Abstract
Type A aortic intramural hematoma (IMH) is a variant of acute aortic syndrome, with emergency surgery traditionally considered the treatment of choice. We report a case of a 69-year-old male patient who presented with chest pain. Computed tomography angiography (CTA) revealed type A aortic intramural hematoma. Given the absence of high-risk progression factors, conservative management with close surveillance was selected. During treatment, periaortic hematoma developed in the descending aorta, but the patient's symptoms significantly improved. Follow-up CTA at 3 months demonstrated complete resolution of the intramural hematoma, and the patient remained in good condition at 2.5 years of follow-up. This case demonstrates that conservative treatment may be a viable option for highly selected type A IMH patients without high-risk progression factors, but should only be considered with rigorous patient selection criteria and intensive monitoring protocols in experienced centers.
Introduction
Acute aortic syndrome (AAS) encompasses a group of aortic wall diseases with high mortality and morbidity rates (1). The mechanism of IMH likely involves spontaneous rupture of the vasa vasorum within the aortic media, leading to intramural bleeding without intimal tear.
Type A IMH represents a cardiothoracic emergency requiring surgical evaluation regardless of patient symptoms and clinical stability, due to increased risk of progression to aortic dissection or rupture. Based on findings from the International Registry of Acute Aortic Dissection (IRAD), conservative treatment is not recommended for type A IMH due to mortality rates of approximately 40% (2). However, controversy remains regarding the optimal treatment strategy for type A IMH, particularly considering geographical and ethnic variations. Asian studies demonstrate lower mortality rates with conservative treatment, while Western reports show higher mortality with conservative management. The 2022 ACC/AHA Guidelines recommend immediate open surgery for uncomplicated IMH (Class I recommendation) (3). Similarly, the 2024 EACTS/STS Guidelines state that emergency surgery is recommended for patients with acute type A IMH with complications or high-risk features (Class I recommendation) (4). However, these same guidelines acknowledge that optimal medical therapy and serial imaging may be considered in patients with type A IMH in the absence of high-risk features. This reflects the ongoing controversy regarding optimal treatment strategy for type A IMH.
This report presents a case of type A IMH treated conservatively with follow-up studies demonstrating disease improvement and favorable outcomes.
Case description
A 69-year-old male patient (height 165 cm, weight 55 kg) presented to the emergency department on December 14, 2022, with chest pain. The chest pain was persistent, not relieved by rest, and gradually worsened over time. The patient had no history of hypertension or diabetes mellitus but was a smoker. Physical examination revealed that the patient was alert and conscious with stable vital signs: blood pressure 140/80 mmHg, heart rate 85 beats per minute, respiratory rate 16 breaths per minute, and temperature 36.8°C. Cardiopulmonary and abdominal examinations were unremarkable, and peripheral pulses were symmetric.
Electrocardiography showed sinus rhythm without significant abnormalities. Chest CTA revealed type A aortic intramural hematoma extending from the ascending aorta to the descending aorta. The ascending aortic length was 108 mm, maximum aortic diameter was 42 mm, and hematoma thickness was 7 mm, without associated ulcer-like projection (ULP). The aortic valve was tricuspid without significant aortic regurgitation.
Following multidisciplinary discussion, considering the absence of high-risk progression factors (aortic diameter <50 mm, hematoma thickness <10 mm, no ULP) and the patient's advanced age, conservative treatment was selected. The patient received strict pain control, heart rate and blood pressure control with target systolic blood pressure of 100–120 mmHg and heart rate of 60–80 bpm. Intravenous medications were used for the first three days, then gradually transitioned to oral medications for ongoing control. Strict bed rest was mandatory during hospitalization. The patient was closely monitored during the entire hospital stay. CTA was recommended at 1 weeks, 2 weeks, 1 month, 3 months, 6 months, and then annually.
Follow-up CTA one week after treatment showed resolution of the ascending aortic intramural hematoma, but periaortic hematoma was noted in the descending aorta. The patient's chest pain symptoms significantly improved, and vital signs remained stable. Follow-up aortic CTA at 3 months post-discharge demonstrated complete resolution of the ascending aortic hematoma and complete disappearance of the periaortic hematoma. The patient returned to normal activities, and clinical follow-up at 2.5 years showed continued good clinical condition. The typical CT evolution process is shown in Figure 1.
Figure 1
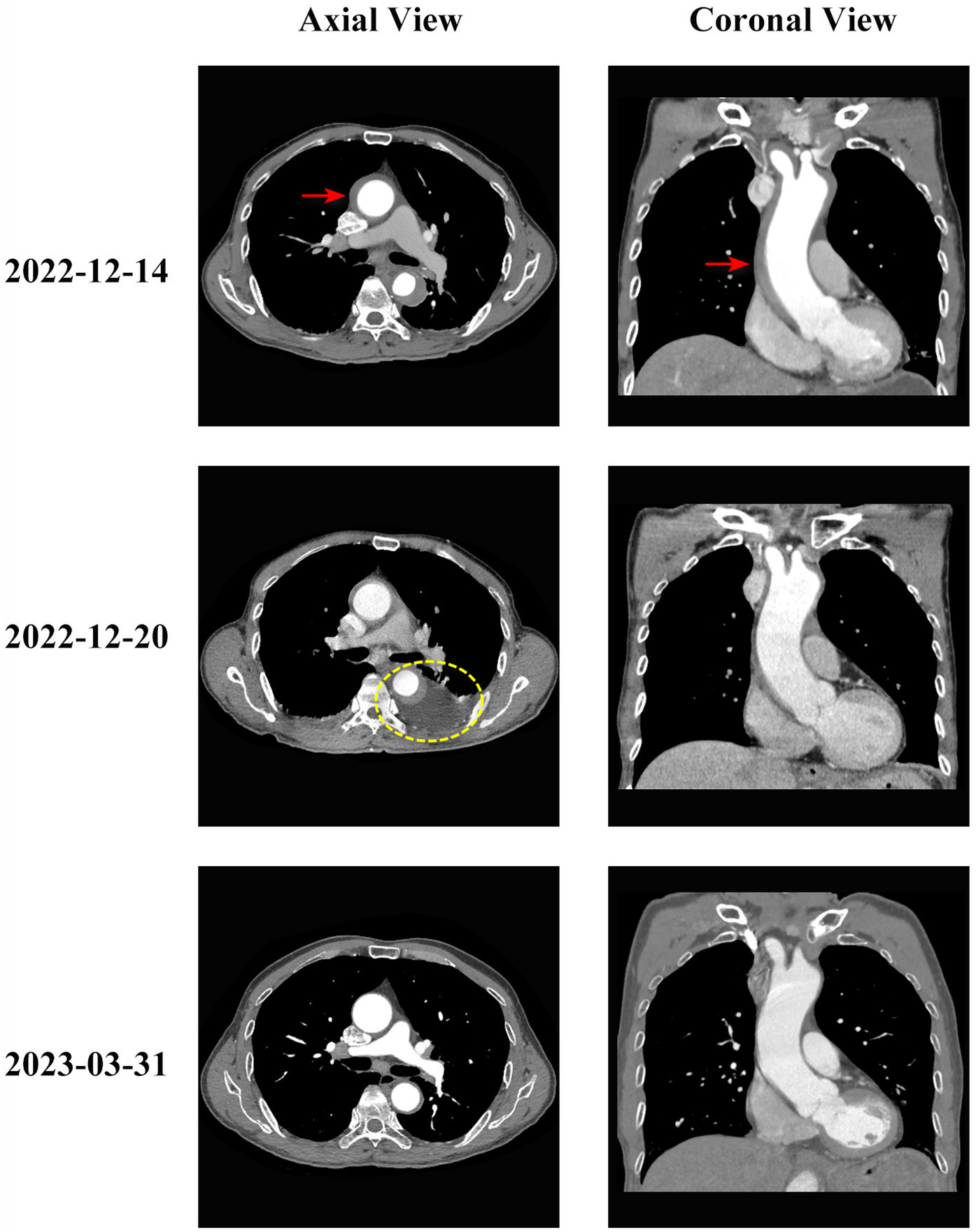
Evolution of type A aortic intramural hematoma during conservative treatment. Serial computed tomography angiography (CTA) images showing the evolution of type A aortic intramural hematoma in axial (left column) and coronal (right column) views. Top row (2022-12-14): Initial presentation showing type A intramural hematoma involving the ascending aorta (red arrows indicate intramural hematoma location) with thickening of the aortic wall (hematoma thickness 7 mm). The ascending aortic diameter measured 42 mm. Middle row (2022-12-20): One weeks after conservative treatment initiation, showing resolution of the ascending aortic intramural hematoma but development of periaortic hematoma around the descending aorta (yellow circle indicates periaortic hematoma). Bottom row (2023-03-31): Three months follow-up demonstrating complete resolution of both the intramural hematoma and periaortic hematoma, with restoration of normal aortic wall appearance. The patient remained asymptomatic throughout the follow-up period.
Discussion
Controversy in type A aortic intramural hematoma treatment
Treatment strategies for type A IMH show significant geographical and ethnic variations. Asian centers, particularly studies from Japan and Korea, demonstrate that conservative treatment can achieve favorable outcomes for patients with hematoma thickness <11 mm and aortic diameter <50 mm, with in-hospital mortality rates <10% (5). In contrast, Western guidelines recommend aggressive surgical treatment, considering that type A IMH behaves similarly to aortic dissection, with conservative treatment mortality rates as high as 40% (1). These study differences likely arise from failure to strictly distinguish between simple and complicated type A hematomas in study inclusion criteria. Additionally, some hematomas may represent the false impression of thrombosed type A dissections. Vigilance regarding this heterogeneity is essential when interpreting results from different studies. Genetic variations and healing responses between ethnic populations might also influence natural history.
Risk factors predicting hematoma progression
Identifying high-risk progression factors is crucial for selecting appropriate treatment strategies. Research indicates that a maximum diameter of the ascending aorta and aortic arch ≥50 mm and hematoma thickness ≥10 mm correlate with mortality in conservative treatment (6). Additionally, ULP, pericardial effusion, uncontrollable chest pain, and hypertension are important factors predicting progression. Our previous research also identified ascending aortic length as a strong risk factor for predicting progression (7).
This 69-year-old patient had no history of diabetes or coronary artery disease, no significant pericardial effusion or valvular disease. The ascending aortic diameter and hematoma thickness were 42 mm and 7 mm, respectively, and CTA revealed no ULP or intimal rupture. Due to the absence of high-risk factors for progression to aortic dissection, conservative treatment was selected. It is crucial to emphasize that the safety and efficacy of conservative management demonstrated in this single case should not be generalized to the broader population of type A IMH patients. This case represents a highly selected patient with specific favorable characteristics. In summary, key factors for successful conservative treatment in this case included: (1) strict blood pressure and heart rate control; (2) close clinical monitoring; (3) timely imaging follow-up; (4) absence of high-risk progression factors in the patient. The combination of these elements ensured treatment safety and effectiveness.
Clinical significance of periaortic hematoma
The unique aspect of this case was the development of periaortic hematoma during conservative treatment. Mukherjee et al. (8) found in the International Registry of Acute Aortic Dissection that periaortic hematoma may be a sign of impending rupture and associated with adverse outcomes. However, these finding lacks confirmation from other centers, and its clinical significance in IMH patients remains unclear. In this case, despite the appearance of periaortic hematoma, the patient's symptoms significantly improved, and subsequent follow-up showed complete hematoma resolution, suggesting that in certain circumstances, periaortic hematoma may not necessarily predict adverse outcomes. This may relate to hematoma size, location, and the patient's overall clinical status. However, this highly unusual favorable outcome should not be interpreted as suggesting that periaortic hematoma is benign or that conservative management is appropriate when this finding develops. More evidence is warranted.
Conclusion
This case report demonstrates that for type A aortic intramural hematoma patients without high-risk progression factors, conservative treatment is a viable therapeutic option under strict blood pressure and heart rate control with close clinical and imaging surveillance. This experience provides important reference for individualized treatment of type A IMH, but additional clinical studies are needed to validate the safety and effectiveness of conservative treatment.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by IRB of Guangdong Provincial People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JW: Supervision, Conceptualization, Validation, Methodology, Investigation, Data curation, Funding acquisition, Resources, Writing – review & editing, Software, Visualization, Project administration, Writing – original draft, Formal analysis. JS: Writing – original draft, Writing – review & editing. JL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Natural Science Foundation of China (82200518), Outstanding Young Talent Trainee Program of Guangdong Provincial People’s Hospital (KY012023331), and Guangdong Provincial Research Institutes Stability Support Project (KD022025216). The funders had no role in study design, data collection, data analysis, data interpretation, and the writing of the report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Sorber R Hicks CW . Diagnosis and management of acute aortic syndromes: dissection, penetrating aortic ulcer, and intramural hematoma. Curr Cardiol Rep. (2022) 24(3):209–16. 10.1007/s11886-022-01642-3
2.
Harris KM Braverman AC Eagle KA Woznicki EM Pyeritz RE Myrmel T et al Acute aortic intramural hematoma. Circulation. (2012) 126(11_suppl_1):S91–6. 10.1161/CIRCULATIONAHA.111.084541
3.
Isselbacher EM Preventza O Hamilton Black J III Augoustides JG Beck AW Bolen MA et al 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American heart association/American college of cardiology joint committee on clinical practice guidelines. Circulation. (2022) 146(24):e334–482. 10.1161/CIR.0000000000001106
4.
Czerny M Grabenwoeger M Berger T Aboyans V Della Corte A Chen EP et al EACTS/STS guidelines for diagnosing and treating acute and chronic syndromes of the aortic organ. Ann Thorac Surg. (2024) 118(1):5–115. 10.1016/j.athoracsur.2024.01.021
5.
Song JK Yim JH Ahn JM Kim DH Kang JW Lee TY et al Outcomes of patients with acute type a aortic intramural hematoma. Circulation. (2009) 120(20):2046–52. 10.1161/CIRCULATIONAHA.109.879783
6.
Ogino H . Uncomplicated type A intramural hematoma: surgery or conservative approach?-conservative approach. Ann Cardiothorac Surg. (2019) 8(5):558–60. 10.21037/acs.2019.06.10
7.
Chen Z Wu J Liu J Song J Qiu H Zhuang J . Ascending aortic length predicts adverse outcomes in type A intramural haematoma. Eur J Cardiothorac Surg. (2024) 66(4):ezae386. 10.1093/ejcts/ezae386
8.
Mukherjee D Evangelista A Nienaber CA Sechtem U Suzuki T Trimarchi S et al Implications of periaortic hematoma in patients with acute aortic dissection (from the international registry of acute aortic dissection). Am J Cardiol. (2005) 96(12):1734–8. 10.1016/j.amjcard.2005.07.098
Summary
Keywords
acute aortic syndrome, aortic intramural hematoma, conservative treatment, case report, aorta, ascending aorta
Citation
Wu J, Song J and Liu J (2025) Successful conservative treatment of type A aortic intramural hematoma with typical CT evolution: a case report. Front. Cardiovasc. Med. 12:1648753. doi: 10.3389/fcvm.2025.1648753
Received
17 June 2025
Accepted
29 September 2025
Published
10 October 2025
Volume
12 - 2025
Edited by
Giuseppe Gatti, Azienda Sanitaria Universitaria Giuliano Isontina, Italy
Reviewed by
Ioan Tilea, George Emil Palade University, Romania
Xiaolang Jiang, Fudan University, China
Updates
Copyright
© 2025 Wu, Song and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Jinlin Wu wujinlin@gdph.org.cn
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.