- 1Institute of Child Health and Human Development, University of the Philippines – National Institutes of Health, Manila, Philippines
- 2Deutsche Gesellschaft für Internationale Zusammenarbeit, Makati, Philippines
Introduction: Climate change poses significant health risks globally, particularly in vulnerable countries like the Philippines. This scoping review examines recent research trends (2018–2023) on the health impacts of climate change in the Philippines, building on previous national reviews and situating findings within global evidence.
Methods: We screened 8,346 articles from various databases and identified 69 studies meeting inclusion criteria. Using a framework-guided thematic synthesis, studies were categorized into 6 themes: vulnerability to disease and injury, direct health impacts of climate and weather, ecosystem-mediated impacts, health impacts mediated through human institutions, adaptation strategies, and co-benefits of mitigation measures.
Results: Results reveal a significant increase in climate-health research compared to a previous review (1980–2017), with notable growth in studies in mental health, gender-based vulnerabilities, and adaptation measures. However, research remains geographically concentrated in Luzon, highlighting regional disparities, and few studies utilized long-term climate-health datasets. Studies quantifying the health co-benefits of mitigation measures also remain limited.
Discussion: This review demonstrates significant progress while identifying persistent gaps. Future research should prioritize long-term surveillance, local adaptation evaluations and health-economic co-benefits studies to strengthen climate-health data integration, improve climate information services and develop equity-oriented, policy-relevant research agenda.
1 Introduction
Climate change is widely recognized as the greatest global health threat of the 21st century (Romanello et al., 2023). Its effects on human health are complex, multifaceted, and mediated by both direct and indirect pathways. Rising global temperatures, extreme weather events, sea-level rise, and shifting disease patterns are already driving increases in heat-related illness, vector- and water-borne diseases, malnutrition, respiratory conditions, and mental health burdens across the world (Romanello et al., 2021). Vulnerable populations, including children, the elderly, persons with disabilities, and people in low- and middle-income countries (LMICs), are disproportionately affected. Climate change also exacerbates existing inequities in healthcare access, economic security, and environmental exposure (World Health Organization, 2023). Health systems around the world are under increasing pressure to adapt, despite major gaps in evidence, financing and implementation capacity. These challenges highlight the need for localized, context-specific climate-health research to inform national policies and resilience strategies.
In 2024, the Philippines has the highest disaster risk in the world in terms of exposure to varying intensity levels of earthquakes, tsunamis, cyclones, coastal and riverine flooding, droughts and sea-level rise and its vulnerability to susceptibility of such disasters, lack of coping capacities and lack of adaptive capacities (Frege et al., 2024). Due to its geographic location, 60% of the total land area is categorized as hazard-exposed, and 74% of the population is susceptible to these risks (Climate Fact Sheet: Philippines, 2024). On average, the country experiences around 20 typhoons annually. While not all make landfall, many still bring strong winds, heavy rainfall, storm surges, and widespread flooding that can cause devastating impacts (Asian Development Bank, 2024; Jha, 2018). With public health systems already challenged, commonly occurring extreme weather events and natural disasters—exacerbated by climate change—pose ongoing threats to public health. These threats include injuries and deaths, water- and vector-borne disease outbreaks, malnutrition due to food insecurity, mental health issues, respiratory illnesses from ash and/or mold exposure. Disasters also displace people, disrupt health services, and increase vulnerability, particularly among children and the elderly. It is estimated that the health impacts of climate change will cost around USD 5 to 19 million if no significant interventions are implemented (Cruz et al., 2017). Because of the potential economic costs, understanding the health impacts of climate change through research is crucial for guiding policymakers and national agencies in making informed decisions about strategies to mitigate and adapt to climate change.
Because of the potential economic costs, understanding the health impacts of climate change through research is crucial for guiding policymakers and national agencies in making informed decisions about strategies to mitigate and adapt to climate change. The 2017–2022 National Unified Health Research Agenda (NUHRA) highlighted health resiliency as a key research priority, emphasizing studies to understand the impacts of climate change on human health (National Unified Health Research Agenda (NUHRA) 2017-2022, 2024). In response, Chua et al. conducted a scoping review in 2018, analyzing literature from 1980 to 2017, to map the state of this research field at that time and identify gaps for future investigation (Chua et al., 2019).
We conducted this review after the completion of the 2017–2022 NUHRA to provide a progress update on locally-conducted climate change and health research, published from January 2018 to December 2023. Specifically, we aimed to (a) identify trends in climate change and health research in the Philippines over the past 6 years; (b) assess the progress made in this research field; and (c) highlight ongoing research gaps regarding the impacts of climate change on health in the Philippines. These findings aim to contribute to both the country’s climate-health research agenda and the broader evidence base, while offering direction for future policy-relevant and equity-driven research.
2 Materials and methods
This scoping review was conducted according to the PRISMA Extension for Scoping Reviews (PRISMA-ScR) guidelines (PRISMA Statement, 2018), with the completed PRISMA checklist (Supplementary Table S1) found in Supplementary materials. A research protocol was developed and approved as “Exempted from Ethics Review” by the University of the Philippines Manila Research Ethics Board (UPMREB 2024-0324-EX). The methodology and search strategies used were based on the approach outlined by Chua et al. (2019).
2.1 Search strategy
The literature search was conducted using online databases and search engines, including Cochrane Library, the National Institute of Environmental Health Sciences (NIEHS), PubMed, Web of Science, CABI Direct, ScienceDirect, and two Philippine research databases: the Philippine Health Research Registry (PHRR) and the Health Research and Development Information Network (HERDIN). This was done during April to August 2024. We utilized English search terms only across these platforms and were comprised of broad terms on climate factors and health outcomes (Table 1). Detailed search terms for each engine are listed in Supplementary Table S2, as some search engines had specific limitations (e.g., ScienceDirect allowed only a limited number of Boolean operators). We limited the time frame to include published studies from 2018 to 2023, and this was also utilized as a filter for the search engines that have this feature. Grey literature sources were excluded to maintain consistency in methodological rigor, access to full texts, and citation traceability.
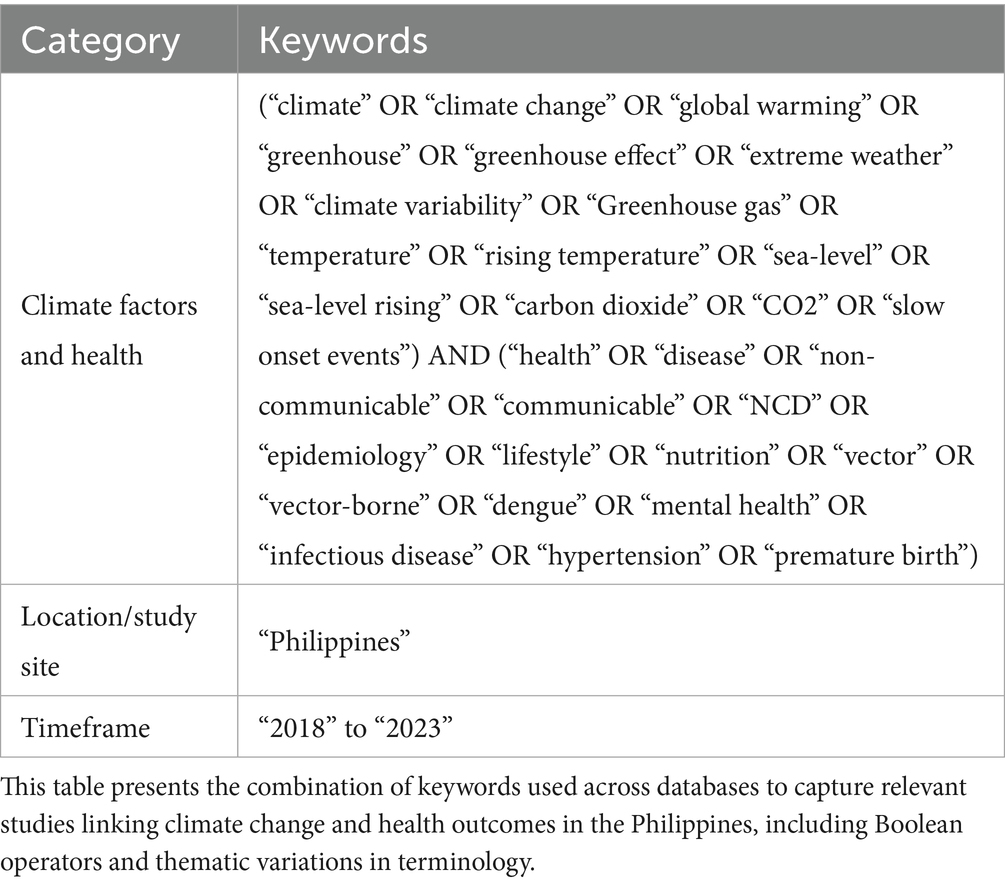
Table 1. Search keywords used to identify climate and health studies in the Philippines (2018–2023).
2.2 Eligibility criteria
We included only full-text original research articles that explicitly outlined objectives, methods, and results. Articles were included if they identified associations between climate factors and human health outcomes, were conducted in the Philippines or Philippine setting, and were published in English, Filipino, or any regional Philippine language translatable to English.
We excluded articles that did not focus on climate change and human health, reported aggregated results from various countries from which findings specific to the Philippines could not be retrieved, or reported the same data from another publication (duplicates). We also excluded reviews and updates (not original research), meeting or news reports, program descriptions, commentaries, theses, book chapters, and studies lacking full-text access or those who are limited to abstract-only access.
2.3 Screening
We compiled articles for screening in Zotero (Corporation for Digital Scholarship, Fairfax, VA, USA). Two reviewers (CD and MLC) independently screened the titles and abstracts only for eligibility. The full-text articles were retrieved and reviewed to confirm compliance with inclusion criteria. Discrepancies in screening were resolved through discussion and consultation with a third (JRL) and fourth (KAA) reviewer to reach a consensus if the articles met the eligibility criteria for inclusion in the final selection list.
2.4 Data analysis and characterization
After the initial screening for inclusion, the full-text papers were downloaded, reviewed in detail, and additional exclusions were applied based on the eligibility criteria. We extracted information such as the year of publication, study location, and the findings from each eligible paper and entered it into a Google Spreadsheet (Google, Mountain View, CA, USA). The studies were then categorized into six research themes, adopted and slightly modified from Smith et al. (2014) (Table 2), which outline various ways climate change affects health. We used excerpts from the papers’ objectives and results to thematically categorize each paper. We utilized Datawrapper (Datawrapper GmbH, Berlin, Germany) to develop the symbol and choropleth maps in this manuscript.
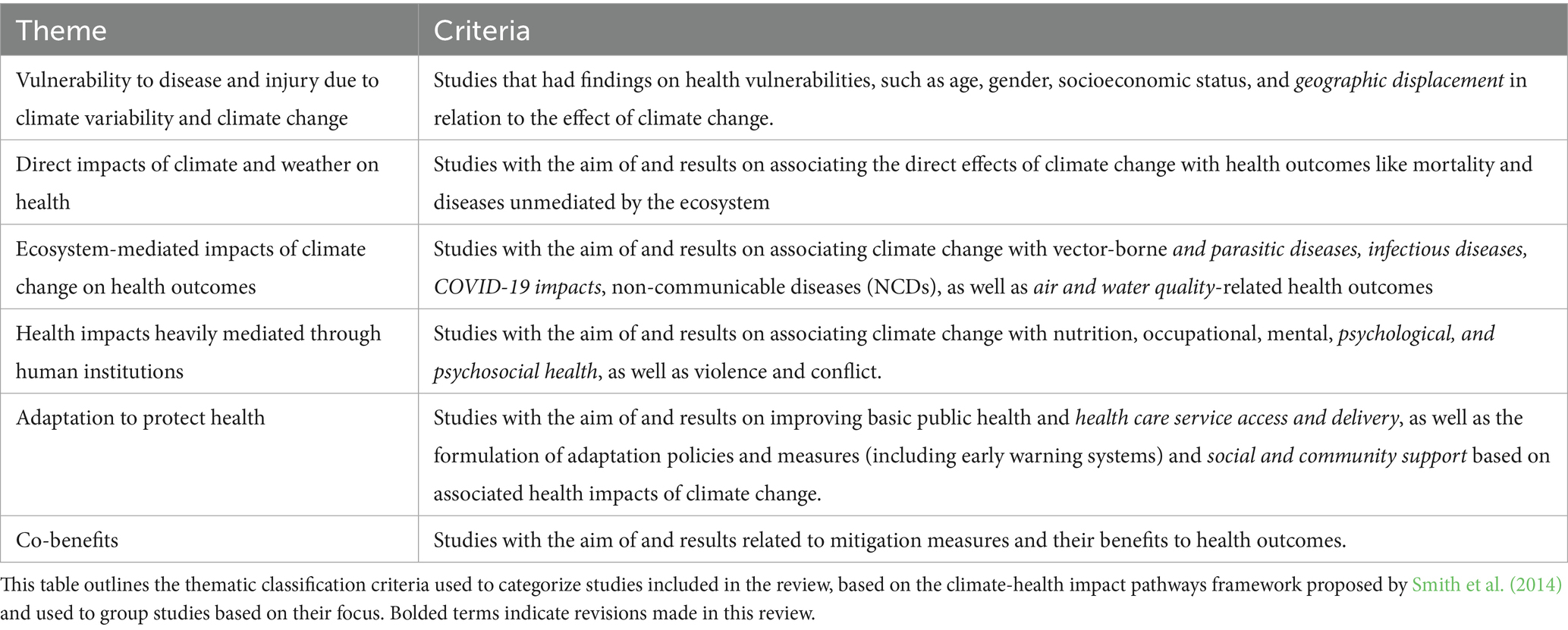
Table 2. Criteria for classifying studies under each climate-health research theme (adopted from Smith et al., 2014).
We conducted a framework-guided thematic synthesis, informed by the climate-health framework developed by Smith et al. (2014), and adapted in the Philippine review by Chua et al. (2019). This approach allowed us to organize studies under the six predefined research themes, enabling structured comparison across study designs, locations and research objectives.
We did not perform a formal risk of bias or quality appraisal of included studies. As the objective of this review was to map research trends and thematic gaps, rather than evaluate treatment effectiveness or establish causality, quality appraisal was deemed not appropriate. This approach aligns with guidance for scoping reviews that include diverse study types and emphasize descriptive synthesis (Munn et al., 2018; Peters et al., 2015).
3 Results
A total of 8,436 articles on climate change and health research in the Philippines from 2018 to 2023 were identified. After removing duplicates (n = 689), 7,747 articles were screened for their titles and abstracts. A majority (53.6%, 4,514) of articles were immediately excluded because they were not focused on climate change and its impacts on human health (Figure 1). Sixty-nine articles were eligible for this review.
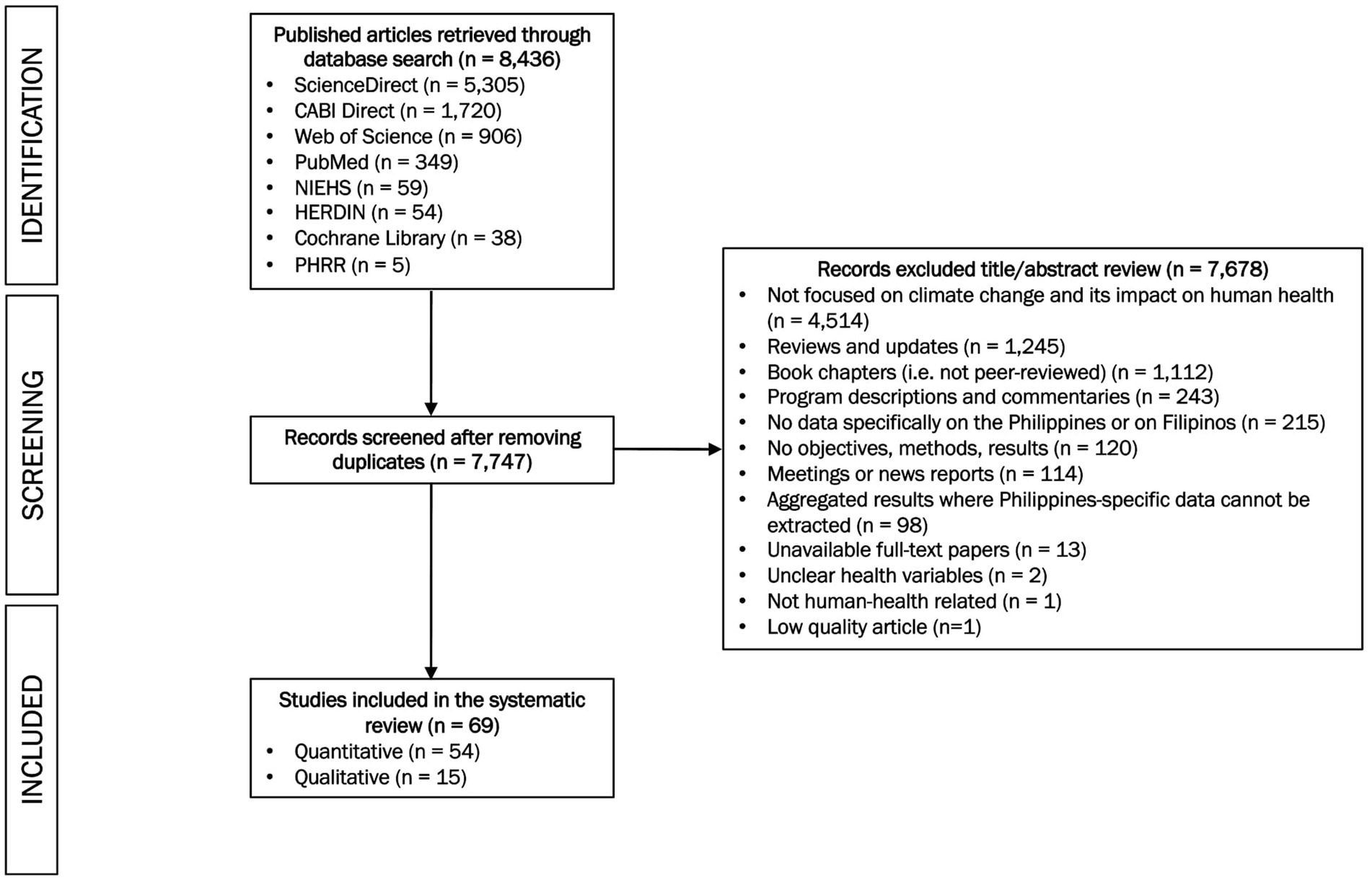
Figure 1. Flowchart of selection process for included articles. This flow diagram illustrates the identification, screening, eligibility assessment and final inclusion of studies in the scoping review.
3.1 General characteristics
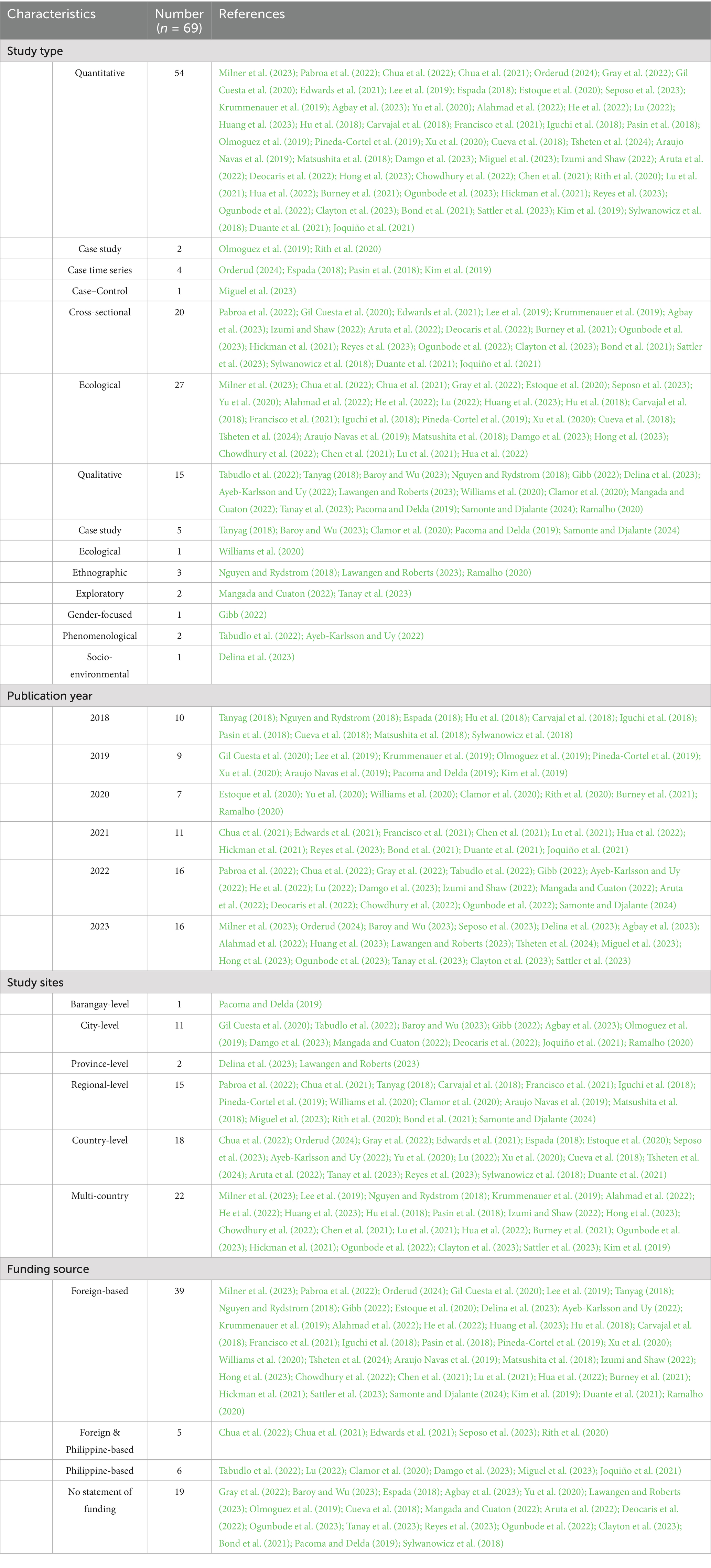
Over three-quarters (78.2%, 54/69) of the included studies used quantitative research study designs (Table 3). Majority of the quantitative study design was ecological (50.0%, 27/54) and cross sectional (37.0%, 20/54) (see Table 3 for more details). Of these studies, 11 (20.4%, 11/54) were on mosquito-borne diseases, 10 on psychological outcomes (18.5%, 10/54), 9 on air quality-related outcomes (16.7%, 9/54), and 9 on temperature-related health outcomes (16.7%, 9/54) due to climate change (Supplementary Table S3). Forty-six percent (46.4%, 32/69) of the selected articles were published in 2022 and 2023, while only 10 % (10.1%, 7/69) were published in 2020 (Table 3). Spatial resolutions of the included studies that were not country or multi-country level were mostly regional-level (21.7%, 15/69). Thirteen studies at the barangay, city, provincial, or regional level were conducted in Luzon, followed by 10 in Mindanao and 7 in the Visayas. Foreign institutions funded the majority of the included studies (56.5%, 39/69), while only 6 (8.7%) were solely funded by Philippine-based institutions (Table 3).
3.2 Research themes
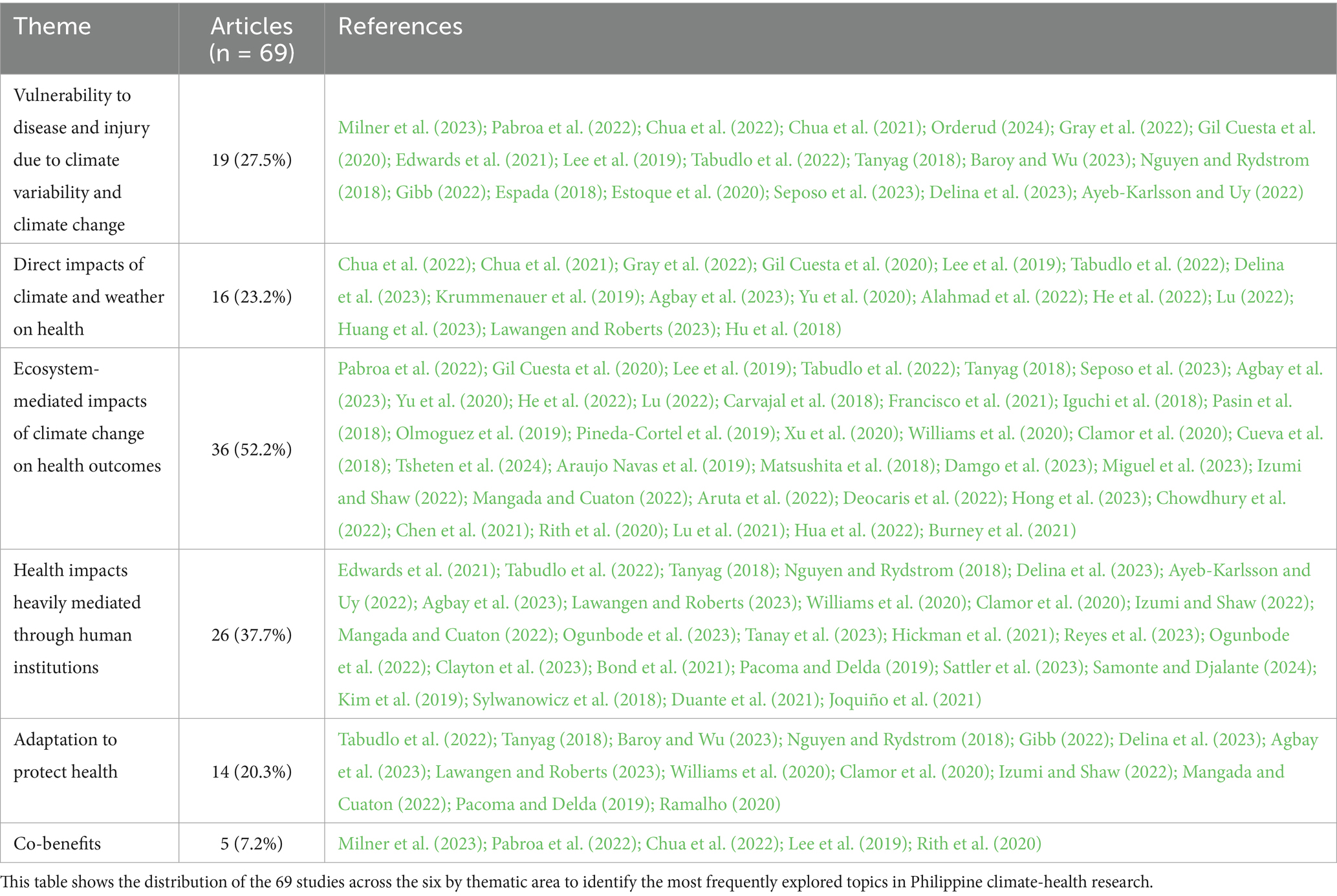
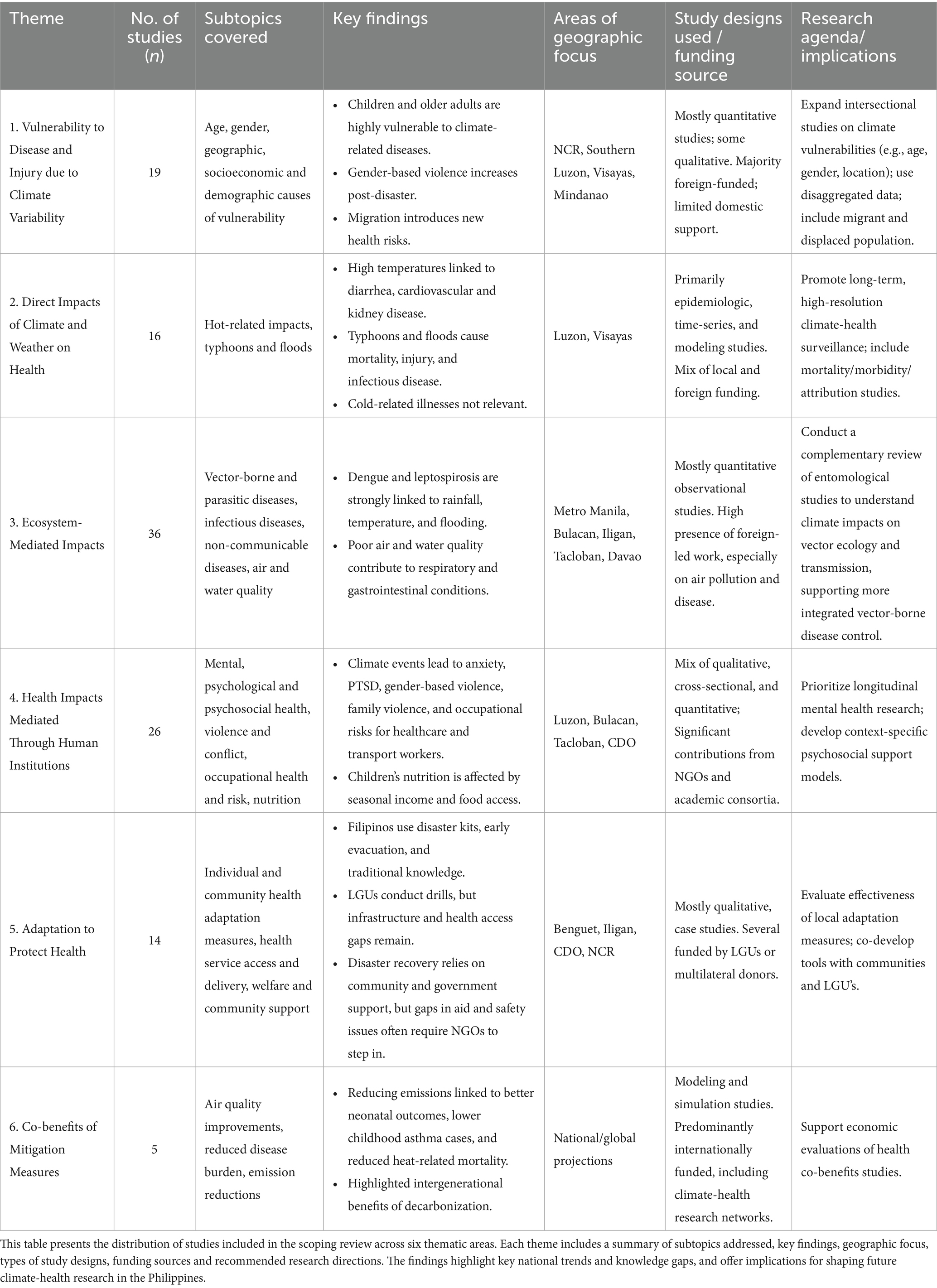
Of the 69 included studies, 36 (52.2%) focused on the theme of “Ecosystem-mediated Impacts of Climate Change on Health Outcomes” (Table 4). Following that, 26 (37.7%) addressed the theme “Health Impacts Heavily Mediated Through Human Institutions.” The research theme with the fewest studies was “Co-benefits,” with only 5 (7.2%) papers.
3.2.1 Vulnerability to disease and injury due to climate variability and climate change
The 19 articles (27.5%) within this theme provide insight into how climate change disproportionately affects vulnerable populations in the Philippines.
3.2.1.1 Age
Children are especially vulnerable to experiencing adverse health outcomes from climate variability. Exposure to fine particulate matter (PM2.5) from combustion-related emissions increases the risk of preterm birth, low birth weight, and carcinogenic risk in children (Milner et al., 2023; Pabroa et al., 2022). Additionally, children under 5 years old are particularly vulnerable to temperature-attributable illnesses, such as enteric infections (Chua et al., 2022). In San Lazaro Hospital in Manila, more than half of the hospitalizations and deaths from severe diarrhea associated with high ambient temperatures occurred in children among this age group (Chua et al., 2021).
While one study found that storms had minimal impact on infant mortality (Orderud, 2024), others highlight the heightened risks for children, including disaster-related mortality, injuries, illnesses, violence, and malnutrition. A study on typhoon mortality in the Philippines (2005–2015) revealed that the mortality count per 100,000 was the second highest among children under 10 (Gray et al., 2022). Following Typhoon Yolanda (known internationally as “Haiyan”), a field hospital in Ormoc City reported that children aged 0 to 4 were most frequently diagnosed with acute respiratory infections (ARIs), acute watery diarrhea, and skin diseases (Gil Cuesta et al., 2020). ARIs were diagnosed in 83.0% of children in this age group (Gil Cuesta et al., 2020). Furthermore, the frequency of natural disasters experienced in each barangay (village) was associated with an increased likelihood of severe food insecurity, stunting, and children’s exposure to violence (Edwards et al., 2021). Each additional disaster increased the likelihood of experiencing family violence by 1.2 times (Edwards et al., 2021).
Older adults also face significant health risks from climate change. Between 2005 and 2015, the typhoon mortality count per 100,000 was highest among those 60 years and older (Incidence rate ratio: 1.227, 95% CI: 0.955–1.576) (Gray et al., 2022). Older adults are also more vulnerable to the effects of non-ambient temperatures. A global study on heat vulnerability found the Philippines had one of the highest vulnerability indexes, rated at 9.15 (Lee et al., 2019). This index reflects regional excess mortality per 1°C increase of regional temperature (%p/°C) and is higher in areas with larger elderly populations (Lee et al., 2019). As temperatures fluctuate, many older adults reported experiencing physical changes and limitations, including increased hypertension and heightened susceptibility to respiratory illnesses (Tabudlo et al., 2022). These findings underscore the heightened risks faced by the elderly as temperatures rise.
3.2.1.2 Gender
There is a complex relationship between gender and climate variability. A study examining typhoon mortality in the Philippines (2005–2015) found higher male mortality rates than female rates, although the reliability of these findings was limited by missing sex information (89%) (Gil Cuesta et al., 2020). Gender differences also emerge in physical and psychological health outcomes following typhoons. After Typhoon Yolanda, men were more likely to suffer typhoon-related injuries than women (65.8% vs. 34.2%), while women more frequently sought care for non-communicable diseases (NCDs) like hypertension, asthma attacks, and diabetes (63.8% vs. 36.2%) (Gil Cuesta et al., 2020).
Gender-based norms and violence often worsen during post-typhoon recovery. Women are more expected to take on caregiving roles in community-based post-disaster recovery efforts, which can lead them to prioritize others’ needs over their own health and well-being (Tanyag, 2018; Baroy and Wu, 2023). Additionally, female survivors reported an increase of domestic and sexual violence post-typhoons (Tanyag, 2018; Nguyen and Rydstrom, 2018; Gibb, 2022), but were often reluctant to report these incidents due to fear of them being blamed for the violence they experienced (Nguyen and Rydstrom, 2018). This suggests how disasters can indirectly perpetuate structural violence and sexism.
3.2.1.3 Geographic, socioeconomic, and demographic causes of vulnerability
Geographic factors contribute to climate vulnerability in the Philippines. A 45-year analysis of tropical typhoon data (1970–2014) revealed that Visayas and southern Luzon were at higher risk for tropical cyclones than northern Luzon and Mindanao (Espada, 2018). However, more recent data (2005–2015) suggest that northern municipalities experienced greater typhoon exposure, with the Visayas region accounting for 59% (n = 7,019) of all typhoon deaths (Gray et al., 2022).
Socioeconomic and demographic factors also influence climate vulnerability. Living in cities exacerbates heat health risk. In a study of 139 Philippine cities, Manila City exhibited very high heat health risk while all other cities in the National Capital Region ranked among the top 20 cities with the highest heat health risks (Estoque et al., 2020). However, the most heat-vulnerable cities were found outside the capital region, where coping capacity is lower (Estoque et al., 2020). In contrast, typhoon mortality rates were higher in rural and peri-rural locations than in urban areas (mortality count per 100,000: 12.8 vs. 26.9) (Gray et al., 2022). Poverty also exacerbates climate risks. Provinces with high population density and poverty incidence had higher dengue risks at upper-temperature ranges (Seposo et al., 2023), and areas like the Cotabato River Basin, a high-poverty incidence area, faced compounded challenges from flooding, siltation, and droughts (Delina et al., 2023).
Migration, a common adaptation to climate change, introduced new vulnerabilities. Domestic and international migrants often face labor and sexual exploitation, as well as human trafficking (Ayeb-Karlsson and Uy, 2022). High migration costs—such as flight tickets, visas, and passports—often trap individuals in debt (Ayeb-Karlsson and Uy, 2022). As climate variability intensifies, protecting vulnerable populations, whether defined by age, gender, or geographical factors, must be prioritized.
3.2.2 Direct impacts of climate and weather on health
The 16 studies (23.2%) within this theme aimed to link the direct impacts of climate change to health outcomes, including mortality and diseases not mediated by the ecosystem.
3.2.2.1 Hot-related impacts
The 9 articles under this sub-theme discussed how temperature variations affect various populations and their health.
The Philippines faces projected increases in excess mortality as global temperatures continue to rise: for every 1°C increase, excess mortality rises by 8.18% globally, and 32.7% in the country (Chua et al., 2021). Climate, topography, and socioeconomic factors are critical in determining temperature mortality rates, particularly in the tropics like the Philippines, where the mortality risk rises significantly above 35.6°C (Krummenauer et al., 2019). High temperatures have been linked to increased diarrhea cases, hospitalizations, and mortality (Chua et al., 2021; Agbay et al., 2023), with one study showing a higher risk of infection for every 1°C increase in temperature (Yu et al., 2020). As the population grows and temperatures rise, projections suggest a significant increase in temperature-related deaths than hospital admissions from enteric infections (Chua et al., 2022), highlighting the country’s vulnerability to heat-related health risks. Pathogen growth due to high temperatures is an important driver of temperature-related mortality. Two studies found that high temperatures are strongly correlated with increased enteric infections caused by Escherichia coli, Shigella spp., Cryptosporidium spp., Entamoeba histolytica, and Salmonella typhi, all linked to pediatric diarrhea-related mortality (Chua et al., 2022; Agbay et al., 2023). Complex interactions between temperature variations and health outcomes exist, demonstrated by one study’s findings that as hospitalizations increase in cooler temperatures, mortality risk from enteric infection increases with higher temperatures (Chua et al., 2022). High temperatures have also exacerbated cardiovascular and chronic kidney diseases, leading to higher mortality risk (Alahmad et al., 2022; He et al., 2022). The elderly population and obese individuals were shown to be particularly vulnerable to heat-related mortality (Lee et al., 2019).
Drought exacerbates health risks by depleting water availability and quality, leading to higher cases of enteric infections, dehydration, skin infections, respiratory problems, heat stroke, and other health issues (Tabudlo et al., 2022; Agbay et al., 2023). Beyond health, drought and extreme heat reduce water availability for irrigation and damage crops, livestock, and food security, which in turn affects people’s health and well-being (Agbay et al., 2023).
3.2.2.2 Typhoons and floods
As one of the most climate-vulnerable nations, the Philippines faces varying disaster-related mortalities, particularly from extreme weather events such as super typhoons and resultant flooding (Lu, 2022). The country frequently experiences tropical cyclones, contributing to high excess deaths (Huang et al., 2023). Rising global temperatures and sea-level rise can exacerbate these impacts, as seen during Typhoon Yolanda, where storms surged up to 5.2 meters and claimed at least 6,000 lives (Lu, 2022). In the aftermath of natural disasters like Typhoon Yolanda, there was a surge in reports of physical injuries (Gil Cuesta et al., 2020), with older adults and men particularly vulnerable to disaster-related mortality (i.e., drowning, landslides) (Gray et al., 2022). Tropical storms with wind velocity exceeding 170 kph resulted in deaths and injuries (Lawangen and Roberts, 2023).
The Philippines has one of the highest flood-induced mortality in Asia, with tropical cyclone-induced floods being a major cause of death in the region (Hu et al., 2018). A multi-country study, including the Philippines, found that Southeast Asia has the highest excess death ratios from tropical cyclones (Huang et al., 2023). For communities living near bodies of water like the Angat River and Cotabato River Basin, recurrent flooding has become a regular and stressful part of their daily lives (Delina et al., 2023; Agbay et al., 2023).
3.2.3 Ecosystem-mediated impacts of climate change on health outcomes
The 36 studies (52.2%) within this theme aimed to establish associations between climate factors and their impacts on health outcomes.
3.2.3.1 Vector-borne and parasitic diseases
Studies have associated rainfall, temperature, and humidity with dengue incidence. Rainfall is a key factor (Carvajal et al., 2018), with dengue risk generally higher during the rainy season (Francisco et al., 2021; Iguchi et al., 2018; Pasin et al., 2018). In Metro Manila, this relationship was most pronounced in densely populated residential and commercial areas (Francisco et al., 2021). Relative humidity also influenced dengue incidence in Metro Manila and Iligan City (Carvajal et al., 2018; Olmoguez et al., 2019).
Temperature’s relationship with dengue incidence was more complex, varying across provinces (Olmoguez et al., 2019; Pineda-Cortel et al., 2019; Xu et al., 2020). In some areas, dengue cases increased with rising temperatures; in others, cases decreased as the temperature rose (Xu et al., 2020). A nationwide study reported that dengue risk increased linearly with average temperature, peaking at 27.5°C before declining (Seposo et al., 2023). In Davao City, lower temperatures around 26°C were linked to higher dengue risk (RR: 1.96, 95% CI: 0.47–8.15), while higher temperatures (27–31°C) were linked to a decreased risk (Iguchi et al., 2018). Similarly, in Metro Manila, they found a positive association between minimum temperature and dengue incidence, while average and maximum temperature showed a negative association (Carvajal et al., 2018).
Despite these associations, a nationwide study using multiple regression analysis suggested that rainfall, humidity, and temperature were poor predictors of dengue incidence (R2 = 0.1436, 0.0461, and 0.0209, respectively) (Yu et al., 2020). In contrast, a more consistent pattern emerged linking dengue outbreaks to flooding events, with survivors observing spikes following periods of heavy flooding (Williams et al., 2020; Clamor et al., 2020).
Other studies on climate change and mosquito-borne diseases found that sea level changes, average temperature anomalies, and global CO2 levels were negatively correlated with malaria incidence and other tropical diseases in the Philippines (Lu, 2022). Another study found no correlation between rainfall and the nationwide Chikungunya prevalence (Cueva et al., 2018).
For parasitic diseases, a 1°C increase in temperature and a 1 mm increase in rainfall was associated with a higher risk of soil-transmitted helminth infections (Tsheten et al., 2024). Day and night land surface temperatures were key factors relevant for modeling schistosomiasis transmission (Araujo Navas et al., 2019).
3.2.3.2 Infectious diseases
Floods, typhoons, and rising temperatures increase the risk of infectious diseases like athlete’s foot, common colds, flu, diarrhea, and leptospirosis (Williams et al., 2020; Clamor et al., 2020). In Manila, heavy rainfall was associated with increased leptospirosis hospitalizations due to flooding (Matsushita et al., 2018). Likewise, in Davao City, precipitation heightened the risk of emerging infectious diseases (Damgo et al., 2023). Following Typhoon Yolanda, most medical consultations in Ormoc City were for communicable diseases (88.2%), especially acute respiratory infection (73.1%) (Gil Cuesta et al., 2020). Female survivors faced heightened risks of STDs and HIV/AIDS due to limited access to contraceptives and healthcare, and post-disaster gender-based violence (Tanyag, 2018).
Some studies also linked climate factors to the COVID-19 pandemic, with increased temperature and rainfall associated with a higher likelihood of COVID-19 spread and infection (Miguel et al., 2023). On the other hand, the pandemic and fear of infection hindered evacuation efforts during natural disasters and led people to resort to natural remedies instead of seeking healthcare (Izumi and Shaw, 2022; Mangada and Cuaton, 2022). During “double disasters,” when extreme weather events and global health crises coincide, community resilience and social responsibility are crucial to Filipinos’ well-being (Aruta et al., 2022).
3.2.3.3 Non-communicable diseases
Extreme weather events can be associated with non-communicable diseases. Flood survivors in Iligan and Cagayan de Oro were burdened with tetanus, hypertension, and cardiac arrest (Clamor et al., 2020), while farmers in Angat, Bulacan reported hypertension, dehydration, heat stroke, and other mild illnesses during droughts (Agbay et al., 2023). In Tacloban 3 years after Typhoon Yolanda, heavy metal levels in the Mangonbangon River indicated the return of anthropogenic activities and pollution-related health problems but with no non-carcinogenic or carcinogenic health risks for adults and children living nearby (Deocaris et al., 2022).
Rising temperatures were positively associated with non-communicable diseases (Lu, 2022). Older adults commonly reported experiencing coughs, colds, and headaches and expressed concerns about hypertension during hot weather (Tabudlo et al., 2022). Additionally, the burden of heat-attributable cardiovascular and chronic kidney disease is increasing in the country, with the Philippines often showing the largest estimated annual percentage changes in age-standardized rates of mortality (ASMR) and disability-adjusted life years (DALYs) (ASDR) globally (He et al., 2022; Hong et al., 2023). Conversely, heat vulnerability positively depended on the proportion of the obese population (Lee et al., 2019). With the increasing trend of obesity in the country (40.2% of adults in 2021) (WHO, 2024), heat vulnerability will also increase.
3.2.3.4 Air and water quality (WASH)
Air pollutants, such as CO2 and particulate matter (PM2.5), are associated with significant health risks. Average global CO2 levels were positively associated with air pollution mortality and negatively associated with household air pollution health risk exposure in the Philippines (Lu, 2022). Long-term exposures to ambient PM2.5 caused approximately 17,511 (95% CI: 10,670–29,902) excess deaths yearly (Chowdhury et al., 2022). The country also had one of the highest risks of respiratory deaths from short-term exposure to wildfire-related PM2.5 (Chen et al., 2021). In Metro Manila, exposure to PM2.5 was linked to high cancer risk in children, and non-carcinogenic diseases in both children and adults (Pabroa et al., 2022). A statistical modeling study projected that health-related economic losses from carbon emissions in the Philippines could reach nearly USD 237 million by 2050 (Rith et al., 2020).
Exposure to household air pollution (HAP) was also linked to adverse health outcomes. A global study (1990–2019) found that the Philippines had an annual increase in ASDR and ASMR of stroke burden attributable to HAP, contrasting with declines in other regions (Lu et al., 2021). Globally, the Philippines also exhibited the highest increases in ASDR and ASMR for ischemic heart disease linked to HAP (Hua et al., 2022). However, one study found no link between burning solid fuels indoors and chronic airflow obstruction due to insufficient data (Burney et al., 2021).
Exposure to poor water quality due to extreme climate events leaves individuals vulnerable to water-borne diseases. For example, residents in Angat, Bulacan exposed to contaminated flood water faced higher risks of skin disease, diarrhea, and other common water-borne diseases (Agbay et al., 2023).
3.2.4 Health impacts heavily mediated through human institutions
The 26 studies (37.7%) within this theme aimed at determining the effects of climate change on mental, psychological, and psychosocial health, violence and conflict, occupational health, and nutrition.
3.2.4.1 Mental, psychological, and psychosocial health
The 18 articles under this sub-theme discussed how certain populations affected by extreme weather events dealt with mental health problems, trauma, and their psychological well-being.
Several studies highlight the significant psychological distress associated with climate anxiety. Climate anxiety is defined as emotional distress caused by concern about climate change and is often used interchangeably with the concept of eco-anxiety, described as a chronic fear of ecological disaster (Ogunbode et al., 2023; Clayton, 2020). Extreme weather events, including typhoons, floods, and temperature extremes, can worsen both physical and mental health (Tabudlo et al., 2022; Tanay et al., 2023). Countries in the Global South, including the Philippines, reported that negative climate-related emotions like fear, sadness, anxiety, guilt, and worry were common, while optimism and indifference were rare (Hickman et al., 2021). These negative emotions were also positively associated with insomnia and negatively related to self-assessed mental health in most countries, including the Philippines (Ogunbode et al., 2023). Among 10,000 young people (ages 16–25) surveyed, a significant proportion (75%) view the future as frightening, with many feeling ignored or dismissed when discussing climate change (Hickman et al., 2021). Climate anxiety is associated with lower overall mental health and pro-environmental behavior (i.e., green consumerism, taking public transport, etc.) particularly among Gen Z Filipinos (Reyes et al., 2023; Ogunbode et al., 2022).
Gender differences also emerge, with women in the Philippines more emotionally distressed by climate change than men, expressing higher levels of worry and a sense of betrayal by governments (Clayton et al., 2023). Vulnerable populations, including children, suffer significant psychological stress from climate change. Many survivors report anxiety, panic, isolation, and posttraumatic stress disorder (PTSD), especially after flooding (Delina et al., 2023; Lawangen and Roberts, 2023; Clamor et al., 2020). Direct experiences of disasters create more vivid and detailed memories, confirming that these experiences are remembered more clearly than other events (Bond et al., 2021). Psychological stress is more intense in disaster-prone areas, especially when caregivers suffer from depression or families face increased violence (Edwards et al., 2021). Healthcare providers, such as nurses, also report difficulties in offering care during extreme weather, further exacerbating challenges for patients, including those with cancer (Tanay et al., 2023).
Psychosocial resilience is vital for mental health recovery, with social networks being crucial for building resilience in disaster-affected communities (Pacoma and Delda, 2019). However, some households still struggle with inadequate resources, unstable finances, and ongoing stress which impedes their recovery (Pacoma and Delda, 2019). Posttraumatic growth, reassessment of one’s values and reinterpretation of life events, can enhance climate change risk perception and rebuild mental health and resilience after climate-related disasters (Sattler et al., 2023).
Migration induced by climate-related disasters also has complex mental health consequences (Ayeb-Karlsson and Uy, 2022). Migrants, particularly children and women, struggle with the loss of familiar surroundings and social networks (Ayeb-Karlsson and Uy, 2022). Children left behind by migrating women face a higher risk of anxiety and depression (Ayeb-Karlsson and Uy, 2022). Forced displacement, such as during Typhoon Ondoy (internationally known as “Ketsana”), alters family dynamics, including roles, separations, and parenting styles (Samonte and Djalante, 2024).
While some studies suggest a link between higher temperatures and increased suicide risk, this relationship is not yet clearly established in the Philippines, possibly due to constant exposure to high temperatures (Kim et al., 2019). Local factors like adaptation to temperature and cultural differences might influence the results (Kim et al., 2019).
Finally, the combined impact of natural disasters and crises like the COVID-19 pandemic has compounded mental health issues in the Philippines (Izumi and Shaw, 2022). Economic stress, loss of social ties, and strict lockdowns exacerbated psychological distress. Effective communication and tailored mental health recovery support are essential for managing these varied impacts (Izumi and Shaw, 2022).
3.2.4.2 Violence and conflict
The 5 articles under this sub-theme discussed how violence and conflicts arise in vulnerable populations and communities in the aftermath of disaster exposure. Extreme weather events, like Typhoons Yolanda and Sendong (international name “Washi”), worsened clan and family conflicts, leading to displacement and creating more problems in evacuation and resettlement sites (Delina et al., 2023). These events also exposed and intensified gender-based violence and social traumas, revealing deeper structural community issues. Disasters worsen domestic violence against women, including financial distress, marital rape, sexual abuse, and human trafficking, rooted in cultural norms that value male authority (Tanyag, 2018; Nguyen and Rydstrom, 2018). Women’s vulnerability is further increased by limited access to reproductive healthcare, leading to unwanted pregnancies and mental and physical stress (Tanyag, 2018). Adolescent pregnancies in displacement camps reflect ongoing issues with rape and gender-based violence, highlighting barriers to reproductive healthcare and reinforcing pre-existing disparities (Tanyag, 2018).
Children are also severely affected, experiencing higher rates of physical abuse and family violence, as well as parental stress in disaster-affected households (Edwards et al., 2021). The strain of frequent disasters leads to an increase in family violence and child abuse, destabilizing family units and harming child welfare (Edwards et al., 2021).
The COVID-19 pandemic further exacerbated these issues, increasing risks of hunger, petty crime, and neighborhood disputes, further destabilizing social cohesion (Mangada and Cuaton, 2022).
3.2.4.3 Occupational health and risk
The 5 articles under this sub-theme examined the impact of extreme weather events on various sectors and its consequences in terms of their occupational health.
In Angat, Bulacan, 39.19% of household farmers reported significant health impacts (i.e., hypertension, dehydration, diarrhea, etc.) brought by drought (Agbay et al., 2023). Transport workers, such as tricycle drivers from Hagonoy, Bulacan and Malabon, were severely impacted by flooding and often reluctant to operate during floods due to safety concerns (Williams et al., 2020).
In healthcare, nurses face climate-related challenges. Flooding, for instance, disrupts clinical shifts, causes staff shortages, and increases fatigue, all of which compromises patient care (Tanay et al., 2023). Furthermore, climate-related disasters have left first-line medical responders with psychological trauma, with 30% showing PTSD symptoms and 7% suffering from depression (Sylwanowicz et al., 2018). Migration from rural areas affected by slow-onset climate events like drought, further reflects the socioeconomic impact of climate change on occupational health, with many farmers in Luzon facing debt and seeking better opportunities (Ayeb-Karlsson and Uy, 2022).
3.2.4.4 Nutrition
The 6 articles under this sub-theme explored the effects of extreme weather events on human nutrition.
In the Philippines, extreme weather events have caused both immediate (e.g., food unavailability and shortages, food and water accessibility) and long-term (e.g., chronic malnutrition and food insecurity) health consequences (Lawangen and Roberts, 2023; Izumi and Shaw, 2022). Studies have shown that children exposed to natural disasters were more likely to be stunted (35%) and experience food insecurity in their households (35%) (Edwards et al., 2021). The 2015 National Nutritional Survey (NNS) found that 37.8 and 24.3% of households were exposed to typhoons and floods, respectively, which reduced their ability to meet the recommended energy intake (REI) (Pacoma and Delda, 2019; Duante et al., 2021).
The NNS surveys also found that households exposed to typhoons and/or floods within 3 months prior to the survey were more likely to meet their REI, likely due to short-term relief efforts such as food aid (Duante et al., 2021). However, those exposed to disasters 6 months prior were less likely to meet the REI, reflecting the challenges of the longer recovery and rehabilitation period (Duante et al., 2021). In contrast, drought exposure did not significantly affect the REI, likely due to its prolonged and indirect effects on food security (Duante et al., 2021). Another study found that droughts exacerbated malnutrition and food insecurity, especially among vulnerable populations (Delina et al., 2023). Flooding and river siltation also disrupt agriculture, leading to income loss and further food insecurity (Delina et al., 2023).
Seasonal changes also impact children’s nutrition. A study among children of fishermen in Davao found that the average daily energy intake dropped from 1523.56 kcal/day during the northeast monsoon to 1403.16 kcal/day in summer, both below the Philippine Dietary Reference Intakes (PDRI) (Joquiño et al., 2021). Protein intake remained adequate, while fat intake declined, resulting in inadequate overall intake (Joquiño et al., 2021). Due to declines in fish catches and income in the summer, families shifted from home-cooked meals to cheaper, processed foods, further reducing children’s nutrient intake (Joquiño et al., 2021).
3.2.5 Adaptation to protect health
The 14 studies (20.3%) related to this theme focused on programs and measures designed to tackle the additional pressures of climate change. This includes individual and community-level health strategies to cope with climate variability, access to and delivery of health services, and social and community support.
3.2.5.1 Health adaptation measures (individual level)
Preparing for natural disasters is a key adaptation strategy for climate change. In one study, 94.8% of surveyed Filipinos took steps to prepare for an incoming natural disaster by staying informed through media outlets (TV, radio, and SNS) and preparing emergency items with supplies like canned goods, water, candles, flashlights, and medicine (Williams et al., 2020; Clamor et al., 2020; Izumi and Shaw, 2022). They also secured important documents, stored belongings on higher floors, and anchored furniture to posts (Williams et al., 2020). Many follow disaster protocols, such as going to the nearest evacuation centers (Clamor et al., 2020).
Additionally, a study on older adults (60–77 years) showed that they adapt to rising temperatures by modifying behaviors, such as wearing weather-appropriate clothing, adjusting diet and water intake, and limiting outdoor activities, demonstrating resilience to climate change (Tabudlo et al., 2022).
3.2.5.2 Health adaptation measures (community level)
Local government units (LGUs) have implemented various disaster risk reduction and management (DRRM) measures to prepare their communities for climate change. In coastal municipalities in Luzon, infrastructure projects like elevating roads, installing floodgates, and dredging waterways help mitigate risks, while penalties for littering and blocking waterways are being more consistently enforced (Williams et al., 2020). Although recent improvements in infrastructure have helped reduce flood risk in some communities, risk from major storms still persist (Williams et al., 2020). When infrastructure improvements are deemed inadequate, barangays shift to using other strategies such as rescue boats and trailer trucks to respond to emergencies (Williams et al., 2020). LGUs also conduct disaster preparedness drills, to teach residents how to respond to warnings, evacuate, and act during disasters (Agbay et al., 2023; Williams et al., 2020). In Iligan and Cagayan de Oro, leaders go house-to-house to inform residents of incoming typhoons and provide emergency relief and health assistance after disasters (Clamor et al., 2020).
In Benguet, Indigenous communities rely on local knowledge and practices to strengthen disaster resilience. Water conservation technologies and activities like maintaining water facilities, clearing drainage canals, and establishing fire lines help reduce risks (Lawangen and Roberts, 2023). During dry spells and periods of water scarcity, farmers adapt by being mindful with choosing climate-resilient crops to plant to ensure stable food sources, availability, and maintenance of farm biodiversity for the community (Lawangen and Roberts, 2023). Social support systems and cultural rituals assist in coping with loss, ensuring food access, and alleviating distress after disasters (Lawangen and Roberts, 2023). These community-based practices promote proactive measures to protect health and safeguard against extreme climate events.
3.2.5.3 Health service access and delivery
Access to quality health services after disasters remains limited in parts of the Philippines. Hospitals and other health facilities are often far from resettlement sites, making them difficult to reach, especially for survivors lacking public transportation or having to navigate rough terrain (Baroy and Wu, 2023; Mangada and Cuaton, 2022; Ramalho, 2020). Women, with distinct sexual and reproductive needs and higher vulnerability to post-disaster violence, are particularly dependent on timely access to quality healthcare, such as prenatal care (Tanyag, 2018; Baroy and Wu, 2023).
When accessible medical assistance is available, challenges persist, such as language barriers between patients and external volunteers, limited medication, and occasional doctor shortages (Clamor et al., 2020). Survivors also report being unable to afford healthcare (Clamor et al., 2020). This demonstrates the unequal access to comprehensive healthcare that fully addresses the survivors’ needs.
3.2.5.4 Welfare and community support (government and non-governmental support)
In the aftermath of disasters, community and social support are crucial for facilitating recovery. Local ties (those living nearby and can offer support on short notice) and translocal ties (individuals residing outside disaster-affected areas) provide food, financial assistance, and psychosocial support to impacted individuals (Pacoma and Delda, 2019). However, their ability to assist depends on having sufficient resources for themselves (Pacoma and Delda, 2019). Additionally, some individuals may not volunteer in post-disaster efforts as they are also impacted by the disaster (Izumi and Shaw, 2022).
Government organizations also play an important part in disaster recovery, launching initiatives to combat gender violence after disasters and offering support to abused women and girls (Nguyen and Rydstrom, 2018). Unfortunately, survivors often report insufficient aid. For instance, individuals in the Cotabato River Basin have called on provincial governments to release calamity funds and provide rice during droughts (Delina et al., 2023). Official evacuation camps are frequently unsafe for women (Gibb, 2022), and resettlement houses often expose survivors to scorching weather due to inadequate shelter (Mangada and Cuaton, 2022). As a result, non-governmental organizations have had to fill in the gaps for unequal access to post-disaster recovery resources (Tanyag, 2018). These challenges highlight the need for government agencies to provide more comprehensive and equitable disaster aid.
3.2.6 Co-benefits
The 5 articles (7.2%) within this theme pertained to mitigation strategies and their advantages to health outcomes.
Two studies projected the health effects of temperature changes under varying amounts of greenhouse gas (GHG) emissions scenarios based on the Representative Concentration Pathway (RCP) (CoastAdapt, 2016). In the worst-case climate scenario (RCP 8.5), global mean temperatures are projected to rise by 3.7°C by 2,100 (CoastAdapt, 2016). Under this scenario, the Philippines may witness a sharp surge in heat-related and enteric infection-related deaths, as well as more severe outcomes for hospital admissions if high-temperature increases continue (Chua et al., 2022). Meanwhile, the lower-emission scenario (RCP2.6) where temperatures might increase by 1°C by 2,100 (CoastAdapt, 2016), could result in lower excess mortality and more moderate temperature increases due to reduced emissions (Lee et al., 2019). Countries like the Philippines can benefit from following lower-emission pathways which could significantly reduce heat-related mortality by slowing temperature increases (Chua et al., 2022), offering both public health and climate change benefits (Milner et al., 2023; Pabroa et al., 2022; Rith et al., 2020). Coastal areas, benefitting from the cooling effect of water, might experience more consistent temperatures, suggesting that maintaining ecosystems might help mitigate temperature rise and indirectly benefit health (Lee et al., 2019).
Reducing vehicle emissions (e.g., CO2, NO, black carbon (BC), and particulate matter (PM)) can improve air quality and lower the risk and incidence of diseases like cancer, cardiovascular disease, and respiratory conditions, especially among vulnerable populations (Milner et al., 2023; Pabroa et al., 2022; Rith et al., 2020). This can be achieved by modernizing public transportation systems, improving accessibility, and upgrading infrastructure (Pabroa et al., 2022).
Lower NO2 levels in a year could save an estimated 3,601 childhood asthma cases under the decarbonization scenario (Milner et al., 2023). For neonatal and infant health, reducing particulate matter could avoid 852 instances of preterm births per 100,000 preterm deliveries and 896 cases of low birthweight infants per 100,000 (Milner et al., 2023). Lowering PM2.5 concentrations could prevent both cancerous and non-cancerous health problems, particularly in children, who are more susceptible to the carcinogenic and non-carcinogenic hazards associated with PM and BC (Pabroa et al., 2022).
Healthier birth outcomes promote long-term health and development, benefiting future generations and the broader community. This highlights the intergenerational benefits of reducing GHG emissions.
4 Discussion
4.1 Comparison of results to the previous scoping review and alignment with global climate-health evidence
We identified 69 articles published between 2018 and 2023 linking climate change and health in the Philippines. This marks a significant increase compared to the previous scoping review by Chua et al. (2019), which found only 40 articles over a 37-year study period (1990–2017)—representing a 72.5% increase in the number of studies identified (Table 5). The surge in publications, particularly in 2022 and 2023, suggests a growing recognition of climate change as a significant public health issue in low- and middle-income countries (LMICs), consistent with global trends showing rising interest in the health impacts of climate extremes (Romanello et al., 2023; Bianco et al., 2024). The earlier Philippine scoping review noted gaps in four research areas—“Vulnerability to Disease and Injury Due to Climate Variability and Climate Change,” “Adaptation to Protect Health,” “Health Impacts Heavily Mediated through Human Institutions,” and “Co-benefits”—and recommended prioritizing health vulnerabilities and adaptation research. Based on our findings (Table 5), these areas have been prioritized in recent years. Although studies quantifying the benefits of reducing GHG emissions remain limited (“Co-benefits” studies), the current scoping review suggests progress in addressing this research gap. This aligns with international findings showing that while co-benefits research is growing, it is still underrepresented in LMICs compared to high-income countries (Dinh et al., 2024).
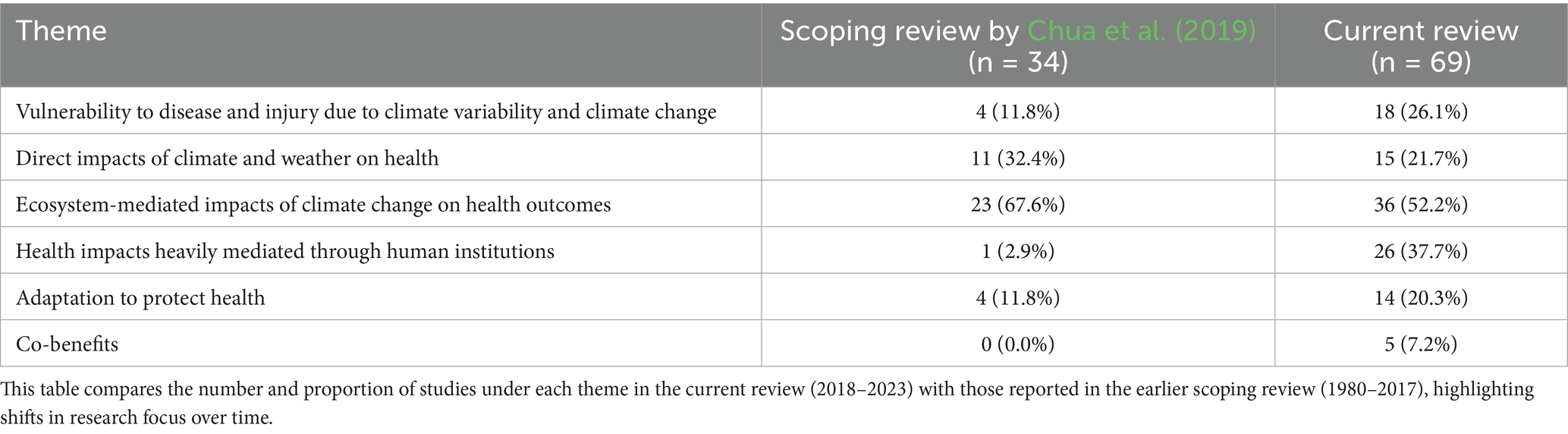
Table 5. Comparison of theme distribution between this review and the 2019 Scoping Review by Chua et al. (2019).
The growth of studies on “Health Impacts Heavily Mediated through Human Institutions” from 1 (2.9%) in 2018 to 26 (37.7%) in this scoping review– mirrors the rising global interest in mental health, gender-based violence, and occupational stress linked to climate change, observed in countries like South Africa, India, Bangladesh and Pakistan (Khine and Langkulsen, 2023; Ngcamu, 2023). In the Philippine setting, this growth may be attributed to the prioritization of mental health research in the through its inclusion in the 2017–2022 National Unified Health Research Agenda (National Unified Health Research Agenda (NUHRA) 2017-2022, 2024), the enactment of the Philippine Mental Health Act in 2018 (Supreme Court E-Library, 2018), and the conception of the first National Mental Health Research Agenda in 2019 (Lazo and Ignacio, 2019). Examining the various health impacts of climate change beyond disease, injury, and mortality offers a more comprehensive understanding of its broad effects on public health and paves the way for more integrative solutions.
Geographically, most studies were concentrated in Luzon, particularly in the National Capital Region (NCR) (Supplementary Figure S1). In contrast, even though there were fewer studies in Mindanao and Visayas, these studies were more spread out across the island group compared to those in Luzon. This imbalance, possibly driven by differences in research funding and institutional capacities, may reflect disparities in climate-health research (Supplementary Figure S2). This also reflects a common global pattern in climate-health research, where urban and capital regions dominate study sites, leaving rural and remote areas underrepresented (Bianco et al., 2024). Moreover, the predominance of foreign-funded studies in the Philippines further highlights the need for greater domestic investment in climate-health research capacity.
4.2 Strengths and limitations
The strengths of this scoping review include its comprehensive scope, covering climate change and health research in the Philippines from 2018 to 2023, and highlights a significant increase in research output compared to previous reviews. The study also benefits from a rigorous methodology, using multiple databases and well-defined inclusion criteria to ensure relevant studies were captured. Additionally, it categorizes research into six key themes adapted from Smith et al. (2014) and Chua et al. (2019), allowing for a structured analysis of trends and gaps in the field. We employed a framework-guided thematic synthesis, which is particularly well-suited for analyzing heterogenous public health evidence in scoping reviews (Thomas and Harden, 2008).
However, some limitations exist. The review acknowledges potential classification biases, as the interpretation of included studies may vary from previous reviews. To maintain a focus on human health, we also excluded entomological studies, which could have provided valuable insights into vector-borne disease transmission related to climate change. While this decision helped preserve the direct human health perspective, we recognize that excluding entomological studies may omit important insights into vector ecology and transmission dynamics that mediate climate-related disease risks. Incorporating entomological findings in future integrated reviews could enrich understanding of the complex pathways linking climate change and health.
Furthermore, studies quantifying the co-benefits of GHG mitigation for health remain limited. Addressing this gap is critical for informing policymakers, as demonstrating broader benefits of climate action beyond direct health impacts can strengthen support for mitigation strategies. Our findings suggest emerging interest in co-benefits research, yet more focused efforts are needed to advance this vital area.
This review also relied exclusively on published, peer-reviewed literature. As a result, relevant but unpublished, ongoing, or community-based research may have been excluded. Some online platforms that host local publications were also excluded after a preliminary assessment found limitations in search functionality, full-text availability, and citation formatting. While these platforms were excluded to preserve methodological rigor and ensure systematic replicability, they may still contain valuable grey literature. We recommend that future reviews consider including such sources through manual or targeted screening protocols.
Lastly, the geographic concentration of studies in Luzon highlights disparities in climate-health research coverage across the Philippines, suggesting a need for more localized studies in Visayas and Mindanao.
4.3 Research agenda setting: opportunities for generating climate information services and climate-health research
The expanding landscape of climate-health research in the Philippines presents key opportunities for enhancing climate information services and guiding future research agendas. First, future studies should consider longer time periods when linking climate variables with disease, as shorter time periods may miss trends and lead to premature conclusions. Because climate is commonly defined as the average weather over time (Intergovernmental Panel On Climate Change (IPCC), 2023), the World Meteorological Organization recommends a 30-year period to determine the average climate (World Meteorological Organization, 2021). This 30-year period is believed to be long enough to filter out any interannual variation or anomalies such as El Niño-Southern Oscillation (ENSO), but also short enough to be able to show longer climatic trends (World Meteorological Organization, 2021). However, only nine studies in this review met this criterion, and all relied on international data sources. To our knowledge, no long-term study of at least 30 years using exclusively local climate and health data from the Philippines currently exists. The lack of long-term studies using local data may be due to poor data quality, such as unavailable or inconsistent climate and health data.
Furthermore, more localized research is needed. Only 11 (15.9%) of the 69 studies were conducted at the city-level, while most were national or multinational level. Local studies will help inform local government units on climate-health trends specific to their area, enabling more targeted interventions.
Developing local databases is also crucial. Only four studies were sourced from the two main Philippine databases (HERDIN and PHRR). HERDIN exclusively publishes finished research studies, while PHRR, a new initiative created by Philippine Department of Science and Technology, allows researchers to publish new and ongoing studies. Strengthening these platforms, including improving accessibility, indexing and search functionality, will help reduce duplication and support national coordination of climate-health research.
Additionally, co-benefits research and cohort studies should be prioritized. Co-benefits research that quantifies the benefits of mitigating GHGs, could help persuade policymakers. Prospective cohort studies, though complex, may offer better insight into the long-term impacts of climate change on human health.
In addition to these system-level priorities, our thematic analysis revealed specific research implications across the six major climate-health domains (Table 6). In the area of Vulnerability to disease and injury, future research should expand intersectional studies that explore how climate-related health vulnerabilities vary by age, gender, geography, socioeconomic status, and displacement. Disaggregated data and population-specific analyses are essential to inform targeted interventions, particularly for marginalized or vulnerable groups such as children, older adults, and migrants.
For Direct health impacts, there is a need to promote long-term, high-resolution climate-health surveillance, especially studies using local meteorological data and health outcomes. This includes mortality/morbidity attribution studies that examine the impact of extreme heat, floods or typhoons on specific diseases or injuries.
Research on Ecosystem-mediated impacts, particularly vector- and water-borne diseases, should be complemented by a separate synthesis of entomological studies. Although excluded from this scoping review due to a focus on direct human health outcomes, these studies offer critical insights into vector ecology and transmission dynamics. To inform integrated vector-borne disease control strategies. This would provide a more comprehensive understanding of how climate influences ecosystem-mediated health risks.
In the domain of Health impacts mediated through human institutions, we identified a growing body of research focused on mental health, gender-based violence, nutrition and occupational risks. To further develop this area, longitudinal studies and context-specific models of psychosocial support are needed, especially in post-disaster contexts. Additional research should also examine how institutional responses (e.g., education systems, labor conditions, food security programs) mediate health outcomes during and after climate shocks.
For Adaptation strategies, future research should evaluate the effectiveness of individual and community-level responses, including the use of traditional knowledge, disaster kits, health-seeking behaviors, and early warning systems. Partnering with local government units and at-risk communities to co-develop and validate adaptation tools and metrics will ensure greater contextual relevance and equity in adaptation planning.
Finally, in the domain of co-benefits of mitigation measures, there is a critical need to quantify the health and economic returns of emissions reduction strategies. This includes modeling how clean energy transitions, improved air quality, or reduced vehicle emissions could yield measurable health outcomes, such as reduced respiratory illnesses or heat-related deaths. Health-focused economic evaluations could help build public and political support for ambitious climate mitigation, especially when integrated into national planning and budgeting processes.
Collectively, these implications point to the need for research that is not only descriptive but also strategic, equity-oriented, and policy-relevant. Building a resilient climate-health research ecosystem in the Philippines will require sustained investment in interdisciplinary approaches, data infrastructure, and meaningful engagement with local actors.
5 Conclusion
This scoping review highlights the growing body of research on climate change and health in the Philippines, reflecting increasing recognition of climate-related health risks. Our findings show clear progress in previously underexplored thematic areas, such as mental health, gender-based vulnerability, and institutional adaptation. These mirror similar trends in other LMICs. At the same time, the persistent gaps in long-term climate-health surveillance, city- and community-level data, and health co-benefits research echo challenges reported globally, where localized, equity-focused studies remain limited. Importantly, this review reinforces the critical need to advance research that is both locally grounded but also strategically aligned with global research priorities. Expanding prospective cohort studies, integrating climate and health information systems, and producing high-resolution local data are essential next steps. In particular, generating context-specific evidence at subnational levels will better equip local government units (LGUs) to design targeted, data-informed adaptation and mitigation strategies– especially for highly vulnerable populations.
Finally, by mapping the evolution of climate-health research in the Philippines and linking it to global gaps and directions, this review offers a foundation for shaping the national climate-health research agenda. Strengthening domestic research systems and embedding public health evidence into climate policy will be vital to building a climate-resilient health system capable of responding to present and future climate risks.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CG: Formal analysis, Writing – original draft, Data curation, Visualization, Validation. MLC: Data curation, Validation, Investigation, Formal analysis, Writing – original draft. JRL: Methodology, Writing – review & editing, Data curation, Investigation. JL: Writing – review & editing, Resources. MVC: Investigation, Funding acquisition, Writing – review & editing, Project administration. MY: Project administration, Writing – review & editing, Funding acquisition, Supervision, Conceptualization, Resources. KA: Supervision, Conceptualization, Writing – review & editing, Validation, Project administration, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Gen AI was used in the creation of this manuscript. Generative AI tools (ChatGPT, OpenAI) were used to refine spelling, grammar, and phrasing, and to ensure compliance with word count requirements in the preparation of this manuscript. The authors reviewed and edited the content as needed and take full responsibility for the final version of the manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fclim.2025.1594793/full#supplementary-material
References
Agbay, V., Sanchez, P., Camus, D., Aquino-Cando, J., Barroga, E., and Velasco, A. (2023). Farmers’ adaptation of floods, droughts and disaster risk preparedness: the case of Angat, Bulacan, Philippines. J. Environ. Sci. Manag. 26, 79–91. doi: 10.47125/jesam/2023_sp1/08
Alahmad, B., Khraishah, H., Royé, D., Vicedo-Cabrera, A. M., Guo, Y. M., Papatheodorou, S. I., et al. (2022). Associations between extreme temperatures and cardiovascular cause-specific mortality: results from 27 countries. Circulation 147, 35–46. doi: 10.1161/CIRCULATIONAHA.122.061832
Araujo Navas, A. L., Osei, F., Leonardo, L. R., Soares Magalhães, R. J., and Stein, A. (2019). Modeling Schistosoma Japonicum infection under pure specification Bias: impact of environmental drivers of infection. Int. J. Environ. Res. Public Health 16:176. doi: 10.3390/ijerph16020176
Aruta, J. J. B. R., Crisostomo, K. A., Canlas, N. F., Almazan, J. U., and Peñaranda, G. (2022). Measurement and community antecedents of positive mental health among the survivors of typhoons Vamco and Goni during the COVID-19 crisis in the Philippines. Int J Disaster Risk Reduct. 72:102853. doi: 10.1016/j.ijdrr.2022.102853
Asian Development Bank (2024). Sector assessment (summary): Public sector management (disaster risk management) [internet]. Available online at: https://www.adb.org/sites/default/files/linked-documents/57309-001-ssa.pdf (Accessed February 6, 2025)
Ayeb-Karlsson, S., and Uy, N. (2022). Island stories: mapping the (im)mobility trends of slow onset environmental processes in three island groups of the Philippines. Humanit. Soc. Sci. Commun. 9, 11, 15. doi: 10.1057/s41599-022-01068-w
Baroy, N. G., and Wu, J. (2023). Post-disaster recovery and bargaining with patriarchy: a case study from Macapaya, Philippines. Int. J. Disaster Risk Reduct. 94:103833. doi: 10.1016/j.ijdrr.2023.103833
Bianco, G., Espinoza-Chávez, R. M., Ashigbie, P. G., Junio, H., Borhani, C., Miles-Richardson, S., et al. (2024). Projected impact of climate change on human health in low- and middle-income countries: a systematic review. BMJ Glob. Health 8:e015550. doi: 10.1136/bmjgh-2024-015550
Bond, G. D., Pasko, B., Solis-Perez, F., Sisneros, C. S., Gonzales, A. F., Bargo, A. J. B., et al. (2021). Remembering the super-typhoon: some, but not all, qualities of first-hand survivor memories of natural disaster are similar to near death experience and flashbulb memory accounts. Psychol. Rep. 124, 2119–2138. doi: 10.1177/0033294120957570
Burney, P., Patel, J., Minelli, C., Gnatiuc, L., Amaral, A. F. S., Kocabaş, A., et al. (2021). Prevalence and population-attributable risk for chronic airflow obstruction in a large multinational study. Am. J. Respir. Crit. Care Med. 203, 1353–1365. doi: 10.1164/rccm.202005-1990OC
Carvajal, T. M., Viacrusis, K. M., Hernandez, L. F. T., Ho, H. T., Amalin, D. M., and Watanabe, K. (2018). Machine learning methods reveal the temporal pattern of dengue incidence using meteorological factors in metropolitan Manila, Philippines. BMC Infect. Dis. 18:183. doi: 10.1186/s12879-018-3066-0
Chen, G., Guo, Y., Yue, X., Tong, S., Gasparrini, A., Bell, M. L., et al. (2021). Mortality risk attributable to wildfire-related PM2·5 pollution: a global time series study in 749 locations. Lancet Planet Health 5, E579–E587. doi: 10.1016/S2542-5196(21)00200-X
Chowdhury, S., Pozzer, A., Haines, A., Klingmüller, K., Münzel, T., Paasonen, P., et al. (2022). Global Health burden of ambient PM2.5 and the contribution of anthropogenic black carbon and organic aerosols. Environ. Int. 159:107020. doi: 10.1016/j.envint.2021.107020
Chua, P. L., Dorotan, M. M., Sigua, J. A., Estanislao, R. D., Hashizume, M., and Salazar, M. A. (2019). Scoping review of climate change and Health Research in the Philippines: A complementary tool in research agenda-setting. Int. J. Environ. Res. Public Health 16:2624. doi: 10.3390/ijerph16142624
Chua, P. L. C., Ng, C. F. S., Madaniyazi, L., Seposo, X., Salazar, M. A., Huber, V., et al. (2022). Projecting temperature-attributable mortality and hospital admissions due to enteric infections in the Philippines. Environ. Health Perspect. 130:027011. doi: 10.1289/EHP9324
Chua, P. L. C., Ng, C. F. S., Rivera, A. S., Salva, E. P., Salazar, M. A., Huber, V., et al. (2021). Association between ambient temperature and severe diarrhoea in the National Capital Region, Philippines. Int. J. Environ. Res. Public Health 18:8191. doi: 10.3390/ijerph18158191
Clamor, W. L., Lamberte, E., Demeterio, F. P., Tanhueco, R., and Regadio, C. (2020). The state of health in flood-prone areas in the Philippines: the case on the cities of Iligan and Cagayan De Oro. J. Hum. Behav. Soc. Environ. 30, 797–808. doi: 10.1080/10911359.2020.1757008
Clayton, S. (2020). Climate anxiety: psychological responses to climate change. J. Anxiety Disord. 74:102263. doi: 10.1016/j.janxdis.2020.102263
Clayton, S., Pihkala, P., Wray, B., and Marks, E. (2023). Psychological and emotional responses to climate change among young people worldwide: differences associated with gender, age, and country. Sustainability 15:5. doi: 10.3390/su15043540
Climate Fact Sheet: Philippines (2024). Red Cross Red Crescent Climate Centre. Available online at: https://www.climatecentre.org/publications/14130/the-philippines/rccc-country-profiles-philippines_2024_final/ (Accessed November 15, 2024)
CoastAdapt (2016). 15-117-NCCARFINFOGRAPHICS-01-UPLOADED-WEB(27Feb).Pdf [Internet]. Available online at: https://coastadapt.com.au/sites/default/files/infographics/15-117-NCCARFINFOGRAPHICS-01-UPLOADED-WEB%2827Feb%29.pdf (Accessed July 8, 2025)
Cruz, R., Aliño, P., Cabrera, O., David, C., David, L., Lansigan, F., et al. (2017). Philippine climate change assessment: impacts, vulnerabilities and adaptation [Internet]. The Oscar M. Lopez center for climate change adaptation and disaster risk management foundation, Inc. and climate change commission. Available online at: https://drive.google.com/file/d/1bPpHaNhuYRvTIoOcMlzVPU_q_aP4eMmQ/view (Accessed February 6, 2025)
Cueva, J. T. D., Ples, M. B., and Vitor, R. J. S. (2018). Relationship between chikungunya virus prevalence, rainfall, and urbanization in the Philippines. Natl. J. Physiol. Pharm. Pharmacol. 8, 977–982. doi: 10.5455/njppp.2018.8.0208204032018
Damgo, M., Bacus, M. G., Bernido, J. D. A., Evangelio, S. A., Ligue, K. D. B., Estaña, L. M. B., et al. (2023). Vulnerability assessment of emerging infectious diseases in Davao City, Southern Philippines: utilizing global predictors to develop localized interventions. Philipp. J. Sci. 152, 1555–1577. doi: 10.56899/152.05.04
Delina, L. L., Ludovice, N. P. P., Gaviola, J., and Cagoco-Guiam, R. (2023). Living with climate and state fragility in a “chaotic paradise:” securitizing livelihoods in the Philippines’ Cotabato River basin. Clim. Risk Manag. 42:100558. doi: 10.1016/j.crm.2023.100558
Deocaris, C. C., Diwa, R. R., and Tucio, P. B. (2022). Assessment of heavy metal levels in an urban river in the Philippines using an unconstrained ordination- and GIS-based approach: evidence of the return of past pollution after the 2013 typhoon Haiyan (Yolanda). H2Open J. 5, 412–423. doi: 10.2166/h2oj.2022.012
Dinh, N. T. T., Tran, J., and Hensher, M. (2024). Measuring and valuing the health co-benefits of climate change mitigation: a scoping review. Lancet Planet Health. 8, E402–E409. doi: 10.1016/S2542-5196(24)00095-0
Duante, C. A., Austria, R. E. G., Borigas, J. M. E., and Acuin, C. S. (2021). Assessment of socioeconomic and climate change-related factors to meeting recommended energy intake (REI) of Filipino households. Philipp. J. Sci. 150, 575–591. doi: 10.56899/150.03.01
Edwards, B., Gray, M., and Borja, J. (2021). The influence of natural disasters on violence, mental health, food insecurity, and stunting in the Philippines: findings from a nationally representative cohort. SSM Popul. Health 15:100825. doi: 10.1016/j.ssmph.2021.100825
Espada, R. (2018). Return period and Pareto analyses of 45 years of tropical cyclone data (1970-2014) in the Philippines. Appl. Geogr. 97, 228–247. doi: 10.1016/j.apgeog.2018.04.018
Estoque, R. C., Ooba, M., Seposo, X. T., Togawa, T., Hijioka, Y., Takahashi, K., et al. (2020). Heat health risk assessment in Philippine cities using remotely sensed data and social-ecological indicators. Nat. Commun. 11:1581. doi: 10.1038/s41467-020-15218-8
Francisco, M. E., Carvajal, T. M., Ryo, M., Nukazawa, K., Amalin, D. M., and Watanabe, K. (2021). Dengue disease dynamics are modulated by the combined influences of precipitation and landscape: a machine learning approach. Sci. Total Environ. 792:148406. doi: 10.1016/j.scitotenv.2021.148406
Frege, I. A., Befus, V., Bih, K. B., Fawwad, M., Ide, T., Kiefer, M., et al. (2024). Worldriskreport 2024 [Internet]. Bündnis Entwicklung Hilft. Available online at: https://weltrisikobericht.de/wp-content/uploads/2023/10/WRR_2023_english_online161023.pdf (Accessed February 6, 2025)
Gibb, C. (2022). The evacuation camp as paradoxical space for women. Polit. Geogr. 93:102546. doi: 10.1016/j.polgeo.2021.102546
Gil Cuesta, J., Van Loenhout, J. A. F., De Lara Banquesio, M. L., Mustaffa, M., and Guha-Sapir, D. (2020). Medical consultations after typhoon Haiyan in a Field hospital in the Philippines. Disaster Med. Public Health Prep. 14, 34–38. doi: 10.1017/dmp.2019.99
Gray, J., Lloyd, S., Healey, S., and Opdyke, A. (2022). Urban and rural patterns of typhoon mortality in the Philippines. Prog. Disaster Sci. 14:100234. doi: 10.1016/j.pdisas.2022.100234
He, L., Xue, B., Wang, B., Liu, C., De, P. D. G. R., Delclos, G. L., et al. (2022). Impact of high, low, and non-optimum temperatures on chronic kidney disease in a changing climate, 1990–2019: a global analysis. Environ. Res. 212:113172. doi: 10.1016/j.envres.2022.113172
Hickman, C., Marks, E., Pihkala, P., Clayton, S., Lewandowski, R. E., Mayall, E. E., et al. (2021). Climate anxiety in children and young people and their beliefs about government responses to climate change: a global survey. Lancet Planet Health 5, E863–E873. doi: 10.1016/S2542-5196(21)00278-3
Hong, L., Yan, M. M., Zhang, Y. Q., Wang, K., Wang, Y. Q., Luo, S. Q., et al. (2023). Global burden of cardiovascular disease attributable to high temperature in 204 countries and territories from 1990 to 2019. Biomed. Environ. Sci. 36, 222–230. doi: 10.3967/bes2023.025
Hu, P., Zhang, Q., Shi, P., Chen, B., and Fang, J. (2018). Flood-induced mortality across the globe: spatiotemporal pattern and influencing factors. Sci. Total Environ. 643, 171–182. doi: 10.1016/j.scitotenv.2018.06.197
Hua, Z. S., Wang, H., Chen, H., Hua, W. S., Ma, J., Dan, Z. D., et al. (2022). Global magnitude and long-term trend of ischemic heart disease burden attributed to household air pollution from solid fuels in 204 countries and territories, 1990-2019. Indoor Air 32:e12981. doi: 10.1111/ina.12981
Huang, W., Li, S., Vogt, T., Xu, R., Tong, S., Molina, T., et al. (2023). Global short-term mortality risk and burden associated with tropical cyclones from 1980 to 2019: a multi-country time-series study. Lancet Planet Health 7, E694–E705. doi: 10.1016/S2542-5196(23)00143-2
Iguchi, J. A., Seposo, X. T., and Honda, Y. (2018). Meteorological factors affecting dengue incidence in Davao, Philippines. BMC Public Health 18:629. doi: 10.1186/s12889-018-5532-4
Intergovernmental Panel On Climate Change (IPCC) (2023) Editor. Annex VII: glossary. In: Climate change 2021 – The physical science basis: Working group I contribution to the sixth assessment report of the intergovernmental panel on climate change [Internet]. Cambridge: Cambridge University Press; pp. 2215–2256. Available online at: https://www.cambridge.org/core/books/climate-change-2021-the-physical-science-basis/annex-vii-glossary/058768DADC00B52E2ED3381D0259B4E0 (Accessed February 6, 2025)
Izumi, T., and Shaw, R. (2022). A multi-country comparative analysis of the impact of COVID-19 and natural hazards in India, Japan, the Philippines, and USA. Int. J. Disaster Risk Reduct. 73:102899. doi: 10.1016/j.ijdrr.2022.102899
Jha, S. (2018) Natural disasters, public spending, and creative destruction: a case study of the Philippines. Available online at: https://www.adb.org/publications/natural-disasters-public-spending-and-creative-destruction-philippines (Accessed March 10, 2025)
Joquiño, C. M., Sarmiento, J. M. P., Estaña, L. M. B., Nañola, C. L. Jr., and Alviola, P. A. IV. (2021). Seasonal change, fishing revenues, and nutrient intakes of fishers’ children in Davao gulf, Philippines. Philipp. J. Sci. 150, 307–323. doi: 10.56899/150.01.28
Khine, M. M., and Langkulsen, U. (2023). The implications of climate change on health among vulnerable populations in South Africa: a systematic review. Int. J. Environ. Res. Public Health 20:3425. doi: 10.3390/ijerph20043425
Kim, Y., Kim, H., Gasparrini, A., Armstrong, B., Honda, Y., Chung, Y., et al. (2019). Suicide and ambient temperature: a multi-country Multi-City study. Environ. Health Perspect. 127:117007. doi: 10.1289/EHP4898
Krummenauer, L., Prahl, B. F., Costa, L., Holsten, A., Walther, C., and Kropp, J. P. (2019). Global drivers of minimum mortality temperatures in cities. Sci. Total Environ. 695:133560. doi: 10.1016/j.scitotenv.2019.07.366
Lawangen, A., and Roberts, J. K. (2023). Interactions between disaster risk reduction and intangible culture among indigenous communities in Benguet, Philippines. Int. J. Disaster Risk Reduct. 94:103801. doi: 10.1016/j.ijdrr.2023.103801
Lazo, L., and Ignacio, L. (2019) National Mental Health Research Agenda in the Philippines: 2019–2022 [Internet]. Philippine Council for Health Research and Development- Department of Science and Technology (PCHRD-DOST). Available online at: https://www.pchrd.dost.gov.ph/wp-content/uploads/2022/03/Annex-4.-National-Mental-Health-Research-Agenda-2019-2022.pdf (Accessed February 6, 2025)
Lee, J. Y., Kim, H., Gasparrini, A., Armstrong, B., Bell, M. L., Sera, F., et al. (2019). Predicted temperature-increase-induced Global Health burden and its regional variability. Environ. Int. 131:105027. doi: 10.1016/j.envint.2019.105027
Lu, J. L. Correlation of climate change indicators with health and environmental data in the Philippines. Acta Med. Philipp. [Internet]. (2022);56. Available online at: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/3976
Lu, H., Tan, Z., Liu, Z., Wang, L., Wang, Y., Suo, C., et al. (2021). Spatiotemporal trends in stroke burden and mortality attributable to household air pollution from solid fuels in 204 countries and territories from 1990 to 2019. Sci. Total Environ. 775:145839. doi: 10.1016/j.scitotenv.2021.145839
Mangada, L. L., and Cuaton, G. P. (2022). Typhoon Haiyan survivors at the resettlement sites: Covid-19 pandemic realities and challenges. Dialogues Health. 1:100005. doi: 10.1016/j.dialog.2022.100005
Matsushita, N., Ng, C. F. S., Kim, Y., Suzuki, M., Saito, N., Ariyoshi, K., et al. (2018). The non-linear and lagged short-term relationship between rainfall and leptospirosis and the intermediate role of floods in the Philippines. PLoS Negl. Trop. Dis. 12:E0006331. doi: 10.1371/journal.pntd.0006331
Miguel, C. B., Logrosa, G. T., Estaña, L. M. B., Tupas, G. D., Lachica, Z. P. T., and Alviola, P. A. IV. (2023). Risk factors associated with contracting COVID-19 infection in selected regions of Mindanao, Philippines. Philipp. J. Sci. 152, 837–848. doi: 10.56899/152.03.07
Milner, J., Hughes, R., Chowdhury, S., Picetti, R., Ghosh, R., Yeung, S., et al. (2023). Air pollution and child health impacts of decarbonization in 16 global cities: modelling study. Environ. Int. 175:107972. doi: 10.1016/j.envint.2023.107972
Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., Mcarthur, A., and Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 18:143. doi: 10.1186/s12874-018-0611-x
National Unified Health Research Agenda (NUHRA) 2017-2022 (2024). Philippine national health research system. Available online at: https://www.pchrd.dost.gov.ph/publications/nuhra-2017-2022/ (Accessed November 25, 2024)
Ngcamu, B. S. (2023). Climate change effects on vulnerable populations in the global south: a systematic review. Nat. Hazards 118, 977–991. doi: 10.1007/S11069-023-06070-2
Nguyen, H. T., and Rydstrom, H. (2018). Climate disaster, gender, and violence: men’s infliction of harm upon women in the Philippines and Vietnam. Womens Stud. Int. Forum 71, 56–62. doi: 10.1016/j.wsif.2018.09.001
Ogunbode, C., Doran, R., Hanss, D., Ojala, M., Salmela-Aro, K., Van Den Broek, K., et al. (2022). Climate anxiety, wellbeing and pro-environmental action: correlates of negative emotional responses to climate change in 32 countries. J. Environ. Psychol. 84:101887. doi: 10.1016/j.jenvp.2022.101887
Ogunbode, C., Pallesen, S., Böhm, G., Doran, R., Bhullar, N., Aquino, S., et al. (2023). Negative emotions about climate change are related to insomnia symptoms and mental health: cross-sectional evidence from 25 countries. Curr. Psychol. 42, 845–854. doi: 10.1007/s12144-021-01385-4
Olmoguez, I., Catindig, M., Amongos, M., and Lazan, F. (2019). Developing a dengue forecasting model: a case study in Iligan City. Int. J. Adv. Comput. Sci. Appl. 10, 281–286. doi: 10.14569/IJACSA.2019.0100936
Orderud, H. (2024). Storms and infant mortality in the Philippines. Int. J. Disaster Risk Reduct. 100:104188. doi: 10.1016/j.ijdrr.2023.104188
Pabroa, P. C. B., Racho, J. M. D., Jagonoy, A. M., Valdez, J. D. G., VII, A. T. B., Yee, J. R., et al. (2022). Characterization, source apportionment and associated health risk assessment of Respirable air particulates in metro Manila, Philippines. Atmos. Pollut. Res. 13:101379. doi: 10.1016/j.apr.2022.101379
Pacoma, A. J. U., and Delda, J. S. (2019). Social capital in the post-Haiyan setting: the role of local and translocal ties in building household resilience. Int. J. Disaster Risk Reduct. 40:101250. doi: 10.1016/j.ijdrr.2019.101250
Pasin, C., Halloran, M. E., Gilbert, P. B., Langevin, E., Ochiai, R. L., Pitisuttithum, P., et al. (2018). Periods of high dengue transmission defined by rainfall do not impact efficacy of dengue vaccine in regions of endemic disease. PLoS One 13:E0207878. doi: 10.1371/journal.pone.0207878
Peters, M. D., Godfrey, C. M., Khalil, H., McInerney, P., Parker, D., and Soares, C. B. JBI Evidence Implementation [Internet]. (2015). Available online at: https://journals.lww.com/ijebh/fulltext/2015/09000/guidance_for_conducting_systematic_scoping_reviews.5.aspx (Accessed July 5, 2025)
Pineda-Cortel, M. R. B., Clemente, B. M., and Nga, P. T. T. (2019). Modeling and predicting dengue fever cases in key regions of the Philippines using remote sensing data. Asian Pac. J. Trop. Med. 12:60. doi: 10.4103/1995-7645.250838
PRISMA Statement [Internet]. (2018). Scoping. Available online at: https://www.prisma-statement.org/scoping (Accessed July 7, 2025)
Ramalho, J. (2020). Engendering disaster risk management and resilience-building: the significance of the everyday in evaluations of the exceptional. Int. J. Disaster Risk Reduct. 50:101830. doi: 10.1016/j.ijdrr.2020.101830
Reyes, M. E. S., Carmen, B. P. B., Luminarias, M. E. P., Mangulabnan, S. A. N. B., and Ogunbode, C. A. (2023). An investigation into the relationship between climate change anxiety and mental health among gen Z Filipinos. Curr. Psychol. 42, 7448–7456. doi: 10.1007/s12144-021-02099-3
Rith, M., Fillone, A. M., and Biona, J. B. M. M. (2020). Energy and environmental benefits and policy implications for private passenger vehicles in an emerging Metropolis of Southeast Asia – a case study of metro Manila. Appl. Energy 275:115240. doi: 10.1016/j.apenergy.2020.115240
Romanello, M., Di Napoli, C., Green, C., Kennard, H., Lampard, P., Scamman, D., et al. (2023). The 2023 report of the lancet countdown on health and climate change: the imperative for a health-centred response in a world facing irreversible harms. Lancet Lond Engl. 402, 2346–2394. doi: 10.1016/S0140-6736(23)01859-7
Romanello, M., McGushin, A., Di Napoli, C., Drummond, P., Hughes, N., Jamart, L., et al. (2021). The 2021 report of the lancet countdown on health and climate change: code red for a healthy future. Lancet 398, 1619–1662. doi: 10.1016/S0140-6736(21)01787-6
Samonte, P., and Djalante, R. (2024). Postdisaster relocation and its impacts on family dynamics: a case study of typhoon Ketsana relocation in the Philippines. Int. J. Disaster Resil. Built Environ. 15, 158–173. doi: 10.1108/IJDRBE-02-2022-0022
Sattler, D. N., Graham, J. M., Whippy, A., Atienza, R., and Johnson, J. (2023). Developing a climate change risk perception model in the Philippines and Fiji: posttraumatic growth plays central role. Int. J. Environ. Res. Public Health 20:1518. doi: 10.3390/ijerph20021518
Seposo, X., Valenzuela, S., and Apostol, G. L. (2023). Socio-economic factors and its influence on the association between temperature and dengue incidence in 61 provinces of the Philippines, 2010-2019. PLoS Negl. Trop. Dis. 17:E0011700. doi: 10.1371/journal.pntd.0011700
Smith, K., Woodward, A., Campbell-Lendrum, D., Chadee, D., Honda, Y., Liu, Q., et al. (2014). “Human health: impacts, adaptation, and co-benefits” in Climate change 2014: Impacts, adaptation, and vulnerability part a: Global and sectoral aspects contribution of working group II to the fifth assessment report of the intergovernmental panel on climate change. eds. C. B. Field, V. Barros, and D. J. Dokken (Cambridge UK: Cambridge University Press), 709–754.
Supreme Court E-Library. Republic act no. 11036 – an act establishing a national mental health policy for the purpose of enhancing the delivery of integrated mental health services (2018). Promoting and protecting the rights of persons UTILIZING psychiatric, neurologic and psychosocial health services, appropriating funds therefor. And for other purposes [Internet]. Available online at: https://elibrary.judiciary.gov.ph/thebookshelf/showdocs/2/83255 (Accessed July 5, 2025)
Sylwanowicz, L., Schreiber, M., Anderson, C., Gundran, C. P. D., Santamaria, E., and Lopez, J. C. F. (2018). Rapid triage of mental health risk in emergency medical workers: findings from Typhoon Haiyan. Disaster Med. Public Health Prep. 12, 19–22. doi: 10.1017/dmp.2017.37
Tabudlo, J. B., Joven, G. F., and Joven, M. F. (2022). Uncovering adaptive mechanisms and resilience among older adults: a qualitative study on the mental health impacts of temperature variations. Belitung Nurs J. 8, 333–339. doi: 10.33546/bnj.2148
Tanay, M. A., Quiambao-Udan, J., Soriano, O., Aquino, G., and Valera, P. M. (2023). Filipino nurses’ experiences and perceptions of the impact of climate change on healthcare delivery and cancer care in the Philippines: a qualitative exploratory survey. Ecancermedicalscience. 17:1622. doi: 10.3332/ecancer.2023.1622
Tanyag, M. (2018). Resilience, female altruism, and bodily autonomy: disaster-induced displacement in post-Haiyan Philippines. Signs 43, 563–585. doi: 10.1086/695318
Thomas, J., and Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 8:45. doi: 10.1186/1471-2288-8-45
Tsheten, T., Alene, K. A., Restrepo, A. C., Kelly, M., Lau, C., Clements, A. C. A., et al. (2024). Risk mapping and socio-ecological drivers of soil-transmitted helminth infections in the Philippines: a spatial modelling study. Lancet Reg Health West Pac. 43:100974. doi: 10.1016/j.lanwpc.2023.100974
WHO (2024). DOH, NNC, WHO, and development partners call for actions to curb obesity in the Philippines [internet]. Available online at: https://www.who.int/philippines/news/detail/05-03-2024-doh--nnc--who--and-development-partners-call-for-actions-to-curb-obesity-in-the-philippines (Accessed November 27, 2024)
Williams, L., Arguillas, M. J. B., and Arguillas, F. (2020). Major storms, rising tides, and wet feet: adapting to flood risk in the Philippines. Int. J. Disaster Risk Reduct. 50:101810. doi: 10.1016/j.ijdrr.2020.101810
World Health Organization. Climate change [internet] (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (Accessed July 7, 2025)
World Meteorological Organization (2021). Updated 30-year reference period reflects changing climate. Available online at: https://wmo.int/media/news/updated-30-year-reference-period-reflects-changing-climate (Accessed November 13, 2024)
Xu, Z., Bambrick, H., Yakob, L., Devine, G., Frentiu, F. D., Villanueva Salazar, F., et al. (2020). High relative humidity might trigger the occurrence of the second seasonal peak of dengue in the Philippines. Sci. Total Environ. 708:134849. doi: 10.1016/j.scitotenv.2019.134849
Yu, A. K., Ytienza, S. I., Yu, A. M., Yu, V. C., Wangkay, K. A., Wong, M. A., et al. Correlation between incidence of dengue and climatic factors in the Philippines: an ecological study. Health Sci. J. [Internet]. (2020);9. Available online at: https://www.herdin.ph/index.php/component/herdin/?view=research&cid=75210
Glossary
ASDR - Age-Standardized Death Rate
ASMR - Age-Standardized Mortality Rate
ARI - Acute Respiratory Infection
BC - Black Carbon
°C - Degrees Celsius
CDO - Cagayan de Oro
CI - Confidence Interval
CO₂ - Carbon Dioxide
COVID-19 - Coronavirus Disease 2019
DALY - Disability-Adjusted Life Year
DOH - Department of Health (Philippines)
DRRM - Disaster Risk Reduction and Management
ENSO - El Niño–Southern Oscillation
GHG - Greenhouse Gas
GIZ - Deutsche Gesellschaft für Internationale Zusammenarbeit
HAP - Household Air Pollution
HERDIN - Health Research and Development Information Network
HIV/AIDS - Human Immunodeficiency Virus / Acquired Immunodeficiency Syndrome
kcal/day - Kilocalories per Day
LGUs - Local Government Units
LMICs - Low- and Middle-Income Countries
mm - Millimeter
NCDs - Non-Communicable Diseases
NCR - National Capital Region
NIEHS - National Institute of Environmental Health Sciences
NNS - National Nutrition Survey
NO - Nitrogen Monoxide
NO₂ - Nitrogen Dioxide
NUHRA - National Unified Health Research Agenda
PAGASA - Philippine Atmospheric, Geophysical and Astronomical Services Administration
PDRI - Philippine Dietary Reference Intakes
PHRR - Philippine Health Research Registry
PM - Particulate Matter
PM₂.₅ - Fine Particulate Matter (≤2.5 micrometers)
PRISMA - Preferred Reporting Items for Systematic Reviews and Meta-Analyses
PTSD - Post-Traumatic Stress Disorder
RCP - Representative Concentration Pathway
REI - Recommended Energy Intake
RR - Relative Risk
SNS - Social Networking Services
STDs - Sexually Transmitted Diseases
TV - Television
UP - University of the Philippines
UPMREB - University of the Philippines Manila Research Ethics Board
USD - United States Dollar
WASH - Water, Sanitation, and Hygiene
WHO - World Health Organization
Keywords: climate change, health, Philippines, scoping review, research agenda-setting
Citation: De Guzman C, Cabaero ML, Lo JR, Loro J, Crisostomo MV, Ylade M and Agrupis KA (2025) Recent trends in research on the health impacts of climate change in the Philippines (2018–2023): a scoping review. Front. Clim. 7:1594793. doi: 10.3389/fclim.2025.1594793
Edited by:
Louis Nyahunda, University of Venda, South AfricaReviewed by:
Meghnath Dhimal, Nepal Health Research Council, NepalEsteban Ortiz-Prado, University of the Americas, Ecuador
Taslim Uddin, Bangabandhu Sheikh Mujib Medical University (BSMMU), Bangladesh
Priscila Neves Silva, Oswaldo Cruz Foundation (Fiocruz), Brazil
Copyright © 2025 De Guzman, Cabaero, Lo, Loro, Crisostomo, Ylade and Agrupis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kristal An Agrupis, a2NhZ3J1cGlzQHVwLmVkdS5waA==
†These authors have contributed equally to this work and share first authorship
 Clarissa De Guzman
Clarissa De Guzman Megan Lorenza Cabaero
Megan Lorenza Cabaero Jude Raphael Lo
Jude Raphael Lo Jimmy Loro
Jimmy Loro Maria Vinna Crisostomo
Maria Vinna Crisostomo Michelle Ylade
Michelle Ylade Kristal An Agrupis
Kristal An Agrupis