- Department of Cardiology, Daqing Oilfield General Hospital, Daqing, Heilongjiang, China
Objective: To explore the effect of folic acid and vitamin B12 plus rosuvastatin in treating coronary heart disease (CHD) complicated with hyperlipidemia.
Methods: One hundred CHD patients combined with hyperlipidemia admitted to our hospital from January 2022 to December 2023 were separated into study group as well as control group. The control group accepted rosuvastatin calcium tablets. The study group received rosuvastatin plus folic acid and vitamin B12. The cardiac function, blood lipid, plasma Hcy, folate and vitamin B12 levels, inflammation, clinical effect along with occurrence of adverse reactions were compared in 2 groups.
Results: Compared to before therapy, LVEDD and LVESD levels were declined while LVEF level was elevated in 2 groups after therapy, TC, TG and LDL-C levels were declined while HDL-C level was elevated in 2 groups after therapy, plasma Hcy level was declined while folate and vitamin B12 levels were elevated in 2 groups after therapy, and IL-6, TNF-α along with CRP levels were declined in 2 groups after therapy. Compared to control group, the improvements of the above cardiac function indicators, blood lipid indexes, plasma Hcy, folate and vitamin B12 levels, serum inflammatory markers in the study group were more apparent, the total effective rate in the study group presented better. No difference was seen in the occurrence of adverse reactions between 2 groups.
Conclusion: Folic acid and vitamin B12 plus rosuvastatin can effectively improve cardiac function, blood lipid, inflammatory response, and has high safety in treating CHD complicated with hyperlipidemia.
Introduction
Hyperlipidemia refers to a condition where the levels of cholesterol, triglycerides, phospholipids and non-free fatty acids in the blood are higher than the normal range (1). It is one of the most common types of lipid metabolism disorders in clinical practice, and it is a major risk factor for coronary artery disease, with a hereditary component (2). As a chronic inflammatory disease caused by abnormal lipid metabolism, the global incidence and mortality rate of coronary heart disease (CHD) continue to rise (3). By 2021, the number of CHD in China had reached 11.39 million (4). Studies have shown that hyperlipidemia increases the risk of developing CHD (5). Clinically, the combination of CHD and hyperlipidemia is quite common. The condition is more severe, the course of the disease is longer, and the quality of life of the patients is lower, which will affect the compliance with treatment (6).
Statins are the main drugs in the treatment of CHD complicated with hyperlipidemia (7). Rosuvastatin calcium is a newly developed statin that can reduce low-density lipoprotein cholesterol (LDL-C) and total cholesterol (TC) and prevent the occurrence and development of CHD (8). Rosuvastatin calcium specifically represses 3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase, delays or prevents the development of atherosclerosis, and can reduce certain inflammatory factors (9). However, the effect of simple use of this drug is limited, and the long-term curative effect is not ideal (10).
Folic acid and vitamin B12 are essential micronutrients during human growth and development. They are involved in the normal development of nerves, blood vessels, and cells, as well as the maintenance of their functions (11). The absence of these two factors and metabolic abnormalities are risk factors for many diseases. Metabolic abnormalities can lead to the accumulation of precursor substances such as cysteine and methylmalonic acid, which disrupt the stability of blood vessels and nerves and cause impaired cellular function (12).
In our study, we aimed to explore the effect of folic acid and vitamin B12 plus rosuvastatin in treating CHD complicated with hyperlipidemia.
Materials and methods
General data
This was a randomized controlled trial. One hundred CHD patients combined with hyperlipidemia admitted to our hospital from January 2022 to December 2023 were chosen and randomly separated into study group (n = 50) as well as control group (n = 50). Inclusion criteria: (1) Patients met the diagnostic criteria of CHD combined with hyperlipidemia; (2) The clinical data of the patients were complete; (3) Informed consent forms were signed by patients and their families. Exclusion criteria: (1) Patients with abnormal liver function and renal function; (2) Patients with malignant tumors; (3) Patients with autoimmune disease, stroke, cognitive impairment, or other serious medical conditions; (4) Patients with allergic reactions to the drugs used in this study; (5) Patients who had taken hormones or other drugs that could affect the results of this study within the month prior to this study; (6) Patients who withdrew from the study halfway; (7) Patients who did not comply with the treatment. This study was approved by the Ethics committee of Daqing Oilfield General Hospital (Ethical Approval Number: 20220111A). Ethical approval covered all operational procedures and complied with the provisions of the Helsinki Declaration. Informed consent was obtained from all participants prior to their inclusion in the study. Our study has been registered with the Chinese Clinical Trial Registry (ChiCTR), with trial registration number ChiCTR2300072425.
Sample size
Sample size was calculated using G*Power software (13). Assuming P-value for significant of less than 0.05 (two-tailed) and the power of 0.80, the calculated sample size was 100, with 50 cases in each group.
Randomization and blinding
The patients were randomly assigned to each group in a 1:1 ratio, and this was achieved through computer-generated random numbers. The random allocation table was prepared by a statistician, and this process did not involve any participation of the research team. No stratification factors were used. The research team received a list of blind, sequential packaging identification numbers, and after being included in the study, the patients would be sequentially assigned to the next packaging number on the list. This study was double-blind, and all researchers and patients kept the allocation of groups confidential.
Treatment methods
The control group took rosuvastatin calcium tablets (Nanjing Zhengda Tianqing Pharmaceutical Co., LTD.) orally, 10 mg each time, once a day.
The study group took rosuvastatin plus folic acid and vitamin B12. The usage of rosuvastatin calcium tablets was the same as the control group. Besides, patients took folic acid (Hangzhou Aoyipollen Pharmaceutical Co., LTD.) orally, 0.4 mg/time, once/day. At the same time, patients took vitamin B12 (Xi'an Disai Biological Pharmaceutical Co., LTD.) orally, 25 μg/time, 3 times/day. The dosages of folic acid and vitamin B12 were adopted according to the standards stipulated in clinical guidelines.
Both groups accepted treatment for 3 months.
Observation indicators
(1) Cardiac function indicators: Left ventricular ejection fraction (LVEF), left ventricular end diastolic diameter (LVEDD) along with left ventricular end systolic diameter (LVESD) were tested by echocardiography.
(2) Blood lipid index: Serum levels of TC, triglyceride (TG), high density lipoprotein cholesterol (HDL-C) and LDL-C were tested by automatic biochemical analyzer.
(3) Plasma homocysteine (Hcy), folate and vitamin B12 levels: Automatic biochemical analyzer was implemented to detect the Hcy level, and an automatic chemiluminescence instrument was used to detect the folic acid and vitamin B12 levels.
(4) Serum inflammatory markers: Serum levels of interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α) along with C-reactive protein (CRP) were tested by enzyme-linked immunosorbent assay.
(5) Clinical effect: After the treatment, the frequency of angina pectoris attacks decreased by more than 75%, the NYHA cardiac function classification improved by 2 levels or more, the TC decreased by ≥20% and the TG decreased by ≥40%, which was markedly improved; After treatment, the frequency of angina pectoris attacks decreased by 50%-75%, the NYHA cardiac function classification improved by 1 level, the TC decreased by 10%-20% and the TG decreased by 20%-40%, which was effective; After the treatment, the frequency of angina pectoris attacks decreased by less than 50%, the NYHA cardiac function classification did not improve, the TC showed a decrease of less than 10% and the TG showed a decrease of less than 20%, which was ineffective. Total effective rate = (number of markedly improved cases + number of effective cases)/Total number of cases ×100%.
(6) The occurrence of adverse reactions (nausea and vomiting, gastrointestinal discomfort, dizziness, and palpitation) was recorded.
Statistical analysis
SPSS 24.0 statistical software was adopted for data analysis. Measurement data were expressed as (x ± s), and t-test was adopted for comparison. Count data were expressed as (n, %), and χ2 test was adopted for comparison. P < 0.05 meant statistical significance.
Results
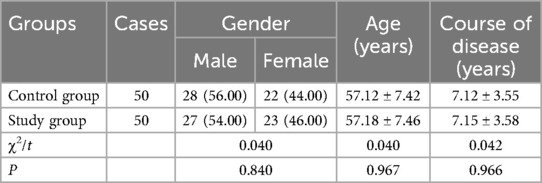
General data of patients in 2 groups
No difference was discovered in general data between 2 groups (P > 0.05, Table 1).
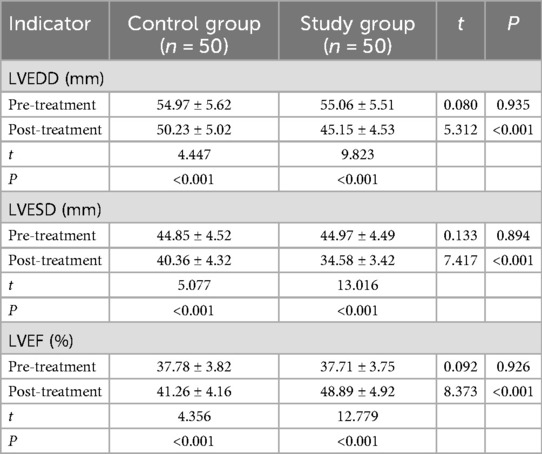
Cardiac function indicators in 2 groups
Compared to before therapy, LVEDD and LVESD levels were declined while LVEF level was elevated in 2 groups after therapy (P < 0.001). Compared to control group, the improvements of the above cardiac function indicators in the study group were more significant (P < 0.001, Table 2).
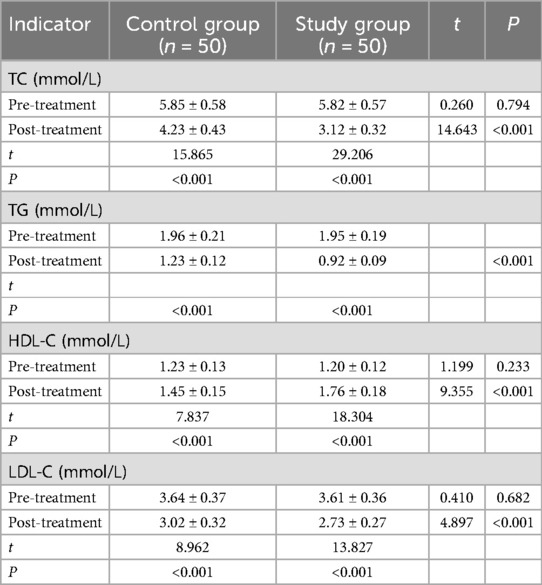
Blood lipid indexes in 2 groups
Compared to before therapy, TC, TG and LDL-C levels were declined while HDL-C level was elevated in 2 groups after therapy (P < 0.001). Compared to control group, the improvements of the above blood lipid indexes in the study group were more significant (P < 0.001, Table 3).
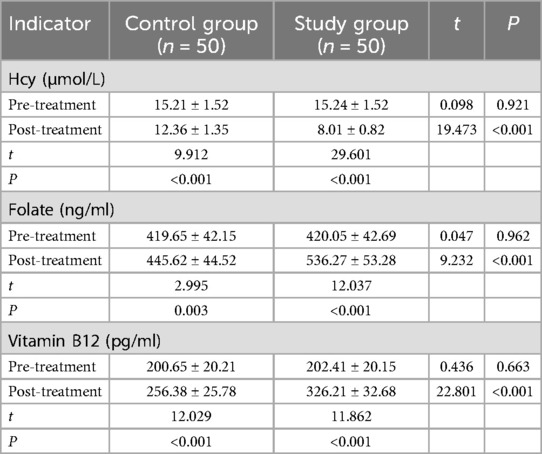
Plasma Hcy, folate and vitamin B12 levels in 2 groups
Compared to before therapy, plasma Hcy level was declined while folate along with vitamin B12 levels were elevated in 2 groups after therapy (P < 0.001 and P = 0.003). Compared to control group, the improvements of plasma Hcy, folate along with vitamin B12 levels in the study group were more significant (P < 0.001, Table 4).
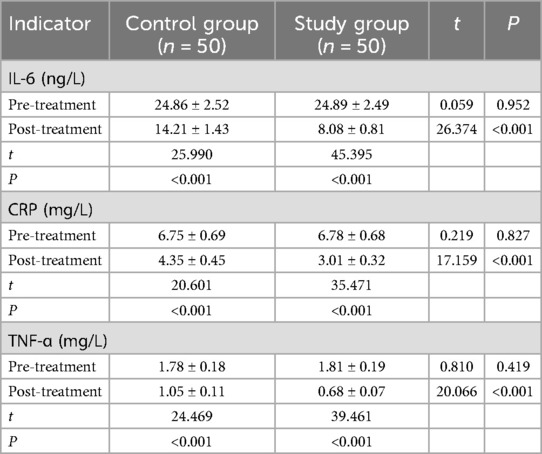
Serum inflammatory markers in 2 groups
Compared to before therapy, IL-6, TNF-α along with CRP levels were declined in 2 groups after therapy (P < 0.001). Compared to control group, the reduction of the above serum inflammatory markers in the study group were more significant (P < 0.001, Table 5).
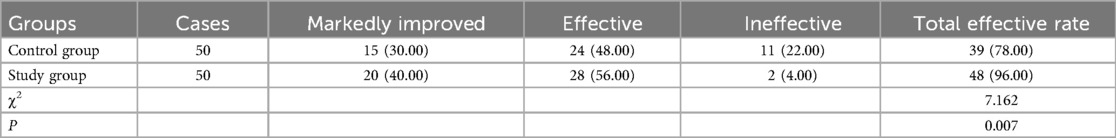
Clinical effect in 2 groups
Relative to control group, the total effective rate in the study group was better (P = 0.007, Table 6).
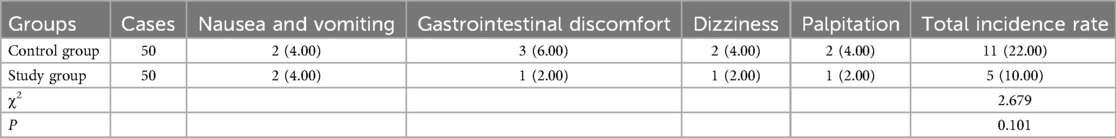
Occurrence of adverse reactions in 2 groups
No difference was seen in the occurrence of adverse reactions between 2 groups (P = 0.101, Table 7).
Discussion
Recently, with the continuous growth of the population in our country, the incidence of CHD has also been increasing year by year (14). Dyslipidemia is the main risk factor of CHD (15). Chronic dyslipidemia can damage vascular endothelial cells through a variety of mechanisms, resulting in cardiovascular lipid infiltration, which leads to atherosclerosis (16). Statins can effectively promote the clearance of cholesterol in cells, and are commonly used in clinical routine drugs to treat dyslipidemia (17). Rosuvastatin is a selective reductase inhibitor that acts mainly on the liver of patients and enables the presence of polar methylsulfonamidos in its molecules (18). However, the effect of this single drug is not ideal, and relevant experts believe that the combined use of drugs can effectively enhance the overall treatment outcome (19).
As a sulfur-containing amino acid and an intermediate product of methionine, Hcy is mainly derived from dietary methionine (20). Numerous studies have validated that the elevated serum Hcy level is an independent risk factor for various cardiovascular diseases (21). High serum Hcy level causes direct or indirect damage to vascular endothelial cells, resulting in increased secretion of endothelin by endothelial cells, thus affecting the balance of nitric oxide and endothelin, leading to atherosclerosis (22). Besides, Hcy can also cause endothelial cell damage through oxidative stress response, lead to proliferation of vascular smooth muscle cells, induce platelet aggregation and adhesion, and promote thrombosis (23).
Folic acid and vitamin B12 are both important substances involved in methionine cycle in human Hcy metabolism (24). The traditional view holds that a deficiency in folic acid and vitamin B12 can lead to a significant accumulation of Hcy in the body, which in turn can cause cardiovascular diseases; while appropriate supplementation of folic acid and vitamin B12 can exert cardiovascular protective effects by reducing Hcy levels (25). However, recent studies have found that folic acid and vitamin B12 may be important risk factors for CHD that are independent of Hcy, However, the specific mechanism of their effects is not yet fully understood. This might be related to the dysfunction of vascular endothelial cells caused by folate deficiency. For instance, folate deficiency can increase the inflammatory response of cells, while the production of nitric oxide will increase the risk of cardiovascular diseases (26).
In our study, the results suggested that relative to control group, the improvements of LVEDD, LVESD and LVEF levels in the study group were more significant, suggesting that folic acid and vitamin B12 plus rosuvastatin could improve the cardiac function in treating CHD complicated with hyperlipidemia. The reason is that vitamin B12 and folic acid both belong to the B group of vitamins. They can participate in the synthesis process of methionine and thymine, and can transfer the methyl group from methyl tetrahydrofolate to methyl donors such as Hcy to form methyl Hcy, which reduces the level of Hcy in the blood, thereby avoiding the damage to endothelial function caused by high Hcy, delaying or even reversing the process of atherosclerosis, and improving cardiac function (27). Consistently, Dkhillon et al. demonstrated that the intake of folic acid and vitamin B could decrease the heart rate and increase LVEF in patients diagnosed with chronic heart failure (27).
Our study also revealed that compared to control group, the improvements of TC, TG, HDL-C along with LDL-C levels in the study group were more significant, implying that folic acid and vitamin B12 plus rosuvastatin could improve the blood lipid in treating CHD complicated with hyperlipidemia. Besides, our study indicated that compared to control group, the improvements of plasma Hcy, folate along with vitamin B12 levels in the study group were more significant. The reason is that the content of folic acid and vitamin B12 is negatively correlated with the content of Hcy. When the content of Hcy decreases, the content of folic acid increases. This further enhances the effect of modifying liposomes and inhibiting oxidative stress, thereby improving the lipid abnormality conditions of patients (28). Likewise, Fogacci et al. discovered that folic acid supplementation may improve plasma lipid levels as well as reduce the risk of cerebrovascular disease (29). Boachie et al. suggested that low vitamin B12 increased fatty acid synthesis and levels of individual fatty acids, and decreased fatty acid oxidation and mitochondrial respiration, thus resulting in dysregulation of lipid metabolism (30).
Moreover, our study indicated that compared to control group, the reduction of IL-6, TNF-α as well as CRP levels in the study group were more significant, reflecting that folic acid and vitamin B12 plus rosuvastatin could improve the inflammatory response in treating CHD complicated with hyperlipidemia. The reason is that after folic acid and vitamin B12 enter the body, they inhibit the body's oxidative stress response, promote the restoration of balance and stability of the body's own system, and thereby reduce the release of inflammatory factors such as IL-6 and TNF-α, and alleviate inflammatory damage (31). Similarly, Chen et al. pointed that folic acid and vitamin B12 supplementation could reduce the inflammatory cytokine levels in patients with Alzheimer's disease (11). In addition, our study indicated that relative to the control group, the total effective rate in the study group presented better, which was also supported by previous reports (32, 33). At the same time, no difference was seen in the occurrence of adverse reactions between 2 groups, indicating the safety of the combination use of folic acid, vitamin B12 and rosuvastatin in treating CHD complicated with hyperlipidemia.
There are some limitations of our study. First, the sample size is relatively small (n = 100 total), which may limit the generalizability and statistical power for detecting less common adverse events or subtle differences. Second, the study duration of 3 months is relatively short for assessing long-term clinical outcomes, such as cardiovascular events or mortality. Furthermore, there are some potential interfering factors (such as factors related to diet or lifestyle) that were not controlled in our study. Therefore, more large-scale and long-term studies should be conducted in the future to further verify our findings.
In conclusion, our study demonstrates that folic acid and vitamin B12 plus rosuvastatin may effectively improve cardiac function, blood lipid, inflammatory response, and has high safety in treating CHD complicated with hyperlipidemia.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by Ethics Committee of Daqing Oilfield General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HW: Writing – original draft, Writing – review & editing. TW: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lai M, Peng H, Wu X, Chen X, Wang B, Su X. IL-38 in modulating hyperlipidemia and its related cardiovascular diseases. Int Immunopharmacol. (2022) 108:108876. doi: 10.1016/j.intimp.2022.108876
2. Yao YS, Li TD, Zeng ZH. Mechanisms underlying direct actions of hyperlipidemia on myocardium: an updated review. Lipids Health Dis. (2020) 19(1):23. doi: 10.1186/s12944-019-1171-8
3. Jiesisibieke ZL, Panter J, Wang M, Au Yeung SL, Luo S, Jang H, et al. Mode of transport, genetic susceptibility, and incidence of coronary heart disease. Int J Behav Nutr Phys Act. (2023) 20(1):79. doi: 10.1186/s12966-023-01484-4
4. Mi Y, Xue Z, Qu S, Yin Y, Huang J, Kou R, et al. The economic burden of coronary heart disease in mainland China. Public Health. (2023) 224:140–51. doi: 10.1016/j.puhe.2023.08.034
5. Alloubani A, Nimer R, Samara R. Relationship between hyperlipidemia, cardiovascular disease and stroke: a systematic review. Curr Cardiol Rev. (2021) 17(6):e051121189015. doi: 10.2174/1573403X16999201210200342
6. Zeng Y, Zhao J, Zhang J, Yao T, Weng J, Yuan M, et al. Development of a nomogram that predicts the risk of coronary heart disease in patients with hyperlipidemia. J Cardiovasc Pharmacol Ther. (2023) 28:10742484231167754. doi: 10.1177/10742484231167754
7. Hong SJ, Lee YJ, Lee SJ, Hong BK, Kang WC, Lee JY, et al. Treat-to-target or high-intensity statin in patients with coronary artery disease: a randomized clinical trial. JAMA. (2023) 329(13):1078–87. doi: 10.1001/jama.2023.2487
8. Zheng H, Li H, Wang Y, Li Z, Hu B, Li X, et al. Rosuvastatin slows progression of carotid intima-Media thickness: the METEOR-China randomized controlled study. Stroke. (2022) 53(10):3004–13. doi: 10.1161/STROKEAHA.120.031877
9. Lee YJ, Hong SJ, Kang WC, Hong BK, Lee JY, Lee JB, et al. Rosuvastatin versus atorvastatin treatment in adults with coronary artery disease: secondary analysis of the randomised LODESTAR trial. Br Med J. (2023) 383:e075837.
10. Moon JS, Park IR, Kim SS, Kim HS, Kim NH, Kim SG, et al. The efficacy and safety of moderate-intensity rosuvastatin with ezetimibe versus high-intensity rosuvastatin in high atherosclerotic cardiovascular disease risk patients with type 2 diabetes Mellitus: a randomized, multicenter, open, parallel, phase 4 study. Diabetes Metab J. (2023) 47(6):818–25.38043782
11. Chen H, Liu S, Ge B, Zhou D, Li M, Li W, et al. Effects of folic acid and vitamin B12 supplementation on cognitive impairment and inflammation in patients with Alzheimer’s disease: a randomized, single-blinded, placebo-controlled trial. J Prev Alzheimers Dis. (2021) 8(3):249–56.34101780
12. Lee CY, Chan L, Hu CJ, Hong CT, Chen JH. Role of vitamin B12 and folic acid in treatment of Alzheimer’s disease: a meta-analysis of randomized control trials. Aging (Albany NY). (2024) 16(9):7856–69.38700503
13. Kang H. Sample size determination and power analysis using the G*power software. J Educ Eval Health Prof. (2021) 18:17.34325496
14. Zaitsu M, Ishimaru T, Tsushima S, Muramatsu K, Ando H, Nagata T, et al. Incidence of coronary heart disease among remote workers: a nationwide web-based cohort study. Sci Rep. (2024) 14(1):8415.38600223
16. Bonaca MP, Hamburg NM, Creager MA. Contemporary medical management of peripheral artery disease. Circ Res. (2021) 128(12):1868–84.34110910
18. Bowman CM, Ma F, Mao J, Chen Y. Examination of physiologically-based pharmacokinetic models of rosuvastatin. CPT Pharmacometrics Syst Pharmacol. (2021) 10(1):5–17.33220025
19. Kim MC, Ahn Y, Kim MH, Kim SY, Hong TJ, Rhee MY, et al. A randomized, multicenter, double-blind, placebo-controlled study to evaluate the efficacy and safety of a quadruple combination of amlodipine, losartan, rosuvastatin, and ezetimibe in patients with concomitant essential hypertension and dyslipidemia. Am J Cardiovasc Drugs. (2023) 23(4):441–54.37395974
20. Yuan D, Chu J, Lin H, Zhu G, Qian J, Yu Y, et al. Mechanism of homocysteine-mediated endothelial injury and its consequences for atherosclerosis. Front Cardiovasc Med. (2022) 9:1109445.36727029
21. Kaplan P, Tatarkova Z, Sivonova MK, Racay P, Lehotsky J. Homocysteine and mitochondria in cardiovascular and cerebrovascular systems. Int J Mol Sci. (2020) 21(20):7698.33080955
22. Wei F, Ding Y, Ou J, Chen X, Li L, Zhou Q, et al. Accurate detection of Hcy in human serum and two-photon visualization of atherosclerosis using a highly specific fluorescent probe. Anal Chem. (2023) 95(24):9173–81.37279018
23. Paradkar MU, Padate B, Shah SAV, Vora H, Ashavaid TF. Association of genetic variants with hyperhomocysteinemia in Indian patients with thrombosis. Indian J Clin Biochem. (2020) 35(4):465–73.33013017
24. Tripathi M, Singh BK, Zhou J, Tikno K, Widjaja A, Sandireddy R, et al. Vitamin B(12) and folate decrease inflammation and fibrosis in NASH by preventing syntaxin 17 homocysteinylation. J Hepatol. (2022) 77(5):1246–55.35820507
25. Levy J, Rodriguez-Guéant RM, Oussalah A, Jeannesson E, Wahl D, Ziuly S, et al. Cardiovascular manifestations of intermediate and major hyperhomocysteinemia due to vitamin B12 and folate deficiency and/or inherited disorders of one-carbon metabolism: a 3.5-year retrospective cross-sectional study of consecutive patients. Am J Clin Nutr. (2021) 113(5):1157–67.33693455
26. Liu Y, Geng T, Wan Z, Lu Q, Zhang X, Qiu Z, et al. Associations of Serum folate and vitamin B12 levels with cardiovascular disease mortality among patients with type 2 diabetes. JAMA Netw Open. (2022) 5(1):e2146124.35099545
27. Dkhillon D, Samogulova A, Kolobov B. B vitamins as adjunctive treatment for chronic heart failure. Cardiovasc Hematol Disord Drug Targets. (2023) 23(1):64–71.37464830
28. Liu M, Wang Z, Liu S, Liu Y, Ma Y, Liu Y, et al. Effect of B vitamins supplementation on cardio-metabolic factors in patients with stable coronary artery disease: a randomized double-blind trial. Asia Pac J Clin Nutr. (2020) 29(2):245–52.32674231
29. Fogacci F, Pizzi C, Bergamaschi L, Di Micoli V, Cicero AFG. Folic acid and plasma lipids: interactions and effect of folate supplementation. Curr Probl Cardiol. (2024) 49(6):102539.38521293
30. Boachie J, Adaikalakoteswari A, Gázquez A, Zammit V, Larqué E, Saravanan P. Vitamin B12 induces hepatic fatty infiltration through altered fatty acid metabolism. Cell Physiol Biochem. (2021) 55(3):241–55.33961354
31. Cheng M, Liang X, Shi L, Zhang Q, Zhang L, Gong Z, et al. Folic acid deficiency exacerbates the inflammatory response of astrocytes after ischemia-reperfusion by enhancing the interaction between IL-6 and JAK-1/pSTAT3. CNS Neurosci Ther. (2023) 29(6):1537–46.36794521
32. Mathew AR, Di Matteo G, La Rosa P, Barbati SA, Mannina L, Moreno S, et al. Vitamin B12 deficiency and the nervous system: beyond metabolic decompensation-comparing biological models and gaining new insights into molecular and cellular mechanisms. Int J Mol Sci. (2024) 25(1):590.38203763
Keywords: coronary heart disease, hyperlipidemia, folic acid, vitamin B12, rosuvastatin, cardiac function, blood lipid
Citation: Wang H and Wang T (2025) Effect of folic acid and vitamin B12 plus rosuvastatin in the treatment of coronary heart disease combined with hyperlipidemia. Front. Cardiovasc. Med. 12:1604862. doi: 10.3389/fcvm.2025.1604862
Received: 15 April 2025; Accepted: 4 June 2025;
Published: 30 July 2025.
Edited by:
Qianman Peng, Harvard Medical School, United StatesReviewed by:
Neven M. Sarhan, Misr International University, EgyptAhmed Qasim Mohammed Alhatemi, Thi Qar University, Iraq
Copyright: © 2025 Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tiezheng Wang, MTM5MzY3NTgyODBAMTYzLmNvbQ==
 Hao Wang
Hao Wang Tiezheng Wang
Tiezheng Wang