- 1Division of Cardiology, Department of Paediatrics, Khoo Teck Puat-National University Children’s Medical Institute, National University Health System, Singapore, Singapore
- 2Department of Neonatology, Khoo Teck Puat-National University Children’s Medical Institute, National University Health System, Singapore, Singapore
- 3Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 4Biostatistics Unit, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
Introduction: Cyanotic congenital heart disease with duct-dependent pulmonary blood flow requires initial palliation before definitive repair. Traditionally, these were surgical systemic-to-pulmonary shunts (SPS) such as the modified Blalock-Taussig-Thomas shunt. Transcatheter procedures are recently emerging as alternative options. Previous reviews have compared ductal stenting (DS) or right ventricular outflow tract (RVOT) intervention to surgical SPS, but none compared all three strategies in a single meta-analysis.
Methods: We performed a systematic review and network meta-analysis for a three-way comparison of DS, RVOT intervention, and surgical SPS as initial palliation in children aged 0–3 with cyanotic congenital heart disease. Primary outcomes were mortality rates, complication rates, and re-intervention rates. MEDLINE, EMBASE, and Cochrane databases were searched for publications from 2003 to 2023. References of previous systematic reviews were screened.
Results: Twenty publications were included for analysis, for a total of 4,441 patients. Transcatheter options consistently ranked superior to surgical SPS for Early and Overall Mortality. DS also outperformed surgical SPS for Procedural Complications. Surgical SPS was worst for Early Re-interventions, but outperforms both transcatheter options for Overall Re-interventions and Intra-procedural Mortality. Both DS and RVOT stenting conferred a shorter overall hospitalization duration compared to surgical SPS, and DS also gave a shorter length of stay in intensive care compared to surgical SPS.
Conclusions: Transcatheter options are viable, safe, and attractive alternatives to traditional surgical shunts in the treatment of duct-dependent cyanotic heart disease. With wider adoption, increased collective expertise will help to further improve patient outcomes of these less-invasive techniques.
Systematic Review Registration: PROSPERO (CRD42024489748).
1 Introduction
Cyanotic congenital heart disease with duct-dependent pulmonary blood flow often requires an initial palliation to allow somatic growth before definitive repair. Traditionally, a surgical systemic-to-pulmonary shunt (SPS) is created to secure a more reliable source of pulmonary blood flow, with the modified Blalock-Taussig-Thomas shunt (mBTS) being the most common.
Transcatheter procedures are emerging as options to a surgical approach (1). One such strategy is ductal stenting (DS), where a stent is placed in the native ductus arteriosus to keep it patent without having a continuous intravenous prostaglandin infusion. This secures a medium-term solution while avoiding the need for immediate surgery.
More recently, right ventricular outflow tract (RVOT) intervention by stenting or ballooning has been explored as another strategy, where the native right ventricular outflow tract is augmented to improve antegrade pulmonary blood flow, thus eliminating the need for a surgical shunt.
Previous reviews have compared either DS or RVOT intervention against the traditional surgical SPS, but there is none comparing all three strategies against each other in a single systematic review or meta-analysis (2–7). The aim of this study is to conduct a systematic review and meta-analysis for a three-way comparison of the safety and efficacy of two transcatheter options (DS and RVOT intervention) and surgical SPS.
2 Methods
This systematic review and meta-analysis was conducted and reported in accordance with the standards established in the Cochrane Handbook for Systematic Reviews of Interventions and Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement (8). The methodology of this paper was published pre-hoc in the International Prospective Register of Systematic Reviews (PROSPERO) registry (CRD42024489748).
2.1 Eligibility criteria
Publications were included for review if they met the following inclusion criteria: English language, full-length articles, human subjects aged 0 to 3 years, comparative study of at least one transcatheter option (DS or RVOT intervention) against SPS as a control group, and described at least one outcome of interest.
Publications which were not a comparative study were excluded (such as case reports, case series, topical reviews, and opinion pieces), as were abstracts, oral presentations, and conference proceedings without a full-length article. While systematic reviews and meta-analyses were excluded from the analysis itself, their references were manually searched for possible source of relevant publications.
2.2 Sources of information
A comprehensive literature search of MEDLINE and EMBASE databases was conducted. All publications from January 2003 to December 2023 inclusive were included. Additionally, the Cochrane Database of Systematic Reviews was searched for relevant systematic reviews.
2.3 Search strategy
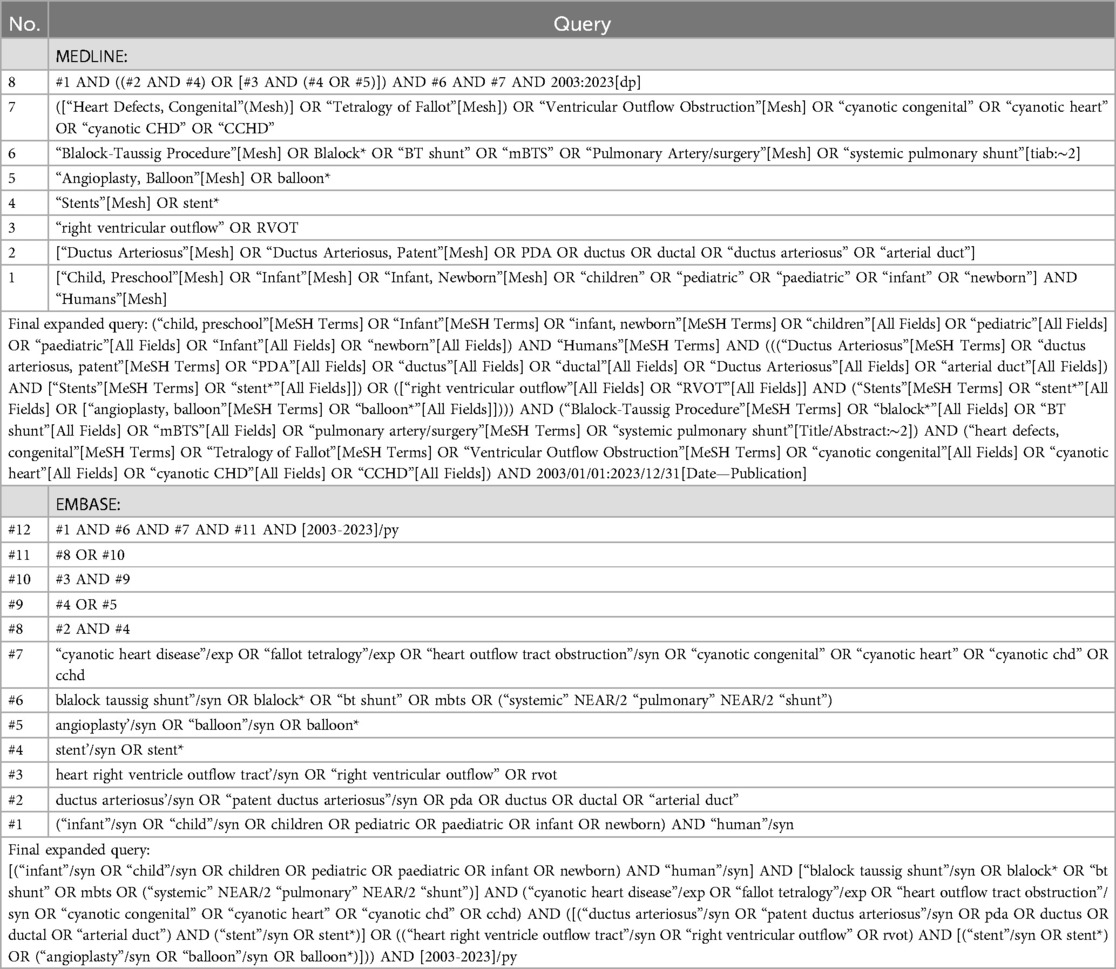
The search strategy was developed by two reviewers (CQZ and SB) in consensus. The search syntax for MEDLINE and EMBASE were constructed to replicate the search logic as similarly as possible. The complete search syntax may be found in Table 1.
The following search terms were used as free text, or where available, equivalent standard MeSH and Emtree terms: human; paediatric or children; ductus arteriosus and stent; right ventricular outflow tract, and stent or balloon; cyanotic congenital heart disease or Tetralogy of Fallot; Blalock-Taussig shunt or systemic-to-pulmonary shunt.
2.4 Data extraction
Two reviewers (CQZ and SB) screened titles and abstracts of the search results for publications relevant to study question. Where the eligibility of the publication was unclear from the title or abstract, the full text was retrieved for screening. Duplicate publications were removed, and data from included publications were extracted for further analysis.
The following outcomes were sought from each publication: Overall and Early Mortality, Overall and Early Re-intervention rate, Procedural Complications, Intra-procedural Mortality, time to second-stage surgery, length of overall hospitalization, and length of stay in intensive care unit (ICU).
As the exact criteria for defining the “Early” period varied across publications, for the purpose of our review, mortality and re-intervention outcome was considered “Early” if it occurred: within 30 days of the initial intervention, within the same admission, or considered by study authors to be directly related to the initial procedure. “Overall” referred to any instance of the outcome reported by the publication, regardless of duration of follow-up. Procedural Complications referred to complications relating to the initial procedure, as reported by each publication. Time to second-stage surgery or definitive surgery was recorded as the same outcome.
2.5 Data synthesis
Where mean and standard deviation of study groups were not directly reported, these statistics were estimated from the statistics reported by each publication, using the Data Estimation and Conversion for Meta-Analysis (DECoMA) tool (Cochrane Taiwan) (9, 10). Meta-analysis and network meta-analysis were conducted with Stata 18.0 software package (StataCorp). Two-tailed alpha was set at 0.05. Adjusted point estimates were pooled using the generic inverse variance method under the fixed-effect model.
Network meta-analysis allowed simultaneous comparison of all three interventions by direct and indirect evidence. The mean rank and surface under the cumulative ranking (SUCRA) of each intervention was calculated for each outcome of interest. Local incoherence was tested by node-splitting, while global incoherence was tested using Design-by-Treatment model to check for the entire network. The overall heterogeneity was assessed using the Chi-square test, with a threshold of p < 0.1 for significant heterogeneity. Papers that might cause significant heterogeneity were identified and removed from the network meta-analysis.
2.6 Quality appraisal
Quality appraisal of each included publication was performed by two reviewers (CQZ and SB) with the relevant risk-of-bias tool (Newcastle-Ottawa Scale was used for retrospective or prospective cohorts) (11).
2.7 Dispute resolution
Non-consensus between the two reviewers was resolved by a third senior author (CCK).
3 Results
3.1 Publication selection
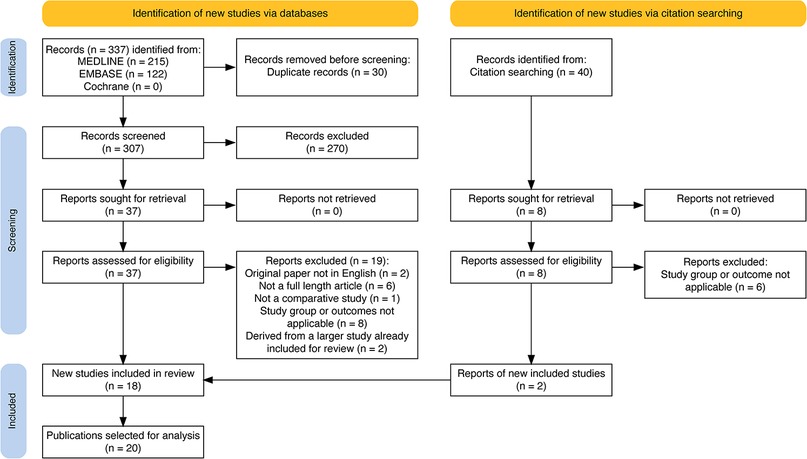
Total of 337 publications were identified from initial search of each database, and 30 duplicate publications removed. From the remaining, 270 publications were excluded during the initial screening of titles and abstracts for relevance. Of 37 left, the following exclusions were made: 2 (non-English language), 6 (not full-length articles), 1 (non-comparative study), 8 (study groups and outcomes were not relevant). Furthermore, 2 studies were identified as a subgroup analysis of a larger study already being included, and hence were removed from analysis (12, 13).
Additionally, 40 publications were identified for screening from the references of relevant systematic reviews (2–7),—from which 2 publications were eventually identified as eligible for inclusion. In effect, a total of 20 publications were selected for analysis (14–33). The PRISMA flow diagram is reported in Figure 1.
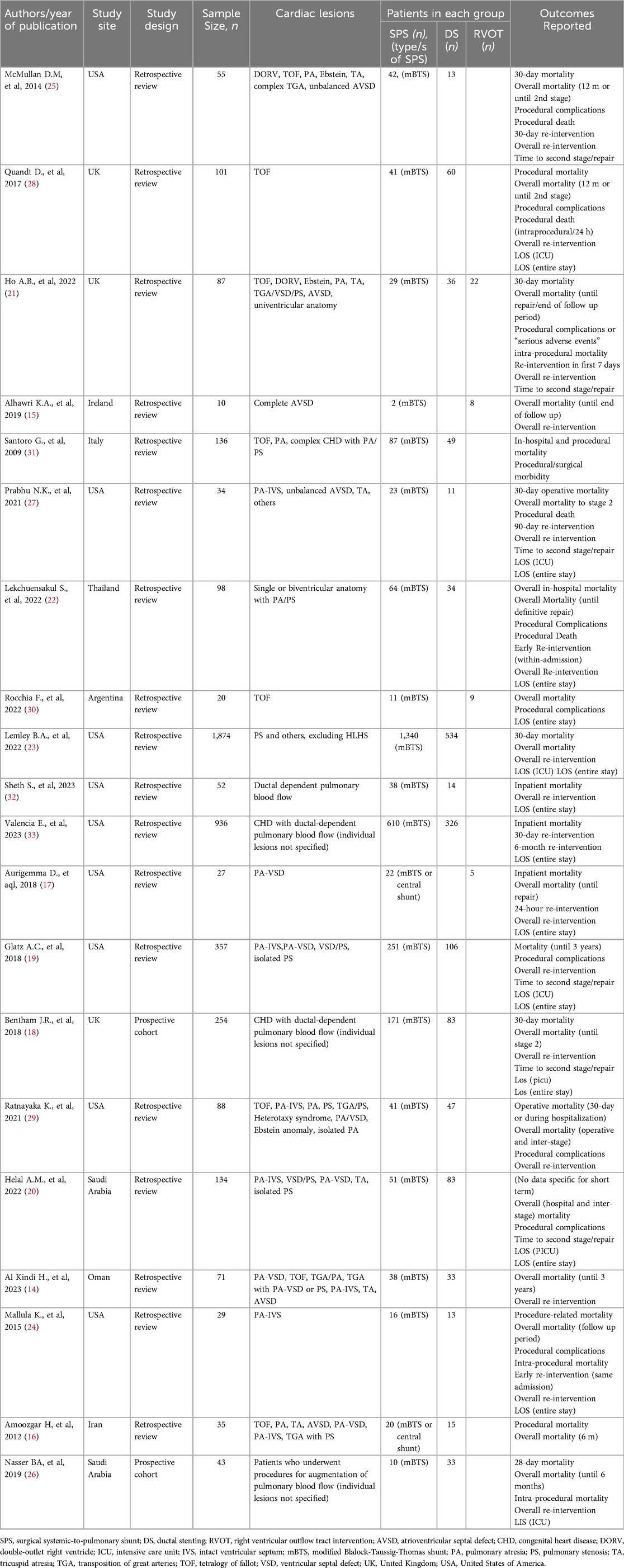
3.2 Study characteristics
The basic characteristics of each included publication are detailed in Table 2 (14–33). Among the 20 selected publications, 15 publications compared DS against SPS and 4 studies compared RVOT intervention against SPS. A single study compared all three modalities of treatment.
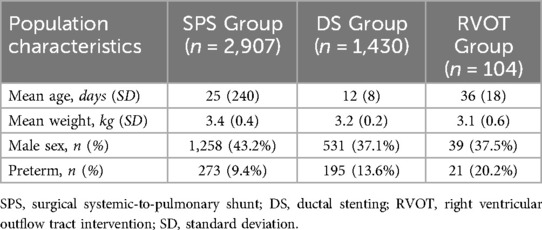
A total of 4,441 patients were analysed across all publications. Patients underwent intervention from 0 to 11 months of age. Surgical SPS included not only the most common modified Blalock-Taussig-Thomas shunt, but also central aorto-pulmonary shunts. All RVOT interventions were performed via RVOT stenting. Among patients with a reported cardiac diagnosis, 352 of 3,694 patients were classified as Tetralogy of Fallot. The baseline characteristics of the included patients are presented in Table 3.
Out of the 20 publications, all reported data for Overall Mortality, while 17 reported data for Early Mortality. Overall Re-intervention data was reported in 16 publications, while 6 reported data for Early Re-intervention. Procedural Complication rates was recorded from 10 publications, and Intra-procedural Mortality from 11 publications.
Network meta-analysis was performed for indirect comparisons and ranking of treatment modalities. There was sufficient data for network meta-analysis for the outcomes of Overall Mortality, Early Mortality, Intra-procedural Mortality, Procedural Complications, Early Re-interventions, and Overall Re-interventions. All network meta-analyses were closed loops, with at least one direct comparison between each treatment modality.
The results of risk of bias assessment done using Newcastle-Ottawa Scale (11), are presented in Table 4.
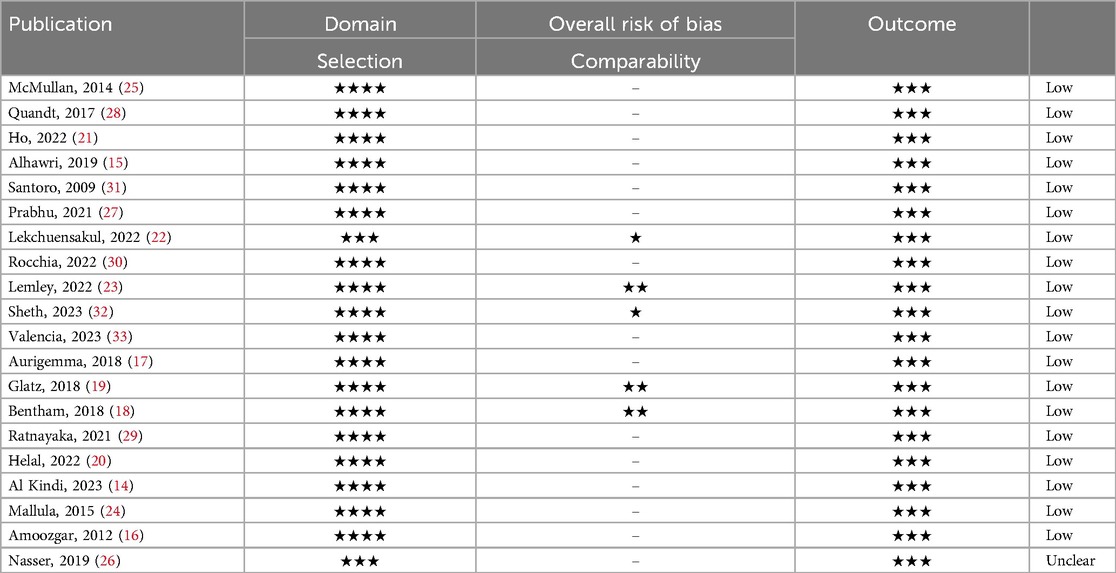
Table 4. Risk of bias assessment of publications selected for analysis by Newcastle-Ottawa scale (10).
3.3 Primary outcomes
By network meta-analysis, RVOT intervention was ranked as best modality for the outcome of Early Mortality (Figure 2), and DS was best for Overall Mortality (Figure 3). Surgical SPS was ranked the poorest modality for both Early and Overall Mortality. However, surgical SPS was the best-ranked modality for Intra-procedural Mortality (mean rank 1.5; cf. DS 2.2 and RVOT 2.3). There was no statistically significant differences between pairwise comparisons of each treatment modality for both Early Mortality and Overall Mortality (Figuress 2,3).
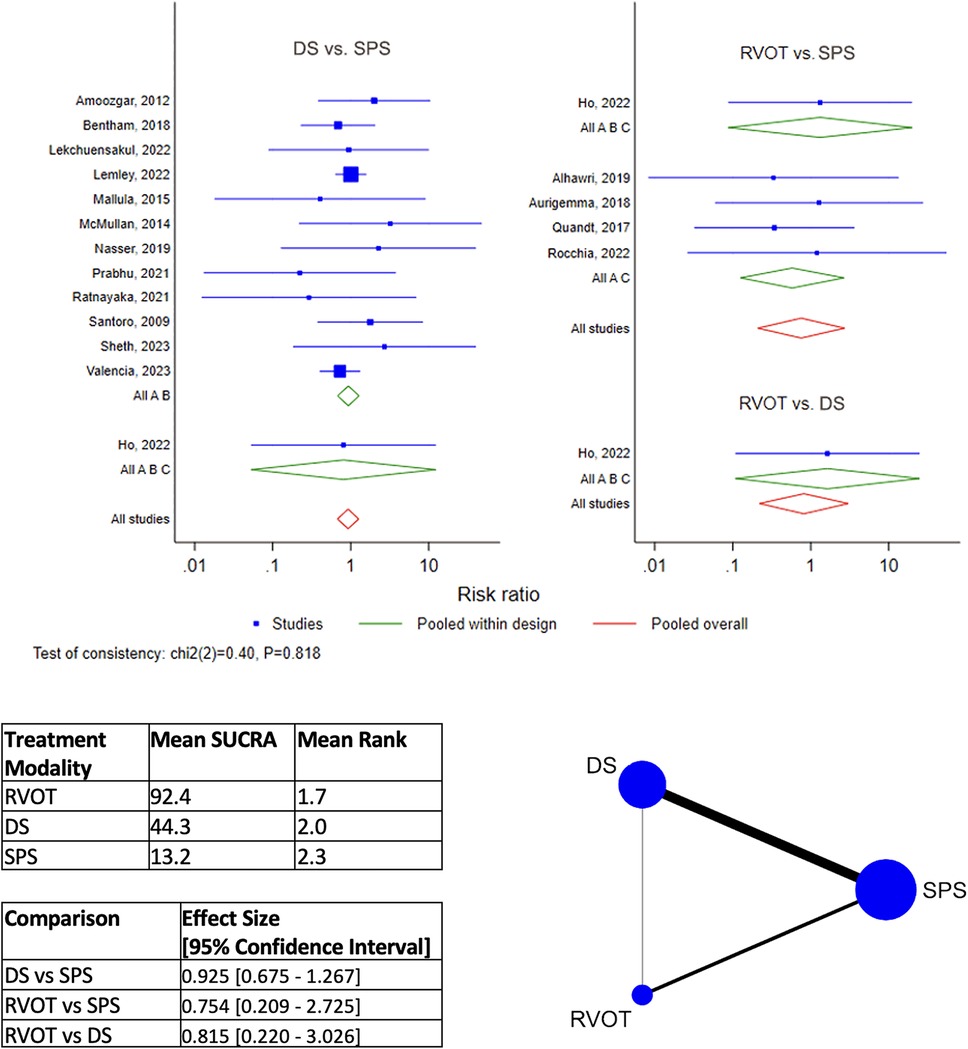
Figure 2. Results of network meta-analysis for early mortality. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; SUCRA: surface under the cumulative ranking).
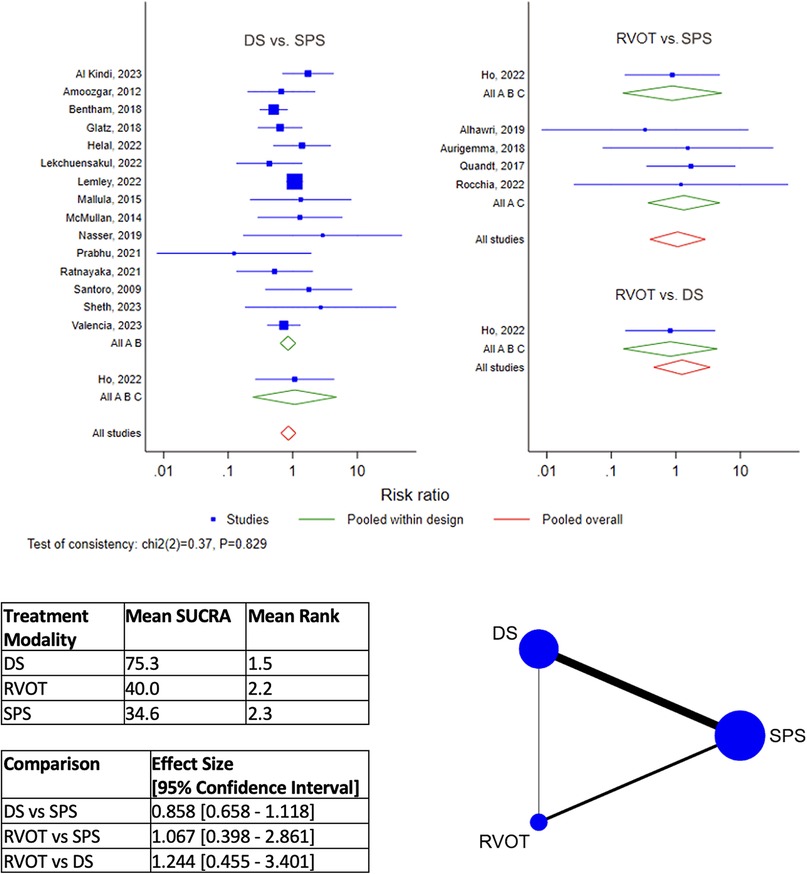
Figure 3. Results of network meta-analysis for overall mortality. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; SUCRA: surface under the cumulative ranking).
DS is the best-ranked modality for Procedural Complications (Mean SUCRA = 92.5, Mean Rank = 1.2), by network meta-analysis (Figure 4). RVOT intervention was worst-ranked for Procedural Complications (Mean SUCRA = 13.2, Men Rank = 2.7). Surgical SPS was worst-ranked by network meta-analysis for Early Re-intervention rate (Mean SUCRA = 11.3, Mean Rank = 2.8) (Figure 5), yet was best-ranked for Overall Re-intervention rate (Mean SUCRA = 95.8, Mean Rank = 1.1) (Figure 6).
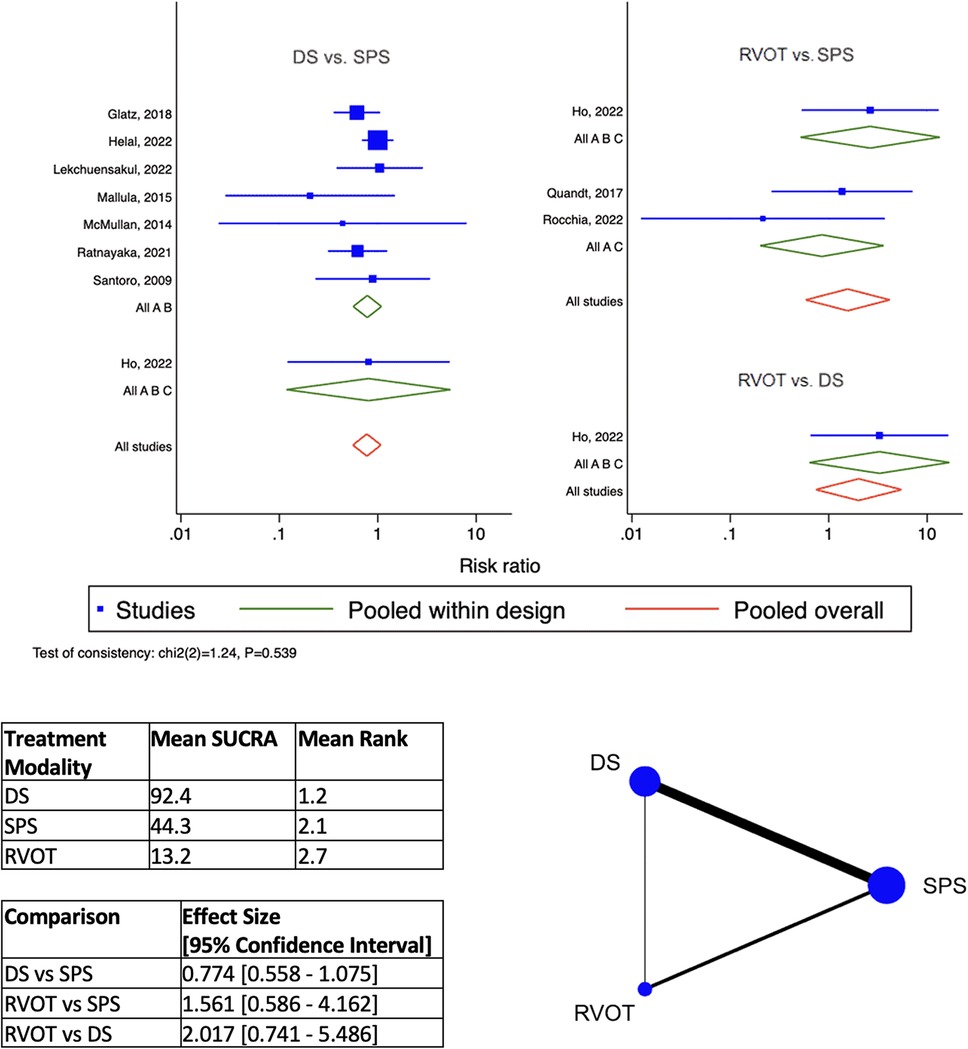
Figure 4. Results of network meta-analysis for procedural complications. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; SUCRA: surface under the cumulative ranking).
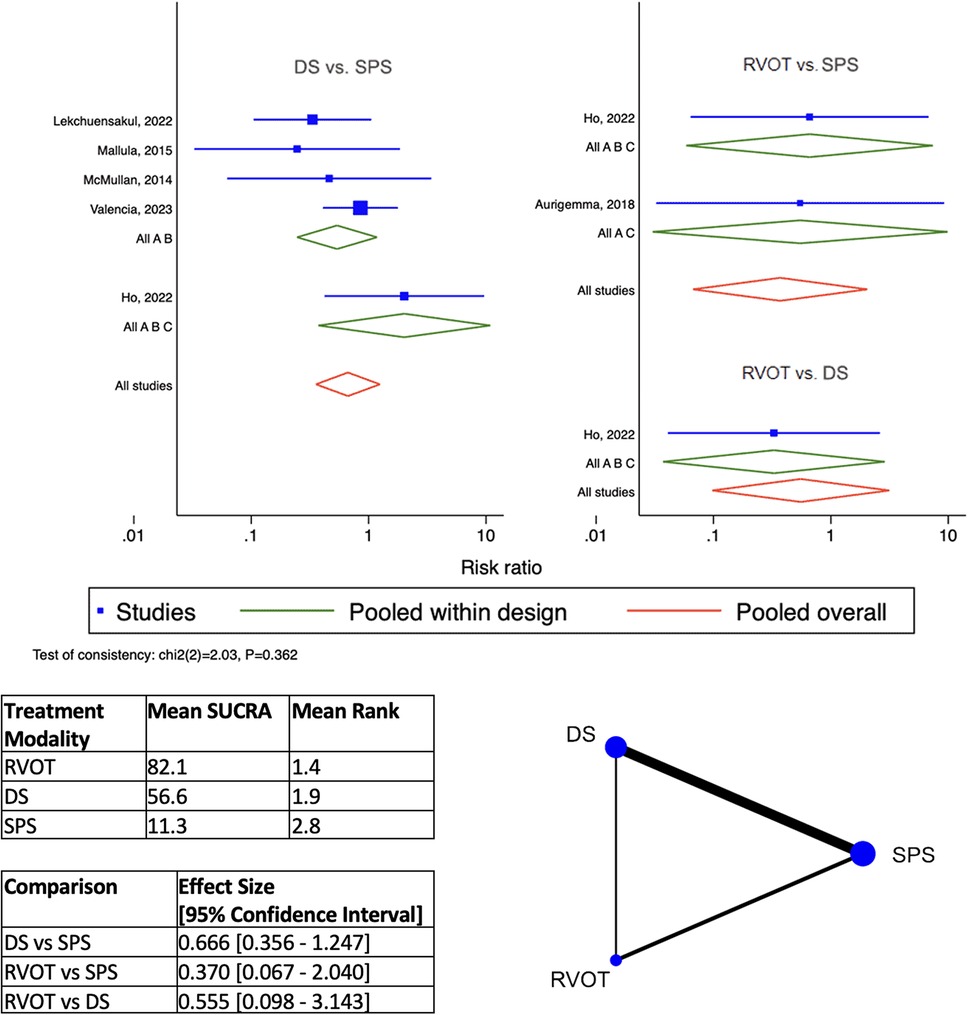
Figure 5. Results of network meta-analysis for early Re-intervention. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; SUCRA: surface under the cumulative ranking).
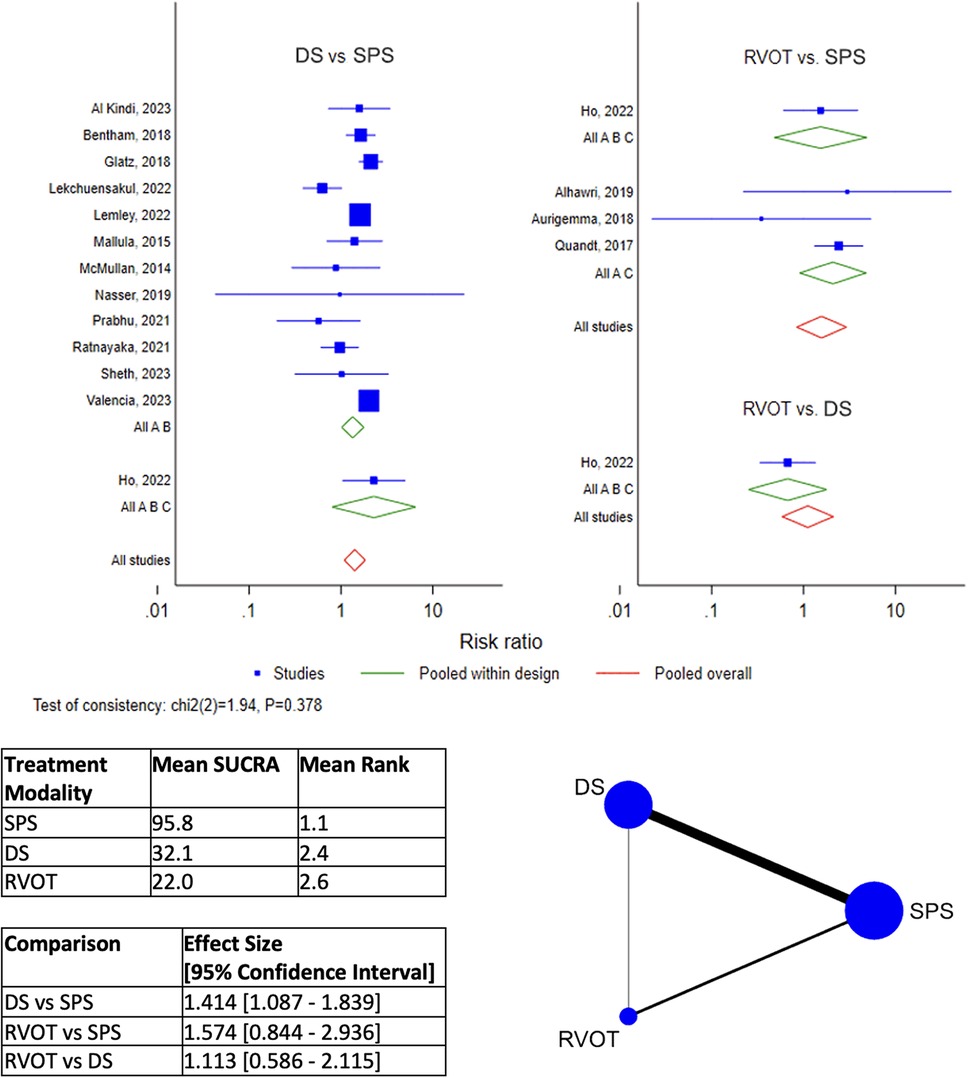
Figure 6. Results of network meta-analysis for overall Re-intervention. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; SUCRA: surface under the cumulative ranking).
3.4 Secondary outcomes
There was no difference in time to second-stage surgery (or definitive repair) between DS or surgical SPS.
Patients who underwent DS compared to surgical SPS as initial treatment had a shorter ICU stay [mean difference −0.60 (−1.06, −0.15)] (Figure 7). Both DS and RVOT intervention conferred a shorter overall hospitalization duration compared to surgical SPS, with results slightly favouring RVOT intervention over DS [RVOT vs. SPS mean difference −0.54 [−0.88 to −0.20]; DS vs. SPS mean difference −0.49 [−0.62 to −0.36]] (Figure 7).
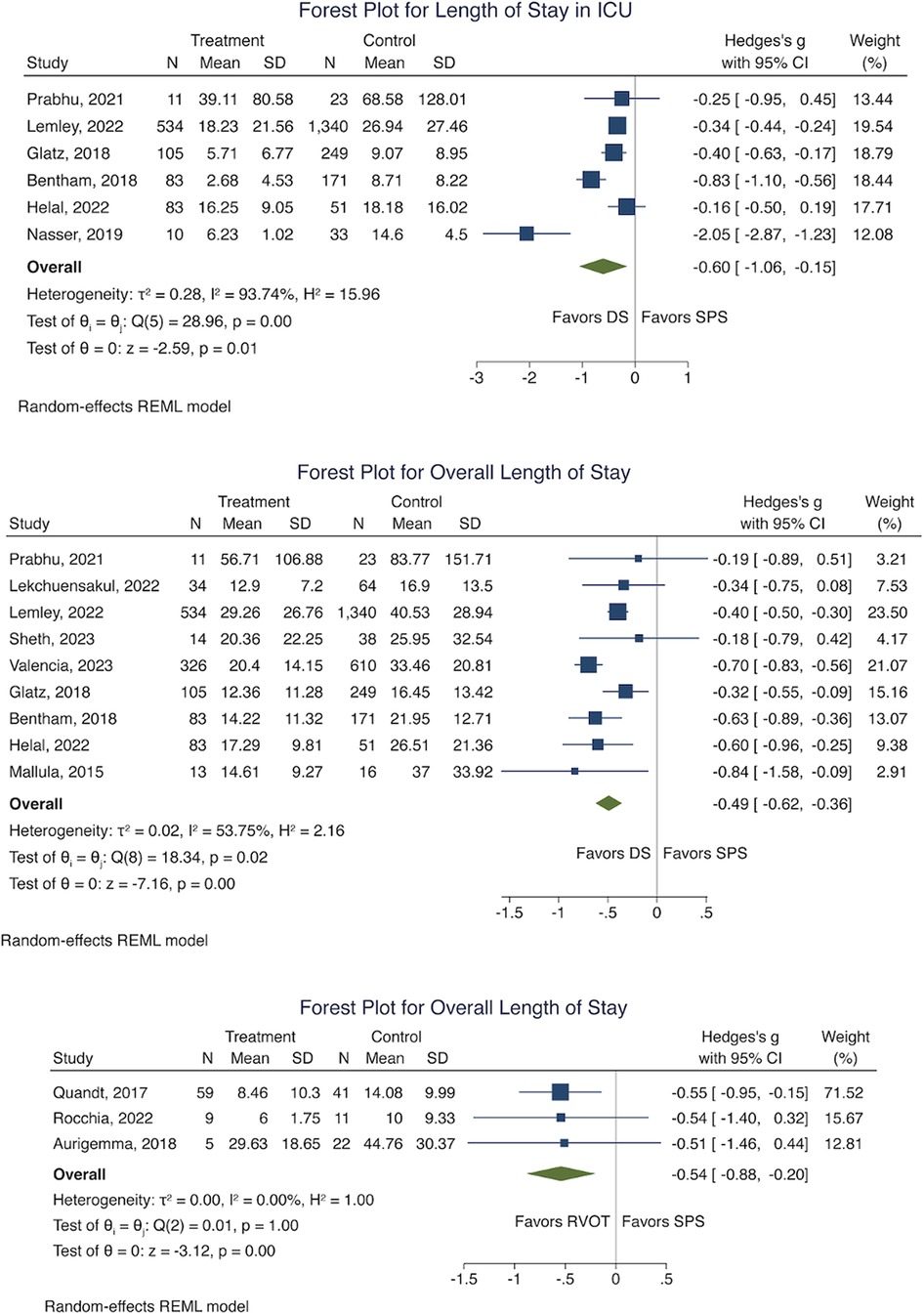
Figure 7. Forest plot for, length of stay in ICU (DS Vs SPS) and oveall length of stay (DS Vs SPS, RVOT Vs SPS). (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention; ICU: intensive care unit).
There was insufficient data to perform meta-analysis of RVOT intervention against SPS for time to second-stage surgery and length of ICU stay. Due to small sample sizes, network meta-analysis of secondary outcomes was not performed.
Funnel plots for pairwise outcomes of Early Mortality, Procedural Complications, and Early Re-intervention did not demonstrate significant asymmetry (Figure 8). These were chosen as they were deemed the most directly consequent adverse outcomes of each intervention. Funnel plots of RVOT vs. SPS was not shown as there was only a single publication with this respective direct comparison. Egger regression-based testing confirmed no statistically significant asymmetry, suggesting the absence of publication bias.
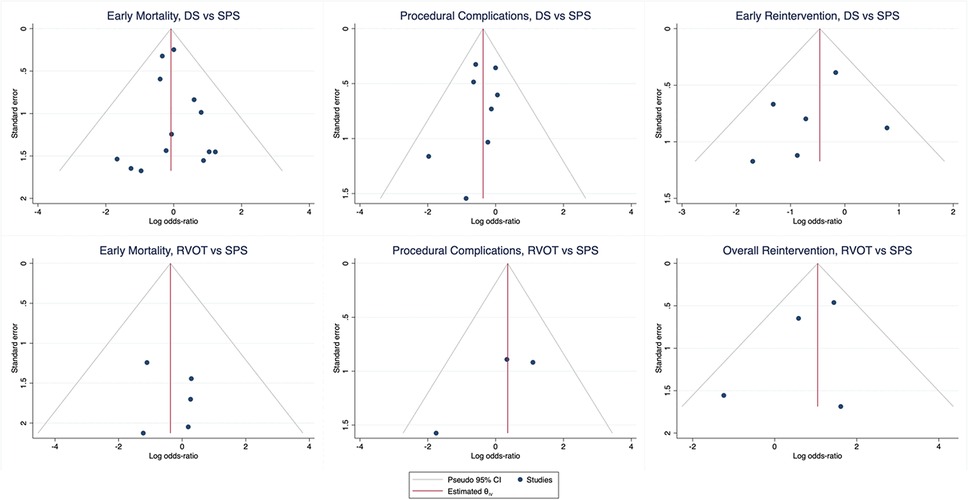
Figure 8. Funnel plots of early outcome, procedural complications, and early Re-intervention for pairwise comparison of DS vs. SPS and RVOT vs. SPS. (SPS: Surgical systemic-to-pulmonary shunt; DS: ductal stenting; RVOT: right ventricular outflow tract intervention).
4 Discussion
Since the introduction of the Blalock-Taussig-Thomas shunt as a pioneering treatment for cyanotic heart disease, there had been significant progress with the development of less-invasive transcatheter options. The growing body of literature on ductal stenting reflects increasing interest in these techniques, particularly for cases where the placement of a surgical shunt is considered risky or even unfeasible.
More recently, the emergence of RVOT stenting has garnered attention, with publications beginning to describe local experiences and outcomes. However, the paucity of large studies highlights the overall limited experience with this newer technique in a relatively rare condition. Where the obstruction is primarily in the RVOT, stenting would in theory address the issue at its root cause, restoring a more physiological pulmonary blood supply compared to ductal stenting, especially in those with difficult or unfavourable ductal anatomy. This provides flexibility in treatment and enables a tailored approach aimed at improving patient outcomes.
As cyanotic heart disease is overall uncommon, and advanced trans-catheter modalities may not be as widely available, unbiased direct comparisons are hard to come by. Our study is the first to compare these three different techniques both directly and indirectly by means of network meta-analysis, addressing the limitation of smaller sample sizes limiting conventional pairwise meta-analysis, (especially for RVOT intervention).
While pairwise comparisons showed no clear advantage of any single modality for Early or Overall Mortality, transcatheter options consistently ranked superior to surgical SPS. RVOT intervention outperformed DS in Early Mortality but not Overall Mortality. The short term outcomes may reflect nature of the procedure, whereas longer term outcomes are likely influenced by the severity and complexity of the underlying heart condition. The discrepancy between early and late outcomes of RVOT intervention may be due to delayed complications, such as re-stenosis of the RVOT over time. Moreover, RVOT stent placement may make subsequent surgical repair technically more challenging. The emergence of bioresorbable stents for RVOT intervention offers a potential solution by not leaving behind foreign material. Although the successful deployment of bioresorbable RVOT stents for paediatric Tetralogy of Fallot has been reported, this remains novel, with concerns about their radial force, resorption rate and cases of early stent failure reported in other use cases (34).
DS has demonstrated a lower rate of Procedural Complications than surgical shunt placement. In patients who underwent DS, the most commonly reported complications, excluding access-related, were stent thrombosis (19 instances in 74 patients) and stent migration (18 instances in 74 patients).
To address the risk of thrombosis, drug-eluting stents present a possible solution, especially when combined with anti-platelet therapy. Although bare-metal stents remain the standard choice for most, a few studies have reported the use of DES. While our study did not perform a direct comparison between bare-metal and drug-eluting stents, accumulating experience with DES may reveal whether they reduce rates of stent thrombosis over time. This is an area of potential interest for future research.
The most common complication in RVOT intervention was RVOT perforation. Although this complication was infrequent, its associated morbidity is high, often requiring emergency surgery or resuscitation. In at least one instance, intra-procedural death was directly attributed to RVOT perforation. Additionally, acute valvular injury has been rarely reported. In one case, the tricuspid valve was injured during stent delivery, and in another, the aortic valve was injured when the stent migrated into the aortic arch.
While the overall complication rate of RVOT intervention remains high, this may reflect the learning curve associated with a new procedure, with rates likely to improve over time. Given the potential for serious complications, it is essential to have a cardiac surgical team on standby during RVOT intervention.
While transcatheter options offer a less invasive strategy, they come with a high rate of re-intervention, primarily due to issues with stent patency. Transcatheter options fared better for Early Re-intervention rates than surgical SPS, suggesting that stent failure tended to occur in a mid-to-long-term time frame. For transcatheter re-interventions, the existing stent or shunt was often balloon dilated or re-stented. In some cases, the native pulmonary arteries were also balloon dilated or stented to improve pulmonary blood flow. The rate of surgical vs. transcatheter re-intervention varies between studies, reflecting the preferences and experience of individual centres.
Despite the promise of transcatheter options, surgical SPS still has a relevant role in the current landscape of treatment strategies. In the setting of a failed transcatheter procedure, a surgical approach would be the necessary fallback.
Our study demonstrated additional advantages of transcatheter modalities, including a shorter ICU stay and reduced overall hospitalization duration compared to surgical approaches. These findings suggest that, as less-invasive options, transcatheter techniques have the potential to match, or even surpass, traditional surgical methods in some outcomes. With further experience and technical refinement, transcatheter options could increasingly offer a viable, effective alternative to surgery for treating cyanotic congenital heart disease.
4.1 Limitations
Due to the rarity of cyanotic congenital heart disease, almost all included studies were retrospective cohorts. There were no randomised studies comparing one intervention against another, and therefore the outcomes are subject to selection bias. Among studies, there remained ambiguity in the definition of “complications”, making this outcome subject to each study's interpretation. There was also significant variability in follow-up durations, and lost-to-follow-up rates were generally unreported, introducing further biases that are difficult to address through statistical adjustments alone.
The greatest limitation is the scarcity of comparative data between RVOT intervention compared to other interventions. In published literature, only 4 studies directly compared RVOT intervention with SPS, and only 1 study performed a three-way comparison. We have attempted to mitigate this limitation in our study by use of network meta-analysis and indirect comparisons.
The patient population selected for RVOT intervention was generally older than the patients selected for DS (Table 3), which limits the comparability of outcomes between the two transcatheter intervention groups.
4.2 Conclusion
Innovative advances in interventional options for cyanotic congenital heart disease are promising, and continue to offer exciting alternatives to treatment. However, the choice of initial intervention remains highly dependent on the training and experience of each centre, as well as patient-specific factors, such as the native anatomy. Tailoring the intervention to both the institution's expertise and the unique anatomical needs of each patient is key to optimizing outcomes.
This study lends further credibility to transcatheter options as viable, safe, and attractive alternatives to traditional surgical shunts in the treatment of duct-dependent cyanotic heart disease. Our findings suggest that, with continued experience and refinement, especially in techniques like RVOT stenting, transcatheter approaches could see wider adoption and potentially lead to further improvements in patient outcomes. Expanding the use of these less-invasive methods may also help build collective expertise, paving the way for optimized care in this complex patient population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
CQZ: Investigation, Validation, Conceptualization, Visualization, Writing – review & editing, Data curation, Methodology, Writing – original draft, Formal analysis. SB: Data curation, Writing – original draft, Visualization, Investigation, Writing – review & editing, Conceptualization, Validation, Formal analysis, Methodology. CCK: Supervision, Investigation, Methodology, Validation, Writing – review & editing. SL: Supervision, Data curation, Writing – review & editing, Methodology, Validation, Formal analysis, Investigation, Visualization. QSC: Supervision, Methodology, Conceptualization, Validation, Writing – review & editing, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank Dr Dimple Rajgor for her assistance in editing, formatting, reviewing, and in submitting the manuscript for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
DS, ductal stenting; ICU, Intensive Care Unit; mBTS, Modified Blalock-Taussig-Thomas shunt; RVOT, right ventricular outflow tract; SPS, systemic-to-pulmonary shunt.
References
1. Flores-Umanzor E, Alshehri B, Keshvara R, Wilson W, Osten M, Benson L, et al. Transcatheter-based interventions for tetralogy of fallot across all age groups. JACC Cardiovasc Interv. (2024) 17:1079–90. doi: 10.1016/j.jcin.2024.02.009
2. Alsagheir A, Koziarz A, Makhdoum A, Contreras J, Alraddadi H, Abdalla T, et al. Duct stenting versus modified Blalock-Taussig shunt in neonates and infants with duct-dependent pulmonary blood flow: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. (2021) 161:379–90.e8. doi: 10.1016/j.jtcvs.2020.06.008
3. Boucek DM, Qureshi AM, Goldstein BH, Petit CJ, Glatz AC. Blalock-Taussig shunt versus patent ductus arteriosus stent as first palliation for ductal-dependent pulmonary circulation lesions: a review of the literature. Congenit Heart Dis. (2019) 14:105–9. doi: 10.1111/chd.12707
4. Fakhry AbdelMassih A, Menshawey R, Menshawey E, El-Maghraby AE, Sabry AO, Kamel A, et al. Blalock-Taussig shunt versus ductal stent in the palliation of duct dependent pulmonary circulation; A systematic review and metanalysis. Curr Probl Cardiol. (2022) 47:100885. doi: 10.1016/j.cpcardiol.2021.100885
5. Ghaderian M, Ahmadi A, Sabri MR, Behdad S, Dehghan B, Mahdavi C, et al. Clinical outcome of right ventricular outflow tract stenting versus Blalock-Taussig shunt in tetralogy of fallot: a systematic review and meta-analysis. Curr Probl Cardiol. (2021) 46:100643. doi: 10.1016/j.cpcardiol.2020.100643
6. Li D, Zhou X, Li M. Arterial duct stent versus surgical shunt for patients with duct-dependent pulmonary circulation: a meta-analysis. BMC Cardiovasc Disord. (2021) 21:9. doi: 10.1186/s12872-020-01817-2
7. Tseng SY, Truong VT, Peck D, Kandi S, Brayer S, Jason DP 3rd, et al. Patent ductus arteriosus stent versus surgical aortopulmonary shunt for initial palliation of cyanotic congenital heart disease with ductal-dependent pulmonary blood flow: a systematic review and meta-analysis. J Am Heart Assoc. (2022) 11:e024721. doi: 10.1161/JAHA.121.024721
8. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed). (2021) 74:790–9. doi: 10.1016/j.rec.2021.07.010
9. Chi KY, Li MY, Chen C, Kang E. Ten circumstancessss and solutions for finding the sample mean and standard deviation for meta-analysis. Syst Rev. (2023) 12:62. doi: 10.1186/s13643-023-02217-1
10. DECoMA Tfot. Data Estimation and Conversion for Meta-Analysis (DECoMA). Taiwan: Cochrane Taiwan. (2023). Available online at: https://taiwan.cochrane.org/resource/decoma (Accessed February 27, 2025).
11. Wells G, Shea B, O’Connell D, Robertson J, Peterson J, Welch V, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In: Ahr H, editor. Newctle.-Ott. Scale NOS Assess. Qual. Nonrandomised Stud. Meta-Anal. Canada: Ottawa Hospital. Available online at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
12. Bauser-Heaton H, Qureshi AM, Goldstein BH, Glatz AC, Ligon RA, Gartenberg A, et al. Comparison of patent ductus arteriosus stent and Blalock-Taussig shunt as palliation for neonates with sole source ductal-dependent pulmonary blood flow: results from the congenital catheterization research collaborative. Pediatr Cardiol. (2022) 43:121–31. doi: 10.1007/s00246-021-02699-7
13. Meadows JJ, Qureshi AM, Goldstein BH, Petit CJ, McCracken CE, Kelleman MS, et al. Comparison of outcomes at time of superior cavopulmonary connection between single ventricle patients with ductal-dependent pulmonary blood flow initially palliated with either Blalock-Taussig shunt or ductus arteriosus stent: results from the congenital catheterization research collaborative. Circ Cardiovasc Interv. (2019) 12:e008110. doi: 10.1161/CIRCINTERVENTIONS.119.008110
14. Al Kindi H, Al Harthi H, Atiq A, Ahlam, Shaikh S, Al Alawi K, et al. Blalock-Taussig shunt versus ductal stenting as palliation for duct-dependent pulmonary circulation. Sultan Qaboos Univ Med J. (2023) 23:10–5. doi: 10.18295/squmj.12.2023.073
15. Alhawri KA, McMahon CJ, Alrih MM, Alzein Y, Khan AA, Mohammed SK, et al. Atrioventricular septal defect and tetralogy of fallot - A single tertiary center experience: a retrospective review. Ann Pediatr Cardiol. (2019) 12(2):103–9. doi: 10.4103/apc.APC_87_18
16. Amoozgar H, Cheriki S, Borzoee M, Ajami G, Soltani M, Ahmadipour M, et al. Short-term result of ductus arteriosus stent implantation compared with surgically created shunts. Pediatr Cardiol. (2012) 33:1288–94. doi: 10.1007/s00246-012-0304-x
17. Aurigemma D, Moore JW, Vaughn G, Moiduddin N, El-Said HG. Perforation and right ventricular outflow tract stenting: alternative palliation for infants with pulmonary atresia/ventricular septal defect. Congenit Heart Dis. (2018) 13(2):226–31. doi: 10.1111/chd.12552
18. Bentham JR, Zava NK, Harrison WJ, Shauq A, Kalantre A, Derrick G, et al. Duct stenting versus modified Blalock-Taussig shunt in neonates with duct-dependent pulmonary blood flow: associations with clinical outcomes in a multicenter national study. Circulation. (2018) 137:581–8. doi: 10.1161/CIRCULATIONAHA.117.028972
19. Glatz AC, Petit CJ, Goldstein BH, Kelleman MS, McCracken CE, McDonnell A, et al. Comparison between patent ductus arteriosus stent and modified Blalock-Taussig shunt as palliation for infants with ductal-dependent pulmonary blood flow: insights from the congenital catheterization research collaborative. Circulation. (2018) 137:589–601. doi: 10.1161/CIRCULATIONAHA.117.029987
20. Helal AM, Elmahrouk AF, Bekheet S, Barnawi HI, Jamjoom AA, Galal MO, et al. Patent ductus arteriosus stenting versus modified Blalock-Taussig shunt for palliation of duct-dependent pulmonary blood flow lesions. J Card Surg. (2022) 37:2571–80. doi: 10.1111/jocs.16692
21. Ho AB, Perry T, Hribernik I, Thomson JD, Bentham JR. Surgical versus transcatheter palliation for insufficient pulmonary blood supply in infants with cyanotic CHD. Cardiol Young. (2022) 32:42–7. doi: 10.1017/S1047951121001505
22. Lekchuensakul S, Somanandana R, Namchaisiri J, Benjacholamas V, Lertsapcharoen P. Outcomes of duct stenting and modified Blalock-Taussig shunt in cyanotic congenital heart disease with duct-dependent pulmonary circulation. Heart Vessels. (2022) 37:875–83. doi: 10.1007/s00380-021-01978-w
23. Lemley BA, Wu L, Roberts AL, Shinohara RT, Quarshie WO, Qureshi AM, et al. Trends in ductus arteriosus stent versus Blalock-Taussig-Thomas shunt use and comparison of cost, length of stay, and short-term outcomes in neonates with ductal-dependent pulmonary blood flow: an observational study using the pediatric health information systems database. J Am Heart Assoc. (2023) 12:e030575. doi: 10.1161/JAHA.123.030575
24. Mallula K, Vaughn G, El-Said H, Lamberti JJ, Moore JW. Comparison of ductal stenting versus surgical shunts for palliation of patients with pulmonary atresia and intact ventricular septum. Catheter Cardiovasc Interv. (2015) 85(7):1196–202. doi: 10.1002/ccd.25870
25. McMullan DM, Permut LC, Jones TK, Johnston TA, Rubio AE. Modified Blalock-Taussig shunt versus ductal stenting for palliation of cardiac lesions with inadequate pulmonary blood flow. J Thorac Cardiovasc Surg. (2014) 147:397–403. doi: 10.1016/j.jtcvs.2013.07.052
26. Nasser BA, Abdulrahman M, Qwaee AAL, Alakfash A, Mohamad T, Kabbani MS. Impact of stent of ductus arteriosus and modified Blalock-Taussig shunt on pulmonary arteries growth and second-stage surgery in infants with ductus-dependent pulmonary circulation. J Saudi Heart Assoc. (2020) 32:86–92. doi: 10.37616/2212-5043.1014
27. Prabhu NK, Zhu A, Meza JM, Hill KD, Fleming GA, Chamberlain RC, et al. Transition to ductal stenting for single ventricle patients led to improved survival: an institutional case series. World J Pediatr Congenit Heart Surg. (2021) 12:518–26. doi: 10.1177/21501351211007808
28. Quandt D, Ramchandani B, Penford G, Stickley J, Bhole V, Mehta C, et al. Right ventricular outflow tract stent versus BT shunt palliation in tetralogy of fallot. Heart. (2017) 103:1985–91. doi: 10.1136/heartjnl-2016-310620
29. Ratnayaka K, Nageotte SJ, Moore JW, Guyon PW, Bhandari K, Weber RL, et al. Patent ductus arteriosus stenting for all ductal-dependent cyanotic infants: waning use of Blalock-Taussig shunts. Circ Cardiovasc Interv. (2021) 14:e009520. doi: 10.1161/CIRCINTERVENTIONS.120.009520
30. Rocchia F, Allub A, Guevara A, Anquín L, Juaneda I, Contreras A, et al. Comparación de resultados inmediatos y a mediano plazo de la anastomosis de Blalock-Taussig versus la colocación de stent en tracto de salida de ventrículo derecho en neonatos sintomáticos con tetralogía de fallot. Rev Argent Cardiol. (2023) 90:25–30. doi: 10.7775/rac.es.v90.i1.20474
31. Santoro G, Capozzi G, Caianiello G, Palladino MT, Marrone C, Farina G, et al. Pulmonary artery growth after palliation of congenital heart disease with duct-dependent pulmonary circulation: arterial duct stenting versus surgical shunt. J Am Coll Cardiol. (2009) 54:2180–6. doi: 10.1016/j.jacc.2009.07.043
32. Sheth SP, Loomba RS. Haemodynamic and clinical variables after surgical systemic to pulmonary artery shunt placement versus arterial ductal stenting. Cardiol Young. (2023) 33(10):2060–5. doi: 10.1017/S104795112200395X
33. Valencia E, Staffa SJ, Kuntz MT, Zaleski KL, Kaza AK, Maschietto N, et al. Transcatheter ductal stents versus surgical systemic-pulmonary artery shunts in neonates with congenital heart disease with ductal-dependent pulmonary blood flow: trends and associated outcomes from the pediatric health information system database. J Am Heart Assoc. (2023) 12:e030528. doi: 10.1161/JAHA.123.030528
Keywords: congenital, paediatric, cyanotic, shunt, stent, transcatheter
Citation: Chee QZ, Buvaneswarran S, Chen CK, Shen L and Quek SC (2025) Systematic review and network meta-analysis of outcomes of transcatheter strategies and surgical shunts for treatment of duct-dependent cyanotic congenital heart disease. Front. Cardiovasc. Med. 12:1594779. doi: 10.3389/fcvm.2025.1594779
Received: 17 March 2025; Accepted: 8 August 2025;
Published: 2 September 2025.
Edited by:
Nazmi Narin, Izmir Katip Celebi University, TürkiyeReviewed by:
Raymond N. Haddad, Hôpital Universitaire Necker-Enfants Malades, Assistance Publique-Hôpitaux de Paris (AP-HP), FranceTommaso Generali, Alder Hey Children’s Hospital, United Kingdom
Copyright: © 2025 Chee, Buvaneswarran, Chen, Shen and Quek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiao Zhi Chee, cWlhb196aGlfY2hlZUBudWhzLmVkdS5zZw==; Santosi Buvaneswarran, c2FudG9zaV9idXZhbmVzd2FycmFuQG51aHMuZWR1LnNn
†These authors have contributed equally to this work and share first authorship
 Qiao Zhi Chee
Qiao Zhi Chee Santosi Buvaneswarran
Santosi Buvaneswarran Ching Kit Chen
Ching Kit Chen Liang Shen
Liang Shen Swee Chye Quek1,3
Swee Chye Quek1,3