Abstract
Background:
Contrast-induced nephropathy (CIN) is a risk in angiographic procedures, especially for patients with acute kidney injury (AKI). To mitigate this risk, ultra-low contrast percutaneous coronary intervention (ULC-PCI) has been developed, which minimizes the use of contrast agents.
Case summary:
A 54-year-old woman with a history of AKI from a prior percutaneous coronary intervention (PCI) was found to have coronary artery disease with three vessels disease and chronic total occlusion in the right coronary artery. To minimize contrast use, she underwent ultra-low contrast PCI using the “microcatheter injection” technique, with only 5 cc of contrast used during the procedure. At one-year follow-up, the patient's LVEF improved from 33% to 56%, symptoms resolved with no chest pain. Her estimated glomerular filtration rate (eGFR) showed no significant decrease, since serum creatinine increased slightly from 1.59 mg/dl to 1.61 mg/dl. and eGFR decreased from 39 to 38 ml/min/1.73 m2 in 72 h.
Conclusions:
The microcatheter injection technique may serve as a viable strategy for percutaneous coronary intervention (PCI) in patients with eGFR < 30 ml/min/1.73 m2 or history of contrast-induced nephropathy.
1 Introduction
Contrast-induced nephropathy (CIN) is a potential complication associated with the use of iodinated contrast agents in angiographic procedures, particularly among patients with acute kidney injury. To mitigate this risk, ultra-low contrast percutaneous coronary intervention (ULC-PCI) has been developed, which minimizes or eliminates the use of contrast agents. Critical procedural steps, including catheter engagement, vessel wiring, and stent deployment, are performed using contrast-free techniques (1, 2). We utilized a microcatheter selective injection technique using ultra low contrast that facilitates ULC-PCI. This case report outlines the microcatheter injection technique that renders ULC-PCI feasible in these patients.
2 Case illustration
A 54-year-old female patient with hypertension, diabetes, and menopause as risk factors for coronary artery disease came to the outpatient clinic. Her chief complaint was chest pain during physical activity. The patient had history of acute kidney injury from previous PCI. Physical examination showed blood pressure of 133/71 mmHg, heart rate of 67 bpm, and oxygen saturation of 98%. The patient exhibited no fever, signs of heart failure, or bronchospasm. ECG revealed inverted T waves at V4-V6, I, aVL, and echocardiography showed mild mitral regurgitation, mild tricuspid regurgitation, akinesia at basal-apical of inferior and basal-mid of inferolateral segments; other segments were hypokinetic, with LVEF 33% and tricuspid annular plane systolic excursion of 15 mm. Even though the echocardiogram revealed akinesia in the inferior and infero-lateral walls, another imaging test was not considered to assess viability due to administration problems.
Coronary angiography from previous hospitalization showed three-vessel coronary artery disease involving the left main artery, along with a chronic total occlusion (CTO) of the right coronary artery (RCA). Laboratory examination showed a decrease in renal function with serum creatinine of 1.59 mg/dl and an eGFR of 39 ml/min/1.73 m2. The patient had been discussed in a surgical conference and was scheduled for coronary artery bypass grafting. However, intra-aortic balloon pump support was not available. As the patient continued to experience refractory chest pain, we proceeded with percutaneous coronary intervention (PCI) by implanting two drug-eluting stents (DES) in the left anterior descending artery, which was identified as the initial culprit lesion. Due to presence of chest pain despite anti-anginal treatment with carvedilol 12.5 mg b.i.d and nitrokaf retard 5 mg b.i.d., we also decided for PCI of RCA CTO.
We opted for treatment using ultra-low contrast PCI with “microcatheter injection” technique to address the presence of chronic total occlusion (CTO) and minimize contrast use (see Figure 1a). Right coronary artery (RCA) cannulation was performed using a Judkins Right 3.5/7F catheter, assisted by Finecross 1.8F microcatheter. The microcatheter was placed prior to the lesion before contrast injection. We injected 10–20 ml of 0.9% saline through the catheter and the amplitude of the T-wave inversion increased. Then, runthrough NS floppy coronary wire was inserted. A hand injection of 0.5 cc of contrast confirmed total occlusion in the proximal segment (see Figure 1b). The coronary wire was anchored to the conus branch. Subsequently, an escalation wire (Fielder XT), was utilized to penetrate the lesion and was positioned distally with the backup microcatheter. After removing the wire, another hand injection of 0.5 cc of contrast was performed to verify that the microcatheter was within the RCA lumen (see Figures 1c,d). Predilatation was conducted multiple times with Sapphire balloons measuring 2.0 × 15 mm and 3.0 × 15 mm, advancing from the proximal to the distal segment.
Figure 1
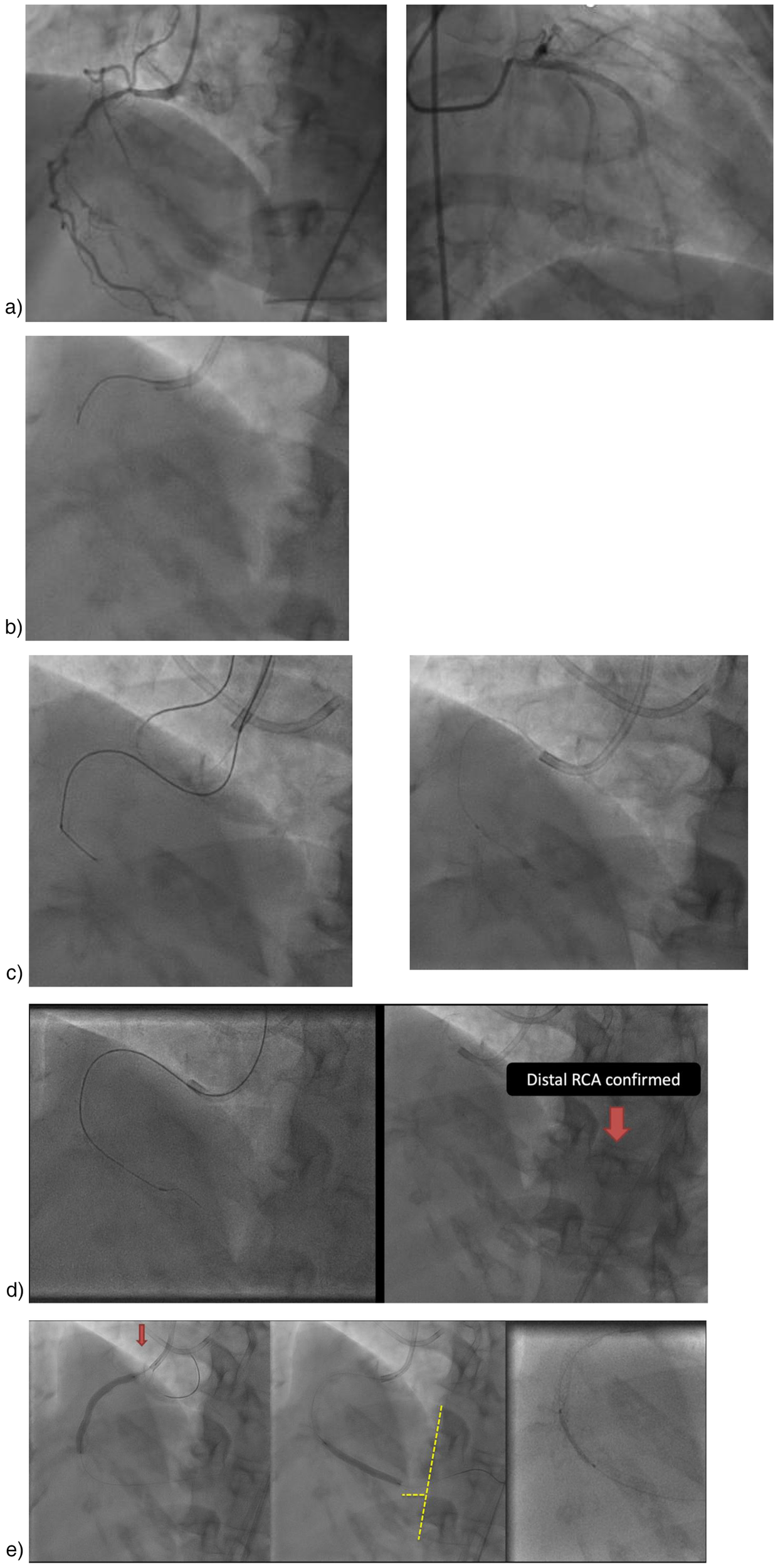
Ultra-Low contrast PCI with microcatheter injection. (a) Initial angiography (3 months earlier), (b) Cannulation and then using saline 10–20 cc and 0.5 cc contrast, (c) A Judkins left catheter can be seen in addition to the right catheter, used to confirm the position of the contralateral wire, if needed. Injections were only made through the right microcatheter. Wiring using Fielder XTA, and confirmed with 0.5 cc contrast for confirmation stump, (d) Micro tip injection, (e) Stent placement.
An anatomical marking technique was employed for the placement of both the distal and proximal landing zones. For the distal landing zone we utilized vertebrae as landmarks, while the proximal landing zone was guided by positioning an additional wire in the conus, allowing precise identification of the ostial location. A drug-eluting stent (DES) Promus Premiere 3.5 × 38 mm was implanted from the ostium to the mid segment, followed by the implantation of a mid to distal DES Xience Xpedition 3.0 × 38 mm. Balloon measurement was performed to ascertain the length of the DES in the mid region by evaluating the gap between the previously placed stents. Subsequently, a third DES Promus Premiere 3.5 × 16 mm was implanted in the mid-right coronary artery (RCA) (see Figure 1E). Angiographic evaluation was conducted using a hand injection of 0.5 cc of contrast (Figure 2), with the total contrast volume utilized during the procedure being only 5 cc. At one-year follow-up, our patient demonstrated a significant improvement in left ventricular ejection fraction (LVEF), increasing from 33% to 56%. Additionally, her symptoms resolved, with no reported chest pain. This patient showed no AKI. There was no significant decline in renal function, as the serum creatinine increased only slightly from 1.59 to 1.61 mg/dl and the estimated glomerular filtration rate (eGFR) decreased minimally from 39 to 38 ml/min/1.73 m2 over 72 h.
Figure 2
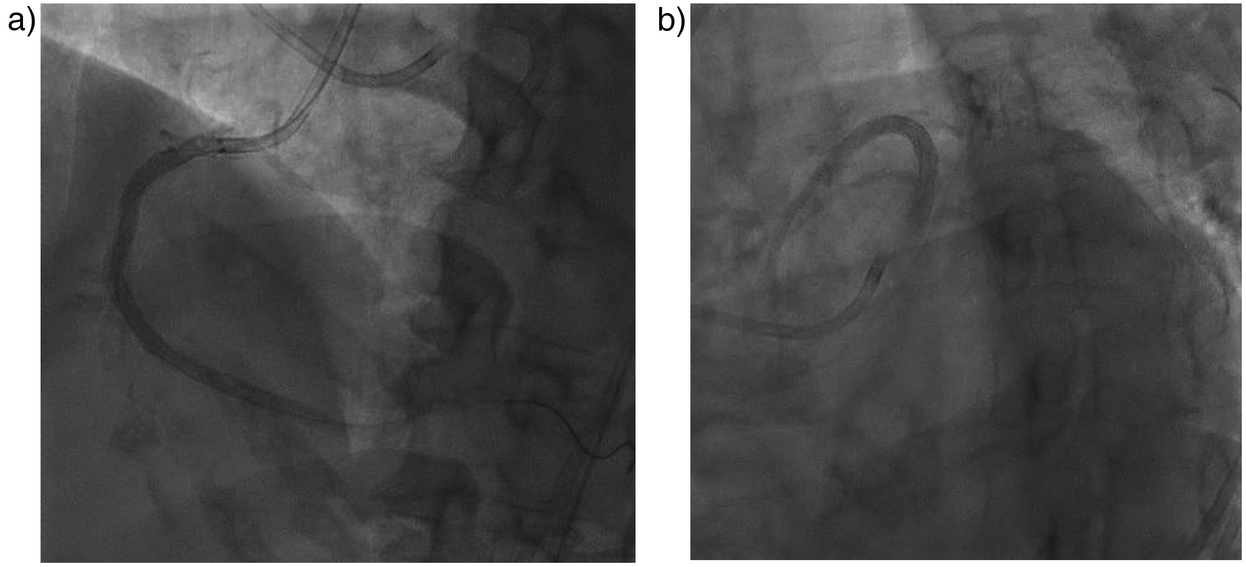
Post PCI angiography evaluation. (a) RCA stent and (b) LAD stent were in good position.
3 Discussions
Percutaneous coronary intervention (PCI) is a well-established and widely utilized treatment for coronary artery disease (CAD) (3, 4). However, one major concern is the risk of CIN (1). We calculated the Mehran score for this patient, identifying key risk factors such as diabetes, an eGFR of 39 ml/min/1.73 m2, and the use of 5 cc contrast. The patient's Mehran score was determined to be 7 points, corresponding to a 14% risk of post-PCI contrast-induced nephropathy (CIN) and a 0.12% risk of requiring dialysis due to post-PCI CIN (5).
The CONSaVE-AKI study (2022) (6) demonstrated a significantly higher incidence of contrast-induced acute kidney injury (CI-AKI) in patients undergoing conventional percutaneous coronary intervention (PCI) compared to those treated with the ultra-low contrast PCI (ULC-PCI) approach [17.1% vs. 0%; p = 0.012]. The volume of contrast used was substantially lower in the ULC-PCI group (41.02 ± 9.8 ml vs. 112.54 ± 25.18 ml; p < 0.0001). Key findings from the study include: (1) a significantly lower rate of CI-AKI in the ULC-PCI group, (2) successful implementation of the ULC-PCI protocol regardless of lesion complexity, (3) comparable safety and efficacy between ULC-PCI and conventional PCI, with no differences in secondary safety outcomes, and (4) in patients with acute coronary syndrome and pre-existing renal dysfunction, PCI was associated with improvement in glomerular filtration rate (GFR).
Ultra-low contrast percutaneous coronary intervention (ULC-PCI), defined as a contrast volume-to-estimated glomerular filtration rate (eGFR) ratio of less than 1, was initially proposed for patients with chronic kidney disease (CKD) who are at elevated risk of contrast-induced nephropathy (CIN) (1). The first pivotal study evaluating the feasibility of this approach was conducted by Ali et al. (7), involving 31 patients with advanced CKD. Subsequently, Rozenbaum et al. (8) performed ULC-angiography in 30 patients, followed by ULC-PCI, without intravascular ultrasound (IVUS), in 16 of them. None of the patients developed contrast-induced acute kidney injury (CI-AKI), marking these studies as the first to demonstrate both the feasibility and cardiovascular safety of ULC-PCI.
3.1 Catheter engagement without contrast administration
Studies have demonstrated that intravascular ultrasound (IVUS) not only reduces contrast volume but also lowers the risk of contrast-induced nephropathy (CIN), making it particularly valuable for patients with renal impairment. IVUS-guided percutaneous coronary intervention enables more accurate lesion assessment and optimal stent deployment, which has been consistently associated with lower rates of target lesion failure and stent-related complications. By highlighting these dual benefits, enhanced procedural safety and improved long-term outcomes, IVUS emerges as an essential tool in modern interventional cardiology practice (9, 10).
In ULC angiography, the use of smaller catheters without side holes (5–6 Fr) is recommended to maximize vessel opacification (2). Techniques to minimize contrast include utilizing coronary calcium to confirm catheter engagement. In a study conducted by Kim et al., 0.9% saline or 5% dextrose was injected into the left coronary artery prior to assessing heart rate, QT interval, and T-wave amplitude. The administration of 10–20 ml of 0.9% saline through the catheter allowed for confirmation of appropriate catheter positioning, as evidenced by T-wave inversion or augmentation, along with accompanying ST-segment depression or elevation (9). For diagnostic angiography, using minimal projections and specific angles is essential for optimal visualization. While diluted contrast allows for more imaging runs, it may reduce luminal opacification. Increasing frame rates can help enhance coronary anatomy visualization (3, 4).
We performed ULC-PCI using a microcatheter, balloon catheter measurement to determine the appropriate length for drug-eluting stent (DES) implantation, and final angiographic assessment with hand-injected contrast. An algorithm was developed to guide technique selection in ULC-PCI(see Figure 3). Patients with an eGFR below 30 ml/min/1.73 m2 or a history of contrast-induced nephropathy (CIN) or acute kidney injury (AKI) were prioritized for this approach. Total occlusion dictated the use of microcatheter injection, while its absence led to further assessment of lesion location. If the lesion was ostial or required precise stenting, live-guided IVUS was preferred. Anatomical landmarks or wire branching were used for landing zone identification. Marking the wire served as the fundamental technique, though various methods were combined as needed during the procedure.
Figure 3
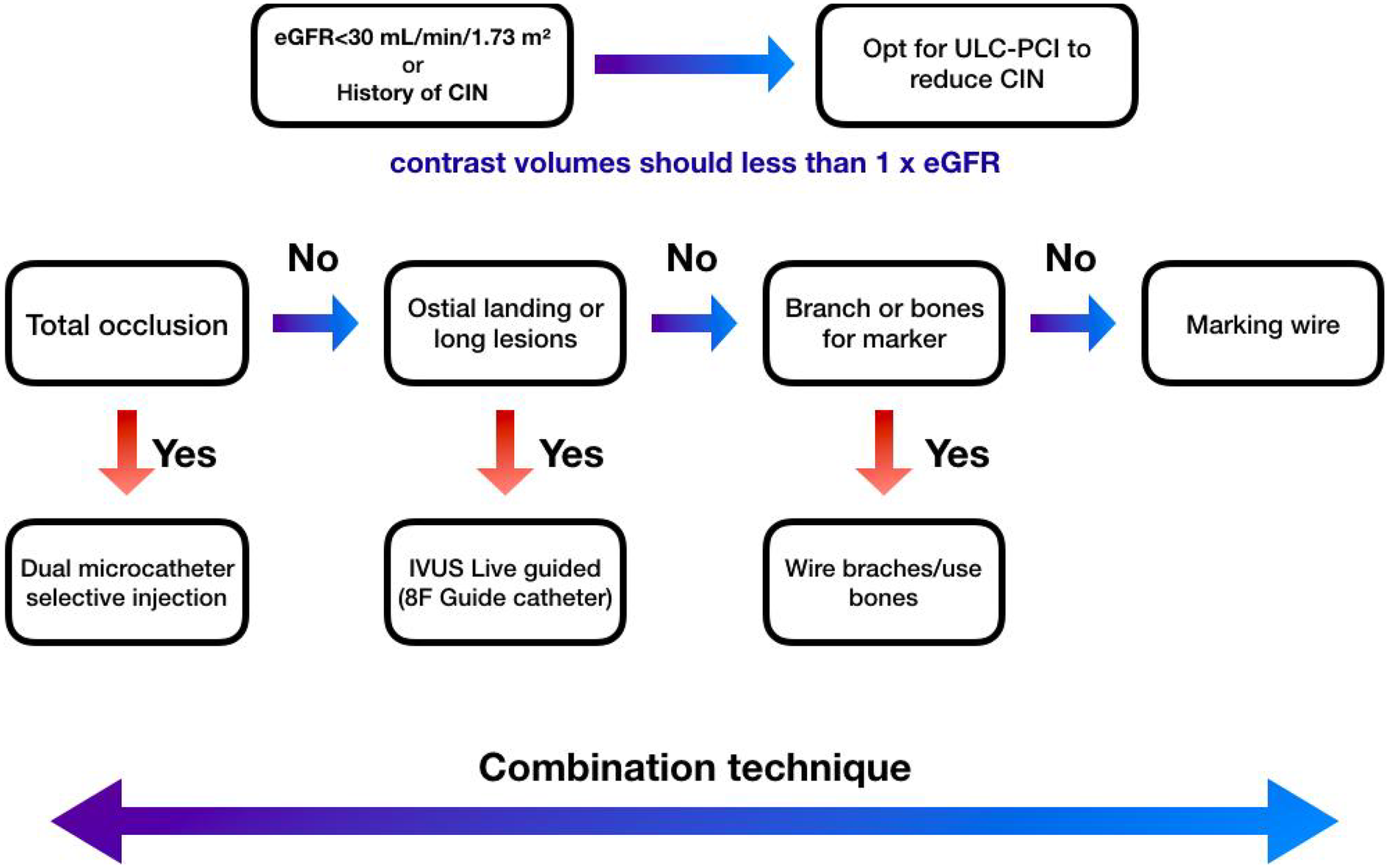
Mangkuanom's algorithm of ultra low-dose contrast percutaneous coronary intervention technique. In patients with an eGFR <30 ml/min/1.73 m2 or history of CIN, we opt for an ultra-low contrast percutaneous coronary intervention (PCI) strategy, adhering to the widely accepted definition of ultra-low contrast PCI as a contrast volume-to-eGFR ratio of less than 1. This approach is specifically indicated for individuals with advanced chronic kidney disease who are at heightened risk of developing post-procedural contrast-induced nephropathy (CIN). Notes: eGFR, estimated Glomerular Filtration Rate; IVUS, intravascular ultrasound; ULC-PCI, ultra low-dose contrast percutaneous coronary intervention.
4 Conclusions
The microcatheter injection technique may represent a feasible and effective strategy for percutaneous coronary intervention (PCI) in patients with acute kidney injury. By enabling revascularization with minimal use of contrast medium, this approach can achieve favorable outcomes while reducing the risk of procedure-related complications.
Statements
Data availability statement
The datasets presented in this article are not readily available because of ethical and privacy restrictions. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the National Cardiovascular Center Harapan Kita. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AM: Conceptualization, Writing – review & editing, Writing – original draft. RS: Writing – review & editing, Writing – original draft. BM: Supervision, Writing – review & editing, Writing – original draft. DF: Writing – review & editing, Writing – original draft. NI: Writing – review & editing, Writing – original draft. AA: Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We would like to thank those who have supported us in the making of this study. We are especially grateful to the Department of Cardiology and Vascular Medicine, Faculty of Medicine Universitas Indonesia, as well as reviewers and editor, for their guidance and assistance in teaching the authors and for proof-reading this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Hennessey B Shabbir A Travieso A Gonzalo N Escaned J . Procedural and technological innovations facilitating ultra-low contrast percutaneous coronary interventions. Interv Cardiol. (2023) 18:e09. 10.15420/icr.2022.32
2.
Mariani J Jr Guedes C Soares P Zalc S Campos CM Lopes AC et al Intravascular ultrasound guidance to minimize the use of iodine contrast in percutaneous coronary intervention: the MOZART (minimizing cOntrast utiliZation with IVUS guidance in coRonary angioplasTy) randomized controlled trial. JACC Cardiovasc Interv. (2014) 7(11):1287–93. 10.1016/j.jcin.2014.05.024
3.
Virani SS Newby LK Arnold SV Bittner V Brewer LC Demeter SH et al 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. (2023) 82(9):833–955. 10.1016/j.jacc.2023.04.003Erratum in: J Am Coll Cardiol. 2023 Oct 31;82(18):1808. doi: 10.1016/j.jacc.2023.09.794. Erratum in: J Am Coll Cardiol. 2024 Apr 30;83(17):1716. doi: 10.1016/j.jacc.2024.03.399.
4.
Vrints C Andreotti F Koskinas KC Rossello X Adamo M Ainslie J et al ESC Scientific document group. 2024 ESC guidelines for the management of chronic coronary syndromes. Eur Heart J. (2024) 45(36):3415–37. 10.1093/eurheartj/ehae177. Erratum in: Eur Heart J. (2025) 46(16):1565. doi: 10.1093/eurheartj/ehaf079
5.
Guo Y Xu X Xue Y Zhao C Zhang X Cai H . Mehran 2 contrast-associated acute kidney injury risk score: is it applicable to the Asian percutaneous coronary intervention population?Clin Appl Thromb Hemost. (2022) 28:10760296221116353. 10.1177/10760296221116353
6.
Shrivastava A Nath RK Mahapatra HS Pandit BN Raj A Sharma AK et al Ultra-low CONtraSt PCI vs conVEntional PCI in patients of ACS with increased risk of CI-AKI (CONSaVE-AKI). Indian Heart J. (2022) 74(5):363–8. 10.1016/j.ihj.2022.08.004
7.
Ali ZA Karimi Galougahi K Nazif T Maehara A Hardy MA Cohen DJ et al Imaging-& physiology-guided percutaneous coronary intervention without contrast administration in advanced renal failure: a feasibility, safety, & outcome study. Eur Heart J. (2016) 37(40):3090–e3095. 10.1093/eurheartj/ehw078
8.
Rozenbaum Z Benchetrit S Rozenbaum E Neumark E Mosseri M Pereg D . Ultra-low contrast volume for patients with advanced chronic kidney disease undergoing coronary procedures. Nephron. (2018) 138(4):296–e302. 10.1159/000485648
9.
Kim Y Bae S Johnson TW Son NH Sim DS Hong YJ et al Role of intravascular ultrasound-guided percutaneous coronary intervention in optimizing outcomes in acute myocardial infarction. J Am Heart Assoc. (2022) 11(5):e023481. 10.1161/JAHA.121.023481
10.
Burlacu A Tinica G Brinza C Crisan-Dabija R Popa IV Covic A . Safety and efficacy of Minimum- or zero-contrast IVUS-guided percutaneous coronary interventions in chronic kidney disease patients: a systematic review. J Clin Med. (2021) 10(9):1996. 10.3390/jcm10091996
Summary
Keywords
AKI, case report, chronic total occlusion, low-dose contrast, microcatheter injection, normal saline, percutaneous coronary intervention
Citation
Mangkuanom AS, Satrio R, Mendel B, Firman D, Iryuza N and Alkatiri AA (2025) Microcatheter selective injection technique using ultra low contrast for percutaneous coronary intervention in patients with previous acute kidney injury: a case report. Front. Cardiovasc. Med. 12:1607466. doi: 10.3389/fcvm.2025.1607466
Received
07 April 2025
Accepted
23 June 2025
Published
10 July 2025
Volume
12 - 2025
Edited by
Tommaso Gori, Johannes Gutenberg University Mainz, Germany
Reviewed by
Abhinav Shrivastava, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, India
Federico Vergni, Ospedale Generale Provinciale Macerata, Italy
Updates
Copyright
© 2025 Mangkuanom, Satrio, Mendel, Firman, Iryuza and Alkatiri.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Brian Mendel brianmendel17@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.