- 1Department of General Surgery, Wuhan Children’s Hospital (Wuhan Maternal and Child Healthcare Hospital), Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2School of Medicine, Jianghan University, Wuhan, China
Background: Postoperative intussusception (PI) is a rare but potentially serious complication following congenital heart surgery in infants, often misdiagnosed due to its atypical presentation.
Case presentation: A 3-month-old male infant underwent aortoplasty, ventricular septal defect (VSD) repair, and patent ductus arteriosus (PDA) ligation for congenital heart disease. Approximately 72 h postoperatively, he developed bloody, jam-like stools. Emergency abdominal ultrasound, the first-line imaging modality, revealed ileocolic intussusception. Three attempts at ultrasound-guided hydrostatic saline enema reduction (pressure: 80 cm H2O) were unsuccessful, necessitating surgical exploration. Laparotomy identified an 8 cm ileocolic intussusceptum and a 10 cm ischemic ileal segment without a pathological lead point. The necrotic bowel was resected, and an end-to-end anastomosis was performed. The patient recovered uneventfully, was discharged three weeks postoperatively, and demonstrated normal growth at 6-month follow-up.
Conclusion: Prompt identification of postoperative intussusception—a rare complication following non-abdominal surgeries like congenital heart disease repair in infants—is of critical importance.
1 Introduction
Postoperative intussusception (PI) is an uncommon complication in children, accounting for approximately 2% of all pediatric intussusception cases (1). Most PI cases are associated with previous abdominal surgery, although isolated occurrences have been reported after thoracic (including cardiac) or cervical procedures (1, 2). Intussusception itself is the most frequent cause of acute intestinal obstruction in infants, with an incidence of 0.3–0.7 per 1,000 live births. Approximately 90%–95% of pediatric intussusception cases are idiopathic, while only 5%–10% are related to identifiable pathological lead points such as polyps or Meckel's diverticulum (3). PI following cardiac surgery is particularly rare. Its pathogenesis is believed to be multifactorial, involving transient intestinal dysmotility induced by anesthetics or opioids, mesenteric hypoperfusion during cardiopulmonary bypass, postoperative inflammation, and electrolyte imbalance (2, 4). Unlike primary intussusception, PI often lacks the classic triad of abdominal pain, vomiting, and bloody stool. Instead, it usually presents with nonspecific signs of progressive intestinal obstruction, which may easily be mistaken for adhesive obstruction (1). This case report, prepared in accordance with the CARE checklist, highlights the diagnostic and therapeutic challenges of postoperative ileocolic intussusception occurring shortly after congenital heart surgery in an infant.
2 Case presentation
2.1 Patient information
A 3-month-old male infant (weight: 5.1 kg; height: 58 cm) was admitted to the Cardiac Surgery Department of Wuhan Children's Hospital in April 2020. He was born at term via spontaneous vaginal delivery with an uneventful perinatal history (Apgar scores: 9 at 1 min, 10 at 5 min). Cyanosis of the lips had been noted since birth and worsened during crying. Preoperative anthropometric measurements were within normal limits for age.
2.2 Clinical timeline
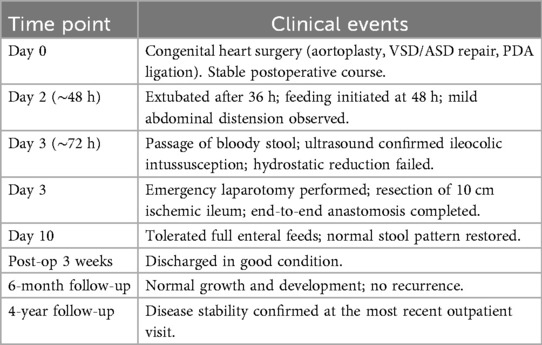
Refer to Table 1.
2.3 Diagnostic assessment and therapeutic interventions
Preoperative echocardiography revealed aortic coarctation, dilated pulmonary artery, a 10.4 mm VSD, a 5 mm ASD, mild tricuspid regurgitation, mild-to-moderate pulmonary valve regurgitation, mild-to-moderate pulmonary hypertension (mean pulmonary artery pressure: 35 mmHg), and a normal left ventricular ejection fraction (65%) (Figure 1A). The patient's hemodynamic condition was stable, with oxygen saturation of 95%–98% in room air and no clinical evidence of heart failure (e.g., hepatomegaly or peripheral edema). Following exclusion of surgical contraindications, the patient underwent aortoplasty, VSD repair with a tissue patch, ASD repair, and PDA ligation. General anesthesia was maintained with sevoflurane, fentanyl, propofol, and oxycodone. Cardiopulmonary bypass (CPB) was established for 93 min with an aortic cross-clamp time of 76 min. Myocardial protection was achieved with cold crystalloid cardioplegia. Analgesia was provided with low-dose fentanyl (1 µg/kg/h for 48 h). The patient was extubated after 36 h, and enteral feeding commenced 48 h postoperatively. At approximately 72 h postoperatively, physical examination revealed abdominal distension and mild tenderness in the right lower quadrant without guarding or rebound tenderness. Laboratory results showed elevated CRP (35 mg/L; pre-op 10 mg/L), normal white blood cell count (12.5 × 10⁹/L), and normal electrolytes (K+ 3.5 mmol/L; Na+ 138 mmol/L). Emergency abdominal ultrasound (7.5 MHz transducer) demonstrated the characteristic “target sign” and “pseudokidney sign” in the right lower quadrant, confirming ileocolic intussusception (Figure 1B).
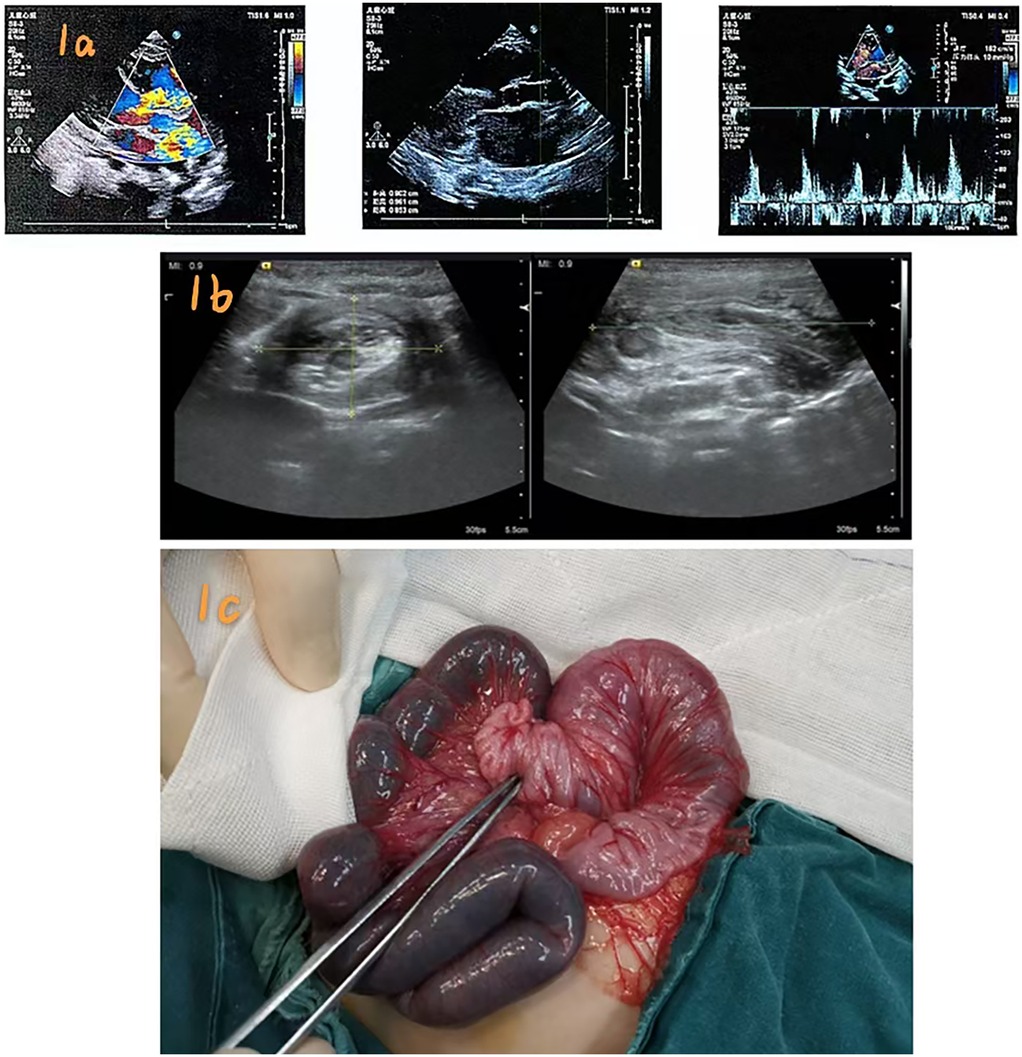
Figure 1. (a) Preoperative echocardiography findings; (b) Ultrasound “target sign” confirming ileocolic intussusception; (c) Intraoperative view showing ischemic ileum and intussuscepted segment.
Differential diagnoses included: (1) adhesive obstruction—excluded due to the absence of previous abdominal surgery and the typical ultrasound “target sign”; (2) necrotizing enterocolitis—ruled out given normal bowel sounds, no fever, and the absence of pneumatosis intestinalis; (3) malrotation/volvulus—excluded based on normal superior mesenteric vein orientation on ultrasound. Ultrasound-guided hydrostatic reduction was attempted using warm saline (37 °C) infused through a Foley catheter under a controlled pressure of 80 cm H2O. Three 10 min attempts were made, but the “target sign” persisted, indicating reduction failure. Due to ongoing symptoms and the risk of bowel ischemia, urgent laparotomy was performed.
Intraoperatively, a transverse abdominal incision revealed an 8 cm ileocolic intussusception with approximately 10 cm of proximal ileum showing dark purple discoloration consistent with ischemic necrosis. Exploration of the entire intestine revealed no Meckel's diverticulum, polyps, or hypertrophied Peyer's patches (Figure 1C). The ischemic segment was resected, and primary end-to-end anastomosis was performed using 5–0 absorbable sutures. Histopathological examination showed transmural ischemic necrosis, mucosal hemorrhage, and submucosal edema, with no evidence of a pathological lead point. The postoperative course was uneventful. The patient tolerated full enteral feeds by day 10 and was discharged three weeks postoperatively. At 6-month and 4-year follow-up visits, he remained asymptomatic, with normal growth and no recurrence.
3 Discussion
The pathogenesis of PI following cardiac surgery is multifactorial. In this case, three mechanisms likely contributed: (1) opioid-induced hypoperistalsis due to continuous fentanyl infusion (2); (2) mesenteric hypoperfusion related to prolonged cardiopulmonary bypass and aortic cross-clamp (4); (3) early enteral feeding that may have triggered premature intestinal motility (1). Age is a key determinant in pediatric intussusception. Idiopathic cases predominate in infants younger than 1 year, while pathological lead points are more common in older children. In contrast to primary intussusception, PI often presents with nonspecific symptoms and lacks the classic triad, increasing the risk of misdiagnosis (1, 2). Ultrasound is the diagnostic modality of choice, offering high sensitivity and specificity without radiation exposure. Computed tomography should be reserved for equivocal cases or when bowel necrosis is suspected (2, 4). A review of 15 pediatric PI cases following cardiac surgery (2018–2025) showed that early diagnosis and timely surgery are key to favorable outcomes, while delays beyond 72 h significantly increase the risk of bowel necrosis (2).
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by Ethics Committee of Wuhan Children's Hospital (Wuhan Maternal and Child Healthcare Hospital), Tongji Medical College, Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
HL: Writing – original draft. MK: Writing – original draft. JY: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kaya C, Karabulut R, Turkyilmaz Z, Sonmez K. Roux limb intussusception: a rare postoperative complication. Afr J Paediatr Surg. (2023) 20(3):241–2. doi: 10.4103/ajps.ajps_100_21
2. Kannaiyan L, Jayaram H, Deb M. Unusual presentation of postoperative intussusception in two infants. J Indian Assoc Pediatr Surg. (2022) 27(4):503–4. doi: 10.4103/jiaps.jiaps_164_21
3. Arena S, Cassaro F, Maisano G, Impellizzeri P, Romeo C. Recurrent ileocolic intussusception in children: a scoping review. Int J Pediatr. (2025) 2025:8860000. doi: 10.1155/ijpe/8860000
Keywords: postoperative intussusception, congenital heart disease, infant, ileocolic, ultrasound, laparotomy
Citation: Li H, Ke M and Yang J (2025) Postoperative ileocolic intussusception 48 hours after congenital heart surgery in an infant: a case report. Front. Cardiovasc. Med. 12:1679567. doi: 10.3389/fcvm.2025.1679567
Received: 4 August 2025; Accepted: 29 October 2025;
Published: 12 November 2025.
Edited by:
Salvatore Arena, University of Messina, ItalyReviewed by:
Fabiola Cassaro, University of Messina, ItalyReza Aditya Digambiro, Trisakti University, Indonesia
Copyright: © 2025 Li, Ke and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huan Li, ZXJ3YWlsaWh1YW5AMTYzLmNvbQ==; Jun Yang, eWFuZzEyMzkxQHRvbS5jb20=
†These authors have contributed equally to this work and share first authorship
 Huan Li1*†
Huan Li1*† Mengyu Ke
Mengyu Ke