Abstract
Malposition of pacemaker leads into the left heart is a rare but clinically significant complication that can lead to systemic thromboembolism. We report the case of a 78-year-old woman who underwent emergency pacemaker implantation due to sinus node dysfunction. Post-procedural imaging incidentally revealed lead malposition into the left heart. Further investigation using transthoracic and transesophageal echocardiography, along with computer tomography, identified a sinus venosus defect and partial anomalous pulmonary venous drainage. Moreover, malposition of the pacemaker leads was confirmed. Given the patient's age, frailty, and absence of thromboembolic events or significant symptoms, a conservative approach was chosen, and lifelong anticoagulation with warfarin was initiated. Surgical intervention and lead extraction were deferred due to high procedural risk. The patient remained clinically stable with preserved pacemaker function and no complications during follow-up. This case underscores the importance of imaging in detecting anomalies associated with pacemaker lead malposition. Management should be individualized, balancing procedural risk against the potential for thromboembolism.
Introduction
Malposition of pacemaker leads into the left ventricle is uncommon. In most cases, inadvertent lead placement into the left heart occurs through congenital defects such as a patent foramen ovale or various types of atrial septal defects. Many patients with malpositioned leads remain asymptomatic (1, 2). However, this anomaly may increase the risk of adverse cardiovascular events such as transient ischemic attacks, strokes, and cardiac perforation leading to tamponade (3). We present a case in which malpositioned pacemaker leads incidentally led to the diagnosis of previously unrecognized partial anomalous pulmonary venous drainage (PAPVD).
Case report
A 78-year-old woman was admitted to our institution 2 weeks after undergoing emergency cardiac pacemaker implantation for evaluation and management of inadvertently positioned pacing leads in the left side of the heart.
The patient's medical history included single-vessel coronary artery disease without prior myocardial infarction, along with well-controlled hypertension. A cardiac pacemaker was implanted in April 2025 due to sinus node dysfunction. The day after pacemaker implantation, a chest x-ray showed a left-sided pneumothorax, which was managed with thoracocentesis. Transthoracic echocardiography (TTE) revealed malpositioned pacing leads within the left heart chambers. Consequently, the patient was referred to our institution for further diagnosis and treatment. The patient was admitted with complaints of dyspnea and fatigue. On physical examination, heart sounds were normal with no murmurs. Lungs were clear to auscultation bilaterally. There was no pedal edema. Before hospitalization, the patient had been receiving rivaroxaban as anticoagulation therapy.
A blood test revealed an elevated level of NT-proBNP 502 pg/mL. The chest x-ray demonstrated that the pacing lead followed an atypical course (Figure 1). TTE showed abnormal lead positioning, dilatation of right heart chambers, and moderate tricuspid regurgitation.
Figure 1
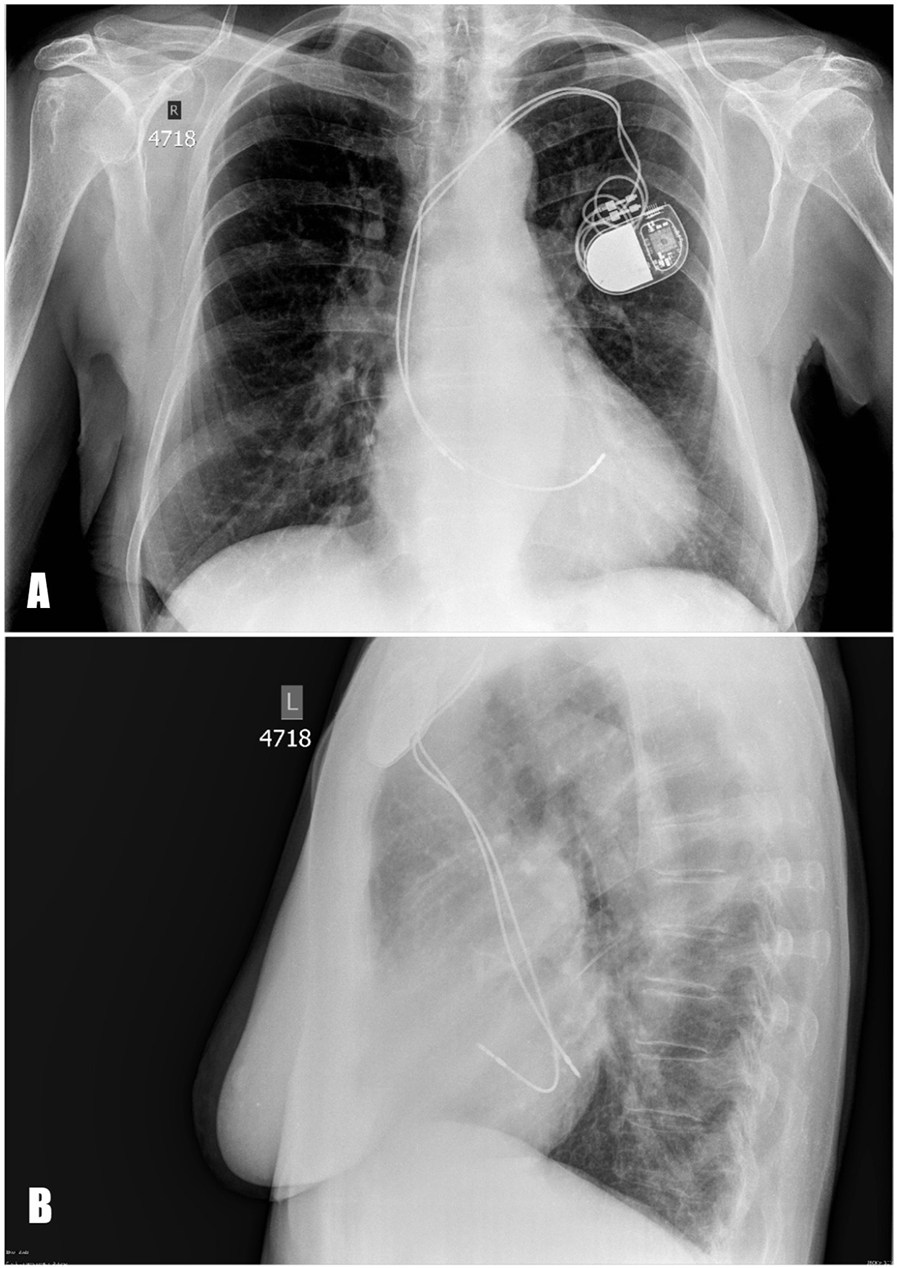
Posteroanterior (А) and lateral (B) chest x-ray. The pacing leads are abnormally positioned, suggesting placement in the left heart instead of the right.
Transesophageal echocardiography (TEE) demonstrated a superior sinus venosus defect near the junction of the superior vena cava (SVC) and right atrium with left-to-right shunting. Two pacing leads pass through the defect from the SVC into the left side of the heart, with one lead affixed to the left atrium roof and the other extending through the mitral valve without any perforations into the left ventricle, where it is fixed to the interventricular septum. No intracardiac thrombi, or “smoke” and thrombi on pacemaker leads were observed during TEE (Figures 2, 3). A contrast-enhanced computer tomography (CT) scan of the chest was performed to further evaluate the suspected congenital defect and confirm the position of malpositioned pacing leads (Figure 4). CT imaging confirmed the presence of a superior sinus venosus defect located near the junction of the SVC and the right atrium. Moreover, CT revealed partial anomalous pulmonary venous return, with the right superior and middle pulmonary veins draining into the SVC. Given the patient's age, moderate frailty, and absence of significant clinical symptoms, a conservative approach was adopted. Lead extraction was not pursued due to high procedural risk. The patient was managed with lifelong oral anticoagulation with warfarin to mitigate the risk of systemic thromboembolism. Surgical correction of the anomalous pulmonary venous return was not indicated, as the patient remained hemodynamically stable without signs of volume overload. Ongoing follow-up includes regular assessment of anticoagulation status, pacemaker function, and clinical condition. The patient remained clinically stable during follow-up. No thromboembolic or bleeding complications were observed. TTE and x-ray demonstrated stable lead positioning within the left heart chambers, without evidence of thrombus formation or endocardial damage. Pacemaker function remained intact with appropriate sensing and pacing parameters.
Figure 2
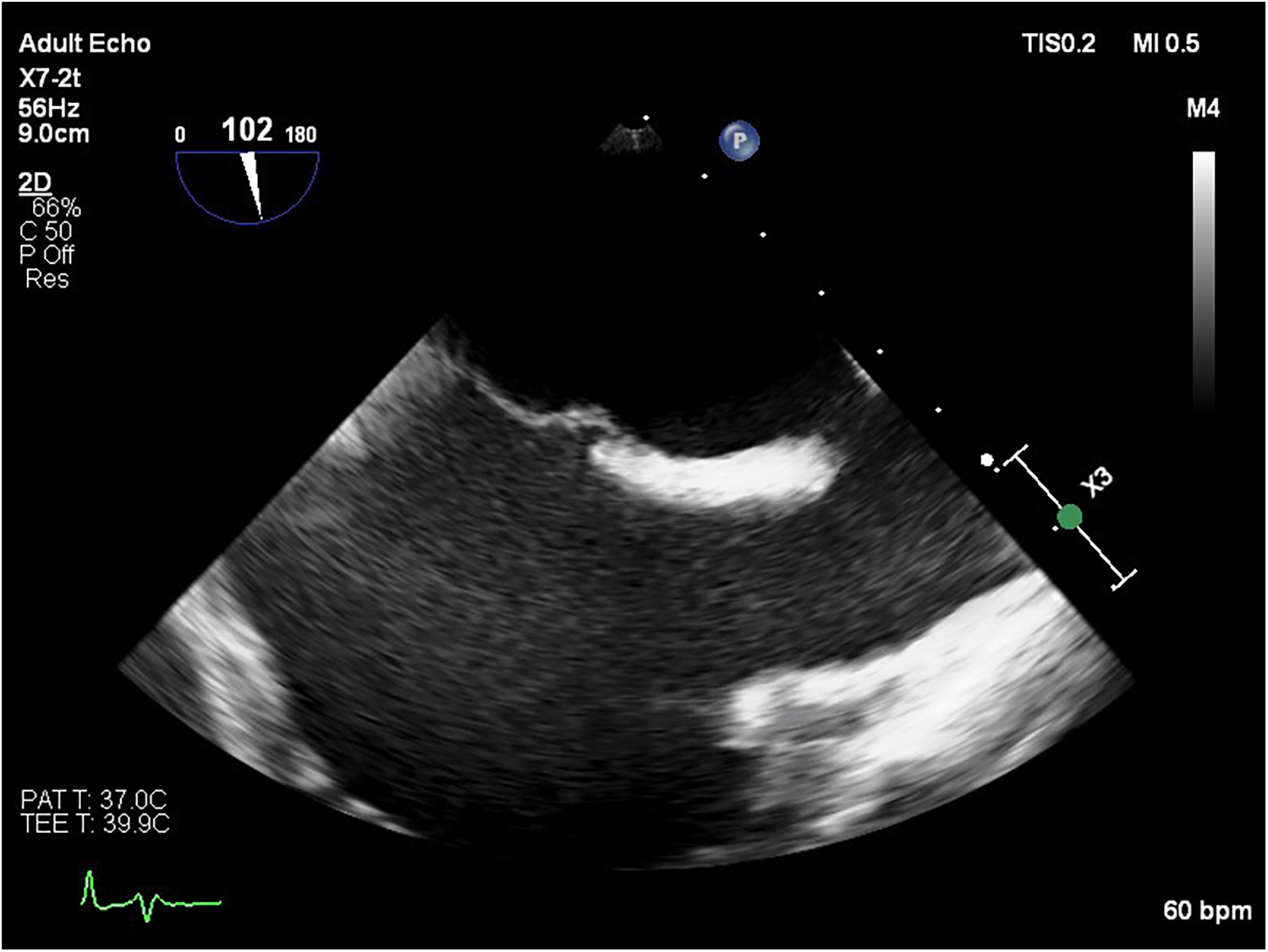
Transesophageal echocardiography image showing a sinus venosus atrial septal defect located near the junction of the SVC and the right atrium.
Figure 3
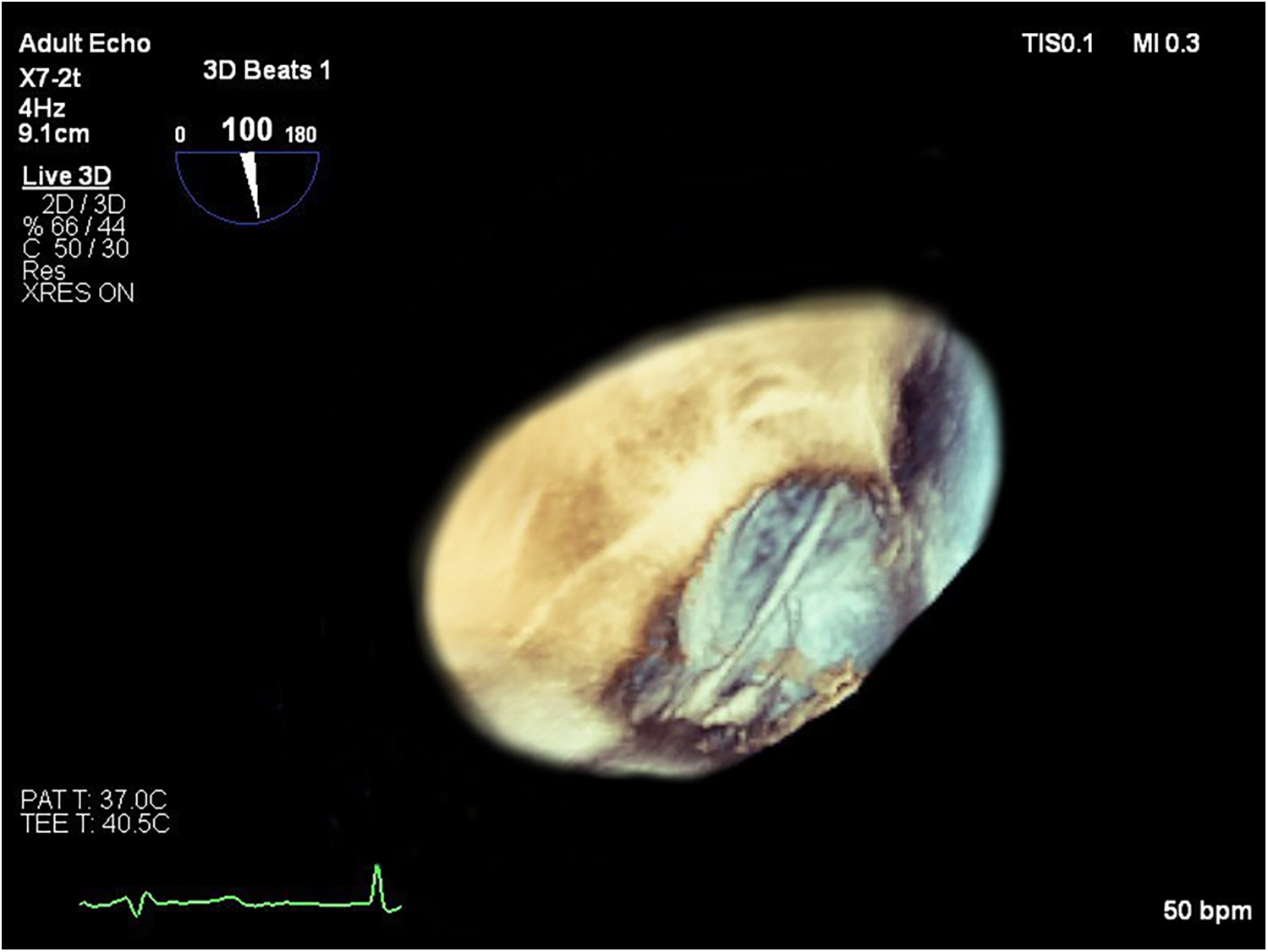
Short-axis left ventricular transesophageal 3D echocardiographic view showing the transit of the two pacing leads across the atrial septal defect. 3D, three-dimensional.
Figure 4

CT scan demonstrating malpositioned cardiac pacing leads located within the left heart.
Discussion
Malpositioned leads involving the left heart are associated with a high risk of thrombus formation and systemic thromboembolism, necessitating careful evaluation of therapeutic options (3, 4). The inadvertent placement of leads in the left atrium or ventricle may occur through congenital or acquired interatrial communications. Several cases in the literature have reported pacemaker misplacement into the left ventricle, most often due to previously unrecognized congenital heart defects (5, 6). Management of inadvertent lead malposition in the left heart is controversial due to limited data and depends on timing, symptoms, complications, and comorbidities. Early cases (<3 months) may allow for simple percutaneous removal before fibrous fixation. Chronic cases (>1 year) generally do not require lead removal unless there are strong indications, such as device-related infection (7, 8). Although lead extraction is typically considered to mitigate embolic risk, especially in younger or symptomatic patients, the decision must balance procedural risk against expected benefits. Lead extraction in elderly, frail patients carries a high risk of complications, including cardiac perforation, vascular injury, and death. Anticoagulation therapy plays a pivotal role in the conservative management of patients with left heart lead malposition. Although no large-scale randomized trials exist, several case reports and small series support the use of vitamin K antagonists (VKAs) or direct oral anticoagulation (DOACs) to reduce the risk of systemic embolism (9–11). According to Ohlow et al., long-term anticoagulation with warfarin is generally recommended, as no thromboembolic events were observed in patients who consistently maintained an international normalized ratio (INR) between 2.5 and 3.5 (12).
Conclusion
The management of patients with malpositioned pacing leads remains non-uniform, due to the lack of standardized guidelines. Therapeutic decisions should be individualized, considering the anatomical anomaly, congenital heart disease, patient comorbidities, and potential complications associated with lead extraction. Further studies are needed to establish evidence-based strategies for optimal management in such cases.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YY: Data curation, Writing – original draft, Resources. MA: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence, and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Ghani M Thakur RK Boughner D Morillo CA Yee R Klein GJ . Malposition of transvenous pacing lead in the left ventricle. Pacing Clin Electrophysiol. (1993) 16(9):1800–7. 10.1111/j.1540-8159.1993.tb01814.x
2.
Kassotis J Mirhoseni N Makan M Reddy CV . Asymptomatic left ventricular permanent pacemaker malposition detected on routine follow-up—a case report. Angiology. (2001) 52(12):859–62. 10.1177/000331970105201208
3.
Sharifi M Sorkin R Lakier JB . Left heart pacing and cardioembolic stroke. Pacing Clin Electrophysiol. (1994) 17(10):1691–6. 10.1111/j.1540-8159.1994.tb02367.x
4.
Arnar DO Kerber RE . Cerebral embolism resulting from a transvenous pacemaker catheter inadvertently placed in the left ventricle: a report of two cases confirmed by echocardiography. Echocardiography. (2001) 18(8):681–4. 10.1046/j.15408175.2001.00681.x
5.
Bobat S How WJ . Inadvertent left ventricular pacing due to lead malpositioning, incidentally discovered seventeen years later. BMJ Case Rep. (2021) 14(11):e246272. 10.1136/bcr-2021-246272
6.
Kaptein YE Yasmeh B Allaqaband SQ Chiang YP Malik IA Mortada ME . Percutaneous retrieval of an atrial leadless pacemaker from the left ventricular outflow tract. HeartRhythm Case Rep. (2024) 10(9):651–5. 10.1016/j.hrcr.2024.06.012
7.
Foley N Sukmawati I Harding SA . Inadvertent lead malposition: prevention is better than cure. JACC Case Rep. (2021) 3(16):1753–5. 10.1016/j.jaccas.2021.09.008
8.
Cayne NS Berland TL Rockman CB Maldonado TS Adelman MA Jacobowitz GR et al Experience and technique for the endovascular management of iatrogenic subclavian artery injury. Ann Vasc Surg. (2010) 24:44–7. 10.1016/j.avsg.2009.06.017
9.
Almomani A Abualsuod A Paydak H Peer W Maskoun W . Chronic lead malposition diagnosis and management: discussion of two cases and literature review. Clin Case Rep. (2017) 5(3):270–6. 10.1002/ccr3.819
10.
Van Gelder BM Bracke FA Oto A Yildirir A Haas PC Seger JJ et al Diagnosis and management of inadvertently placed pacing and ICD leads in the left ventricle: a multicenter experience and review of the literature. Pacing Clin Electrophysiol. (2000) 23(5):877–83. 10.1111/j.15408159.2000.tb00858.x
11.
Borgquist R Farouq M Markstad H Brandt J Mörtsell D Jensen S et al Diagnosis and treatment of the rare procedural complication of malpositioned pacing leads in the left heart: a single center experience. Scand Cardiovasc J. (2022) 56(1):302–9. 10.1080/14017431.2022.2099013
12.
Ohlow MA Roos M Lauer B Von Korn H Geller JC . Incidence, predictors, and outcome of inadvertent malposition of transvenous pacing or defibrillation lead in the left heart. Europace. (2016) 18:1049–54. 10.1093/europace/euv270
Summary
Keywords
pacemaker, malpositioned pacemaker leads, echocardiography, sinus venosus defect, PAPVD
Citation
Yana Y and Marat A (2025) Case Report: A wrong turn: malpositioned pacemaker leads reveal undiagnosed PAPVD after emergency implantation. Front. Cardiovasc. Med. 12:1683645. doi: 10.3389/fcvm.2025.1683645
Received
11 August 2025
Accepted
08 September 2025
Published
30 September 2025
Volume
12 - 2025
Edited by
Grigorios Korosoglou, GRN Klinik Weinheim, Germany
Reviewed by
Nachiket Apte, University of Louisville, United States
Abdalhakim Shubietah, Advocate Illinois Masonic Medical Center, United States
Updates
Copyright
© 2025 Yana and Marat.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Yakhimovich Yana yana.yahim@mail.ru
ORCID Yakhimovich Yana orcid.org/0009-0003-5313-0378 Aripov Marat orcid.org/0000-0003-2413-5818
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.