- 1Department of Neurology, University Hospital of Southern Denmark, Aabenraa, Denmark
- 2Neurological Research Unit, University Hospital of Southern Denmark, Aabenraa, Denmark
- 3Department of Regional Health Research, University of Southern Denmark, Odense, Denmark
The authors describe the case of a 54-year-old man with sudden onset severe headache accompanied by transitory sensory-motor deficits in all extremities, and mild abdominal pain as the initial manifestation of acute aortic dissection. Despite clinical symptoms mimicking subarachnoid hemorrhage and transitory cerebral ischemia, CT-angiography of the cerebrum and thorax revealed a Stanford type A aortic dissection. Consequently, the patient underwent insertion of a prosthesis at the aortic root and arch. In this case report, we suggest a high level of suspicion for aortic dissection in patients presenting with a sudden severe headache and/or neurological deficits accompanied by chest/back/abdominal pain, nausea, and loss of consciousness. At the same time, asymmetry of pulse and blood pressure asymmetry of the arms should also raise suspicion. An acute CT angiography with the aim of timely diagnosis will allow earlier treatment for this life-threatening condition.
Introduction
Acute aortic dissection (AAD) is a serious life-threatening condition often resulting in death due to cardiac tamponade and aortic rupture (1, 2). Clinical manifestations of aortic dissection are highly variable, which can challenge the diagnosis (2, 3). Untreated, it has a mortality rate of 50% in the first 3 days and 80% during the first two weeks (4). It usually manifests as a sudden excruciating pain anterior in the chest, which can radiate to the back (5). 17%–40% of all cases of aortic dissection present with neurological symptoms despite being a rare cause of ischemic stroke (6, 7). This is especially important for neurologists, as patients with focal neurologic symptoms due to acute aortic dissections who receive thrombolysis with recombinant tissue plasminogen activator (r-TPA) have a 71% mortality rate (7, 8). Furthermore, it has been estimated that aortic dissections are unsuspected in approximately 15%-43% of cases upon admission to hospitals, which underlines the importance of a high level of suspicion in a clinical setting (7, 9).
In this study, we present the case of a 54-year-old man who presented with thunderclap headache and focal neurological deficits as the presenting symptoms of acute aortic dissection.
Case report
A 54-year-old man with no prior medical history, no use of medication, non-smoker, and no prior traumatic injuries in the days leading up to admission presented to the emergency department with a sudden thunderclap headache that originated in the neck and radiated to the top of the head. Within seconds, the headache became holocranial and was rated as 10 out of 10 on a numeric rating scale (NRS). This was followed by a sensation of pins and needles in his right arm, which spread to both legs, followed by weakness in both legs and his left arm. After a few minutes, the sensory-motor deficits on the right-sided extremities subsided, while symptoms on the left-sided extremities subsided after approximately 30 min. Before admission, the patient had regained normal strength in all four extremities. Upon admission, the patient was still complaining of holocranial headache, which was reduced to 3 out of 10 on a NRS, nausea without vomiting, nautical dizziness, photophobia, and slight discomfort in the abdomen. There were no visual symptoms, complaints of chest pain, back pain, or cardiopulmonary symptoms.
The neurological exam was unremarkable except for slight unsteadiness in the Romberg Test, and the patient had a National Institutes of Health Stroke Scale score of 0. The patient had no cranial nerve dysfunction, did not have neck stiffness, and had a Glasgow coma scale score of 15 points. There were no clinical findings suggestive of connective tissue disease, such as a marfanoid habitus.
Upon arrival, his blood pressure was 127/56 mmHg, pulse rate 80 beats per minute, oxygen saturation 97%, and temperature 36.6 degrees Celsius. Blood tests revealed normal white blood cell counts, C-reactive protein levels, and liver and kidney parameters. Electrocardiogram demonstrated sinus rhythm with premature atrial complexes and without ST-segment deviations.
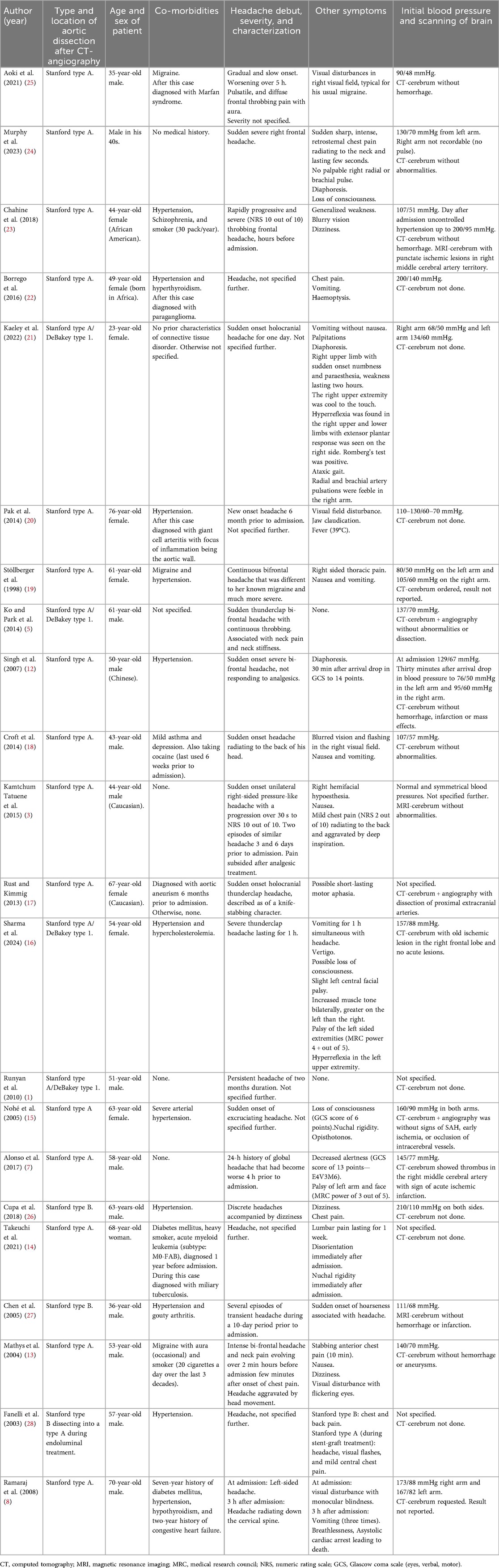
Non-contrast-enhanced computed tomography (CT) of the cerebrum revealed no intracranial abnormalities, including hemorrhage or ischemic lesions. Subarachnoidal hemorrhage was still suspected due to the thunderclap nature of the headache despite the normal CT scan of the cerebrum, while transitory cerebral ischemia was also considered a differential diagnosis. CT angiography of the cerebrum did not reveal any vascular abnormalities. Due to complaints of slight abdominal discomfort shortly after admission alongside the severe headache, CT angiography of the thorax and abdomen in the context of differential diagnostic purposes on the suspicion of aortic dissection was done, revealing a Stanford type A aortic dissection without concomitant affection of the carotid or vertebral arteries (Figure 1). Subsequent transthoracic echocardiography also visualized the extent of the aortic dissection from the aortic annulus to the femoral artery.
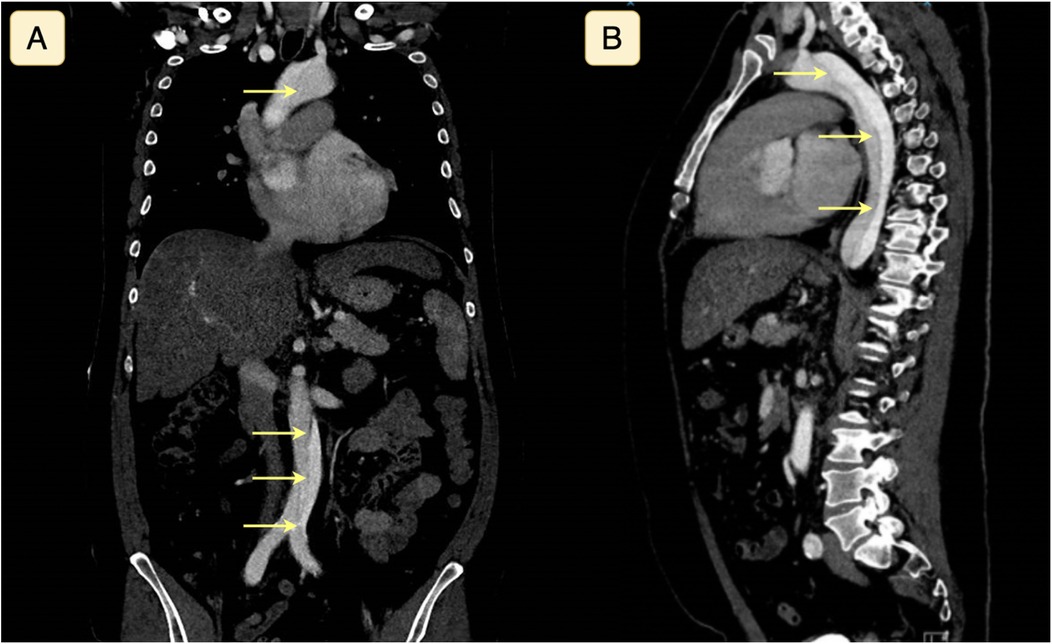
Figure 1. Computed tomography with angiography of the thorax and abdomen seen in coronal (A) and sagittal (B) plane, demonstrating a Stanford type A aortic dissection. The yellow arrows highlight the dissection plane separating the true and false lumina.
Subsequently, the patient was transferred to the department of thoracic surgery, undergoing a surgical insertion of a freestyle prosthesis at the aortic root and arch. The postoperative phase was complicated with atrial fibrillation and pericardial exudate, treated with amiodarone and subxiphoid pericardiotomy, respectively. The patient was discharged after a few weeks with follow-up in the cardiology department.
Discussion
Aortic dissection occurs because of a breach in the intima, penetrating the intima due to high blood pressure, causing blood to enter this space with further dissection propagation (10). Hypertension and atherosclerosis are the most common predisposing factors, while Marfan's syndrome, prior cardiac surgery, and aortic aneurysm are some of the other risk factors involved in developing aortic dissection (2, 10). The incidence is approximately 3 per 100.000 each year (11).
Aortic dissections are classified based on their anatomic location and time from onset, where Stanford type A dissections involve the ascending aorta and Stanford type B dissections occur distal to the left subclavian artery without involvement of the ascending aorta (2).
A systematic search of the literature in the PubMed database was performed in March 2025. We aimed to include all case reports with aortic dissection with headache as a presenting symptom, where the search term “aortic dissection AND headache” was applied. 405 studies were reviewed, of which 22 case reports were included (Table 1). One study was not included due to unavailable full text. Included cases were divided into Stanford type A (n = 19 case reports) (1, 7, 8, 12–25), Stanford type B aortic dissection (n = 2 case reports) (26, 27), and one case with a patient presenting with a Stanford type A dissection progressing into a Stanford type B (Figure 2) (28). The major risk factor (n = 11) was hypertension, and one case reports the underlying cause as Marfan syndrome (25), one case reported paraganglioma on the right side of the aorta on the level of the celiac trunk (22), and one case reported giant cell arteritis with the focus of inflammation being the aortic wall (20). Alongside headache as the initial symptom, nausea/vomiting (n = 9 case reports) and loss of consciousness (n = 6 case reports) were the most prevalent initial symptoms. CT of the cerebrum was done in 10 studies, of which two were abnormal; one case was with dissection of extracranial arteries (17) and one case with thrombus in the right middle cerebral artery (7). Two cases of Stanford type A aortic dissections were with feeble or not palpable pulses in the brachial or radial arteries in one arm (21, 24), and 3 cases (out of 11 reporting blood pressure) reported lateralized blood pressure difference of 20–66 mmHg (12, 19, 21), with one case reporting an unrecordable blood pressure in one arm (24).
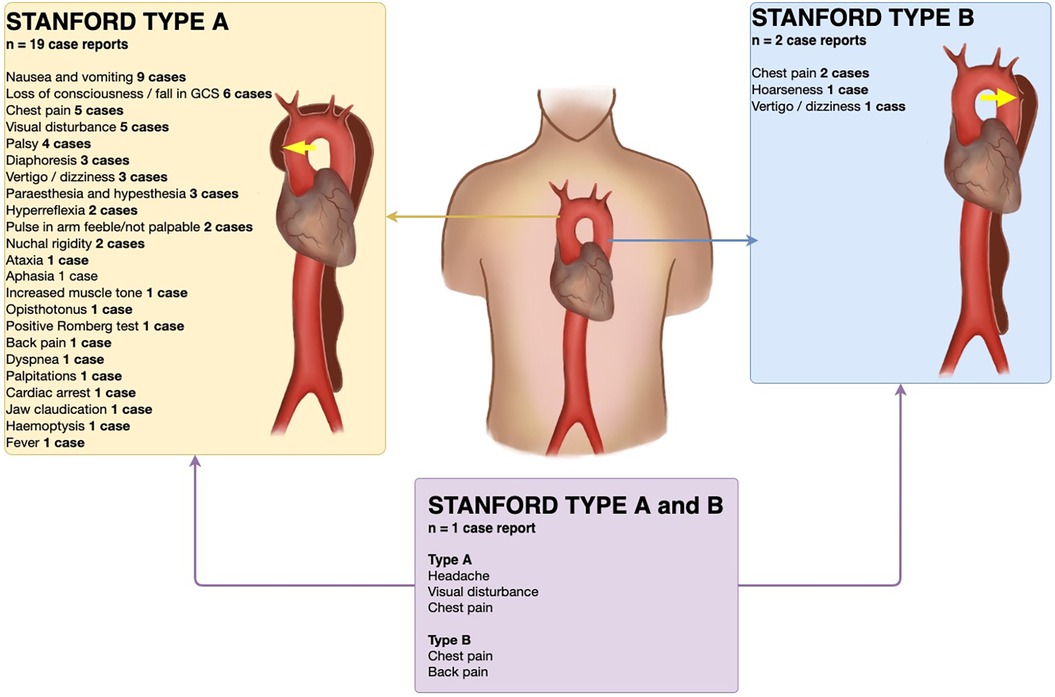
Figure 2. Findings and symptoms in reviewed case reports of Stanford type A and type B aortic dissections with headache as presenting symptom. Yellow arrow signifies site of dissection. Illustrated by Cecilia Ebratt. Copyright © 2025, all rights reserved.
Patients with aortic dissections typically present with acute onset severe chest pain (72.7%) or back pain (53.2%) (2). Anterior chest pain is usually observed in patients with Stanford type A aortic dissections, while type B dissection typically presents with pain in the back and abdomen (2). In this case report, the patient complained of mild abdominal pain. However, neurological symptoms such as headache, paraplegia, transitory cerebral ischemia, or stroke are seen in about a third of patients with aortic dissection (29). Headache as the initial manifestation of aortic dissection may be due to vessel wall distension, ischemia of the pericarotid plexus, or decreased cerebral perfusion due to antegrade flow and subclavian steal (1, 17, 19). A disruption of sympathetic projections could also be a cause of pain sensations due to the affection of the ciliary ganglion and pterygopalatine ganglion by mechanical irritation of or occlusion of the vasa nervorum of the cardiac plexus and the internal carotid plexus (17).
The abovementioned neurological manifestations can divert attention away from an underlying aortic dissection (3), contributing to the substantial percentage of up to 43% of cases missed upon initial clinical evaluation (7, 9). This can ultimately have devastating consequences for the patient as treatment with r-TPA due to the suspicion of stroke has shown to have a 71% mortality rate (7, 8).
Aortic dissection can diagnosed using CT angiography, magnetic resonance imaging, and transoesophageal echocardiography (2, 12), while chest x-ray showing a widening of the mediastinum can support the diagnosis (15). Normal echocardiography or chest x-ray findings do not exclude the possibility of aortic dissection (15).
Conclusion
This case report demonstrates a 54-year-old man presenting with thunderclap headache and focal neurological deficits as the initial manifestations of acute aortic dissection. These atypical manifestations can sometimes mimic neurological conditions, thus increasing the possibility of overlooking an aortic dissection.
Therefore, a high level of clinical suspicion for aortic dissection is warranted when patients present with a sudden severe headache accompanied by mild complaints of pain in the abdomen, chest, or back, nausea, and loss of consciousness. At the same time, asymmetry of pulse and blood pressure asymmetry of the arms should also raise suspicion. Furthermore, CT-angiography of the thorax and cerebrum is necessary to establish a timely diagnosis and subsequent treatment of aortic dissection.
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the patient for the publication of any potentially identifiable images or data included in this article.
Author contributions
MR: Writing – review & editing, Writing – original draft. VN: Investigation, Writing – review & editing, Writing – original draft. ES: Writing – review & editing, Supervision. SM: Writing – original draft, Writing – review & editing, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issue please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Runyan D, Alexander P, Saba S. Ascending aortic dissection with atypical presentation of headache. Tex Heart Inst J. (2010) 37(5):614–5.20978585
2. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The international registry of acute aortic dissection (IRAD). JAMA. (2000) 283(7):897. doi: 10.1001/jama.283.7.897
3. Kamtchum Tatuene J, Excoffier S, Vallee JP, Kleinschmidt A. Putative pathophysiological mechanisms in recurrent hemicrania from aortic dissection: a case report. BMC Res Notes. (2015) 8(1):10–3. doi: 10.1186/s13104-015-1223-8
4. Criado FJ. 8th Current trends in aortic and cardiothoracic surgery. Tex Heart Inst J. (2011) 38(6):7.
5. Ko JI, Park T. Headache: a rare manifestation of debakey type i aortic dissection. Am J Emerg Med. (2014) 32(3):291.e5–e6. doi: 10.1016/j.ajem.2013.10.022
6. MacKerricher W, Klein RR, Winston DC. Association of antemortem central nervous system symptoms and location of aortic dissections; A retrospective study from 2001 to 2014. Acad Forensic Pathol. (2016) 6(3):517–23. doi: 10.23907/2016.051
7. Alonso JV, Martin D, Kinderman H, Farhad I, Swallow P, Siggers A. Acute ischemic stroke what is hidden behind? J Cardiol Cases. (2017) 16(5):174–7. doi: 10.1016/j.jccase.2017.07.010
8. Ramaraj R, O’Beirn D, Bracewell RM. Aortic dissection presenting as uniocular blindness. South Med J. (2008) 101(8):842–4. doi: 10.1097/SMJ.0b013e31817dfd5f
9. Spittell PC, Spittell JA Jr, Joyce JW, Tajik AJ, Edwards WD, Schaff HV, et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990). Mayo Clin Proc. (1993) 68(7):642–51. doi: 10.1016/s0025-6196(12)60599-0
10. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. J Am Coll Cardiol. (2010) 55(14):266–369. doi: 10.1016/j.jacc.2010.02.015
11. Golledge J, Eagle KA. Acute aortic dissection. Lancet. (2008) 372(9632):55–66. doi: 10.1016/S0140-6736(08)60994-0
12. Singh S, Huang JY, Sin K, Charles RA. Headache: an unusual presentation of aortic dissection. Eur J Emerg Med. (2007) 14(1):47–9. doi: 10.1097/01.mej.0000224435.89740.bc
13. Mathys J, Lachat M, Herren T. Headache as a manifestation of a life-threatening vascular disorder. Headache J Head Face Pain. (2004) 44(7):706–9. doi: 10.1111/j.1526-4610.2004.04130.x
14. Takeuchi S, Takayama N, Soejima K, Yoshino H. A penetrating atherosclerotic ulcer rapidly growing into a saccular aortic aneurysm during treatment of leukaemia: a case report. Stathogiannis K, Abumuaileq RRY, Filomena D, Carazo CM, Thomson R, eds. Eur Heart J - Case Rep. (2021) 5(7):ytab196. doi: 10.1093/ehjcr/ytab196
15. Nohé B, Ernemann U, Tepe G, Ritz R, Bail D. Aortic dissection mimicking subarachnoidal hemorrhage. Anesth Analg. (2005) 101(1):233–4. doi: 10.1213/01.ANE.0000154190.06408.38
16. Sharma M, Daren A, Pretorius E, Keeler L, Fonarov I. Transient neurological deficits in a patient with prior DeBakey type 1 aortic dissection. Cureus. (2024):1–8. doi: 10.7759/cureus.67839
17. Rust H, Kimmig H. Thunderclap headache as the main symptom of an acute aortic dissection type A. J Neurol. (2013) 260(7):1925–6. doi: 10.1007/s00415-013-6969-0
18. Croft AP, Nader K, Arulanantham N. A very unusual headache. Clin Med. (2014) 14(1):58–60. doi: 10.7861/clinmedicine.14-1-58
19. Stöllberger C, Finsterer J, Fousek C, Waldenberger F, Haumer H, Lorenz W. Headache as the initial manifestation of acute aortic dissection type A. Cephalalgia. (1998) 18(8):583–4. doi: 10.1046/j.1468-2982.1998.1808583.x
20. Pak M, Ito S, Takeda M, Watanabe N, Sato H, Ito S, et al. A case of ascending aortic dissection and rupture caused by giant cell arteritis. Int Heart J. (2014) 55(6):555–9. doi: 10.1536/ihj.14-059
21. Kaeley N, Gangdev A, Galagali SS, Kabi A, Shukla K. Atypical presentation of aortic dissection in a young female and the utility of point-of-care ultrasound in identifying aortic dissection in the emergency department. Cureus. (2022):1–7. doi: 10.7759/cureus.27236
22. Borrego A, Carrilho Ferreira P, Pinto FJ. Acute type A aortic dissection in a patient with paraganglioma. Rev Port Cardiol Engl Ed. (2017) 36(10):777.e1–e6. doi: 10.1016/j.repce.2017.09.011
23. Chahine J, Thapa B, Gajulapalli RD, Kadri A. Acute aortic dissection presenting with a headache: an easily missed life-threatening emergency. Cureus. (2018):1–6. doi: 10.7759/cureus.3531
24. Murphy M. Aortic dissection during endurance cycling. BMJ Case Rep. (2023) 16(11):e257207. doi: 10.1136/bcr-2023-257207
25. Aoki T, Soh M, Hifumi T, Otani N. A case of Stanford type A aortic dissection complaining only of headache with a history of migraine. Cureus. (2021). doi: 10.7759/cureus.20716
26. Cupa J, Hippe HJ, Schäfer P, Frey N, Langer C. Renovascular hypertension: endovascular therapy in complicated aortic Stanford type B dissection. Cardiovasc Diagn Ther. (2018) 8(2):173–5. doi: 10.21037/cdt.2017.11.06
27. Chen HC, Lin CJ, Tzeng YS, Tsai CS, Wang CH. Hoarseness as an unusual initial presentation of aortic dissection. Eur Arch Otorhinolaryngol. (2005) 262(3):189–91. doi: 10.1007/s00405-004-0765-5
28. Fanelli F, Salvatori FM, Marcelli G, Bezzi M, Totaro M, Vagnarelli S, et al. Type a aortic dissection developing during endovascular repair of an acute type B dissection. J Endovasc Ther. (2003) 10:254–9. doi: 10.1177/152660280301000215
Keywords: headache, aortic dissection, computed tomography, neurologic deficits, emergency medicine, differential diagnosis
Citation: Ranjeevan M, Nielsen V, Stenager E and Mamoei S (2025) Thunderclap headache as an initial manifestation of acute aortic dissection: a case report and review of literature. Front. Cardiovasc. Med. 12:1598757. doi: 10.3389/fcvm.2025.1598757
Received: 24 March 2025; Accepted: 6 October 2025;
Published: 23 October 2025.
Edited by:
Sabina Cevoli, IRCCS Institute of Neurological Sciences of Bologna (ISNB), ItalyReviewed by:
Simone Quintana, IRCCS Local Health Authority of Reggio Emilia, ItalyLuigi d'Onofrio, Campus Bio-Medico University of Rome, Italy
Copyright: © 2025 Ranjeevan, Nielsen, Stenager and Mamoei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sepehr Mamoei, c21hbW9laUBoZWFsdGguc2R1LmRr
†ORCID:
Mario Ranjeevan
orcid.org/0000-0001-7089-8408
Valeriia Nielsen
orcid.org/0009-0003-4715-3696
Egon Stenager
orcid.org/0000-0002-4877-5193
Sepehr Mamoei
orcid.org/0000-0003-3140-4983
 Mario Ranjeevan1,2,†
Mario Ranjeevan1,2,† Egon Stenager
Egon Stenager Sepehr Mamoei
Sepehr Mamoei