- 1Department of Cardiovascular Area Ⅲ, Handan Mingren Hospital, Handan, Hebei, China
- 2Department of Anesthesiology, Handan Central Hospital, Handan, Hebei, China
Objective: This study aims to investigate the effect of Yiqi Huoxue Tongluo decoction (YHTD) in combination with conventional medicine therapy on restenosis rates and clinical efficacy in patients with coronary heart disease undergoing percutaneous coronary intervention.
Methods: A total of 80 patients with coronary artery disease who underwent PCI between August 2019 and February 2021 were selected, and the patients were assigned to either the control group (n = 40) or the observation group (n = 40) according to a randomized numerical table. The control group received conventional medicine treatment, while the observation group took YHTD alongside conventional medicine treatment. Coronary angiography was performed after 6 months of treatment to compare the changes in coronary restenosis, TCM syndrome scores, Seattle Angina Questionnaire (SAQ) scores, cardiac function indexes, and related serum biomarkers between the two groups.
Results: After treatment, the TCM syndrome scores of patients in both groups were lower than those before treatment, and the post-treatment TCM syndrome scores of the observation group were significantly lower than those of the control group. Similarly, the SAQ scores of patients in both groups were significantly higher than those before treatment, and the SAQ scores of the observation group were significantly higher than those of the control group. After treatment, both groups showed significant reductions in the LVEDD and LVESD compared with those before treatment, and the LVEDD and LVESD values of the observation group were significantly lower than those of the control group. Similarly, the LVEF and SV of patients in both groups increased compared with those before treatment; however, the LVEF and SV values of the observation group were significantly higher than those of the control group, and the difference was statistically significant. After treatment, hs-CRP, Hcy, and sST2 were significantly reduced in both groups, and the levels of hs-CRP, Hcy, and sST2 in the observation group were significantly lower than those in the control group.
Conclusion: YHTD combined with conventional medicine therapy can significantly reduce the rate of coronary restenosis in post-PCI patients, improve the TCM symptoms, alleviate angina symptoms, enhance cardiac function indexes, and effectively regulate serum biomarker levels, which offers a better choice for the treatment of post-PCI coronary artery disease.
Introduction
Coronary heart disease (CHD) is one of the most common chronic cardiovascular conditions worldwide, posing a serious threat to human health and life expectancy (1). In recent years, the incidence and mortality rate of CHD have remained high, largely due to an aging population, lifestyle changes, and the accumulation of adverse environmental factors (2–5). The pathological basis of coronary heart disease is coronary atherosclerosis, which can lead to blood vessel narrowing or obstruction. This, in turn, triggers myocardial ischemia and hypoxia and, in severe cases, may lead to myocardial infarction, which can be life-threatening (6).
Percutaneous coronary intervention (PCI), as an effective treatment method, has emerged as a major breakthrough in the treatment of coronary heart disease due to its many advantages, such as minimal trauma, faster recovery, and rapid restoration of myocardial blood flow (7–9). A large number of clinical practices and studies have confirmed that PCI can significantly relieve angina symptoms, effectively reduce the incidence of acute myocardial infarction and other serious cardiovascular events, and greatly improve the quality of life of patients in the near future (10). However, post-PCI revascularization remains a critical problem, affecting the long-term prognosis and quality of life of patients (11, 12). Relevant studies have shown that drug-eluting stent (DES) in-stent restenosis (ISR) occurs in 3%–20% of patients (8, 11). The occurrence of in-stent restenosis (ISR) not only necessitates repeat interventions or surgical bypass surgery, which greatly increases healthcare costs and patient suffering, but also significantly reduces patient survival and quality of life (13).
Currently, conventional medicine mainly adopts comprehensive treatment strategies such as antiplatelet therapy, lipid regulation, and blood pressure and glucose control for the occurrence of ISR after PCI (14–16). Antiplatelet drugs, such as aspirin and clopidogrel, help reduce the risk of restenosis by inhibiting platelet aggregation and reducing thrombosis (14); additionally, statins, which are lipid-regulating agents, play a role in restenosis prevention by lowering lipid levels and stabilizing plaques (17, 18). However, these treatments have obvious limitations. For example, long-term use of antiplatelet drugs can lead to bleeding and other serious adverse reactions, and some patients may also develop drug resistance, which reduces the therapeutic efficacy (19).
In China, traditional Chinese medicine (TCM) is widely used for the prevention and treatment of cardiovascular diseases (20). In Chinese medicine, coronary artery disease belongs to the category of blood stasis syndrome, characterized byblood stasis, phlegm obstruction, qi deficiency, and cold condensation (20, 21). Post-PCI restenosis is thought to be caused by arterial and meridian damage resulting from qi deficiency, blood stasis, and cardiac meridian paralysis (22). Therefore, the principle of benefiting qi and activating blood has become a general treatment method for managing post-PCI restenosis (22, 23). In recent years, with the vigorous development of integrated Chinese and conventional medicine, the study of combining Chinese medicine with conventional medicine for the post-PCI treatment of coronary artery disease has gradually become a hotspot, which is expected to provide a new solution to reduce the rate of post-PCI restenosis and improve clinical outcomes for patients (20, 24).
Yiqi Huoxue Tongluo decoction (YHTD) originates from traditional Chinese medicine theory and has the main effects of benefiting qi, promoting blood circulation, and dredging the collaterals. Modern pharmacological studies have shown that qi-benefiting and blood-activating Chinese herbal compounds can exert anti-atherosclerotic effects by regulating blood lipids, inhibiting platelet activation, suppressing the expression of MCP-1 and NF-κB, and reducing the levels of inflammatory markers (25). Multiple studies have demonstrated that active components of Chinese herbs can improve vascular endothelial function by inhibiting the TLR4/NF-κB signaling pathway (26, 27). Based on this background, this study aims to systematically observe the effects of YHTD in combination with conventional medicine on restenosis rates and clinical efficacy in patients with coronary artery disease undergoing PCI to provide a more reliable basis and reference for clinical treatment.
Materials and methods
Study design and subjects
This study was an open-label, randomized controlled trial. The sample size was calculated based on preliminary data indicating a late lumen loss (LLL) difference of d = 0.75, with α = 0.05 and a power of 0.8, requiring at least 34 patients per group. Considering a 15% dropout rate, 40 patients per group were enrolled. While patient blinding was not feasible due to the nature of the intervention, outcome assessors were blinded to group allocation when evaluating angiographic results and questionnaire scores.
Eighty patients with coronary artery disease who were hospitalized in the Department of Cardiovascular Medicine at our hospital from August 2019 to February 2021 were enrolled. All patients successfully underwent PCI. The patients were assigned to either the control group (n = 40) or the observation group (n = 40) according to the random number table method. The control group received conventional medicine treatment, while the observation group was given YHTD in addition to conventional therapy. This study was reviewed and approved by the Ethics Committee of Handan Central Hospital, in accordance with the Declaration of Helsinki.
Inclusion and exclusion criteria
Patients were eligible for inclusion if they met the following criteria: (1) coronary angiography (CAG) suggested coronary artery stenosis, and stent implantation was performed; (2) diagnosis of qi deficiency and blood stasis syndrome according to traditional Chinese medicine, characterized by the presence of at least two main symptoms (chest pain, chest tightness, shortness of breath, fatigue) and two secondary symptoms (dark complexion, purple tongue, thready and hesitant pulse, dark sublingual veins); (3) no cognitive dysfunction and verbal communication disorders; and (4) provided a written informed consent to voluntarily participate in the trial.
Patients were excluded from the study if they met any of the following conditions: (1) presence of acute complications after PCI; (2) underwent repeat PCI due to restenosis after the initial PCI; (3) diagnosed with severe cardiac arrhythmia or had a pacemaker implanted; (4) suffering from serious primary diseases of the liver, kidney, or hematopoietic system or had psychiatric disorders; (5) known allergy to the study drugs; (6) pregnant or lactating women.
Note: Intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was used only for high-risk lesions due to cost constraints and procedural limitations. This study used CAG as the standard method for assessing restenosis, which is acknowledged as a limitation in the Discussion section.
Treatment methods
The control group received conventional medicine treatment, consisting of oral administration of 100 mg aspirin tablets once daily, 75 mg clopidogrel once daily, and 20 mg atorvastatin calcium tablets once nightly. These oral drugs were taken continuously for 6 months.
In the observation group, on the basis of the conventional medicine treatment, YHTD was administered starting in the same week as the PCI operation and continuing for 6 months. The Chinese herbal formula consisted of astragalus 30 g, Salvia miltiorrhiza 20 g, Rhizoma Ligustici chuanxiong 15 g, safflower 10 g, leeches 6 g, dilong 10 g, scorpion 3 g, and Glycyrrhiza glabra 6 g. The herbs were decocted twice (20 min each) in 500 ml of water, the filtrates were combined and concentrated to 300 ml, and patients took 150 ml twice daily (bid) for 6 months.
Clinical assessment
Comparison of coronary restenosis: Vascular restenosis was assessed using coronary angiography. At 6 months post-operation, follow-up coronary angiography was performed, and restenosis was defined as ≥50% stenosis of the inner diameter of coronary vessels. The restenosis rate was calculated as follows: restenosis rate = (number of restenosis cases/total number of cases) × 100%. The following indexes were measured and recorded: minimal lumen diameter (MLD) was defined as the inner diameter of the narrowest part of the coronary lesion; LLL was defined as the difference between the lumen diameter immediately after stent implantation and the lumen diameter at follow-up; late loss index (LLI) was defined as the ratio of late lumen loss to lumen diameter immediately after stent implantation; net lumen gain (NG) was defined as the difference between the lumen diameter after stent implantation and the preoperative stenosis diameter; net lumen gain index (NGI) was defined as the ratio of the net gain to the preoperative stenosis diameter.
TCM syndrome score: The TCM syndrome score is a tool used to quantify the severity of a patient's symptoms by assigning point values based on symptom intensityand adding them together to obtain a total score: 2 points for mild symptoms (slight discomfort with no impact on everyday life); 4 points for moderate symptoms (significant discomfort that partially affects daily life); and 6 points for severe symptoms (severe discomfort that significantly affects daily life). Common symptoms include chest pain, chest tightness, shortness of breath, insomnia, and fatigue. This scoring system was adapted from the State Administration of TCM guidelines (ZY/T 001.1-1994) (28).
Seattle Angina Questionnaire (SAQ): The SAQ is used to assess the symptoms of CHD and their impact on daily life (29, 30). It contains 19 items that can be categorized into five dimensions: physical limitation, anginal stability, anginal frequency, treatment satisfaction, and disease perception. The scoring of the questionnaire is first based on the questions answered by the patients. First, raw scores are calculated for each of the five dimensions, and these raw scores are then converted into the standardized formula to calculate the standard score of each dimension: standard score = (actual score−minimum score)/(maximum score−minimum score) × 100. Each dimension score ranges from 0 to 100, with higher SAQ scores indicating better functioning and better health-related quality of life.
Cardiac function indexes: Color ultrasound was used to compare the cardiac function [left ventricular ejection fraction (LVEF), left ventricular end-diastolic internal diameter (LVEDD), left ventricular end-systolic internal diameter (LVESD), and stroke volume (SV)] in both groups of patients with coronary artery disease before and after treatment.
Serum biomarkers: Serum levels of high-sensitivity C-reactive protein (hs-CRP), homocysteine (Hcy), and soluble suppression of tumorigenicity 2 (sST2) were determined according to the instructions of the ELISA kit. The hs-CRP ELISA kit (XY-1967) was purchased from Shanghai Xinyu Biotechnology Co., Ltd., and the Hcy (JL10022) and sST2 (JL18366) ELISA kits were purchased from Shanghai Jianglai Biotechnology Co. All procedures were performed in strict accordance with the instructions.
Clinical data collection and follow-up
In the early morning, 5 ml of fasting venous blood was drawn from the elbow of each patient in a collection tube and naturally agglutinated for 30 min at room temperature; after the blood had coagulated, it was centrifuged at 2,000 r/min for 20 min; the upper serum layer was collected and stored at −80°C for future analysis. Information on patients' age, gender, body mass index (BMI), smoking history, alcohol consumption history, family history of coronary heart disease, and comorbidities (hypertension, hyperlipidemia, diabetes mellitus) was collected. In addition, the levels of fasting blood glucose (FBG), total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and other markers were measured using an automatic biochemical analyzer (Beijing Plan New Technology Co., Ltd.).
During the 6-month follow-up period, adverse events were recorded. Two patients in the YHTD group reported mild gastric distension; however, no patients discontinued treatment. The average medication adherence rate was 93%.
Statistical analysis
Data were statistically analyzed and graphed using GraphPad Prism 9.5.0 software (GraphPad Software Inc., San Diego, CA, USA). The Shapiro–Wilk test was used to assess normality of data distribution, and variables conforming to a normal distribution were expressed as mean ± standard deviation. Comparisons between two groups were performed using an independent samples t-test, while within-group comparisons (pre- and post-treatment) were performed using a paired samples t-test. Count data were expressed as the number of cases and percentages, and comparisons between groups were performed using the chi-square test. All P values were two-sided, and the difference was considered statistically significant at P < 0.05.
Results
Comparison of baseline data between the two groups of subjects
Eighty patients with coronary artery disease who underwent PCI at our hospital from August 2019 to February 2021 were enrolled in this study. Patients were assigned to either the control group (n = 40) or the observation group (n = 40) according to the method of a randomized numerical table. The control group received conventional medicine treatment, while the observation group was given YHTD alongside conventional medicine. There were no significant differences between the two groups in terms of age, gender, BMI, smoking history, drinking history, family history of coronary heart disease, comorbidities (hypertension, hyperlipidemia, diabetes mellitus), FBG, TG, TC, HDL-C, and LDL-C, among others (all P’s > 0.05) (Table 1).
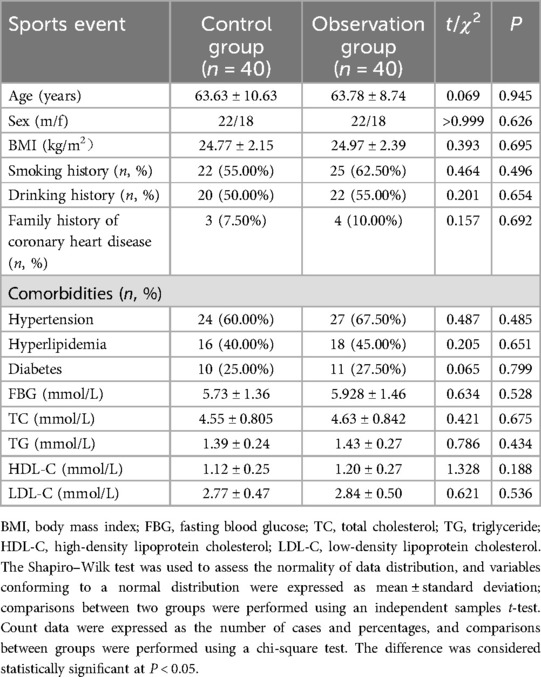
Comparison of coronary restenosis in two groups
We compared the coronary restenosis in two groups of patients, and the results showed that after 6 months of treatment, 10 cases of restenosis occurred in the control group and 3 cases of restenosis occurred in the observation group, and the rate of restenosis in the observation group (7.50%) was significantly lower than that in the control group (25.00%), and the difference was statistically significant (χ² = 4.501, P = 0.034). In addition, compared with the control group, MLD, NG, and NGI were significantly larger, and LLL and LLI were significantly lower in the observation group (all P's < 0.05), as shown in Figure 1.
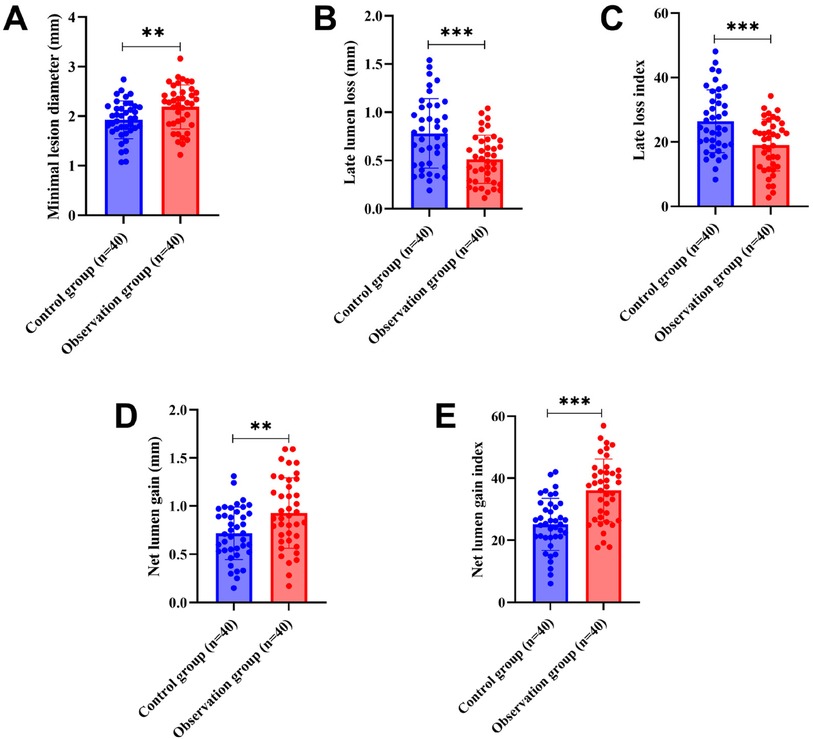
Figure 1. Comparison of coronary restenosis between the two groups of patients (A: MLD, B: LLL, C: LLI, D: NG, E: NGI). MLD, minimal lumen diameter; LLL, late lumen loss; LLI, late loss index; NG, net lumen gain; NGI, net lumen gain index.
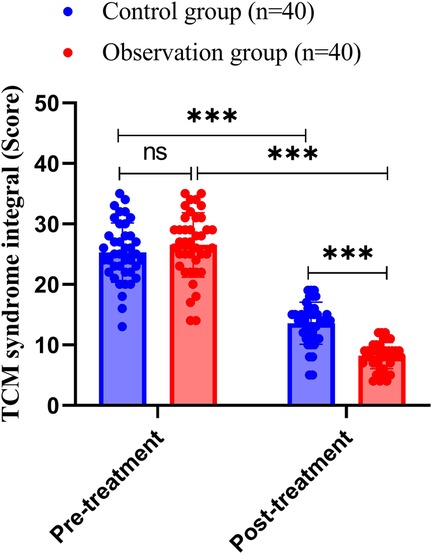
Comparison of TCM syndrome scores between the two groups of patients
We compared the TCM syndrome scores of the two groups of patients, and the results showed that before treatment, the TCM syndrome score of the control group was 25.25 ± 4.88, while that of the observation group was 26.53 ± 5.32; the difference between the two groups was not statistically significant (P = 0.268). After treatment, the TCM syndrome score of the control group was 13.58 ± 3.47, while that of the observation group was 8.23 ± 2.17; both groups showed significantly lower TCM syndrome scores than those before the treatment (both P < 0.001), and the post-treatment TCM syndrome scores of the observation group were significantly lower than those of the control group (all P’s < 0.001), as shown in Figure 2.
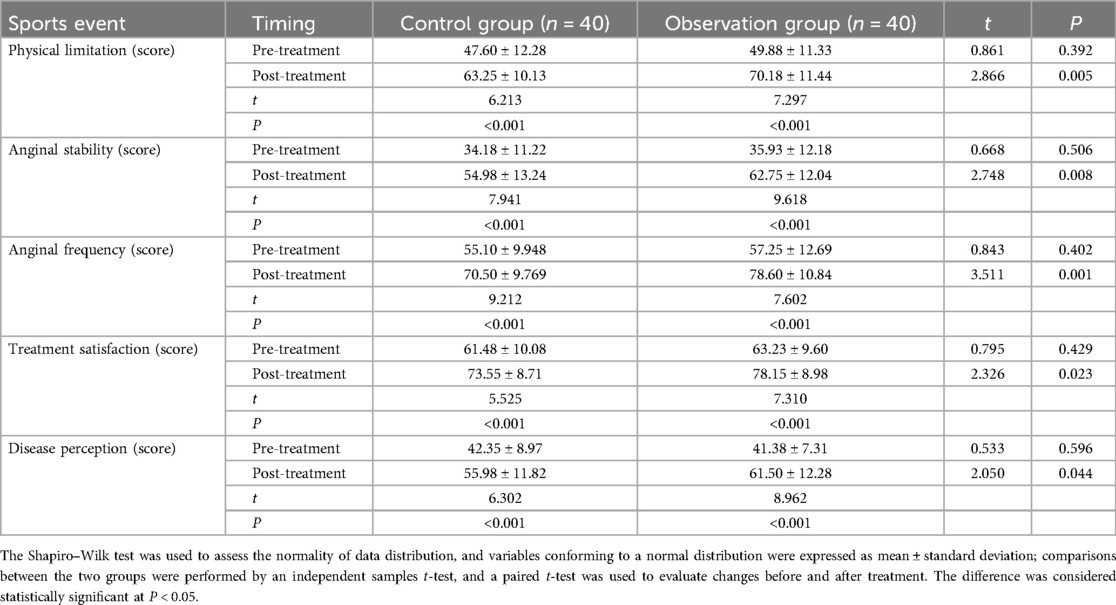
Comparison of the Seattle Angina Questionnaire scores between the two groups
The SAQ was used to assess the CHD symptoms and their impact on daily life. It was found that there were no statistical differences between the two groups of patients across all SAQ dimensions before treatment (physical limitation, anginal stability, anginal frequency, treatment satisfaction, and disease perception) (all P’s > 0.05); after 6 months of treatment, SAQ scores of the patients in both groups were significantly higher than those before treatment (all P’s < 0.001). In addition, the post-treatment SAQ scores of the observation group were significantly higher than those of the control group (all P’s < 0.05) (Table 2).
Comparison of cardiac function indexes before and after treatment in two groups
We compared LVEF, LVEDD, LVESD, and SV between the two groups. The results showed no statistical differences in LVEF, LVEDD, LVESD, and SV between the two groups before treatment (P > 0.05); after 6 months of treatment, LVEDD and LVESD were significantly reduced in both groups compared to pre-treatment values, and the reductions were were more pronounced in the observation group than in the control group (both P’s < 0.05). Additionally, LVEF and SV significantly increased in both groups after treatment, with the observation group showing greater improvements in LVEF and SV than the control group, and the differences were statistically significant (all P's < 0.05) (see Table 3).
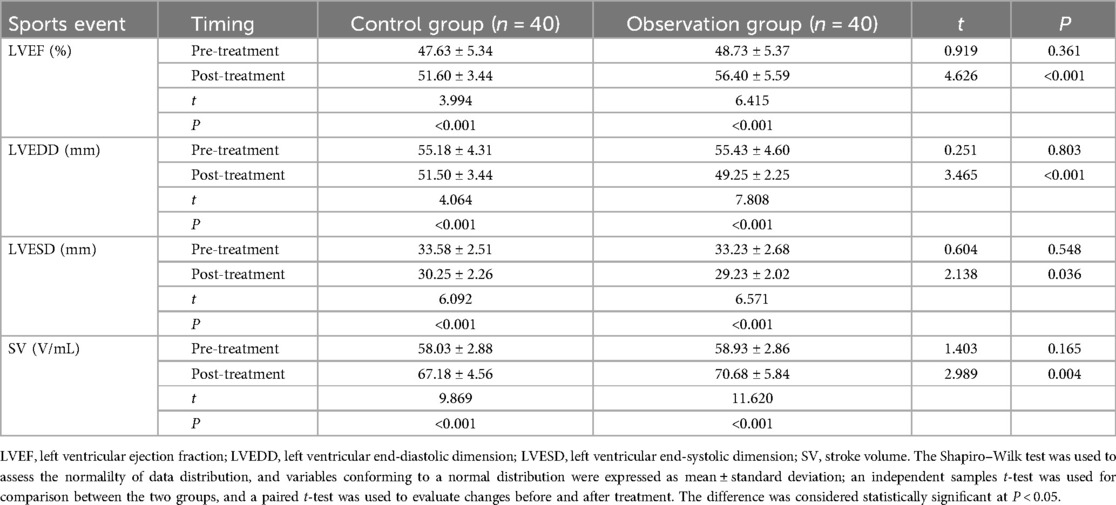
Table 3. Comparison of cardiac function indexes before and after treatment in the two groups of patients.
Comparison of serum biomarkers between the two groups of patients
Previous studies have reported that elevated levels of hs-CRP and Hcy are associated with a higher risk of ISR after PCI in patients with coronary artery disease (31–33). In addition, elevated levels of sST2 are strongly associated with adverse cardiovascular outcomes after PCI (34). Therefore, we determined serum levels of hs-CRP, Hcy, and sST2 by ELISA, and the results showed no statistically significant differences in the levels of hs-CRP, Hcy, and sST2 between the two groups of patients before treatment (all P’s > 0.05). After treatment, the serum hs-CRP level in the control group was 3.55 ± 1.17 mg/L, the Hcy level was 17.41 ± 2.01 μmol/L, and the sST2 level was 39.67 ± 3.98 ng/mL; in contrast, the serum hs-CRP level in the observation group was 2.81 ± 0.90 mg/L, the Hcy level was 15.03 ± 2.07 μmol/L, and the sST2 level was 37.10 ± 4.19 ng/mL. These results indicate that hs-CRP, Hcy, and sST2 levels were significantly reduced in both groups after treatment (all P’s < 0.001), with the reductions in the observation group being significantly lower than those in the control group after treatment (all P’s < 0.01), as shown in Figure 3. Additional atherosclerosis-specific markers, including ox-LDL and Lp-PLA2, were also measured, showing consistent intergroup differences (Supplementary Table S1).
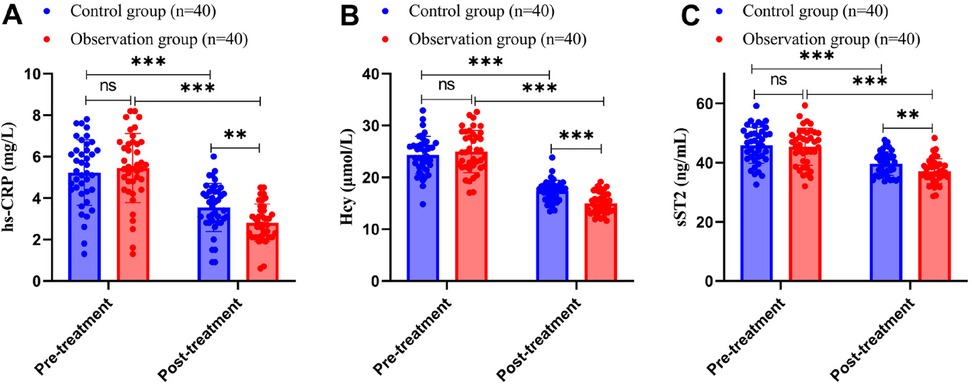
Figure 3. Comparison of serum biomarkers between the two groups of patients (A: hs-CRP, B: Hcy, C: sST2). hs-CRP, high-sensitivity C-reactive protein; Hcy, homocysteine; sST2, soluble suppression of tumorigenicity 2.
The Shapiro-Wilk test was used to test for normal distribution, and measurements conforming to normal distribution were expressed as mean ± standard deviation. Independent samples t-test was used for comparison between the two groups, and paired t-test was used before and after treatment. Differences were considered statistically significant at P < 0.05. ns indicates P > 0.05, ** indicates P < 0.01, and *** indicates P < 0.001.
Discussion
Coronary heart disease is a common chronic cardiovascular condition and remains a serious threat to human health (35). Although PCI has brought a major breakthrough in the treatment of coronary heart disease, post-operative restenosis continues to affect the long-term prognosis of patients (36, 37). In this study, we compared the effects of conventional medicine treatment alone versus YHTD combined with conventional medicine on post-operative PCI patients with coronary artery disease, and the results showed that the combination therapy offered significant advantages in several aspects.
In terms of coronary restenosis, the observation group exhibited a significantly lower restenosis rate than the control group; additionally, the observation group showed increased values of MLD, NG, and NGI and decreased values of LLL and LLI. This suggests that YHTD combined with conventional medicine therapy can effectively inhibit endothelial proliferation, maintain vascular patency, and reduce the risk of restenosis (20, 38). From the perspective of Chinese medicine theory, coronary heart disease belongs to the category of blood stasis syndrome, characterized by blood stasis, phlegm obstruction, qi deficiency, and cold condensation; post-operative restenosis after PCI is believed to be associated with qi deficiency, blood stasis, and cardiac meridian paralysis (22). In YHTD, astragalus tonifies qi and elevates yang; danshen, chuanxiong, and safflower promote blood circulation and remove blood stasis; leech, dilong, and scorpion penetrate the channels to alleviate pain; and Glycyrrhiza tonifies the medicines to work together to activate qi and blood and penetrate the channels to alleviate pain (39, 40). Modern pharmacological studies have also confirmed that Chinese medicines with blood-activating and blood-stasis-eliminating properties exert effects such as antiplatelet aggregation, improvement of microcirculation, and inhibition of the proliferation of smooth muscle cells (40, 41). From the perspective of integrative medicine, the concept of qi deficiency in TCM corresponds to endothelial dysfunction and impaired energy metabolism at the cellular level, while blood stasis reflects the pathological states such as increased platelet aggregation, inflammation, and microcirculatory disturbances. Similarly, the meridian blockage concept aligns with vascular stenosis and impaired blood flow.
The therapeutic effects of YHTD can be attributed to its key bioactive components. Astragaloside IV, the main active component of astragalus, exhibits anti-inflammatory and endothelial protective effects by inhibiting the TLR4/NF-κB signaling pathway, thereby reducing the expression of inflammatory cytokines (IL-6, TNF-α) and adhesion molecules (VCAM-1, ICAM-1) while enhancing NO production (42). Tanshinone IIA protects against oxidative stress and inhibits the proliferation and migration of VSMCs, contributing to plaque stabilization (43). Tetramethylpyrazine exerts antiplatelet and anti-inflammatory effects via inhibition of the P38 MAPK and NF-κB signaling pathways (44). These components act synergistically to inhibit phenotypic transformation of VSMCs from a contractile to a synthetic state and suppress neointimal formation by downregulating PDGF and TLR4/NF-κB signaling pathways (45), which may explain the observed reductions in inflammatory markers (hs-CRP, Hcy, sST2) and the decreased restenosis rate in our study. Our findings are consistent with previous studies. For example, Mao et al. (40) reported a similar reduction in restenosis rates in post-PCI patients treated with Tongxinluo capsules. However, our study showed a more pronounced improvement in cardiac function parameters.
TCM, with its multi-component, multi-target, and holistic characteristics, plays an active and vital role in the prevention and treatment of various cardiovascular diseases in China, and it offers significant advantages in stabilizing the condition and improving the quality of life of patients (46). TCM has been recognized as a potential approach for relieving symptoms and improving quality of life in patients with cardiovascular disease (21). The SAQ is the most commonly used tool for assessing comprehensive and sensitive changes in the quality of life of cardiac patients (47). In this study, the TCM syndrome scores and SAQ scores improved after treatment; specifically, TCM syndrome scores of both groups decreased after treatment, with the observation group exhibiting lower scores than the control group; after 6 months of treatment, the scores of all SAQ dimensions increased in both groups, with the observation group exhibiting higher scores than the control group. These findings suggest that combination therapy effectively alleviates angina symptoms, improves TCM symptoms, and enhances the quality of life of patients (48, 49).
It has been reported that herbal formulas containing astragalus, or herbal astragalus alone, can enhance myocardial contractility and improve cardiac diastolic function (50, 51). In addition, shenmai injection may improve cardiac function in patients with chronic heart failure (CHF) through its anti-apoptotic effects, antioxidant activity, anti-inflammatory properties, and improvement of myocardial metabolism (52). Cardiac function indexes showed that LVEF and SV increased, while LVEDD and LVESD decreased in both groups after treatment, and the degree of improvement was better in the observation group than in the control group. These findings indicate that the combination therapy can effectively improve cardiac function and enhance myocardial contractility. This may be due to the synergistic effect of Chinese medicine and conventional medicine in improving myocardial blood perfusion and inhibiting myocardial remodeling, thus enhancing the pumping ability of the heart (53).
hs-CRP is a highly sensitive indicator of inflammatory response, and a decrease in its level reflects a reduction in the degree of inflammation in the body. Inflammation plays a key role in the development and progression of coronary artery disease, and elevated serum levels of hs-CRP have been significantly associated with the occurrence of restenosis (ISR) after coronary intervention (31, 54). In addition, studies have reported that homocysteine (Hcy) levels are positively correlated with the severity of restenosis after coronary intervention and can be used as an important biomarker for predicting the severity of restenosis (55, 56). Meanwhile, sST2 has been identified as an important indicator for assessing the prognosis of cardiovascular disease after PCI (34). The results of serum biomarker analysis showed that YHTD combined with conventional medicine therapies more effectively reduced the levels of hs-CRP, Hcy, and sST2, thus providing new ideas and methods for the post-PCI treatment of patients with coronary artery disease.
However, this study has some limitations. The relatively small sample size of only 80 patients may not comprehensively capture the diversity of patient characteristics, and there is a sampling error, so the representativeness and generalizability of the study results need to be improved. With a follow-up period of only 6 months, it is difficult to accurately assess the long-term efficacy and safety of interventions for post-PCI restenosis, which is a problem with a long-term dynamic process, because the observation period is relatively short. Additionally, this study used an open-label design in which patient blinding was not feasible; however, outcome assessors were blinded. The use of coronary angiography, instead of more sensitive techniques like IVUS or OCT, may have limited the accuracy of restenosis assessment. Future studies can be improved in the following aspects: by expanding the sample size and conducting multi-center, large-sample clinical studies to enhance the reliability and representativeness of the results; by extending the follow-up period to observe the long-term efficacy and safety of the combination therapy; and by incorporating advanced imaging techniques like IVUS or OCT to achieve a more accurate assessment of vascular changes.
Future research directions should include: (1) the application of multi-omics approaches to identify biomarkers predicting treatment response; (2) systematic investigations of specific bioactive compounds and their synergistic effects using network pharmacology; (3) mechanistic studies using advanced molecular techniques such as single-cell RNA sequencing to understand cell-specific responses; and (4) the development of standardized quality control methods for TCM preparations.
Conclusion
In conclusion, YHTD combined with conventional medicine therapy demonstrates significantly better outcomes than conventional medicine therapy alone in patients undergoing PCI for coronary artery disease; the combination therapy more effectively improves coronary restenosis, reduces TCM syndrome scores, alleviates angina symptoms, enhances cardiac function, and lowers the levels of related serum biomarkers. These findings suggest that YHTD may serve as an adjuvant therapy for post-PCI management. However, to further validate these results and establish its role in clinical practice, multi-center studies with larger sample sizes and advanced imaging techniques (IVUS/OCT) are needed.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Handan Central Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
XZ: Writing – review & editing, Formal analysis, Methodology, Resources, Writing – original draft. LZ: Writing – original draft, Project administration, Software, Validation. ZL: Conceptualization, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Hebei Provincial Medical Science Research Project (20220474).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1600189/full#supplementary-material
References
1. Wu H, Chiou J. Potential benefits of probiotics and prebiotics for coronary heart disease and stroke. Nutrients. (2021) 13(8):2878. doi: 10.3390/nu13082878
2. Akbari T, Al-Lamee R. Percutaneous coronary intervention in multi-vessel disease. Cardiovasc Revasc Med. (2022) 44:80–91. doi: 10.1016/j.carrev.2022.06.254
3. Peng Y, Jiang Y, Zhou Q, Jia Z, Tang H. SGK1 contributes to ferroptosis in coronary heart disease through the NEDD4l/NF-κB pathway. J Mol Cell Cardiol. (2024) 196:71–83. doi: 10.1016/j.yjmcc.2024.09.001
4. Bae JW, Woo SI, Lee J, Park S-D, Kwon SW, Choi SH, et al. Mhealth interventions for lifestyle and risk factor modification in coronary heart disease: randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9(9):e29928. doi: 10.2196/29928
5. Mallah MA, Soomro T, Ali M, Noreen S, Khatoon N, Kafle A, et al. Cigarette smoking and air pollution exposure and their effects on cardiovascular diseases. Front Public Health. (2023) 11:967047. doi: 10.3389/fpubh.2023.967047
6. Zhao J, Fan H, Wang T, Yu B, Mao S, Wang X, et al. Tyg index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients. Cardiovasc Diabetol. (2022) 21(1):123. doi: 10.1186/s12933-022-01548-y
7. Tao S, Tang X, Yu L, Li L, Zhang G, Zhang L, et al. Prognosis of coronary heart disease after percutaneous coronary intervention: a bibliometric analysis over the period 2004–2022. Eur J Med Res. (2023) 28(1):311. doi: 10.1186/s40001-023-01220-5
8. He W, Xu C, Wang X, Lei J, Qiu Q, Hu Y, et al. Development and validation of a risk prediction nomogram for in-stent restenosis in patients undergoing percutaneous coronary intervention. BMC Cardiovasc Disord. (2021) 21(1):435. doi: 10.1186/s12872-021-02255-4
9. Alfonso F, Kastrati A. Clinical burden and implications of coronary interventions for in-stent restenosis. EuroIntervention. (2021) 17(5):e355–7. doi: 10.4244/EIJV17I5A60
10. Chai Z, Fan Y, Gong X, Zhang Y, Hu Y, Li X, et al. Adherence to phase I cardiac rehabilitation in post-PCI patients: a latent class analysis. Front Cardiovasc Med. (2025) 12:1460855. doi: 10.3389/fcvm.2025.1460855
11. Dangas GD, Claessen BE, Caixeta A, Sanidas EA, Mintz GS, Mehran R. In-stent restenosis in the drug-eluting stent era. J Am Coll Cardiol. (2010) 56(23):1897–907. doi: 10.1016/j.jacc.2010.07.028
12. Alfonso F, Coughlan JJ, Giacoppo D, Kastrati A, Byrne RA. Management of in-stent restenosis. EuroIntervention. (2022) 18(2):e103–23. doi: 10.4244/EIJ-D-21-01034
13. Moussa ID, Mohananey D, Saucedo J, Stone GW, Yeh RW, Kennedy KF, et al. Trends and outcomes of restenosis after coronary stent implantation in the United States. J Am Coll Cardiol. (2020) 76(13):1521–31. doi: 10.1016/j.jacc.2020.08.002
14. Fiedler KA, Maeng M, Mehilli J, Schulz-Schüpke S, Byrne RA, Sibbing D, et al. Duration of triple therapy in patients requiring oral anticoagulation after drug-eluting stent implantation: the ISAR-TRIPLE trial. J Am Coll Cardiol. (2015) 65(16):1619–29. doi: 10.1016/j.jacc.2015.02.050
15. Thomas R, Braganza A, Oommen LM, Muliyil J. Confidence with confidence intervals. Indian J Ophthalmol. (1997) 45(2):119–23.9475032
16. Ziyad M, Shah ST, Rauf MA, Shah SM, Ullah S, Ullah R, et al. Evaluating drug-eluting balloons versus stenting for provisional bifurcation lesions: short-term outcomes and future directions. Cureus. (2025) 17(2):e78436. doi: 10.7759/cureus.78436
17. Lin MJ, Lin HD, Cai CZ, Chuang M-J, Yang F-C, Chiang KF, et al. Effect of statin on long-term outcomes in persistent tobacco users receiving percutaneous coronary intervention: a longitudinal, retrospective cohort study. Medicine (Baltimore). (2024) 103(45):e40463. doi: 10.1097/MD.0000000000040463
18. Lampropoulos K, Megalou A, Bazoukis G, Tse G, Manolis A. Pre-loading therapy with statins in patients with angina and acute coronary syndromes undergoing PCI. J Interv Cardiol. (2017) 30(6):507–13. doi: 10.1111/joic.12421
19. Mugo P, Jeilan M, Msunza M, Orwa J, Ngunga M. Incidence of bleeding and performance of the PRECISE-DAPT score in predicting bleeding in patients on dual antiplatelet therapy after treatment for acute coronary syndrome in Kenya. BMC Cardiovasc Disord. (2025) 25(1):137. doi: 10.1186/s12872-024-04434-5
20. Wang D, Wang P, Zhang R, Xi X. Efficacy and safety of Xuefu Zhuyu decoction combined with Western medicine for angina pectoris in coronary heart disease: a protocol for systematic review and meta-analysis. Medicine (Baltimore). (2020) 99(50):e23195. doi: 10.1097/MD.0000000000023195
21. Zhao JN, Zhang Y, Lan X, Chen Y, Li J, Zhang P, et al. Efficacy and safety of Xinnaoning capsule in treating chronic stable angina (qi stagnation and blood stasis syndrome): study protocol for a multicenter, randomized, double-blind, placebo-controlled trial. Medicine (Baltimore). (2019) 98(31):e16539. doi: 10.1097/MD.0000000000016539
22. Hou Y, Li X, Wang X, Dong T, Yang J. The effect of Huoxue Huayu decoction on restenosis after percutaneous coronary intervention in patients with coronary heart disease: a protocol for systematic review and meta-analysis. Medicine (Baltimore). (2022) 101(4):e28677. doi: 10.1097/MD.0000000000028677
23. Liu D, Zeng Y, Liang P, Jiang Y, An S, Ren P. Efficacy and safety of Xuefu Zhuyu Granules combined with western medicine in the treatment of angina pectoris of coronary heart disease: a study protocol of a randomized, double-blind, placebo-controlled clinical trial. Medicine (Baltimore). (2022) 101(43):e31235. doi: 10.1097/MD.0000000000031235
24. Zheng GH, Liu JP, Chu JF, Mei L, Chen HY. Xiongshao for restenosis after percutaneous coronary intervention in patients with coronary heart disease. Cochrane Database Syst Rev. (2013) 2013(5):CD009581. doi: 10.1002/14651858.CD009581.pub2
25. Du WT, Liu P. Treatment of atherosclerosis from the perspective of deficiency syndrome. Shanghai J Tradit Chin Med. (2016) 50(6):18–21.
26. Leng B, Tang F, Lu M, Zhang Z, Wang H, Zhang Y. Astragaloside IV improves vascular endothelial dysfunction by inhibiting the TLR4/NF-κB signaling pathway. Life Sci. (2018) 209:111–21. doi: 10.1016/j.lfs.2018.07.053
27. Meng P, Yang R, Jiang F, Guo J, Lu X, Yang T, et al. Molecular mechanism of astragaloside IV in improving endothelial dysfunction of cardiovascular diseases mediated by oxidative stress. Oxid Med Cell Longev. (2021) 2021:1481236. doi: 10.1155/2021/1481236
28. State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effect of Diseases and Syndromes in Traditional Chinese Medicine (ZY/T 001.1-1994). Beijing: China Standard Press (1994).
29. Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonnell M, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. (1995) 25(2):333–41. doi: 10.1016/0735-1097(94)00397-9
30. Dou L, Mao Z, Fu Q, Chen G, Li S. Health-related quality of life and its influencing factors in patients with coronary heart disease in China. Patient Prefer Adherence. (2022) 16:781–95. doi: 10.2147/PPA.S347681
31. Baktashian M, Saffar Soflaei S, Kosari N, Salehi M, Khosravi A, Ahmadinejad M, et al. Association of high level of hs-CRP with in-stent restenosis: a case-control study. Cardiovasc Revasc Med. (2019) 20(7):583–7. doi: 10.1016/j.carrev.2018.08.015
32. Wang P, Kuang Y, Liu Y, Zhang Y, Gao H, Ma Q. Levels of plasma Quaking and cyclooxygenase-2 predict in-stent restenosis in patients with coronary artery disease after percutaneous coronary intervention. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2022) 47(6):739–47. English, Chinese. doi: 10.11817/j.issn.1672-7347.2022.210716
33. Alexandrescu DM, Mitu O, Costache II, Macovei L, Mitu I, Alexandrescu A, et al. Risk factors associated with intra-stent restenosis after percutaneous coronary intervention. Exp Ther Med. (2021) 22(4):1141. doi: 10.3892/etm.2021.10575
34. Huang S, Yu LJ, Sun GF, Zhang ZX. Short-term predictive value of sST2 in patients with STEMI following primary PCI: a prospective observational study. BMC Cardiovasc Disord. (2025) 25(1):21. doi: 10.1186/s12872-025-04488-z
35. Zhang TY, Chen HL, Shi Y, Jin Y, Zhang Y, Chen Y. The relationship between system inflammation response index and coronary heart disease: a cross-sectional study (NHANES 2007–2016). Front Cardiovasc Med. (2024) 11:1439913. doi: 10.3389/fcvm.2024.1439913
36. Lee MS, Banka G. In-stent restenosis. Interv Cardiol Clin. (2016) 5(2):211–20. doi: 10.1016/j.iccl.2015.12.006
37. Donisan T, Madanat L, Balanescu DV, Mertens A, Dixon S. Drug-eluting stent restenosis: modern approach to a classic challenge. Curr Cardiol Rev. (2023) 19(3):e030123212355. doi: 10.2174/1573403X19666230103154638
38. Li Y, Li Y, Li B, Liu Y, Zhang J, Kuang W, et al. Antiplatelet therapy with integrated traditional Chinese and western medicine for use in myocardial ischemia-reperfusion injury: a review of clinical applications and mechanisms. Evid Based Complement Alternat Med. (2021) 2021:7409094. doi: 10.1155/2021/7409094
39. Xiao S, Lina W, Jianpeng HU, Limiao Z, Jin W. Effect of naoluoxintong formula and its split prescriptions on cerebral vascular regeneration in rats with the cerebral ischemia-reperfusion. J Tradit Chin Med. (2023) 43(6):1140–9. doi: 10.19852/j.cnki.jtcm.20221230.001
40. Mao C, Fu XH, Yuan JQ, Yang ZY, Chung VC, Qin Y, et al. Tong-xin-luo capsule for patients with coronary heart disease after percutaneous coronary intervention. Cochrane Database Syst Rev. (2015) 2015(5):CD010237. doi: 10.1002/14651858.CD010237.pub2
41. Huang S, Chen J, Liu X, Xing C, Zhao L, Chan K, et al. Evaluation of the pharmaceutical activities of Chuanxiong, a key medicinal material in traditional Chinese medicine. Pharmaceuticals (Basel). (2024) 17(9):1157. doi: 10.3390/ph17091157
42. Ren S, Zhang H, Mu Y, Sun M, Liu P. Pharmacological effects of Astragaloside IV: a literature review. J Tradit Chin Med. (2013) 33(3):413–6. doi: 10.1016/s0254-6272(13)60189-2
43. Chen Z, Gao X, Jiao Y, Qiu Y, Wang A, Yu M, et al. Tanshinone IIA exerts anti-inflammatory and immune-regulating effects on vulnerable atherosclerotic plaque partially via the TLR4/MyD88/NF-κB signal pathway. Front Pharmacol. (2019) 10:850. doi: 10.3389/fphar.2019.00850
44. Zhang H, Tang W, Wang S, Zhang J, Fan X. Tetramethylpyrazine inhibits platelet adhesion and inflammatory response in vascular endothelial cells by inhibiting P38 MAPK and NF-κB signaling pathways. Inflammation. (2020) 43:286–97. doi: 10.1007/s10753-019-01119-6
45. An C, Xu ZY. Regulatory mechanism of vascular smooth muscle cell phenotype switch in aortic disease: an update. Second Mil Med Univ J. (2016) 37(8):992–5.
46. Dai J, Qiu L, Lu Y, Li M. Recent advances of traditional Chinese medicine against cardiovascular disease: overview and potential mechanisms. Front Endocrinol (Lausanne). (2024) 15:1366285. doi: 10.3389/fendo.2024.1366285
47. Wu HL, Wang YF, Li JZ, Zhang M-Z, Sheng X-G, Wang X, et al. A multicentre randomized clinical trial on efficacy and safety of huxin formula in patients undergoing percutaneous coronary intervention. Evid Based Complement Alternat Med. (2014) 2014:143064. doi: 10.1155/2014/143064
48. Sun Z, Zhong D, Zhang J, Wang Q, Li C, Yuan T, et al. Tongxinshu capsules in the treatment of stable angina pectoris due to qi deficiency and blood stasis in coronary heart disease: a multicenter, randomized, double-blind, placebo-controlled trial. J Ethnopharmacol. (2025) 343:119437. doi: 10.1016/j.jep.2025.119437
49. Zhu W, Wang S, Zhang L, Xie F-Q, Cheng J, Li X-K, et al. Efficacy and safety of Tongxin formula after stent implantation for acute coronary syndrome: a multicenter, double-blind, placebo-controlled randomized trial. Explore (NY). (2024) 20(5):102992. doi: 10.1016/j.explore.2024.02.010
50. Lu C, Li H, Wang X, Song L, Zhao J, Liu Y. Investigating the mechanism of Chinese medicine formula AACO against chronic heart failure by network pharmacology analysis and experimental validation. Altern Ther Health Med. (2024) 30(11):354–68.38430163
51. Zhao P, Su G, Xiao X, Hao E, Zhu X, Ren J. Chinese medicinal herb Radix Astragali suppresses cardiac contractile dysfunction and inflammation in a rat model of autoimmune myocarditis. Toxicol Lett. (2008) 182(1–3):29–35. doi: 10.1016/j.toxlet.2008.08.002
52. Wu Y, Li T, Li P, Peng H, Gao A, Wang J, et al. Effects of Shenmai injection against chronic heart failure: a meta-analysis and systematic review of preclinical and clinical studies. Front Pharmacol. (2023) 14:1338975. doi: 10.3389/fphar.2023.1338975
53. Shen Q, Chen W, Wang W, Kang S, Du Y, Shi J, et al. Drug interactions between traditional Chinese medicines and cardiovascular drugs. Eur J Drug Metab Pharmacokinet. (2024) 49(5):559–82. doi: 10.1007/s13318-024-00905-4
54. Li JJ, Ren Y, Chen KJ, Yeung AC, Xu B, Ruan XM, et al. Impact of C-reactive protein on in-stent restenosis: a meta-analysis. Tex Heart Inst J. (2010) 37(1):49–57.20200627
55. Guo J, Gao Y, Ahmed M, Dong P, Gao Y, Gong Z, et al. Serum homocysteine level predictive capability for severity of restenosis post percutaneous coronary intervention. Front Pharmacol. (2022) 13:816059. doi: 10.3389/fphar.2022.816059
Keywords: Yiqi Huoxue Tongluo decoction, conventional medicine therapy, percutaneous coronary intervention (PCI), restenosis (RS), Seattle Angina Questionnaire, cardiac function indexes
Citation: Zhao X, Zhang L and Liu Z (2025) Yiqi Huoxue Tongluo decoction combined with conventional medicine therapy: effects on restenosis rates and clinical efficacy in patients with coronary heart disease undergoing percutaneous coronary intervention. Front. Cardiovasc. Med. 12:1600189. doi: 10.3389/fcvm.2025.1600189
Received: 26 March 2025; Accepted: 16 July 2025;
Published: 22 September 2025.
Edited by:
Ilia Fishbein, University of Pennsylvania, United StatesReviewed by:
Ke Liu, Sichuan University, ChinaTian Song, China Academy of Chinese Medical Sciences, China
Copyright: © 2025 Zhao, Zhang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhijie Liu, aGRzenh5eWx6akAxNjMuY29t
 Xing Zhao1
Xing Zhao1 Zhijie Liu
Zhijie Liu