- 1Department of Health Science, UniCamillus-Saint Camillus International Medical University, Rome, Italy
- 2Department of Oral and Maxillofacial Sciences, Sapienza University of Rome, Rome, Italy
Objective: The aim of this retrospective study was to assess the soft tissues changes resulting from Class II treatment with functional appliances (Twin Block vs. Mandibular Advancement), when compared to an untreated Class II control group.
Materials and methods: The records of 45 Class II patients who underwent treatment with Twin Block (TB group: n = 22; mean age: 11.3 ± 1.4 years) or Mandibular Advancement (MA group: n = 23; mean age: 11.2 ± 1.3 years) were analyzed in comparison with a control sample of untreated Class II subjects (Untreated Control group = 24; mean age: 11.2 ± 1.1 years). The data were collected before treatment (T1) and at the conclusion of the functional therapy phase (T2). Cephalometric modifications were assessed among the three groups using ANOVA and Tukey's post hoc tests.
Results: Significant improvements were observed for mandibular sulcus and the facial profile angle in the treated groups compared to the Untreated control group (facial profile angle: TB group: +5.67°; MA group: +6.34°; mandibular sulcus: TB group: +10.0°; MA group: 11.77°). The distance of Pogonion (Pg) to the True Vertical Line (TVL) exhibited significant differences among the three groups, with a more pronounced advancement of the soft tissue pogonion in the TB group (TVL-Pg': TB group: +3 mm; MA group: +0.9 mm; untreated control group: −1.6 mm).
Conclusions: Treatment with removable functional devices (TB or MA) during puberty produced beneficial effects on the soft tissue profile. Both treated groups demonstrated a significant improvement in the Class II convex profile, accompanied by a less evident mandibular sulcus.
1 Introduction
Class II dento-skeletal malocclusion is often associated to a backward-positioned mandible (1–3). In growing patients, functional therapy encourages mandibular growth by repositioning the lower jaw forward, allowing the condyles to settle in a more anterior and inferior position within the glenoid fossa (2–6).
A key therapeutic goal of all functional appliances is to enhance facial aesthetics by decreasing the convexity of the profile while improving lip projection and closure (5).
Various functional devices, including Andersen's activator, Bionator, Frankel, Sanders, and Twin Block (TB) appliances, have been specifically developed to promote mandibular advancement and facilitate its forward repositioning, aiming to correct Class II skeletal imbalances (7).
The dentoskeletal effects of functional appliances have been widely studied in the literature, as well as their impact on soft tissues. Twin Block appliance demonstrated significant improvements in facial profile aesthetics and mandibular advancement when applied in patients at the pubertal growth peak (3, 8–13). In particular, Baysal et al. evaluated 25 patients (mean age: 12.9 ± 1.4 years) treated with the Twin Block appliance and reported a significant reduction in facial convexity and advancement of the lower lip, improving soft tissue profile (12). In addition, Varlık et al., in a prospective study on 28 growing patients (mean age: 12.2 ± 1.3 years), highlighted a significant increase in soft tissue pogonion projection and a reduction in upper lip protrusion following Twin Block therapy (13).
In recent years, with the spread of clear aligner therapy, Align Technology (San Jose, CA, USA) introduced the Mandibular Advancement (MA) feature. Precision wings built into the aligners, gradually posture the mandible forward.
Despite numerous studies evaluating the skeletal and dental effects of MA therapy (11–18), research on its impact on soft tissue changes remains limited (18–21).
Sabouni et al. reported a significant decrease in facial convexity and a marked increase in the nasolabial angle among 32 patients with an average age of 13 years old treated with the MA appliance, while changes in the chin angle were not significant (18).
In a retrospective study by Sadek et al. involving 15 growing patients (mean age: 11.6 ± 2.35 years), a significant reduction in both facial convexity and upper lip protrusion was observed (19).
In addition, Goje et al., examined 20 patients with a mean age of 13 years treated with the MA appliance and highlighted a significant improvement in the nasolabial angle and a not significant reduction of the chin (20).
However, only a recent study (21) directly compared the dentoskeletal and soft tissue changes in a group of 50 subjects (mean age: 11.98 ± 2.18 years) treated with MA vs. an untreated control group of patients with Class II malocclusion. The findings highlighted significant improvements in mandibular positioning and overall skeletal and dental changes, which contributed to better facial profiles and soft tissue adaptation.
To our best knowledge no studies have analyzed the esthetic outcomes comparing the single-step advancement of the TB appliance and the gradual advancement of the MA with clear aligners.
Therefore, the present retrospective study aimed to analyze the soft tissue modifications induced by Class II treatment with functional therapy (TB vs. MA) compared to an untreated Class II control group.
2 Materials and methods
This retrospective controlled study received approval from the Ethical Committee of the Hospital of Rome “Tor Vergata” (protocol no. 48/23). Written informed consent was obtained from all participants' parents.
The sample size was calculated considering an effect size for the primary outcome variable Facial profile angle (G'-SubN-Pg') of 1.0, an alpha value of 0.05 and a power of 0.80. At least 15 subjects were required for each group.
Two groups of subjects with a Class II Malocclusion were selected from files of the Departments of Orthodontics at the Hospital of Rome “Tor Vergata” between January 1, 2019, and January 1, 2022. The first group (TB group) consisted of 22 patients (14 males, 8 females; mean age: 11.3 ± 1.4 years) treated with Twin Block appliance (Figure 1).
The second group (MA group) was composed of 23 patients (11 males, 12 females; mean age: 11.2 ± 1.3 years) treated with clear aligners with MA feature appliance (Figure 2).
Inclusion criteria consisted of: Caucasian ethnicity, overjet greater than 5 mm, full Class II or end-to-end molar relationships, ANB angle greater than 4°, improvement in facial profile when the lower jaw was postured in a forward position and circumpubertal stage (stage 2 and 3) according to the Cervical Vertebral Maturation (CVM) at the start of treatment (22). CVM staging was performed by an expert examiner (RL).
Subjects with facial asymmetry, craniofacial syndromes, previous orthodontic treatment were excluded. No permanent teeth were congenitally missing or extracted before or during treatment.
Lateral cephalograms were available: before treatment (T1) and at the end of functional therapy (T2), before orthodontic therapy with both fixed appliance or the continuing phase with additional aligners. Functional treatment was discontinued after the achievement of Class I molar relationship.
24 untreated subjects with Class II division 1 malocclusion (Untreated Control group) were selected from the American Association of Orthodontists Foundation (AAOF) Craniofacial Growth Legacy Collection (http://www.aaoflegacycollection.org, Bolton–Brush Growth Study, Michigan Growth Study, Denver Growth Study, Oregon Growth Study, and Iowa Growth Study) and were matched with treated groups for age, skeletal development, dentition development, skeletal features and observation time intervals. The inclusion criteria of the control group were the same as those of the treated samples.
2.1 Cephalometric analysis
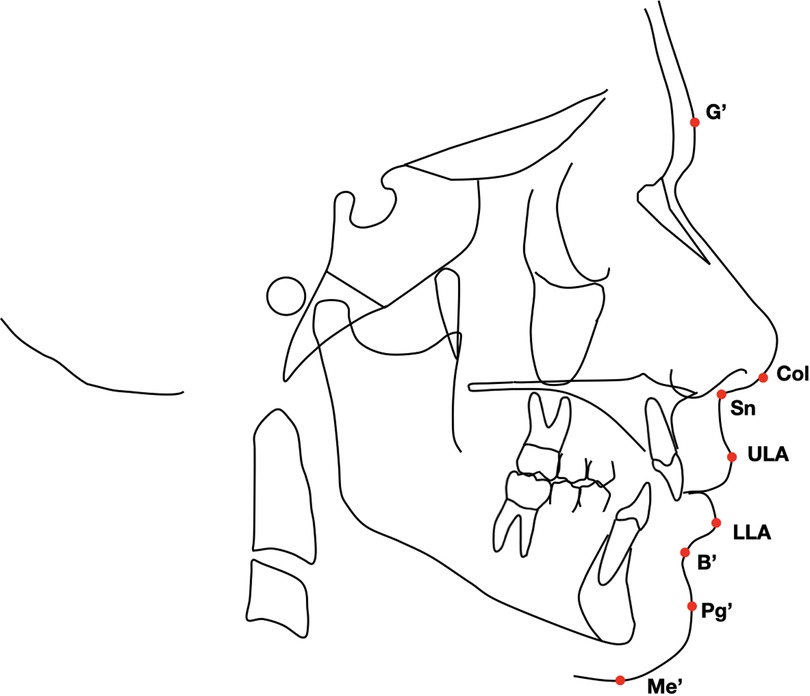
Lateral cephalograms for both treated and untreated subjects were scanned at the same resolution (150 dpi). A customized digitization regimen and cephalometric analysis provided by Viewbox (version 3.0; dHAL Software, Kifissia, Greece) were used for all cephalograms selected. The customized soft tissue cephalometric analysis (Figure 3), containing measurements from the analysis of Bergman (23), generated six variables, three angular and two linear, and one percentage value. In addition to these soft tissue cephalometric traits, the distance from the soft tissue pogonion to the true vertical line (TVL) was measured using Arnett's analysis (24).
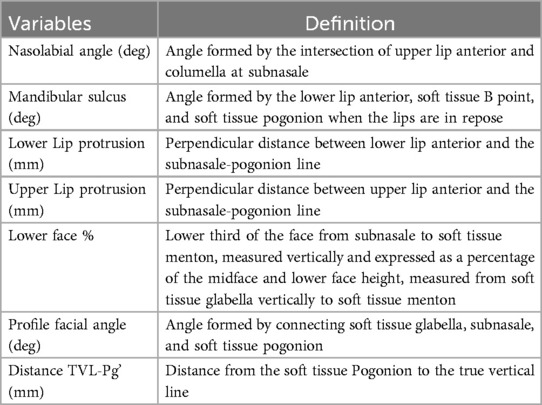
All the soft tissue cephalometric measurements are summarized in Table 1.
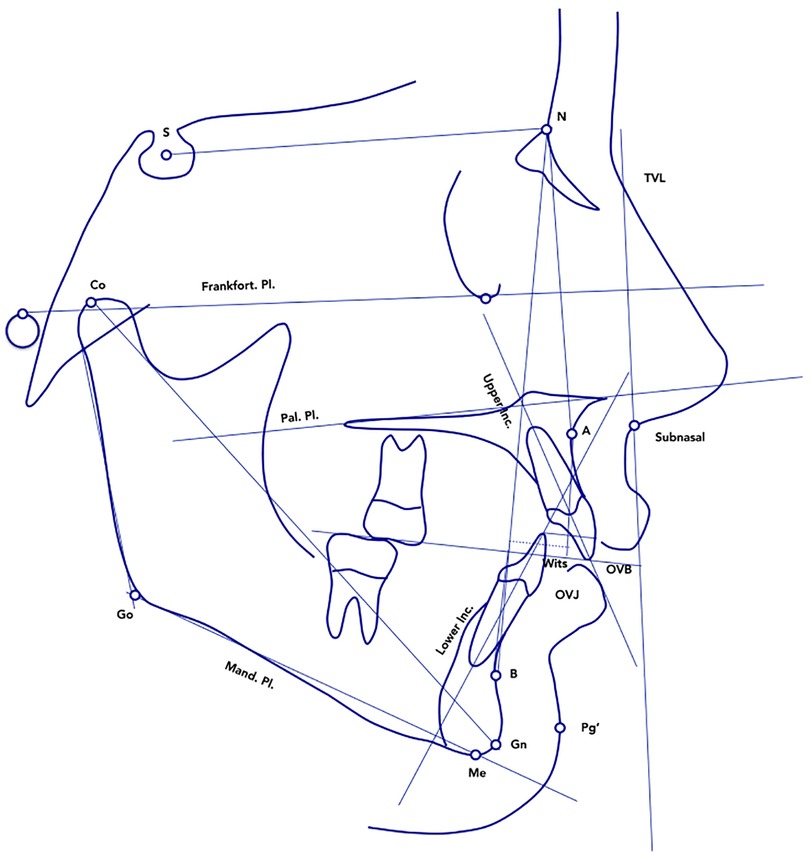
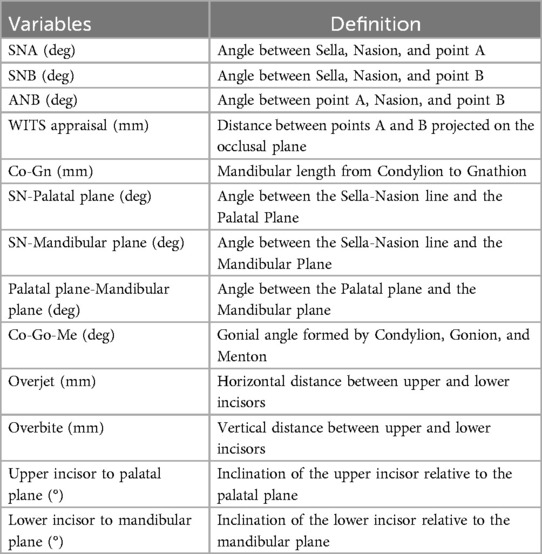
Additional cephalometric variables were digitized for each patient at T1 and T2 in order to provide data on the dento-skeletal correction (Figure 4 and Table 2).
All lateral cephalograms at T1 and T2 were standardized to life size (0% enlargement).
2.2 Statistical analysis
The Chi-square test of independence was used to assess differences in gender distribution between the three groups.
Descriptive statistics and intergroup comparisons of cephalometric changes were performed using ANOVA and Tukey's post hoc tests at T1 (starting forms) and for the T2–T1 changes. When the variables were not normally distributed (Shapiro–Wilk test), Kruskal–Wallis with Dunn's post hoc tests were performed (25).
2.3 Method error
To determinate the method accuracy, one trained examiner (LL) with an experience of 4 years performed all the measurements on lateral cephalograms and 20 radiographs were retraced after an interval of approximately 2 weeks. Intra-observer reproducibility was assessed with the intraclass correlation coefficient (ICC), while for the assessment of the random error the method of moments' estimator (MME) was applied (26).
3 Results
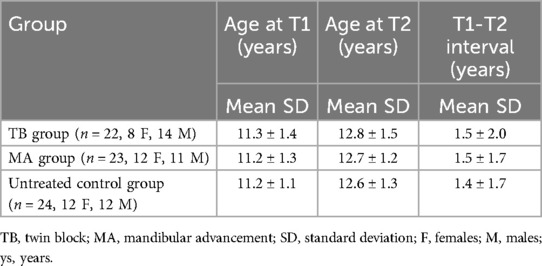
The demographic data of the treated and the control groups are reported in Table 3.
No significant between-group differences were found either for chronologic age at T1 (P = 0.492), chronologic age at T2 (P = 0.896), chronologic age at T2-T1 interval (P = 0.545) and for gender distribution (P = 0.789). The chi-square test showed no statistically significant difference in gender distribution within the examined group (p = 0.49).
The intra-observer reproducibility, evaluated with the ICCs, indicated a high level of intraobserver agreement (ICCs varied between 0.897 and 0.999). As for the measurement errors they varied from 0.2° to 0.4° for the angular measurements and from 0.4 to 0.5 mm for the linear measurements.
No significant between-group differences were found in any of the variables at T1 (Table 4).
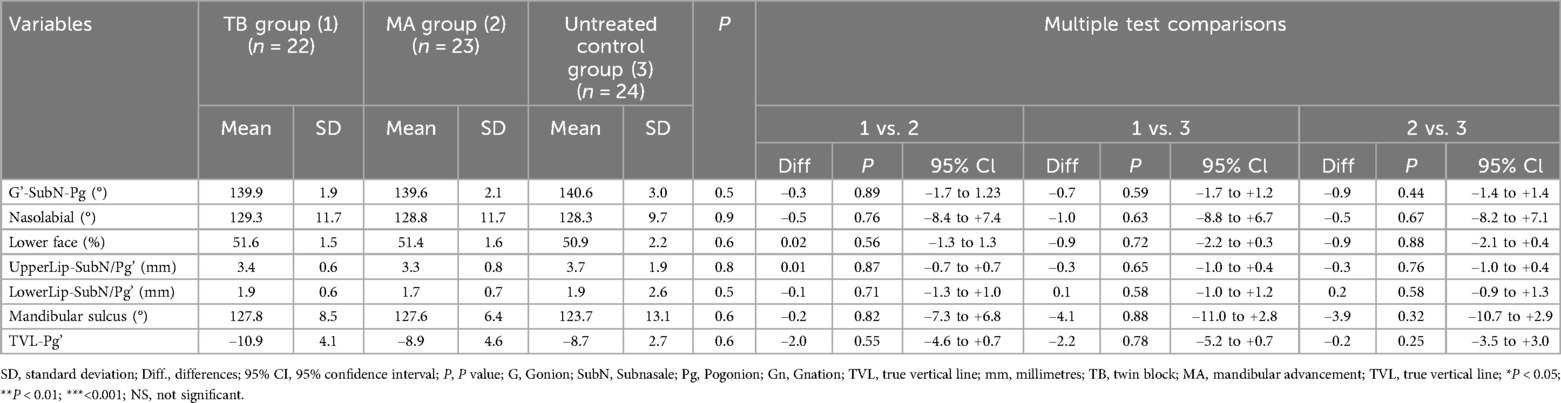
Table 4. Descriptive statistics and statistical comparisons of baseline characteristics. Analysis of variance (ANOVA) with Tukey's post hoc tests or ANOVA on ranks with Dunn's post hoc tests.
The statistical comparisons of the T2–T1 changes between TB, MA and control groups (Table 5) showed significant modifications produced by functional therapy.
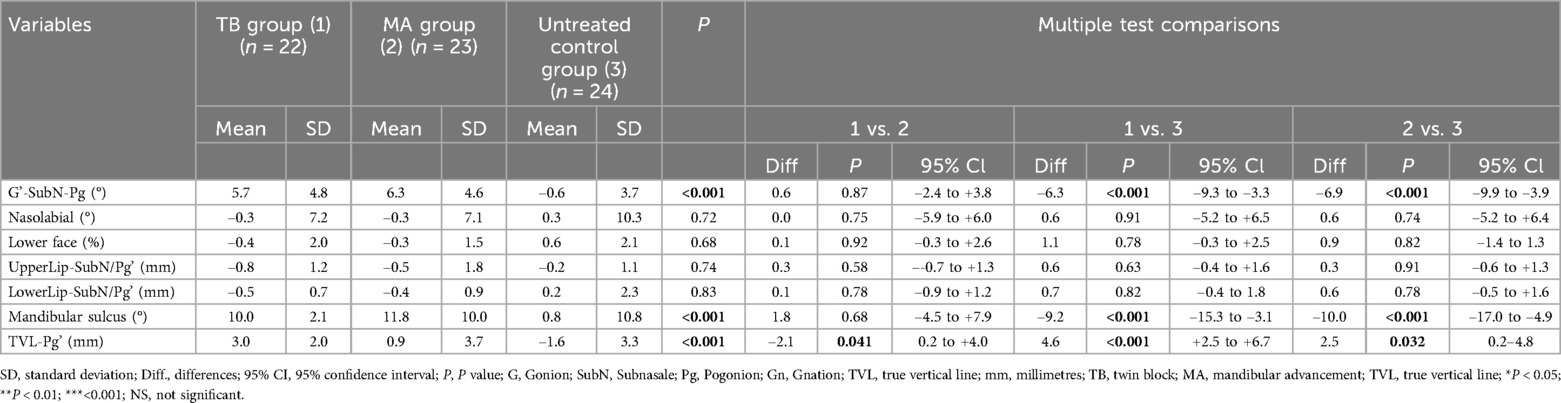
Table 5. Descriptive statistics and statistical comparisons of the T2–T1 changes. Analysis of variance (ANOVA) with Tukey's post hoc tests or ANOVA on ranks with Dunn's post hoc tests.
Both the TB and MA groups showed a significant and clinically relevant increase in the profile facial angle (G'-SubN-Pg') compared to the untreated control group (TB: +5.7°; MA: +6.3°; Untreated Control group: −0.6°). Additionally, for the mandibular sulcus parameter, the TB and MA groups demonstrated significant increases (TB: +10°; MA: +11.8°) compared to the control group (Untreated Control group: 0.8°).
The increase in the distance of Pg to TVL from T1 to T2 showed a statistically significant difference across the three groups, with a greater advancement of the soft tissue pogonion in the TB group compared to both the MA group and the Untreated Control group (TB group: +3 ± 2 mm; MA group: +0.9 ± 3.7 mm; Untreated Control group: −1.6 ± 3.3 mm).
During the T2–T1 interval, the TB and MA groups showed significant dento-skeletal changes compared to controls (Supplementary Table S1), including a reduction in the ANB angle (TB: −1.5°; MA: −1.5°; Untreated Control group: +0.2°) and an increase in Co-Gn values (TB: +8.4 mm; MA: +8.3 mm). Both groups also demonstrated a greater reduction in the palatal plane-mandibular plane angle and improvements in overjet and vertical overbite values.
4 Discussion
Functional therapy affects skeletal and dentoalveolar structures as well as soft tissue organization, leading to a more balanced and aesthetically pleasing facial profile in relation to craniofacial structures (26–30).
The present study aimed to assess the impact of functional therapy (TB vs. MA) on the soft tissue facial profile in growing Class II patients, when compared with untreated Class II control group.
One of the main strengths of our study was the inclusion of a control group. This allowed for a direct comparison of the outcomes observed in the treatment group against a baseline, enhancing the validity of our results on soft tissue changes. The control group was carefully selected to minimize confounding variables, such as age, sex, and initial craniofacial morphology, ensuring that the observed differences can be attributed primarily to the treatment.
As reported by many authors treatment with removable functional appliances produced significant skeletal long-term changes when it begins at puberty (3, 31). Therefore, one of the inclusion criteria for subject selection was the circumpubertal stage of cervical vertebral maturation at the start of treatment (CVM2-CVM3). Moreover, the study compared two removable functional appliances, TB and MA, which are based on the same mechanism of the inclined planes that posture the jaw to an advanced forced position.
Despite soft tissue changes induced by TB have been evaluated in the literature (12, 13, 31–35), data concerning aesthetic improvements and soft tissue modifications produced by MA are limited.
Overall, T2–T1 changes showed a significantly more harmonious facial profile in treated groups (TB and MA) compared to the untreated control group.
Profile facial angle significantly increased in treated groups with respect to the control group (TB group = +5.67° ± 4.76°; MA group: +6.34° ± 4.58°; untreated control group: −0.64° ± 3.67°). Our results are consistent with those reported in the literature, which highlighted a reduction in facial convexity in patients treated with MA (18, 21).
For the mandibular sulcus parameter, statistically significant differences were observed in the TB and MA groups compared to the untreated control group, with an increase of 10° in the TB group and 11.77° in the MA group. The straightening of the mandibular sulcus appears to be primarily a result of mandibular advancement.
To the best of our knowledge, no previous study has specifically analyzed this parameter. Our findings also revealed a statistically significant difference among the TB, MA, and control groups concerning chin advancement, assessed by measuring the distance of the soft tissue pogonion from the true vertical line (TVL). In this study, the TB appliance appeared to be more effective in promoting chin advancement and, consequently, in improving the facial profile. This result could be attributed to the different mandibular advancement mechanisms applied, specifically the one-step advancement with the TB appliance vs. the progressive advancement with the MA feature.
In the literature there are very conflicting opinions on which is the most effective advancement protocol. Nowadays, there is greater scientific evidence in favor of incremental mandibular advancement in terms of mandibular response and increase in mandibular length (15). It is interesting to note that on the basis of our results, the different advancement protocol applied by these two devices did not produce differences in the improvement of soft tissues.
All the profile modifications were mainly determined during the functional active treatment phase and were supported by dento-skeletal changes, as detailed in the Supplementary Table S1.
The results obtained should be supported and corroborated by further investigations to be conducted by means of long-term observation. The limitations of the present study are the use of historical controls, and the relatively small sample size. Ideally, a contemporary control sample should have been used because it has been shown that our face and its changes are influenced by secular trends (36). However, it would be unethical to leave a Class II sample without any treatment in the long term. Despite these limitations, the study design allowed for meaningful comparisons, and the sample size was justified through statistical computation to achieve sufficient power.
5 Conclusions
Treatment with removable functional appliances (TB or MA) at puberty induced a reduction in the convexity of the soft tissue facial profile. All modifications observed were mainly sustained by significant sagittal skeletal changes. In the treated groups, there was a notable improvement in the normalization of the Class II convex profile, accompanied by a more harmonious lip position, largely attributed to the straightening of the mandibular sulcus. Based on these results, both TB and MA appliances can be considered effective options for improving the soft tissue profile in growing Class II patients with mandibular deficiency. However, it remains essential to carefully assess the optimal treatment timing to maximize treatment effectiveness and stability.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
LL: Data curation, Investigation, Resources, Software, Writing – original draft. CP: Conceptualization, Supervision, Validation, Visualization, Writing – original draft. FD: Methodology, Writing – original draft. FG: Methodology, Resources, Writing – review & editing. SL: Investigation, Software, Writing – review & editing. EC: Validation, Writing – original draft. PC: Project administration, Validation, Writing – review & editing. RL: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors report a funding relationship between themselves and Align Technology. However, Align Technology had no role in the design of the study, in the collection, analyses or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdmed.2025.1581032/full#supplementary-material
References
1. McNamara JA Jr. Components of class II malocclusion in children 8–10 years of age. The Angle Orthod. (1981) 51:177–202. doi: 10.1043/0003-3219(1981)051%3C0177:COCIMI%3E2.0.CO;2
2. Gazzani F, Ruellas ACDO, Faltin K, Franchi L, Cozza P, Bigliazzi R, et al. 3D comparison of mandibular response to functional appliances: Balters Bionator versus sander bite jumping. BioMed Res Int. (2018) 2018(1):2568235. doi: 10.1155/2018/2568235
3. Franchi L, Pavoni C, Faltin K Jr, McNamara JA Jr, Cozza P. Long-term skeletal and dental effects and treatment timing for functional appliances in class II malocclusion. Angle Orthod. (2013) 83(2):334–40. doi: 10.2319/052912-450.1
4. McNamara JA Jr, Bookstein FL, Shaughnessy TG. Skeletal and dental changes following functional regulator therapy on class II patients. Am J Orthod. (1985) 88(2):91–110. doi: 10.1016/0002-9416(85)90233-7
5. Lione R, Brunelli V, Franchi L, Pavoni C, Quiroga Souki B, Cozza P. Mandibular response after rapid maxillary expansion in class II growing patients: a pilot randomized controlled trial. Prog Orthod. (2017) 18:1–7. doi: 10.1186/s40510-017-0189-6
6. Lione R, Franchi L, Laganà G, Cozza P. Effects of cervical headgear and pendulum appliance on vertical dimension in growing subjects: a retrospective controlled clinical trial. Eur J Orthod. (2015) 37(3):338–44. doi: 10.1093/ejo/cju061
7. Franchi L, Pavoni C, Faltin K, Bigliazzi R, Gazzani F, Cozza P. Thin-plate spline analysis of mandibular shape changes induced by functional appliances in class II malocclusion a long-term evaluation. J Orofac Orthop. (2016) 77(5):325–33. doi: 10.1007/s00056-016-0041-5
8. Lione R, Balboni A, Di Fazio V, Pavoni C, Cozza P. Effects of pendulum appliance versus clear aligners in the vertical dimension during class II malocclusion treatment: a randomized prospective clinical trial. BMC Oral Health. (2022) 22(1):441. doi: 10.1186/s12903-022-02483-w
9. Perinetti G, Primožič J, Franchi L, Contardo L. Treatment effects of removable functional appliances in pre-pubertal and pubertal class II patients: a systematic review and meta-analysis of controlled studies. PLoS One. (2015) 10:e0141198. doi: 10.1371/journal.pone.0141198
10. Idris G, Hajeer MY, Al-Jundi A. Soft-and hard-tissue changes following treatment of class II division 1 malocclusion with activator versus trainer: a randomized controlled trial. Eur J Orthod. (2019) 41(1):21–8. doi: 10.1093/ejo/cjy014
11. Cretella Lombardo E, Franchi L, Gastaldi G, Giuntini V, Lione R, Cozza P, et al. Development of a prediction model for short-term success of functional treatment of class II malocclusion. Int J Environ Res Public Health. (2020) 17(12):4473. doi: 10.3390/ijerph17124473
12. Baysal A, Uysal T. Soft tissue effects of twin block and Herbst appliances in patients with class II division 1 mandibular retrognathy. Eur J Orthod. (2013) 35(1):71–81. doi: 10.1093/ejo/cjq187
13. Varlık SK, Gültan A, Tümer N. Comparison of the effects of twin block and activator treatment on the soft tissue profile. Eur J Orthod. (2008) 30(2):128–34. doi: 10.1093/ejo/cjm121
14. Ravera S, Castroflorio T, Galati F, Cugliari G, Garino F, Deregibus A, et al. Short term dentoskeletal effects of mandibular advancement clear aligners in class II growing patients. A prospective controlled study according to STROBE guidelines. Eur J Paediatr Dent. (2021) 22(2):119–24. doi: 10.23804/ejpd.2021.22.02.6
15. Pavoni C, Lione R, Lugli L, Loberto S, Cozza P. Treatment timing considerations for mandibular advancement with clear aligners in skeletal class II malocclusions. J Clin Orthod. (2022) 56(8):464–71.36572047
16. Cretella Lombardo E, Lugli L, Cozza P, Lione R, Loberto S, Pavoni C. Comparison between twin block appliance and mandibular advancement on clear aligners in the improvement of airway dimension: incremental versus maximum bite advancement. Front Oral Health. (2024) 5:1463416. doi: 10.3389/froh.2024.1463416
17. Laganà G, Malara A, Lione R, Danesi C, Meuli S, Cozza P. Enamel interproximal reduction during treatment with clear aligners: digital planning versus OrthoCAD analysis. BMC Oral Health. (2021) 21:1–6. doi: 10.1186/s12903-021-01487-2
18. Sabouni W, Hansa I, Al Ali SM, Adel SM, Vaid N. Invisalign treatment with mandibular advancement: a retrospective cohort cephalometric appraisal. J Clin Imaging Sci. (2022) 12. doi: 10.25259/JCIS_64_2022
19. Sadek M, Awad S. Cephalometric evaluation of the short-term skeletal, dental and soft tissue changes in subjects with class II division 1 malocclusion treated with invisalign® with mandibular advancement feature. Ain Shams Dental Journal. (2022) 25(1):63–73. doi: 10.21608/asdj.2023.211868.1176
20. Goje SK, Dandwate AA. Cephalometric effects of class II correction using invisalign’s mandibular advancement in growing patients. Library of progress-library science. Inf Technol Computer. (2024) 44(2s). doi: 10.48165/bapas.2024.44.2.1
21. Al Subaie H, Alturki G, Alsulaimani F, Ghoneim S, Baeshen H. Assessment of dental, skeletal, and soft tissue changes following mandibular advancement with invisalign in skeletal class II. Saudi Dent J. (2024) 36(1):66–71. doi: 10.1016/j.sdentj.2023.09.005
22. Baccetti T, Franchi L, McNamara JA Jr. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. (2005) 11(3):119–29. doi: 10.1053/j.sodo.2005.04.005
23. Bergman RT, Waschak J, Borzabadi-Farahani A, Murphy NC. Longitudinal study of cephalometric soft tissue profile traits between the ages of 6 and 18 years. Angle Orthod. (2014) 84(1):48–55. doi: 10.2319/041513-291.1
24. Arnett GW, Jelic JS, Kim J, Cummings DR, Beress A, Worley CM Jr, et al. Soft tissue cephalometric analysis: diagnosis and treatment planning of dentofacial deformity. Am J Orthod Dentofacial Orthop. (1999) 116(3):239–53. doi: 10.1016/S0889-5406(99)70234-9
25. Springate SD. The effect of sample size and bias on the reliability of estimates of error: a comparative study of Dahlberg’s formula. Eur J Orthod. (2012) 34(2):158–63. doi: 10.1093/ejo/cjr010
26. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. (1977) 33(1):159–74. doi: 10.2307/2529310
27. Hourfar J, Lisson JA, Gross U, Frye L, Kinzinger GSM. Soft tissue profile changes after functional mandibular advancer or Herbst appliance treatment in class II patients. Clin Oral Investig. (2018) 22:971–80. doi: 10.1007/s00784-017-2177-0
28. Loberto S, Pavoni C, Fanelli S, Lugli L, Cozza P, Lione R. Predictability of expansion movements performed by clear aligners in mixed dentition in both arches: a retrospective study on digital casts. BMC Oral Health. (2024) 24(1):694. doi: 10.1186/s12903-024-04435-y
29. Staderini E, Patini R, Meuli S, Camodeca A, Guglielmi F, Gallenzi P. Indication of clear aligners in the early treatment of anterior crossbite: a case series. Dental Press J Orthod. (2020) 25:33–43. doi: 10.1590/2177-6709.25.4.033-043.oar
30. Ballanti F, Lione R, Fiaschetti V, Fanucci E, Cozza P. Low-dose CT protocol for orthodontic diagnosis. Eur J Paediatr Dent. (2008) 9(2):65–70.18605887
31. Baccetti T, Franchi L, Toth LR, McNamara JA Jr. Treatment timing for twin-block therapy. Am J Orthod Dentofacial Orthop. (2000) 118(2):159–70. doi: 10.1067/mod.2000.105571
32. Ehsani S, Nebbe B, Normando D, Lagravere MO, Flores-Mir C. Short-term treatment effects produced by the twin-block appliance: a systematic review and meta-analysis. Eur J Orthod. (2015) 37(2):170–6. doi: 10.1093/ejo/cju030
33. Tepedino M, Colasante P, Staderini E, Masedu F, Ciavarella D. Short-term effect of orthodontic clear aligners on muscular activity and occlusal contacts: a cohort study. Am J Orthod Dentofacial Orthop. (2023) 164(1):34–44. doi: 10.1016/j.ajodo.2022.10.025
34. Patini R, Arrica M, Di Stasio E, Gallenzi P, Cordaro M. The use of magnetic resonance imaging in the evaluation of upper airway structures in paediatric obstructive sleep apnoea syndrome: a systematic review and meta-analysis. Dentomaxillofac Radiol. (2016) 45(7):20160136. doi: 10.1259/dmfr.20160136
35. Gazzani F, Franchi L, Lione R, Cozza P, Pavoni C. Soft tissue evaluation of functional therapy in growing patients with class II malocclusion: a long-term study. Eur J Orthod. (2022) 44(1):37–42. doi: 10.1093/ejo/cjab008
Keywords: class II malocclusion, functional therapy, clear aligners, twin block, mandibular advancement
Citation: Lugli L, Pavoni C, De Razza FC, Gazzani F, Loberto S, Cretella Lombardo E, Cozza P and Lione R (2025) Soft tissue evaluation of functional therapy in growing patients with class II malocclusion: mandibular advancement vs. twin block—a retrospective study. Front. Dent. Med. 6:1581032. doi: 10.3389/fdmed.2025.1581032
Received: 21 February 2025; Accepted: 28 July 2025;
Published: 2 September 2025.
Edited by:
Elif Bahar Tuna Ince, Istanbul University, TürkiyeReviewed by:
Michele Tepedino, University of L'Aquila, ItalyRomeo Patini, Agostino Gemelli University Polyclinic (IRCCS), Italy
Floriane Remy, UMR5199 De la Prehistoire A l'actuel Culture, Environnement et Anthropologie (PACEA), France
Copyright: © 2025 Lugli, Pavoni, De Razza, Gazzani, Loberto, Cretella Lombardo, Cozza and Lione. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: P. Cozza, cGFvbGEuY296emFAdW5pY2FtaWxsdXMub3Jn
 L. Lugli
L. Lugli C. Pavoni1
C. Pavoni1 F. C. De Razza
F. C. De Razza