- 1Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Environmental Health, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 3Department of Public Health, College of Medicine and Health Sciences Injibara University, Injibara, Ethiopia
- 4Department of Pediatrics and Child Health Nursing, School of Nursing and Midwifery, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 5Department of Public Health, College of Medicine and Health Sciences, Debre Markos University, Debre Markos, Ethiopia
- 6Department of Nutrition and Dietetics, School of Public Health, College of Medicine Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 7Department of Health Promotion and Behavioral Sciences, School of Public Health, College of Medicine & Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 8Department of Epidemiology and Biostatistics, School of Public Health, Asrat Woldeyes Health Science Campus, Debre Berhan University, Debre Berhan, Ethiopia
Introduction: Climate change presents profound public health challenges, particularly in low-income countries like Ethiopia. Chronic respiratory diseases and chronic respiratory symptoms, are exacerbated by environmental factors such as air pollution, extreme temperatures, and occupational exposure. Despite its vulnerability, Ethiopia lacks comprehensive data on impacts of climate change on chronic respiratory health, limiting effective policy and intervention strategies. Therefore, the aims of this study to assess the impact of climate change on chronic respiratory health in Ethiopia.
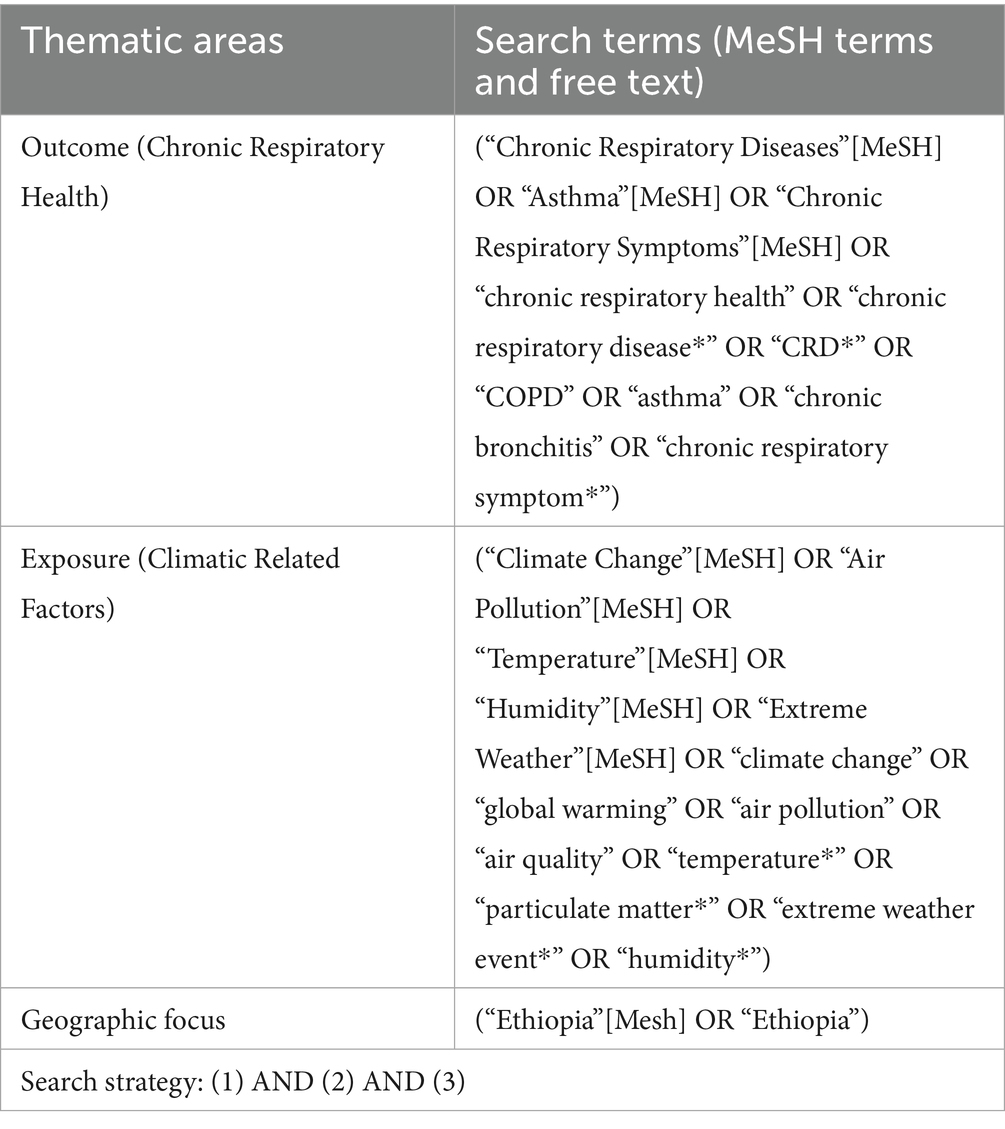
Methods: A systematic review and meta-analysis were conducted using Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Studies published between 2015 and 2024 were retrieved from PubMed, Embase, Google Scholar, and institutional repositories. Eligible studies focused on chronic respiratory diseases and chronic respiratory symptoms in Ethiopia and employed observational designs. Data extraction followed Joanna Briggs Institute protocols, and risk of bias was assessed using Hoy et al.’s checklist. Statistical analyses were performed in STATA 14, including pooled prevalence estimation using a random-effects model, subgroup analyses by region and study design, and publication bias assessment using Egger’s test and funnel plots.
Results: A total of 21 studies with 10,785 participants were included, the pooled prevalence of chronic respiratory health was 39% (95% CI: 31–48%). The most common symptoms were cough, phlegm, wheezing, and shortness of breath. Air pollution, particularly particulate matter (PM2.5 and PM10), temperature, and altitude were reported as a significant contributor. Subgroup analysis revealed the highest prevalence in Oromia (61, 95% CI: 58–64%) and the lowest in the Southern Nations, Nationalities and People Region (23, 95% CI: 13–33%). Study design influenced prevalence estimates, with cross-sectional studies reporting higher rates (46%) than case–control studies (14%). Significant heterogeneity (I2 = 99%, p < 0.001) was observed across studies.
Conclusion: The findings highlight a substantial burden of chronic respiratory health in Ethiopia, resulting from climatic, environmental, and occupational exposures. Decreasing biomass fuel use, enhancing air quality, and incorporating climate adaptation measures into public health policy are key interventions.
Introduction
Climate change is one of the most critical global issues, significantly affecting public health (Simane et al., 2016). The World Health Organization (WHO) considers climate change a health determinant that worsens existing vulnerabilities and introduces new health risks (Rawat et al., 2024; Watts et al., 2018). Chronic respiratory diseases (CRDs) like COPD, asthma, and allergies are key health outcomes linked to climate change, driven by poor air quality, increased allergens, temperature changes, precipitation patterns, and extreme weather events. CRDs, particularly asthma and COPD, account for about 7% of global deaths (Xu et al., 2025; Momtazmanesh et al., 2023; Lee and Yoon, 2024). Environmental factors such as air pollution, occupational exposures, and climate change-induced factors exacerbate these conditions (Momtazmanesh et al., 2023; Lee and Yoon, 2024).
Climate change adversely affects respiratory health through multiple mechanisms (D’Amato et al., 2014). Rising temperatures enhance ground-level ozone formation, causing oxidative stress and lung inflammation. Particulate matter (PM2.5 and PM10) from natural and human activities aggravates airway inflammation and existing respiratory conditions (Abdul-Nabi et al., 2025). Heatwaves, wildfires, and increased allergen production, such as pollen, contribute to acute and chronic respiratory issues (Anenberg et al., 2012; Scheerens et al., 2022). Air pollution remains the leading global environmental risk for respiratory diseases. Urbanization and industrialization have heightened emissions of pollutants like nitrogen dioxide (NO2), sulfur dioxide (SO2), and black carbon (Andersen et al., 2023). Heatwaves increase respiratory-related hospitalizations, particularly in vulnerable groups. Additionally, longer growing seasons and elevated CO2 levels make allergens like mold and pollen more potent and widespread, exacerbating respiratory problems (Smith and Pillarisetti, 2017).
Africa faces disproportionate impacts from climate change due to its dependence on climate-sensitive sectors, limited adaptive capacity, and existing health challenges (Wright et al., 2024). Rising temperatures, recurrent droughts, and extreme weather worsen health disparities and disrupt livelihoods (Simane et al., 2016; Teku and Eshetu, 2024). Sub-Saharan Africa is particularly vulnerable as climate change exacerbates infectious diseases, malnutrition, and non-communicable diseases like chronic respiratory diseases (Abdrabo et al., 2014). Household air pollution, driven by widespread biomass fuel use for cooking and heating, affects about 80% of African households. Women and children face the greatest exposure, leading to higher rates of respiratory diseases. Additionally, rapid urbanization has increased outdoor air pollution in African cities, where emissions regulations are often insufficient (Jestin-Guyon et al., 2023).
Data on chronic respiratory diseases (CRDs) in Africa are scarce but indicate a rising burden. COPD is increasing due to tobacco use and biomass smoke, while asthma affects millions, with prevalence reaching 20% in some urban areas. Dust storms in arid regions are linked to higher respiratory hospitalizations (Georgakopoulou et al., 2024). Efforts to mitigate climate-related health risks include National Adaptation Plans (NAPs) and regional strategies like the African Union’s Agenda 2063 (Commission and Cooke, 2022). However, progress is hindered by financial and institutional challenges. Key public health measures, such as promoting clean cooking technologies and strengthening health systems, remain underfunded (Abdrabo et al., 2014).
Ethiopia is particularly vulnerable to climate change, facing rising temperatures, erratic rainfall, and recurrent droughts. These shifts significantly affect health, especially in rural, agriculture-dependent communities, where geographic and socioeconomic factors compound vulnerabilities (Alemu and Mengistu, 2019; Fekad and Bekalu, 2020). Indoor air pollution is a significant health concern in Ethiopia, where over 90% of households rely on solid fuels for cooking, exposing women and children to high levels of particulate matter and respiratory diseases. Urban air pollution is also rising, with vehicle emissions and industrial activities causing PM2.5 levels in Addis Ababa to exceed WHO guidelines (Mulgeta et al., 2024; Tarekegn and Gulilat, 2018). CRDs like COPD and asthma are often underdiagnosed and underreported, especially in rural areas reliant on biomass fuels. Seasonal factors, including dust storms and pollen blooms, further worsen respiratory conditions (Mebrahtom et al., 2024).
Ethiopia’s healthcare system faces major challenges, including limited diagnostic facilities, healthcare worker shortages, and poor access to treatment. Poverty and low awareness further impede the prevention and management of chronic respiratory diseases (Aschalew et al., 2022). Comprehensive data on CRD prevalence and determinants are lacking, and studies on the impacts of climate change on respiratory health are scarce (Smith and Pillarisetti, 2017). This systematic review and meta-analysis synthesize findings from multiple studies to provide robust evidence. By consolidating data, this study aims to assess the impacts of climate change on chronic respiratory health in Ethiopia.
Methods
Search strategy and information sources
The PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) statement was used as a guide for this review. The search terms and keywords were identified based on the purpose of this study (Table 1). PubMed, Embase, Google scholar, and University repository databases were used. Peer-reviewed full-text articles in English language, published between 2015 and 2024 were included in the study.
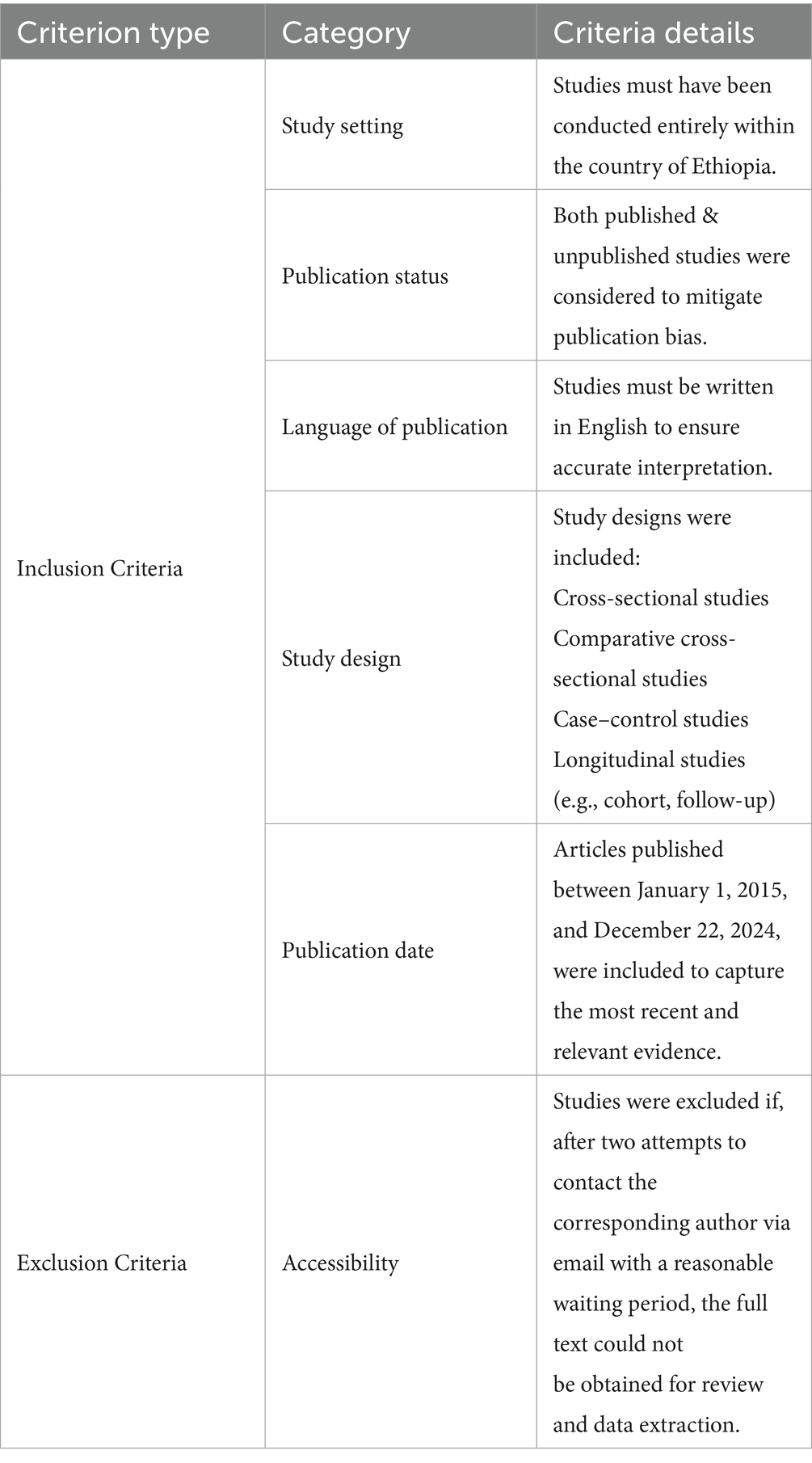
Eligibility criteria
Studies were selected for inclusion in this systematic review and meta-analysis based on the eligibility criteria summarized in the table.
Study selection procedures
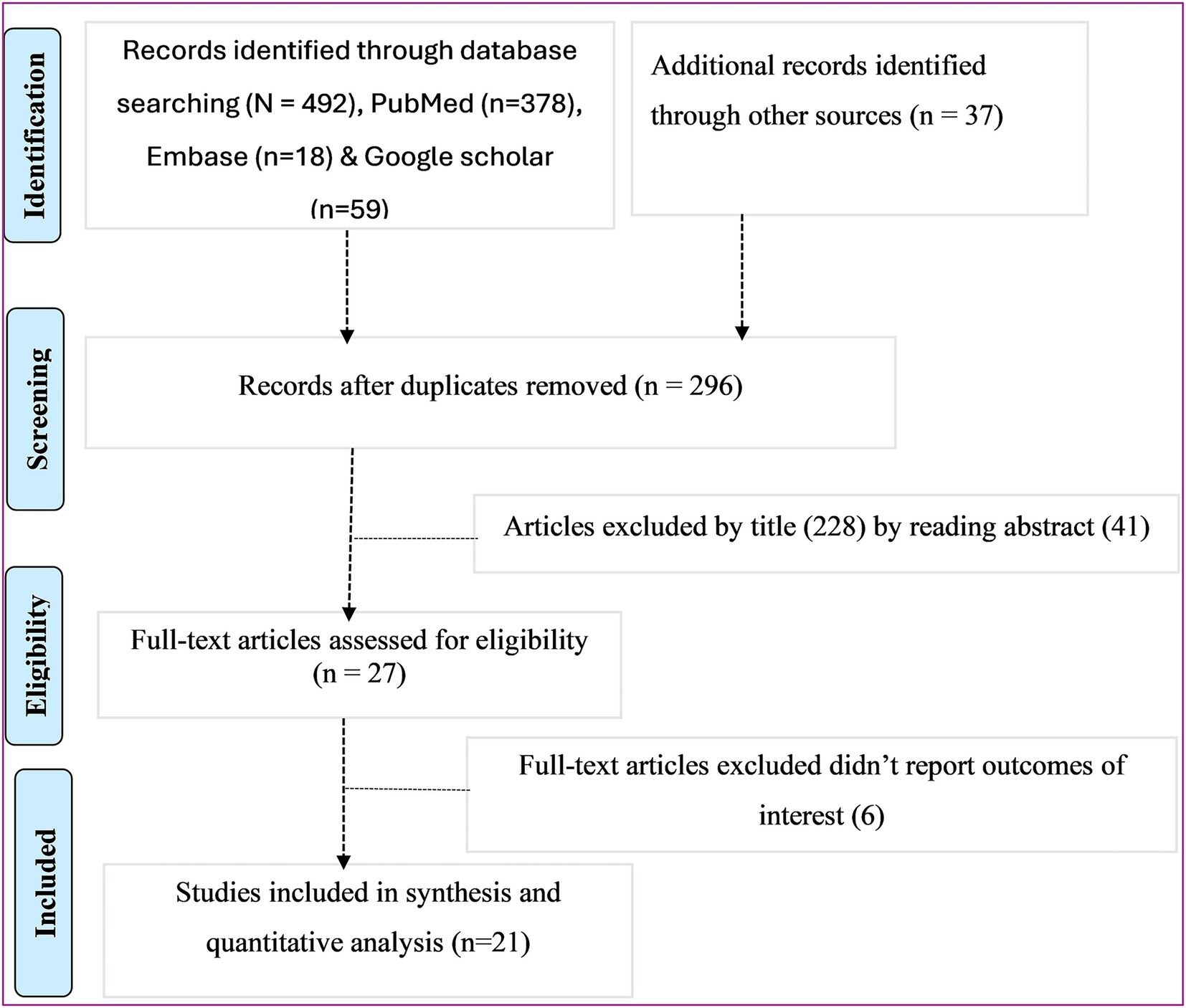
Studies identified by our search strategy were retrieved and managed using Endnote X8 software to remove duplicate studies. Two independent authors [ZA, GGK] screened the title and abstract. The disagreement was handled based on established article selection criteria. Two independent authors [ZA, GGK] conducted the full text review.
Outcome measurement
The objectives of this study explore the impacts of climate change on chronic respiratory health. Chronic Respiratory Health refers to the condition of the respiratory system over an extended period, assessed in terms of the presence or absence of chronic respiratory diseases (CRDs) and/or chronic respiratory symptoms (CRS). CRDs: Long-term conditions affecting the airways and other structures of the lungs, including but not limited to: Chronic Obstructive Pulmonary Disease (COPD), Asthma, Bronchiectasis, Interstitial lung disease diagnosed based on clinical, radiographic, or spirometric criteria, or by a healthcare professional. Where, CRS: Persistent symptoms lasting at least 3 months in a year for at least two consecutive years, such as: Chronic cough, chronic sputum production, wheezing, and shortness of breath dyspnea; (GBD Chronic Respiratory Disease Collaborators, 2020).
Data extraction and quality assessment
Data from included articles were extracted using a standardized data extraction format, adapted from the Joanna Briggs Institute (JBI), by two authors [GGK & ZA]. The data extraction format included primary author, study design, sample size, response rate, prevalence of chronic respiratory health, publication year, chronic respiratory health symptoms, and region(s) of the country where the study was conducted. Two authors (ZA & GGK) independently assessed the risk of bias for each original study by using a quality assessment checklist for prevalence studies adapted from Hoy et al.
Data processing and analysis
Pertinent data from every primary study were extracted using Microsoft Excel format. Data were then exported to STATA Version 14 statistical software for analysis. Heterogeneity of the studies was assessed by computing p-values of I2 statics and publication bias was checked objectively via Egger’s regression test. In the current meta-analysis, the pooled proportion was estimated by using the back-transform of the weighted mean of the transformed proportions, using arcsine variance weights for the fixed-effects model and DerSimonian-Laird weights for the random-effects model. Point prevalence, as well as 95% confidence intervals, was presented in the forest plot format.
Result
Characteristics of included studies
Initially, 492 articles reporting the prevalence of chronic respiratory health issues were identified from various databases. After removing duplicates, 296 studies remained. Of these, 228 were excluded based on their titles, and 41 were excluded after reviewing their abstracts. Ultimately, 27 studies were selected for full-text review, with 21 articles included in the synthesis and meta-analysis (Figure 1).
Description of included studies
As shown in (Table 2; Supplementary Table 1), a total of 21 studies published between 2015 and 2024 were included in the analysis. Of these, 9 utilized a cross-sectional (Woldeamanuel et al., 2019; Awoke et al., 2021; Wubet, 2018; Agedew et al., 2021; Hailu Tesfaye et al., 2023; Manaye et al., 2022; Mekasha et al., 2018; Gizaw et al., 2016; Alemseged et al., 2020), 1 case control (Asfaw et al., 2017) and one longitudinal study design (Debela et al., 2023), while 10 employed a comparative cross-sectional study design (Beyene, 2016; Bogale, 2021; Abay, 2019; Negash et al., 2023; Jabur et al., 2022; Abateneh et al., 2024; Badima et al., 2024; Lagiso et al., 2020; Woldeamanuel et al., 2020; Feleke et al., 2023). Additionally, 11 of the studies were conducted at the industry level in Addis Ababa. The current meta-analysis included 10,785 participants to estimate the pooled prevalence of chronic respiratory health at different study design. More than half of the studies reported a 100% response rate. However, no studies were reported in the regions of Benishangul Gumuz, Tigray, Gambella, Dire Dawa, Harari, Afar, and Somalia Region.
Chronic respiratory disease and symptoms
Nineteen studies were reported cough, phlegm and wheezing are most common chronic respiratory symptoms and have highest prevalence, respectively. However, one study reported wheezing were reported highest prevalence among study participants and one study reported prevalence of chronic obstructive pulmonary disease.
Climate change and chronic respiratory health
Air pollution
Air pollutants can exacerbate symptoms in individuals with chronic respiratory conditions. Particulate matter (PM2.5 and PM10) and other pollutants are affected by weather conditions and can contribute to the worsening of chronic respiratory health. Seventeen studies (80.95%) reported that dust exposure was a major contributing factor to chronic respiratory symptoms. Additionally, at the industry level six studies identified PM2.5 as a contributing factor to chronic respiratory health. At the household level, three studies reported that the type of household energy source was a contributing factor to chronic respiratory health.
Temperature and altitude
High temperatures can increase ground-level ozone and other pollutants, exacerbating respiratory conditions, while low temperatures can lead to airway constriction and an increased risk of respiratory infections. One study reported that both higher and lower temperatures contribute to chronic respiratory health. One study reported that high altitude living environment has impact on chronic respiratory health
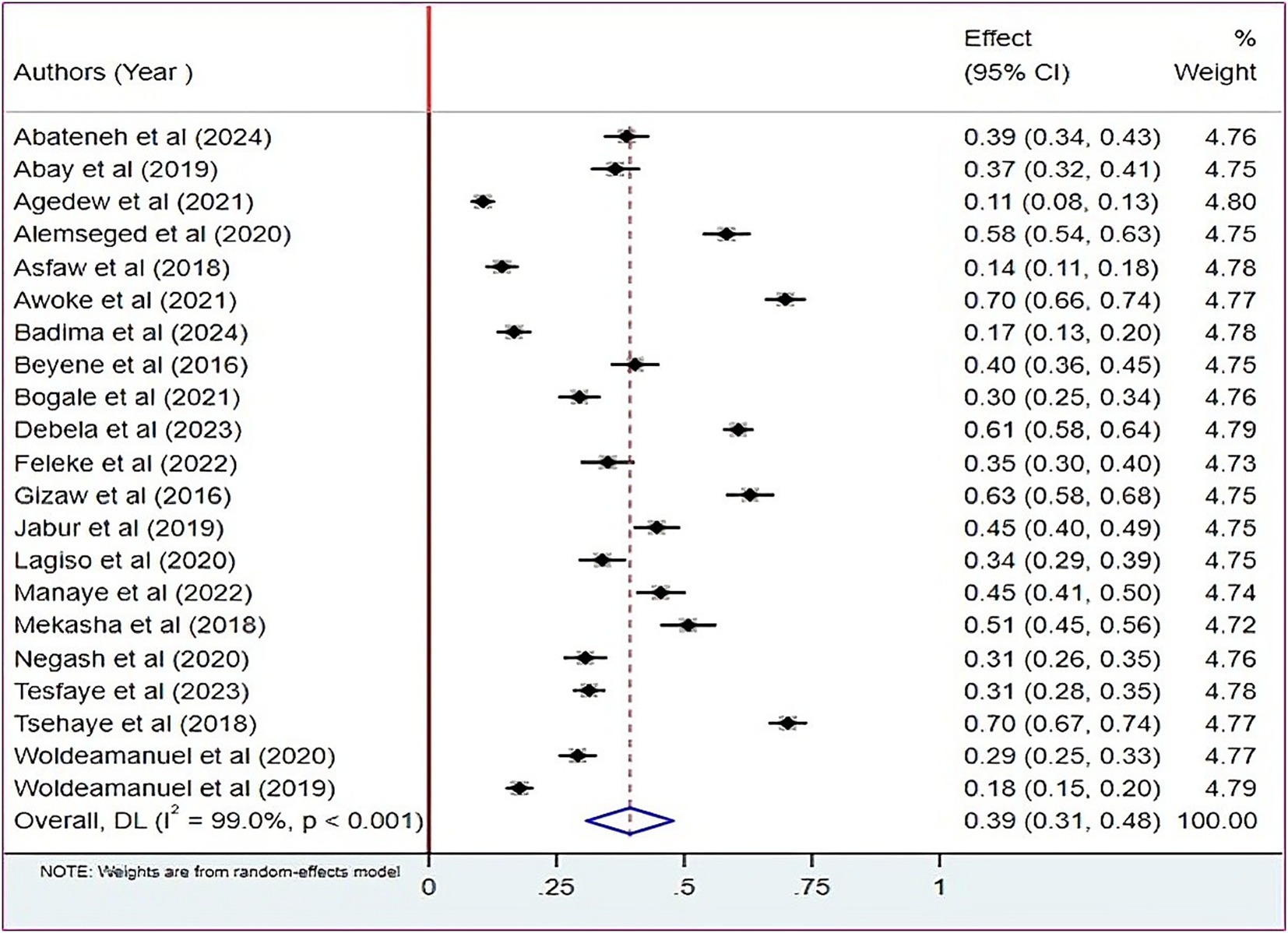
Prevalence of chronic respiratory health in Ethiopia
The estimated pooled proportion of chronic respiratory health in Ethiopia was 39% (at 95% CI: 31, 48) (Figure 2). Moderate heterogeneity was observed among the included studies, as shown in the Figure 2 there is the presence of non-overlapping confidence interval in the forest plot with true variability across studies beyond chance estimated at 99.00% (I2 = 99.00% at p < 0.001).
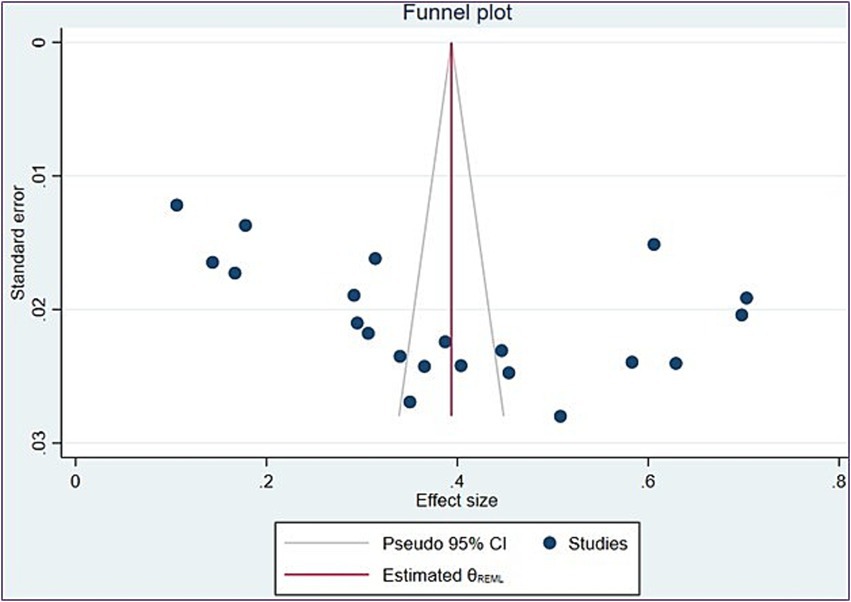
Figure 2. Forest plot showing the pooled proportion of chronic respiratory health in Ethiopia. Black boxes and lines represent the effect size (ES) and 95% confidence intervals (CIs) for each study. The overall ES, indicated by a blue diamond, includes a width corresponding to the 95% CI. The height of boxes and the diamond reflects the precision of the ES estimate.
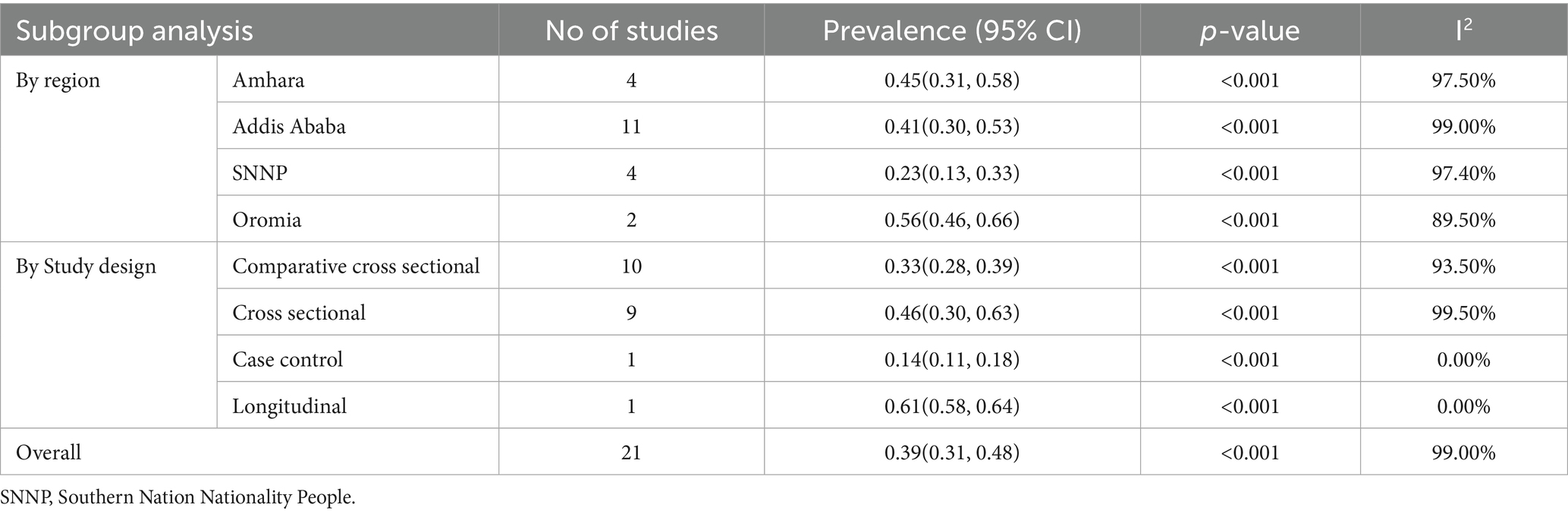
Subgroup analysis
A subgroup analysis by region and study design was conducted to compare the effect of chronic respiratory health across different regions of the country. The highest proportion was observed in Oromia [0.56, CI: (0.46, 0.66)], while the lowest effect was observed in SNNP [0.23, CI: (0.13, 33)]. By study design, the proportion was [0.32, CI: (0.26, 0.38)] for comparative cross-sectional studies and [0.46, CI: (0.30, 0.63)] for cross-sectional studies (Table 3).
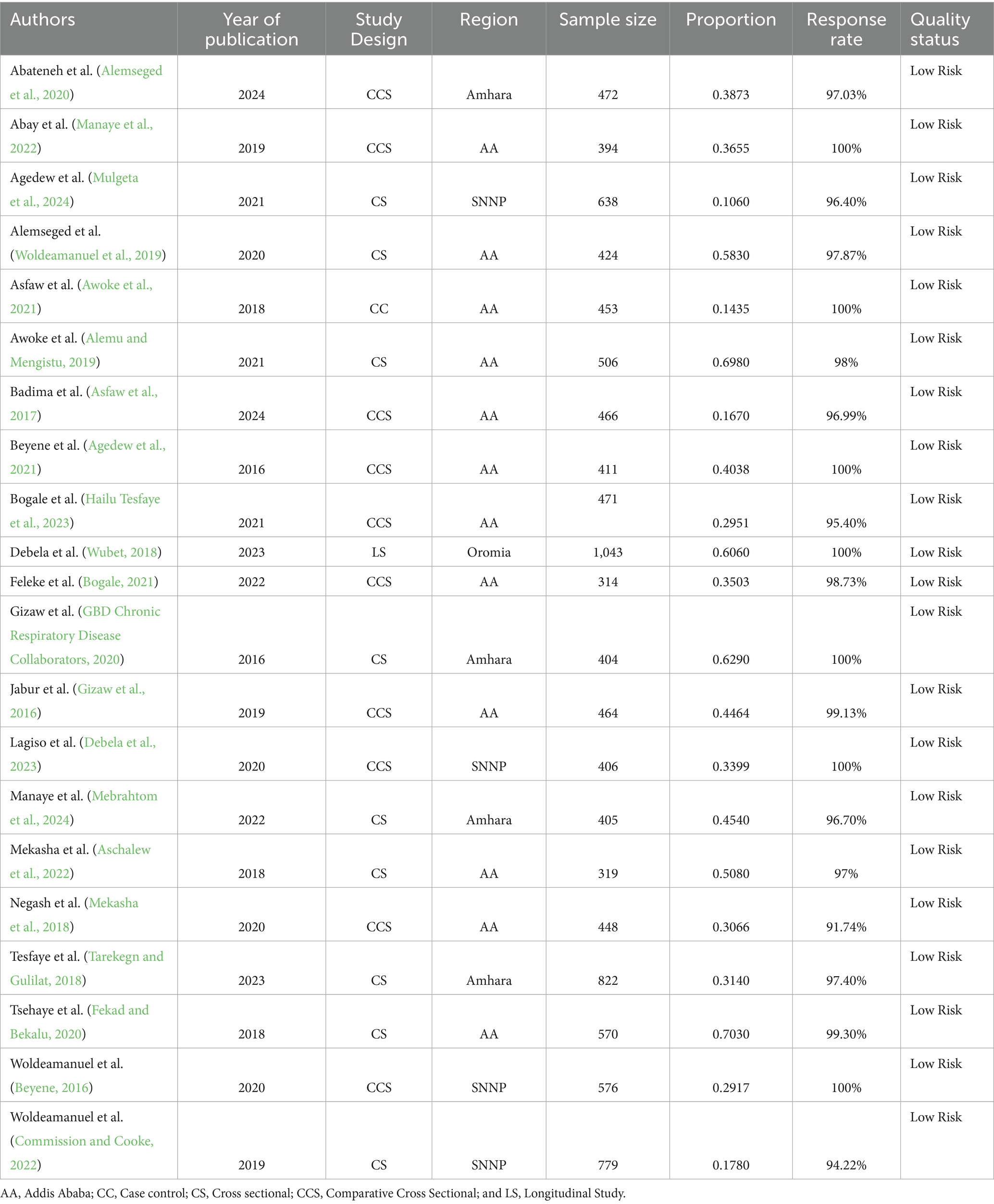
Table 3. Characteristics and quality status of the studies included in systematic review and meta-analysis chronic respiratory health in Ethiopia, 2024.
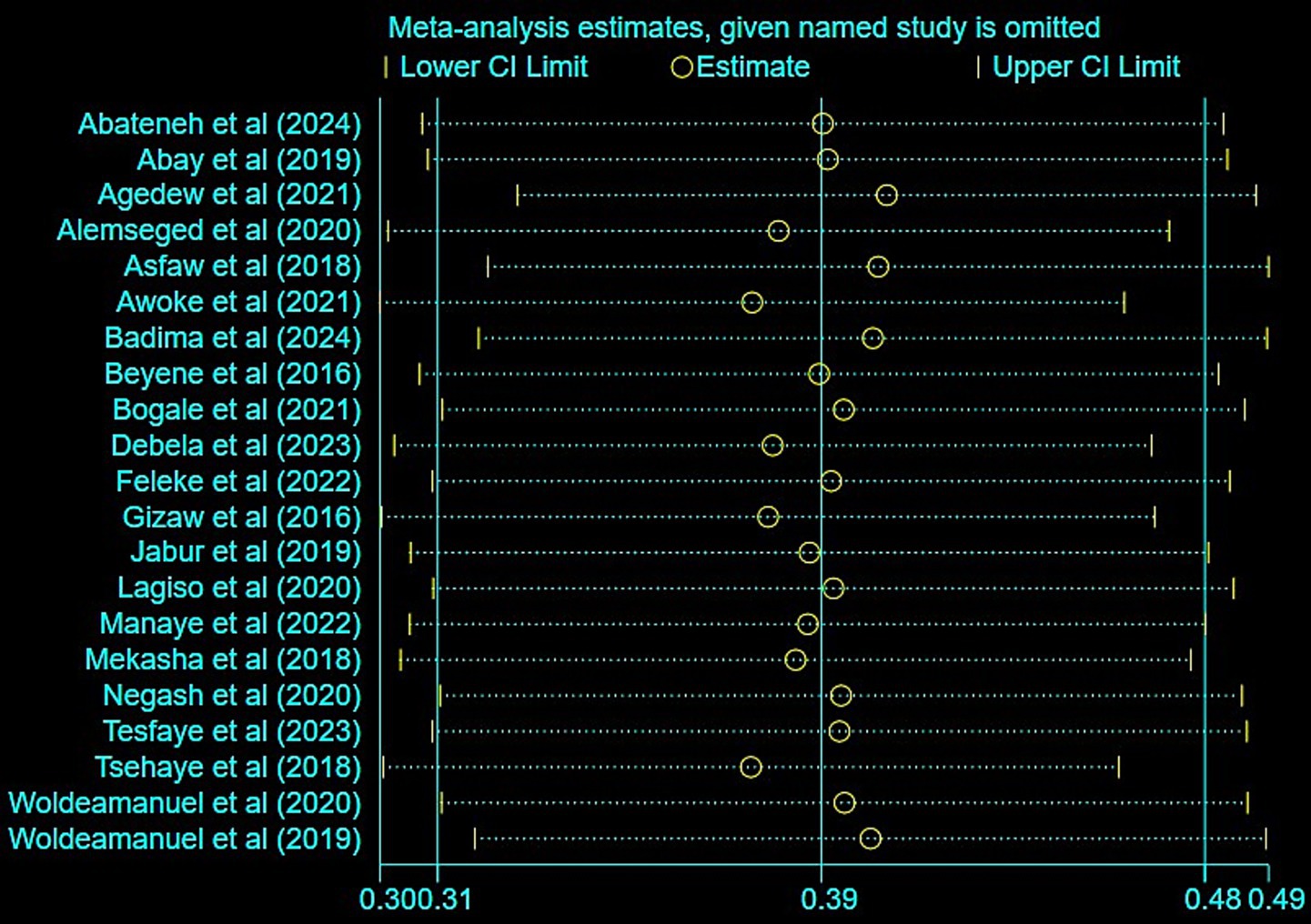
Sensitivity analysis
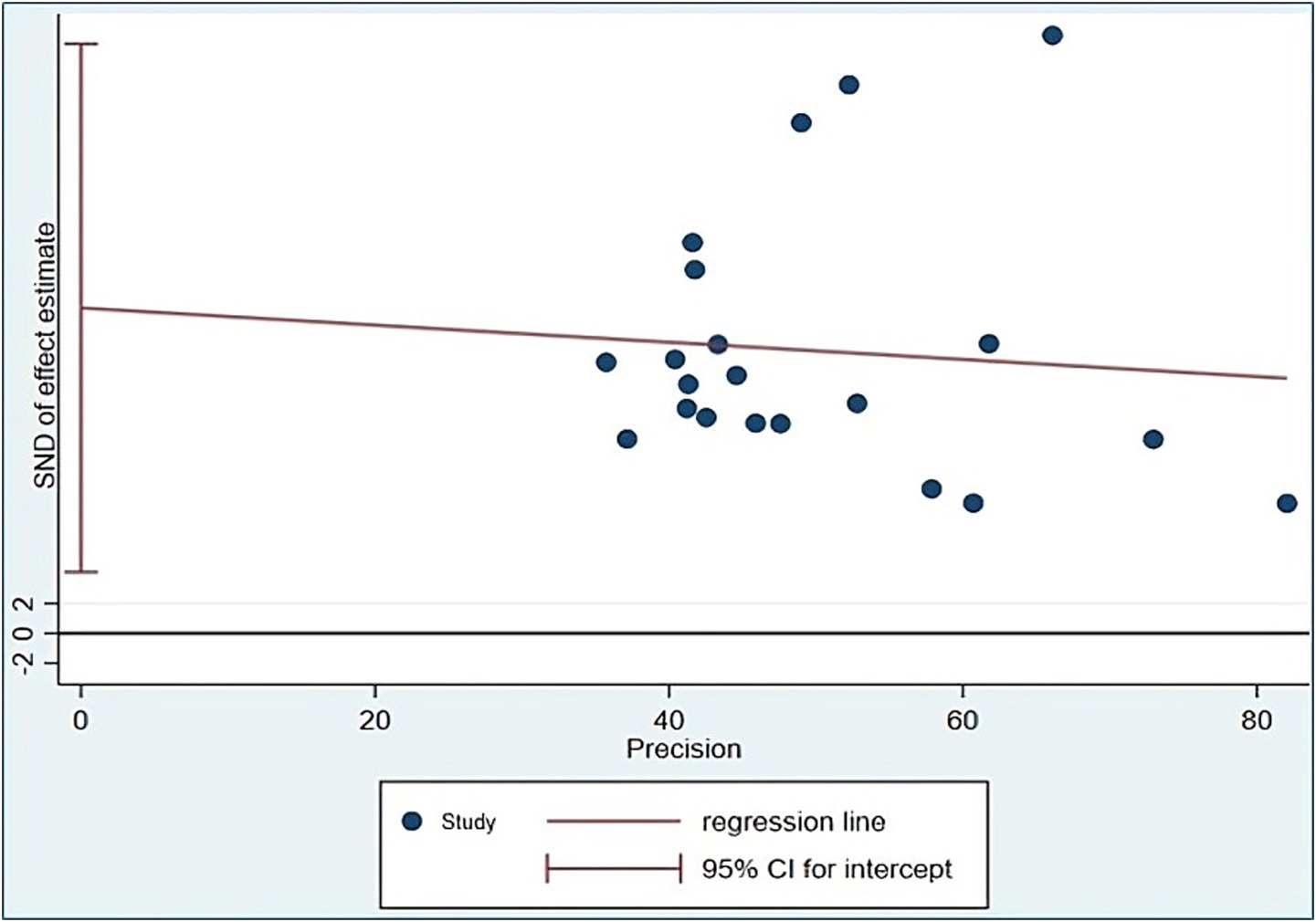
We looked at how each study affected the combined prevalence using a sensitivity analysis. The results showed that no single study significantly changed the overall estimate in the meta-analysis (Figure 3).
Publication bias
All 21 included studies were assessed for publication bias using a funnel plot and Egger’s test. The funnel plot (Figure 4) showed an asymmetric distribution, indicating a small study effect. Additionally, Egger’s test results confirmed evidence of publication bias (p value = 0.018; Table 4).
Trim and fill analysis
Publication bias was indicated by a significant Egger’s test and asymmetry in the funnel plot. To correct for this bias, we employed the trim-and-fill method. The adjusted meta-analysis estimate derived from this procedure revealed a prevalence of chronic respiratory health of 0.394 (95% CI: 0.318 to 0.470), as presented in Figure 5. The trim-and-fill adjustment indicates that the true pooled prevalence of chronic respiratory health may be approximately 0.4 percentage points higher than the original estimate. However, the original finding of 39% (95% CI: 31 to 48%) can be considered robust, as the adjusted value of 39.4% falls well within the original confidence interval. This suggests that while publication bias may be present, its effect on the overall point estimate is minimal.
The pooled estimate may be biased due to the underrepresentation of specific regions and study designs in the available literature. For instance, the low prevalence (23%) reported in the SNNP region, the relative scarcity of case–control (14%), and longitudinal studies (61%) could introduce bias if their true effects are systematically underreported in the literature.
Discussion
The meta-analysis found a pooled prevalence of chronic respiratory health was 39% at (95% CI: 31–48%), highlighting a major public health issue. Commonly reported chronic respiratory symptoms included chronic cough, phlegm, wheezing, and shortness of breath, consistent with global trends linking CRDs to prolonged exposure to environmental pollutants and climatic factors (Viegi et al., 2020; Oluwole et al., 2017; Doherty et al., 2017). High heterogeneity among studies (I2 = 99.0%, p < 0.001) reflects differences in exposure levels, healthcare access, and regional disparities within Ethiopia.
Seventeen studies identified air pollutants, including particulate matter (PM2.5 and PM10), as significant contributors to respiratory health deterioration. At the household level, biomass fuel usage was frequently associated with respiratory symptoms, consistent with findings from studies conducted in sub-Saharan Africa (Smith and Pillarisetti, 2017; Azanaw and Melaku, 2023; Oluwatosin et al., 2022). Industrial activities, particularly in Addis Ababa, exacerbated exposure to harmful pollutants, with seven studies directly linking industrial particulate matter to chronic respiratory symptoms. Studies show that particulate matter (PM2.5 and PM10) exacerbates chronic respiratory symptoms by penetrating deep into the respiratory system, causing inflammation and oxidative stress in the airways. Prolonged exposure has been linked to increased prevalence of symptoms such as chronic cough, wheezing, and shortness of breath due to structural and functional changes in the lungs (Liu et al., 2017; Mebrahtu et al., 2023; Hansel et al., 2016).
Temperature extremes, both high and low, were linked to increased respiratory symptoms. This finding aligns with research from other low-income settings, where rising temperatures have been shown to increase ground-level ozone, exacerbating asthma and COPD symptoms (Scheerens et al., 2022; Hansel et al., 2016; Tran et al., 2023). Similarly, low temperatures are known to constrict airways and elevate the risk of infections, further burdening individuals with pre-existing conditions (Lee and Yoon, 2024; D'Amato et al., 2018).
High-altitude regions presented unique challenges for respiratory health, as evidenced in one included study. Living at high altitudes can exacerbate hypoxia, impacting individuals with chronic respiratory conditions. While limited, these findings call for further investigation into altitude’s role in modulating respiratory health in Ethiopia.
The regional sub group analysis revealed marked disparities in chronic respiratory health prevalence. Oromia exhibited the highest prevalence (61%, CI: 58–64%), attributed to a combination of industrial exposure and biomass fuel usage. In contrast, the SNNP region had the lowest prevalence (23%, CI: 13–33%), likely reflecting regional differences in study design, healthcare access, and environmental exposures. These disparities emphasize the need for region-specific interventions.
The variability by study design revealed that cross-sectional studies reported higher prevalence estimates (46%) compared to comparative cross-sectional (33%) and case–control designs (14%). This finding underscores the importance of considering study design when interpreting prevalence rates, as cross-sectional designs often capture acute exposure effects.
Generally, particulate matter (PM2.5 and PM10) damages the respiratory system by causing inflammation, oxidative stress, and fibrosis, which may progress to COPD, chronic bronchitis, or lung cancer if left untreated (Xing et al., 2016). Temperature extremes cause bronchoconstriction and mucus change, increasing asthma attacks and risk of respiratory failure (Tran et al., 2025; Han et al., 2023). High altitude induces hypoxic stress, which may lead to pulmonary hypertension, if not appropriately treated (Sydykov et al., 2021).
Implications for policy and practice
The high burden of chronic respiratory symptoms linked to climate change necessitates integrated policies addressing air quality, sustainable energy use, and climate adaptation strategies. Public awareness campaigns, coupled with enhanced healthcare access and targeted interventions in high-prevalence regions, are critical to mitigating the impact of climate change on respiratory health in Ethiopia.
Future research should prioritize underrepresented regions and employ longitudinal designs to capture long-term impacts of climate change on chronic respiratory health. Addressing the identified gaps will be vital for developing comprehensive strategies to combat the growing burden of CRDs in Ethiopia.
Conclusion
This systematic review and meta-analysis reveal a high burden of chronic respiratory diseases in Ethiopia, primarily attributed to climatic, environmental, and occupational factors, including air pollution, biomass fuel use, and temperature extremes. Regional disparities, such as the highest prevalence in Oromia and the lowest in Southern Nations, Nationalities and People, underscore the need for targeted interventions. The findings emphasize the urgency of integrating climate adaptation strategies, promoting clean energy alternatives, and strengthening healthcare systems to mitigate chronic respiratory diseases risks. Addressing these challenges requires multisectoral collaboration to reduce exposure hazards and improve respiratory health outcomes in Ethiopia. Future research should prioritize longitudinal studies and underrepresented regions to inform evidence-based policies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. AA: Writing – original draft, Writing – review & editing. AG: Writing – original draft, Writing – review & editing. GK: Data curation, Methodology, Writing – original draft, Writing – review & editing, Validation. KM: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. MS: Writing – original draft, Writing – review & editing. SC: Writing – original draft, Writing – review & editing. WT: Writing – original draft, Writing – review & editing. YM: Writing – original draft, Writing – review & editing. YW: Writing – original draft, Writing – review & editing. ZG: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fclim.2025.1555383/full#supplementary-material
Abbreviations
COPD, Chronic Obstructive Pulmonary Disease; CRDs, Chronic respiratory diseases; CRS, Chronic Respiratory Symptoms; NAPs, National Adaptation Plans; PM, Particulate Matter; PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses; SNNP, Southern Nation Nationality People.
References
Abateneh, G., Gizaw, Z., Gebrehiwot, M., and Worede, E. A. (2024). Prevalence of chronic respiratory symptoms and associated factors among woodwork workers in Bahir Dar City, Ethiopia; a comparative cross-sectional study. BMC Pulm. Med. 24:3. doi: 10.1186/s12890-023-02812-x
Abay, Bezayit Girma (2019) Assessment of prevalence of chronic Respiratory Symptoms and lung function among fuel station workers in Addis Abeba, Ethiopia
Abdrabo, M., Ama, E., Lennard, C., Africa, P., Adelekan, I., Archibald, S., et al. (2014). “Africa” in Climate change 2014: Impacts, adaptation, and vulnerability. Part B: Regional aspects. Contribution of working group II to the fifth assessment report of the intergovernmental panel on climate change. eds. D. Pauline and L. Neil (United Kingdom and New York: Cambridge University Press), 1199–1265.
Abdul-Nabi, S. S., Al Karaki, V., Khalil, A., and El Zahran, T. (2025). Climate change and its environmental and health effects from 2015 to 2022: a scoping review. Heliyon. 11:e42315. doi: 10.1016/j.heliyon.2025.e42315
Agedew, E., Boda, B., Kanko, T., Estifanos, W., and Shibiru, T. (2021). Chronic obstructive pulmonary disease and associated factors in Arba Minch health and demographic surveillance site, 2020. Int. J. Chron. Obstruct. Pulmon. Dis. 16, 2953–2962. doi: 10.2147/COPD.S319721
Alemseged, E. A., Takele, A. K., Zele, Y., Abaya, S. W., Kiros, K. G., Mehari, M., et al. (2020). Assessment of chronic respiratory health symptoms and associated factors among flour mill factory Workers in Addis Ababa, Ethiopia, 2019: a cross-sectional study. J. Asthma Allergy. 13, 483–492. doi: 10.2147/JAA.S273820
Alemu, T., and Mengistu, A. (2019). “Impacts of climate change on food security in Ethiopia: Adaptation and mitigation options: A review” in Climate change-resilient agriculture and agroforestry: Ecosystem services and sustainability. eds. P. Castro, A. Azul, W. Leal Filho, and U. Azeiteiro (Switzerland: Springer, Cham), 397–412.
Andersen, Z. J., Vicedo-Cabrera, A. M., Hoffmann, B., and Melén, E. (2023). Climate change and respiratory disease: clinical guidance for healthcare professionals. Breathe (Sheff.) 19:220222. doi: 10.1183/20734735.0222-2022
Anenberg, S. C., Schwartz, J., Shindell, D., Amann, M., Faluvegi, G., Klimont, Z., et al. (2012). Global air quality and health co-benefits of mitigating near-term climate change through methane and black carbon emission controls. Environ. Health Perspect. 120, 831–839. doi: 10.1289/ehp.1104301
Aschalew, A., Kebed, R. A., Demie, T. G., and Weldetsadik, A. Y. (2022). Assessment of level of asthma control and related factors in children attending pediatric respiratory clinics in Addis Ababa, Ethiopia. BMC Pulm. Med. 22:70. doi: 10.1186/s12890-022-01865-8
Asfaw, S. J., Enquselassie, F., Tefera, Y., Gizaw, M., Wakuma, S., and Woldemariam, M. (2017). Determinants of chronic respiratory symptoms among pharmaceutical factory workers. J. Trop. Med. doi: 10.1155/2018/3815689
Awoke, T. Y., Takele, A. K., Mekonnen, W. T., Abaya, S. W., Zele, Y. T., Alemseged, E. A., et al. (2021). Assessment of dust exposure and chronic respiratory symptoms among workers in medium scale woodwork factories in Ethiopia; a cross sectional study. BMC Public Health 21:309. doi: 10.1186/s12889-021-10357-z
Azanaw, J., and Melaku, M. S. (2023). Spatial variation and factors associated of solid fuel use in Ethiopia a multilevel and spatial analysis based on EDHS 2016. Sci. Rep. 13:20279. doi: 10.1038/s41598-023-46897-0
Badima, H., Kumie, A., Meskele, B., and Abaya, S. W. (2024). Welding fume exposure and prevalence of chronic respiratory symptoms among welders in micro- and small-scale enterprise in Akaki Kality sub-city, Addis Ababa, Ethiopia: a comparative cross-sectional study. BMC Pulm. Med. 24:147. doi: 10.1186/s12890-024-02958-2
Beyene, Tsegay Gebrezgher. (2016). Comparative Cross Sectional Study on Chronic Respiratory Symptoms and Associated Factors among Addis Ababa city municipal Street Sweepers, Addis Ababa, Ethiopia.
Bogale, Ephrem (2021) Assessment of chronic respiratory symptoms and associated factors among marble factory workers in Addis Ababa Ethiopia: A comparative cross-sectional study
Commission, A., and Cooke, S. (2022) Africa’s Climate Change and Resilient Development Strategy and Action Plan (2022–2032)
D’Amato, G., Cecchi, L., D’Amato, M., and Annesi-Maesano, I. (2014). Climate change and respiratory diseases. Eur. Respir. Rev. 23, 161–169.
D'Amato, M., Molino, A., Calabrese, G., Cecchi, L., Annesi-Maesano, I., and D'Amato, G. (2018). The impact of cold on the respiratory tract and its consequences to respiratory health. Clin. Transl. Allergy 8:20. doi: 10.1186/s13601-018-0208-9
Debela, M., Kebeta, N. D., Begosaw, A. M., Okello, G., and Azage, M. (2023). Bagasse dust exposure and chronic respiratory symptoms among workers in the Metehara and Wonji sugar factories in Ethiopia: a longitudinal study design. BMJ Open Respir. Res. 10:e001511. doi: 10.1136/bmjresp-2022-001511
Doherty, R. M., Heal, M. R., and O’Connor, F. M. (2017). Climate change impacts on human health over Europe through its effect on air quality. Environ. Health 16:118. doi: 10.1186/s12940-017-0325-2
Fekad, M., and Bekalu, Y. (2020). Climate change impacts on household food security and its adaptation options in rural Ethiopia: a systematic review. EPRA Int J Res Develop. 5:2455–7838. doi: 10.36713/epra4142
Feleke, M. G., Alemu, Y., Shentema, M. G., Wakuma, S., Emiru, Z., and Chichiabellu, T. Y. (2023). Chronic respiratory symptoms and associated factors among fruit and vegetable Workers in Addis Ababa, Ethiopia: a comparative cross sectional study. Saf. Health Work 14, 287–294. doi: 10.1016/j.shaw.2023.07.001
GBD Chronic Respiratory Disease Collaborators (2020). Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir. Med. 8, 585–596. doi: 10.1016/S2213-2600(20)30105-3
Georgakopoulou, V. E., Taskou, C., Diamanti, A., Beka, D., Papalexis, P., Trakas, N., et al. (2024). Saharan dust and respiratory health: understanding the link between airborne particulate matter and chronic lung diseases. Exp. Ther. Med. 28:460.
Gizaw, Z., Yifred, B., and Tadesse, T. (2016). Chronic respiratory symptoms and associated factors among cement factory workers in Dejen town, Amhara regional state, Ethiopia, 2015. Multidiscip. Respir. Med. 11:13. doi: 10.1186/s40248-016-0043-6
Hailu Tesfaye, A., Gebrehiwot, M., Aragaw, F. M., and Dessie, A. (2023). Prevalence and risk factors of chronic respiratory symptoms in public and private school teachers in North-Western Ethiopia: results from a multicentre cross-sectional study. BMJ Open 13:e069159. doi: 10.1136/bmjopen-2022-069159
Han, A., Deng, S., Yu, J., Zhang, Y., Jalaludin, B., and Huang, C. (2023). Asthma triggered by extreme temperatures: from epidemiological evidence to biological plausibility. Environ. Res. 216:114489. doi: 10.1016/j.envres.2022.114489
Hansel, N. N., McCormack, M. C., and Kim, V. (2016). The effects of air pollution and temperature on COPD. COPD 13, 372–379. doi: 10.3109/15412555.2015.1089846
Jabur, B., Ashuro, Z., and Abaya, S. W. (2022). Chronic respiratory symptoms and lung function parameters in large-scale wood factory workers in Addis Ababa, Ethiopia: a comparative cross-sectional study. Int. Arch. Occup. Environ. Health 95, 1221–1230. doi: 10.1007/s00420-022-01857-5
Jestin-Guyon, N., Ouaalaya, E. H., Harison, M. T., Ravahatra, K., Rakotomizao, J., Raharimanana, R. N., et al. (2023). Impact of biomass fuel smoke on respiratory health of children under 15 years old in Madagascar. Respiratory Med. Res. 83:100989. doi: 10.1016/j.resmer.2023.100989
Lagiso, Z. A., Mekonnen, W. T., Abaya, S. W., Takele, A. K., and Workneh, H. M. (2020). Chronic respiratory symptoms, lung function and associated factors among flour mill factory workers in Hawassa city, southern Ethiopia: “comparative cross-sectional study”. BMC Public Health 20:909. doi: 10.1186/s12889-020-08950-9
Lee, H., and Yoon, H. Y. (2024). Impact of ambient temperature on respiratory disease: a case-crossover study in Seoul. Respir. Res. 25:73. doi: 10.1186/s12931-024-02699-0
Liu, S., Zhou, Y., Liu, S., Chen, X., Zou, W., Zhao, D., et al. (2017). Association between exposure to ambient particulate matter and chronic obstructive pulmonary disease: results from a cross-sectional study in China. Thorax 72, 788–795. doi: 10.1136/thoraxjnl-2016-208910
Manaye, E., Manaye, Y., and Birkie, M. (2022). Magnitude and risk factors of chronic respiratory symptoms among municipal street sweepers in Dessie and Kombolcha City, northeast, Ethiopia: cross-sectional study. SAGE Open Med. 10. doi: 10.1177/20503121221105329
Mebrahtom, G., Hailay, A., Mariye, T., Haile, T. G., Girmay, G., Zereabruk, K., et al. (2024). Chronic obstructive pulmonary disease in East Africa: a systematic review and meta-analysis. Int. Health 16, 499–511. doi: 10.1093/inthealth/ihae011
Mebrahtu, T. F., Santorelli, G., Yang, T. C., Wright, J., Tate, J., and McEachan, R. R. C. (2023). The effects of exposure to NO2, PM2.5 and PM10 on health service attendances with respiratory illnesses: a time-series analysis. Environ. Pollut. 333:122123. doi: 10.1016/j.envpol.2023.122123
Mekasha, M., Haddis, A., Shaweno, T., and Mereta, S. T. (2018). Emission level of PM2.5 and its association with chronic respiratory symptoms among workers in cement industry: a case of Mugher cement industry, Central Ethiopia. Avicenna J. Environ. Health Eng. 5, 1–7. doi: 10.15171/ajehe.2018.01
Momtazmanesh, S., Moghaddam, S. S., Ghamari, S.-H., Rad, E. M., Rezaei, N., Shobeiri, P., et al. (2023). Global burden of chronic respiratory diseases and risk factors, 2019: an update from the global burden of disease study 2019. Eclinmed. 59, 1–19. doi: 10.1016/j.eclinm.2023.101936
Mulgeta, D., Gotu, B., Temesgen, S., Feyasa, M., Likassa, H., and Tsegaye, D. (2024). Statistical analysis of spatial distribution of ambient air pollution in Addis Ababa, Ethiopia. Stoch. Env. Res. Risk A., 1–19. doi: 10.1007/s00477-024-02748-6
Negash, B. M., Abaya, S. W., Abegaz, T., Takele, A. K., Mekonnen, W. T., Negatu, H. B., et al. (2023). Assessment of paper dust exposure and chronic respiratory symptoms among paper factory workers in, Ethiopia; a comparative cross-sectional study. BMC Pulm. Med. 23:48. doi: 10.1186/s12890-023-02338-2
Oluwatosin, D, Ola, K, and Adewumi, O The Impacts of the Use of Biomass Solid Fuels for Household Cooking in Sub-Saharan Africa - A Review (2022)
Oluwole, O., Arinola, G., Huo, D., and Olopade, C. (2017). Household biomass fuel use, asthma symptoms severity, and asthma underdiagnosis in rural schoolchildren in Nigeria: a cross-sectional observational study. BMC Pulm. Med. 17:3. doi: 10.1186/s12890-016-0352-8
Rawat, A., Kumar, D., and Khati, B. S. (2024). A review on climate change impacts, models, and its consequences on different sectors: a systematic approach. J. Water Clim. Change 15, 104–126. doi: 10.2166/wcc.2023.536
Scheerens, C., Nurhussien, L., Aglan, A., Synn, A. J., Coull, B. A., Koutrakis, P., et al. (2022). The impact of personal and outdoor temperature exposure during cold and warm seasons on lung function and respiratory symptoms in COPD. ERJ Open Res. 8, 00574–02021. doi: 10.1183/23120541.00574-2021
Simane, B., Beyene, H., Deressa, W., Kumie, A., Berhane, K., and Samet, J. (2016). Review of climate change and health in Ethiopia: status and gap analysis. Ethiopian J. Health Develop. = Ya'Ityopya tena lemat mashet 30, 28–41.
Smith, K. R., and Pillarisetti, A. (2017). “Household air pollution from solid Cookfuels and its effects on health” in Injury prevention and environmental health. eds. C. N. Mock, R. Nugent, O. Kobusingye, and K. R. Smith (Washington (DC): The International Bank for Reconstruction and Development / The World Bank).
Sydykov, A., Mamazhakypov, A., Maripov, A., Kosanovic, D., Weissmann, N., Ghofrani, H. A., et al. (2021). Pulmonary hypertension in acute and chronic high altitude maladaptation disorders. Int. J. Environ. Res. Public Health 18:1692. doi: 10.3390/ijerph18041692
Tarekegn, M., and Gulilat, T. (2018). Trends of ambient air pollution and the corresponding respiratory diseases in Addis Ababa. Medical Insight. 2, 1–5.
Teku, D., and Eshetu, S. (2024). Impact of climatic variabilities and extreme incidences on the physical environment, public health, and people’s livelihoods in Ethiopia. Front. Climate. 6:6. doi: 10.3389/fclim.2024.1435138
Tran, H. M., Tsai, F.-J., Lee, Y.-L., Chang, J.-H., Chang, L.-T., Chang, T.-Y., et al. (2023). The impact of air pollution on respiratory diseases in an era of climate change: a review of the current evidence. Sci. Total Environ. 898:166340. doi: 10.1016/j.scitotenv.2023.166340
Tran, H. M., Tsai, F.-J., Lee, K.-Y., Wang, Y.-H., Yang, F.-M., Ho, S.-C., et al. (2025). Extreme temperature increases the risk of COPD morbimortality: a systematic review and meta-analysis. Sci. Total Environ. 958:178087. doi: 10.1016/j.scitotenv.2024.178087
Viegi, G., Maio, S., Fasola, S., and Baldacci, S. (2020). Global burden of chronic respiratory diseases. J. Aerosol Med. Pulm. Drug Deliv. 33, 171–177. doi: 10.1089/jamp.2019.1576
Watts, N., Amann, M., Arnell, N., Ayeb-Karlsson, S., Belesova, K., Berry, H., et al. (2018). The 2018 report of the lancet countdown on health and climate change: shaping the health of nations for centuries to come. Lancet (London, England). 392, 2479–2514. doi: 10.1016/S0140-6736(18)32594-7
Woldeamanuel, G. G., Mingude, A. B., and Geta, T. G. (2019). Prevalence of chronic obstructive pulmonary disease (COPD) and its associated factors among adults in Abeshge District, Ethiopia: a cross sectional study. BMC Pulm. Med. 19, 1–9. doi: 10.1186/s12890-019-0946-z
Woldeamanuel, G. G., Mingude, A. B., Yitbarek, G. Y., and Taderegew, M. M. (2020). Chronic respiratory symptoms and pulmonary function status in Ethiopian agricultural workers: a comparative study. BMC Pulm. Med. 20:86. doi: 10.1186/s12890-020-1120-3
Wright, C. Y., Kapwata, T., Naidoo, N., Asante, K. P., Arku, R. E., Cissé, G., et al. (2024). Climate change and human health in Africa in relation to opportunities to strengthen mitigating potential and adaptive capacity: strategies to inform an African "brains trust". Ann. Glob. Health 90:7. doi: 10.5334/aogh.4260
Wubet, Kenfe Tsehaye (2018) Assessing Personal Dust Exposure and Chronic Respiratory Health Symptoms among Street Sweepers in Addis Ababa, Ethiopia, 2017/18
Xing, Y. F., Xu, Y. H., Shi, M. H., and Lian, Y. X. (2016). The impact of PM2.5 on the human respiratory system. J. Thorac. Dis. 8, E69–E74. doi: 10.3978/j.issn.2072-1439.2016.01.19
Keywords: climate change, chronic respiratory diseases, Ethiopia, systematic review, meta-analysis
Citation: Andualem Z, Alemu AT, Geddif A, Kassie GG, Mitiku KW, Belay MA, Simegn MB, Chanie SD, Tilahun WM, Menber Y, Wasihun Y and Gebreegziabher ZA (2025) Impacts of climate change on chronic respiratory health in Ethiopia: a systematic review and meta-analysis. Front. Clim. 7:1555383. doi: 10.3389/fclim.2025.1555383
Edited by:
Warren Dodd, University of Waterloo, CanadaReviewed by:
Worradorn Phairuang, Chiang Mai University, ThailandDiego Marcelo Conti, Department of Microbiology and Immunology, KU Leuven, Belgium
Copyright © 2025 Andualem, Alemu, Geddif, Kassie, Mitiku, Belay, Simegn, Chanie, Tilahun, Menber, Wasihun and Gebreegziabher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zewudu Andualem, emV3dWR1YW5kdWFsZW0xMkBnbWFpbC5jb20=
 Zewudu Andualem
Zewudu Andualem Ayenew Takele Alemu
Ayenew Takele Alemu Azeb Geddif
Azeb Geddif Genet Gedamu Kassie
Genet Gedamu Kassie Kalkidan Worku Mitiku
Kalkidan Worku Mitiku Mahider Awoke Belay
Mahider Awoke Belay Mulat Belay Simegn
Mulat Belay Simegn Samuel Dagne Chanie
Samuel Dagne Chanie Werkneh Melkie Tilahun
Werkneh Melkie Tilahun Yonatan Menber
Yonatan Menber Yosef Wasihun
Yosef Wasihun Zenebe Abebe Gebreegziabher
Zenebe Abebe Gebreegziabher