- 1Department of Cardiology, Wuhan Asia Heart Hospital, Wuhan, China
- 2Department of Cardiac Surgery, Wuhan Asia Heart Hospital, Wuhan, China
- 3Department of Cardiology, Wuhan Asia General Hospital, Wuhan, China
Background: Treatment strategies for multivessel coronary artery disease (MV-CAD) include percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), and the increasingly adopted hybrid coronary revascularization (HCR). HCR combines minimally invasive left internal mammary artery (LIMA)–to–left anterior descending (LAD) grafting with PCI of non-LAD lesions. However, comparative evidence in high-risk MV-CAD remains limited.
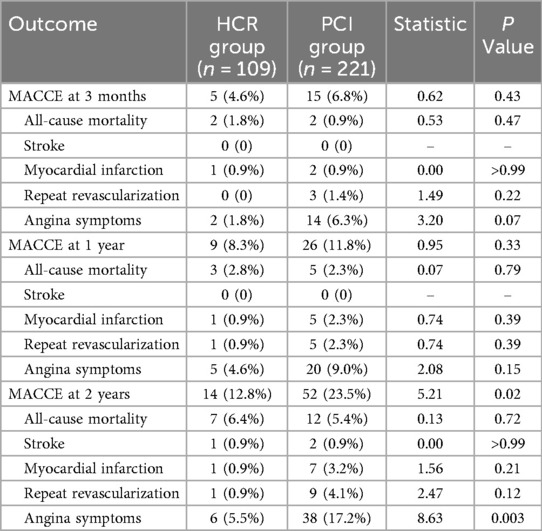
Methods: We retrospectively analyzed 330 high-risk MV-CAD patients from two centers (HCR n = 109; PCI n = 221) over 2 years. The primary endpoint was major adverse cardiac and cerebrovascular events (MACCE: all-cause death, stroke, myocardial infarction, repeat revascularization, and angina). Kaplan–Meier survival analysis and conventional statistical tests were applied.
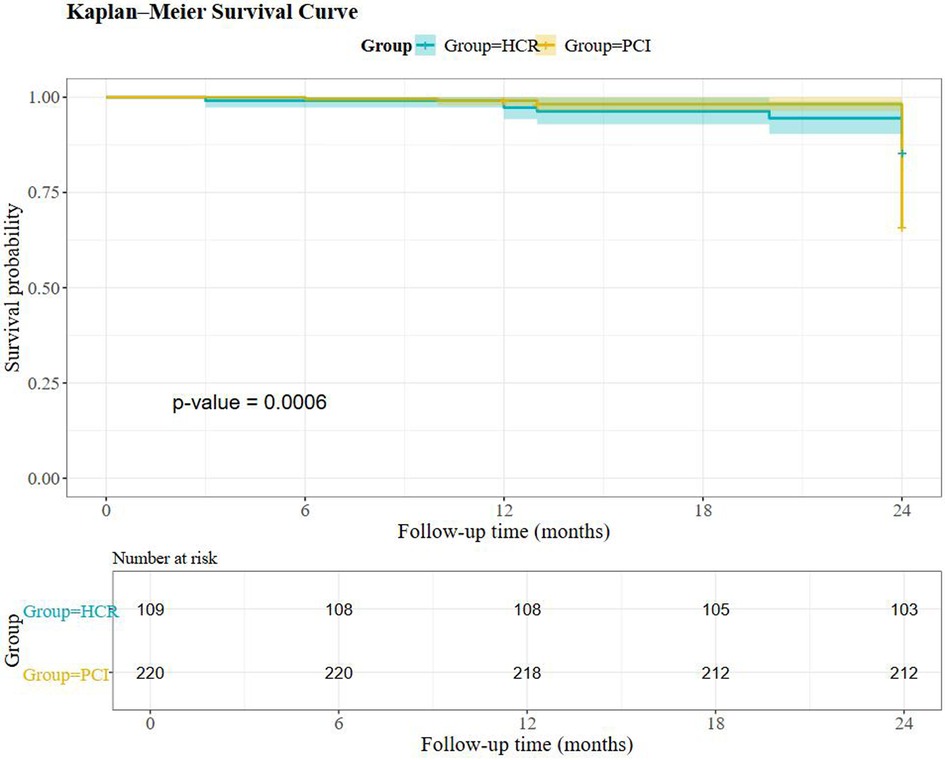
Results: Baseline demographics and SYNTAX scores were similar between groups. HCR involved fewer and shorter stents than PCI. Hospital stay, ICU duration, and total costs were higher with HCR. At 2 years, angina (5.5% vs. 17.2%; P = 0.003) and MACCE (12.8% vs. 23.5%; P = 0.02) were lower with HCR; overall survival by Kaplan–Meier favored HCR (log-rank P = 0.0006).
Conclusions: Despite longer hospitalization and higher costs, HCR was associated with superior long-term symptom relief and lower MACCE compared with PCI in high-risk MV-CAD. These findings support HCR as a viable strategy in carefully selected patients and warrant validation in prospective multicenter studies.
Introduction
Cardiovascular diseases remain the leading cause of mortality worldwide. In China, the number of coronary artery disease (CAD) patients exceeds 11 million (1). With population aging and a rising prevalence of metabolic comorbidities, the incidence of multivessel CAD (MV-CAD) is increasing. Treatment selection becomes particularly complex in patients with high-risk features, such as advanced age, diabetes, and impaired left ventricular function.
Contemporary revascularization strategies include PCI, CABG, and hybrid coronary revascularization (HCR) (2, 3). According to the 2018 ESC/EACTS Guidelines on myocardial revascularization (4), CABG is preferred in patients with complex anatomy or diabetes, whereas PCI is reasonable for less complex anatomy or when surgical risk is high. HCR integrates minimally invasive LIMA-to-LAD bypass with PCI for non-LAD lesions, and is often considered for left main disease, three-vessel disease, chronic total occlusions, heavy calcification, and bifurcation lesions (5, 6).
Despite its theoretical appeal, HCR adoption is limited by procedural complexity, the need for multidisciplinary coordination, and institutional experience. Most prior reports are single-center with small samples or short follow-up (7–11). Here, we compare 2-year outcomes of HCR vs. PCI in high-risk MV-CAD using real-world data from two centers.
Materials and methods
Study design and population
This retrospective, two-center observational study included 330 high-risk MV-CAD patients treated between November 2008 and February 2022. Patients were assigned to HCR (n = 109) or PCI (n = 221) according to the strategy received.
High-risk definition
High-risk MV-CAD was defined by anatomical and/or clinical criteria: left main disease, three-vessel disease, chronic total occlusion (CTO), severe calcification, complex bifurcation or tortuous lesions, diabetes, or reduced left ventricular function. In addition, SYNTAX II–predicted 4-year mortality was calculated for each patient (HCR 10.6% ± 3.4; PCI 10.2% ± 3.1). Treatment strategy was determined by a multidisciplinary Heart Team after comprehensive assessment of safety and risk.
HCR strategy
Staged HCR combined minimally invasive direct coronary artery bypass (MIDCAB) for LAD revascularization with PCI to non-LAD vessels (12–14). Among HCR patients, 37 underwent PCI first and 72 underwent MIDCAB first; the interval between procedures was ≤30 days (mean 10 ± 5 days). When MIDCAB was performed first, dual antiplatelet therapy (DAPT) was not discontinued; before MIDCAB after PCI, clopidogrel was held for 3 days and aspirin was continued; DAPT was resumed post-procedure.
Inclusion criteria
(1) Age ≥18 years; (2) Angiographic diagnosis of MV-CAD (LAD plus ≥1 major non-LAD epicardial vessel); (3) At least one high-risk feature as defined above; (4) Heart-Team–based decision-making.
Exclusion criteria
(1) STEMI patients requiring emergent primary PCI; (2) Pregnancy or breastfeeding; (3) Active malignancy or life expectancy <2 years; (4) Severe hepatic or renal dysfunction; (5) Prior CABG; (6) Contraindications to antiplatelet therapy; (7) Incomplete follow-up or missing data.
Endpoints
The primary endpoint was 2-year MACCE (all-cause mortality, non-fatal MI per the Fourth Universal Definition (15), ischemic stroke confirmed by neuroimaging, repeat revascularization, and clinically diagnosed angina based on CCS class and nitroglycerin response).
Statistical analysis
Continuous variables are presented as mean ± SD or median (IQR) and were compared using t tests or Wilcoxon rank-sum tests, as appropriate. Categorical variables are presented as n (%) and were compared using chi-square or Fisher's exact tests. Kaplan–Meier curves were compared using the log-rank test. Two-sided P < 0.05 was considered statistically significant.
Ethics
The study complied with the Declaration of Helsinki and was approved by the Ethics Committee of Wuhan Asia Heart Hospital (Approval No.: 2025-B028). Informed consent was obtained from all patients.
Results
Study cohort
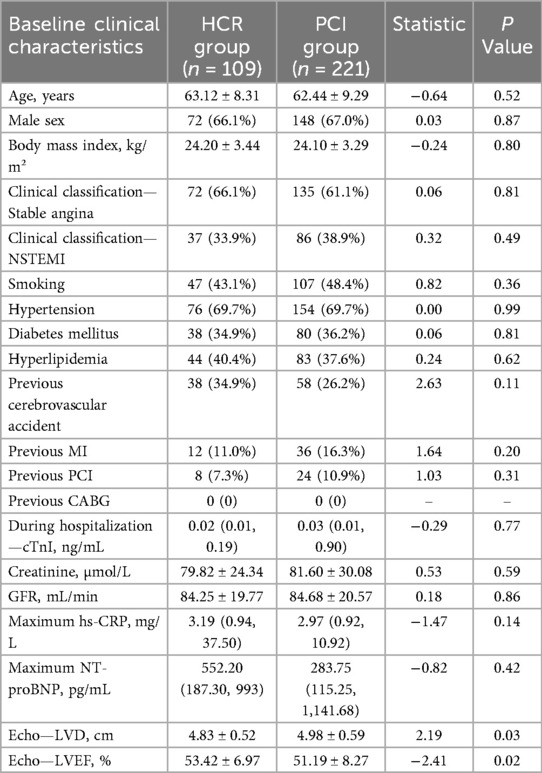
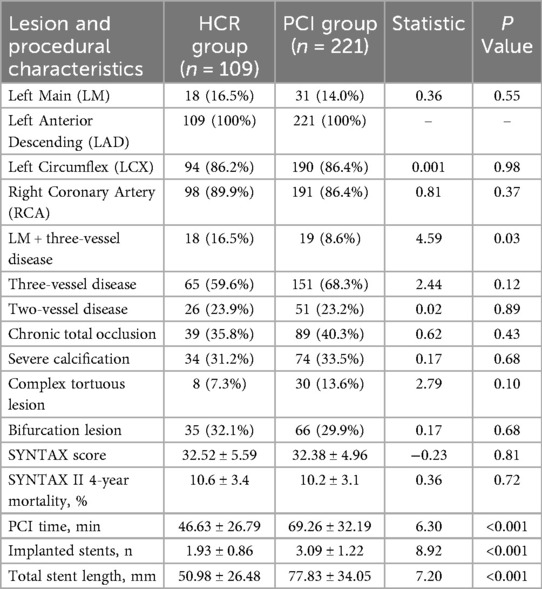
We included 330 patients (HCR n = 109; PCI n = 221). In the HCR group, 72 had stable angina and 37 had acute coronary syndrome (ACS); in the PCI group, 135 had stable angina and 86 had ACS. Baseline demographics (age 63.1 ± 8.3 vs. 62.4 ± 9.3 years; male 66.1% vs. 67.0%) and SYNTAX scores were similar between groups (Tables 1, 2).
Procedural profile
HCR used fewer stents (1.93 ± 0.86 vs. 3.09 ± 1.22) and shorter total stent length (50.98 ± 26.48 mm vs. 77.83 ± 34.05 mm; both P < 0.001). PCI procedure time was longer in the PCI group (69.26 ± 32.19 vs. 46.63 ± 26.79 min; P < 0.001) (Table 2).
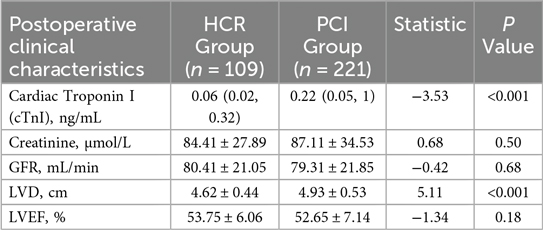
Periprocedural and postoperative markers
Postoperative cTnI was lower in HCR; left ventricular diameter (LVD) was smaller and LVEF modestly higher in HCR. Renal function and inflammatory markers did not differ materially between groups (Table 3).
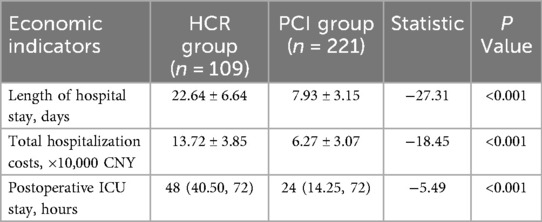
Economics
Length of stay (22.64 ± 6.64 vs. 7.93 ± 3.15 days), ICU stay, and total hospitalization costs (13.72 ± 3.85 vs. 6.27 ± 3.07 × 10,000 CNY) were higher with HCR (all P < 0.001) (Table 4).
Clinical outcomes
MACCE did not differ at 3 months or 1 year. At 2 years, HCR had lower angina (5.5% vs. 17.2%; P = 0.003) and MACCE (12.8% vs. 23.5%; P = 0.02) (Table 5). Overall survival favored HCR by Kaplan–Meier analysis (log-rank P = 0.0006) (Figure 1).
Discussion
In this real-world, two-center cohort of high-risk MV-CAD, HCR yielded lower 2-year angina and MACCE than PCI, despite longer hospitalization and higher costs. The combination of durable LIMA–LAD patency with reduced stent burden in non-LAD vessels likely contributed to these findings.
Patients treated with PCI alone required more and longer stents, potentially increasing the risks of restenosis and stent-related events. Our observations align with prior randomized and observational studies reporting symptom reduction and fewer repeat interventions with HCR in complex disease subsets.
Safety of HCR in high-risk patients is a key consideration. In our cohort, serious perioperative complications were infrequent; for transparency, we added a summary table of complications (e.g., IABP use, major bleeding, prolonged ventilation), supporting the feasibility of staged HCR.
Importantly, the MACCE difference was driven mainly by angina reduction, highlighting HCR's effect on symptom control and quality of life. While encouraging, this pattern warrants cautious interpretation of prognostic benefit and underscores the need for adequately powered, prospective multicenter trials with longer follow-up and advanced adjustment methods (e.g., propensity matching or weighting).
Future directions include refined patient selection using comprehensive risk models (e.g., SYNTAX II/III), incorporation of physiology-guided PCI and intravascular imaging, and evaluation of cost-effectiveness (16–18). Advances in minimally invasive and robotic techniques may further enhance the precision and scalability of HCR.
Conclusion
HCR is a feasible and effective option for selected high-risk MV-CAD patients, providing superior 2-year symptom relief and lower MACCE compared with PCI, albeit with greater resource use. These real-world data support broader evaluation of HCR in prospective, multicenter studies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TL: Data curation, Investigation, Writing – review & editing, Validation, Project administration, Writing – original draft, Formal analysis, Methodology, Conceptualization. DY: Writing – review & editing, Supervision. LQ: Supervision, Writing – review & editing. ZY: Supervision, Writing – review & editing. XX: Writing – review & editing, Supervision. DS: Writing – review & editing, Supervision, Methodology. ZH: Methodology, Supervision, Writing – review & editing. XC: Methodology, Supervision, Writing – review & editing. BW: Data curation, Methodology, Formal analysis, Supervision, Writing – review & editing. HY: Funding acquisition, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. This study was supported by the Knowledge Innovation Program of Wuhan-Basic Research (2022020801010576) and the Hubei Province Chutian Talent Medical and Health Talent Project.
Acknowledgments
We thank all patients and study coordinators for their contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1661189/full#supplementary-material
References
1. China National Center for Cardiovascular Diseases. Report on cardiovascular health and diseases in China 2022. Chin Circ J. (2023) 38(6):583–612. doi: 10.3969/j.issn.1000-3614.2023.06.001
2. El-Andari R, Bozso SJ, Fialka NM, Kang JJH, Fatehi Hassanabad A, Nagendran J. Alternative approaches to coronary artery bypass grafting versus percutaneous coronary intervention, how do they compare?: a systematic review and meta-analysis. Cardiol Rev. (2024) 32(5):392–401. doi: 10.1097/CRD.0000000000000524
3. Xia Y, Katz AN, Forest SJ, Pyo RT, Greenberg MA, DeRose JJ Jr. Hybrid coronary revascularization has improved short-term outcomes but worse mid-term reintervention rates compared to CABG: a propensity matched analysis. Innovations. (2017) 12(3):174–9. doi: 10.1097/IMI.0000000000000376
4. Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. (2019) 40(2):87–165. doi: 10.1093/eurheartj/ehy394
5. Dixon LK, Akberali U, Di Tommaso E, George SJ, Johnson TW, Bruno VD. Hybrid coronary revascularization versus coronary artery bypass grafting for multivessel coronary artery disease: a systematic review and meta-analysis. Int J Cardiol. (2022) 359:20–7. doi: 10.1016/j.ijcard.2022.04.030
6. Willard R, Scheinerman J, Pupovac S, Patel NC. The current state of hybrid coronary revascularization. Ann Thorac Surg. (2024) 118(2):318–28. doi: 10.1016/j.athoracsur.2024.04.010
7. Patel NC, Hemli JM, Kim MC, Seetharam K, Pirelli L, Brinster DR, et al. Short- and intermediate-term outcomes of hybrid coronary revascularization for double-vessel disease. J Thorac Cardiovasc Surg. (2018) 156:1799–807.e3. doi: 10.1016/j.jtcvs.2018.04.078
8. Puskas JD, Halkos ME, DeRose JJ, Bagiella E, Miller MA, Overbey J, et al. Hybrid coronary revascularization for the treatment of multivessel coronary artery disease: a multicenter observational study. J Am Coll Cardiol. (2016) 68(4):356–65. doi: 10.1016/j.jacc.2016.05.032
9. Hannan EL, Wu YF, Cozzens K, Tamis-Holland J, Ling FSK, Jacobs AK, et al. Hybrid coronary revascularization vs. percutaneous coronary interventions for multivessel coronary artery disease. J Geriatr Cardiol. (2021) 18(3):159–67. doi: 10.11909/j.issn.1671-5411.2021.03.003
10. Gąsior M, Zembala MO, Tajstra M, Filipiak K, Gierlotka M, Hrapkowicz T, et al. Hybrid revascularization for multivessel coronary artery disease. JACC Cardiovasc Interv. (2014) 7(11):1277–83. doi: 10.1016/j.jcin.2014.05.025
11. Choi HJ, Kang J, Song H, Kim DY, Choi KB. Comparison of coronary artery bypass graft-first and percutaneous coronary intervention-first approaches for 2-stage hybrid coronary revascularization. Korean J Thorac Cardiovasc Surg. (2017) 50(4):247–54. doi: 10.5090/kjtcs.2017.50.4.247
12. Gaudino M, Benedetto U, Fremes S, Biondi-Zoccai G, Sedrakyan A, Puskas JD, et al. Radial-Artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. (2018) 378(22):2069–77. doi: 10.1056/NEJMoa1716026
13. Purmessur R, Wijesena T, Ali J. Minimal-Access coronary revascularization: past, present, and future. J Cardiovasc Dev Dis. (2023) 10(8):326. doi: 10.3390/jcdd10080326
14. Fatehi Hassanabad A, Kang J, Maitland A, Adams C, Kent WDT. Review of contemporary techniques for minimally invasive coronary revascularization. Innovations. (2021) 16(3):231–43. doi: 10.1177/15569845211010767
15. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. (2019) 40(3):237–69. doi: 10.1093/eurheartj/ehy462
16. Ganyukov V, Kochergin N, Shilov A, Tarasov R, Skupien J, Szot W, et al. HREVS randomized clinical trial: surgical vs. percutaneous vs. hybrid revascularization in multivessel CAD—residual ischemia and clinical outcomes at one year. J Interv Cardiol. (2020) 2020:5458064. doi: 10.1155/2020/5458064
17. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. (2009) 360(10):961–72. doi: 10.1056/NEJMoa0804626
18. Serruys PW, Kogame N, Katagiri Y, Modolo R, Buszman PE, Íñiguez-Romo A, et al. Clinical outcomes of state-of-the-art percutaneous coronary revascularisation in patients with three-vessel disease: two-year follow-up of the SYNTAX II study. EuroIntervention. (2019) 15(3):e244–52. doi: 10.4244/EIJ-D-18-00980
Keywords: hybrid coronary revascularization, percutaneous coronary intervention, multivessel coronary artery disease, MACCE, outcomes
Citation: Luo T, Yi D, Qiu L, Yang Z, Xu X, Song D, Hua Z, Chen X, Wang B and Yan H (2025) Hybrid coronary revascularization vs. PCI in high-risk multivessel coronary artery disease: a two-center, two-year utcome comparison. Front. Cardiovasc. Med. 12:1661189. doi: 10.3389/fcvm.2025.1661189
Received: 7 July 2025; Accepted: 31 October 2025;
Published: 1 December 2025.
Edited by:
Ellie Tzima, University of Oxford, United KingdomReviewed by:
Matteo Ferrarini, INCO, Istituto Clinico Sant'Ambrogio, ItalyKrzysztof Sanetra, Andrzej Frycz Modrzewski Krakow University, Poland
Copyright: © 2025 Luo, Yi, Qiu, Yang, Xu, Song, Hua, Chen, Wang and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Yan, eWFuaHVhMDgwN0BhbGl5dW4uY29t
 Ting Luo1
Ting Luo1 Dong Yi
Dong Yi Xiaodie Xu
Xiaodie Xu Hua Yan
Hua Yan