exercise programs have distinct characteristics and may yield varying effects on patients with chronic cardiopulmonary dyspnoea. Currently, there is a lack of evidence-based recommendations to determine which exercise program is most suitable for patients with chronic cardiopulmonary dyspnoea. Compared to traditional treatment, practicing Tai Chi was effective in alleviating depressive symptoms in HF patients (17, 18). Mind-body exercise could reduce levels of anxiety and depression in those with COPD (19).
Currently, there is no consensus on the best practice plans for different mind-body exercises in the rehabilitation of patients with chronic cardiopulmonary dyspnoea. Therefore, the primary objective of this study is to conduct a network meta-analysis (NMA) of randomized controlled trials (RCTs) to determine the effects of different mind-body exercises, evaluate the impact of these exercises on the Minnesota Living with Heart Failure Questionnaire (MLHFQ), 6-minute walk distance (6MWD), St. George's Respiratory Questionnaire (SGRQ), COPD Assessment Test (CAT), and N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with chronic cardiopulmonary dyspnoea, and provide a better understanding of the effects of these mind-body exercises for patients and clinicians.
2 Materials and methods
2.1 Search strategy
The researchers in this study searched five electronic databases (PubMed, EMBASE, Cochrane Library, Web of Science, and China National Knowledge Infrastructure) from their inception until November 21, 2024. The detailed search strategy can be found in Supplementary Table S1. INPLASY registration number: INPLASY2020100052.
2.2 Inclusion criteria
(1) Experimental group utilizing different mind-body exercise methods as interventions for cardiopulmonary dyspnoea; (2) Control group receiving only standard care and patient rehabilitation; (3) Clinical randomized controlled trials; (4) Outcomes must include at least one of the following indicators: MLHFQ, 6MWD, SGRQ, CAT, and NT-proBNP.
2.3 Exclusion criteria
(1) Studies with incomplete or unreported data; (2) Studies from non-randomized controlled trials [including quasi-randomized controlled trials, letters to editors, case reports, reviews, animal studies, protocols, or conference abstracts]; (3) No language restrictions exist.
2.4 Outcomes
The MLHFQ is a health-related quality of life (HRQoL) questionnaire specifically for patients with this heart condition, with potential value in both research and clinical practice (20). Scores range from 0 to 105, with lower scores reflecting better health-related quality of life (21). This questionnaire is effective and reliable for assessing quality of life (QOL) in patients with HF (22) (Supplementary Table S2). The 6MWD test was used to assess physical functional capacity. Patients were required to walk back and forth in a corridor with a length of 30 m as soon as possible, and the test was terminated at 6 min, and the walking distance was measured (23). The longer the distance, the better the exercise endurance of patients. The SGRQ was selected as the primary outcome due to its validated use in COPD trials (Supplementary Table S3). This disease-specific instrument assesses health-related quality of life (HRQoL) through three domains (symptoms, impact, and activity) and a total score (0–100), where higher scores indicate worse health status (24). Extensively validated in Western and Chinese COPD populations, the SGRQ demonstrates strong reliability, sensitivity, and responsiveness to clinical change, making it ideal for evaluating treatment effects (25–28). The CAT is an 8-item patient-reported questionnaire assessing COPD impact on quality of life (29) (Supplementary Table S4). Patients score each item from 0 (no impairment) to 5 (severe impairment) (30). Total scores range from 0 to 40, with higher scores indicating worse symptoms and poorer health status. Normal range of NTproBNP is <125 pg/ml (31). The minimal clinically important difference (MCID) for MLHFQ ranged from 3.59 to 19.14 points (32). The MCID for the 6MWD is 26 m (33). Mean and range of MCID estimates for SGRQ is 3.9 (0.7–5.5) (34). The estimated MCID of the CAT for the improvement directions was at least −3 points (35). The MCID for the NT-proBNP is a reduction of more than 30% (36).
2.5 Study selection
The literature was screened and excluded using the reference management software EndNote. Two researchers initially screened the titles of duplicate literature, non-randomized controlled trials, review articles, conference papers, protocols, and letters. The same two researchers then reviewed the abstracts to determine which literature to include and which to exclude. Finally, the researchers conducted a full reading of the remaining literature and made further determinations for inclusion. Throughout this process, the two researchers independently screened the literature and compared the remaining studies; if they agreed, the studies were included, and if they disagreed, a third researcher discussed and resolved the differences.
2.6 Data extraction
A five-item, standardised and pre-selected data extraction form was used to record data for inclusion in the study under the following headings: (1) author, (2) country, (3) year of publication, (4) sample size, and (5) details of the exercise intervention.
2.7 Risk of bias of individual studies
Two researchers independently assessed the risk of bias in randomized controlled trials using the Cochrane Handbook version 5.1.0. The following seven domains were considered: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants, (4) blinding of personnel, (5) incomplete outcome data, (6) selective reporting, and (7) other sources of bias. Trials were categorized into three risk levels based on the number of components with a potential high risk: high risk, unclear risk, and low risk. Based on the number of components with a potential high risk ratio, trials were classified into three risk ratio levels: high risk (five or more), moderate risk (three or four), and low risk (two or fewer) (37).
2.8 Data analysis
In studies where exercise is used as an intervention, all variables are continuous and are reported as mean values with standard deviation (SD) (38). Continuous variables in the study will be reported with 95% confidence intervals (CIs) and analyzed as mean differences (MDs), defined as the absolute difference between the means of the treatment and control groups, calculated using the same scale. Given the potential heterogeneity among different studies, we opted for a random effects model for the analysis rather than a fixed effects model (39). Egger's test, Begg's test, and funnel plots were used to test for publication bias.
We used Stata software (version 15.1) and, following the PRISMA NMA guidelines, conducted network meta-analysis aggregation and analysis using Markov Chain Monte Carlo simulations within a Bayesian framework (40). If the P-value > 0.05, we will use the node-splitting method to quantify and demonstrate the consistency between indirect and direct comparisons calculated using commands in Stata software. The consistency test was passed (41).
Stata software was used to present and describe network diagrams of different exercise interventions. In the generated network diagrams, each node represents different exercise interventions and various control conditions, while the lines connecting the nodes represent direct comparisons between interventions. The size of each node and the width of the connecting lines are proportional to the number of studies (42).
The levels of intervention were summarized and reported as P-values. P-values are considered as frequency simulation values under the cumulative ranking curve (SUCRA), which measure the degree of certainty that one treatment is superior to another and represent the average of all competing treatments. P-values range from 0 to 1, where 1 indicates the best treatment with no uncertainty, and 0 indicates the worst treatment with no uncertainty. Although P-scores or SUCRA can be effectively reinterpreted as percentages of effectiveness or acceptability for exercise interventions, such scores should be interpreted cautiously unless there are meaningful clinical differences between the interventions (43). To assess whether there is bias in small-scale studies (which may lead to publication bias in NMA), a network funnel plot was generated and visually inspected using symmetry criteria (44).
3 Results
3.1 Study and identification and selection
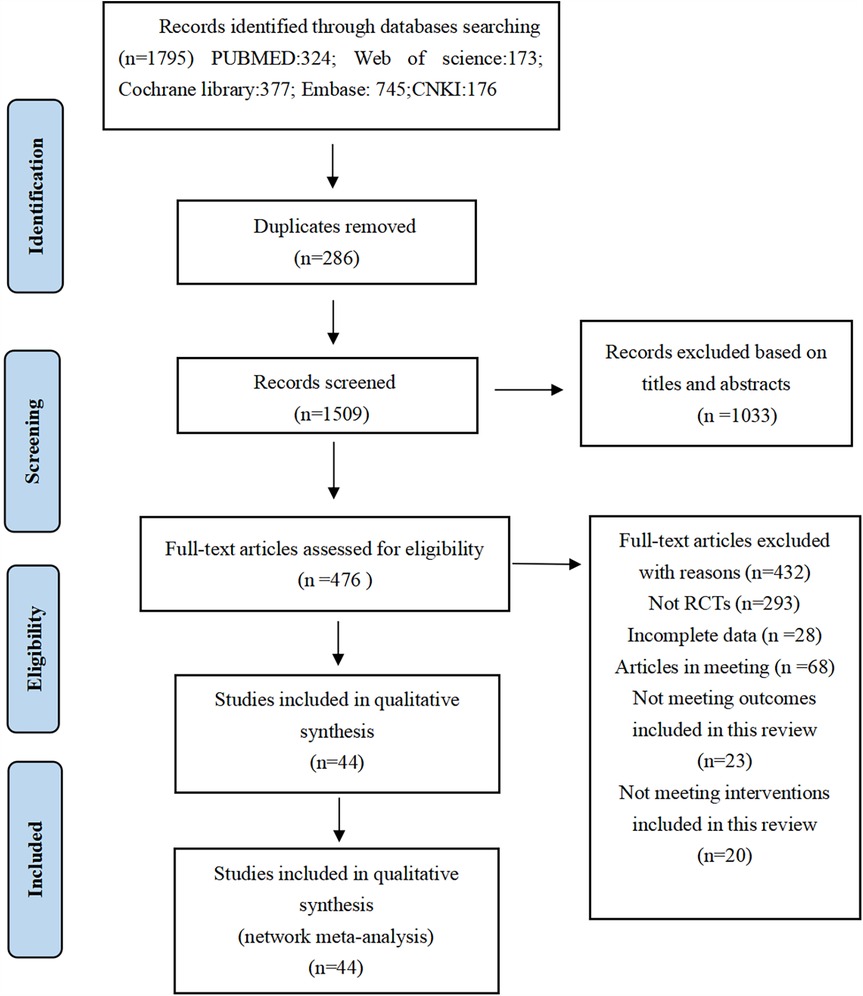
A total of 1,795 documents were retrieved from electronic databases. After removing duplicates, the remaining 1,509 documents had their titles and abstracts reviewed, resulting in the exclusion of 1,033 documents. The remaining 476 documents were read in full, and 432 documents were excluded for reasons including, but not limited to, the following: non-randomized controlled trials, incomplete data, conference papers, and interventions that did not meet the criteria for this review. Ultimately, 44 documents were included in this study (Figure 1).
3.2 Quality assessment of the included studies
Nineteen studies were defined as low risk, four as high risk, and 21 as moderate risk. None of these studies achieved blinding of both participants and assessors, but it was difficult to blind both participants and assessors due to the nature of the interventions, which involved exercise, as patients and their families were required to sign informed consent forms before the start of the trial. Specific details will be presented in Supplementary Table S5, Supplementary Figure S1, Supplementary Figure S2.
3.3 Characteristics of the included studies
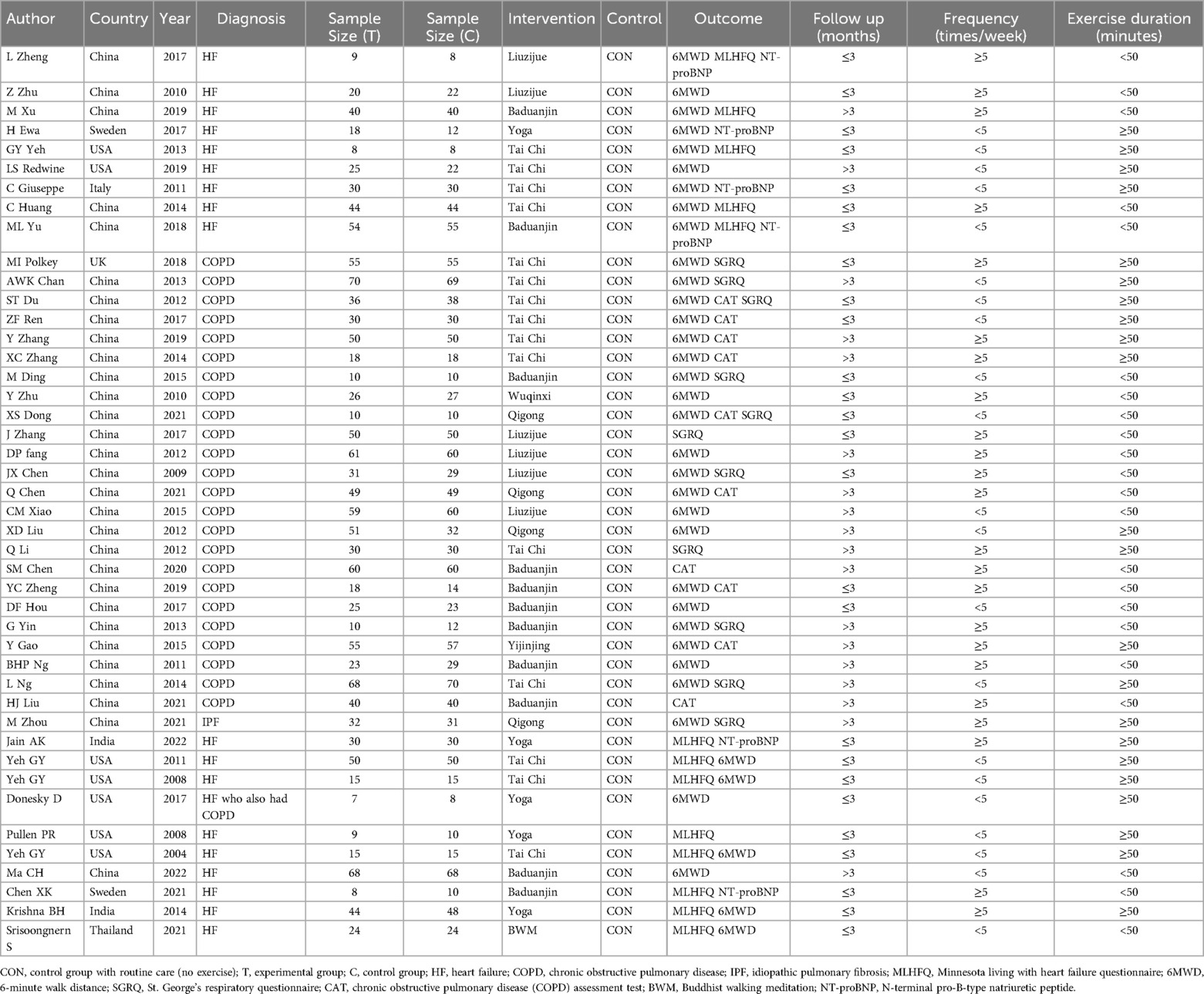
In summary, we included 44 randomized controlled trials, involving a total of 2,957 patients diagnosed with chronic cardiopulmonary dyspnoea (16, 45–89). The interventions in the treatment group included Liuzijue (6 studies), Baduanjin (11 studies), BWM (1 studies), Qigong (4 studies), Tai Chi (15 studies), Wuqinxi (1 studies), Yijinjing (1 studies), and Yoga (5 studies). Eleven studies reported MLHFQ as an outcome measure, 32 studies reported MLHFQ, 2 studies reported CAT, 4 studies reported SGRQ, and 6 studies reported NT-proBNP. Of the 44 studies, 7 was conducted in USA, 1 in the UK, 1 in Thailand, 2 in Sweden, 1 in the Italy, 2 in India, and the rest were from different regions in China. The follow-up durations of the studies ranged from 1 months to 6 months. Table 1 presents the characteristics of the included studies.
3.4 Network meta-analysis
The full NMA figure will be shown in Supplementary Figures S3A–S3E.
3.4.1 Minnesota living with heart failure questionnaire (MLHFQ)
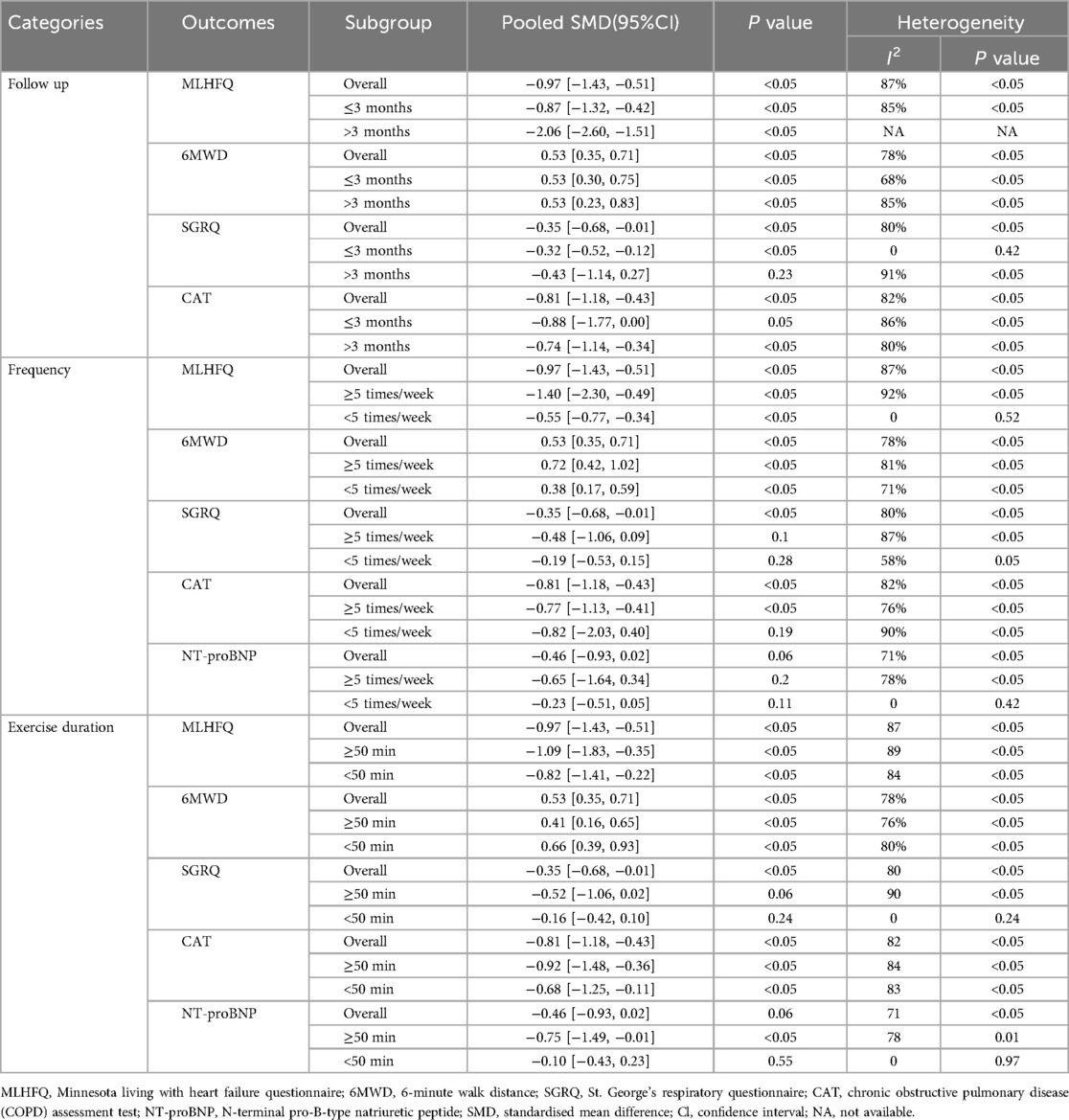
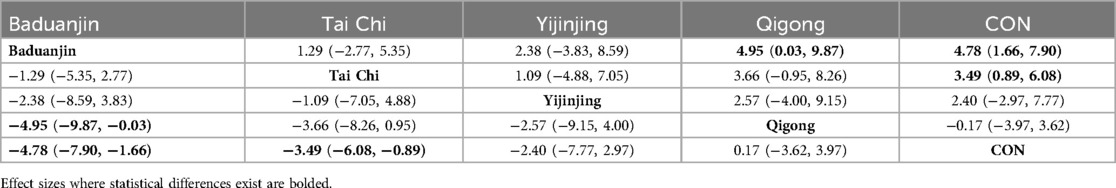
Thirteen studies examined the effects of mind-body exercise on the MLHFQ. The meta-analysis shown that mind-body exercise was effective in reduce the MLHFQ [standardised mean difference (SMD) = −0.97, 95%CI −1.43 to −0.51, p < 0.05, I2 = 87%; Figure 2A], as compared to control groups.
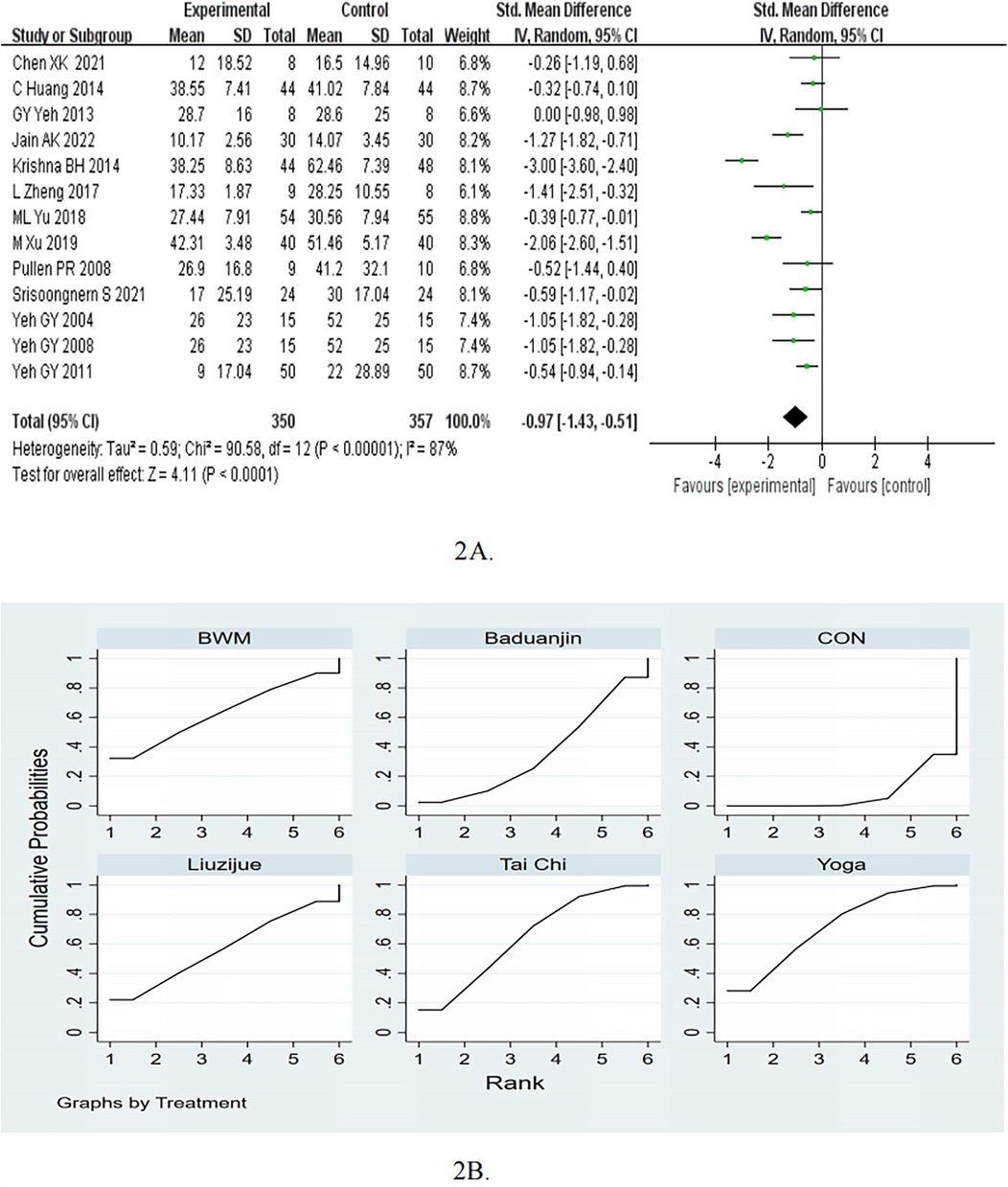
Figure 2. (A) Forest plots for the effects of mind-body exercise on MLHFQ. (B) SUCRA plot for MLHFQ.
In the subgroup of follow up, the mind-body exercise showed a significant improvement in MLHFQ compared to the control group for ≤3months (pooled SMD: −0.87, 95% CI: −1.32 to −0.42, p < 0.05) and >3months (pooled SMD: −2.06, 95% CI: −2.60 to −1.51, p < 0.05), as shown in Table 2. In the subgroup of frequency, the mind-body exercise showed a significant improvement in MLHFQ compared to the control group for ≥5 times/week (pooled SMD: −1.40, 95% CI: −2.30 to −0.49, p < 0.05) and <5 times/week (pooled SMD: −0.55, 95% CI: −0.77 to −0.34, p < 0.05). In the subgroup of exercise duration, the mind-body exercise showed a significant improvement in MLHFQ compared to the control group for ≥50 min (pooled SMD: −1.09, 95% CI: −1.83 to −0.35, p < 0.05) and <50 min (pooled SMD: −0.82, 95% CI: −1.41 to −0.22, p < 0.05).
Consistency and inconsistency tests were conducted on all P-values for indirect and direct comparisons between the studies, with all P-values greater than 0.05, indicating that the influence of consistency among the studies is acceptable. Details will be listed in Supplementary Table S6.
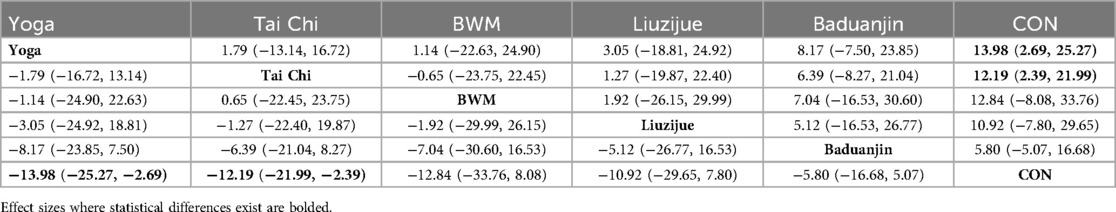
The results of the network meta-analysis indicate that yoga [MD = −13.98, 95% CI = (−25.27,−2.69)] and Tai Chi [MD = −12.19, 95% CI = (−21.99,−2.39)] were more effective than control group in reducing the MLHFQ scores. Based on the SUCRA rankings, Yoga had the highest probability of being the most effective therapy for reducing MLHFQ scores, followed by Tai Chi, BWM, Liuzijue, Baduanjin, and control (Table 3A; Figure 2B). Compared to the control group, Yoga showed a decrease of −13.98 (95% CI −25.27 to −2.69) and reach the MCID.
3.4.2 6-minute walk distance (6MWD)
A meta-analysis of the 37 RCTs showed that mind-body exercise was effective in improving 6MWD (SMD = 0.53, 95%CI 0.35–0.71, p < 0.05, I2 = 78%; Figure 3A), as compared to control groups. Subgroup analyses for 6MWD were performed according to different diseases. In the subgroup of HF, the mind-body exercise showed a significant improvement in 6MWD compared to the control group (pooled SMD: 0.47, 95% CI: 0.09–0.85, p = 0.01), as shown in Figure 3B. In the subgroup of COPD, the mind-body exercise showed a significant improvement in 6MWD compared to the control group (pooled SMD: 0.49, 95% CI: 0.33–0.66, p < 0.01), as shown in Figure 3B.
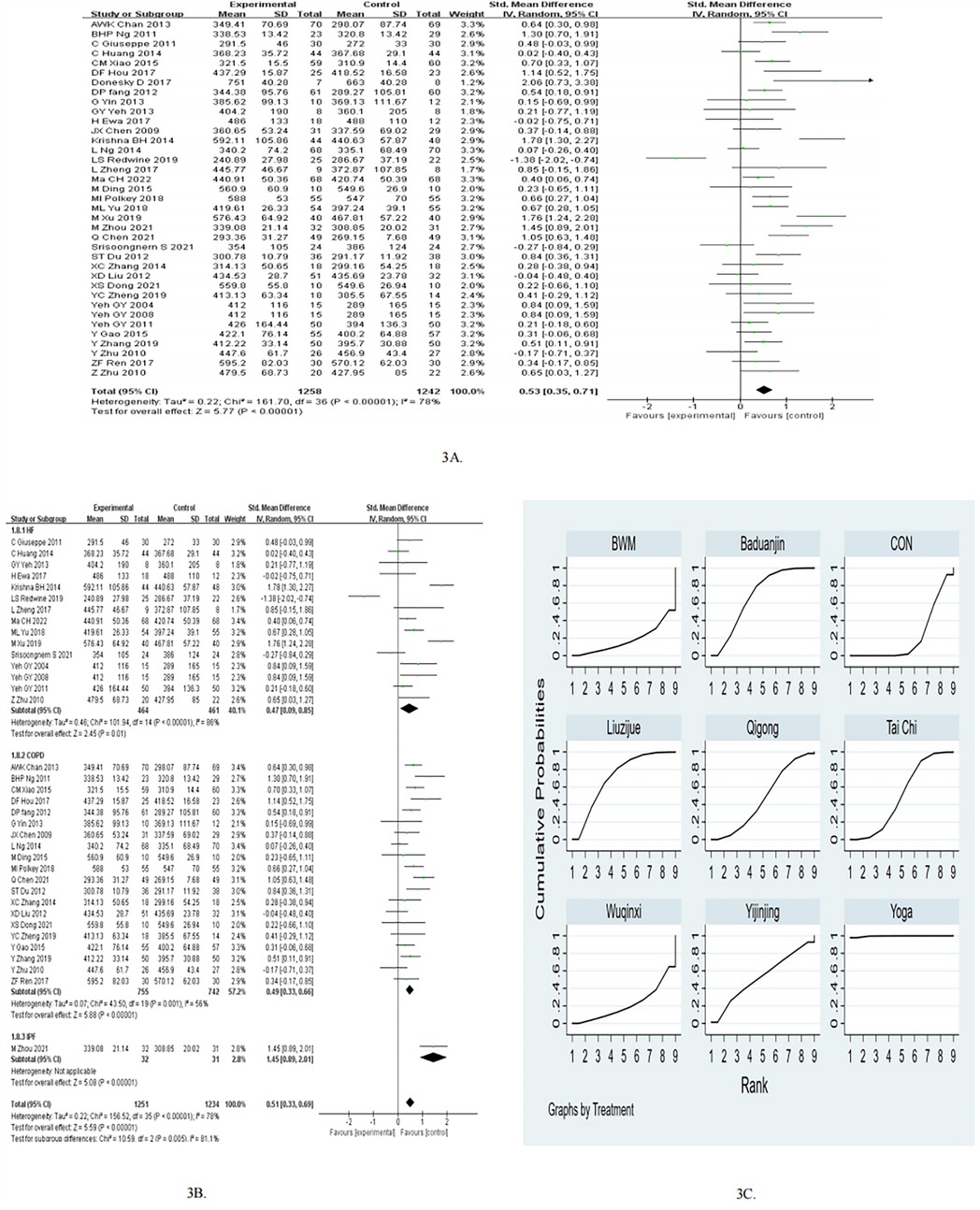
Figure 3. (A) Forest plots for the effects of mind-body exercise on 6MWD. (B) Subgroup meta-analysis of 6MWD. (C) SUCRA plot for 6MWD.
In the subgroup of follow up, the mind-body exercise showed a significant improvement in 6MWD compared to the control group for ≤3months (pooled SMD: 0.53, 95% CI: 0.30–0.75, p < 0.05) and >3months (pooled SMD: 0.53, 95% CI: 0.23–0.83, p < 0.05), as shown in Table 2. In the subgroup of frequency, the mind-body exercise showed a significant improvement in 6MWD compared to the control group for ≥5 times/week (pooled SMD: 0.72, 95% CI: 0.42–1.02, p < 0.05) and <5 times/week (pooled SMD: 0.38, 95% CI: 0.17–0.59, p < 0.05). In the subgroup of exercise duration, the mind-body exercise showed a significant improvement in 6MWD compared to the control group for ≥50 min (pooled SMD: 0.41, 95% CI: 0.16–0.65, p < 0.05) and <50 min (pooled SMD: 0.66, 95% CI: 0.39–0.93, p < 0.05).
Consistency and inconsistency tests were conducted on all P-values for indirect and direct comparisons among the studies, with all P-values greater than 0.05, indicating that the influence of consistency among the studies is acceptable. Details will be provided in Supplementary Table S7.
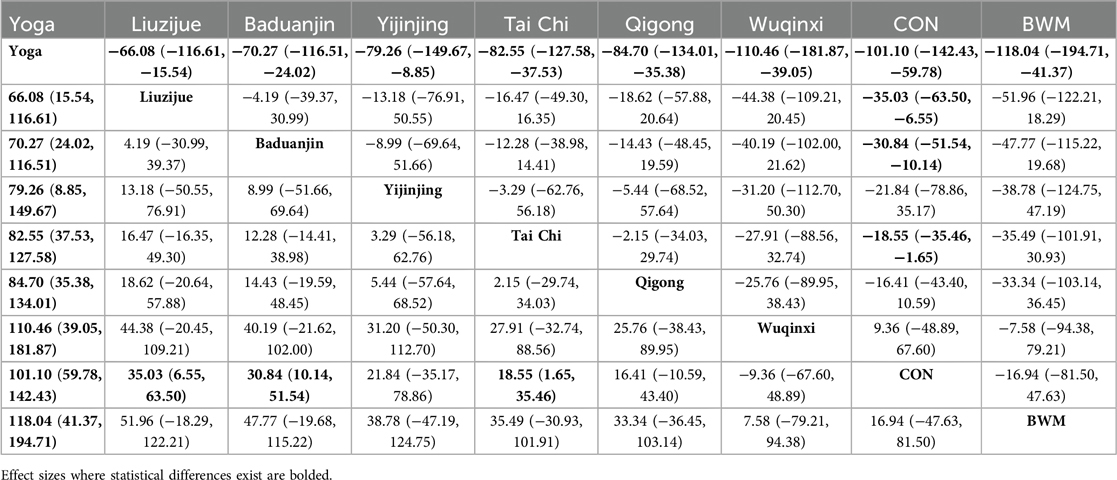
The results of the network meta-analysis indicate that the Liuzijue group [MD = 35.03, 95% CI = (6.55, 63.50)], Baduanjin group [MD = 30.84, 95% CI = (10.14, 51.54)], and the Tai Chi group [MD = 18.55, 95% CI = (1.65, 35.46)] significantly improved the 6MWD compared to the control group. Compared to Liuzijue [MD = 66.08, 95% CI = (15.54, 116.61)], Baduanjin [MD = 70.27, 95% CI = (24.02, 116.51)], Yijinjing [MD = 79.26, 95% CI = (8.85, 149.67)], Tai Chi [MD = 82.55, 95% CI = (37.53, 127.58)], Qigong [MD = 84.70, 95% CI = (35.38, 134.01)], Wuqinxi [MD = 110.46, 95% CI = (39.05, 181.87)], control [MD = 101.10, 95% CI = (59.78, 142.43)], and BWM [MD = 118.04, 95% CI = (41.37, 194.71)], Yoga demonstrated a statistically significant effect on the increase in 6MWD. In terms of increasing 6MWD, the probability rankings for different exercise interventions indicate that Yoga ranked highest in SUCRA (SUCRA: 99.7%, as shown in Figure 3C), followed by the Liuzijue, Baduanjin, Yijinjing, Tai Chi, Qigong, Wuqinxi, CON, and BWM (Table 3B; Figure 3C). As for Yoga, pooling evidence for the 6MWD showed an increase of 101.10 m (95% CI 59.78–142.43) and successed to reach the MCID of 26 m.
3.4.3 St. George's respiratory questionnaire (SGRQ)
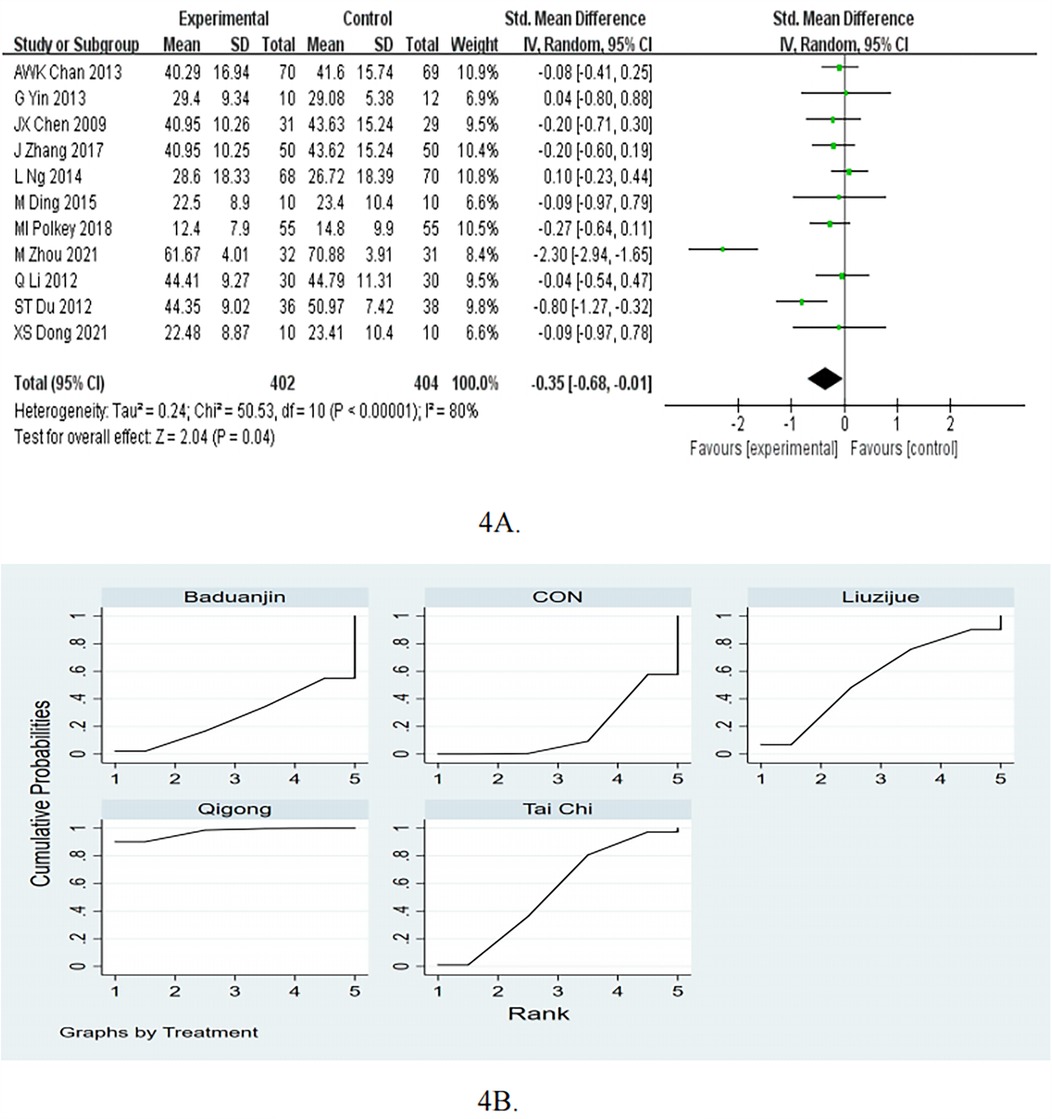
The pooled results of the 11 studies showed that the SGRQ was significantly improved in the mind-body exercise group (SMD = −0.35, 95%CI −0.68 to −0.01, p < 0.05, I2 = 80%; Figure 4A).
In the subgroup of follow up, the mind-body exercise showed a significant improvement in SGRQ compared to the control group for ≤3months (pooled SMD: −0.32, 95% CI: −0.52 to −0.12, p < 0.05). As for >3 months, compared with the control intervention, mind-body exercise did not significantly reduce SGRQ (SMD = −0.43, 95%CI = −1.14 to 0.27, P = 0.23), as shown in Table 2. In the subgroup of frequency, the mind-body exercise did not significant reduce SGRQ score compared to the control group for ≥5 times/week (pooled SMD: −0.48, 95% CI: −1.06 to 0.09, p = 0.1) and <5 times/week (pooled SMD: −0.19, 95% CI: −0.53 to 0.15, p = 0.28). In the subgroup of exercise duration, the mind-body exercise did not significant reduce SGRQ score compared to the control group for ≥50 min (pooled SMD: −0.52, 95% CI: −1.06 to 0.02, p = 0.06) and ≥50 min (pooled SMD: −0.16, 95% CI: −0.42 to 0.10, p = 0.24).
Consistency and inconsistency tests were conducted on all P-values for indirect and direct comparisons among the studies, with most P-values greater than 0.05, indicating that the influence of consistency among the studies is acceptable. Details will be provided in Supplementary Table S8.
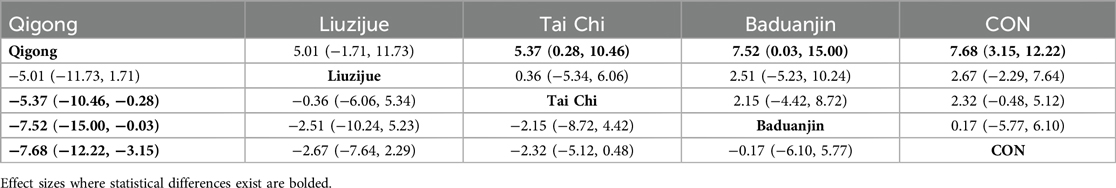
The results of the network meta-analysis indicate that Qigong was more effective than the Tai Chi [MD = −5.37, 95% CI = (−10.46, −0.28)], Baduanjin [MD = −7.52, 95% CI = (−15.00, −0.03)], and the control group [MD = −7.68, 95% CI = (−12.22, −3.15)] in improving SGRQ (Table 3C). In terms of increasing SGRQ, the probability rankings for different exercise interventions indicate that Qigong ranked first in SUCRA (SUCRA: 97.1%, as shown in Figure 4B). Compared to the control group, Qigong showed a decrease of −7.68 (95% CI −12.22 to −3.15) and reach the MCID.
3.4.4 Chronic obstructive pulmonary disease (COPD) assessment test (CAT)
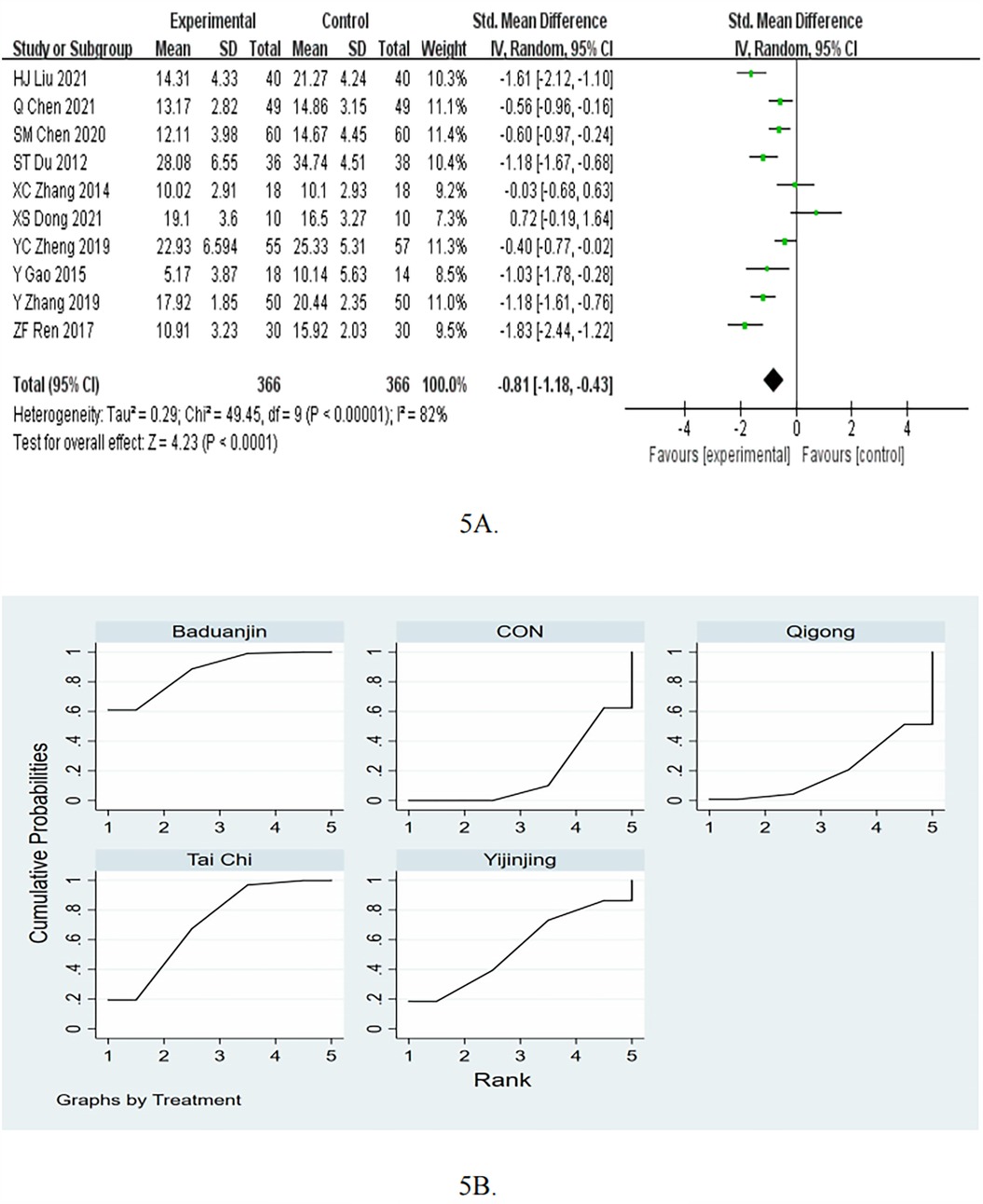
The meta-analysis of the 10 RCTs showed that mind-body exercise was effective in reduce CAT (SMD = −0.81, 95%CI −1.18 to −0.43, p < 0.05, I2 = 82%; Figure 5A).
In the subgroup of follow up, the mind-body exercise showed a significant improvement in CAT compared to the control group for >3months (pooled SMD: −0.74, 95% CI: −1.14 to −0.34, p < 0.05). As for ≤3months, compared with the control intervention, mind-body exercise did not significantly reduce CAT (SMD = −0.88, 95%CI = −1.77 to 0.00, P = 0.05), as shown in Table 2. In the subgroup of frequency, the mind-body exercise showed a significant improvement in CAT compared to the control group for ≥5 times/week (pooled SMD: −0.77, 95% CI: −1.13 to −0.41, p < 0.05). As for <5 times/week, compared with the control intervention, mind-body exercise did not significantly reduce CAT (SMD = −0.82, 95%CI = −2.03 to 0.40, P = 0.19). In the subgroup of exercise duration, the mind-body exercise showed a significant improvement in CAT compared to the control group for ≥50 min (pooled SMD: −0.92, 95% CI: −1.48 to −0.36, p < 0.05) and <50 min (pooled SMD: −0.68, 95% CI: −1.25 to −0.11, p < 0.05).
Consistency and inconsistency tests were conducted on all P-values for indirect and direct comparisons among the studies, with most P-values greater than 0.05, indicating that the influence of consistency among the studies is acceptable. Details will be provided in Supplementary Table S9.
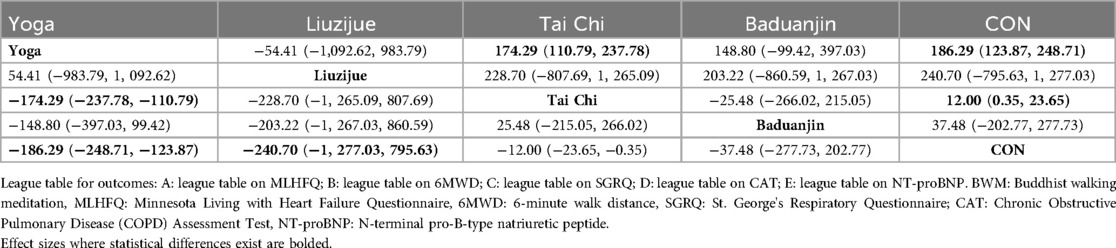
Figure 5B; Table 3D present the pooled MDs and 95%CIs for CAT among different interventions in the NMA. Compared to the control group, Baduanjin [MD = −4.78, 95% CI = (−7.90, −1.66)] and Tai Chi [MD = −3.49, 95% CI = (−6.08, −0.89)] demonstrated a statistically significant effect in reducing CAT. Additionally, Baduanjin [MD = −4.95, 95% CI = (−9.87, −0.03)] was more effective than Qigong. Based on the SUCRA rankings, Baduanjin had the highest probability of being the most effective therapy for reducing CAT, followed by the Tai Chi, Yijinjing, Qigong, and control group. As for Baduanjin, pooling evidence for the CAT showed a decrease of 4.78 and reach the MCID of 3 points.
3.4.5 N-terminal pro-B-type natriuretic peptide (NT-proBNP)
Compared with the control intervention, mind-body exercise did not significantly reduce NT-proBNP (RCTs: n = 6; SMD = −0.46, 95%CI = −0.93 to 0.02, P = 0.06, I2 = 71%, Figure 6A).
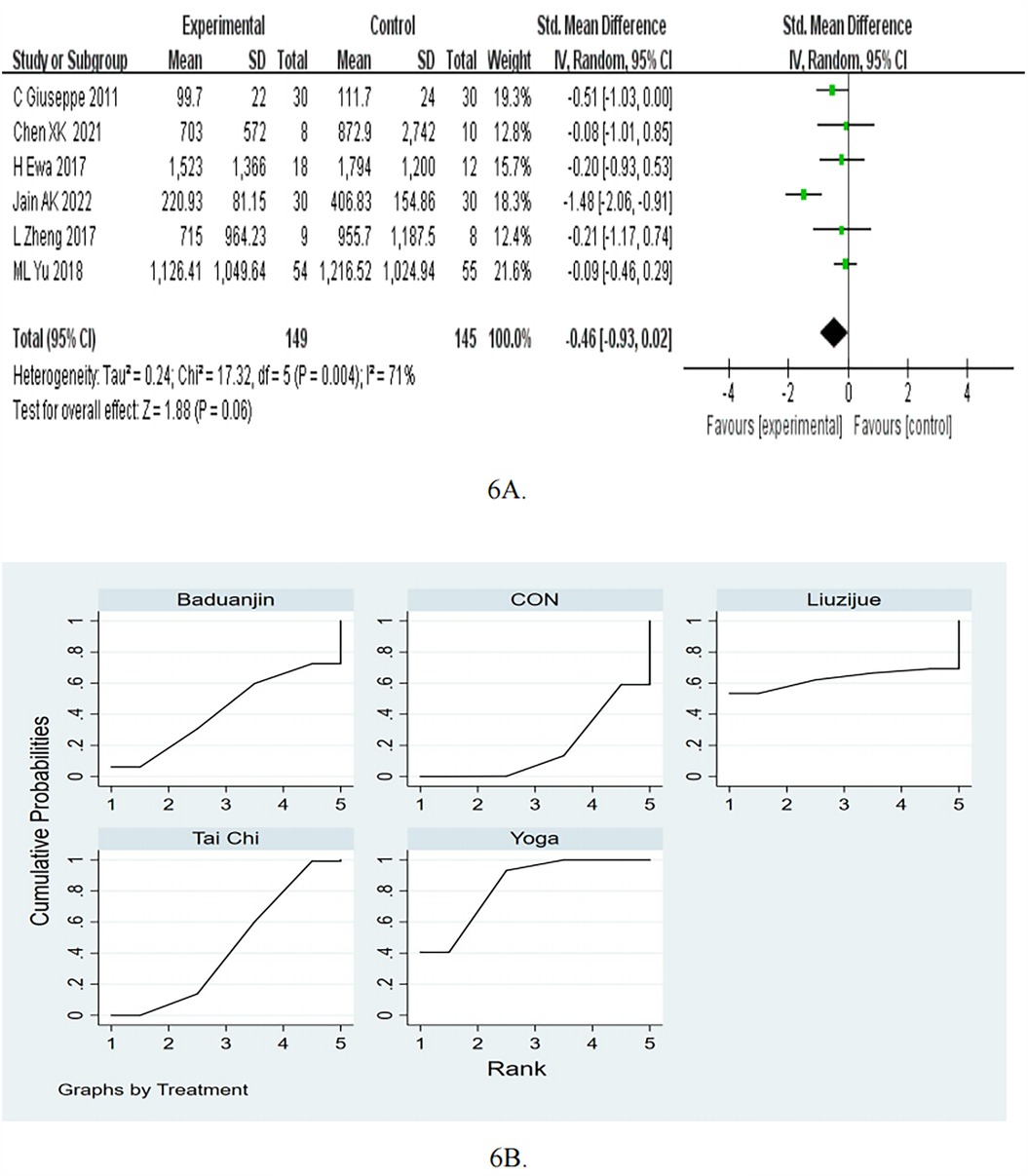
Figure 6. (A) Forest plots for the effects of mind-body exercise on NT-proBNP. (B) SUCRA plot for NT-proBNP.
In the subgroup of frequency, the mind-body exercise did not significant reduce NT-proBNP compared to the control group for ≥5 times/week (pooled SMD: −0.65, 95% CI: −1.64 to 0.34, p = 0.2) and <5 times/week (pooled SMD: −0.23, 95% CI: −0.51 to 0.05, p = 0.11), as shown in Table 2. In the subgroup of exercise duration, the mind-body exercise showed a significant improvement in NT-proBNP compared to the control group for ≥50 min (pooled SMD: −0.75, 95% CI: −1.49 to −0.01, p < 0.05). As for <50 min, compared with the control intervention, mind-body exercise did not significantly reduce NT-proBNP (SMD = −0.10, 95%CI = −0.43 to 0.23, P = 0.55).
Consistency and inconsistency tests were conducted on all P-values for indirect and direct comparisons between the studies, with all P-values greater than 0.05, indicating that the influence of consistency among the studies is acceptable. Details will be listed in Supplementary Table S10.
The results of the network meta-analysis indicate that Yoga [MD = −186.29, 95% CI = (−248.71, −123.87)] and Tai Chi [MD = −12.00, 95% CI = (−23.65, −0.35)] were more effective than control group in reducing the NT-proBNP. Moreover, Yoga [MD = −174.29, 95% CI = (−237.78, −110.79)] was more effective than Tai Chi. Based on the SUCRA rankings, Yoga had the highest probability of being the most effective therapy for reducing NT-proBNP, followed by Liuzijue, Tai Chi, Baduanjin, and control (Table 3E; Figure 6B). As for NT-proBNP, compared to the control group, Yoga showed a decrease of −186.29 (95% CI −248.71 to −123.87, p < 0.05).
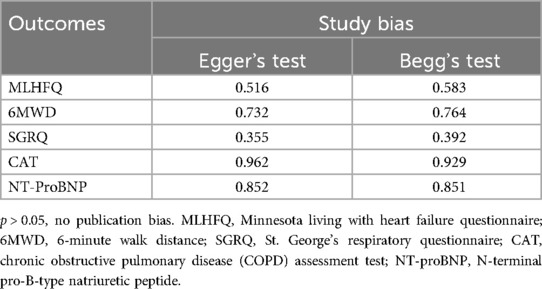
3.5 Publication bias test
We constructed separate funnel plots for all outcome measures to test for potential publication bias. Visual inspection of the funnel plots revealed no significant publication bias. Details are shown in Figure 7. The findings of Egger's and Begg's tests to identify study bias (Table 4). From the results, it could be considered that there was no publication bias.
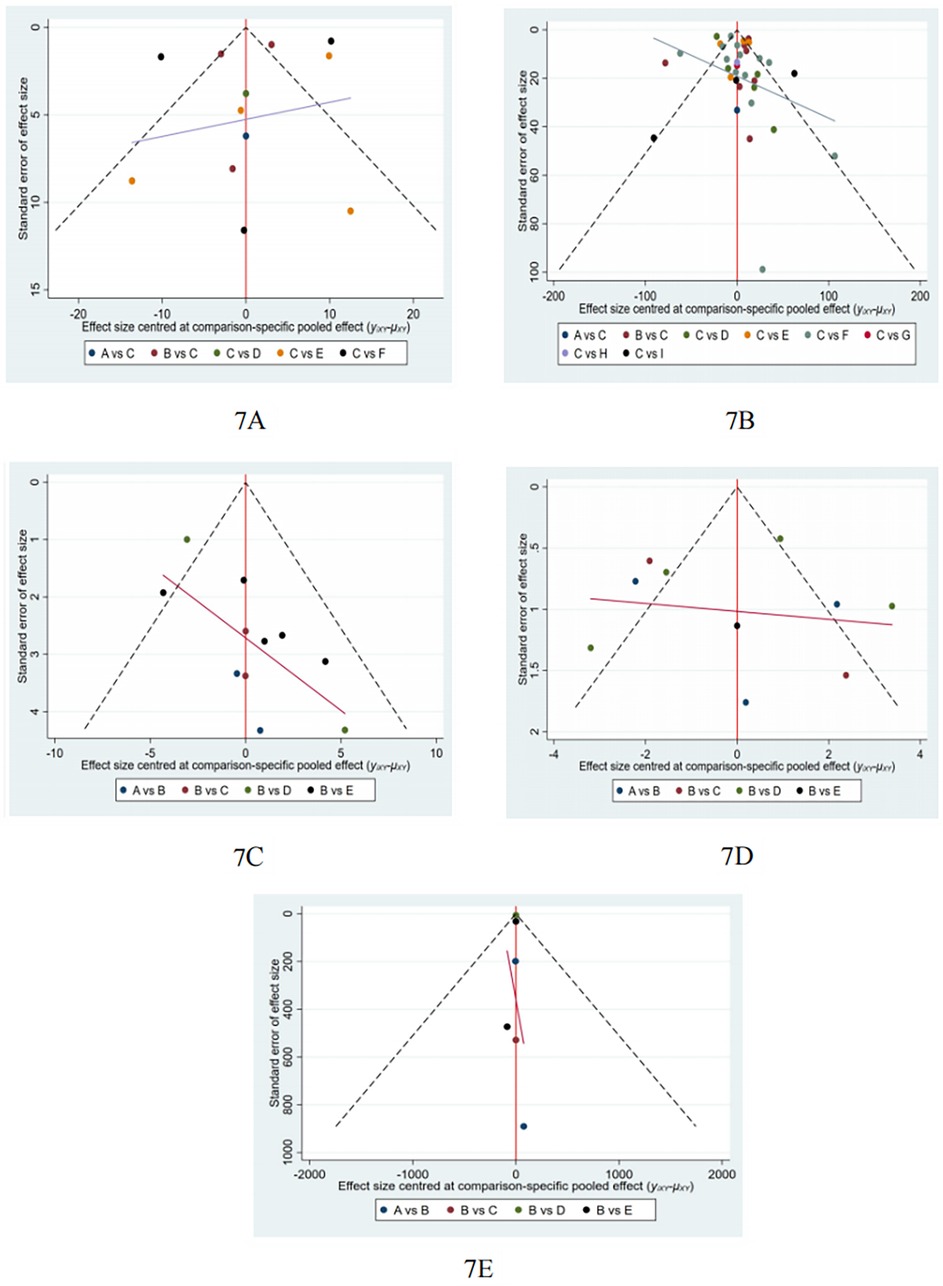
Figure 7. Funnel plot on publication bias. (A): MLHFQ; (B): 6MWD; (C): SGRQ; (D), CAT; (E): NT-proBNP.
4 Discussion
In this study, we compared the effects of different exercise interventions on the rehabilitation of patients with chronic cardiopulmonary dyspnoea. A total of 44 studies were included, encompassing eight different exercise protocols and involving 2,957 patients diagnosed with chronic cardiopulmonary dyspnoea, which constitutes a substantial sample size. Firstly, our study suggests that Yoga may be the most effective exercise intervention to reduce MLHFQ scores (SUCRA: 71.8%). Secondly, Yoga training demonstrated better results in increasing the 6MWD (SUCRA: 99.7%). Thirdly, Qigong was also identified as the most effective exercise intervention for decreasing SGRQ (SUCRA: 97.1%). Fourthly, compared to other treatment methods, Baduanjin may be the most suitable intervention for lowering CAT (SUCRA: 87.1%). Fifthly, Yoga might be more advantageous for decreasing the NT-proBNP (SUCRA: 83.4%).
The findings of this NMA are largely consistent with the findings of other recently published systematic reviews for chronic cardiopulmonary dyspnoea (90–92). Zhang et al. evaluate whether traditional mind-body therapy can be used as a complementary or alternative therapy for chronic cardiopulmonary dyspnoea (90). This systematic review enrolled only 34 studies involving 2,456 patients (90). This meta-analysis revealed that mind-body exercise significant improvements in the 6MWD for COPD and HF patients (90). Besides, Luo et al. revealed that mind-body exercises could significant improvements in the 6MWD for COPD patients (92). However, in this current NMA, study number and sample size were significantly increased (44 studies enrolling 2,957 patients). Moreover, many more types of outcomes have been evaluated, such as MLHFQ score, SGRQ, CAT, and NT-proBNP. Sujie, M. et al. revealed that mind-body exercises can reduced COPD patients' SGRQ score and CAT score (91). This is similar to our study. In our study, we revealed that Qigong was also identified as the most effective exercise intervention for decreasing SGRQ. When compared with other treatments, Baduanjin is likely the most appropriate intervention for decreasing CAT.
Our study indicates that Yoga is the most effective exercise intervention for reducing the MLHFQ scores. Yoga is a mind-body intervention that purposefully influences mental and physical health through concepts related to autonomic function (93). These findings are consistent with previous research. Previous studies have shown that MLHFQ scores are associated with depressive symptoms, and lower HRQoL is linked to a higher incidence of depression (94). The significant improvement of Yoga on MLHFQ score of patients with heart failure stems from its multi-target regulation of the autonomic nervous system and the immune system. Slow abdominal breathing, which is unique to Yoga, can enhance the tension of the cardiac vagus nerve (95). Acetylcholine released from vagus nerve endings can specifically bind to alpha7 acetylcholine receptor (α7Achr) (96, 97) inhibits the phosphorylation of the NF-κB signaling pathway, thus reducing the release of pro-inflammatory factors TNF-α and IL−6 (98). Clinical research shows that the decrease of inflammatory factors is directly related to the improvement of patients' fatigue and sitting breathing (98). Previous studies have shown that the hippocampal α7nAchr/NF-κB signal pathway is related to the antidepressant effect, and the depression score is also one of the MLHFQ scale (97). Taken together, these results suggest that Yoga may serve as a novel therapeutic approach for improving physical and mental function in elderly individuals (99).
Yoga training demonstrated better results in improving the 6MWD. These findings are consistent with previous research. Meta-analyses have shown a significant improvement in the 6MWD associated with Yoga (100). Results from Krishna et al. indicated that the Yoga group had a significant increase in 6MWD compared to the control group (88). Similarly, Jayadevappa et al. found significant improvements in 6MWD in the Yoga group at 6 months post-treatment compared to the health education group (101). The 6MWD has been shown to independently predict mortality, making it an important surrogate marker in the absence of hard clinical endpoints (102, 103). Numerous researchers have investigated how Yoga affects hypertension (104). A thorough meta-exploration of 44 randomized controlled trials found that nine studies showed Yoga to be more effective than traditional treatments in improving blood pressure (104). Measurements of diastolic and systolic blood pressure averaged reductions of 6 mmHg and 4 mmHg, respectively (105). Previous studies found that a Yoga therapy program, which included asanas and breath control, significantly reduced both systolic blood pressure (SBP) and diastolic blood pressure (DBP) (106–109). Although not a hard clinical endpoint, it is known that reductions in blood pressure translate to fewer cardiovascular events in other cardiovascular populations (110), and improvements in 6MWD are associated with lower cardiovascular mortality (111, 112). A community study focused on elderly populations observed a significant relationship between persistently elevated systolic blood pressure and the incidence of heart failure (113). During heart failure, sympathetic nervous activity is significantly increased and persists for a longer duration (113). Concurrently, the withdrawal of the vagus nerve is also an important aspect of heart failure (108). Elevated blood pressure is a strong predictor of outcomes in congestive heart failure (114–116). In addition to hemodynamic disturbances, increased neurohormonal activation through the sympathetic nervous system and the renin-angiotensin system is also associated with the progression of heart failure (117, 118). Previous studies have shown that adding Yoga therapy to standard medical treatment leads to significant reductions in blood pressure, resulting in a shift towards vagal dominance (108). Yoga is thought to improve baroreceptor sensitivity while reducing sympathetic activity, serving as a potential strategy for lowering blood pressure, which has significant implications for heart failure (104, 119). In addition to physical activity, Yoga also incorporates breathing exercises, relaxation techniques, and meditation (100). It is believed that breathing, meditation, and relaxation techniques may enhance parasympathetic activity, reduce sympathetic activity, and improve baroreflex sensitivity (119). By increasing baroreflex sensitivity and heart rate variability, a lower breathing frequency can facilitate vagal activation and diminish the effects of the sympathetic branch of the autonomic nervous system (100). As vagal impairment increases, both blood pressure and heart rate may decline (100). In addition, Yoga up-regulates the activity of endothelial nitric oxide synthase (eNOS) (120), reduces the peripheral vascular resistance through endothelium-dependent vasodilatation, and further optimizes the oxygen transport-utilization matching (121–123).
We implemented CAT and SGRQ scores, which are commonly used in the clinic to assess the QoL in patients with COPD. Baduanjin is also the most effective exercise intervention for decreasing CAT. Baduanjin, as a traditional aerobics exercise, is listed as the 97th sports item officially launched by the State General Administration of Sport in 2003 and has been widely promoted in China (124). Previous studies have confirmed that Baduanjin has a strong clinical effect on lung rehabilitation in COPD patients (125). Thus, Baduanjin has become an exercise prescription for COPD (126). These findings are consistent with previous research. Shuai et al. revealed that Baduanjin exercise may have the potential to enhance mental status, exercise ability, health status, quality of life, and lung function of COPD patients (127). The CAT scale, developed based on the St. George's Respiratory Questionnaire, has been shown to reliably assess the health status of COPD patients and has validity in measuring the effects of pulmonary rehabilitation and the impact of exercise interventions (128–130). Improvements in exercise capacity, lung function, and quality of life of patients with COPD may be closely related to the exercise patterns of the Baduanjin. The upper limb stretching and trunk extension movements of Baduanjin, as well as the combination of thoracic and abdominal respiration, effectively exercise the pectoral muscles, diaphragm, and abdominal muscles, thereby enhancing respiratory muscle contraction and improving lung capacity (131, 132). Baduanjin also combines mental focus and physical relaxation to reduce patient fatigue and increase psychological pleasure, thus enhancing exercise compliance (126, 133). In addition, the upper and lower extremity synergistic movements of Baduanjin can strengthen the assistive respiratory muscles, improve respiratory efficiency by increasing gas exchange, delay the deterioration of lung function, and reduce the levels of IL−8 and C-reactive protein in sputum to alleviate the inflammatory response (125, 134–136). Long-term training can improve the patient's respiratory muscle strength and endurance, thus improving respiratory function and alleviating the symptoms of dyspnea (136).
This NMA showed that Yoga showed better results in improving NT-proBNP. These findings are consistent with previous studies. The meta-analysis showed that Yoga improves NT-proBNP (137). The mechanism is closely related to the regulation of neuroendocrine and cardiovascular function. NT-proBNP, an inactive precursor of brain natriuretic peptide (BNP), is secreted by the ventricles in response to volume loading or pressure overload, and its elevated concentration is an important marker for the diagnosis of heart failure and assessment of the disease (138, 139). Studies have shown that Yoga, through a combination of asana training, breath control, and meditation, enhances parasympathetic activity and decreases sympathetic activity, which reduces ventricular filling pressures and myocardial wall tension-all key factors in stimulating NT-proBNP release (137, 140, 141). In addition, Yoga stretches can increase the efficiency of oxygen uptake by peripheral tissues, improve muscle strength, endurance and flexibility, and improve oxygen uptake, thereby reducing myocardial metabolic load and cardiovascular risk (137, 142, 143). Long-term practice can also reduce the secretion of stress hormones such as catecholamines, cortisol and aldosterone by regulating the hypothalamic-pituitary-adrenal axis, further alleviating the cardiac load and inflammatory response, and further inhibiting the release of NT-proBNP (46, 143). The synergistic effect of the above multiple pathways ultimately reduces NT-proBNP levels, suggesting that Yoga may provide a non-pharmacological intervention strategy for cardiovascular disease management by improving cardiac function and neuroendocrine homeostasis. Activation of the vagus nerve suppresses the renin-angiotensin-aldosterone system (RAAS), leading to decreased plasma renin activity and angiotensin II levels, which in turn reduces ventricular preload (144). Concurrently, Yoga enhances endothelial nitric oxide synthase (eNOS) activity, promoting endothelium-dependent vasodilation (120, 123). This mechanism lowers peripheral vascular resistance, reduces mean arterial pressure and vascular resistance index, and ultimately decreases ventricular wall stress (120, 123). Both of these pathways are closely associated with changes in NT-proBNP levels. However, future studies with larger samples are needed to demonstrate the above results.
Our research shows that Yoga may be the most effective mind-body exercise intervention method to improve MLHFQ, 6MWD and NT-proBNP. At present, there is no study on the economic benefits of Yoga in treating chronic cardiopulmonary dyspnoea, and it is impossible to make a horizontal comparison through QALY and other indexes. Philipson et al. demonstrated that Yoga interventions for young girls with functional abdominal pain disorders generate small quality-adjusted life years (QALYs) gains and monetary savings compared to standard healthcare, suggesting potential cost-effectiveness (145). Tew et al. found that Yoga was associated with an additional cost of £80.85 per participant and yielded an incremental 0.0178 QALYs per participant on average compared to usual care, indicating cost-effectiveness at conventional willingness-to-pay thresholds (146). Hartfiel et al. reported that, from a healthcare system perspective, Yoga interventions for musculoskeletal conditions incurred higher total costs than usual care due to implementation expenses (£54.52 more per participant), though healthcare resource utilization costs were £20.86 lower per person in the yoga group (147). Previous studies further revealed that Yoga was cost-effective from an organizational perspective and dominant from a societal perspective, delivering both health benefits and cost savings (148). Collectively, these studies suggest that Yoga interventions are associated with reduced healthcare resource utilization costs. Future research can carry out Yoga to analyze the economic benefits of patients with chronic cardiopulmonary dyspnoea to guide clinical application.
In the process of analysis, we conducted subgroup analysis according to follow-up, frequency and exercise duration. Our subgroup analyses stratified by follow-up duration, exercise frequency, and exercise duration consistently demonstrated that mind-body exercise produced statistically significant improvements in both 6MWD and MLHFQ scores compared to control interventions. These findings suggest the therapeutic benefits of mind-body exercise on 6MWD and MLHFQ are robust across varying implementation parameters. While the meta-analysis demonstrated significant improvements in SGRQ scores with mind-body exercise compared to controls, subsequent subgroup analyses stratified by intervention frequency (≥5 times/week vs. <5 times/week) and exercise duration (≥50 min vs. <50 min) revealed non-significant between-group differences. The observed attenuation of the therapeutic effects in the implementation parameters of the scheme indicates that the preliminary findings may need careful interpretation, which may reflect the sample size limitations in subgroup comparisons or the different reactivity based on exercise dose parameters. Meta-analysis showed that compared with the control group, the CAT score in the mind-body exercise group was significantly improved. Subsequently, the subgroup analyses stratified by follow-up duration revealed differential effects: in the >3 months cohort, interventions showed clinically meaningful CAT score reduction, whereas the ≤3 months subgroup exhibited non-significant changes. This subgroup analysis indicates that the possible cumulative treatment effects require longer intervention durations to show measurable clinical impacts.
This systematic review and NMA has several advantages, including being the first study to evaluate the effects of mind-body exercises on patients with chronic cardiopulmonary dyspnoea. The strength of this study lies in its methodology, which adheres to PRISMA guidelines and employs a robust search strategy designed to capture all types of adaptive mind-body activities for patients with chronic cardiopulmonary dyspnoea. Secondly, the studies included in this review were conducted across different continents, including Asia, the Americas, and Europe, highlighting that mind-body exercises are a global practice with the potential for widespread dissemination and impact. One of the strengths of this review is that it is based on a comprehensive search of several databases, focusing exclusively on randomized controlled trials.
However, when interpreting our findings, it is important to consider some limitations of the studies. Firstly, over half the studies had moderate/high risk of bias. However, this is unavoidable since participants in the mind-body exercise group were aware of the treatment involved during the intervention, and using unblinded coaches during the intervention would be unethical for enhancing training efficacy and patient safety. Future research should address blinding limitations by using sham exercises or objective outcome assessors for the control group. Secondly, the significant improvements in mind-body exercises require careful interpretation due to the heterogeneity of study designs and the short duration of interventions. Lack of standardization across studies can lead to differences in results. In addition, there is heterogeneity in study design and interventions, which makes analysis tricky and potentially error-prone. Compared with large-scale trials, small-scale trials can exaggerate the curative effects. Follow-up studies should standardize the duration of exercise and intensity of treatment for mind-body exercise. Thirdly, exercise outcomes are influenced by various factors such as the duration of each intervention session, intervention frequency, intervention period, patient physical condition, and severity of illness. Due to the limitations of our methodological approach, we could only focus on the overall effects of mind-body exercises, without considering the impact of other exercise parameters such as frequency, duration, and intensity. This study included 44 RCTs to examine the effects of different mind-body exercises on patients with chronic cardiopulmonary dyspnoea, but these mind-body exercises had different styles, intensities, and instructor-led variations, which would have had an impact on outcome metrics. In addition, the placebo effect from positive expectations during the study could have biased the results. When conducting multiple comparisons, we were unable to control for other variables, such as gender and age differences in exercise types and experimental settings. Additionally, the included studies had difficulty controlling for all external variables as rigorously as laboratory studies: On one hand, the varying characteristics of mind-body practices, such as the level of Tai Chi postures, skill proficiency, and the seamless experience brought by the mind-body integration, can influence the effectiveness of the exercise interventions. On the other hand, variations in the duration of chronic cardiopulmonary dyspnoea and health status contribute to the variability in outcomes related to improvements in MLHFQ, 6MWD, SGRQ, CAT, and NT-proBNP among chronic cardiopulmonary dyspnoea patients.
5 Conclusion
This study aimed to conduct a network meta-analysis to compare the effectiveness of different mind-body exercise interventions on the rehabilitation of patients with chronic cardiopulmonary dyspnoea. Our findings indicate that Yoga might be the most effective exercise intervention for reducing the MLHFQ scores, increasing the 6MWD, and decreasing the NT-proBNP. Qigong is also identified as the most effective exercise intervention for decreasing SGRQ. Compared to other treatment methods, Baduanjin may be the most suitable intervention for lowering CAT. Although there are variations in the effects of the interventions, the rankings of their effectiveness need to be interpreted cautiously due to the quality limitations of the original studies. Therefore, our study recommends that patients with chronic cardiopulmonary dyspnoea select appropriate mind-body exercises based on their individual conditions and adhere to them under the guidance of healthcare professionals. Future research should conduct more high-quality randomized controlled trials to investigate the impact of various forms of mind-body exercise on the effective prevention and treatment of chronic cardiopulmonary dyspnoea. Follow-up studies should standardize the duration of exercise and intensity of treatment for mind-body exercise.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
YL: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Formal analysis. JW: Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. RL: Conceptualization, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank all the reviewers for their assistance and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1546996/full#supplementary-material
References
1. Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet. (2022) 399(10342):2227–42. doi: 10.1016/S0140-6736(22)00470-6
3. Campbell P, Rutten FH, Lee MM, Hawkins NM, Petrie MC. Heart failure with preserved ejection fraction: everything the clinician needs to know. Lancet. (2024) 403(10431):1083–92. doi: 10.1016/S0140-6736(23)02756-3 Erratum in: Lancet. 2024 March 16;403(10431):1026. doi: 10.1016/S0140-6736(24)00494-X.38367642
4. Vicent L, Nuñez Olarte JM, Puente-Maestu L, Oliva A, López JC, Postigo A, et al. Degree of dyspnoea at admission and discharge in patients with heart failure and respiratory diseases. BMC Palliat Care. (2017) 16(1):35. doi: 10.1186/s12904-017-0208-x
5. Hayen A, Herigstad M, Pattinson KT. Understanding dyspnea as a complex individual experience. Maturitas. (2013) 76:45–50. doi: 10.1016/j.maturitas.2013.06.005
6. Budhwar N, Syed Z. Chronic dyspnea: diagnosis and evaluation. Am Fam Physician. (2020) 101:542–8.32352727
7. Karnani NG, Reisfield GM, Wilson GR. Evaluation of chronic dyspnea. Am Fam Physician. (2005) 71:1529–37.15864893
8. Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats AJS. Global burden of heart failure: a comprehensive and updated review of epidemiology. Cardiovasc Res. (2023 Jan 18) 118(17):3272–87. doi: 10.1093/cvr/cvac013. Erratum in: Cardiovasc Res. 2023 Jun 13;119(6):1453. doi: 10.1093/cvr/cvad026.
9. Moll M, Silverman EK. Precision approaches to chronic obstructive pulmonary disease management. Annu Rev Med. (2024) 75:247–62. doi: 10.1146/annurev-med-060622-101239
10. Dibben GO, Faulkner J, Oldridge N, Rees K, Thompson DR, Zwisler AD, et al. Exercise-based cardiac rehabilitation for coronary heart disease: a meta-analysis. Eur Heart J. (2023) 44(6):452–69. doi: 10.1093/eurheartj/ehac747
11. Patti A, Merlo L, Ambrosetti M, Sarto P. Exercise-based cardiac rehabilitation programs in heart failure patients. Heart Fail Clin. (2021) 17(2):263–71. doi: 10.1016/j.hfc.2021.01.007
12. Molloy CD, Long L, Mordi IR, Bridges C, Sagar VA, Davies EJ, et al. Exercise-based cardiac rehabilitation for adults with heart failure - 2023 cochrane systematic review and meta-analysis. Eur J Heart Fail. (2023) 25(12):2263–73. doi: 10.1002/ejhf.3046
13. Hui J, Wang Y, Zhao J, Cong W, Xu F. Effects of tai chi on health status in adults with chronic heart failure: a systematic review and meta-analysis. Front Cardiovasc Med. (2022) 9:953657. doi: 10.3389/fcvm.2022.953657
14. Jiang W, Liao S, Chen X, Lundborg CS, Marrone G, Wen Z, et al. Taichi and Qigong for depressive symptoms in patients with chronic heart failure: a systematic review with meta-analysis. Evid Based Complement Alternat Med. (2021) 2021:5585239. doi: 10.1155/2021/5585239
15. Gok Metin Z, Ejem D, Dionne-Odom JN, Turkman Y, Salvador C, Pamboukian S, et al. Mind-Body interventions for individuals with heart failure: a systematic review of randomized trials. J Card Fail. (2018) 24(3):186–201. doi: 10.1016/j.cardfail.2017.09.008
16. Xiao CM, Zhuang YC. Efficacy of Liuzijue Qigong in individuals with chronic obstructive pulmonary disease in remission. J Am Geriatr Soc. (2015) 63:1420–5. doi: 10.1111/jgs.13478
17. Redwine LS, Tsuang M, Rusiewicz A, Pandzic I, Cammarata S, Rutledge T, et al. A pilot study exploring the effects of a 12-week t'ai chi intervention on somatic symptoms of depression in patients with heart failure. J Altern Complement Med. (2012) 18(8):744–8. doi: 10.1089/acm.2011.0314
18. Barrow DE, Bedford A, Ives G, O'Toole L, Channer KS. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J. (2007) 83(985):717–21. doi: 10.1136/pgmj.2007.061267
19. Li Z, Liu S, Wang L, Smith L. Mind-body exercise for anxiety and depression in COPD patients: a systematic review and meta-analysis. Int J Environ Res Public Health. (2019) 17(1):22. doi: 10.3390/ijerph17010022
20. Infeld M, Wahlberg K, Cicero J, Plante TB, Meagher S, Novelli A, et al. Effect of personalized accelerated pacing on quality of life, physical activity, and atrial fibrillation in patients with preclinical and overt heart failure with preserved ejection fraction: the myPACE randomized clinical trial. JAMA Cardiol. (2023) 8(3):213–21. doi: 10.1001/jamacardio.2022.5320
21. Carvalho VO, Guimarães GV, Carrara D, Bacal F, Bocchi EA. Validation of the Portuguese version of the Minnesota living with heart failure questionnaire. Arq Bras Cardiol. (2009) 93(1):39–44. doi: 10.1590/S0066-782X2009000700008
22. Tian C, Zhang J, Rong J, Ma W, Yang H. Impact of nurse-led education on the prognosis of heart failure patients: a systematic review and meta-analysis. Int Nurs Rev. (2024) 71(1):180–8. doi: 10.1111/inr.12852
23. Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. (1985) 132(8):919–23.3978515
24. Spencer S, Calverley PM, Sherwood Burge P, Jones PW. Inhaled steroids in obstructive lung disease. Health status deterioration in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. (2001) 163(1):122–8. doi: 10.1164/ajrccm.163.1.2005009
25. Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St. George’s respiratory questionnaire. Am Rev Respir Dis. (1992) 145(6):1321–7. doi: 10.1164/ajrccm/145.6.1321
26. Meguro M, Barley EA, Spencer S, Jones PW. Development and validation of an improved, COPD-specific version of the St. George respiratory questionnaire. Chest. (2007) 132(2):456–63. doi: 10.1378/chest.06-0702
27. El Rhazi K, Nejjari C, Benjelloun MC, Bourkadi J, Afif H, Serhier Z, et al. Validation of the St. George’s respiratory questionnaire in patients with COPD or asthma in Morocco. Int J Tuberc Lung Dis. (2006) 10(11):1273–8.17131788
28. Furukawa T, Taniguchi H, Ando M, Kondoh Y, Kataoka K, Nishiyama O, et al. The St. George’s respiratory questionnaire as a prognostic factor in IPF. Respir Res. (2017) 18(1):18. doi: 10.1186/s12931-017-0503-3
29. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. (2009) 34(3):648–54. doi: 10.1183/09031936.00102509
30. Tsiligianni IG, van der Molen T, Moraitaki D, Lopez I, Kocks JW, Karagiannis K, et al. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm Med. (2012) 12:20. doi: 10.1186/1471-2466-12-20
31. Bay M, Kirk V, Parner J, Hassager C, Nielsen H, Krogsgaard K, et al. NT-proBNP: a new diagnostic screening tool to differentiate between patients with normal and reduced left ventricular systolic function. Heart. (2003) 89(2):150–4. doi: 10.1136/heart.89.2.150
32. Gonzalez-Saenz de Tejada M, Bilbao A, Ansola L, Quirós R, García-Perez L, Navarro G, et al. Responsiveness and minimal clinically important difference of the Minnesota living with heart failure questionnaire. Health Qual Life Outcomes. (2019) 17(1):36. doi: 10.1186/s12955-019-1104-2
33. Ammous O, Feki W, Lotfi T, Khamis AM, Gosselink R, Rebai A, et al. Inspiratory muscle training, with or without concomitant pulmonary rehabilitation, for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. (2023) 1(1):CD013778. doi: 10.1002/14651858.CD013778.pub2
34. Prior TS, Hoyer N, Hilberg O, Shaker SB, Davidsen JR, Bendstrup E. Responsiveness and minimal clinically important difference of SGRQ-I and K-BILD in idiopathic pulmonary fibrosis. Respir Res. (2020) 21(1):91. doi: 10.1186/s12931-020-01359-3
35. Matsuda T, Kondoh Y, Takei R, Sasano H, Fukihara J, Yamano Y, et al. Responsiveness and minimal clinically important difference of the COPD assessment test in fibrotic interstitial lung disease. Respir Investig. (2024) 62(6):1088–93. doi: 10.1016/j.resinv.2024.08.006
36. Stienen S, Salah K, Moons AH, Bakx AL, van Pol P, Kortz RAM, et al. NT-proBNP (N-Terminal pro-B-type natriuretic peptide)-guided therapy in acute decompensated heart failure: pRIMA II randomized controlled trial (can NT-ProBNP-guided therapy during hospital admission for acute decompensated heart failure reduce mortality and readmissions? Circulation. (2018) 137(16):1671–83. doi: 10.1161/CIRCULATIONAHA.117.029882
37. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
38. Li D, Chen P. Effects of aquatic exercise and land-based exercise on cardiorespiratory fitness, motor function, balance, and functional independence in stroke patients-a meta-analysis of randomized controlled trials. Brain Sci. (2021) 11(8):1097. doi: 10.3390/brainsci11081097
39. Jackson D, Riley R, White IR. Multivariate meta-analysis: potential and promise. Stat Med. (2011) 30:2481–98. doi: 10.1002/sim.4172
40. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al.; PRISMA-P group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J. (2015) 350:g7647. doi: 10.1136/bmj.g7647 Erratum in: BMJ. 2016 July 21;354:i4086. doi: 10.1136/bmj.i4086.
41. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. (2011) 64:163–71. doi: 10.1016/j.jclinepi.2010.03.016
42. Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One. (2013) 8(10):e76654. doi: 10.1371/journal.pone.0076654
43. Marotta N, Demeco A, Moggio L, Marinaro C, Pino I, Barletta M, et al. Comparative effectiveness of breathing exercises in patients with chronic obstructive pulmonary disease. Complement Ther Clin Pract. (2020) 41:101260. doi: 10.1016/j.ctcp.2020.101260
44. Khera R, Murad MH, Chandar AK, Dulai PS, Wang Z, Prokop LJ, et al. Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis. JAMA. (2016) 315(22):2424–34. doi: 10.1001/jama.2016.7602 Erratum in: JAMA. 2016 September 6;316(9):995. doi: 10.1001/jama.2016.11657.27299618
45. Ma C, Zhou W, Jia Y, Tang Q. Effects of home-based baduanjin combined with elastic band exercise in patients with chronic heart failure. Eur J Cardiovasc Nurs. (2022) 21(6):587–96. doi: 10.1093/eurjcn/zvab128
46. Jain AK, Subhash CM, Bhola SV, Kushal M, Ashwini M, Jitendrapal SS. Effect of yoga lifestyle in patients with heart failure: a randomized control trial. Int J Yoga. (2022) 15(1):40–4. doi: 10.4103/ijoy.ijoy_183_21
47. Zhou M, Zhang H, Li F, Yu Z, Yuan C, Oliver B, et al. Pulmonary daoyin as a traditional Chinese medicine rehabilitation programme for patients with IPF: a randomized controlled trial. Respirology. (2021) 26(4):360–9. doi: 10.1111/resp.13972
48. Liang Z, Chi Z, Xian- kui W. Influence of healthcare Qigong- 6- character formulas (Liuzijue) on heart function in patients with chronic heart failure. Chin J Evid Based Cardiovasc Med. (2017) 9:659–62.
49. Zhen Z, Shiqin Z. Clinical study on the effect of early intervention of health Qigong·Liu Zi Jue on cardiac function of patients with chronic pulmonary heart disease. Jiangsu Tradit Chin Med. (2010) 42:18–9.
50. Min X. The effect of horizontal baduanjin rehabilitation exercise on the quality of life of patients with stable heart failure of grade III − IV of cardiac function. Electron J Clin Med Lit. (2019) 6(99):33–4. doi: 10.16281/j.cnki.jocml.2019.99.025
51. Hägglund E, Hagerman I, Dencker K, Strömberg A. Effects of yoga versus hydrotherapy training on health-related quality of life and exercise capacity in patients with heart failure: a randomized controlled study. Eur J Cardiovasc Nurs. (2017) 16(5):381–9. doi: 10.1177/1474515117690297
52. Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. (2013) 19(2):77–84. doi: 10.1111/chf.12005
53. Redwine LS, Wilson K, Pung MA, Chinh K, Rutledge T, Mills PJ, et al. A randomized study examining the effects of mild-to-moderate group exercises on cardiovascular, physical, and psychological well-being in patients with heart failure. J Cardiopulm Rehabil Prev. (2019) 39(6):403–8. doi: 10.1097/HCR.0000000000000430
54. Caminiti G, Volterrani M, Marazzi G, Cerrito A, Massaro R, Arisi A, et al. Tai chi enhances the effects of endurance training in the rehabilitation of elderly patients with chronic heart failure. Rehabil Res Pract. (2011) 2011:761958. doi: 10.1155/2011/761958
55. Chao H. Tai chi baoqiu yunshou’s effect on the rehabilitation of cardiac function in patients with coronary heart disease and chronic heart failure (NYHA III) (dissertation). Fujian University of Traditional Chinese Medicine (2014).
56. Meili Y. A randomized controlled study of baduanjin in the second- stage rehabilitation of patients with coronary heart disease and chronic heart failure (dissertation). Beijing University of Chinese Medicine (2018).
57. Polkey MI, Qiu ZH, Zhou L, Zhu MD, Wu YX, Chen YY, et al. Tai chi and pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest. (2018) 153(5):1116–24. doi: 10.1016/j.chest.2018.01.053
58. Chan AW, Lee A, Lee DT, Suen LK, Tam WW, Chair SY, et al. The sustaining effects of Tai Chi Qigong on physiological health for COPD patients: a randomized controlled trial. Complement Ther Med. (2013) 21(6):585–94. doi: 10.1016/j.ctim.2013.09.008
59. Chan AW, Lee A, Lee DT, Sit JW, Chair SY. Evaluation of the sustaining effects of Tai Chi Qigong in the sixth month in promoting psychosocial health in COPD patients: a single-blind, randomized controlled trial. ScientificWorldJournal. (2013) 2013:425082. doi: 10.1155/2013/425082
60. Shuting D, Bin X, Chunxia W, Lianming D, Fubin Y, Zhenlan L, et al. The influence of Tai Chi exercise on bode index and SGRQ score of patients with chronic obstructive pulmonary disease. Chin J Sports Med. (2013) 32(05):403–7. doi: 10.16038/j.1000-6710.2013.05.007
61. Shuting D, Lianming D, Chunxia W, Fubin Y, Bin X, Zhenlan L, et al. Effects of tai chi exercise on exercise tolerance and pulmonary function in patients with chronic obstructive pulmonary disease. Chin J Rehabil Med. (2013) 28:374–6.
62. Zaifang R, Xia Z, Gaihua H. The effect of Tai Chi Zen on exercise capacity and quality of life in patients with chronic obstructive pulmonary disease. Chin J Tradit Chin Med. (2017) 32:3507–10.
63. Yu Z. Study on the effect of pulmonary rehabilitation treatment on lung function and quality of life in patients with stable chronic obstructive pulmonary disease. Chin Foreign Med Res. (2019) 17(08):167–9. doi: 10.14033/j.cnki.cfmr.2019.08.081
64. Xingcai Z, Yuli C, Wei Z, Xianhai C, Xinhua J, Xinyue Z, et al. The effect of twenty- four- style taijiquan and respiratory function training assisted by western medicine on patients with chronic obstructive pulmonary disease in stable stage. Chin Med J. (2014) 55(22):1937–41. doi: 10.13288/j.11-2166/r.2014.22.014
65. Meng D, Chenguang G, Yan M. A comparative study on the rehabilitation effects of health Qigong and aerobic power vehicle exercise on chronic obstructive pulmonary disease. 2015 tenth national sports science conference; Hangzhou, Zhejiang, China (2015) 3.
66. Yi Z, Ning L, Hongzhu J. The effect of early intervention of Wuqinxi on patients with stable chronic obstructive pulmonary disease. J Liaoning Univ Tradit Chin Med. (2010) 12(06):107–10. doi: 10.13194/j.jlunivtcm.2010.06.109.zhuy.024
67. Dong X, Wang X, Jia N, Chen X, Ding M. A comparison between qigong exercise and cycle ergometer exercise for the rehabilitation of chronic obstructive pulmonary disease: a pilot randomized controlled trial (CONSORT). Medicine (Baltimore). (2021) 100(21):e26010. doi: 10.1097/MD.0000000000026010
68. Jia Z, Xueqin L. Effect of health education combined with breathing exercises on pulmonary function of COPD patients. J Clin Lab. (2017) 6:522–3.
69. Dongping F, Ying L, Xiulan Z. Application and effect of “Liu zi jue breathing exercise” in continuous nursing of patients with chronic obstructive pulmonary disease in stable stage. J Nurs Manage. (2012) 12:813–5.
70. Jinxiu C. The effect of traditional Liuzijue breathing exercises on the quality of life of patients with chronic obstructive pulmonary disease in stable stage. Chin J Nat Med. (2009) 11(06):412–4. doi: 10.16505/j.2095-0136.2009.06.021
71. Qi C, Zhonghao T, Lingyi M, Xing Z, Wei Z. Evaluation of the curative effect of improved TCM breathing guidance technology based on comprehensive pulmonary rehabilitation management on patients with stable COPD in southern Xinjiang. J Shanghai Univ Tradit Chin Med. (2021) 35(03):33–8. doi: 10.16306/j.1008-861x.2021.03.007
72. Liu X-D, Jin H-Z, Ng BHP, Gu YH, Wu YC, Lu G. Therapeutic effects of qigong in patients with COPD: a randomized controlled trial. Hong Kong J Occup Ther. (2012) 22:38–46. doi: 10.1016/j.hkjot.2012.06.002
73. Qing L, Weihua F, Cui L. The effect of Tai Chi combined with breathing function training on the rehabilitation of patients with chronic obstructive pulmonary disease in stable stage. Chin J Rehabil Med. (2012) 27:825–8.
74. Songmei C. Effects of Baduanjin combined with multiple respiratory rehabilitation training on lung function, MMRC score and quality of life in elderly patients with chronic obstructive pulmonary disease. Lab Med Clin. (2020) 17:2669–72.
75. Yanchan Z. Clinical study of breath baduanjin on pulmonary rehabilitation of severe and extremely severe COPD in stable phase (dissertation). Guangzhou University of Chinese Medicine (2019).
76. Dafan H, Fang H, Shiping Y. Study on the effect of Baduanjin combined with breathing training on patients with chronic obstructive pulmonary disease in the community. Guangzhou Med. (2017) 48:29–32.
77. Ge Y. Clinical study on the influence of baduanjin and breathing exercises on the quality of life of patients with moderate and severe COPD (dissertation). Guangzhou University of Chinese Medicine (2013).
78. Ying G. Study on health qigong·yijin channel promoting pulmonary rehabilitation of patients with chronic obstructive pulmonary disease in stable stage (dissertation). Nanjing University of Chinese Medicine (2015).
79. Ng BH, Tsang HW, Jones AY, So CT, Mok TY. Functional and psychosocial effects of health Qigong in patients with COPD: a randomized controlled trial. J Altern Complement Med. (2011) 17(3):243–51. doi: 10.1089/acm.2010.0215
80. Ng L, Chiang LK, Tang R, Siu C, Fung L, Lee A, et al. Effectiveness of incorporating tai chi in a pulmonary rehabilitation program for chronic obstructive pulmonary disease (COPD) in primary care-a pilot randomized controlled trial. Eur J Integr Med. (2014) 6:248–58. doi: 10.1016/j.eujim.2014.01.007
81. Haijuan L, Yongwei X, Chao Y, Jianlin Z, Huilin L. The effect of Baduanjin combined with pulmonary function rehabilitation training on lung function, exercise endurance and quality of life in patients with chronic obstructive pulmonary disease in stable stage. Mod Biomed Prog. (2021) 21(10):1859–62. doi: 10.13241/j.cnki.pmb.2021.10.012
82. Yeh GY, McCarthy EP, Wayne PM, Stevenson LW, Wood MJ, Forman D, et al. Tai Chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. (2011) 171(8):750–7. doi: 10.1001/archinternmed.2011.150
83. Yeh GY, Wayne PM, Phillips RS. T’ai Chi exercise in patients with chronic heart failure. Med Sport Sci. (2008) 52:195–208. doi: 10.1159/000134300
84. Donesky D, Selman L, McDermott K, Citron T, Howie-Esquivel J. Evaluation of the feasibility of a home-based TeleYoga intervention in participants with both chronic obstructive pulmonary disease and heart failure. J Altern Complement Med. (2017) 23(9):713–21. doi: 10.1089/acm.2015.0279
85. Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, et al. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J Card Fail. (2008) 14(5):407–13. doi: 10.1016/j.cardfail.2007.12.007
86. Yeh GY, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, et al. Effects of Tai Chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. (2004) 117(8):541–8. doi: 10.1016/j.amjmed.2004.04.016
87. Chen X, Jiang W, Olson TP, Lundborg CS, Wen Z, Lu W, et al. Feasibility and preliminary effects of the BESMILE-HF program on chronic heart failure patients: a pilot randomized controlled trial. Front Cardiovasc Med. (2021) 8:715207. doi: 10.3389/fcvm.2021.715207
88. Krishna BH, Pal P, Pal GK, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. Yoga improves quality of life and functional capacity in heart failure patients. Biomed Res India. (2014) 25:178–82.
89. Srisoongnern S, Pajareya K, Sriboon R, Thanakiatpinyo T, Chirakarnjanakorn S, Thirapatarapong W. Effects of buddhist walking meditation on exercise capacity and quality of life of patients with chronic heart failure: a randomized controlled trial. Heart Lung. (2021) 50(3):363–8. doi: 10.1016/j.hrtlng.2021.02.005
90. Zhang T, Zhou R, Wang T, Xin Y, Liu X, Huang H. Effects of traditional mind-body movement therapy on chronic cardiopulmonary dyspnoea: a systematic review and meta-analysis. Thorax. (2023) 78(1):69–75. doi: 10.1136/thoraxjnl-2021-218030
91. Sujie M, Kaiwen X, Hong X, Xiujin G. The impact of traditional mind-body exercises on pulmonary function, exercise capacity, and quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne). (2024) 11:1359347. doi: 10.3389/fmed.2024.1359347
92. Luo X, Zhang J, Castelberg R, Wu T, Yu P, He C, et al. The effects of traditional Chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. PLoS One. (2016) 11(9):e0161564. doi: 10.1371/journal.pone.0161564
93. Alexander GK, Rollins K, Walker D, Wong L, Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health Saf. (2015) 63(10):462–70. quiz 471. doi: 10.1177/2165079915596102
94. Trindade AFV, Silva WT, Lima VP, Mendonça VA, Lacerda ACR, Ávila MR, et al. Assessment of health-related quality of life in patients with Chagas cardiomyopathy using Minnesota living with heart failure questionnaire: a validation study. Trop Med Int Health. (2024) 29(1):6–12. doi: 10.1111/tmi.13944
95. Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. (2012) 78(5):571–9. doi: 10.1016/j.mehy.2012.01.021
96. Guo L, Chen Q, Gao Y, Jiang H, Zhou F, Zhang F, et al. CDP-choline modulates cholinergic signaling and gut microbiota to alleviate DSS-induced inflammatory bowel disease. Biochem Pharmacol. (2023) 217:115845. doi: 10.1016/j.bcp.2023.115845
97. Wang JY, Zhang Y, Chen Y, Wang Y, Li SY, Wang YF, et al. Mechanisms underlying antidepressant effect of transcutaneous auricular vagus nerve stimulation on CUMS model rats based on hippocampal α 7nAchR/NF-κ B signal pathway. J Neuroinflammation. (2021) 18(1):291. doi: 10.1186/s12974-021-02341-6
98. Pavón-Romero GF, Serrano-Pérez NH, García-Sánchez L, Ramírez-Jiménez F, Terán LM. Neuroimmune pathophysiology in asthma. Front Cell Dev Biol. (2021) 9:663535. doi: 10.3389/fcell.2021.663535
99. Kwok JYY, Kwan JCY, Auyeung M, Mok VCT, Lau CKY, Choi KC, et al. Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with Parkinson disease: a randomized clinical trial. JAMA Neurol. (2019) 76(7):755–63. doi: 10.1001/jamaneurol.2019.0534
100. Dutta A, Mooventhan A, Nivethitha L. Yoga as adjunct therapy for chronic heart failure: a systematic review and meta-analysis of randomized controlled trials. Avicenna J Med. (2023) 13:151–62. doi: 10.1055/s-0043-1774738
101. Jayadevappa R, Johnson JC, Bloom BS, Nidich S, Desai S, Chhatre S, et al. Effectiveness of transcendental meditation on functional capacity and quality of life of African Americans with congestive heart failure: a randomized control study. Ethn Dis. (2007) 17(1):72–7. Erratum in: Ethn Dis. 2007 Summer;17(3):595.17274213
102. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. (2022) 79(17):e263–421. doi: 10.1016/j.jacc.2021.12.012 Erratum in: J Am Coll Cardiol. 2023 April 18;81(15):1551. doi: 10.1016/j.jacc.2023.03.002.35379503
103. Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, et al. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD investigators. JAMA. (1993) 270(14):1702–7. doi: 10.1001/jama.1993.03510140062030
105. Yadav R, Yadav RK, Sarvottam K, Netam R. Framingham risk score and estimated 10-year cardiovascular disease risk reduction by a short-term yoga-based LifeStyle intervention. J Altern Complement Med. (2017) 23(9):730–7. doi: 10.1089/acm.2016.0309
106. McCaffrey R, Ruknui P, Hatthakit U, Kasetsomboon P. The effects of yoga on hypertensive persons in Thailand. Holist Nurs Pract. (2005) 19(4):173–80. doi: 10.1097/00004650-200507000-00009
107. Sieverdes JC, Mueller M, Gregoski MJ, Brunner-Jackson B, McQuade L, Matthews C, et al. Effects of hatha yoga on blood pressure, salivary α-amylase, and cortisol function among normotensive and prehypertensive youth. J Altern Complement Med. (2014) 20(4):241–50. doi: 10.1089/acm.2013.0139
108. Krishna BH, Pravati P, Pal GK, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. Effect of yoga therapy on heart rate, blood pressure and cardiac autonomic function in heart failure. J Clin Diagn Res. (2014) 8(1):14–6. doi: 10.7860/JCDR/2014/7844.3983
109. Mathew D, Rangasamy M. Effect of yoga therapy on insomnia severity and systolic blood pressure in aged women: a 12-week intervention study conducted in Kerala. Cureus. (2024) 16(3):e57169. doi: 10.7759/cureus.57169
110. Lee VYJ, Houston L, Perkovic A, Barraclough JY, Sweeting A, Yu J, et al. The effect of weight loss through lifestyle interventions in patients with heart failure with preserved ejection fraction-A systematic review and meta-analysis of randomised controlled trials. Heart Lung Circ. (2024) 33(2):197–208. doi: 10.1016/j.hlc.2023.11.022
111. Wilson PW, D'Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the framingham experience. Arch Intern Med. (2002) 162(16):1867–72. doi: 10.1001/archinte.162.16.1867
112. Dasari TW, Patel B, Wayangankar SA, Alexander D, Zhao YD, Schlegel J, et al. Prognostic value of 6-minute walk distance in patients undergoing percutaneous coronary intervention: a veterans affairs prospective study. Tex Heart Inst J. (2020) 47(1):10–4. doi: 10.14503/THIJ-17-6471
113. Conen D, Chae CU, Guralnik JM, Glynn RJ. Influence of blood pressure and blood pressure change on the risk of congestive heart failure in the elderly. Swiss Med Wkly. (2010) 140(13-14):202–8. doi: 10.4414/smw.2010.12780
114. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiems. Lancet. (2002) 360(9349):1903–13. doi: 10.1016/s0140-6736(02)11911-8 Erratum in: Lancet. 2003 March 22;361(9362):1060.12493255
115. Conen D, Ridker PM, Buring JE, Glynn RJ. Risk of cardiovascular events among women with high normal blood pressure or blood pressure progression: prospective cohort study. Br Med J. (2007) 335(7617):432. doi: 10.1136/bmj.39269.672188.AE
116. Bernardi L, Gabutti A, Porta C, Spicuzza L. Slow breathing reduces chemoreflex response to hypoxia and hypercapnia, and increases baroreflex sensitivity. J Hypertens. (2001) 19(12):2221–9. doi: 10.1097/00004872-200112000-00016
117. Sigurdsson A, Swedberg K. The role of neurohormonal activation in chronic heart failure and postmyocardial infarction. Am Heart J. (1996) 132:229–34. doi: 10.1016/S0002-8703(96)90558-X
118. Johnson W, Omland T, Hall C, Lucas C, Myking OL, Collins C, et al. Neurohormonal activation rapidly decreases after intravenous therapy with diuretics and vasodilators for class IV heart failure. J Am Coll Cardiol. (2002) 39(10):1623–9. doi: 10.1016/s0735-1097(02)01814-4
119. Prabhu S, Nayak K, Kadiyali A, Devasia T, Varadaraju R, Moodukudru M. Physical and psychological impact of yoga therapy in improving heart failure. Trop Doct. (2023) 53(4):455–9. doi: 10.1177/00494755231180633
120. Shetty SP, Patil AV, Khodnapur JP, Kotennavar M, Jaju P, Savanth M, et al. The impact of bhramari pranayama and om chanting on post-operative wound healing: a focus on the nitric oxide pathway. Cureus. (2024) 16(11):e73511. doi: 10.7759/cureus.73511
121. Wang M, Deng J, Lai H, Lai Y, Meng G, Wang Z, et al. Vagus nerve stimulation ameliorates renal ischemia-reperfusion injury through inhibiting NF- κ B activation and iNOS protein expression. Oxid Med Cell Longev. (2020) 2020:7106525. doi: 10.1155/2020/7106525
122. Shahrokhi N, Khaksari M, Nourizad S, Shahrokhi N, Soltani Z, Gholamhosseinian A. Protective effects of an interaction between vagus nerve and melatonin on gastric ischemia/reperfusion: the role of oxidative stress. Iran J Basic Med Sci. (2016) 19(1):72–9.27096067
123. Hunter SD, Laosiripisan J, Elmenshawy A, Tanaka H. Effects of yoga interventions practised in heated and thermoneutral conditions on endothelium-dependent vasodilatation: the bikram yoga heart study. Exp Physiol. (2018) 103(3):391–6. doi: 10.1113/EP086725
124. Bi J, Yang W, Hao P, Zhao Y, Wei D, Sun Y, et al. WeChat as a platform for baduanjin intervention in patients with stable chronic obstructive pulmonary disease in China: retrospective randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9(2):e23548. doi: 10.2196/23548
125. Yang Y, Chen K, Tang W, Xie X, Xiao W, Xiao J, et al. Influence of baduanjin on lung function, exercise capacity, and quality of life in patients with mild chronic obstructive pulmonary disease. Medicine (Baltimore). (2020) 99(37):e22134. doi: 10.1097/MD.0000000000022134
126. Liu SJ, Ren Z, Wang L, Wei GX, Zou L. Mind-body (Baduanjin) exercise prescription for chronic obstructive pulmonary disease: a systematic review with meta-analysis. Int J Environ Res Public Health. (2018) 15(9):1830. doi: 10.3390/ijerph15091830
127. Shuai Z, Xiao Q, Ling Y, Zhang Y, Zhang Y. Efficacy of traditional Chinese exercise (Baduanjin) on patients with stable COPD: a systematic review and meta-analysis. Complement Ther Med. (2023) 75:102953. doi: 10.1016/j.ctim.2023.102953
128. Watz H, Pitta F, Rochester CL, Garcia-Aymerich J, ZuWallack R, Troosters T, et al. An official European respiratory society statement on physical activity in COPD. Eur Respir J. (2014) 44(6):1521–37. doi: 10.1183/09031936.00046814
129. van der Molen T, Miravitlles M, Kocks JW. COPD management: role of symptom assessment in routine clinical practice. Int J Chron Obstruct Pulmon Dis. (2013) 8:461–71. doi: 10.2147/COPD.S49392
130. Jones PW, Brusselle G, Dal Negro RW, Ferrer M, Kardos P, Levy ML, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. (2011) 38(1):29–35. doi: 10.1183/09031936.00177210. Erratum in: Eur Respir J. 2012 Jan;39(1):230.21565915
131. Cao A, Feng F, Zhang L, Zhou X. Baduanjin exercise for chronic obstructive pulmonary disease: an updated systematic review and meta-analysis. Clin Rehabil. (2020) 34(8):1004–13. doi: 10.1177/0269215520926635
132. Jing L, Jin Y, Zhang X, Wang F, Song Y, Xing F. The effect of baduanjin qigong combined with CBT on physical fitness and psychological health of elderly housebound. Medicine (Baltimore). (2018) 97(51):e13654. doi: 10.1097/MD.0000000000013654
133. Zou L, Pan Z, Yeung A, Talwar S, Wang C, Liu Y, et al. A review study on the beneficial effects of Baduanjin. J Altern Complement Med. (2018) 24(4):324–35. doi: 10.1089/acm.2017.0241
134. Chan JS, Ho RT, Chung KF, Wang CW, Yao TJ, Ng SM, et al. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Complement Alternat Med. (2014) 2014:106048. doi: 10.1155/2014/106048
135. Shi D. Influence of exercise health care on airway inflammatory response in patients with chronic obstructive pulmonary disease. Guide China Med. (2011) 9(09):142–4. doi: 10.15912/j.cnki.gocm.2011.09.102
136. Chen Y, Zhang P, Dong Z, Zhu Y, Liu Y, Qiao C, et al. Effect of Baduanjin exercise on health and functional status in patients with chronic obstructive pulmonary disease: a community-based, cluster-randomized controlled trial. NPJ Prim Care Respir Med. (2024) 34(1):43. doi: 10.1038/s41533-024-00400-y
137. Krishna BH, Pal P, Pal G, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. A randomized controlled trial to study the effect of yoga therapy on cardiac function and N terminal pro BNP in heart failure. Integr Med Insights. (2014) 9:1–6. doi: 10.4137/IMI.S13939
138. Mei B, Yuan L, Shu Y. Quantitative evidence of the effect of Baduanjin exercise on quality of life and cardiac function in adults with chronic heart failure. Complement Ther Clin Pract. (2023) 53:101775. doi: 10.1016/j.ctcp.2023.101775
139. Zhang L, Xie Y, Zhu Q, Chen Y. Clinical study on the effect of Baduanjin on heart function and psychology in patients with heart failure. Cont Med Educ. (2022) 36:137–40.
140. Cao Z, Jia Y, Zhu B. BNP and NT-proBNP as diagnostic biomarkers for cardiac dysfunction in both clinical and forensic medicine. Int J Mol Sci. (2019) 20(8):1820. doi: 10.3390/ijms20081820
141. Teramoto K, Tay WT, Tromp J, Ouwerkerk W, Teng TK, Chandramouli C, et al. Longitudinal NT-proBNP: associations with echocardiographic changes and outcomes in heart failure. J Am Heart Assoc. (2024) 13(9):e032254. doi: 10.1161/JAHA.123.032254
142. Pullen PR, Thompson WR, Benardot D, Brandon LJ, Mehta PK, Rifai L, et al. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. (2010) 42(4):651–7. doi: 10.1249/MSS.0b013e3181bf24c4
143. Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. (2001) 4(4):165–70. doi: 10.1111/j.1520-037x.2001.00542.x
144. Triebel H, Castrop H. The renin angiotensin aldosterone system. Pflugers Arch. (2024) 476:705–13. doi: 10.1007/s00424-024-02908-1
145. Philipson A, Duberg A, Hagberg L, Högström S, Lindholm L, Möller M, et al. The cost-effectiveness of a dance and yoga intervention for girls with functional abdominal pain disorders. Pharmacoecon Open. (2023) 7(2):321–35. doi: 10.1007/s41669-022-00384-w
146. Tew G, Wiley L, Ward L, Hugill-Jones J, Maturana C, Fairhurst C, et al. Effectiveness and cost-effectiveness of offering a chair-based yoga programme in addition to usual care in older adults with multiple long-term conditions: a pragmatic, parallel group, open label, randomised controlled trial. NIHR Open Res. (2024) 3:52. doi: 10.3310/nihropenres.13465.2
147. Hartfiel N, Clarke G, Havenhand J, Phillips C, Edwards RT. Cost-effectiveness of yoga for managing musculoskeletal conditions in the workplace. Occup Med (Lond). (2017) 67(9):687–95. doi: 10.1093/occmed/kqx161
Keywords: exercise interventions, chronic cardiopulmonary dyspnoea, yoga, network meta-analysis, mind-body exercises
Citation: Li Y, Wu J and Lei R (2025) Effects of mind-body exercise in chronic cardiopulmonary dyspnoea patients—a network meta-analysis of randomized controlled trials. Front. Cardiovasc. Med. 12:1546996. doi: 10.3389/fcvm.2025.1546996
Received: 21 December 2024; Accepted: 19 May 2025;
Published: 4 June 2025.
Edited by:
Rajeev Gupta, Spectrum Medical Center, United Arab EmiratesReviewed by:
Amrish Agrawal, Fujairah Hospital, United Arab EmiratesRam Manohar Talupula, Aster Ramesh Hospitals, India
TIa Bimal, Mount Sinai Hospital, United States
Copyright: © 2025 Li, Wu and Lei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Wu, d2ppbmcwMTAzQDE2My5jb20=
 Yilin Li
Yilin Li Jing Wu1*
Jing Wu1*