- 1Cardiology Department, Heart Hospital, Hamad Medical Corporation, Doha, Qatar
- 2Pharmacy Department, Heart Hospital, Hamad Medical Corporation, Doha, Qatar
- 3Internal Medicine Department, Hamad General Hospital, Hamad Medical Corporation, Doha, Qatar
Background: Unplanned readmissions after percutaneous coronary intervention (PCI) in patients with ST-elevation myocardial infarction (STEMI) significantly impact healthcare systems. However, most of the existing literature focuses on short-term readmission rates and causes, with limited data on long-term readmissions. To date, no studies have evaluated the unplanned readmission post-PCI in STEMI patients within the Arab Gulf region. This study aimed to determine the rates, causes, and predictors of readmission post-PCI among STEMI patients over a one-year follow-up in Qatar, one of the Arab Gulf countries.
Methods: We conducted a single-center retrospective cohort study at Hamad Medical Corporation in Qatar, involving 1,257 patients who underwent PCI during their index STEMI admission between January 1, 2016, and September 30, 2018. Patients were divided into two groups; (1) those who had one or more unplanned readmission within one year after PCI; (2) and those who did not have readmissions. The outcomes evaluated were the rates, causes, and predictors of all-cause and cardiac readmissions within one year post-PCI.
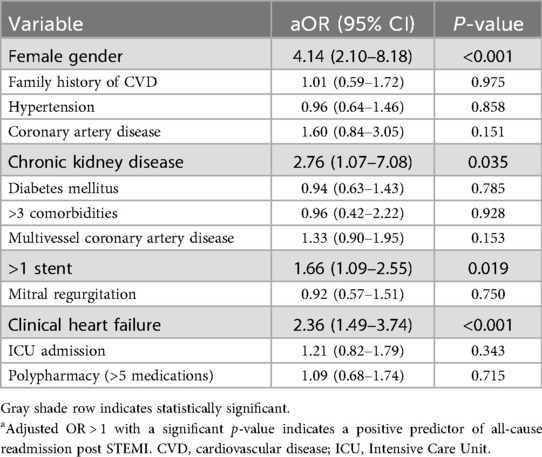
Results: The mean age of the study population was 51 ± 10 years, and male gender presented 96%. The rate of all-cause readmission within one year post-PCI was 11.5%, with 8.2% due to cardiac reasons. Positive predictors of all-cause readmission included female gender (aOR = 4.14, 95% CI 2.10–8.18, p < 0.001), chronic kidney disease (aOR = 2.76, 95% CI 1.07–7.08, p = 0.035), more than one stent during PCI (aOR = 1.66, 95% CI 1.09–2.55, p = 0.019), and clinical heart failure during the index admission (aOR = 2.36, 95% CI 1.49–3.74, p < 0.001).
Conclusion: This study highlights the need for targeted management strategies for high-risk populations to reduce readmission rates.
1 Introduction
ST-elevation myocardial infarction (STEMI) is a critical cardiac event that requires prompt and effective intervention to reduce mortality and morbidity. Primary percutaneous coronary intervention (PCI) is the standard of care for STEMI, serving as the primary revascularization modality that significantly improves both short- and long-term outcomes. Advances in stent technology, pharmacotherapy, and interventional practices have further enhanced procedural outcomes post-PCI, resulting in reduced in-hospital mortality and complication rates (1, 2). However, unplanned readmissions following PCI in STEMI patients have a substantial impact on patient quality of life and the healthcare system, particularly since some of these readmissions could be preventable by recognizing and addressing modifiable causes and risk factors (3–6).
The nature and impact of readmissions post-PCI, in the context of acute coronary syndrome (ACS) in general and STEMI in particular, are complex. Despite the numerous efforts to reduce these readmissions, their incidence remains substantial, with reported rates roughly ranging between 5% and 20% (3, 7, 8). Most previous studies have primarily focused on short-term readmissions within 30 days (3, 9–20), with limited literature evaluating long-term readmission rates within one year and their predictors post-PCI (7, 21). Moreover, to the best of our knowledge, no study has evaluated unplanned readmissions post-PCI in patients with STEMI in the Arab Gulf region, including Qatar. In this region, the population and cardiac patients tend to be younger compared to other countries, making them a unique group that may experience different post-PCI outcomes.
Previous studies showed that heart failure, recurrent ischemia, and chest pain were the most frequent causes for readmission post-PCI (3, 7, 14, 16). Reported risk factors associated with higher readmission rates include female sex, chronic kidney disease (CKD), and prior heart failure (3, 4, 9, 10).
This study aimed to evaluate the incidence, predictors, and causes of unplanned hospital readmissions within one year following PCI in patients with STEMI. The study will provide valuable insights for healthcare providers to improve treatment and discharge policies and develop outpatient follow-up schedules tailored to high-risk patients, potentially reducing morbidity and mortality following PCI in STEMI patients. Additionally, identifying and addressing the preventable causes of readmissions may help decrease unnecessary costs and optimize bed capacity and financial resources within the healthcare system (22, 23).
2 Methods
2.1 Study design and population
We conducted a retrospective observational cohort study at Heart Hospital, which is the main tertiary cardiology center with Hamad Medical Corporation in Qatar. The study was approved by Hamad Medical Corporation Medical Research Centre and Institutional Review Board in Qatar (MRC-01-21-474).
The study included all patients admitted to Heart Hospital with a diagnosis of STEMI who underwent PCI during the index admission and were discharged alive between January 1, 2016, and September 30, 2018, using whole population sampling. Patients who died during the index admission or were admitted for elective PCI were excluded. Patients were divided into two groups: those who had one or more unplanned readmissions within one year after PCI (group 1), and those who did not (group 2).
2.2 Data collection
Data were extracted from electronic medical records using pretested data collection through MS excel, and data entry was verified by two study authors. Data included baseline demographics, clinical characteristics, comorbidities, initial and peak cardiac biomarkers (troponin-T), echocardiographic parameters, procedural details, inpatient outcomes, discharge medications, and one-year clinical outcomes. The outcomes of interest were the rates, causes, and predictors of all-cause, cardiac readmissions, and heart failure readmission within one year post-PCI.
2.3 Statistical analysis
Descriptive statistics were used to summarize baseline characteristics and outcomes. Continuous variables were expressed as mean ± standard deviation or median [interquartile range] where appropriate. Categorical variables were expressed as frequencies and percentages. Univariate logistic regression analysis for baseline patient- and disease-related characteristics was conducted. Then multivariate logistic regression model using pre-specified clinically significant variables was used to identify predictors of readmission, and results were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI). A p-value < 0.05 was considered statistically significant.
3 Results
3.1 Baseline characteristics
A total of 1,257 patients were included in the analysis (Table 1). The mean age was 51 ± 10 years, and the majority were male (95.9%). Most patients were of Asian origin (76.6%), followed by those from the Middle East (19.9%). A significant proportion were current smokers (50.8%). Common comorbidities included diabetes mellitus (41.8%), hypertension (32.7%), and dyslipidemia (31.0%). Primary PCI was performed in 99.6% of patients, with the most frequent culprit vessel being the Left Anterior Descending artery (LAD) (56.3%), followed by right coronary artery (RCA) (33.3%). Around half of the study population (52.2%) had multivessel disease and 8.1% underwent staged PCI as inpatient, while 14.9% underwent staged PCI as outpatient. Around 17.7% of patients had reduced ejection fraction of less than 40% during the index admission.
3.2 Inpatient outcomes
During the index admission, clinical heart failure was noted in 13.4% of patients, and 55.1% required ICU admission. The median length of stay was 3 days with interquartile range of 1. Other inpatient complications included cardiogenic shock (4.8%), cardiac arrest (6.7%), and acute kidney injury (6.3%) (Table 2).
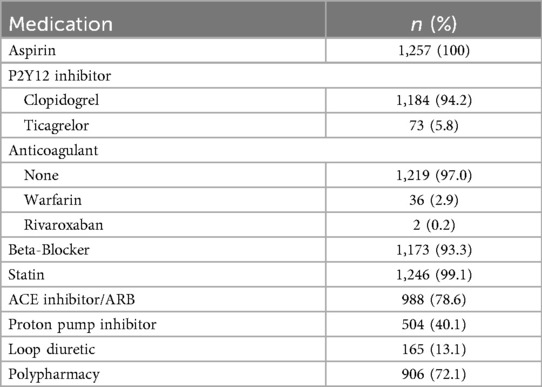
3.3 Discharge medications
At discharge, 100% of patients were prescribed aspirin and P2Y12 inhibitors, with clopidogrel being the most common (94.2%), 99.1% were on statins. Other commonly prescribed medications included beta-blockers (93.3%), ACE inhibitors/ARBs (78.6%) (Table 3).
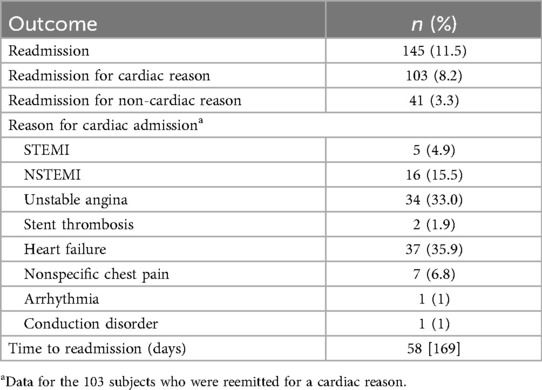
3.4 One-year clinical outcomes
The all-cause readmission rate within one year was 11.5%, with 8.2% attributed to cardiac causes and 3.3% to non-cardiac causes. The most common cardiac causes for readmissions were heart failure (35.9% of cardiac causes) and unstable angina (33.0%), followed by NSTEMI (15.5%) and STEMI (4.9%). Nonspecific chest pain accounted for 6.8% of cases. The median time to readmission was 58 days (Table 4).
3.5 Predictors of all-cause readmission
Multivariate analysis identified female gender (aOR = 4.14, 95% CI 2.10–8.18, p < 0.001), chronic kidney disease (CKD) (aOR = 2.76, 95% CI 1.07–7.08, p = 0.035), use of more than one stent during PCI (aOR = 1.66, 95% CI 1.09–2.55, p = 0.019), and clinical heart failure during the index admission (aOR = 2.36, 95% CI 1.49–3.74, p < 0.001) as significant predictors of all-cause readmission (Table 5).
3.6 Predictors of cardiac readmission
Predictors of cardiac readmission included female gender (aOR = 3.20, 95% CI 1.46–7.00, p = 0.004), CKD (aOR = 3.65, 95% CI 1.32–10.09, p = 0.013), and clinical heart failure (aOR = 2.98, 95% CI 1.79–4.96, p < 0.001) (Table 6).
3.7 Predictors of readmission for heart failure
Female gender (aOR = 3.80, 95% CI 1.22–11.86, p = 0.021), CKD (aOR = 4.56, 95% CI 1.22–17.03, p = 0.024), mitral regurgitation (aOR = 3.13, 95% CI 1.39–7.03, p = 0.006), and clinical heart failure (aOR = 4.82, 95% CI 1.53–15.15, p = 0.007) were associated with an increased likelihood of readmission due to heart failure (Table 7).
4 Discussion
Unplanned readmissions following PCI in patients with STEMI impact patient quality of life and place considerable strain on the healthcare system. They may also be considered as indicators of care quality, making it essential to evaluate their causes and predictors (3–6).
Our study provides comprehensive data on the rates, causes, and predictors of unplanned readmissions within one-year post-PCI in patients with STEMI. The overall unplanned one-year readmission rate was 11.5%, with 8.2% of the readmissions being cardiac-related and 3.3% due to non-cardiac causes. These results are consistent with the broader literature. However, compared to our study, most of the related studies evaluated a relatively short-term readmission within 30 days (8, 9, 11–13, 15, 17). In a multicenter randomized trial involving 1,137 STEMI patients undergoing PCI, the rate of all-cause re-hospitalization, including both cardiac and non-cardiac causes, at one year was 18.6%, which is slightly higher than the incidence observed in our study (7). Kwok et al. reported that 30-day readmission rates range between 4.7% and 15.6% in patients undergoing PCI, aligning with our findings over a longer one-year follow-up (3). Additionally, Rymer et al. and Jang et al. further support our results with similar 30-day readmission rates after PCI, reported as 14% and 12%, respectively, indicating that the majority of readmissions occur early, within the first month post-PCI (8, 15).
The variance between studies in the timeframe of follow-up (30-day vs. one-year) is critical in understanding and comparing readmission rates. Despite these variations, our study's readmission rate falls within the expected range for this patient population. The median time to readmission in our study was 58 days, which means that more than half of the patients were readmitted within the first two months after being discharged. This suggests that the risk of readmission is highest early post-discharge with the incidence declining thereafter over the one-year follow-up period.
In our cohort, among the cardiac readmissions, the most common causes were heart failure (35.9%) and unstable angina (33.0%), followed by NSTEMI (15.5%) and STEMI (4.9%). Nonspecific chest pain accounted for 6.8% of cases. Likewise Sud et al., found that the leading causes of 30-day readmission after STEMI were congestive heart failure (25.7%) and ACS (9.4%) (14). Similarly, Tripathi et al. also identified heart failure and ischemic heart disease as the most common etiologies for readmission (16). Spitzer et al. reported that one-year readmissions post-PCI in STEMI patients due to chest pain without evidence of ischemia were more frequent than those with ischemic evidence (20.4% vs. 16.9%, respectively). These observations align with our findings, where unstable angina was a more common cause of readmission compared to STEMI and NSTEMI combined. This highlights the prevalence of non-ischemic chest pain as a significant contributor to readmissions in this patient population (7).
In our multivariate analysis, we identified female gender, CKD, and clinical heart failure during the index admission as significant predictors of all-cause readmissions, cardiac-related readmissions, and readmissions due to heart failure. Additionally, the use of more than one stent during PCI was found to be a predictor of all-cause readmission, while mitral regurgitation was a significant predictor of heart failure-related readmission.
Interestingly, our study did not find age or reduced LVEF to be independent predictors, contrary to prior studies (3, 7, 24). These differences may reflect our unique study population characteristics. As noted in the Introduction, the majority of patients were younger males (mean age 51 years; 95.9% male), and the prevalence of certain comorbidities such as peripheral vascular disease was low. Additionally, our cohort was predominantly composed of migrant workers from South and Southeast Asia, who may have different health behaviors, access patterns, and outcomes compared to Western populations.
Kwok et al. also identified female sex, CKD, and heart failure as major predictors of readmission, closely matching our results (3). Similarly, Arnold et al. found that female sex and prior heart failure were strong predictors of re-hospitalization for ACS post-PCI, highlighting the commonality of these risk factors across different populations (4).
Notably, O'Brien et al. observed that women, particularly younger women, had significantly higher risks of readmission after STEMI compared to men (9). Similarly, studies by Atti et al., Steitieh et al., and Dreyer RP et al., also documented higher readmission rates among women (10, 11, 25). These findings align with our study, where female sex was associated with a 4-fold increase in the likelihood of readmission reinforcing the evidence that gender plays a critical role in post-STEMI outcomes.
While our study focused on readmissions over one-year duration post-PCI, many of the referenced studies primarily assessed 30-day readmission (3, 4, 8). Despite this difference, the predictors of readmission remain similar across both short and long-term follow-up, indicating that certain factors (e.g., female gender, CKD, heart failure) consistently influence readmission risk over time. However, our study did not identify some predictors noted in other studies, such as LVEF, age, diabetes, and peripheral vascular disease (3, 7, 24). This discrepancy may be attributed to differences in the study populations, healthcare settings, or the relatively low prevalence of these conditions in our cohort.
The strong association between clinical heart failure during the index admission and subsequent readmissions reflects the vulnerability of this subgroup and highlights the importance of optimal management of heart failure in STEMI patients. Heart failure may contribute to a higher readmission risk through multiple mechanisms; including persistent volume overload, residual myocardial dysfunction, arrhythmias, and medication intolerance. These patients usually require intensive monitoring, strict adherence to multi medications, and close follow-up to avoid decompensation. Suboptimal outpatient care or lack of structured heart failure programs may further increase their risk of readmission.
By understanding the factors driving post-PCI readmissions in STEMI patients, valuable insights can be gained that may help improve treatment protocols, discharge planning, and outpatient follow-up schedules. Tailoring these aspects to high-risk patients could potentially reduce morbidity and mortality rates. Additionally, addressing preventable causes of readmission can help lower unnecessary costs, conserve bed capacity, and optimize financial resources within the healthcare system (22, 23).
This study was a retrospective cohort study with inherit limitations. First, participants’ completion of the one year follow up duration was not ensured in view of the retrospective design, which might have under-estimated the readmission rates. Second, we determined the readmission rates using the electronic medical records at Hamad Medical Corporation without accounting for admissions to other health sectors. Nevertheless, Hamad Medical Corporation is the leading healthcare sector in Qatar and the study site is the primary cardiac tertiary center and the main referral center in the country with an integrated electronic system across the organization, which limits the possibility of missing readmission outcomes. Third, the study population was relatively young with a mean age of 51 years which might have contributed to limited impact of comorbidities as predictors of readmission.
The male predominance in our study population (95.9%) reflects the demographic structure of Qatar, where the majority of the population consists of immigrant workers who are predominantly male. According to the World Bank, males account for approximately 71.52% of the total population. This disparity is largely attributed to the influx of male migrant workers, particularly in the construction and service industries. Therefore, the gender distribution in our study represents the underlying population rather than any selection or randomization bias.
Based on our findings, future research should focus on developing and validating predictive models tailored to Middle Eastern and South Asian populations, incorporating demographic, procedural, and social factors. Prospective cohort studies or multicenter registries could assess the generalizability of our results and help refine patient-specific post-discharge interventions. In addition, qualitative studies exploring psychosocial determinants of readmission—especially among women and younger patients—may uncover modifiable factors. Finally, randomized trials evaluating structured discharge planning and heart failure transitional care in high-risk STEMI patients could provide evidence to reduce preventable readmissions.
5 Conclusion
The rate of one-year unplanned readmissions after PCI among patients with STEMI was 11.5%, with over two-thirds of these readmissions attributed to cardiac causes. Acute coronary syndromes and heart failure were the most common causes of readmission. Identified predictors of all-cause readmission were female gender, CKD, multiple stents, and clinical heart failure. Implementing targeted follow-up strategies and personalized discharge planning for high-risk groups may help reduce unplanned readmissions and optimize resource utilization.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by HMC Medical Research Centre (MRC) and Institutional Review Board (IRB) in Qatar (MRC-01-21-474). The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
OA: Project administration, Supervision, Writing – original draft, Writing – review & editing. AR: Data curation, Formal analysis, Methodology, Writing – review & editing. MAlt: Data curation, Investigation, Writing – original draft. MAb: Investigation, Methodology, Writing – original draft. MS: Investigation, Methodology, Writing – review & editing. KS: Data curation, Investigation, Writing – review & editing. MH: Investigation, Validation, Writing – original draft. YH: Data curation, Investigation, Writing – review & editing. MB: Data curation, Investigation, Writing – review & editing. MAlk: Investigation, Methodology, Writing – original draft. MA-H: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. AA: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The open-access publication fees were covered by the Medical Research Center (MRC) at Hamad Medical Corporation (HMC), Qatar.
Acknowledgments
We thank the Medical Research Center (MRC) at Hamad Medical Corporation (HMC) in Qatar for funding the publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. During the preparation of this study, the authors used ChatGPT in order to improve the readability and language of the manuscript. After using this tool, the authors reviewed and edited the content as needed and take full responsibility for the content of the published article.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stathopoulos I, Jimenez M, Panagopoulos G, Kwak EJ, Losquadro M, Cohen H, et al. The decline in PCI complication rate: 2003–2006 versus 1999–2002. Hellenic J Cardiol. (2009) 50(5):379–87.19767279
2. Valle JA, Smith DE, Booher AM, Menees DS, Gurm HS. Cause and circumstance of in-hospital mortality among patients undergoing contemporary percutaneous coronary intervention. Circ Cardiovasc Qual Outcomes. (2012) 5:229–35.
3. Kwok CS, Hulme W, OLier I, Holroyd E, Mamas MA. Review of early hospitalizations after percutaneous coronary intervention. Int J Cardiol. (2017) 227:370–7.27839805
4. Arnold SV, Smolderen KG, Kennedy KF, Li Y, Shore S, Stolker JM, et al. Risk factors for rehospitalization for acute coronary syndromes and unplanned revascularization following acute myocardial infarction. J Am Heart Assoc. (2015) 4(2):e001352. doi: 10.1161/JAHA.114.001352
5. Goldfield NI, McCullough EC, Hughes JS, Tang AM, Eastman B, Rawlins LK, et al. Identifying potentially preventable readmissions. Health Care Financ Rev. (2008) 30(1):75–91.19040175
6. Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. (2006) 44:972–81.17063128
7. Spitzer E, Frei M, Zaugg S, Hadorn S, Kelbaek H, Ostojic M, et al. Rehospitalizations following primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: results from a multi-center randomized trial. J Am Heart Assoc. (2017) 6(8):e005926. doi: 10.1161/JAHA.117.005926
8. Rymer JA, Chen AY, Thomas L, Fonarow GC, Peterson ED, Wang TY. Readmissions after acute myocardial infarction: how often do patients return to the discharging hospital? J Am Heart Assoc. (2019) 8(19):e012059. doi: 10.1161/JAHA.119.012059
9. O'Brien C, Valsdottir L, Wasfy JH, Strom JB, Secemsky EA, Wang Y, et al. Comparison of 30-day readmission rates after hospitalization for acute myocardial infarction in men versus women. Am J Cardiol. (2017) 120(7):1070–6. doi: 10.1016/j.amjcard.2017.06.046
10. Atti V, Patel NJ, Kumar V, Tripathi B, Basir MB, Voeltz M, et al. Frequency of 30-day readmission and its causes after percutaneous coronary intervention in acute myocardial infarction complicated by cardiogenic shock. Catheter Cardiovasc Interv. (2019) 94(2):E67–77. doi: 10.1002/ccd.28161
11. Steitieh DA, Lu DY, Kalil RK, Kim LK, Sharma G, Yeo I, et al. Sex-based differences in revascularization and 30-day readmission after ST-segment-elevation myocardial infarction in the United States. Cardiovasc Revasc Med. (2021) 31:41–7. doi: 10.1016/j.carrev.2020.12.016
12. Li J, Dharmarajan K, Bai X, Masoudi FA, Spertus JA, Li X, et al. Thirty-day hospital readmission after acute myocardial infarction in China. Circ Cardiovasc Qual Outcomes. (2019) 12(5):e005628. doi: 10.1161/CIRCOUTCOMES.119.005628
13. Wang H, Zhao T, Wei X, Lu H, Lin X. The prevalence of 30-day readmission after acute myocardial infarction: a systematic review and meta-analysis. Clin Cardiol. (2019) 42(10):889–98. doi: 10.1002/clc.23238
14. Sud K, Haddadin F, Tsutsui RS, Parashar A, Bandyopadhyay D, Ellis SG, et al. Readmissions in ST-elevation myocardial infarction and cardiogenic shock (from nationwide readmission database). Am J Cardiol. (2019) 124(12):1841–50. doi: 10.1016/j.amjcard.2019.08.048
15. Jang SJ, Yeo I, Feldman DN, Cheung JW, Minutello RM, Singh HS, et al. Associations between hospital length of stay, 30-day readmission, and costs in ST-segment-elevation myocardial infarction after primary percutaneous coronary intervention: a nationwide readmissions database analysis. J Am Heart Assoc. (2020) 9(11):e015503. doi: 10.1161/JAHA.119.015503
16. Tripathi B, Yeh RW, Bavishi CP, Sardar P, Atti V, Mukherjee D, et al. Etiologies, trends, and predictors of readmission in ST-elevation myocardial infarction patients undergoing multivessel percutaneous coronary intervention. Catheter Cardiovasc Interv. (2019) 94(7):905–14. doi: 10.1002/ccd.28344
17. Chen J, Kiefe CI, Gagnier M, Lessard D, McManus D, Wang B, et al. Non-specific pain and 30-day readmission in acute coronary syndromes: findings from the TRACE-CORE prospective cohort. BMC Cardiovasc Disord. (2021) 21(1):383. doi: 10.1186/s12872-021-02195-z
18. Cholack G, Garfein J, Krallman R, Feldeisen D, Montgomery D, Kline-Rogers E, et al. Predictors of early (0–7 days) and late (8–30 days) readmission in a cohort of acute coronary syndrome patients. Int J Med Stud. (2022) 10(1):38–48. doi: 10.5195/ijms.2022.1058
19. Mahmoud AN, Elgendy IY, Mojadidi MK, Wayangankar SA, Bavry AA, Anderson RD, et al. Prevalence, causes, and predictors of 30-day readmissions following hospitalization with acute myocardial infarction complicated by cardiogenic shock: findings from the 2013–2014 national readmissions database. J Am Heart Assoc. (2018) 7(6):e008235. doi: 10.1161/JAHA.117.008235
20. Tang L, Li K, Wu CJ. Thirty-day readmission, length of stay and self-management behaviour among patients with acute coronary syndrome and type 2 diabetes mellitus: a scoping review. J Clin Nurs. (2020) 29(3-4):320–9. doi: 10.1111/jocn.15087
21. Shah IT, Keeley EC. Unplanned readmissions after acute myocardial infarction: 1-year trajectory following discharge from a safety net hospital. Crit Pathw Cardiol. (2019) 18(2):72–4. doi: 10.1097/HPC.0000000000000170
22. Murad H, Basheikh M, Zayed M, Albeladi R, Alsayed Y. The association between medication non-adherence and early and late readmission rates for patients with acute coronary syndrome. Int J Gen Med. (2022) 15:6791–9. doi: 10.2147/IJGM.S376926
23. Rashidi A, Whitehead L, Glass C. Factors affecting hospital readmission rates following an acute coronary syndrome: a systematic review. J Clin Nurs. (2022) 31(17-18):2377–97. doi: 10.1111/jocn.16122
24. Bustea C, Tit DM, Bungau AF, Bungau SG, Pantea VA, Babes EE, et al. Predictors of readmission after the first acute coronary syndrome and the risk of recurrent cardiovascular events-seven years of patient follow-up. Life (Basel). (2023) 13(4):950. doi: 10.3390/life13040950
Keywords: ST-elevation myocardial infarction, readmission, percutaneous coronary intervention, predictors, causes
Citation: Alkhalaila O, Rahhal A, Altermanini M, Abdelghani MS, Shehadeh M, Shunnar K, Habib MB, Hailan Y, Barakat M, Alkhateeb MH, Al-Hijji M and Arabi AR (2025) One-year unplanned readmission after percutaneous coronary intervention in ST-elevation myocardial infarction: rates, causes, and predictors—a retrospective cohort study. Front. Cardiovasc. Med. 12:1581371. doi: 10.3389/fcvm.2025.1581371
Received: 22 February 2025; Accepted: 25 August 2025;
Published: 16 September 2025.
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Sally Aman Nasution, University of Indonesia, IndonesiaJehangir Ali Shah Sheerazi, National Institute of Cardiovascular Diseases, Pakistan
Copyright: © 2025 Alkhalaila, Rahhal, Altermanini, Abdelghani, Shehadeh, Shunnar, Habib, Hailan, Barakat, Alkhateeb, Al-Hijji and Arabi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: O. Alkhalaila, b2Fsa2hhbGFpbGFAaGFtYWQucWE=
 O. Alkhalaila
O. Alkhalaila A. Rahhal
A. Rahhal M. Altermanini
M. Altermanini M. S. Abdelghani1
M. S. Abdelghani1 A. R. Arabi
A. R. Arabi