Abstract
Background:
Rapid diagnosis of patients with acute coronary syndrome (ACS) is crucial for saving their lives. The de Winter electrocardiogram (ECG) pattern is rare and is treated similarly to ST-segment elevation myocardial infarction (STEMI) and acute thrombotic occlusion of the coronary artery. The de Winter ECG pattern has been previously reported, but its dynamic evolution and characteristics have not been summarized.
Methods:
We reported two male patients who presented with de Winter ECG pattern at rest, and neither patient had a family history of hypertension, diabetes, or coronary heart disease. An urgent examination in our hospital showed elevated levels of cardiac troponin T. Both patients underwent emergency coronary angiography, which revealed subtotal proximal left anterior descending (LAD) stenosis. There was an improvement in chest tightness and pain after stent implantation. Serial ECGs before and after percutaneous coronary intervention showed dynamic evolution of ECG. A literature review was conducted to examine reported coronary angiography findings in patients with the de Winter pattern. The review focused on the dynamic evolution of the ECG and the accuracy of this pattern in diagnosing acute coronary artery occlusion (culprit vessel). It also highlighted the danger of the de Winter ECG pattern and the importance of emergency treatment.
Results:
Eighteen patients, including two of our patients, presented with the de Winter ECG pattern. Our two cases demonstrated two different forms of ST-segment dynamic evolution, with Case 2 being the only one among 18 cases that dynamically evolved into a life-threatening non-STEMI (NSTEMI). All cases were male patients with sudden chest pain. ECG examination showed an upward-sloping ST-segment depression with tall symmetrical T waves in the chest leads, and multiple follow-up ECGs revealed dynamic ST-segment evolution. Emergency coronary angiography showed occlusion of the LAD, left main artery (LMA), right coronary artery (RCA), first diagonal branch (D1), and left circumflex (LCX) artery as well as multiple vascular lesions. Most cases support subtotal stenosis or complete occlusion of the anterior descending artery. Timely identification of the de Winter ECG pattern and prompt transfer to the catheterization laboratory for emergency revascularization can be lifesaving and improve prognosis.
Conclusion:
These two cases and the literature review indicated that the de Winter ECG pattern is dynamically evolving. Its ECG pattern evolution is variable, progressing to STEMI, NSTEMI, Wellens, or even a normal. In patients presenting with chest pain, a de Winter ECG pattern, regardless of the subsequent dynamic evolution of the ECG, indicates the presence of severe coronary artery stenosis. The de Winter ECG pattern may be an early manifestation of ACS and requires urgent coronary angiography to save the patient's life and improve prognosis.
Introduction
Acute coronary syndrome (ACS) is a clinical syndrome characterized by acute myocardial ischemia. It includes unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI) (1). However, a portion of less commonly overlooked electrocardiograms (ECGs) do not conform to the typical electrocardiographic features of STEMI, nor do they differ from the common downward-sloping or horizontal ST-segment depression changes seen in NSTEMI. The main electrocardiographic features are upward-sloping ST-segment depression and symmetrical T-wave elevation, known as de Winter ECG patterns. This pattern is associated with acute thrombotic occlusion of the coronary artery and was first reported in 2008, specifically for proximal left anterior descending (LAD) artery occlusion (2).
In an era where coronary computed tomography angiography (CTA) and coronary angiography are the main diagnostic methods for myocardial infarction, traditional ECG still plays an irreplaceable role. The 12-lead ECG is the main diagnostic tool for detecting the de Winter patterns, especially in communities and primary medical institutions where coronary CTA and coronary angiography are unavailable. Early identification of the de Winter ECG patterns can be lifesaving by enabling rapid transfer of patients to the catheterization room for emergency revascularization to restore coronary blood flow. Various ECG patterns, especially atypical patterns and dynamic evolution of ECG, should be monitored frequently to ensure timely and accurate diagnosis.
Here, we present two patients with dynamic evolution of the de Winter ECG pattern, review the literature on its clinical characteristics, and emphasize the importance of repeated and continuous ECG monitoring in patients with acute typical chest pain to prevent treatment delays and adverse outcomes.
Case presentation
Case 1
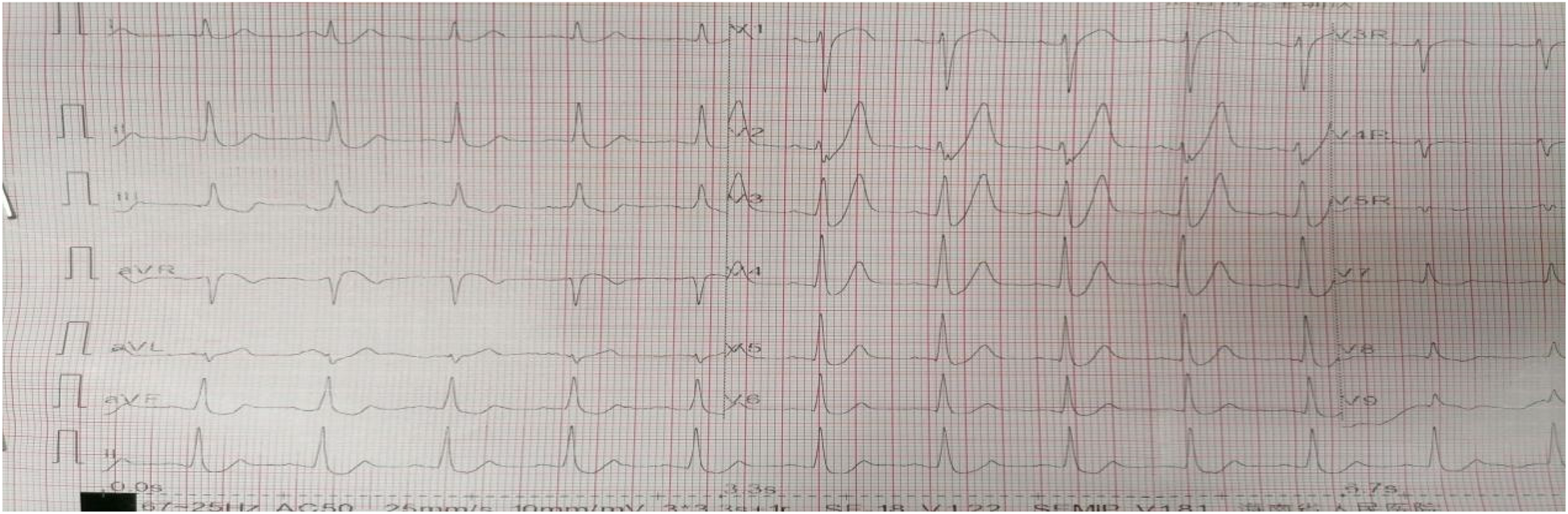
A 61-year-old male with no history of hypertension, diabetes, or coronary heart disease was urgently referred to our hospital's emergency department. He initially presented to a local hospital with persistent chest pain for 4 h. The chest pain was described as a squeezing sensation in the chest area, accompanied by profuse sweating, palpitations, shortness of breath, radiating pain in the back and left upper limb, limb weakness, and dizziness, which persisted without relief. Physical examination showed body temperature of 36.2°C, pulse at 65 beats/min, respiratory rate at 20 breaths/min, and blood pressure at 104/70 mmHg. He had a clear consciousness and regular heart rhythm with no murmurs. Bilateral breath sounds were mildly coarse, accompanied by scattered moist rales in the lower lung fields. The abdominal examination revealed no abnormalities. The initial ECG examination in our hospital showed an upward-sloping ST-segment depression of 0.1–0.4 mV in leads V2–V6, tall symmetrical T waves in leads V1–V4, absence of R waves in leads V1–V3, and ST elevation in lead aVR (Figure 1).
Figure 1
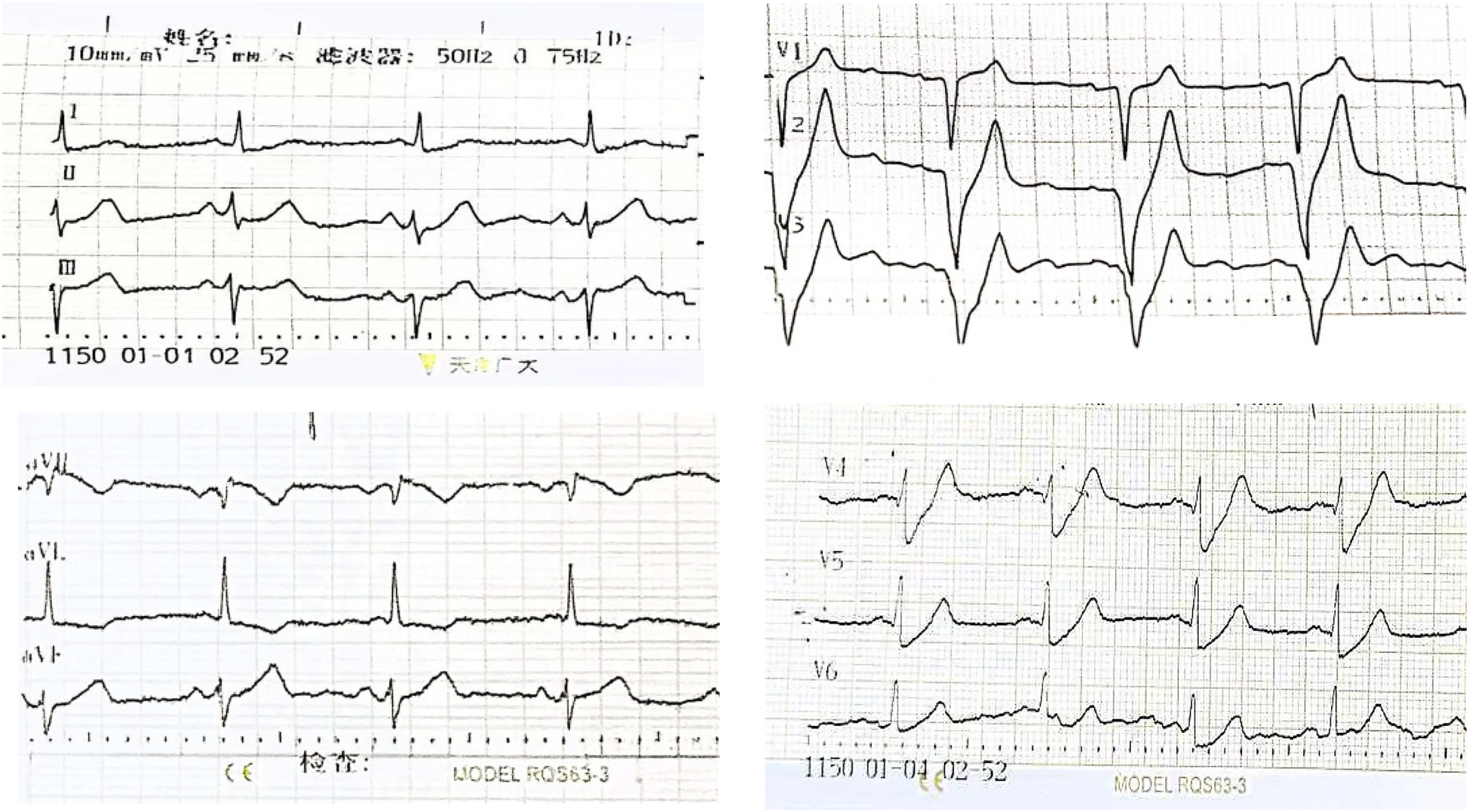
The initial ECG of Case 1 showed the de Winter ECG pattern: upsloping ST-segment depression of 0.1–0.4 mV in leads V2–V6 and persistent tall symmetrical T waves in leads V1–V4, along with an absence of R waves in leads V1–V3 and ST elevation in lead aVR.
Multiple rechecks of ECG showed a dynamic evolution of the ST-segment, which is gradually rising. In our hospital, emergent coronary angiography demonstrated 75%–90% stenosis in the proximal and middle segments of the LAD (Figures 2A,B). One stent was implanted, and the blood flow was restored to TIMI III (Figure 2C). Five hours after the initial ECG, QS complexes were observed on the follow-up ECG in leads V1–V6, with ST-segment elevation of 0.1–0.9 mV in leads II, III, aVL, and V2–V6, accompanied by upright T waves in leads V2–V6, consistent with a typical acute extensive anterior wall myocardial infarction (Figure 3). Ultrasensitive troponin T (TNT) was 10.0 µg/L, creatinine kinase (CK) was 5,382.4 U/L, CK-MB was 485.3 U/L, and D-dimer was 0.74 µg/mL. On the third day after percutaneous coronary intervention (PCI), the ECG showed that the ST-segment gradually decreased to the isoelectric baseline level, and pathological Q waves still existed in leads V1–V5, with inverted T waves (Figure 4). Echocardiography showed left heart enlargement, weakened motion of the anteroseptal segments, anterior wall, and apex, mild pulmonary hypertension, and a small amount of pericardial effusion. The patient had impaired left ventricular systolic and diastolic functions with left ventricular ejection fractions (LVEF) 35% and E′/A′ = 0.71. The patient received dual-antiplatelet therapy (aspirin 100 mg/day and ticagrelor 90 mg/12 h), and chest pain was relieved. The patient’s chest pain symptoms were significantly relieved, and he was discharged on the 14th day after PCI.
Figure 2
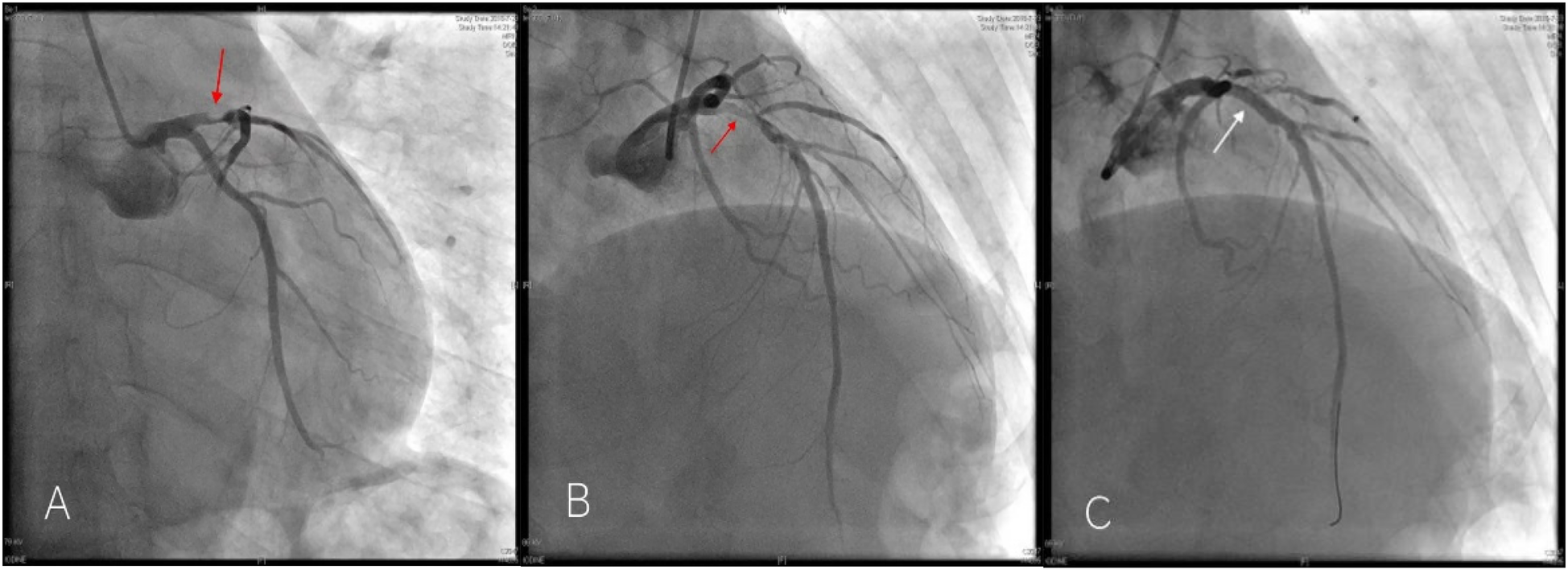
Emergency coronary angiography of Case 1 patient showed 75%–90% stenosis in the proximal LAD [(A,B) red arrow] and was successfully recanalized after stent implantation. [(C) white arrow].
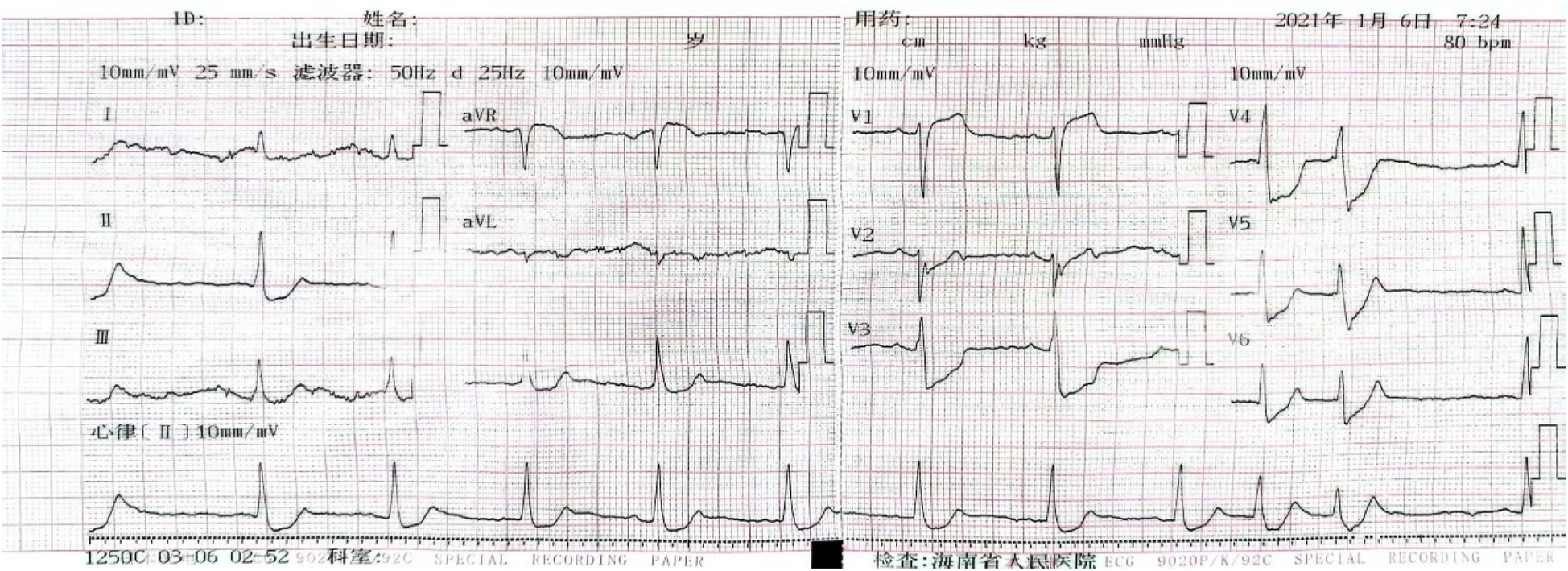
Figure 3
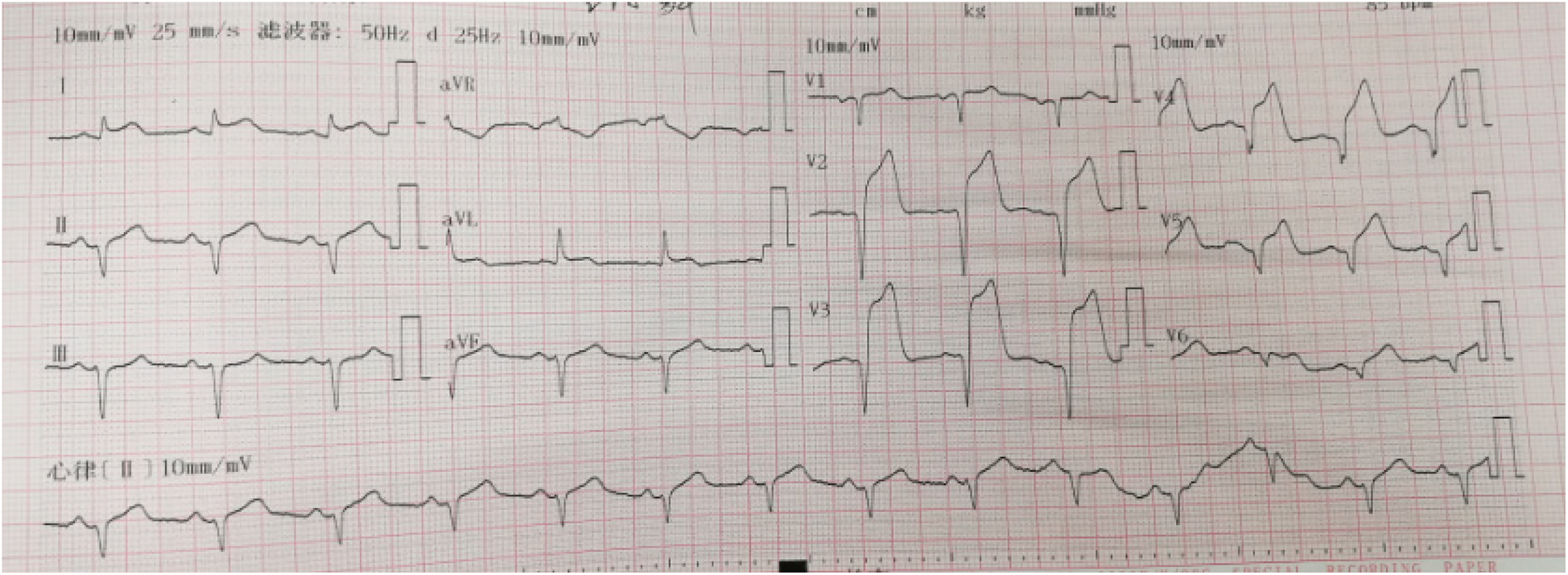
The second ECG of Case 1 showed an acute extensive anterior wall myocardial infarction: ST-segment elevation of 0.1–0.9 mV in leads II, III, aVL, and V2–V6. The most significant ST-segment elevation was observed in lead V3, accompanied by QS complexes in leads V1–V6, and upright T waves in leads V2–V6.
Figure 4
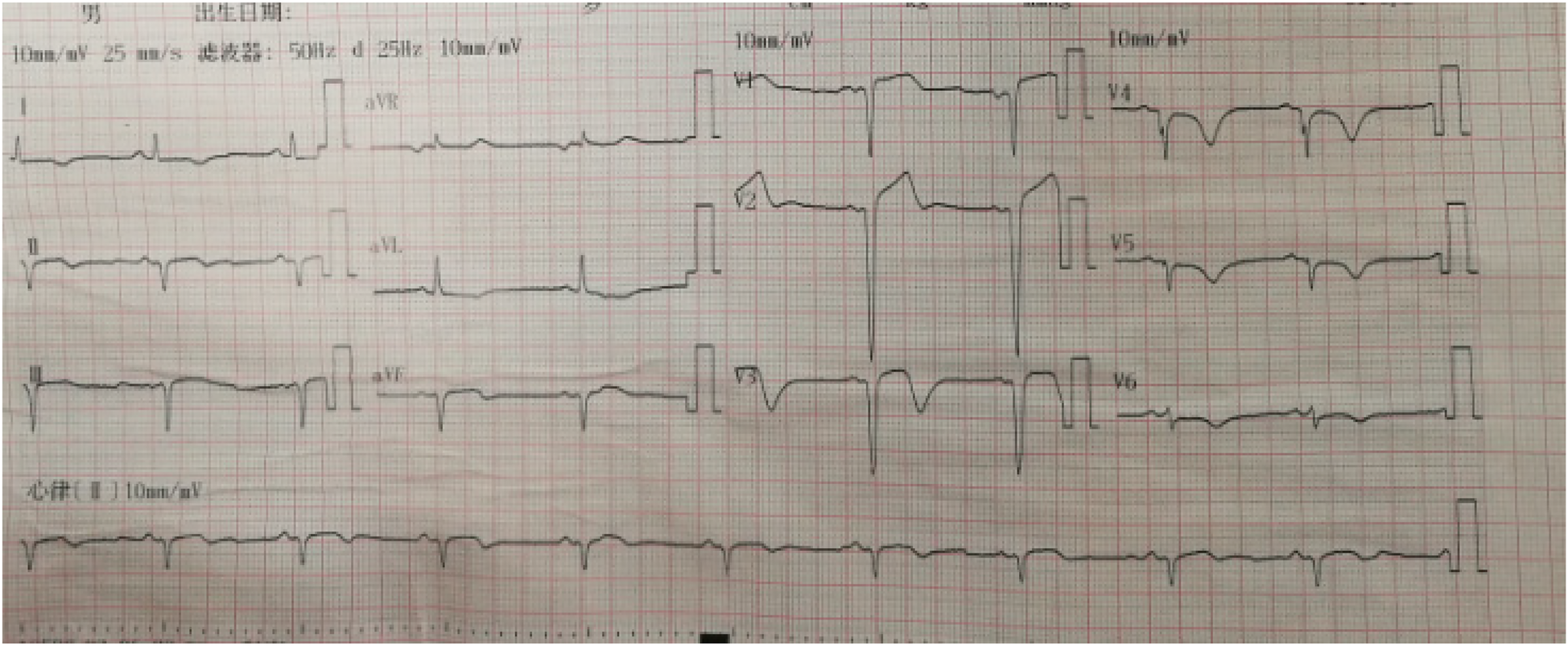
In the third ECG of Case 1, on the third day of PCI stent implantation, the ECG showed that the ST-segment gradually decreased to the isoelectric baseline, and pathological Q waves still existed in leads V1–V5, with inverted T waves.
Case 2
A 55-year-old smoker without a history of hypertension, diabetes, or coronary heart disease presented to our emergency department with acute typical chest pain and continuous squeezing sensation behind the sternum, accompanied by profuse sweating and a feeling of impending death, which occurred during 2 h before waking. Physical examination showed body temperature of 37.0°C, pulse at 85 beats/min, respiratory rate at 20 breaths/min, and blood pressure at 130/80 mmHg. He had a regular rhythm and no pathological murmurs. Bilateral lung auscultation detected coarse breath sounds accompanied by mild wet rales in both lower lung fields. The results of the abdominal examination were unremarkable. The initial ECG showed 0.1–0.35 mV upward-sloping ST-segment depression with tall symmetrical T waves in leads V2–V6; 0.1–0.2 mV downward-sloping ST-segment depression in leads I, II, III, and aVF; and 0.1–0.15 mV ST-segment elevation in leads V1, and aVR. The ECG meets the diagnostic criteria of the de Winter ECG pattern (Figure 5). TNT was 6.13 µg/L, CK was 78.0 U/L, CK-MB was 27.6 U/L, and D-dimer was 0.91 µg/mL. Emergency coronary angiography indicates a stenosis of 85% in the proximal segment of the LAD, with a patent left circumflex (LCX) artery and right coronary artery (RCA) (Figure 6A). A 3.0 mm × 21 mm GuReater stent was implanted into the LAD (Figure 6B). The second ECG was taken 46 min later from the initial ECG, which showed a sinus rhythm; paired atrial premature contractions; a sharp T-wave regression; significant horizontal and upsloping ST-segment depression (0.1–0.7 mV) in leads II, III, AVF, and V2–V6; and ST-segment elevation in leads aVR and V1. ST-T morphological changes were different from the typical de Winter ECG pattern but similar to the “8 + 2” ECG pattern in acute left main artery (LMA) occlusion (Figure 7). After PCI, the patient received dual-antiplatelet therapy (aspirin 100 mg/day and ticagrelor 90 mg/12 h). Ten hours after the initial ECG, a third ECG showed QS type in leads V1–V3, with ST-segment and T wave returning to normal (Figure 8). Echocardiography showed left atrial enlargement, small pericardial effusion, mild mitral regurgitation, and normal left ventricular systolic function [ejection fractions (EF) = 68%]. The patient's chest pain improved, and the condition was stabilized. The patient's chest pain was significantly relieved, and he was discharged on the 5th day after PCI.
Figure 5
The initial ECG of Case 2 revealed the de Winter ECG pattern: upsloping ST-segment depression of 0.1–0.3 mV in leads V2–V6 and persistent tall symmetrical T waves in leads (V1–V4), ST-segment elevation of 0.1 mV in leads V1 and aVR.
Figure 6
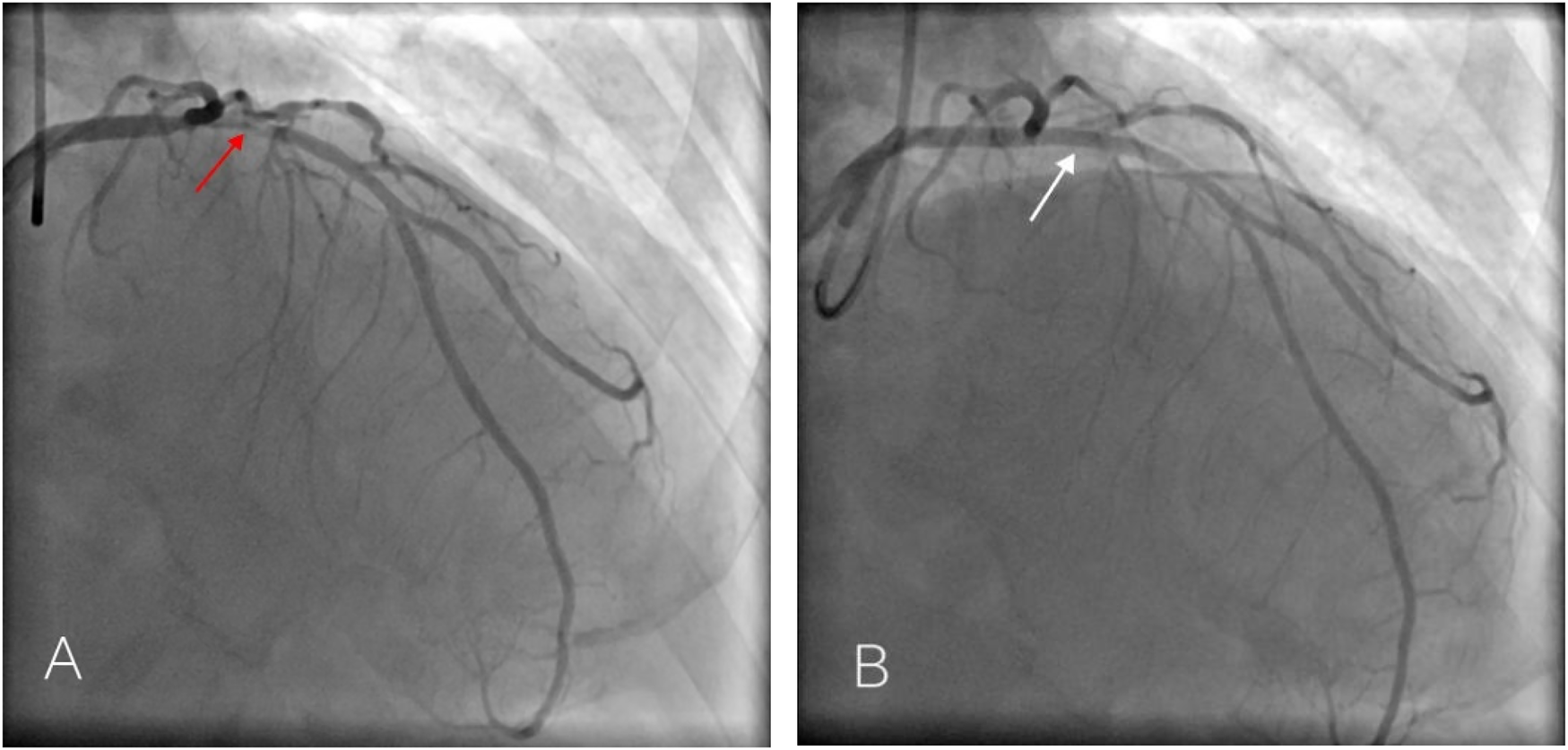
Emergency coronary angiography of Case 2 patient showed 85% stenosis in the proximal LAD [(A) red arrow] and was successfully recanalized after stent implantation [(B) white arrow].
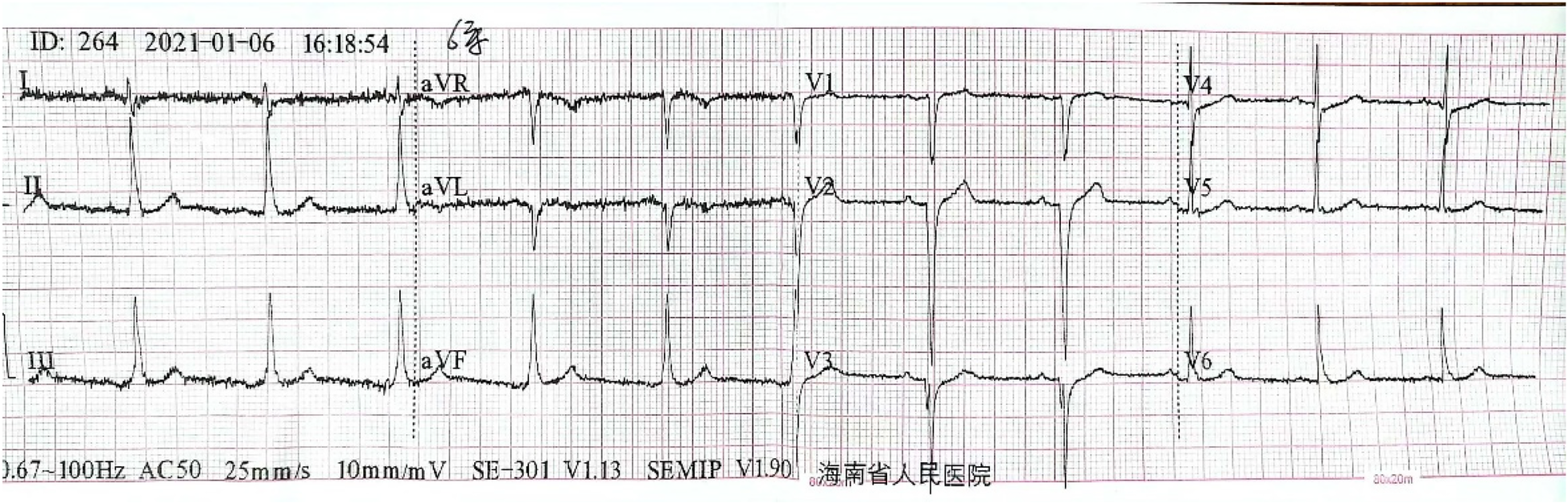
Figure 7
The second ECG of Case 2 revealed an NSTEMI different from de Winter ECG pattern: sinus rhythm; paired atrial premature beats; tall symmetrical T waves returning to normal; significant ST-segment horizontal and upsloping depression (0.1–0.7 mV) in leads II, III, aVF, and V2–V6; ST-segment depression in leads V3 and V4 which were most significant, and ST-segment elevation (0.1–0.2 mV) in leads aVR and V1.
Figure 8
The third ECG of Case 2: V1–V3 leads were QS type, with ST-segment and T wave returning to normal.
Discussion
ECG is a crucial diagnostic technique that is rapid, cost-effective, accessible, radiation-free, and easy to track and observe. With the popularization, improvement, and development of electrocardiographic knowledge, ECG continues to provide valuable information for disease prevention, diagnosis, treatment, and prognosis in outpatient, emergency, and inpatient settings. In clinical diagnosis and treatment activities, it is difficult to detect the de Winter ECG pattern if the observation is limited to ST-segment elevation. The diagnostic criteria for the de Winter ECG pattern include the following: (1) upsloping ST-segment depression of 0.1–0.3 mV (1 mV = 10 mm) at the J-point below the isoelectric baseline in precordial leads (V1–V6), with tall, positive symmetrical T waves; (2) normal or slightly widened QRS wave morphology; (3) poor R-wave progression in the chest leads; (4) a narrow range of 0.1–0.2 mV ST-segment elevation in aVR. Among them, the V3 lead has the highest degree of upsloping depression in the ST-segment and the highest T-wave amplitude (2, 3). In this ECG pattern report, ST-segment depression accompanied by taller T waves is not limited to the chest leads (4) but may also occur in the inferior wall leads (5, 6). It is necessary to differentiate it from ST-segment depression caused by tachycardia and tall spike T waves caused by hyperkalemia.
The presence of ST-segment depression in a routine 12-lead ECG is commonly observed in non-ST-segment elevation myocardial ischemia, which is often associated with coronary atherosclerosis. It can also be seen in more critical conditions such as left main coronary artery occlusion. The de Winter ECG pattern can easily be confused with the ECG characteristics of typical LMA occlusion; typical ECG changes in LMA are ST-segment depression in multiple leads and ST-segment elevation in aVR. Upon close observation of our two typical cases and previously published reports regarding the de Winter ECG pattern, ST-segment depression was the most common finding, often manifesting as upsloping depression. Clinicians may mistakenly categorize all ECGs with ST-segment depression as stable myocardial ischemia, overlooking their significance, potentially leading to delayed treatment and more unfavorable outcomes. The typical de Winter ECG pattern primarily features upsloping ST-segment depression, suggesting a possibility of more severe myocardial ischemia compared with horizontal or downsloping ST-segment depression.
Previous studies have indicated that the de Winter ECG pattern is primarily observed in single-vessel coronary artery disease, which was useful for diagnosing an acute proximal LAD artery occlusion. This pattern remains static without significant evolution in typical acute ST-segment elevation myocardial infarction (STEMI) (7). In a recent retrospective study, the de Winter ECG pattern, also known as the de Winter syndrome, was identified as a transient and dynamic ischemic phenomenon in the progression of ACS. It reflects the formation of coronary artery thrombi and strongly suggests severe coronary artery disease. The culprit vessel is most commonly the LAD, although this ECG pattern has also been associated with other coronary artery occlusions (8). Previously, this mode was considered static, but in reality, it is transient and dynamic. The ECG pattern of STEMI and de Winter can evolve into one another. To further observe the dynamic evolution of the de Winter phenomenon, based on the summary of 2 typical cases collected in our hospital, 18 cases were selected that met the characteristics of the de Winter ECG pattern and showed dynamic evolution of the ECG. The basic literature and clinical characteristics of each case are shown in Table 1 (9–21). All 18 cases were male, with a median age of 55.0 years (P25 = 49.2, P75 = 65). Previous studies have observed that patients with de Winter ECG patterns were younger males with hypercholesterolemia (7, 22). Compared with patients with STEMI, the baseline characteristics of patients presenting with de Winter ECG patterns were found to be younger. Among the 18 cases, except for 1 case (10) where angiography was not performed to determine the location of vascular lesions, 10 cases were single-vessel occlusions, while 7 cases indicated multiple-vessel occlusions. Although there have been reports of patients with de Winter ECG pattern changes who underwent emergent coronary angiography showing no coronary stenosis and diagnosed with myocarditis subsequently confirmed by cardiac magnetic resonance imaging (23), de Winter ECG changes still indicate acute LAD occlusion to some extent. Such ECG patterns can suggest acute coronary artery occlusion, including the LMA, LCX, RCA, and first diagonal branch. There are also case reports related to multivessel disease.
Table 1
| Study | Gender | Age | Clinical presentation | Location of vascular occlusion | Evolution situation | Evolution time point |
|---|---|---|---|---|---|---|
| Cabezas et al. (9) | Male | 53 | Chest pain | D1 | de Winter to anterolateral ischemia | After treatment |
| Pranata et al. (10) | Male | 65 | Chest pain | NA | de Winter to STEMI | Before treatment |
| Lin et al. (11) | Male | 65 | Chest pain, diaphoresis | LAD, LCX | de Winter to STEMI | Before treatment |
| Male | 50 | Chest pain radiating to the left shoulder and back, accompanied by diaphoresis | LAD | STEMI to de Winter | Before treatment | |
| Grandjean et al. (12) | Male | 56 | Chest pain | LAD | de Winter to STEMI | After treatment |
| Wang et al. (13) | Male | 31 | Chest pain | LAD | de Winter to STEMI | Before treatment |
| Lu et al. (14) | Male | 51 | Chest tightness and pain | LAD | de Winter to STEMI | After treatment |
| Zhang et al. (15) | Male | 55 | Chest pain | LAD, LCX | STEMI to de Winter | Before treatment |
| Male | 70 | Chest pain | LAD, large diagonal branch | de Winter to STEMI | Before treatment | |
| Chen et al. (16) | Male | 47 | Chest pain | RCA, LAD, LCX | STEMI to de Winter | After treatment |
| He et al. (17) | Male | 76 | Chest pain, along with dyspnea and sweating | LAD, RCA, LCX | de Winter to STEMI | Before treatment |
| Zhu et al. (18) | Male | in his 50s | Chest pain radiating to the left arm, sweating, and nausea | LAD | de Winter to Wellens | After treatment |
| Wang et al. (19) | Male | 56 | Chest pain | LAD | de Winter to STEMI to normal | Before treatment |
| Liu et al. (20) | Male | 47 | Chest pain | LAD, LCX, LMA | de Winter to STEMI | Before treatment |
| Male | 76 | Chest pain | LMA | de Winter to STEMI | Before treatment | |
| Huang et al. (21) | Male | 34 | Chest pain | LAD, LCX, RCA | STEMI to de Winter | Before treatment |
| This study | Male | 61 | Chest pain radiating to the shoulder and back and left upper limb, accompanied by diaphoresis | LAD | de Winter to STEMI | After treatment |
| Male | 55 | Chest pain, diaphoresis | LAD | de Winter to NSTEMI | After treatment |
Summary of the clinical features of cases with dynamic evolution in the de Winter pattern.
D1, first diagonal branch; LAD, left anterior descending; LCX, left circumflex; RCA, right coronary artery; LMA, left main artery; NA, not available.
Currently, the pathophysiological mechanism and dynamic evolution of the de Winter ECG pattern remain elusive. The following mechanisms are speculated to be involved: (1) anatomical variations in Purkinje fibers leading to delayed endocardial conduction, or the lack of activation of sarcolemma ATP-sensitive potassium channels (2); (2) severe ischemia and hypoxia increasing the permeability of myocardial cell membranes, resulting in potassium ion efflux, delayed repolarization, and ischemic myocardial stunning; (3) an area of transmural ischemia so extensive that it does not generate injury currents toward the precordial leads, but only upwards toward the aVR lead; (4) the presence of collateral circulation or ischemic preconditioning, which protects the myocardium from transmural ischemic damage, thereby preventing ST-segment elevation; (5) subendocardial ischemia delaying endocardial repolarization, and prolonged epicardial repolarization leading to an increase in repolarization vectors in the same direction as a normal heart, forming a transmembrane action potential difference that causes ST-segment depression with tall symmetrical T waves; (6) the differential sensitivity of the epicardium and endocardium to ischemia, and the reaction of M-cells at the junction of the myocardial midlayer and endocardium to ischemia and hypoxia, which may be the main cause of the de Winter pattern (24); (7) ischemic mirror changes due to multivessel disease.
During subendocardial ischemia, prominent and elevated T waves can be recorded in the hyperacute phase. As the ischemia further progresses to transmural ischemia, the ECG evolves to show typical ST-segment elevation, sometimes even accompanied by pathological Q waves. He et al. (17) suggested that this dynamic evolution may be due to the gradual occlusion of coronary arteries, while Donato et al. (25) and Sunbul et al. (26) proposed that it could be related to changes in the anatomical structure of coronary arteries or the recruitment of collateral circulation. The distribution of ischemic myocardium and the progression of thrombosis may contribute to the occurrence of the de Winter ECG pattern. The evolution of de Winter ECG depends on factors such as unstable thrombosis, spontaneous thrombolysis, and coronary artery reperfusion. It reflects subtotal occlusion of the proximal or mid-LAD artery rather than total occlusion. If the thrombosis progresses to complete occlusion, it can evolve into STEMI (21).
Including our 2 cases, there were a total of 18 cases with dynamic ECG evolution. Among them, 10 cases evolved from the de Winter pattern to STEMI, as exemplified by our reported Case 1, where the ECG progressed from the de Winter pattern to the typical STEMI. Conversely, there were four cases where STEMI evolved into the de Winter pattern. Zhang et al. (15) reported two cases fitting these evolution patterns. In one case of acute extensive anterior wall myocardial infarction, the ECG evolved into a typical de Winter pattern just 8 min later. Emergency coronary angiography revealed a 90% stenosis in the proximal and mid-segments of the LAD and a 70% stenosis in the distal segment of the LCX artery. The other case showed the opposite trend, with the initially recorded de Winter ECG evolving into an acute anterior wall myocardial infarction after 1 h. Emergency coronary angiography indicated approximately 95% stenosis at the junction of the proximal and mid-segments of the LAD and 90% stenosis in the proximal and mid-segments of the large diagonal branch. In this study, there was one case of the de Winter pattern evolving into Wellens (18). This rare dynamic evolution might be associated with spontaneous recanalization after acute complete LAD occlusion. There was also one case where the de Winter ECG pattern evolved into STEMI and then into a normal ECG. This evolution could be due to incomplete occlusion caused by a coronary artery thrombus, with spontaneous thrombolysis of the occlusive thrombus leading to a transition from ST-segment elevation to an upsloping ST-segment depression characteristic of the de Winter ECG pattern and even normalization of the ECG (27). Dynamic evolution occurred in 11 cases before coronary angiography and in 7 cases after PCI with stent implantation. The dynamic changes in ECG may be related to timely blood reperfusion therapy. The intervals between dynamic evolutions varied, mostly occurring within minutes to hours, and even up to 3 days in one case (14). Yang et al. (28) suggested that delayed and atypical ECG changes in this pattern might be attributed to individual differences in coronary anatomy, recurrent ischemic attacks, and different stages of thrombus occlusion. Liu et al. (20) reported two cases of de Winter ECG pattern dynamically evolving into STEMI or even death in a short time. In one case, it evolved into an extensive anterior wall and high lateral wall myocardial infarction after 1.5 h. Emergency coronary angiography showed complete occlusion of the proximal LAD and LCX artery, with a blurred thrombus at the bifurcation of the LMA. Despite timely stent implantation, the patient died of refractory cardiac arrest 3 h later. In another case, ST-segment elevation gradually appeared after 25 min. Emergency coronary angiography indicated LMA occlusion, and the patient died of severe multiorgan failure despite stenting. They believed that in cases of acute complete LM occlusion, the de Winter ECG pattern can evolve into STEMI.
The electrocardiographic manifestations of NSTEMI in ACS are qualitative and risk-quantitative markers. The number and degree of ST-segment depression in leads are often related to the degree of ischemia and prognosis. Multi-lead ST-segment depression (greater than six-lead depression >0.1 mV), accompanied by aVR and/or V1 lead ST-segment elevation, often indicates the presence of severe coronary artery stenosis. Case 2 dynamically progressed from de Winter ECG pattern to NSTEMI. The dynamic evolution of ECG is mainly manifested as more significant ST-segment depression in multiple leads and ST-segment elevation in leads aVR and V1. Coronary angiography showed subtotal occlusion of the proximal segment of the LAD. Insufficient understanding of this condition could lead to underestimation of its risks and misclassification as stable angina pectoris, potentially missing the therapeutic window (29) and delaying diagnosis and treatment.
Not all patients with acute subtotal or total LAD occlusion exhibit typical STEMI ECG patterns. Approximately 2% of patients initially present with the de Winter ECG pattern (2). In cases of LAD occlusion, if spontaneous recanalization occurs, there may be a transition between STEMI and the de Winter ECG pattern. This could potentially progress to myocardial infarction before coronary blood flow is restored (7, 30, 31). If the thrombus undergoes spontaneous thrombolysis, the ECG may evolve back to normal. In Case 2, an elevated D-dimer level indicated spontaneous thrombolysis of the coronary thrombus. Pranata et al. (10) and Rao et al. (32) also suggested that the de Winter syndrome may be a thrombotic condition, supporting thrombolytic therapy. The ECG pattern of STEMI can shift to the de Winter ECG pattern due to spontaneous thrombolysis of coronary thrombi. Therefore, early intervention can prevent the progression from endocardial ischemia to transmural myocardial ischemia, thus avoiding the development of STEMI and irreversible myocardial damage. The importance of timely recognition of dynamic ECG changes lies in its ability to confirm acute coronary artery occlusion, guiding the direction of further patient management.
Electrocardiographers and emergency physicians must recognize the de Winter ECG pattern, not only because of its rarity but also due to the lack of typical ECG characteristics during its dynamic evolution, which often leads to clinicians' disregard. To our knowledge, patients presenting with the de Winter ECG pattern carry a high risk of death and adverse events. On 25 August 2018, the European Society of Cardiology (ESC) announced the globally unified definition, the Fourth Global Definition of Myocardial Infarction (FUDMI), at its annual meeting held in Munich, Germany, which first elaborated the de Winter ECG pattern and identified it as a very high-risk NSTEMI caused by anterior descending artery occlusion. The de Winter ECG pattern should be treated like other STEMI equivalents, with prompt revascularization therapy administered promptly. Therefore, early recognition of the de Winter ECG pattern is essential, and primary PCI with concurrent stent implantation is considered the optimal reperfusion strategy (33).
Conclusions
We suggest the de Winter ECG pattern is dynamically evolving, transitioning between STEMI, Wellens, hyperacute T, NSTEMI, and a normal ECG. Although the 2023 ESC guidelines do not specifically mention the de Winter ECG pattern, they emphasize that patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) who exhibit any very high-risk features—particularly dynamic ST-T changes—should undergo urgent coronary angiography and an early invasive approach as soon as possible (34). The de Winter ECG pattern should be regarded as an electrocardiographic equivalent of STEMI. It is important to keep in mind this rare and dangerous ECG pattern that needs attention. Emergency physicians, electrocardiogram physicians, and cardiologists should recognize these patterns and closely monitor dynamic ECG changes. These characteristics of ECG changes can aid in the rapid identification of patients, emphasizing the diagnostic and treatment philosophy that “time is cardiac muscle.” Urgent coronary angiography and prompt revascularization therapy should be performed. Early diagnosis of the de Winter ECG pattern can be lifesaving. Prompt identification of atypical ECG signs of ACS is essential for saving patients' lives and improving outcomes.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Hainan General Hospital. The research procedures were carried out strictly in accordance with local laws, regulations, and institutional ethical requirements. Written informed consent to participate in this study was provided by the participants. They were fully informed that any images or data related to them in this article would not include any sensitive or identifiable personal information. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
YC: Data curation, Investigation, Writing – original draft, Writing – review & editing, Conceptualization. BC: Data curation, Writing – original draft, Writing – review & editing, Conceptualization, Investigation. LZ: Data curation, Resources, Writing – original draft. WL: Funding acquisition, Writing – review & editing. MW: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (NSFC) (No. 82160074).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence, and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Thießen N Schnabel R . Diagnosis of acute coronary syndrome. Deutsch Med Wochenschr. (2024) 149(09):488–95. 10.1055/a-2163-2586
2.
de Winter RJ Verouden NJW Wellens HJJ Wilde AAM . A new ECG sing of proximal LAD occlusion. N Engl J Med. (2008) 359(19):2071–3. 10.1056/NEJMc0804737
3.
Morris NP Body R . The de Winter ECG pattern: morphology and accuracy for diagnosing acute coronary occlusion: systematic review. Eur J Emerg Med. (2017) 24(4):236–42. 10.1097/MEJ.0000000000000463
4.
Shao D Yang N Zhou S Cai Q Zhang R Zhang Q et al The “criminal” artery of de Winter may be the left circumflex artery. Medicine (Baltimore). (2020) 99(24):e20585. 10.1097/MD.0000000000020585
5.
Ghaffari S Pourafkari L Nader ND . “de Winter” electrocardiogram pattern in inferior leads in proximal right coronary artery occlusion. Arch Cardiol Méx. (2021) 91(3):366–8. 10.24875/ACM.20000308
6.
Chen Q Zou T Pang Y Ling Y Zhu W . The de Winter-like electrocardiogram pattern in inferior and lateral leads associated with left circumflex coronary artery occlusion. ESC Heart Fail. (2020) 7(6):4301–4. 10.1002/ehf2.12946
7.
Verouden NJ Koch KT Peters RJ Henriques JP Baan J van der Schaaf RJ et al Persistent precordial “hyperacute” T-waves signify proximal left anterior descending artery occlusion. Heart. (2009) 95(20):1701–6. 10.1136/hrt.2009.174557
8.
Wall J White LD Lee A . Novel ECG changes in acute coronary syndromes. Would improvement in the recognition of ‘STEMI-equivalents’ affect time until reperfusion?Intern Emerg Med. (2018) 13(2):243–9. 10.1007/s11739-016-1595-3
9.
Cabezas J Karalis I Schalij MJ . de Winter electrocardiographic pattern related with a non-left anterior descending coronary artery occlusion. Ann Noninvasive Electrocardiol. (2016) 21(5):526–8. 10.1111/anec.12358
10.
Pranata R Huang I Damay V . Should de Winter T-wave electrocardiography pattern be treated as ST-segment elevation myocardial infarction equivalent with consequent reperfusion? a dilemmatic experience in rural area of Indonesia. Case Rep Cardiol. (2018) 2018:1. 10.1155/2018/6868204
11.
Lin Y-Y Wen Y-D Wu G-L Xu X-D . de Winter syndrome and ST-segment elevation myocardial infarction can evolve into one another: report of two cases. World J Clin Cases. (2019) 7(20):3296–302. 10.12998/wjcc.v7.i20.3296
12.
Grandjean T Degrauwe S Tessitore E Iglesias JF . The ‘de Winter’ electrocardiogram pattern as a ST-elevation myocardial infarction equivalent: a case report. Eur Heart J Case Rep. (2019) 3(4):1–5. 10.1093/ehjcr/ytz210
13.
Wang H Dai XC Zhao YT Cheng XH . Evolutionary de Winter pattern: from de Winter ECG to STEMI-A case report. BMC Cardiovasc Disord. (2020) 20(1):324. 10.1186/s12872-020-01611-0
14.
Lu B Fu D Zhou X Gui M Yao L Li J . A middle-aged male patient with de Winter syndrome: a case report. BMC Cardiovasc Disord. (2020) 20(1):342. 10.1186/s12872-020-01619-6
15.
Zhang L Fan Y Xu J Yan J Ruan Q Jiang X . de Winter syndrome may be an early electrocardiogram pattern of acute myocardial infarction, two cases report. Ann Noninvasive Electrocardiol. (2020) 25(4):e12729. 10.1111/anec.12729
16.
Chen S Wang H Huang LW . The presence of de Winter electrocardiogram pattern following elective percutaneous coronary intervention in a patient without coronary artery occlusion: a case report. Medicine (Baltimore). (2020) 99(5):e18656. 10.1097/MD.0000000000018656
17.
He DM Liu ZH Wang XG Jiang YM Zhang Y Li JP et al de Winter syndrome and dynamic ECG evolvement. QJM Int J Med. (2020) 113(4):280–2. 10.1093/qjmed/hcz277
18.
Zhu YS Luo SX Huang B . Evolution of de Winter into Wellens on electrocardiogram-what happened?JAMA Intern Med. (2021) 181(12):1647–9. 10.1001/jamainternmed.2021.5734
19.
Wang J Diao SL Ma BX . Dynamic evolvement of the de Winter ECG pattern. Ann Noninvasive Electrocardiol. (2021) 26(5): e12881. 10.1111/anec.12881
20.
Liu C Zhang J Hu Y Wang L Zhang Y Cong H . The de Winter electrocardiographic pattern evolves to ST elevation in acute total left main occlusion: a case series. Ann Noninvasive Electrocardiol. (2022) 27(1):e12855. 10.1111/anec.12855
21.
Huang W Mai L Lu J Li W Huang Y Hu Y . Evolutionary de Winter pattern: from STEMI to de Winter ECG—a case report. ESC Heart Fail. (2022) 9(1):771–4. 10.1002/ehf2.13711
22.
de Winter RW Adams R Amoroso G Appelman Y ten Brinke L Huybrechts B et al Prevalence of junctional ST-depression with tall symmetrical T-waves in a pre-hospital field triage system for STEMI patients. J Electrocardiol. (2019) 52:1–5. 10.1016/j.jelectrocard.2018.10.092
23.
García-Izquierdo E Parra-Esteban C Mirelis JG Fernández-Lozano I . The de Winter ECG pattern in the absence of acute coronary artery occlusion. Can J Cardiol. (2018) 34(2):209.e1–e3. 10.1016/j.cjca.2017.11.014
24.
Xu J Wang A Liu L Chen Z . The de Winter electrocardiogram pattern is a transient electrocardiographic phenomenon that presents at the early stage of ST-segment elevation myocardial infarction. Clin Cardiol. (2018) 41(9):1177–84. 10.1002/clc.23002
25.
Donato M Evelson P Gelpi RJ . Protecting the heart from ischemia/reperfusion injury: an update on remote ischemic preconditioning and postconditioning. Curr Opin Cardiol. (2017) 32(6):784–90. 10.1097/HCO.0000000000000447
26.
Sunbul M Erdogan O Yesildag O Mutlu B . De Winter sign in a patient with left main coronary artery occlusion. Postep Kardiol Interwenc. (2015) 11(4):239–40. 10.5114/pwki.2015.54019
27.
Zhao YT Wang L Yi Z . Evolvement to the de Winter electrocardiographic pattern. Am J Emerg Med. (2016) 34(2):330–2. 10.1016/j.ajem.2015.11.057
28.
Yang Y Ma Y Yin D Zhang Y Song W Cheng Y et al Atypical and delayed de Winter electrocardiograph pattern. Medicine (Baltimore). (2019) 98(18):e15436. 10.1097/MD.0000000000015436
29.
Carr MJ O’Shea JT Hinfey PB . Identification of the STEMI-equivalent de Winter electrocardiogram pattern after ventricular fibrillation cardiac arrest: a case report. J Emerg Med. (2016) 50(6):875–80. 10.1016/j.jemermed.2016.03.022
30.
Montero-Cabezas JM van-der-Kley F Karalis I Schalij MJ . Oclusión aguda de la arteria descendente anterior proximal con patrón electrocardiográfico inusual: no todo es ascenso del ST. Rev Esp Cardiol. (2015) 68(6):541–3. 10.1016/j.recesp.2015.02.014
31.
Sala MF de Luna AB López AC García-Niebla J . The “de Winter pattern” can progress to ST-segment elevation acute coronary syndrome. Rev Esp Cardiol. (2015) 68(11):1042–3. 10.1016/j.recesp.2015.07.009
32.
Rao MY Wang YL Zhang GR Zhang Y Liu T Guo AJ et al Thrombolytic therapy to the patients with de Winter electrocardiographic pattern, is it right? QJM Int J Med. (2018) 111(2):125–7. 10.1093/qjmed/hcx253
33.
Yip H-K Wu C-J Chen M-C Chang H-W Hsieh KY-K Hang C-L et al Effect of primary angioplasty on total or subtotal left main occlusion: analysis of incidence, clinical features, outcomes, and prognostic determinants. Chest. (2001) 120(4):1212–7. 10.1378/chest.120.4.1212
34.
Byrne RA Rossello X Coughlan JJ Barbato E Berry C Chieffo A et al 2023 ESC guidelines for the management of acute coronary syndromes: developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J Acute Cardiovasc Care. (2024) 13(1):55–161. 10.1093/ehjacc/zuad107
Summary
Keywords
acute coronary syndrome, de Winter ECG pattern, coronary angiography, left anterior descending, upsloping ST-segment depression, electrocardiogram
Citation
Chen Y, Chen B, Zhang L, Liao W and Wang M (2025) The dynamic evolution of the de Winter ECG pattern that is easily overlooked and life-threatening: a case report and literature review. Front. Cardiovasc. Med. 12:1574829. doi: 10.3389/fcvm.2025.1574829
Received
11 February 2025
Accepted
21 August 2025
Published
10 September 2025
Volume
12 - 2025
Edited by
Dragos Cretoiu, Carol Davila University of Medicine and Pharmacy, Romania
Reviewed by
Natallia Maroz-Vadalazhskaya, Belarusian State Medical University, Belarus
Dongpu Shao, First Affiliated Hospital of Jilin University, China
Updates
Copyright
© 2025 Chen, Chen, Zhang, Liao and Wang.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Miao Wang 04benwangmiao@163.com Wang Liao crain_lw@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.