Abstract
Background:
We aimed to analyze the impact of socioeconomic status (SES) on management and in-hospital outcomes of patients with cardiogenic shock (CS).
Methods:
This was a prospective observational registry conducted (December 2018–November 2019) in Intensive Cardiac Care Units (ICCU) across 8 tertiary care centers. Consecutive patients aged ≥18 years with a primary diagnosis of cardiogenic shock were included. SES was defined using a numerical index that incorporates mean income levels, premature mortality, and avoidable hospitalizations observed within a specific health area. SES values were categorized into tertiles. In-hospital procedures, complications, length of stay, and in-hospital mortality were collected.
Results:
A total of 382 patients were included (mean age: 65.3 years). There were no differences in age, sex, or major comorbidities across SES groups. CS was more frequently due to acute coronary syndrome (ACS) in patients with low SES (66.9% vs. 58%, p = 0.022). No significant differences were observed regarding SCAI stage or other severity markers of CS across SES groups. Patients with low SES were more likely to receive pulmonary artery catheterization (p = 0.029) and mechanical circulatory support (p = 0.038). After adjusting for potential confounders, clinical management was similar regardless SES. Lower SES patients exhibited a higher incidence of bleeding (p = 0.018). There were no differences in length of stay or in-hospital mortality among SES groups.
Conclusions:
Beyond a higher rate of ACS-related CS, patients with low SES exhibited a clinical profile and shock severity comparable to other SES groups. Therapeutic management aligned with guideline recommendations even in patients with low SES.
Introduction
Cardiogenic shock (CS) is associated with high morbidity and mortality rates and significant healthcare resource utilization (1, 2). One of the key recommendations in clinical practice guidelines is to transfer patients to centers with full availability of interventional cardiology and mechanical circulatory support (MCS), advocating for the organization of care through regional networks that integrate centers of varying complexity (3). Moreover, an association has been described between lower socioeconomic status (SES), differences in therapeutic management, and worse outcomes in patients with cardiovascular disease (4–7). However, data on the impact of SES in CS remain scarce. Most available information originates from administrative databases (8–11), which lack critical clinical variables. Furthermore, most published studies come from countries with healthcare systems significantly different from the free and universal Healthcare Spanish system. Therefore, the primary objective of this study was to assess the impact of SES on clinical management and in-hospital outcomes in a cohort of consecutive patients with CS admitted to Intensive Cardiac Care Units (ICCU).
Methods
Study population
The Shock-CAT registry is a prospective observational study performed between December 2018 and November 2019 in the ICCU of eight Spanish university hospitals (12). All participating centers had dedicated ICCU staffed by personnel with specialized training in the management of critically ill cardiac patients. Additionally, all centers had full access to interventional cardiology laboratories, and most of hospitals (75%) had on-site cardiac surgery and advanced MCS availability. The study included consecutive patients aged ≥18 years with a primary diagnosis of CS due to various etiologies.
CS was defined as a systolic blood pressure <90 mmHg (after adequate volume resuscitation) for at least 30 min or the need for vasopressor therapy to maintain a systolic blood pressure >90 mmHg, along with signs of hypoperfusion (altered mental status/confusion, peripheral coldness, oliguria, or lactate >2 mmol/L), in accordance with the classical definition of CS (13). Patients with postcardiotomy CS or those in whom CS was related to non-cardiac surgery were excluded. The underlying cause of CS was determined locally by investigators based on the primary admission diagnosis. CS management was performed according to current guideline recommendations (3) and at the discretion of the treating medical team.
Data collection and definitions
Data were prospectively collected by local investigators using standardized case report forms. Collected variables included demographic data, baseline clinical characteristics, echocardiographic and angiographic findings, laboratory results, the need for invasive procedures during hospitalization, and the occurrence of in-hospital complications (bleeding, infections, arrhythmic and mechanical complications, severe brain damage, and in-hospital mortality). Advanced mechanical circulatory support (aMCS) was defined as the use of venoarterial ECMO, Levitronix Centrimag® or Impella® devices. MCS included both aMCS and the use of intraaortic balloon pump. Hospitalization events were assigned through a review of electronic medical records. The Cardshock score was calculated for each patient (14). CS severity was evaluated using the SCAI classification (15), with SCAI stages D and E categorized as profound shock. SES was defined using a numeric index developed by the Agència de Qualitat i Avaluació Sanitàries de Catalunya (AQuAS) (16). This index ranges from 0 to 100 and is collectively assigned to the entire population from a specific healthcare area (Àrea Bàsica de Salut). It incorporates factors such as average annual individual income, premature mortality, and avoidable hospitalizations within each healthcare area. Higher index values correspond to lower SES. For the purpose of this study SES values were categorized into tertiles (high SES: <39; medium SES 39–52, low SES >52). Despite its use has not been valitaded among patients with CS, this score has been associated with other healthcare indicators at an ecological level (17).
Ethical considerations
Confidential patient information was protected in accordance with national legislation. This study was approved by the corresponding Institutional Ethics Committee. All study procedures were conducted in compliance with the ethical standards outlined in the Declaration of Helsinki. All patients provided written informed consent for the use of their clinical data for research purposes. In cases where patients were comatose or unable to provide consent, consent was obtained from their relatives.
Statistical analysis
Results are presented as absolute numbers (n) and percentages (%). Categorical variables are expressed as frequencies and percentages, while continuous variables are reported as median and interquartile range (p25–p75). Comparisons of clinical characteristics, treatment variables, and prognostic outcomes across SES groups were performed using the χ2 test for categorical variables and analysis of variance (ANOVA) for continuous variables, including a test for linear trend.
The potential association between SES and in-hospital management was also assessed by multivariate analysis. Binary logistic regression models were performed considering main in-hospital procedures [MCS, angiography, percutaneous coronary intervention (PCI), therapeutic hypothermia, invasive mechanical ventilation, pulmonary artery catheter, respectively] as dependent variables, SES as a fixed independent variable and the rest of potential confounders (variables with an association p < 0.2 both with SES and in-hospital procedures) as independent variables. The association between SES and mortality was assessed by the same method. A two-tailed p value <0.05 was considered statistically significant. Statistical analyses were conducted using IBM SPSS Statistics 21 (Chicago, Illinois, USA).
Results
A total of 382 patients were included, with a mean age of 65.3 years (SD 14). The majority of cases were male (287/382, 75.1%). The most frequent cause of CS was acute coronary syndrome (ACS) (232/382, 60.7%). Profound CS was observed in 139/382 patients (36.4%), and 133 cases (34.8%) experienced cardiac arrest during hospitalization.
No significant differences were observed regarding age or gender across SES groups. The proportion of major comorbidities was similar across the different SES groups (Figure 1). The cause of CS was ACS more frequently in patients with low SES as compared to the rest (66.9% vs. 58%, p = 0.022). The severity of CS was similar across SES groups. While systolic blood pressure was slightly lower among patients from the high SES group, no significant differences were observed in other markers of CS severity such as cardiac arrest, renal function, lactate levels, left ventricular ejection fraction, or Cardshock score values (Table 1).
Figure 1
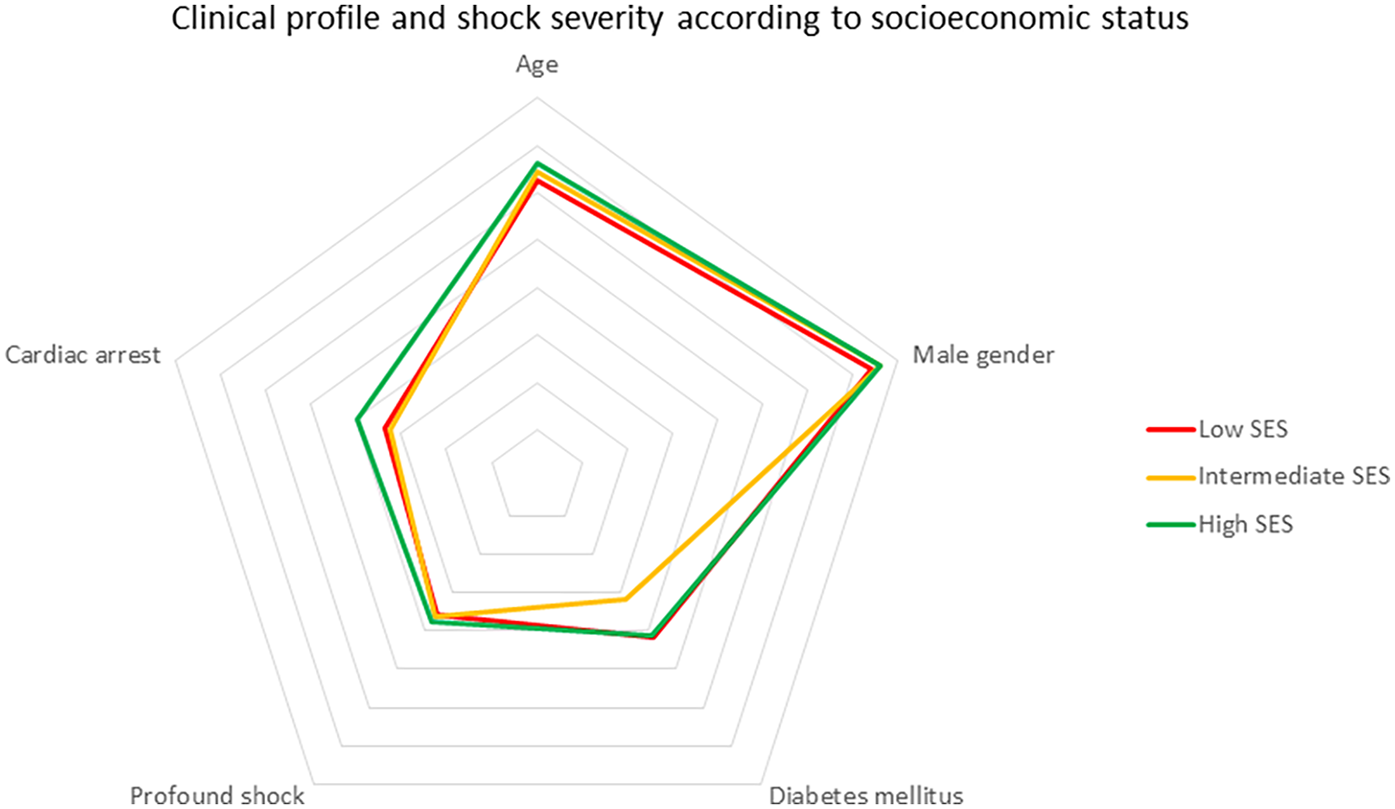
Clinical profile and shock severity according to socioeconomic status.
Table 1
| Clinical Characteristics | Low SES (n =125) | Intermediate SES (n=130) | High SES (n=127) | p-value |
|---|---|---|---|---|
| Age (years, mean, SD) | 64.4 (16.0) | 64.7 (13.0) | 66.7 (13.0) | 0.277 |
| Male sex (n, %) | 96 (74.2) | 99 (76.0) | 92 (76.0) | 0.915 |
| Arterial hypertension (n, %) | 79 (63.7) | 77 (59.2) | 85 (67.5) | 0.535 |
| Dyslipidemia (n, %) | 80 (64.5) | 65 (50.0) | 79 (62.7) | 0.780 |
| Active smoking (n, %) | 39 (31.2) | 48 (36.9) | 34 (26.8) | 0.448 |
| Diabetes mellitus (n, %) | 51 (41.1) | 41 (31.8) | 52 (41.3) | 0.975 |
| Peripheral artery disease (n, %) | 14 (11.4) | 16 (12.4) | 16 (12.6) | 0.770 |
| Previous stroke (n, %) | 16 (12.9) | 7 (5.4) | 14 (11.0) | 0.626 |
| Chronic obstructive pulmonary disease (COPD) (n, %) | 18 (14.5) | 15 (11.5) | 16 (12.8) | 0.688 |
| Chronic kidney disease (n, %) | 14 (11.5) | 17 (13.1) | 15 (11.8) | 0.939 |
| Previous neoplasia (n, %) | 10 (8.1) | 15 (11.5) | 15 (11.9) | 0.335 |
| Cause of Shock | 0.022 | |||
| Acute coronary syndrome (n, %) | 83 (66.9) | 77 (59.2) | 72 (56.7) | |
| Decompensated chronic heart failure (n, %) | 20 (16.0) | 19 (14.6) | 15 (11.8) | |
| Electrical storm (n, %) | 8 (6.5) | 9 (6.9) | 16 (12.6) | |
| Valvular heart disease (n, %) | 1 (0.8) | 8 (6.2) | 3 (2.4) | |
| Myocarditis (n, %) | 4 (3.2) | 4 (3.1) | 3 (2.4) | |
| Others (n, %) | 8 (6.5) | 13 (10.0) | 18 (14.2) | |
| SCAI Shock Classification at Admission | 0.743 | |||
| A (n, %) | 0 | 1 (0.8) | 0 | |
| B (n, %) | 20 (16.0) | 15 (11.5) | 18 (14.2) | |
| C (n, %) | 60 (48.0) | 67 (51.5) | 62 (48.8) | |
| D (n, %) | 23 (18.4) | 25 (19.2) | 33 (26.0) | |
| E (n, %) | 22 (17.6) | 22 (16.9) | 14 (11.0) | |
| Cardiac arrest (n, %) | 41 (33.1) | 42 (32.6) | 50 (39.7) | 0.272 |
| Systolic blood pressure (mmHg) | 92 (23) | 95 (30) | 85 (24) | 0.011 |
| Heart rate (bpm) | 93 (29) | 95 (29) | 93 (34) | 0.822 |
| Glomerular filtration rate (mL/min/1.73 m²) | 64 (34) | 63 (29) | 54 (25) | 0.231 |
| Cardshock score | 4.2 (2) | 4.1 (2) | 4.6 (2) | 0.106 |
| Left ventricular ejection fraction (%) | 31 (13) | 33 (15) | 32 (13) | 0.489 |
| Glucose at admission (mg/dL) | 199 (82) | 201 (106) | 231 (166) | 0.096 |
| Hemoglobin (g/dL) | 12.5 (2) | 12.7 (2) | 13.2 (2) | 0.039 |
| Lactate at admission (mmol/L) | 5.9 (5) | 5.5 (5) | 5.5 (5) | 0.789 |
Baseline clinical characteristics based on socioeconomic status (SES).
Management and outcomes according to SES subgroups
The crude analysis showed significant differences in the therapeutic approach among the different SES groups (Figure 2). Patients with low and intermediate SES underwent pulmonary artery catheterization, percutaneous coronary intervention (PCI), and MCS more frequently during hospitalization compared to the high SES group (Table 2). However, after adjusting for potential confounders, only a slight (non-significant) higher proportion of pulmonary artery catheter use was observed among patients from the low and intermediate SES groups (Supplementary Table S1c). No differences were observed regarding the rest of in-hospital procedures according to SES (Supplementary Tables S1a–f).
Figure 2
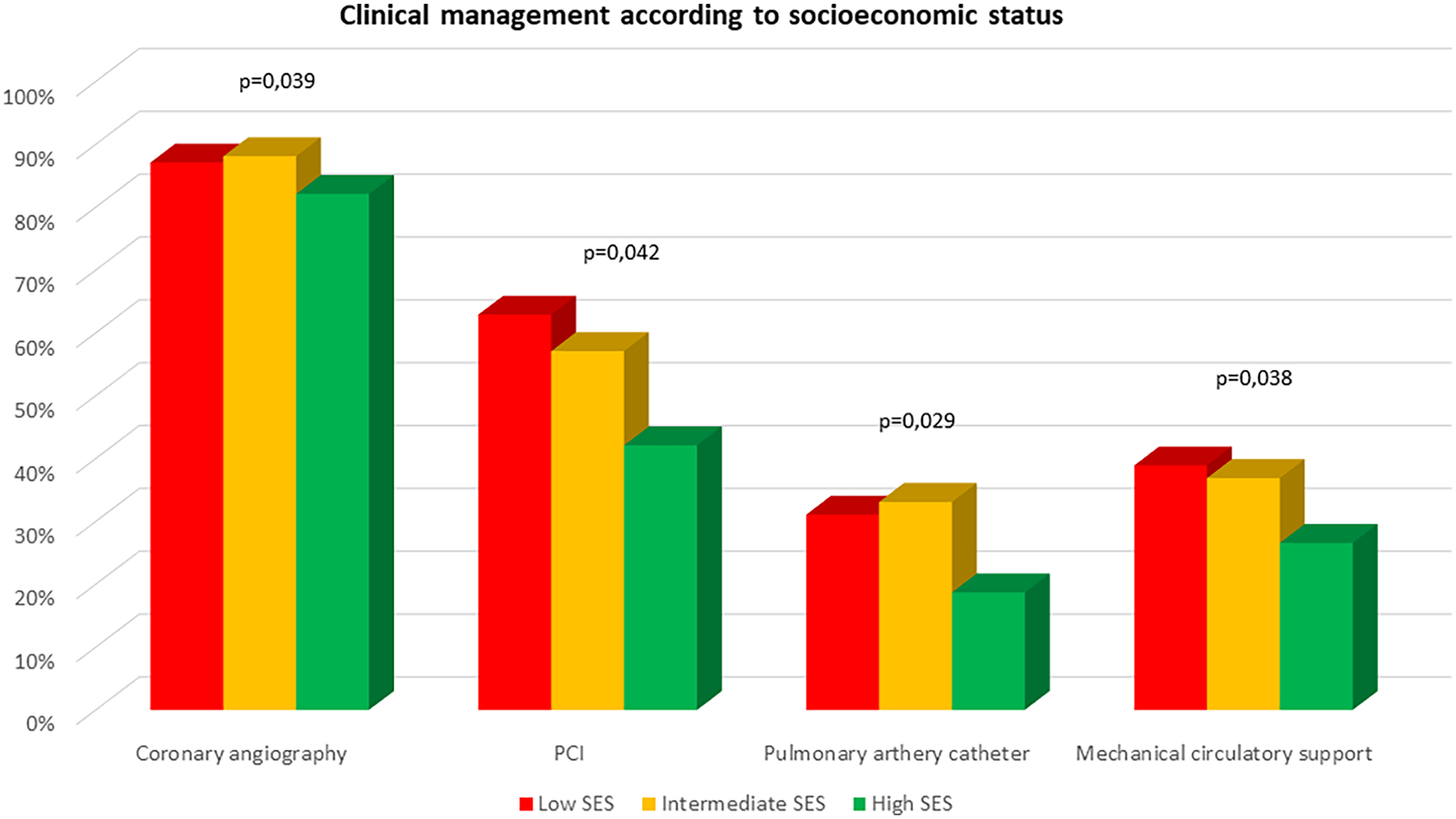
Clinical management according to socioeconomic status.
Table 2
| Therapeutic approach | Low SES (n = 125) | Intermediate SES (n = 130) | High SES (n = 127) | p-value |
|---|---|---|---|---|
| Pulmonary artery catheter (n, %) | 38 (31.1) | 42 (33.1) | 23 (18.7) | 0.029 |
| Coronary angiography (n, %) | 108 (86.4) | 111 (85.4) | 101 (79.5) | 0.139 |
| Percutaneous coronary intervention (n, %) | 78 (62.4) | 72 (55.4) | 60 (47.2) | 0.016 |
| Invasive mechanical ventilation (n, %) | 78 (62.4) | 82 (63.1) | 81 (63.8) | 0.772 |
| Mechanical circulatory support (n, %) | 49 (39.2) | 48 (36.9) | 34 (26.8) | 0.038 |
| Advanced circulatory support (n, %) | 22 (17.6) | 18 (13.8) | 14 (11.0) | 0.135 |
| Extracorporeal renal replacement therapy (n, %) | 21 (16.9) | 10 (7.9) | 20 (16.3) | 0.873 |
| Therapeutic hypothermia (n, %) | 24 (19.4) | 10 (15.5) | 30 (24.2) | 0.338 |
| In-hospital Evolution | ||||
| Bleeding events (n, %) | 36 (28.8) | 29 (22.3) | 20 (15.7) | 0.018 |
| Infectious complications (n, %) | 67 (53.6) | 58 (44.6) | 69 (54.3) | 0.647 |
| Delirium (n, %) | 27 (21.6) | 19 (14.6) | 22 (17.3) | 0.379 |
| In-hospital mortality (n, %) | 49 (39.2) | 34 (26.2) | 40 (31.5) | 0.194 |
| ICU stay (mean, SD) | 14 (13.0) | 13 (12.0) | 15 (15.0) | 0.369 |
| Hospital length of stay (mean, SD) | 22 (21.0) | 22 (22.0) | 23 (22.0) | 0.687 |
Therapeutic approach and in-hospital outcomes according to socioeconomic status (SES).
Patients in the lower SES groups experienced bleeding events more frequently during hospitalization (Table 2). No differences were observed in the incidence of delirium or infectious complications. Hospital length of stay and ICCU length of stay were similar across the three SES groups. Although mortality was slightly higher in the low SES group, this difference did not reach statistical significance. After adjusting for potential confounders, no association was observed between SES and mortality (Supplementary Table S2). Independent predictors of mortality included age, chronic kidney disease, severity of CS as measured by the SCAI class definition and cardiac arrest.
Impact of socioeconomic status on therapeutic management and prognosis by sex and age
Supplementary Table S3 shows clinical profile, management and outcomes according to gender. Overall, women exhibited lower utilization rates of pulmonary artery catheter (17.9% vs. 29.3%, p = 0.029) and aMCS (6.3% vs. 16.4%, p = 0.015).
The impact of SES on clinical management varied slightly by gender. Among men, a higher proportion of patients in the low and intermediate SES groups received pulmonary artery catheterization (Supplementary Table S4). Additionally, a slightly higher use of PCI and MCS was observed in these patients, although this difference was statistically non-significant. Among women, the only significant difference was a higher utilization of aMCS in those from low and intermediate SES groups, with no significant differences in pulmonary artery catheter use or other invasive procedures (Supplementary Table S5). Regarding clinical outcomes, men from low and intermediate SES groups exhibited a higher incidence of bleeding complications, along with slightly increased mortality in these groups, without being statistically significant. In women, the only significant difference was a higher incidence of infectious complications in the high SES group. Hospital and ICCU length of stay did not significantly differ by SES in either men or women.
In general, older patients received pulmonary artery catheterization (19.3% vs. 37.4%, p < 0.001), MCS (28.7% vs. 40.8%, p = 0.013), and aMCS (6.9% vs. 22.3%, p < 0.001) less frequently. Once again, the impact of SES on treatment and prognosis was slightly different depending on age. Among younger patients, a slight non-significant higher use of pulmonary artery catheterization and MCS was observed in the low and intermediate SES groups (Supplementary Table S6). In contrast, among older patients, only a higher indication for PCI was noted in the low SES group (Supplementary Table S4). Younger patients from lower SES groups exhibited a significantly higher incidence of bleeding complications. However, these differences were not statistically significant in older patients. The incidence of other complications and in-hospital mortality was similar across SES groups both in younger and older patients. Finally, both ICCU and overall hospital length of stay were comparable across SES groups in younger patients. In contrast, among older patients, those in the higher SES group had a slightly shorter length of stay (both in the ICCU and overall hospitalization), although this difference did not reach statistical significance (Supplementary Table S7).
Discussion
The main findings of this study are: (a) Patients with low SES admitted for CS in ICCU exhibited a similar clinical profile, comorbidity burden, and CS severity compared to other SES groups; (b) CS was more frequently caused by ACS in patients with low SES; (c) Clinical management adhered to guideline recommendations across SES groups; (d) Despite a higher incidence of bleeding in low SES patients, overall complication rates, in-hospital mortality, and length of stay were similar across SES groups.
Low SES has been associated with a higher comorbidity burden, lower adherence to guideline-directed therapy, and increased adverse event rates and mortality in various cardiovascular conditions, including chronic heart failure (6, 18), aortic stenosis (5), resuscitated sudden cardiac arrest (7), and coronary artery disease (4, 19). In ST-segment elevation myocardial infarction (STEMI), low SES is linked to worse clinical profiles and prolonged reperfusion times (20).
Data on the impact of SES on CS are scarce. Vallabhajosyula et al. (8) analyzed 402,182 patients with ACS-related CS in the United States (2000–2016), comparing uninsured patients to those with private insurance. Uninsured patients were younger, predominantly male, had lower SES, fewer comorbidities, and a higher incidence of multiorgan failure. Moreover, they were less likely to undergo coronary angiography, PCI, or MCS and had higher in-hospital mortality. Bloom et al. (9) examined 2,628 patients with CS transported by emergency medical services in Australia, reporting a progressive increase in CS incidence from the lowest to the highest SES quintile. Low SES patients were less likely to present to metropolitan hospitals and were more frequently treated at non-revascularization centers. These patients underwent fewer coronary angiographies and had higher 30-day mortality. The authors emphasized the need for equitable care in CS management regardless of SES. Similarly, Patlolla et al. (10) found that patients from lower-income areas (based on median district-level income) underwent fewer early coronary angiographies, PCI, MCS, and pulmonary artery catheterization and exhibited higher in-hospital mortality in a large cohort (n = 409,294) of patients with ACS-related CS. Other studies have also reported an association between low SES, reduced MCS utilization, and increased in-hospital mortality in this setting (11, 21). Notably, most data on the relationship between SES, treatment, and outcomes in CS derive from administrative databases, which often lack key clinical predictors. Furthermore, no data are available on the impact of SES on CS outcomes in Spain. This is a key aspect, since the public and universal nature of the healthcare system in this setting makes equity in the treatment of these highly complex patients a priority objective.
This is the first clinical registry to examine the association between SES, therapeutic approach, and prognosis in CS patients treated in routine clinical practice. The study design allowed for the analysis of key prognostic predictors (SCAI classification, lactate levels, heart rate, renal function), which are unavailable in most prior studies. In our cohort, SES was not associated with significant differences in clinical presentation or CS severity. Interestingly, a higher rate of ACS-related CS was observed among low SES patients, which may be closely related to the higher rate of PCI, other in-hospital procedures (MCS, pulmonary artery catheter) and in-hospital bleeding in this group. After adjusting for confounders, both management and outcomes were similar across SES subgroups These findings suggest a reasonably equitable approach to CS management in ICCU in our healthcare system, regardless of SES.
The analysis of the association between SES, therapeutic approach, and prognosis based on gender is particularly relevant, as significant interactions have been described between gender, the burden of cardiovascular risk factors, and patient outcomes (22). Data on the potential association between gender and SES in patients with CS are conflicting (8, 10). A different clinical profile and therapeutic approach have been described in women with CS, who tend to be older and present a higher burden of comorbidities. In a study by Sambola et al. (23), women with CS were less frequently referred to tertiary centers and had higher adjusted mortality compared to men. It has been suggested that women with acute heart failure often receive less optimized pharmacological treatment and fewer invasive procedures during hospitalization (24). Similarly, data from our series show that the use of pulmonary artery catheterization and aMCS was lower in women. Unlike other series, no differences in SES levels were observed between women and men in our study. On the other hand, some differences were noted in the impact of SES on the therapeutic approach based on gender, with greater use of aMCS in the lower SES groups among women. These findings should be interpreted with caution due to the size of the subgroups and require validation in larger cohorts. Given their potential relevance, the possible interactions between SES and gender in CS patients warrant further specific studies.
The interaction between SES and age is another important point, considering the ongoing population aging and the elevated risk faced by elderly patients. Older patients with CS receive MCS less frequently and are less likely to receive other recommended treatments, resulting in higher mortality (25). Additionally, a higher proportion of younger patients has been described in low SES groups (8, 10). Unlike these studies, data from our series did not show a significant association between age and SES. Older patients in this series received a more conservative approach, with less frequent use of pulmonary artery catheterization and MCS. The impact of SES on the therapeutic approach varied slightly by age, with a non-significant trend toward greater use of MCS in the low SES group only among younger patients. Again, the fragmentation of the sample limits the ability to draw robust conclusions from these data.
This study has several limitations. Its observational nature precludes the exclusion of residual confounding. Sample size was moderate, so these findings should be validated in larger cohorts. The inclusion of only ICCU-admitted patients may introduce selection bias, as the likelihood of ICCU admission may vary by SES (26). Data about excluded patients (postcardiotomy CS or those in whom CS was related to non-cardiac surgery) were not available. The SES index was assigned collectively to the entire population within each healthcare area, rather than on an individual basis, which may lead to an ecological bias. In addition, this SES score has not been previously validated in patients with CS. Therefore, this study was planned as a pilot study.
Despite these limitations, this study provides novel and relevant insights into the impact of SES on therapeutic strategies and prognosis in patients with CS managed in routine clinical practice within our healthcare system. In our view, the findings suggest a reasonably equitable approach to CS management, regardless of SES. Nevertheless, larger-scale studies are warranted to further optimize care strategies in this setting.
In conclusion, patients with low SES admitted to the ICCU for CS exhibit a similar clinical profile, comorbidity burden, and severity of CS compared to other patients. ACS was a more frequent etiology of CS in the low-SES group. Adherence to guideline-recommended therapy was observed across all SES groups. SES was not associated with significant differences in therapeutic management or prognosis in patients with CS admitted to the ICCU within routine clinical practice in our setting.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Hospital Universitari Germans Trias i Pujol, Badalona, Barcelona, Spain. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MM-M: Data curation, Methodology, Writing – review & editing. TL-S: Software, Supervision, Validation, Writing – review & editing. AA-S: Conceptualization, Writing – original draft. FR-S: Supervision, Validation, Writing – review & editing. ES-G: Supervision, Validation, Writing – review & editing. JA: Supervision, Validation, Writing – review & editing. PP: Supervision, Validation, Writing – review & editing. IB: Supervision, Validation, Writing – review & editing. AS: Supervision, Validation, Writing – review & editing. RA: Supervision, Validation, Writing – review & editing. JR-L: Supervision, Validation, Writing – review & editing. CT: Supervision, Validation, Writing – review & editing. JB: Supervision, Validation, Writing – review & editing. IL: Validation, Writing – review & editing, Writing – original draft. JS-S: Validation, Writing – review & editing. CG-G: Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We thank CERCA Programme/Generalitat de Catalunya for institutional support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Correction Note
A correction has been made to this article. Details can be found at: 10.3389/fcvm.2025.1708500.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1597225/full#supplementary-material
References
1.
Osman M Syed M Patibandla S Sulaiman S Kheiri B Shah MK et al Fifteen-year trends in incidence of cardiogenic shock hospitalization and in-hospital mortality in the United States. J Am Heart Assoc. (2021) 10(15):e021061. 10.1161/JAHA.121.021061
2.
Collado E Luiso D Ariza-Solé A Lorente V Sánchez-Salado JC Moreno R et al Hospitalization-related economic impact of patients with cardiogenic shock in a high-complexity reference centre. Eur Heart J Acute Cardiovasc Care. (2021) 10(1):50–3. 10.1093/ehjacc/zuaa003
3.
McDonagh TA Metra M Adamo M Gardner RS Baumbach A Böhm M et al 2023 Focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. (2023) 44(37):3627–39. 10.1093/eurheartj/ehad195
4.
Topel ML Kim JH Mujahid MS Sullivan SM Ko YA Vaccarino V et al Neighborhood socioeconomic status and adverse outcomes in patients with cardiovascular disease. Am J Cardiol. (2019) 123(2):284–90. 10.1016/j.amjcard.2018.10.011
5.
von Kappelgaard L Gislason G Davidsen M Zwisler AD Juel K . Temporal trends and socioeconomic differences in treatment and mortality following a diagnosis of aortic stenosis. Int J Cardiol. (2021) 336:87–92. 10.1016/j.ijcard.2021.05.039
6.
Hawkins NM Jhund PS McMurray JJV Capewell S . Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. (2012) 14(2):138–46. 10.1093/eurjhf/hfr168
7.
Mehta NK Allam S Mazimba S Karim S . Racial, ethnic, and socioeconomic disparities in out-of-hospital cardiac arrest within the United States: now is the time for change. Heart Rhythm O2. (2022) 3(6 Part B):857–63. 10.1016/j.hroo.2022.07.009
8.
Vallabhajosyula S Kumar V Sundaragiri PR Cheungpasitporn W Miller PE Patlolla SH et al Management and outcomes of acute myocardial infarction-cardiogenic shock in uninsured compared with privately insured individuals. Circ Heart Fail. (2022) 15(5):e008991. 10.1161/CIRCHEARTFAILURE.121.008991
9.
Bloom JE Wong N Nehme E Dawson LP Ball J Anderson D et al Association of socioeconomic status in the incidence, quality-of-care metrics, and outcomes for patients with cardiogenic shock in a pre-hospital setting. Eur Heart J Qual Care Clin Outcomes. (2024) 10(1):89–98. 10.1093/ehjqcco/qcad010
10.
Patlolla SH Kanwar A Belford PM Applegate RJ Zhao DX Singh M et al Influence of household income on management and outcomes of acute myocardial infarction complicated by cardiogenic shock. Am J Cardiol. (2022) 177:7–13. 10.1016/j.amjcard.2022.04.044
11.
Vallabhajosyula S Prasad A Bell MR Sandhu GS Eleid MF Dunlay SM et al Extracorporeal membrane oxygenation use in acute myocardial infarction in the United States, 2000 to 2014. Circ Heart Fail. (2019) 12(12):e005929. 10.1161/CIRCHEARTFAILURE.119.005929
12.
García-García C López-Sobrino T Sanz-Girgas E Cueto MR Aboal J Pastor P et al Cardiogenic shock mortality according to aetiology in a Mediterranean cohort: results from the shock-CAT study. ESC Heart Fail. (2025) 12(2):1336–45. 10.1002/ehf2.15148
13.
Hochman JS Buller CE Sleeper LA Boland J Dzavik V Sanborn TA et al Cardiogenic shock complicating acute myocardial infarction - etiologies, management and outcome: a report from the SHOCK trial registry. J Am Coll Cardiol. (2000) 36(3 SUPPL. A):1063–70. 10.1016/S0735-1097(00)00879-2
14.
Harjola VP Lassus J Sionis A Køber L Tarvasmäki T Spinar J et al Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail. (2015) 17:501–9. 10.1002/ejhf.260
15.
Naidu SS Baran DA Jentzer JC Hollenberg SM van Diepen S Basir MB et al SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies: this statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC), International Society for Heart and Lung Transplantation (ISHLT), Society of Critical Care Medicine (SCCM), and Society of Thoracic Surgeons (STS) in December 2021. J Am Coll Cardiol. (2022) 79:933–46. 10.1016/j.jacc.2022.01.018
16.
Desigualtats socioeconòmiques en el nombre de casos i la mortalitat per COVID-19 a Catalunya. Available online at:https://scientiasalut.gencat.cat/handle/11351/4934 (Accessed July 11, 2024).
17.
Serra-Pujadas S Alonso-Buxadé C Serra-Colomer J Folguera J Carrilero N García-Altés A . Geographical, socioeconomic, and gender inequalities in opioid use in Catalonia. Front Pharmacol. (2021) 12:750193. 10.3389/fphar.2021.750193
18.
Wang X Luke AA Vader JM Maddox TM Joynt Maddox KE . Disparities and impact of medicaid expansion on left ventricular assist device implantation and outcomes. Circ Cardiovasc Qual Outcomes. (2020) 13(6):e006284. 10.1161/CIRCOUTCOMES.119.006284
19.
Bergström G Redfors B Angerås O Dworeck C Shao Y Haraldsson I et al Low socioeconomic status of a patient’s residential area is associated with worse prognosis after acute myocardial infarction in Sweden. Int J Cardiol. (2015) 182:141–7. 10.1016/j.ijcard.2014.12.060
20.
Tizón-Marcos H Vaquerizo B Ferré JM Farré N Lidón RM Garcia-Picart J et al Socioeconomic status and prognosis of patients with ST-elevation myocardial infarction managed by the emergency-intervention “codi IAM” network. Front Cardiovasc Med. (2022) 9:847982. 10.3389/fcvm.2022.847982
21.
Thangam M Luke AA Johnson DY Amin AP Lasala J Huang K et al Sociodemographic differences in utilization and outcomes for temporary cardiovascular mechanical support in the setting of cardiogenic shock. Am Heart J. (2021) 236:87–96. 10.1016/j.ahj.2020.12.014
22.
Ryu H Moon J Jung J . Sex differences in cardiovascular disease risk by socioeconomic Status (SES) of workers using national health information database. Int J Environ Res Public Health. (2020) 17(6):2047. 10.3390/ijerph17062047
23.
Sambola A Elola FJ Buera I Fernández C Bernal JL Ariza A et al Sex bias in admission to tertiary-care centres for acute myocardial infarction and cardiogenic shock. Eur J Clin Invest. (2021) 51:e13526. 10.1111/eci.13526
24.
Collado-Lledó E de la Cuerda F Ariza-Solé A . Sex differences in acute heart failure management: is there a gap in treatment quality?Curr Heart Fail Rep. (2023) 20(2):121–8. 10.1007/s11897-023-00593-2
25.
Jentzer JC Schrage B Holmes DR Dabboura S Anavekar NS Kirchhof P et al Influence of age and shock severity on short-term survival in patients with cardiogenic shock. Eur Heart J Acute Cardiovasc Care. (2021) 10:604–12. 10.1093/ehjacc/zuaa035
26.
Mnatzaganian G Hiller JE Fletcher J Putland M Knott C Braitberg G et al Socioeconomic gradients in admission to coronary or intensive care units among Australians presenting with non-traumatic chest pain in emergency departments. BMC Emerg Med. (2018) 18(1):32. 10.1186/s12873-018-0185-2
Summary
Keywords
socioeconomic status, cardiogenic shock, intensive cardiac care units, mortality, intensive care management
Citation
Marcos-Mangas M, López-Sobrino T, Ariza-Solé A, Rueda-Sobella F, Sanz-Girgas E, Aboal J, Pastor P, Buera I, Sionis A, Andrea R, Rodríguez-López J, Tomas C, Bañeras J, Llaó I, Sánchez-Salado JC and Garcia-Garcia C (2025) Socioeconomic status and equity among patients with cardiogenic shock. Front. Cardiovasc. Med. 12:1597225. doi: 10.3389/fcvm.2025.1597225
Received
20 March 2025
Accepted
15 August 2025
Published
09 September 2025
Corrected
20 November 2025
Volume
12 - 2025
Edited by
Ivan Cavero-Redondo, Universidad de Castilla-La Mancha, Spain
Reviewed by
Stephen Forest, Albert Einstein College of Medicine, United States
Manoj Kumar, John H. Stroger, Jr. Hospital of Cook County, United States
David Sulman, Hôpitaux Universitaires Pitié Salpêtrière, France
Updates
Copyright
© 2025 Marcos-Mangas, López-Sobrino, Ariza-Solé, Rueda-Sobella, Sanz-Girgas, Aboal, Pastor, Buera, Sionis, Andrea, Rodríguez-López, Tomas, Bañeras, Llaó, Sánchez-Salado and Garcia-Garcia.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Albert Ariza-Solé aariza@bellvitgehospital.cat
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.