Abstract
A 75-year-old woman was admitted for the treatment of uterine fibroids and underwent laparoscopic total hysterectomy with bilateral salpingo-oophorectomy under general anesthesia. On the first postoperative day, the patient experienced sudden convulsion followed by loss of consciousness while transitioning from a seated to standing position. Subsequent examinations revealed pulmonary embolism and partial thrombosis in the muscular veins of the right lower leg. Anticoagulant therapy was immediately initiated. On postoperative day 3, early morning, the patient was found to be agitated with a positive Babinski sign on the right side. A CT scan of the brain revealed a cerebral infarction. Following the sequential occurrence of pulmonary embolism and cerebral infarction, paradoxical embolism drew the physician's attention. After discussion, the cause was attributed to either an arteriovenous fistula or a patent foramen ovale. Subsequent transesophageal echocardiography (TEE) and bubble study confirmed a patent foramen ovale (PFO) in the patient. This case highlights the critical importance of proactively searching for underlying etiologies when faced with such abnormal clinical presentations.
Introduction
Patent foramen ovale (PFO) refers to the failure of the normal fetal communication between the left and right atria (the foramen ovale) to close after birth (1). PFO is a common condition, occurring in approximately 25% of the population. Diagnostic options include transthoracic echocardiography (TTE), transesophageal echocardiography (TEE), and transcranial Doppler ultrasonography (TCD) (2). A meta-analysis demonstrated an association between PFO and an elevated risk of perioperative stroke during non-cardiac surgery (3). The potential mechanisms of stroke include paradoxical embolism from venous thrombi traversing the PFO, in situ thrombosis within the PFO, and atrial arrhythmias resulting from electrical conduction disturbances (4).
Globally, stroke is the second leading cause of death, and the disease is clinically characterised by sudden-onset neurological deficits (5). Approximately 25%–40% of ischemic strokes occur without an identifiable cause and are classified as cryptogenic stroke (6). In 1988, P Lechat et al. first reported that the presence of a PFO increases the risk of ischemic stroke and is a common cause of cryptogenic stroke (7). Thrombi derived from the venous circulation embolize into the systemic circulation through right-to-left shunting permitted by the PFO, leading to stroke (8). A prospective cohort study demonstrated that among patients with symptomatic pulmonary embolism, the patient with PFO had a higher incidence of recent stroke compared to those without PFO (9). This finding further supports paradoxical embolism as a significant mechanism of ischemic stroke in PFO patients. The study reported a case of a uterine fibroid patient who developed pulmonary embolism followed by cerebral stroke after undergoing total hysterectomy with bilateral adnexectomy. This clinical presentation promptly prompted clinicians to suspect paradoxical embolism, ultimately leading to the diagnosis of a PFO.
Case presentation
A 75-year-old female patient was admitted to the Department of Gynecology due to uterine fibroids (measuring 6.2 × 4.1 cm). She reported no recent symptoms such as headache, dizziness, or fatigue. The patient underwent left thyroid cystectomy 30 years ago and denied other significant medical history.
The patient underwent laparoscopic total hysterectomy with bilateral salpingo-oophorectomy under general anesthesia after admission. Intraoperative vital signs remained stable, and the procedure was completed uneventfully. On the first postoperative day, the patient experienced sudden convulsion and loss of consciousness while transitioning from a sitting to standing position, becoming unresponsive to verbal stimuli. Immediate physical examination revealed: Blood pressure 92/64 mmHg, heart rate 72 bpm, oxygen saturation 67%. Bilateral pupils were equal and round with preserved light reflex. Clear breath sounds were heard in both lung fields without rales or rhonchi. Arterial blood gas analysis revealed: pH 7.27, PO₂ 59.0 mmHg, PCO2 35 mmHg, Glucose 10.6 mmol/L, Lactate 3.5 mmol/L, Base Excess (BEb) −9.9 mmol/L. Immediate endotracheal intubation was performed with initiation of mechanical ventilation. Enhanced pulmonary CT angiography revealed pulmonary embolism (Figure 1A), while brain CT showed no significant abnormalities (Figure 1B). Transthoracic echocardiography (TTE) demonstrated trivial tricuspid regurgitation and impaired left ventricular relaxation. Lower extremity venous doppler ultrasound demonstrated partial muscular vein thrombosis in the right calf. Low molecular weight heparin calcium (0.6 ml Q12 h) was promptly initiated for anticoagulation. Subsequently, intermittent pneumatic compression (IPC) was initiated for the patient. Due to critical condition, the patient was immediately transferred to the Intensive Care Unit (ICU).
Figure 1
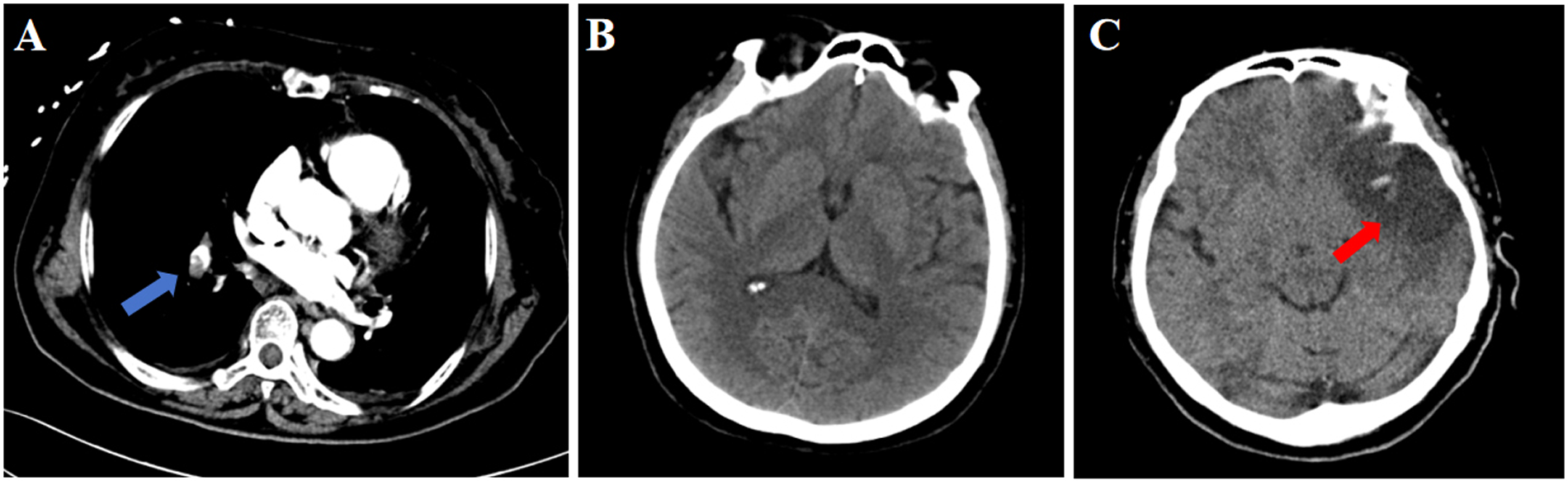
CT findings of the patient. (A) Pulmonary CT on postoperative day 1; (B). Cranial CT on postoperative day 1; (C). Cranial CT on postoperative day 3. Blue arrow: pulmonary embolism; Red arrow: stroke.
On postoperative day 3, early morning, the patient developed agitation and right-sided limb weakness with a positive Babinski sign on the right. Further brain CT demonstrated hypodense lesions indicating large-territory cerebral infarction in the left hemisphere (Figure 1C). Given the sequential occurrence of pulmonary embolism and cerebral infarction, the treating physicians clinically suspected a pathological right-to-left shunt pathway, such as arteriovenous fistula or PFO. TEE and bubble study was performed, revealing: Patent foramen ovale with significant right-to-left shunt (Figures 2A,B). Strongly positive bubble study (Figure 2C). The final diagnosis was PFO, pulmonary embolism and cerebral infarction.
Figure 2
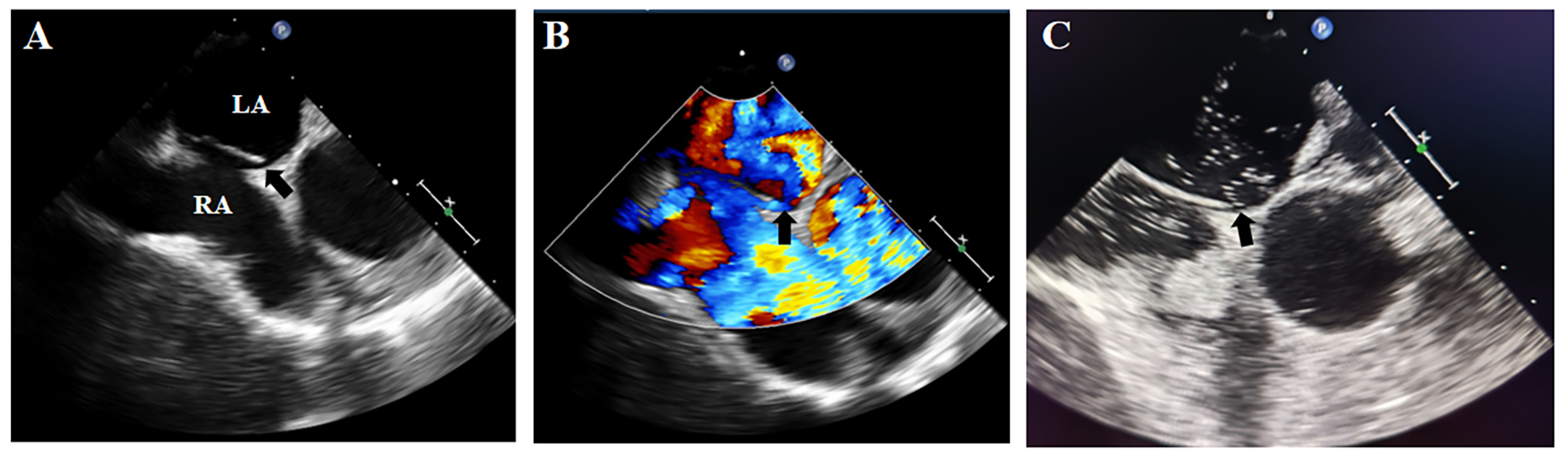
Transesophageal echocardiographic findings. (A,B) Demonstrated a significant PFO with right-to-left shunting; (C): strongly positive bubble study. Black arrow: PFO. LA, left atrium; RA, right atrium.
The patient was successfully stabilized from the critical condition and discharged from the ICU. We have advised the patient to consult an interventional cardiologist to evaluate the feasibility of PFO closure.
Case review
To further enhance our comprehension of this disease category, we conducted a systematic review of case reports spanning the past two decades (January 2005–June 2025). We performed a PubMed search spanning all fields from 2005 to present using the query “(patent foramen ovale) AND (Pulmonary Embolism) AND (stroke)”, yielding 148 initial results. To ensure quality assurance, only Science Citation Index-indexed case reports were considered. Given the predominance of publications describing PFO patients with either stroke or pulmonary embolism alone, we manually curated articles documenting concurrent or sequential pulmonary embolism and stroke in PFO patients (≥18 years), ultimately identifying 32 qualifying cases (Supplementary Figure S1). Among these cases, 18 were male and 14 were female. Thrombotic events manifested abruptly in the majority of patients, with only 4 cases having recent surgical procedures prior to onset. The sequence of thrombotic events was documented as follows: pulmonary embolism preceding cerebral stroke in 9 patients, cerebral stroke detected prior to pulmonary embolism in 4 patients, and 19 patients with simultaneous detection of pulmonary embolism and stroke or unrecorded order of detection. Although the median age of patients with first-diagnosed cryptogenic stroke associated with PFO is around 45 years, showing regional trends toward younger onset (10), our analysis of reported cases identified 19 patients aged over 60 years. This requires heightened vigilance as PFO-related stroke in older patients should not be overlooked; PFO closure was confirmed in 12 cases. While studies indicate that PFO closure reduces stroke recurrence rates in patients with high-risk PFO features, the reported mean patient age was only 51.8 years (11). A multicenter study on PFO closure in elderly patients demonstrated that compared to the control group's recurrent cerebrovascular events and stroke rate of 1.21%, the intervention group exhibited a reduced incidence of 0.55%; however, it must be emphasized that diabetes, aspirin use, and advanced age are factors associated with increased risk of adverse clinical outcomes; cautious consideration is therefore required in clinical decision-making regarding PFO closure for this specific population (12).
Table 1
| No. | Authors | Date of publication | Patient's age | Pre-onset intervention | Symptom | Embolism site | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Bracey et al. (13) | 2006 | 29 | NA | Severe chest pain and dyspnea at rest, with right-sided limb weakness, loss of consciousness, and respiratory arrest | Lung, brain, deep vein of the left lower extremity, right atrium, right ventricle, left atrium, and aortic arch extending to the left common carotid artery | NA |
| 2 | Iwanaga et al. (14) | 2007 | 84 | NA | Coma, tetraplegia | Brain, lung, lower limb deep venous | NA |
| 3 | Shibazaki et al. (15) | 2007 | 79 | NA | Sudden onset of consciousness disturbance, left central facial palsy and left hemiplegia were evident | Lung, brain | NA |
| 4 | Pavesi et al. (16) | 2008 | 65 | Air travel | Worsening dyspnea, chest pain | Lung, brain | NA |
| 5 | Seetharaman et al. (17) | 2011 | 62 | NA | Left-sided weakness, left-sided hemianopia, hemineglect, hemiplegia and hemianaesthesia, and a swollen left calf | Brain, lung | PFO closure procedure |
| 6 | Chow et al. (18) | 2012 | 35 | NA | Collapsed, loss of consciousness, unable to speak | Brain, lung | NA |
| 7 | Lewis et al. (19) | 2012 | 66 | NA | Speech loss, right-sided weakness | Brain, lung | PFO closure procedure |
| 8 | Kumar et al. (20) | 2013 | 32 | NA | Right-sided hemiparesis | Brain, lung, right popliteal vein, common iliac vein | NA |
| 9 | Omar et al. (21) | 2013 | 69 | Right total hip replacement | Sudden dyspnoea, wheezing and confusion | Brain, lung | NA |
| 10 | Cameron et al. (22) | 2015 | 53 | NA | Left gaze preference, dysarthria, and flaccid right hemiplegia | Brain, lung | NA |
| 11 | Miriyala et al. (23) | 2016 | 72 | NA | Left-sided weakness, confusion, and altered speech | Brain, lung | NA |
| 12 | Urja et al. (24) | 2017 | 73 | NA | Slurred speech, near-syncope, dizziness, and progressive left-sided limb weakness | Lung, brain | NA |
| 13 | Barros-Gomes et al. (25) | 2018 | 68 | NA | Facial deviation, right upper extremity weakness, and aphasia | Bilateral lower extremities, brain, lung | NA |
| 14 | Konala et al. (26) | 2019 | 82 | NA | Lightheadedness, mild dyspnea, and sudden syncope. | Lung, brain | NA |
| 15 | De Sousa Bispo et al. (27) | 2019 | 80 | NA | Positional dyspnoea that develops upon sitting up, accompanied with refractory hypoxaemia | Brain, lung | PFO closure procedure |
| 16 | Lak et al. (28) | 2020 | 68 | NA | Acute visual impairment manifesting as partial hemianopsia | Brain, lung, superior mesenteric artery | PFO closure procedure |
| 17 | Jena et al. (29) | 2020 | 64 | NA | Confusion, slurred speech, right-sided weakness with pronator drift, right facial droop, and preserved forehead movement | Brain, lung | NA |
| 18 | Gunn et al. (30) | 2020 | 66 | NA | Acute respiratory failure | Lung, brain | PFO closure procedure |
| 19 | Suenaga et al. (31) | 2021 | 55 | NA | Syncope resulting in a fall | Lung, brain | NA |
| 20 | Kass et al. (32) | 2021 | 67 | Prostatic surgery | Hematuria, urinary retention, and hypoxemia with dysarthria | Lung, brain, bladder | PFO closure procedure |
| 21 | Galtes et al. (33) | 2021 | 42 | NA | Agitation, confusion accompanied by generalized weakness, aphasia, and right-sided hemiplegia. | Brain, lung | PFO closure procedure |
| 22 | Jayalakshmi et al. (34) | 2021 | 52 | NA | Sudden left hemiparesis | Brain, lung | NA |
| 23 | Takemoto et al. (35) | 2021 | 77 | NA | Dyspnea followed by cardiac arrest | Lung, brain | NA |
| 24 | Dattani et al. (36) | 2022 | 55 | NA | Sudden dyspnoea, left limb weakness | Lung, brain | PFO closure procedure |
| 25 | He et al. (37) | 2022 | 42 | NA | Left chest pain, shortness of breath and lower extremity edema | Brain, lung, left common femoral vein, femoral vein, popliteal vein, inferior vena cava, bilateral external iliac veins, and bilateral internal iliac veins | PFO closure procedure |
| 26 | Uecker et al. (38) | 2023 | 57 | NA | Dyspnoea | Lung, brain | PFO closure procedure |
| 27 | Zaussinger et al. (39) | 2023 | 36 | Cosmetic breast augmentation-mastopexy | Frequent generalized seizures | Lung, brain | NA |
| 28 | Alaboud Alkheder et al. (40) | 2024 | 61 | NA | Loss of consciousness, tachypnea accompanied by right-sided limb weakness and visual changes | brain, lung | NA |
| 29 | Tyler et al. (41) | 2024 | 66 | Orthotopic liver transplantation | Acute onset of shortness of breath, left-sided limb weakness, facial droop, and altered mental status | Brain, lung | PFO closure procedure |
| 30 | Ahmad et al. (42) | 2024 | 50 | NA | Chest pain and respiratory distress | Brain, lung | PFO closure procedure |
| 31 | Quasem et al. (43) | 2025 | 33 | A history of intravenous drug use | Infection, acute confusion | Lung, brain | NA |
| 32 | Monteiro et al. (44) | 2025 | 86 | NA | Acute onset global aphasia, right-sided hemiplegia, left conjugate gaze deviation, right homonymous hemianopsia with facial weakness | Brain, lung | NA |
Case review details.
Discussion
The incidence of postoperative venous thromboembolism (VTE), including pulmonary embolism, following laparoscopic hysterectomy is reported to be approximately 0.3% (45). In the case we presented, the patient underwent a laparoscopic total hysterectomy with bilateral salpingo-oophorectomy. On postoperative day 1, she developed a pulmonary embolism. A brain CT scan revealed no abnormalities. Additionally, TTE did not detect pulmonary hypertension in the patient. Based on the patient's medical history, the physicians initially suspected the pulmonary embolism was a postoperative complication. However, on the night of the second postoperative day, the patient became agitated and developed impaired motor function in the right limbs. A Babinski sign was positive on the right side. Suspecting an intracranial abnormality, the physicians performed a further brain CT scan, which confirmed the presence of a stroke. Based on human physiology, physicians noted that pulmonary embolism does not typically lead to stroke under normal circumstances. This paradoxical embolism prompted significant concern among the treating physicians, who suspected the presence of either an arteriovenous fistula or a PFO. The diagnosis of PFO was ultimately confirmed through TEE with a bubble study. We had hypothesized that pulmonary hypertension might facilitate paradoxical embolism; however, TTE showed no evidence of this phenomenon in the patient.
A notable feature of this case is that the patient developed cerebral infarction (stroke) shortly after pulmonary embolism in the postoperative period. This leading to the diagnosis of a PFO. Existing case reports have documented similar occurrences of paradoxical embolism due to a PFO in postoperative patients (32). However, acute sequential pulmonary embolism and cerebral infarction following total hysterectomy with bilateral salpingo-oophorectomy have not been documented. Current preventive strategies for postoperative thromboembolism—early ambulation, intermittent pneumatic compression, and indicated early anticoagulation—are relatively low-cost. A large-scale observational study revealed that preoperatively diagnosed patent PFO is associated with an increased risk of ischemic stroke within 30 days after surgery (46). A meta-analysis of PFO and perioperative stroke in non-cardiac surgery revealed that PFO presence correlates with heightened stroke risk in surgical patients (3). The study proposes that early PFO identification and preventive protocol development may potentially improve perioperative outcomes. Therefore, perioperative screening for PFO could be beneficial, but the high cost and low detection rate might make it impractical. Certainly, the impact of preoperative diagnosis of PFO and its corresponding treatment on stroke prevention still requires validation through large-scale randomized clinical trials. We hope our report will provide clinicians with valuable reference.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LZ: Conceptualization, Investigation, Writing – original draft. BW: Data curation, Methodology, Writing – original draft. BZ: Software, Visualization, Writing – original draft. YT: Investigation, Project administration, Writing – original draft. RZ: Investigation, Validation, Visualization, Writing – original draft. MH: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2025.1666061/full#supplementary-material
References
1.
Calvert PA Rana BS Kydd AC Shapiro LM . Patent foramen ovale: anatomy, outcomes, and closure. Nat Rev Cardiol. (2011) 8(3):148–60. 10.1038/nrcardio.2010.224
2.
Mac Grory B Ohman EM Feng W Xian Y Yaghi S Kamel H et al Advances in the management of cardioembolic stroke associated with patent foramen ovale. Br Med J. (2022) 376:e063161. 10.1136/bmj-2020-063161
3.
Rais G Vassallo P Schorer R Bollen Pinto B Putzu A . Patent foramen ovale and perioperative stroke in noncardiac surgery: a systematic review and meta-analysis. Br J Anaesth. (2022) 129(6):898–908. 10.1016/j.bja.2022.06.036
4.
Caso V Turc G Abdul-Rahim AH Castro P Hussain S Lal A et al European Stroke Organisation (ESO) guidelines on the diagnosis and management of patent foramen ovale (PFO) after stroke. Eur Stroke J. (2024) 9(4):800–34. 10.1177/23969873241247978
5.
Hilkens NA Casolla B Leung TW de Leeuw FE . Stroke. Lancet. (2024) 403(10446):2820–36. 10.1016/S0140-6736(24)00642-1
6.
Fukutomi M Wilkins B Søndergaard L . The role of device closure of patent foramen ovale in patients with cryptogenic stroke. J Intern Med. (2020) 288(4):400–9. 10.1111/joim.13143
7.
Lechat P Mas JL Lascault G Loron P Theard M Klimczac M et al Prevalence of patent foramen ovale in patients with stroke. N Engl J Med. (1988) 318(18):1148–52. 10.1056/NEJM198805053181802
8.
Di Tullio MR . Prevention of patent foramen ovale-related stroke: an evolving concept. Stroke. (2021) 52(11):3427–9. 10.1161/STROKEAHA.121.035735
9.
Le Moigne E Timsit S Ben Salem D Didier R Jobic Y Paleiron N et al Patent foramen ovale and ischemic stroke in patients with pulmonary embolism: a prospective cohort study. Ann Intern Med. (2019) 170(11):756–63. 10.7326/M18-3485
10.
Wöhrle J Kochs M Hombach V Merkle N . Prevalence of myocardial scar in patients with cryptogenic cerebral ischemic events and patent foramen ovale. JACC Cardiovasc Imaging. (2010) 3(8):833–9. 10.1016/j.jcmg.2010.05.013
11.
Lee PH Song JK Kim JS Heo R Lee S Kim DH et al Cryptogenic stroke and high-risk patent foramen ovale: the DEFENSE-PFO trial. J Am Coll Cardiol. (2018) 71(20):2335–42. 10.1016/j.jacc.2018.02.046
12.
Farjat-Pasos JI Guedeney P Horlick E Abtan J Nombela-Franco L Hibbert B et al Determinants of adverse outcomes following patent foramen ovale closure in elderly patients. EuroIntervention. (2024) 20(16):1029–38. 10.4244/EIJ-D-24-00156
13.
Bracey TS Langrish C Darby M Soar J . Cerebral infarction following thrombolysis for massive pulmonary embolism. Resuscitation. (2006) 68(1):135–7. 10.1016/j.resuscitation.2005.05.017
14.
Iwanaga T Iguchi Y Shibazaki K Inoue T Kimura K . Paradoxical brain embolism in an acute stroke. J Neurol Sci. (2007) 254(1–2):102–4. 10.1016/j.jns.2007.01.006
15.
Shibazaki K Iguchi Y Inoue T Ueno Y Kimura K . Serial contrast saline transcranial Doppler examination in a patient with paradoxical brain embolism associated with pulmonary embolism. J Clin Neurosci. (2007) 14(8):788–91. 10.1016/j.jocn.2006.05.011
16.
Pavesi PC Pedone C Crisci M Piacentini A Fulvi M Di Pasquale G . Concomitant submassive pulmonary embolism and paradoxical embolic stroke after a long flight: which is the optimal treatment?J Cardiovasc Med (Hagerstown). (2008) 9(10):1070–3. 10.2459/JCM.0b013e328306f2ea
17.
Seetharaman S Lams B Rudd A Birns J . Pulmonary and paradoxical embolism with platypnoea-orthodeoxia. Br J Hosp Med (Lond). (2011) 72(11):652–3. 10.12968/hmed.2011.72.11.652
18.
Chow V Wang W Wilson M Yiannikas J . Thrombus in transit within a patent foramen ovale: an argument for consideration of prophylactic closure?J Clin Ultrasound. (2012) 40(2):115–8. 10.1002/jcu.20820
19.
Lewis G McDonald P . Pulmonary embolism and patent foramen ovale causing an ischaemic stroke. Br J Hosp Med (Lond). (2012) 73(10):592–3. 10.12968/hmed.2012.73.10.592
20.
Kumar T Budnur SC Mahadevappa NC Singla V . Paradoxical embolism via a patent foramen ovale. BMJ Case Rep. (2013) 2013:bcr2013009818. 10.1136/bcr-2013-009818
21.
Omar HR Huang C Miller JH Mangar D Kabemba A Camporesi EM . Simultaneous pulmonary embolism and cerebrovascular stroke. Herz. (2013) 38(8):884–6. 10.1007/s00059-013-3782-6
22.
Cameron SJ Laskurain E Holcman K Richeson JF Mieszczanska H . Treacherous travelers: emboli. Am J Med. (2015) 128(7):695–8. 10.1016/j.amjmed.2015.01.038
23.
Miriyala V Awan MU Faraj K Nagra B . Traversing boundaries: thrombus in transit with paradoxical embolism. J Community Hosp Intern Med Perspect. (2016) 6(4):31438. 10.3402/jchimp.v6.31438
24.
Urja P Nippoldt EH Barak V Valenta C . High-value care in the evaluation of stroke. Cureus. (2017) 9(8):e1532. 10.7759/cureus.1532
25.
Barros-Gomes S El Sabbagh A Eleid MF Mankrad SV . Concomitant acute stroke, pulmonary and myocardial infarction due to in-transient thrombus across a patent foramen ovale. Echo Res Pract. (2018) 5(4):I9–10. 10.1530/ERP-18-0044
26.
Konala VM Naramala S Adapa S Aeddula NR Bose S . An elderly man with syncope, hypoxia, and confusion: a case report and review of literature. Cureus. (2019) 11(9):e5567. 10.7759/cureus.5567
27.
De Sousa Bispo J Ramires I Pestana J Café H . A case report of platypnea-orthodeoxia syndrome: an interplay of pressure and blood flow. Eur Heart J Case Rep. (2019) 3(4):1–4. 10.1093/ehjcr/ytz187
28.
Lak HM Ahmed T Nair R Maroo A . Simultaneous multifocal paradoxical embolism in an elderly patient with patent foramen ovale: a case report. Cureus. (2020) 12(2):e6992. 10.7759/cureus.6992
29.
Jena N Ibrahim R Tirunagari D Patel K . Impending paradoxical embolism traversing three cardiac chambers presenting with stroke and pulmonary embolism. Cureus. (2020) 12(7):e9416. 10.7759/cureus.9416
30.
Gunn TM Gurley JC Keshavamurthy S . Cannula migration through an undiagnosed patent foramen ovale and embolic cerebrovascular accident in a patient with femoral venoarterial extracorporeal membrane oxygenation. J Card Surg. (2020) 35(7):1681–2. 10.1111/jocs.14618
31.
Suenaga H Tsurukiri J Kato T Matsunaga K Ogawa N Oiwa A et al Paradoxical cerebral embolization caused by thrombus-in-transit via a patent foramen ovale in a patient with symptomatic pulmonary embolism: a case report. J Neuroendovasc Ther. (2021) 15(12):805–10. 10.5797/jnet.cr.2021-0003
32.
Kass M Grocott HP Shah AH . Constellation of stroke, pulmonary embolism, and platypnea orthodeoxia syndrome: the elusive patent foramen ovale. JACC Cardiovasc Interv. (2021) 14(14):e165–7. 10.1016/j.jcin.2021.03.034
33.
Galtes I Suraci N Presti SL Santana O . Thrombus in transit across a patent foramen ovale in a patient with cerebrovascular accidents, pulmonary embolism, and deep vein thrombosis. Ann Card Anaesth. (2021) 24(3):362–4. 10.4103/aca.ACA_120_19
34.
Jayalakshmi S Khandalia H Vooturi S Jiwani PA Kaul S . Simultaneous acute pulmonary thromboembolism and stroke—a management dilemma. Neurol India. (2021) 69(5):1371–3. 10.4103/0028-3886.329553
35.
Takemoto K Nakamura M Atagi K . Concomitant acute pulmonary embolism, myocardial infarction and ischemic stroke due to paradoxical embolism from a patent foramen ovale: a case report. Oxf Med Case Reports. (2021) 2021(10):omab101. 10.1093/omcr/omab101
36.
Dattani A Safwan K Ansari M Somani R . Bi-atrial thrombus straddling a patent foramen ovale with bilateral embolization: a therapeutic challenge. Echocardiography. (2022) 39(1):125–31. 10.1111/echo.15269
37.
He L Xue JY Du YJ Xie XG Wang XY Zhang YS . Transjugular approach to closure of patent foramen Ovale under the guidance of fluoroscopy and transthoracic echocardiography: a case report. Front Cardiovasc Med. (2022) 9:905614. 10.3389/fcvm.2022.905614
38.
Uecker NA Rosenkranz S Bunck A Tichelbäcker T . Unexpected paradoxical embolization following catheter-directed thrombectomy with the FlowTriever™ system in a patient with pulmonary embolism: a case report. Eur Heart J Case Rep. (2023) 7(3):ytad074. 10.1093/ehjcr/ytad074
39.
Zaussinger M Speiser S Wenny R Schmidt M . Undiagnosed patent foramen ovale and thrombophilic gene mutations resulting in pulmonary embolism with cryptogenic stroke after cosmetic breast surgery. Plast Reconstr Surg Glob Open. (2023) 11(3):e4867. 10.1097/GOX.0000000000004867
40.
Alaboud Alkheder K Al-Khafaji YB Al-Nahhas OF . Acute ischemic stroke superimposed on acute pulmonary embolism in the presence of patent foramen Ovale: a case report. Cureus. (2024) 16(5):e61036. 10.7759/cureus.61036
41.
Tyler JH Fleetwood V Kamel G Verma DR Rangrass G . Planned venovenous-extracorporeal membrane oxygenation as a bridge to orthotopic liver transplant performed for very severe hepatopulmonary syndrome: a case report. Cureus. (2024) 16(7):e63962. 10.7759/cureus.63962
42.
Ahmad S Goldsweig AM . Left atrial appendage occlusion and patent foramen ovale closure using a steerable sheath and intracardiac echocardiography. Catheter Cardiovasc Interv. (2024) 104(2):416–8. 10.1002/ccd.31132
43.
Quasem K Carrasquel M George V Elisevich L Maser H . Tricuspid endocarditis leading to a stroke: a case report of paradoxical embolism in a young intravenous drug user. Cureus. (2025) 17(1):e78304. 10.7759/cureus.78304
44.
Monteiro AS Domingos RR Amalio SR . Platypnea-orthodeoxia syndrome secondary to patent foramen ovale and pulmonary thromboembolism. Cureus. (2025) 17(2):e79082. 10.7759/cureus.79082
45.
Duyar S Mou T Mueller MG Kenton KS Bretschneider CE . Incidence of and risk factors for postoperative venous thromboembolism in benign hysterectomy. J Minim Invasive Gynecol. (2022) 29(2):231–6.e1. 10.1016/j.jmig.2021.08.004
46.
Friedrich S Ng PY Platzbecker K Burns SM Banner-Goodspeed V Weimar C et al Patent foramen ovale and long-term risk of ischaemic stroke after surgery. Eur Heart J. (2019) 40(11):914–24. 10.1093/eurheartj/ehy402
Summary
Keywords
patent foramen ovale, pulmonary embolism, cerebral infarction, paradoxical embolism, status post total hysterectomy with bilateral salpingo-oophorectomy, case report
Citation
Zhao L, Wang B, Zhao B, Tian Y, Zhai R and Hu M (2025) A patient with sudden pulmonary embolism and stroke after total hysterectomy and bilateral salpingo-oophorectomy was diagnosed with patent foramen ovale: case report and review. Front. Cardiovasc. Med. 12:1666061. doi: 10.3389/fcvm.2025.1666061
Received
15 July 2025
Accepted
12 August 2025
Published
29 August 2025
Volume
12 - 2025
Edited by
Luca Spiezia, University of Padua, Italy
Reviewed by
Polina Kuznetsova, Research Center of Neurology (Russia), Russia
K. Parr, GW Medical Faculty Associates, United States
Updates
Copyright
© 2025 Zhao, Wang, Zhao, Tian, Zhai and Hu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mei Hu humei306@126.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.