- 1Department of Internal Medicine, 21 September University for Medical and Applied Sciences, Sana'a, Yemen
- 2Department of Internal Medicine, Ibn Mussa International Hospital, Al Hodaidah, Yemen
- 3Department of Medicine, College of Medicine and Health Sciences, Sana’a University, Sana'a, Yemen
Background: Hypertension is a major contributor to cardiovascular and renal disease worldwide, particularly in low-resource settings such as Yemen.
Objective: To identify demographic, clinical, and lifestyle-related factors associated with hypertension among heart disease (HD) and kidney disease (KD) patients in Sana'a.
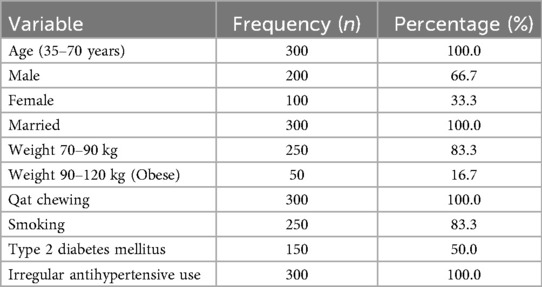
Methods: A cross-sectional study was conducted on 300 patients (200 men, 100 women; aged 35–70 years) between March and August 2024. Data on age, sex, weight, smoking, Qat chewing, diabetes, and antihypertensive medication adherence were collected. Blood pressure was measured using a standardized sphygmomanometer. Logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
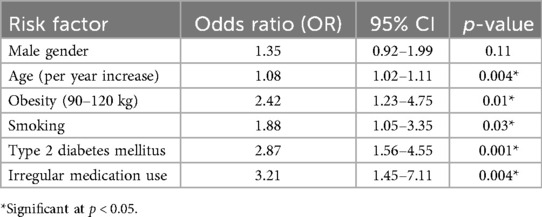
Results: Hypertension was significantly associated with age (OR: 1.08; 95% CI: 1.02–1.11), obesity (OR: 2.42; 95% CI: 1.23–4.75), smoking (OR: 1.88; 95% CI: 1.05–3.35), type 2 diabetes (OR: 2.87; 95% CI: 1.56–4.55), and irregular medication use (OR: 3.21; 95% CI: 1.45–7.11). All participants reported Qat chewing (100%).
Conclusion: Age, obesity, smoking, diabetes, and poor medication adherence are major predictors of hypertension in Yemeni HD and KD patients. The universal irregularity in medication use highlights systemic healthcare gaps. Strategies to improve adherence, promote lifestyle modification, and strengthen healthcare systems are urgently needed.
1 Introduction
Hypertension is one of the most significant risk factors for cardiovascular and renal diseases. In LMICs, including Yemen, limited healthcare infrastructure exacerbates the burden of hypertension. The disease accelerates progression to myocardial infarction, stroke, and end-stage kidney failure, particularly in individuals already suffering from HD or KD (1, 2).
Regional studies have identified obesity, smoking, diabetes, and poor adherence to therapy as key drivers of hypertension (1, 2). In Yemen, widespread Qat chewing further complicates the risk profile, though its precise contribution remains unclear (3).
This study investigates demographic, clinical, and behavioral risk factors for hypertension among Yemeni HD and KD patients (1, 3–5), aiming to inform culturally appropriate prevention and management strategies (6).
2 Methods
2.1 Study design and setting
A cross-sectional study was carried out in hospitals and outpatient clinics in Sana'a, Yemen, between March and August 2024.
2.2 Study population
300 patients with HD, KD, or both were recruited via convenience sampling.
Inclusion criteria:
• Age 35–70 years
• Diagnosed with HD or KD
• Provided informed consent
2.3 Data collection
Structured interviews and medical records were used.
• Demographics: age, sex, marital status
• Clinical data: weight, diabetes, blood pressure
• Lifestyle: smoking, Qat chewing
• Medication adherence: self-reported regular vs. irregular
Blood pressure measurement: Conducted with a calibrated sphygmomanometer, two readings averaged after 5 min rest. Hypertension defined as ≥130/80 mmHg (ACC/AHA 2017).
2.4 Statistical analysis
SPSS v25 was used. Logistic regression assessed associations between risk factors and hypertension. Significance: p < 0.05.
3 Results
3.1 Baseline characteristics
3.2 Logistic regression analysis
4 Discussion
This study demonstrated that age, obesity, smoking, diabetes, and irregular antihypertensive drug use were significant predictors of hypertension (7–9). The 100% prevalence of irregular drug adherence reflects systemic issues in the Yemeni healthcare system (1, 2).
Key findings:
• Age: Vascular stiffening and cumulative exposure to risk factors explain the increased risk.
• Obesity: Strong predictor of hypertension via increased cardiac output and vascular resistance.
• Smoking: Nicotine contributes to endothelial dysfunction and sympathetic activation.
• Diabetes: Insulin resistance and arterial stiffness exacerbate BP rise.
• Medication adherence: The strongest predictor, highlighting systemic deficiencies (9, 10).
Qat chewing: Could not be analyzed statistically due to uniform exposure but remains a critical cultural factor requiring future comparative studies.
Strengths: First study in Yemen on this specific patient population; robust statistical analysis.
Limitations: Cross-sectional design; convenience sampling; lack of control group; inability to analyze Qat chewing due to uniformity.
Implications:
• Improve medication access and adherence programs (10).
• Strengthen public education on lifestyle modification.
• Develop system-level policies for better hypertension management.
5 Conclusion
Hypertension among Yemeni HD and KD patients is significantly associated with age, obesity, smoking, diabetes, and poor medication adherence (11, 12). Addressing these factors through systemic reforms and culturally tailored interventions is essential to reduce the growing cardiovascular and renal burden in Yemen.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ibn Mussa International Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HM: Writing – original draft, Writing – review & editing. MB: Conceptualization, Data curation, Analysis, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Al-Motarreb A, Al-Habori M, Broadley KJ. Khat chewing, cardiovascular diseases and other internal medical problems: the current situation and directions for future research. J Ethnopharmacol. (2010) 132:540–8. doi: 10.1016/j.jep.2010.07.001
2. Bin Dahman L, Al-Awbathani AM, Bawazir AA, Al-Awbathani AS, Alhabshey HA, Saad HO, et al. Prevalence of hypertension and its associated risk factors among adults attending medical outpatient clinics at Ibn Sina general hospital authority in Mukalla city, Yemen. Cureus. (2024) 16(5):e60540. doi: 10.7759/cureus.60540
3. Nawata K. Risk factors for heart, cerebrovascular, and kidney diseases: evaluation of potential side effects of medications to control hypertension, hyperglycemia, and hypercholesterolemia. Front Cardiovasc Med. (2023) 10:1103250. doi: 10.3389/fcvm.2023.1103250
4. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. (2018) 137(2):109–18. doi: 10.1161/CIRCULATIONAHA.117.032582
5. The SPRINT Research Group. Intensive vs. standard BP control. N Engl J Med. (2015) 373:2103–16. doi: 10.1056/NEJMoa1511939
6. International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels: International Diabetes Federation (2021).
7. Alshahrani S. Renin–angiotensin–aldosterone pathway modulators in chronic kidney disease: a comparative review. Front Pharmacol. (2023) 14:1101068. doi: 10.3389/fphar.2023.1101068
8. Reaven G. Insulin resistance, hypertension, and coronary heart disease. J Clin Hypertens (Greenwich). (2003) 5(4):269–74. doi: 10.1111/j.1524-6175.2003.01764.x
9. Eadon MT, Maddatu J, Moe SM, Sinha AD, Ferreira RM, Miller BW, et al. Pharmacogenomics of hypertension in CKD: the CKD-PGX study. Kidney360. (2022) 3(2):307–16. doi: 10.34067/kid.0005362021
10. Zazzara MB, Palmer K, Vetrano DL, Carfì A, Onder G. Adverse drug reactions in older adults: a narrative review of the literature. Eur Geriatr Med. (2021) 12(3):463–73. doi: 10.1007/s41999-021-00481-9. Erratum in: Eur Geriatr Med. 2022 Feb;13(1):307. doi: 10.1007/s41999-021-00591-433738772
Keywords: hypertension, heart disease, kidney disease, risk factors, Yemen, Qat, smoking, medication adherence
Citation: Muafa HM and Balkam MA (2025) A cross-sectional study of risk factors associated with hypertension in heart and kidney disease patients in Sana'a, Yemen. Front. Cardiovasc. Med. 12:1621750. doi: 10.3389/fcvm.2025.1621750
Received: 1 May 2025; Accepted: 7 October 2025;
Published: 24 October 2025.
Edited by:
Chengxing Shen, Shanghai Jiao Tong University, ChinaReviewed by:
Yaman Walid Kassab, National University of Science and Technology (Muscat), OmanRadhwan Hussein, Ninevah University, Iraq
Copyright: © 2025 Muafa and Balkam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hussein Mussa Muafa, aC5tLm11YWZhQDIxdW1hcy5lZHUueWU=
 Hussein Mussa Muafa
Hussein Mussa Muafa Malika Abdu Balkam3
Malika Abdu Balkam3