- 1Department of CICU, Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, Guangzhou, Guangdong, China
- 2Department of Cardiac Surgery, Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, Guangzhou, Guangdong, China
- 3Department of Ultrasound Diagnostics, Sunshine Union Hospital, Affiliated Teaching Hospital of Weifang Medical University, Weifang, Shangdong, China
Objective: Various clinical indicators can increase the likelihood of early identification of fulminant myocarditis, the identification of which is important for early treatment.
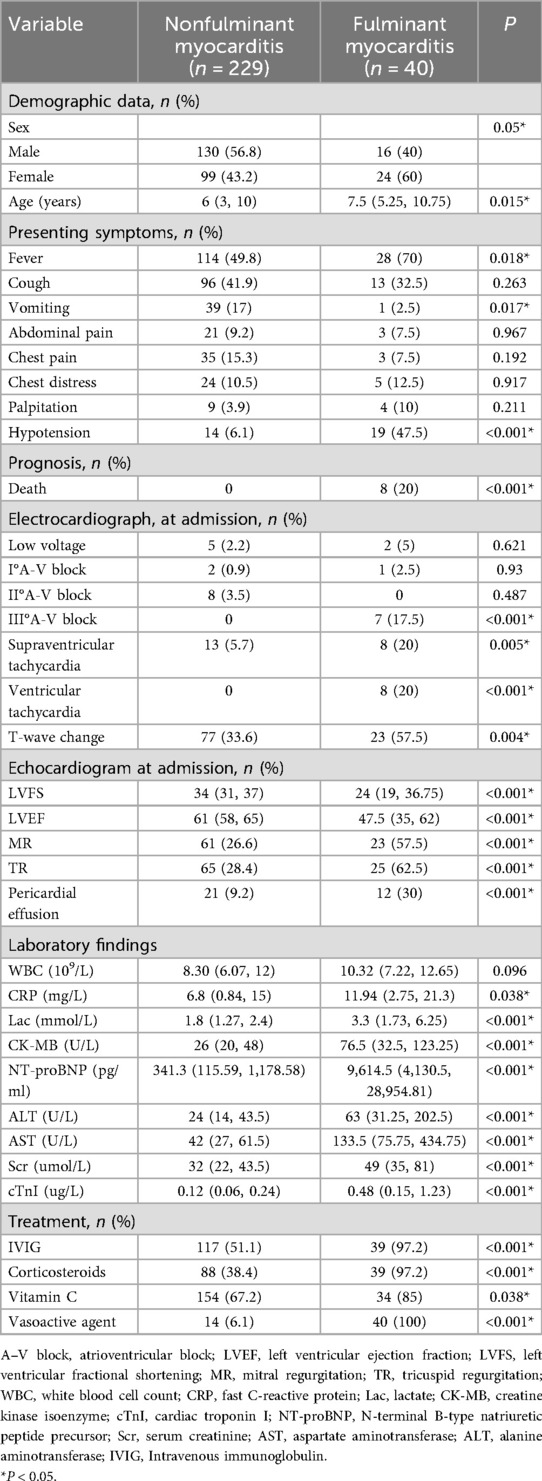
Method: The medical records of all patients (n = 269) who were diagnosed with acute myocarditis between January 2014 and December 2023 were retrospectively analyzed. Patients were divided into two groups: the nonfulminant myocarditis group (n = 229) and the fulminant myocarditis group (n = 40). Baseline demographics, laboratory findings, electrocardiograms, echocardiograms, and treatment regimens were compared between the two groups via multifactorial analysis. A receiver operating characteristic (ROC) curve was used to explore the predictive value of related factors.
Results: The median age of patients with fulminant myocarditis was significantly greater than that in the nonfulminant group (P = 0.015). The presenting symptoms at admission varied and included fever and respiratory, digestive, and circulatory symptoms. Among them, fever and hypotension were more common in the fulminant myocarditis group (P < 0.05), and vomiting was significantly more common in the nonfulminant myocarditis group (P = 0.017). Logistic regression analysis revealed that N-terminal pro-B-type natriuretic peptide (NT-proBNP), lactate (Lac), alanine aminotransferase (ALT), cardiac troponin I (cTnI), chest distress, and hypotension were early risk factors for fulminant myocarditis. ROC curve analysis demonstrated that NT-proBNP, ALT, cTnI, and Lac can serve as predictors for the early diagnosis of fulminant myocarditis. The optimal predictive values for these markers are 2,783.5 pg/ml for NT-pro BNP, 34.5 U/L for ALT, 0.2 µg/ml for cTnI, and 3.05 mmol/L for Lac.
Conclusions: This study revealed that NT-proBNP, cTnI, ALT, and Lac can serve as predictive factors for the early identification of fulminant myocarditis. These findings emphasize the importance of early identification and timely diagnosis for improving the overall prognosis of patients.
Introduction
Acute myocarditis in children can be caused by both infectious and noninfectious factors, with viral myocarditis being the most common cause (1–3). The clinical manifestations of acute myocarditis in children vary in severity. Children with mild myocarditis generally have a good prognosis. However, approximately 20% of children with fulminant myocarditis experience a sudden onset, leading to hemodynamic disorders and the need for circulatory auxiliary support (4). This condition can rapidly progress to refractory cardiogenic shock, lethal arrhythmic events, and even cardiac arrest, accounting for approximately 10%–38% of all acute myocarditis cases (5, 6). Currently, endocardial myocardial biopsy (EMB) remains the gold standard for diagnosing acute myocarditis. However, EMB is an invasive procedure that depends on the sampling site and has low sensitivity (7). More importantly, few institutions can perform this procedure and possess extensive relevant experience. As a result, it is difficult to widely promote this method in clinical practice (7). Previous studies have shown that LVEF, NT-proBNP, hypotension, and prolonged QRS are risk factors for identifying pediatric fulminant myocarditis in the early stage (5, 8). The aim of this study is to examine the early predictors of the collection of various clinical indicators can increase the likelihood of early identification of fulminant myocarditis, which is important for guiding early treatment.
Method
Study population
All patients admitted to Guangzhou Women and Children’s Medical Center, Guangzhou Medical University, with a diagnosis of acute myocarditis between January 2014 and December 2023 were retrospectively included in the analysis. The inclusion criteria were as follows: (1) age less than 18 years and (2) a diagnosis of acute myocarditis. According to the 2021 scientific statement of the American Heart Association (AHA), the typical diagnosis of acute myocarditis in children is ventricular dysfunction (with or without ventricular dilation), new-onset heart failure, and viral infection several weeks before onset (2). Currently, there are no clear diagnostic criteria for fulminant myocarditis in children; these criteria were based on the Chinese Medical Association Cardiovascular Society guidelines for adult fulminant myocarditis diagnosis and treatment, created with Chinese expert consensus. When acute myocarditis suddenly and rapidly progresses, severe heart failure, hypotension or cardiogenic shock soon appear, and the use of positive inotropic drugs, vascular active drugs or mechanical circulation adjuvant therapy can lead to a diagnosis of fulminant myocarditist (9). Thus, we classified acute myocarditis into fulminant myocarditis and nonfulminant myocarditis groups based on the severity of the condition. Ethical approval for the present study was granted by the Ethics Committee of Guangzhou Women and Children's Medical Center, Guangzhou Medical University (Approval No. 257A01). Informed consent was obtained from the parents or legal guardians.
Clinical data collection
The following clinical data were collected: demographic information; hemodynamic parameters; cardiac rhythm; and laboratory findings, including white blood cell (WBC) counts; and C-reactive protein (CRP), aminotransferase (AST), alanine aminotransferase (ALT), creatine kinase-MB isoenzyme (CK-MB), cardiac troponin I (cTnI), serum creatinine (Scr), N-terminal pro-B-type natriuretic peptide (NT-proBNP), and lactate (Lac) levels measured at admission. Twelve-lead electrocardiogram (ECG) and echocardiogram examinations were performed on all patients. All admitted patients received treatments, including intravenous immunoglobulin (IVIG), corticosteroids, and vitamin C. Vasoactive drugs were used for those with hypotension. For patients whose conditions remained critical after treatment, extracorporeal membrane oxygenation (ECMO) support was initiated, and some patients received continuous renal replacement therapy (CRRT) when indicated.
Statistical analysis
All the statistical analyses were performed using SPSS software, version 29.0, for Windows. Continuous variables are reported as the means ± SDs or medians and interquartile ranges, in line with a normal or non-normal distribution according to the Shapiro–Wilk normality test. Groups were compared via the unpaired Student's t test when normally distributed, whereas the Mann–Whitney U test was applied to those with a non-normal distribution. The Wilcoxon matched-paired signed-rank test was used to analyze paired data at different time points. Categorical variables were compared using Fisher's exact test. Factors with statistical significance in the univariate analysis and those considered clinically or previously significant were included in a logistic regression model for multivariate analysis. A receiver-operating characteristic (ROC) curve was used to explore the predictive value of related factors. A two-tailed P < 0.05 was considered statistically significant.
Results
Demographic features
A total of 269 patients were enrolled in this study. There were two groups: the nonfulminant myocarditis group (n = 229) and the fulminant myocarditis group (n = 40). The median age of patients with fulminant myocarditis was significantly greater than that of patients with nonfulminant myocarditis (p = 0.015). In the non-fulminant myocarditis group, age ranged from 3 months to 16 years, whereas in the fulminant myocarditis group it ranged from 1 year to 17 years. In this study, there were no neonatal patients. Age <3 years old, there were 79 patients. The presenting symptoms at admission varied and included fever and respiratory, digestive and circulatory symptoms. Among these patients, those with fever and hypotension were more likely to be in the fulminant myocarditis group (p < 0.05), and those with vomiting were significantly more likely to be in the nonfulminant myocarditis group (p = 0.017). Among all the patients, only 8 patients with fulminant myocarditis died (Table 1).
Electrocardiograms and echocardiograms
Approximately, 75.5% of patients had varying degrees of abnormal manifestations observed by electrocardiogram. Patients with fulminant myocarditis were significantly more likely to have severe arrhythmias with unstable circulation, including III°A–V block (p < 0.05), supraventricular tachycardia (P = 0.005), and ventricular tachycardia (p < 0.05). The left ventricular ejection fraction (LVEF) and left ventricular fractional shortening (LVFS) of patients with fulminant myocarditis were significantly lower than those of patients with nonfulminant myocarditis. The incidences of mitral regurgitation (MR), tricuspid regurgitation (TR), and pericardial effusion were significantly higher in patients with fulminant myocarditis (Table 1).
Laboratory data
Table 1 summarizes the results of the initial laboratory tests conducted at admission. Compared to the nonfulminant myocarditis group, the fulminant myocarditis group had significantly increased CRP, CK-MB, NT-proBNP, cTnI, ALT, AST, and Lac levels at admission (p < 0.05).
Early identification of risk factors for fulminant myocarditis
Logistic regression analysis suggested that hypotension, chest distress, Lac, ALT, cTnI and NT-proBNP were independent risk factors for fulminant myocarditis (Table 2). ROC curves revealed that NT-proBNP, cTnI, ALT, and Lac could predict independent risk factors for fulminant myocarditis. NT-proBNP had the strongest predictive value for risk factors, followed by ALT, cTnI and Lac (Figure 1, Table 3).
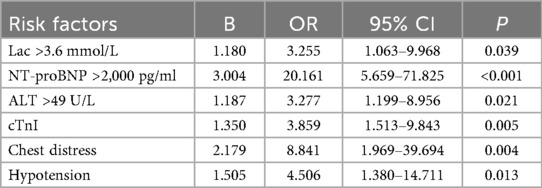
Table 2. Logistic regression analysis of early identification risk factors in the fulminant myocarditis.
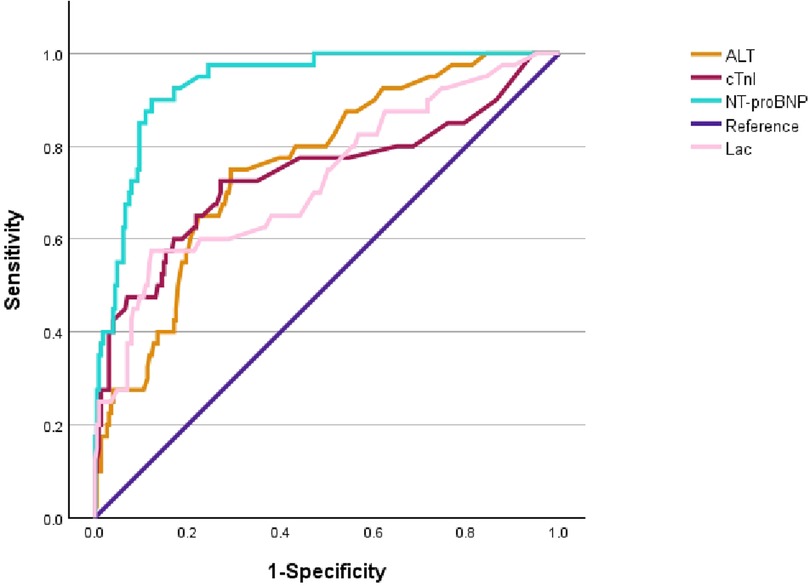
Figure 1. Receiver operating characteristic (ROC) curve analysis of early identification of fulminant myocarditis.
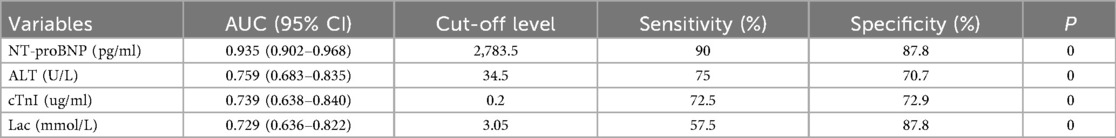
Table 3. Analysis of coincidence rate, sensitivity and specificity of NT-pro BNP, ALT, cTnI and Lac in the independent risk factors for the fulminant myocarditis.
Patient management
All patients received treatments, including IVIG (58.0%), corticosteroids (47.2%), vitamin C (69.9%), and vasoactive drugs (20.1%). However, ECMO was indicated for patients with severe heart failure, cardiac arrest and refractory shock, and some patients with combined renal failure received CRRT support. In the nonfulminant myocarditis group, the use of IVIG, corticosteroids, and vasoactive drugs by patients was significantly lower than that in the fulminant myocarditis group (Table 1).
ECMO was initiated in 19 patients, among whom 2 patients had temporary pacemakers installed before ECMO. 6 patients received CRRT due to renal failure. Notably, one patient with fulminant myocarditis was complicated because of also having Kawasaki disease (KD) (Table 4).
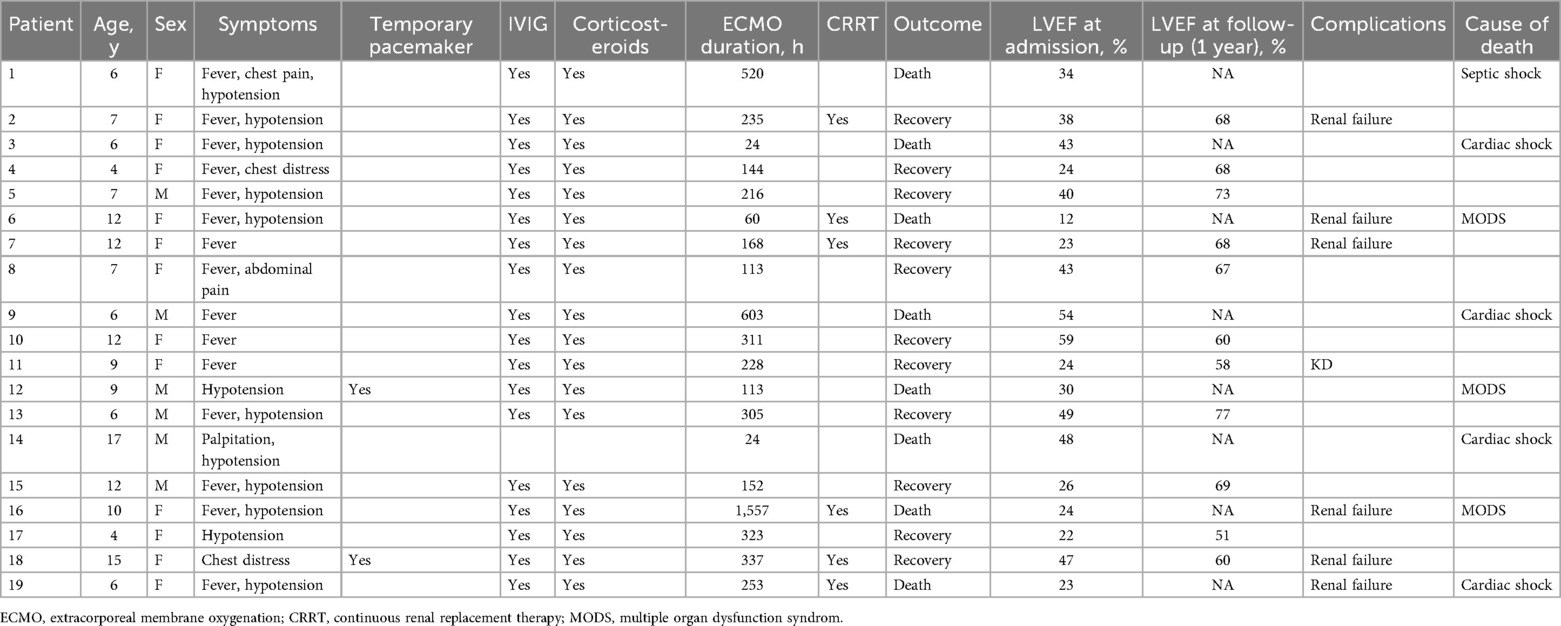
Table 4. Characteristics, treatment, and outcomes of ECMO in patients with the fulminant myocarditis.
Survival rate and follow-up
In this study, 8 patients died; the overall survival rate of patients with acute myocarditis was 97.03%. The survival rate of patients with fulminant myocarditis treated with ECMO was 57.89%. The causes of death were cardiac shock (n = 4), multiple organ dysfunction syndrome (n = 3), and septic shock (n = 1) (Table 4). Long-term follow-up of patients with fulminant myocarditis was performed. The median follow-up time was 3.5 yeas (range 8 months–9 years), and there were no late deaths or heart transplants. The follow-up method was echocardiography. There was no cardiac MR.
Among the 19 patients with fulminant myocarditis who required ECMO support, only one surviving patient exhibited delayed recovery of left ventricular function, however, by the third year of follow-up, the LVEF had still not returned to normal (LVEF < 55%). In contrast, all 21 patients with fulminant myocarditis who were managed without ECMO survived. Among the patients who survived from fulminant myocarditis, 31 of tnem had thier LVEF returned to normal 6 months after discharge.
Discussion
The incidence rate of acute myocarditis in children in China remains unknown. However, research reports indicate that the annual incidence rate of acute myocarditis in Japanese children is approximately 3 per 1,000,000 (10). Owing to the insidious onset of myocarditis in some children, the true incidence and prevalence of myocarditis in children may be underestimated (11). The early clinical symptoms of acute myocarditis in children have no obvious specificity. In this study, the clinical manifestations of patients upon admission were primarily respiratory symptoms such as cough and shortness of breath, and digestive symptoms such as nausea, vomiting, and abdominal pain. These symptoms were more prominent than those typically associated with cardiovascular diseases, which often led to misdiagnosis or missed diagnosis. In the fulminant myocarditis group, fever and vomiting were more common at onset. Children with fulminant myocarditis often experience rapid symptom progression, which may include severe hemodynamic disturbances (12). This study revealed that children in the fulminant myocarditis group were more prone to hypotension than those in the nonfulminant myocarditis group.
Acute myocarditis lacks specific diagnostic methods, and myocardial injury markers are often used as reference indicators for the diagnosis of acute myocarditis. NT-proBNP is an indicator that reflects the left ventricular end-diastolic pressure and measures the filling pressure in the heart's main pump chamber (13). It is secreted by ventricular myocytes in response to volume or pressure overload to counteract the effects of the renin-angiotensin-aldosterone system and the sympathetic nervous system during heart failure (14). Therefore, NT-proBNP can serve as a key prognostic factor for evaluating disease severity and patient outcomes (15). cTn is currently the marker with the highest specificity for diagnosing myocardial injury that has been discovered. cTnI is released into the blood in the early stage of myocardial injury, begins to increase at 3–12 h and reaches its peak at 12–24 h; the detection window lasts for 7–14 days. Although elevated cTnI is a good biomarker for myocarditis, higher levels are not associated with the severity of the disease. In a multicenter review of pediatric myocarditis, the cTnI level in patients with mild ventricular dysfunction was significantly higher than that in patients with moderate or severe ventricular dysfunction (16). Sachdeva et al. reported no association between cTnI levels and outcomes in a single-center retrospective study, and late enhancement on CMR was a risk factor for poor prognosis in the early or late stages of myocarditis (17). Therefore, elevated cTnI levels should be considered an important indicator for the diagnosis of myocarditis, but should not be used to classify its severity or predict prognosis. Lactic acid, a product of anaerobic glycolysis, plays a crucial role in metabolism and exercise. It is a common laboratory indicator that shows the severity of different diseases (18). Lactate has become useful as a risk factor for predicting patient mortality and an important prognostic indicator in intensive care settings (19, 20). In this study, almost half of the patients with acute myocarditis presented elevated transaminase levels, which may be associated with shock and congestive heart failure or could be caused by the same viral triggers responsible for myocarditis. A retrospective single-center pediatric study revealed that serum AST levels were elevated in children with myocarditis (20). However, in our study, we found that the increase in ALT was more obvious. Previous studies have reported that serum markers reflecting the inflammatory state of the heart and the function of terminal organs, including troponin-I, liver enzymes, creatinine, and serum lactic acid, are correlated with the course of the disease (21, 22). This study suggested that NT-proBNP, ALT, cTnI, and Lac can serve as predictors for the early diagnosis of fulminant myocarditis. The optimal predictive values for these markers are 2,783.5 pg/ml for NT-proBNP, 34.5 U/L for ALT, 0.2 µg/ml for cTnI, and 3.05 mmol/L for Lac. In previous studies, Moises et al. reported that NT-proBNP can predict risk factors for the early identification of fulminant myocarditis. The test AUC was 0.931, the optimal cutoff value was 2,000 ng/ml, the sensitivity was 90%, and the specificity was 81% (23). Lee et al. reported that the lactate level before ECMO can predict risk factors for cardiac arrest death, with an AUC of 0.848, an optimal cutoff value of 79.8 mg/dl, a sensitivity of 70%, and a specificity of 91% (4). Relevant studies on cTnI have been conducted in adults with myocarditis, indicating that elevated cTnI has a very low sensitivity (34%) for the entire myocardial group, but the specificity is satisfactory (89%) (24). Freedman also reported that AST measurement might be a useful laboratory-assisted means, reporting sensitivity in 85% of patients with myocarditis. The median AST value in the determined group was 66 U/L, and that in the possible group was 116 U/L (20). However, no reports related to ALT levels have been published.
Acute myocarditis can damage the myocardium, and surrounding tissues, leading to ventricular systolic dysfunction. It can also simultaneously affect the cardiac conduction system, causing changes in automaticity and conductivity (25). In this study, the fulminant myocarditis group was more prone to supraventricular tachycardia, ventricular tachycardia, and III° atrioventricular block than the nonfulminant myocarditis group (57.5%). Teele et al. previously reported (26) that approximately 55% (11/20) of pediatric patients with fulminant myocarditis have ventricular tachycardia and Ⅲ° atrioventricular block. This finding is consistent with previous research results. Echocardiography is an important tool for evaluating cardiac function. As the disease progresses, patients may exhibit abnormal left ventricular systolic function, a decreased ejection fraction, reduced ventricular wall motion, valvular regurgitation, and pericardial effusion (27). In this study, statistically significant differences were observed in LVEF, LVFS, MR, TR, and pericardial effusion between the fulminant myocarditis group and the nonfulminant myocarditis group.
Currently, there are no specific drugs for the treatment of myocarditis. The main treatment, including corticosteroids and IVIG, is symptomatic and only supportive. A recent retrospective analysis of 112 pediatric patients with myocarditis indicated that the combination of IVIG and high-dose corticosteroids is beneficial for improving left ventricular systolic function, with no obvious serious adverse events reported (28). However, currently, there is still controversy regarding the use of both treatments (29). In this study, the utilization rates of early IVIG and corticosteroids in the nonfulminant myocarditis group were 51.1% and 28.4%, respectively. In contrast, in the fulminant myocarditis group, IVIG and corticosteroids were administered to all patients except one, and they achieved noticeable effects. Some patients with fulminant myocarditis experience rapid disease progression. Even with timely drug treatment, circulation challenges remain difficult to correct in some patients, necessitating ECMO support to maintain circulation and allow time for myocardial recovery. The survival rate of patients with pediatric fulminant myocarditis treated with ECMO ranges from 64.3% to 83.3% (30, 31). Among patients with fulminant myocarditis, 19 received ECMO treatment, and there were a total of 8 deaths. The ECMO survival rate was 57.9%, slightly lower than the rates reported in the previous literature. This may be attributed to the relatively recent development and potentially limited experience with ECMO technology. At the onset of the disease, 2 patients were initially fitted with temporary pacemakers to support III° atrioventricular block. However, as cardiac output and tissue perfusion could not be effectively restored, ECMO circulatory assistance was eventually initiated. Additionally, 6 patients were treated with CRRT simultaneously, but due to the severity of their conditions, 3 of them still died.
Among patients with fulminant myocarditis, one patient had concomitant Kawasaki disease (KD), which is particularly noteworthy. After the patient was diagnosed with fulminant myocarditis, IVIG and corticosteroid therapy were immediately administered. At 15 days after ECMO withdrawal, the patient developed a fever, a diffuse red miliary rash on the trunk, red and chapped lips, swelling of the hands and feet, and enlarged cervical lymph nodes. Echocardiography revealed the formation of small aneurysms in the left coronary artery (Figure 2). Therefore, the diagnosis of KD was confirmed according to diagnostic criteria. Myocarditis often occurs in patients with KD. A previous study revealed that the incidence of myocarditis in individuals with KD can reach 50% (32). Generally, myocarditis in KD patients is self-limiting or well managed with IVIG. This type of myocarditis is mostly mild and is accompanied by subclinical left ventricular dysfunction. However, in a small number of patients, left ventricular dysfunction can be observed, leading to congestive heart failure or cardiogenic shock (33). However, based on the patient's medical history and the course of the disease, the pathogenesis remains unclear.
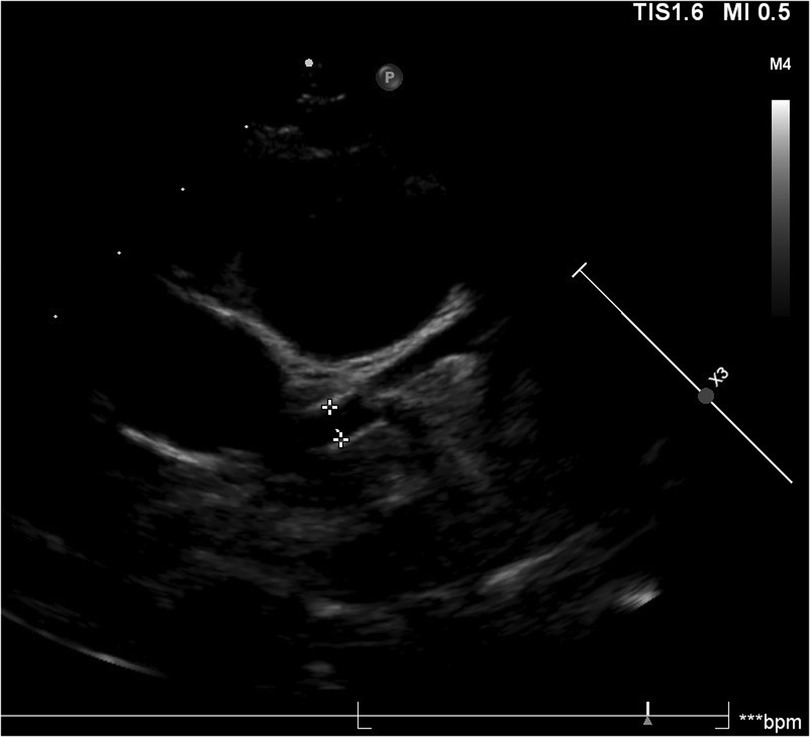
Figure 2. Images of small aneurysms in patient with concomitant kawasaki disease. On the 20th day of the disease course, the patient presented with fever, generalized diffuse rash, red and chapped lips, bayberry tongue, bilateral cervical lymph node enlargement and swelling of hands and feet, and diagnosed with KD. On the second day after the diagnosis of KD, echocardiography revealed that the left coronary artery small aneurysms (Z = 2.53).
Most patients with myocarditis have a good prognosis and can be cured. However, approximately 16% of patients are at increased risk of developing cardiomyopathy during the follow-up period (23, 33, 34). Studies have shown that patients with acute myocarditis have a good long-term prognosis if effective treatment is given in the early stage of the acute phase (35). In this study, long-term follow-up of patients with fulminant myocarditis was conducted by this center. The median follow-up duration was 3.5 years (range 8 months–9 years), during which no late deaths or heart-transplant procedures occurred. The functional recovery mainly occurs in the first few weeks of the disease, which means that rapid therapeutic intervention is necessary. Surveillance relied on serial echocardiography. Cardiac MRI was not performed. However, during the subsequent follow-up visits, cardiac MR examinations will be gradually conducted. This has been listed by us as one of the directions for further research in the future. In this study, the LVEF of one patient still had not returned to normal (LVEF < 55%) at the 3rd year of follow-up, while the EF values of the remaining patients returned to normal within half a year after discharge.
This study has several limitations. Acute myocarditis was diagnosed clinically without confirmation through myocardial biopsy. Furthermore, the incidence of fulminant myocarditis is low, resulting in a small sample size. This may introduce certain biases into the results, and a larger sample size with a multicenter design is needed for further research. Additionally, owing to incomplete follow-up data, it is not possible to evaluate the long-term outcomes of patients with acute myocarditis.
Conclusions
Early identification of fulminant myocarditis, coupled with timely administration of effective treatment measures, can significantly improve patient prognosis. In this study, the survival rate of patients with acute myocarditis reached 100%, whereas that of patients with fulminant myocarditis was 80%. This study focused on the follow-up of patients with fulminant myocarditis. During the follow-up period, no deaths were reported. However, the LVEF of one patient had not yet fully normalized. NT-proBNP, cTnI, ALT, and Lac can serve as predictive factors for the early identification of fulminant myocarditis. These findings emphasize the importance of early identification and timely diagnosis in improving the overall prognosis of myocarditis patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Guangzhou Women and Children's Medical Center, Guangzhou Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
JY: Writing – original draft, Methodology, Writing – review & editing. ML: Data curation, Writing – review & editing. LM: Writing – review & editing, Methodology, Funding acquisition. ZW: Writing – review & editing, Investigation, Software. YW: Resources, Writing – review & editing. YH: Writing – review & editing, Data curation. ZY: Validation, Writing – review & editing. NZ: Writing – review & editing, Formal analysis, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Guangzhou Major clinical technology project (2023C-ZD10). Guanghzou Science and Technology Bureau Project (2024A03J1165). The Basic and Applied Basic Research Project of Guangzhou Municiple Sccience and Technology Bureau (2025A03J4265).
Acknowledgments
We would like to thank the Guangzhou Women and Children's Medical Center, Guangzhou Medical University for proving support and guidance. The above opinions are those of the authors alone.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Law YM, Lal AK, Chen S, Chen S. Diagnosis and management of myocarditis in children: a scientific statement from the American Heart Association. Circulation. (2021) 144(6):e123–35. doi: 10.1161/CIR.0000000000001001
3. Ammirati E, Moslehi JJ. Diagnosis and treatment of acute myocarditis: a review. JAMA. (2023) 329(13):1098–113. doi: 10.1001/jama.2023.3371
4. Lee EP, Chu SC, Huang WY, Hsia S-H, Chan O-W, Lin C-Y, et al. Factors associated with in-hospital mortality of children with acute fulminant myocarditis on extracorporeal membrane oxygenation. Front Pediatr. (2020) 8(8):488. doi: 10.3389/fped.2020.00488
5. Lee EJ, Lee HL, Kim HT, Lee HD, Park JA. Clinical features and short-term outcomes of pediatric acute fulminant myocarditis in a single center. Korean J Pediatr. (2014) 57(11):489–95. doi: 10.3345/kjp.2014.57.11.489
6. Zhao YH, Da M, Yang X. A retrospective analysis of clinical characteristics and outcomes of pediatric fulminant myocarditis. BMC Pediatr. (2024) 24(1):553. doi: 10.1186/s12887-024-05022-4
7. Fung G, Luo H, Qiu Y, Yang D, McManus B. Myocarditis. Cir Red. (2016) 118(3):496–514. doi: 10.1161/CIRCRESAHA.115.306573
8. Kwon HW. When should mechanical circulatory support be considered in pediatric patients with acute fulminant myocarditis? Clin Exp Pediatr. (2021) 64(5):227–8. doi: 10.3345/cep.2020.01165
9. Section of Precision Medical of Chinese Society of Cardiology of Chinese Medical Association, Editorial Board of Chinese Journal of Cardiology, Working Group on Adult Myocarditis. Chinese Expert consensus statement on clinical diagnosis and treatment of fulminant myocarditis in adults. Chin J Cardiol. (2017) 45:742–52. doi: 10.3760/cma.j.issn.0253-3758.2017.09.004
10. Nagai T, Inomata T, Kohno T, Sato T, Tada A, Kubo T, et al. JCS 2023 Guideline on the diagnosis and treatment of myocarditis. Cir J. (2023) 87(5):674–754. doi: 10.1253/circj.CJ-22-0696
11. Putschoegl A, Auerbach S. Diagnosis, evaluation, and treatment of myocarditis in children. Pediatr Clin N Am. (2020) 67(5):855–74. doi: 10.1016/j.pcl.2020.06.013
12. Arola A, Pikkarainen E, Sipilä JO, Pykäri J, Rautava P, Kytö V. Occurrence and features of childhood myocarditis: a nationwide study in Finland. J Am Heart Assoc. (2017) 6(11):e005306. doi: 10.1161/JAHA.116.005306
13. Hsich EM, Grau-Sepulveda MV, Hernandez AF, Eapen ZJ, Xian Y, Schwamm LH, et al. Relationship between sex, ejection fraction, and B-type natriuretic peptide levels in patients hospitalized with heart failure and associations with inhospital outcomes: findings from the get with the guideline-heart failure registry. Am Heart J. (2013) 166(6):1063–71.e3. doi: 10.1016/j.ahj.2013.08.029
14. Fu SH, Ping P, Zhu QW. Brain natriuretic peptide and its biochemical, analytical, and clinical issues in heart failure: a narrative review. Front Physiol. (2018) 9:692. doi: 10.3389/fphys.2018.00692
15. Li XO, Tuo H, Huang YJ, Li Y, Zhao N, Wang J, et al. The diagnosis and treatment of pediatric clinical myocarditis in China: a multicenter retrospective study. Eur J Pediatr. (2024) 183(3):1233–44. doi: 10.1007/s00431-023-05362-w
16. Butts RJ, Boyle GJ, Deshpande SR, Gambetta K, Knecht KR, Prada-Ruiz CA, et al. Characteristics of clinically diagnosed pediatric myocarditis in a contemporary multi-center cohort. Pediatr Cardiol. (2017) 38(6):1175–82. doi: 10.1007/s00246-017-1638-1
17. Sachdeva S, Song XY, Dham N, Heath DM, DeBiasi RL. Analysis of clinical parameters and cardiac magnetic resonance imaging as predictors of outcome in pediatric myocarditis. Am J Cardiol. (2015) 115(4):499–504. doi: 10.1016/j.amjcard.2014.11.029
18. Andersen LW, Mackenhauer J, Roberts JC, Berg KM, Cocchi MN, Donnino MW. Etiology and therapeutic approach to elevated lactate levels. Mayo Clin Proc. (2013) 88(10):1127–40. doi: 10.1016/j.mayocp.2013.06.012
19. Bao L, Zhang M, Yan PX, Wu X, Shao J, Zheng R. Retrospective analysis of the value of arterial blood lactate level and its clearance rate on the prognosis of septic shock patients. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2015) 27(1):38–42. doi: 10.3760/cma.j.issn.2095-4352.2015.01.009
20. Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J. Pediatric myocarditis: emergency department clinical findings and diagnostic evaluation. Pediatrics. (2007) 120(6):1278–85. doi: 10.1542/peds.2007-1073
21. Duncan BW, Bohn DJ, Atz AM, French JW, Laussen PC, Wessel DL. Mechanical circulatory support for the treatment of children with acute fulminant myocarditis. J Thorac Cardiovasc Surg. (2001) 122(3):440–8. doi: 10.1067/mtc.2001.115243
22. Canter CE, Simpson KE. Diagnosis and treatment of myocarditis in children in the current era. Circulation. (2014) 129(1):115–28. doi: 10.1161/CIRCULATIONAHA.113.001372
23. Rodriguez-Gonzalez M, Sanchez-Codez MI, Lubian-Gutierrez M, Castellano-Martinez A. Clinical presentation and early predictors for poor outcomes in pediatric myocarditis: a retrospective study. World J Clin Cases. (2019) 7(05):548–61. doi: 10.12998/wjcc.v7.i5.548
24. Smith SC, Ladenson JH, Mason JW, Jaffe AS. Elevations of cardiac troponin I associated with myocarditis: experimental and clinical correlates. Circulation. (1997) 95(1):163–8. doi: 10.1161/01.CIR.95.1.163
25. Ichikawa R, Sumitomo N, Komori A, Abe Y, Nakamura T, Fukuhara J, et al. The follow-up evaluation of electrocardiogram and arrhythmias in children with fulminant myocarditis. Circ J. (2011) 75(4):932–8. doi: 10.1253/circj.CJ-10-0918
26. Teele SA, Allan CK, Laussen PC, Newburger JW, Gauvreau K, Thiagarajan RR. Management and outcomes in pediatric patients presenting with acute fulminant myocarditis. J Pediatr. (2011) 158(4):638–43. doi: 10.1016/j.jpeds.2010.10.015
27. Melao F, Paiva M, Pinho T, Goncalves A, Madureira A, Martins E, et al. Late left ventricular systolic dysfunction in patients with acute myocarditis: echocardiographic and cardiac magnetic resonance predictors. Eur Heart J. (2013) 34(Suppl 1):P3862. doi: 10.1093/eurheartj/eht309.P3862
28. Schauer J, Newland D, Hong B, Albers E, Friedland-Little J, Kemna M, et al. Treating pediatric myocarditis with high dose steroids and immunoglobulin. Pediatr Cardiol. (2023) 44(2):441–50. doi: 10.1007/s00246-022-03004-w
29. Li YT, Yang LF, Chen ZG, Pan L, Duan M-Q, Hu Y, et al. ECMO as an effective rescue therapeutic for fulminant myocarditis complicated with refractory cardiac arrest. Ther Clin Risk Manag. (2017) 13:1507–11. doi: 10.2147/TCRM.S147845
30. Asaumi Y, Yasuda S, Morii I, Kakuchi H, Otsuka Y, Kawamura A, et al. Favourable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation. Eur Heart J. (2005) 26(20):2185–92. doi: 10.1093/eurheartj/ehi411
31. Nahum E, Dagan O, Lev A, Shukrun G, Amir G, Frenkel G, et al. Favorable outcome of pediatric fulminant myocarditis supported by extracorporeal membranous oxygenation. Pediatr Cardiol. (2010) 31(7):1059–63. doi: 10.1007/s00246-010-9765-y
32. Yoshikawa H, Nomura Y, Masuda K, Hazeki D, Yotsumoto K, Arata M, et al. Four cases of kawasaki syndrome complicated with myocarditis. Circ J. (2006) 70(2):202–5. doi: 10.1253/circj.70.202
33. Veronese G, Ammirati E, Cipriani M, Frigerio M. Fulminant myocarditis: characteristics, treatment, and outcomes. Anatol J Cardiol. (2018) 19(4):279–86. doi: 10.14744/AnatolJCardiol.2017.8170
34. Ammirati E, Cipriani M, Lilliu M, Sormani P, Varrenti M, Raineri C, et al. Survival and left ventricular function changes in fulminant versus nonfulminant acute myocarditis. Circulation. (2017) 136(6):529–45. doi: 10.1161/CIRCULATIONAHA.117.026386
Keywords: acute myocarditis, fulminant myocarditis, children, factors risk, clinical indicators
Citation: Yuan J, Li M, Ma L, Wu Z, Wu Y, Huang Y, Yin Z and Zhou N (2025) Early clinical predictors of fulminant myocarditis in pediatric patients: a retrospective cohort study. Front. Cardiovasc. Med. 12:1678220. doi: 10.3389/fcvm.2025.1678220
Received: 2 August 2025; Accepted: 29 September 2025;
Published: 9 October 2025.
Edited by:
Harvey Ho, University of Auckland, New ZealandReviewed by:
Nesrine Farhat, University Hospital of Liège, BelgiumStiljan Hoxha, University of Verona, Italy
Copyright: © 2025 Yuan, Li, Ma, Wu, Wu, Huang, Yin and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Zhou, MjAyMzc2MTEwMkBnemhtdS5lZHUuY24=
 Jia Yuan
Jia Yuan Ming Li1
Ming Li1 Yujian Wu
Yujian Wu