- Global Center for Mass Gatherings Medicine, Ministry of Health, Riyadh, Saudi Arabia
Background: The Hajj pilgrimage, a significant spiritual journey for Muslims, occurs annually in Mecca, Saudi Arabia, attracting millions of participants from diverse backgrounds worldwide. This surge in pilgrims poses substantial challenges for healthcare services, as many face health risks due to physical exertion, dehydration, and exposure to infectious diseases. The unique healthcare demands during Hajj necessitate a thorough understanding of the quality of care provided and the challenges faced by medical convoys.
Objectives: This study aims to assess the quality of care provided by medical convoys to medical conditions transferred to secondary or tertiary healthcare facilities during the Hajj season in 2023, while also examining the difficulties and challenges encountered by healthcare providers throughout the trip.
Methods and materials: This observational retrospective cross-sectional study involved 295 patients transferred from Makkah and Madinah hospitals to Arafat via a specialized medical convoy service during the 2023 Hajj season. Data were collected from electronic patient data sheets, documenting demographic characteristics, comorbidities, clinical diagnoses, transfer details, and the Risk Score for Transported Patients (RSTP). Ethical approval was obtained under IRB log Number: 23-452E from the Research Ethics Committee at King Fahad Medical City.
Results: Among the 295 patients, the majority were males with an average age of 63.16 years. The most common nationalities were Asian (48.1%) and African (28.5%). Significant comorbidities included hypertension (34.2%) and diabetes mellitus (33.2%). RSTP indicated that 96.6% of patients had scores below 6. Nearly half were discharged within 72 h post-transfer, while a small percentage experienced deterioration or mortality. Most patients (58.3%) did not receive any medications or anesthesia, although 31.2% were administered analgesics. Common diagnoses included fractures (15.3%) and heat stroke (10.5%). Univariate logistic regression analysis revealed significant associations between higher RSTP and factors such as older age, presence of arrhythmias, need for respiratory support, lower Glasgow Coma Scale scores, total score, and blood pressure.
Conclusion: This study highlights the diverse demographic characteristics and significant comorbidities of patients transferred during the Hajj season, indicating the need for tailored healthcare strategies that address the complexities of managing these patients. The strong association between higher RSTP scores and factors such as older age and arrhythmias underscores the importance of enhanced monitoring during transport. It is crucial to develop protocols that ensure patient safety and optimize outcomes in future healthcare delivery during Hajj.
Introduction
The Hajj pilgrimage, a significant spiritual journey for Muslims, occurs annually in Mecca, Saudi Arabia, attracting millions of participants from diverse backgrounds worldwide (1). As one of the five pillars of Islam, Hajj requires rigorous physical effort, often exposing pilgrims to extreme weather conditions and overcrowded environments. Consequently, many pilgrims present with pre-existing medical conditions or develop health complications during their journey, highlighting the critical need for effective healthcare services (2, 3).
The number of pilgrims has dramatically increased over the years, with the Saudi Ministry of Hajj and Umrah reporting over 2.5 million participants in recent years (4). This surge poses substantial challenges for healthcare services, as pilgrims face various health risks due to crowded conditions which exacerbate these risks. The influx of pilgrims not only strains existing healthcare facilities but also necessitates proactive measures to meet their unique health needs effectively (5).
The Hajj pilgrimage presents unique healthcare challenges that distinguish it from other large-scale mass gatherings. Pilgrims face a range of physical and environmental stressors, including overcrowding, extreme temperatures, dehydration, and exhaustion, all of which contribute to an increased risk of medical emergencies. These factors, combined with the high density of people from diverse geographical regions with varying health statuses, present significant obstacles for healthcare providers (6, 7).
Historically, the Hajj has seen outbreaks of infectious diseases, such as meningococcal meningitis, which led to extensive preventive measures, including mandatory vaccination for pilgrims (8). Additionally, cardiovascular emergencies are common, particularly among older pilgrims or those with pre-existing comorbidities, due to the physical strain of the pilgrimage and the environmental stressors (9). These issues highlight the need for comprehensive healthcare strategies tailored specifically for the pilgrimage setting. Proactive measures, including early detection, targeted screening, and optimized resource allocation, are essential to prevent and manage such crises during Hajj.
A key aspect of managing healthcare during Hajj is the coordination among stakeholders, including the Ministry of Health, local hospitals, and healthcare providers. This collaboration is crucial for streamlining the process of treating pilgrims who require medical attention (10, 11). The medical convoy system serves as an organized response to these challenges, providing essential care by transporting patients from Makkah hospitals to Arafat during the Hajj season (12). With well-defined protocols for triaging patients, the convoy aims to minimize treatment delays and improve outcomes for those experiencing medical emergencies. The unique infrastructure established for Hajj, including temporary medical facilities and specialized healthcare teams, reflects the commitment to safeguarding pilgrims' health (13).
While previous research has explored various facets of healthcare during the Hajj (1, 14–16), significant gaps remain in understanding the overall quality of care provided by medical convoys, the challenges faced by healthcare providers, and the specific medical conditions encountered during these critical transfers. Understanding the logistical, clinical, and administrative challenges faced by healthcare workers in these settings is vital for improving service delivery (17–19).
This study aims to assess the quality of care provided by medical convoys to medical conditions transferred to secondary or tertiary healthcare facilities during the Hajj season in 2023, while also examining the difficulties and challenges encountered by healthcare providers throughout the trip. By exploring these aspects, this study seeks to contribute valuable insights that can inform policy decisions, improve healthcare delivery, and ultimately enhance patient outcomes during the Hajj pilgrimage. Through rigorous analysis, this research aspires to pave the way for more effective and efficient healthcare strategies, ensuring that the spiritual journey of millions is accompanied by adequate medical support.
Methods and materials
Study design and participants
This was an observational retrospective cross-sectional study aimed to assess the quality of care provided by medical convoys to medical conditions transferred to secondary or tertiary healthcare facilities while also evaluating the difficulties and challenges encountered by healthcare providers throughout the trip. The study was conducted during the Hajj season of 2023, a period characterized by a significant influx of pilgrims to the holy sites in Saudi Arabia. Data were collected from patients transferred from Makkah and Madinah hospitals to Arafat via a specialized medical convoy service established by Saudi Arabia to cater to pilgrims. Participants in the study were characterized by various demographic and clinical variables, including age, gender, nationality, and pre-existing medical conditions, which were documented alongside their clinical presentations upon arrival at the medical convoy.
Sample size
The sample size for this study consisted of 295 patients, representing all patients transferred by the medical convoy during the Hajj season in 2023. This comprehensive inclusion ensured that the data collected would provide a reliable and representative analysis of the population, capturing the full scope of medical conditions and challenges encountered.
Inclusion/exclusion criteria
Eligible participants included pilgrims of all ages and genders who required transfer due to medical conditions from hospitals in Makkah and Madinah to Arafat via the medical convoy during the 2023 Hajj season. Exclusion criteria involved patients who were intubated patients, clinically unstable patients who scored seven or more based on the National Early Warning Score, patients using more than one inotrope medication, and patients needing isolation or contact precautions. These patients were excluded due to the high complexity of their condition, which demands intensive care and continuous monitoring. The focus of this study was on patients who required transfer but were considered clinically stable for the transport process.
Patient selection and transfer process
Patients requiring transfer by the medical convoy were selected primarily based on the severity of their medical conditions, as assessed by the attending medical personnel at the healthcare facilities in Makkah and Madinah. Medical teams followed established guidelines for patient transfer, prioritizing those with acute and urgent medical needs that necessitated specialized care at the designated facilities in Arafat. This selection process ensured that only patients with critical health conditions were transferred, irrespective of time of day or personnel on duty. To minimize any potential variability in patient care due to time of day, personnel availability, or medical resource fluctuations, the medical convoy system was designed to provide 24-h medical support and ensure the consistent availability of essential medical equipment and medications. While these factors could have contributed to some degree of variation in care and outcomes, the convoy system was structured to address these challenges, ensuring that medical services were delivered according to standardized protocols. The potential impact of these factors on the study findings has been considered and discussed in the manuscript.
Procedure and data collection
Data were collected from the electronic patient data sheets for the 295 pilgrims included in the study, focusing on medical conditions transferred to secondary or tertiary healthcare facilities during the Hajj season in 2023. Patients' data were extracted via a standardized electronic evaluation form used to collect data from the pilgrims by trained healthcare workers from the medical convoy.
The collected variables encompassed demographic characteristics such as age, gender, and nationality, as well as comorbidities, which included various cardiac conditions (e.g., ischemic heart disease, heart failure), renal issues (e.g., chronic kidney disease, acute kidney injury), hepatic conditions (e.g., liver cirrhosis), neurological disorders (e.g., cerebrovascular accident, dementia), respiratory diseases (e.g., asthma, COPD), hypertension, diabetes mellitus, hypothyroidism, and other conditions like benign prostatic hyperplasia and cancer. Additionally, clinical diagnoses at presentation were recorded, including fractures, heat stroke, hypertension, diabetes mellitus, heart failure, pneumonia, stroke, and various renal and neurological conditions, as well as other conditions such as cellulitis, gastrointestinal issues, and infectious diseases. Transfer and follow-up details were also documented, including Risk Score for Transported Patient (RSTP), outcomes at 72 h post-trip (e.g., discharged, improved, stable, deteriorated, death), and discharge against medical advice (DAMA). Hemodynamic monitoring and cardiovascular findings included the assessment of hemodynamic status (stable or unstable), electrocardiographic changes (e.g., T wave inversion, left ventricular hypertrophy), and the presence of arrhythmias. Respiratory parameters such as respiratory rate, the need for respiratory support, and oxygen saturation were also recorded, along with neurological status as indicated by Glasgow Coma Scale (GCS) scores. Furthermore, vital signs and clinical measurements included systolic and diastolic blood pressure, heart rate, and a total score measuring clinical condition or risk. Finally, information regarding medications and anesthesia administered to the patients, such as analgesics, steroids, vasopressors, and the use of general anesthesia, was collected to assess the clinical status and outcomes of the patients and to analyze the association between the RSTP and various patient characteristics.
In this study, we utilized the Risk Score for Transported Patients (RSTP), a tool designed to assess the risk of adverse events during patient transfers. The RSTP score is based on a range of clinical parameters, including age, comorbidities, and vital signs, such as blood pressure, respiratory rate, and Glasgow Coma Scale (GCS) score. The scoring system assigns points to each parameter, with higher scores indicating an increased risk of complications during transport. The RSTP has been validated in multiple settings, demonstrating its predictive value for patient outcomes during transfers. For the Hajj context, we adapted the RSTP to account for unique factors, including the extreme environmental stressors, such as high temperatures and physical strain from overcrowding, that can exacerbate existing medical conditions. Given the specific health challenges posed by the pilgrimage, we modified the scoring thresholds to incorporate these external factors, enhancing the accuracy of risk assessments for patients transferred during the Hajj season. This adaptation ensures that the RSTP remains relevant and robust in assessing risk in this unique setting.
Ethical considerations
This study was performed in line with the principles of the Declaration of Helsinki. Ethical approval was obtained under IRB log Number: 23-452E from the Research Ethics Committee at King Fahad Medical City.
Statistical analysis
Statistical analysis was done by SPSS version 28 (IBM Co., Armonk, NY, USA). Numerical data were presented as the mean and standard deviation (SD) and analyzed using Unpaired t-test. Categorical data were presented as the frequency and percentage and analyzed using Chi-square test or exact test as appropriate. Univariate logistic regression analysis was performed to identify factors associated with RSTP. A two tailed P < 0.05 was considered statistically significant.
Results
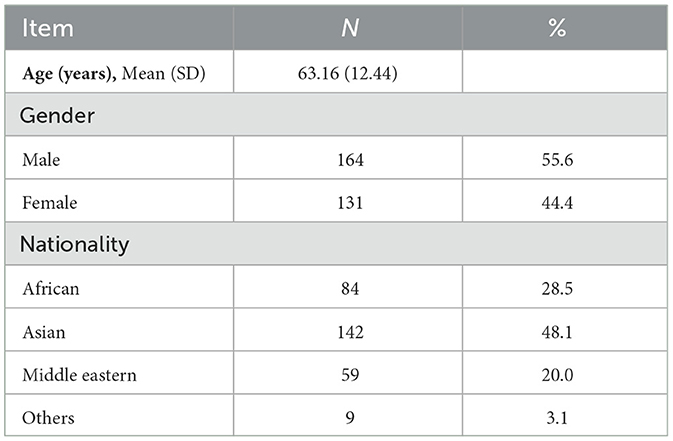
Demographic characteristics of the study population are presented in Table 1. A total of 295 patients were included in the study. The average age of the patients was 63.16 (±12.44) years. Regarding gender distribution, the majority of the patients were males, accounting for 55.6% (n = 164), while females comprised 44.4% (n = 131). The largest proportion of patients were of Asian origin, making up 48.1% (n = 142) of the sample. African patients represented 28.5% (n = 84), while those of Middle Eastern descent constituted 20.0% (n = 59). A small percentage of the participants (3.1%, n = 9) were from other nationalities.
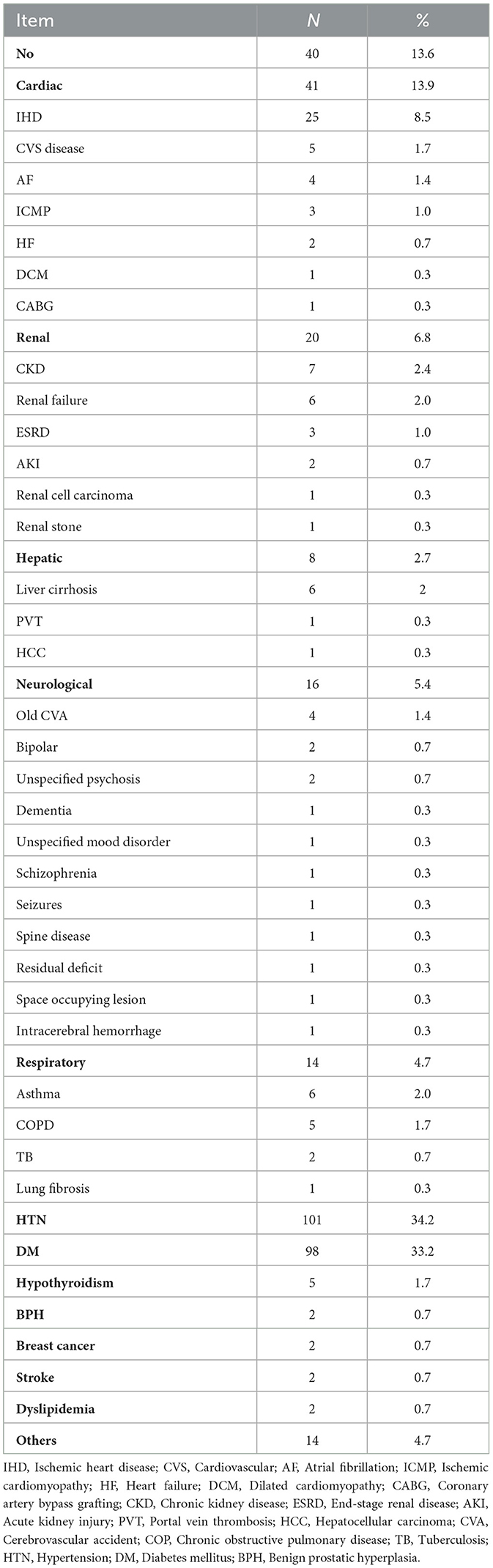
Comorbidities in the study population are presented in Table 2. It was shown that 40 patients (13.6%) reported no comorbidities. Among those with comorbidities, cardiac conditions were observed in 41 patients (13.9%), with ischemic heart disease (IHD) being the most prevalent at 25 patients (8.5%). Other cardiac conditions included cardiovascular disease (CVS) in five patients (1.7%), atrial fibrillation (AF) in four patients (1.4%), ischemic cardiomyopathy (ICMP) in three patients (1.0%), heart failure (HF) in two patients (0.7%), and dilated cardiomyopathy (DCM) and coronary artery bypass grafting (CABG) in one patient each (0.3%). Renal comorbidities were present in 20 patients (6.8%), with chronic kidney disease (CKD) affecting seven patients (2.4%), renal failure in six patients (2.0%), and end-stage renal disease (ESRD) in three patients (1.0%). Additional renal conditions included acute kidney injury (AKI) in two patients (0.7%) and both renal cell carcinoma and renal stones in one patient each (0.3%). Hepatic conditions were reported in eight patients (2.7%), predominantly liver cirrhosis affecting six patients (2.0%). Neurological conditions were noted in 16 patients (5.4%), with old cerebrovascular accident (CVA) in four patients (1.4%) and various other neurological disorders in one patient each (0.3%). Respiratory conditions were present in 14 patients (4.7%), primarily asthma in six patients (2.0%) and COPD in five patients (1.7%). Notably, hypertension (HTN) and diabetes mellitus (DM) were the most common metabolic conditions, affecting 101 patients (34.2%) and 98 patients (33.2%), respectively, with hypothyroidism in five patients (1.7%) and other unspecified comorbidities affecting 14 patients (4.7%).
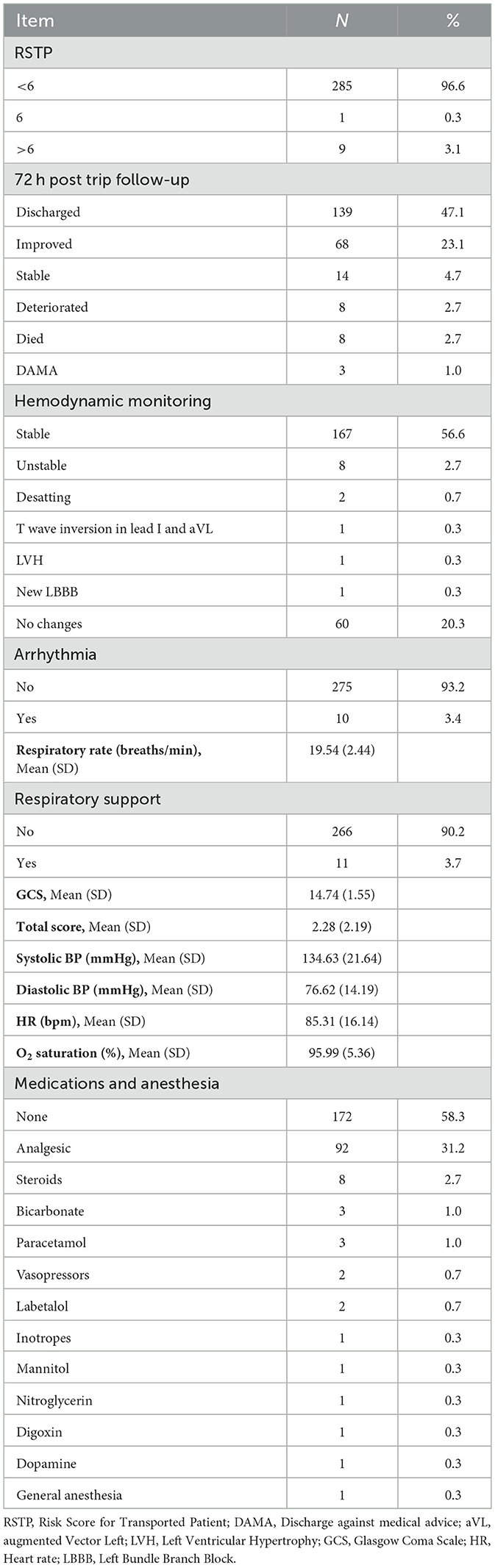
Transfer details of the study population are presented in Table 3. The majority of patients (96.6%) had a RSTP below 6, while only 3.1% had scores above 6. At the 72-h post-trip follow-up, nearly half of the patients (47.1%) were discharged, 23.1% showed improvement, 4.7% remained stable, 2.7% deteriorated, and another 2.7% died. Moreover, three patients (1.0%) were discharged against medical advice (DAMA). Hemodynamic monitoring indicated that 56.6% of patients were stable, while a small portion exhibited instability (2.7%), desaturation (0.7%), or cardiac changes, including T wave inversion (0.3%), left ventricular hypertrophy (0.3%), new left bundle branch block (0.3%), and 20.3% showed no ECG changes. Arrhythmias were uncommon, with 93.2% of patients showing no arrhythmic activity. Respiratory rate averaged 19.54 breaths per minute, with 90.2% of patients not requiring respiratory support. The Glasgow Coma Scale (GCS) mean was 14.74, the total score averaged 2.28, systolic blood pressure was 134.63 mmHg, diastolic blood pressure 76.62 mmHg, heart rate 85.31 bpm, and oxygen saturation 95.99%. Regarding medications, 58.3% received none, while analgesics were administered to 31.2%. Steroids were given to 2.7%, and other medications, including bicarbonate, paracetamol, vasopressors, labetalol, and inotropes, were used in <1% of cases. General anesthesia was used for one patient (0.3%).
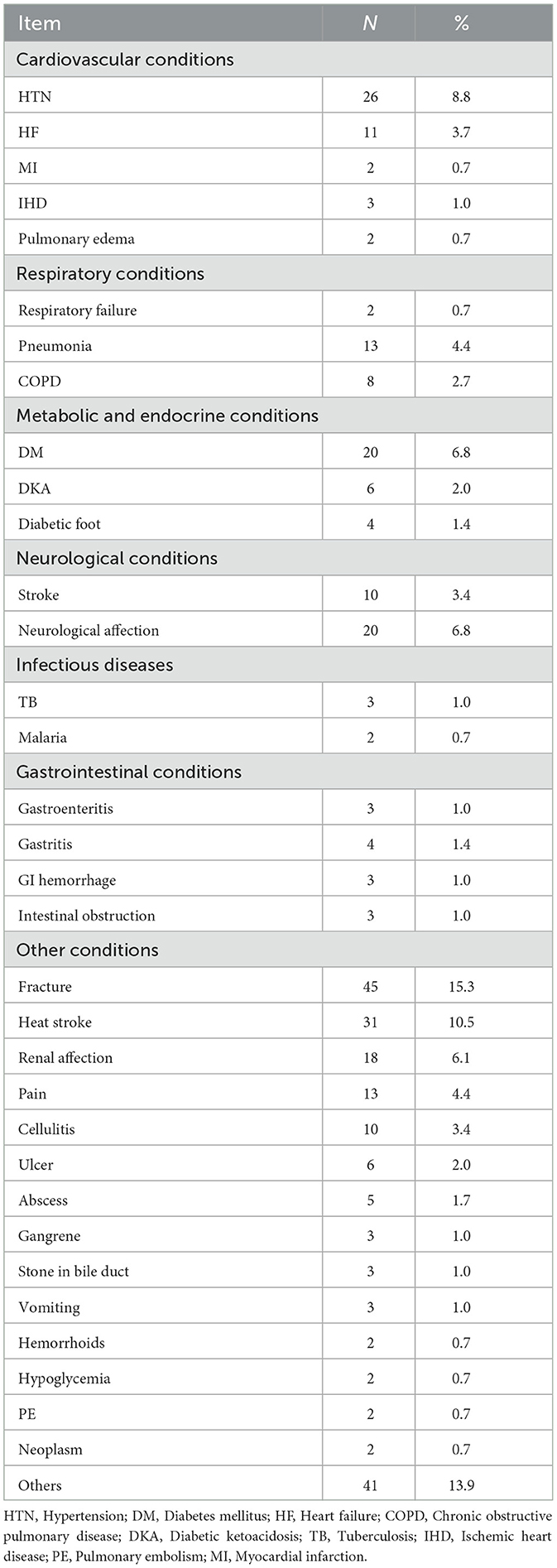
Diagnoses of the study population are represented in Table 4. Fractures were the most common diagnosis, affecting 45 patients (15.3%). Heat stroke was identified in 31 patients (10.5%), while hypertension (HTN) was present in 26 patients (8.8%), and diabetes mellitus (DM) in 20 patients (6.8%). Both neurological and renal conditions were noted in 20 (6.8%) and 18 patients (6.1%), respectively. Pain and pneumonia each affected 13 patients (4.4%), while heart failure (HF) was observed in 11 patients (3.7%). Cellulitis and stroke were present in 10 patients each (3.4%), and chronic obstructive pulmonary disease (COPD) was noted in eight patients (2.7%). Diabetic ketoacidosis (DKA) and ulcers were diagnosed in six patients each (2.0%), while abscesses affected five patients (1.7%). Less common conditions included diabetic foot and gastritis in four patients each (1.4%), and gangrene, gastroenteritis, gastrointestinal hemorrhage, intestinal obstruction, bile duct stones, tuberculosis (TB), ischemic heart disease (IHD), and vomiting, each occurring in three patients (1.0%). Additional diagnoses, each affecting two patients (0.7%), included hemorrhoids, hypoglycemia, pulmonary embolism (PE), myocardial infarction (MI), pulmonary edema, respiratory failure, malaria, and neoplasms. Other miscellaneous conditions were reported in 41 patients (13.9%).
The association between RSTP and various patient characteristics is presented in Table 5. There was a statistically significant association between RSTP of patients and their age, the incidence of arrythmias, respiratory rate, requiring respiratory support, GCS, total score and BP (P < 0.05) as the univariate logistic regression model revealed that: Older age was associated with higher RSTP as each 1 unit increase in the first resulted in increasing the odds of having >6 RSTP by 1.1 (95%CI: 1.02 to 1.18). In comparison to patients not experiencing arrhythmias, those who had arrhythmias showed higher odds of having >6 RSTP (OR = 45.17, 95%CI: 9.08 to 224.77). Also, those who required respiratory support had 463.75 times the odds of having >6 RSTP as others (95%CI: 45.74 to 4701.39). Each 1 unit increase in respiratory rate, GCS, systolic and diastolic BP resulted in decreasing the odds of having >6 RSTP, respectively by 0.59 (95%CI: 0.44 to 0.8), 0.5 (95%CI: 0.32 to 0.79), 0.91 (95%CI: 0.87 to 0.96), and 0.82 (95%CI: 0.74 to 0.89), however, each 1 unit increase in total score was associated with increasing the odds of having >6 RSTP by 2.26 (95%CI: 1.55 to 3.3).
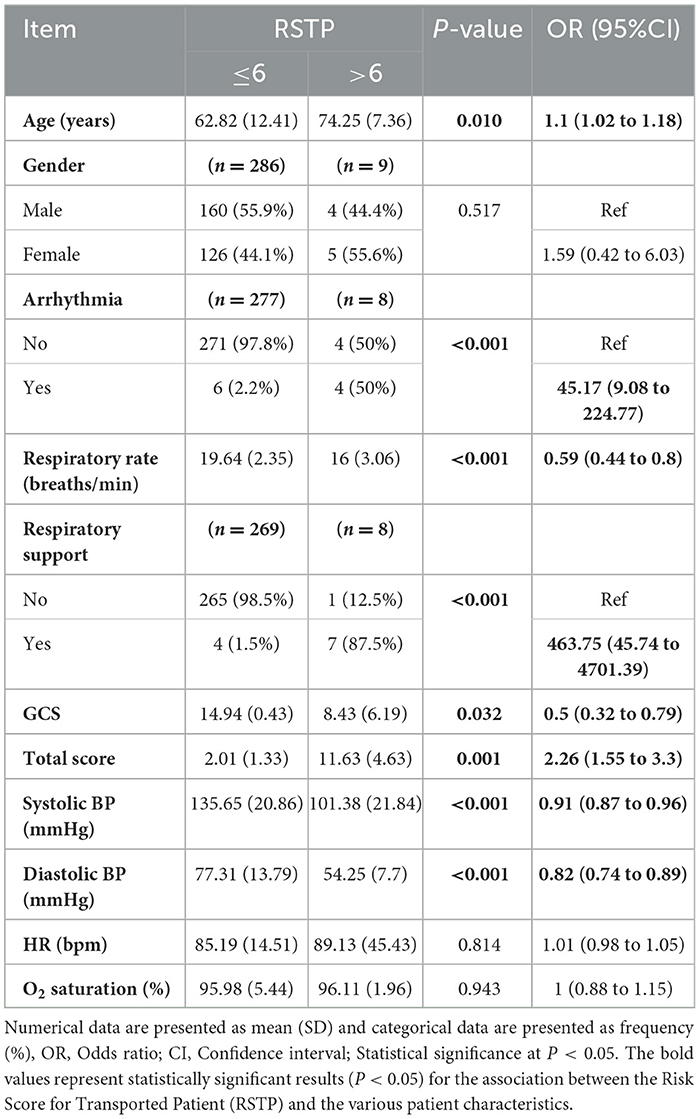
Table 5. Association between Risk Score for Transported Patient (RSTP) and various patient characteristics.
Discussion
The quality of care during medical transfers is crucial, especially during the Hajj season, where the demand for healthcare services surges (20). This study aimed to assess the quality of care and challenges in medical convoys transporting patients from Makkah and Madinah to Arafat during Hajj season 2023. Our findings revealed that among the 295 patients, a significant proportion were males, with an average age of 63.16 years. The most common nationalities were Asian and African. There was also a notable prevalence of comorbidities such as hypertension and diabetes mellitus. The RSTP indicated that 96.6% of patients had scores below 6. Nearly half of the patients were discharged within 72 h post-transfer, while a small percentage experienced deterioration or mortality. Additionally, most patients did not receive any medications or anesthesia, although nearly a third were administered analgesics. The most common diagnoses included fractures and heat stroke. Notably, univariate logistic regression analysis revealed significant associations between higher RSTP and older age, presence of arrhythmias, need for respiratory support, lower Glasgow Coma Scale scores, total score, and blood pressure.
The study's patient population had an average age of 63.16 years, with a predominance of males (55.6%) and a significant representation of Asian (48.1%) and African (28.5%) nationalities. These findings align with the results of Khan et al., who reported that 36.1% of transferred patients were older adults (>60 years), and 55.8% were males, while 59.9% were Asian and 36.4% were African (21). Similarly, Alrufaidi et al. observed that a considerable proportion of emergency cases at the Hajj terminal involved middle-aged individuals, with the highest number of patients aged 30–59 years. Although Alrufaidi et al. reported a slightly higher representation of females (51.3%) than males, their findings on the most common nationalities, including Indonesians and Egyptians, correlate with the substantial representation of Asian and African origins in the current study (20). This demographic profile suggests that older males face greater health challenges during Hajj, which could be due to the physical demands and harsh environmental conditions. Moreover, socioeconomic factors and limited access to preventive healthcare in some Asian and African communities may contribute to increased health risks. Consequently, these findings underscore the need for targeted health strategies that consider the cultural and demographic context, promoting preventive measures and addressing common health conditions for these populations during Hajj. Implementing culturally tailored healthcare programs, including health education and medical resources, could improve health outcomes and reduce hospitalizations among these vulnerable groups.
Cardiovascular and metabolic comorbidities, particularly hypertension (34.2%) and diabetes mellitus (33.2%), were the most common in this study. These findings contrast with a systematic review conducted by Yezli et al. (22), which reported a much lower weighted pooled prevalence of hypertension at 12.2% and diabetes at 5.0% among Hajj pilgrims. This discrepancy may stem from differences in study populations and methodologies, as Yezli et al. analyzed data from 26 studies encompassing over 285,000 participants, highlighting a potentially underdiagnosed burden of these conditions (22). Furthermore, the study by Alzahrani et al. (23) indicated that diabetes, asthma, and hypertension each constituted <3% of the total diseases among Hajj pilgrims, which further emphasizes the variability in disease patterns (23). The lower prevalence rates of these comorbidities in the literature suggest that while hypertension and diabetes remain prevalent in the current study, there may be differences in health service utilization and management strategies among different populations of pilgrims. This finding underscores the importance of targeted screening and management programs specifically designed for pilgrims with hypertension and diabetes, especially during high-stress events like Hajj. Effective pre-pilgrimage assessments could help identify undiagnosed cases and optimize disease management, thus reducing the risk of acute complications during the pilgrimage.
The majority of patients (96.6%) had RSTP scores below 6, suggesting a relatively low risk during transfer. Hemodynamic monitoring indicated a high rate of stability (56.6%), with minimal cases of arrhythmias or respiratory support needed, underscoring the effectiveness of the medical convoy system. These findings align with the study by Markakis et al., who classified patients into two severity groups using the RSTP, revealing that major en route complications were more common in group II patients, with a significantly higher mean risk score compared to group I (11.04 vs. 4.48) (24). Similarly, Srithong et al. reported that patients with a pre-transfer risk score of eight or higher experienced a higher incidence of clinical deterioration (28.69%) during inter-facility transfers, particularly due to hemodynamic instability and respiratory distress (25). The low RSTP scores among most patients in our study can be interpreted as an indicator of effective pre-transfer assessments and interventions that adequately managed patients' health status prior to transport. This suggests that rigorous screening processes are crucial for identifying patients who may require additional monitoring during transfers.
At 72 h post-transfer, approximately half of the patients were discharged (47.1%), indicating that prompt medical care during transfer was effective for many. This finding aligns with data from the Indian Medical Mission by Khan et al. (26), where timely interventions significantly improved patient outcomes during mass gatherings, reflecting similar discharge rates when rapid care is available (26). Moreover, the low proportion of deaths (2.7%) and deterioration (2.7%) in our study during this period suggests favorable transfer outcomes despite the patients' advanced age and multiple comorbidities. This contrasts with findings from Madani et al. (27), who reported higher complication rates among older pilgrims requiring intensive care during Hajj (27). The results can be interpreted as highlighting the critical role of organized emergency medical services during high-risk events, as emphasized in the study by Srithong et al. (25), which identified risk factors associated with clinical deterioration during inter-facility transfers. The presence of trained personnel and efficient protocols likely facilitated timely interventions that contributed to improved outcomes for patients (25). Therefore, the favorable discharge rates underscore the effectiveness of rapid medical interventions in enhancing patient outcomes during transfers, particularly for vulnerable populations. Continued investment in pre-hospital care systems and ongoing training for emergency personnel are essential for further enhancing patient safety and outcomes during high-stress situations like the Hajj.
A significant finding from this study is that the majority of patients (58.3%) did not receive any medications or anesthesia during their transfer, while 31.2% were administered analgesics. This observation contrasts with previous studies, such as those by Alzahrani et al. (23) and Khan et al. (26), which highlighted a higher prevalence of medication administration among similar patient populations (23, 26). Alzahrani et al. found that the most frequently prescribed drugs were analgesics and antipyretics (79.4%) (23), while Khan et al. reported that analgesics were administered to 66.38 per 100 patients among Indian Hajj pilgrims, reflecting a more aggressive approach to symptom management (26). The lower rate of medication administration observed in our study may suggest a more conservative approach to patient management, potentially influenced by factors such as patient stability and assessment protocols. This finding raises important questions about the adequacy of pain management and the overall comfort of patients during transfer. Unmanaged pain can lead to increased physiological stress, exacerbating existing health issues and potentially worsening patient outcomes. Therefore, our results underscore the need for healthcare providers to evaluate and implement guidelines for effective pain management in similar settings, particularly during critical transport periods. By ensuring appropriate analgesic administration and addressing patient comfort proactively, healthcare systems can enhance patient safety and reduce the risks associated with inadequate symptom management during high-stress events like the Hajj.
Fractures (16.1%) and respiratory diseases (15.3%) were among the most common diagnoses observed in patients transferred by the medical convoy team during the Hajj season, highlighting the physical and environmental challenges faced by pilgrims. This aligns with findings from Alrufaidi et al. (20), who reported that among 7,643 pilgrims treated at King Abdulaziz International Airport Health Care Center, emergency cases included hypertension (19.9%), bronchial asthma (17.9%), and myocardial infarction (5.4%) (20). The prevalence of these conditions emphasizes the need for targeted health interventions during the Hajj, particularly for older adults who are at a higher risk of complications. The trends in prevalent injuries among Iranian pilgrims reported by Razavi et al. (28), in Hajj period across 2004 to 2008, further underscore the significance of environmental factors contributing to health issues during Hajj. Injuries such as tissue contusions, tendon lesions, and ankle sprains were prevalent, with tissue contusions occurring at a rate of 76 per 10,000 pilgrims (28). The high incidence of injuries during the pilgrimage reflects the hazards of overcrowding and the physical exertion associated with Hajj activities, necessitating preventive measures, including crowd management and health education initiatives. Furthermore, the significant change in injury patterns over the years highlights the importance of continuous surveillance and adaptive strategies to improve safety for pilgrims. The findings from these studies collectively suggest a pressing need for comprehensive pre-Hajj health assessments and the implementation of targeted management strategies for at-risk populations, particularly older adults and those with pre-existing health conditions. By understanding the health challenges faced by pilgrims, healthcare authorities can enhance the preparedness of medical teams and ensure the provision of timely and effective care, ultimately improving health outcomes during this significant religious event. This emphasizes the importance of integrating health education and resources into the pilgrimage experience to mitigate the risks associated with the Hajj.
The analysis of the association between RSTP and various patient characteristics revealed several key findings. Older age was significantly associated with higher RSTP scores, with each additional year increasing the odds of having an RSTP score >6 by 1.1 times. The presence of arrhythmia showed a striking association with higher RSTP scores (OR = 45.17), indicating that patients with an RSTP score above six were ~45 times more likely to have arrhythmia than those with a score of six or less. This suggests that arrhythmia is a strong predictor of higher transport risk. Similarly, respiratory rate showed a significant association with RSTP scores, where an odds ratio of 0.59 indicated that lower respiratory rates were linked to higher transport risk, possibly indicating compromised respiratory function. The need for respiratory support was another critical factor, with those requiring it having odds 463.75 times greater for a higher RSTP score, underscoring the role of respiratory compromise as a predictor of transport-related complications. These findings highlight the importance of comprehensive pre-transport assessments to identify patients at elevated risk due to respiratory issues. Additionally, lower GCS scores and blood pressure were associated with higher RSTP scores, with increases in GCS and blood pressure reducing the odds of an RSTP score above 6.
Understanding the associations between these characteristics and transport risk can improve pre-transport assessments, enabling healthcare providers to identify high-risk patients and take necessary precautions to reduce risks. By tailoring transport plans and enhancing monitoring strategies according to individual patient needs, the likelihood of adverse events can be minimized, ultimately improving patient safety and care quality (29). These findings emphasize the importance of thorough evaluations and risk stratification in patient transport scenarios. Consequently, healthcare systems should integrate RSTP scores into triage protocols to identify patients who may need more intensive monitoring or immediate care during transfers (24).
Strengths and limitations
The study has several strengths and limitations. Among its strengths, it employs a comprehensive data collection approach using a standardized electronic evaluation form, which enhances the reliability and validity of data on medical conditions and patient demographics. The focus on the Hajj pilgrimage provides a unique context, offering insights into the health needs of a diverse patient population and the effectiveness of the medical convoy system. Additionally, the study assesses the quality of care provided, which can inform healthcare improvements, training, and resource allocation during the Hajj. The findings may also guide policy decisions to enhance healthcare coordination and identify service gaps. However, the study's retrospective design limits causal inferences between patient characteristics and health outcomes. The focus on patients transferred by the medical convoy may introduce selection bias, affecting generalizability. The accuracy of data relies on thorough documentation by healthcare workers, and any inaccuracies could impact the findings' reliability. The diverse range of medical conditions presented complicates the assessment of care quality, requiring nuanced analysis. Additionally, the lack of data on other sociodemographic characteristics may affect the interpretation of disease incidence, and patient-reported comorbidity data may be subject to report and recall bias. Finally, conducting research during the Hajj, with high patient loads and limited resources, poses challenges for data collection and participant engagement. While the sample of patients in this study consisted of those requiring medical transfer due to specific health conditions during the Hajj season, we acknowledge that this group may not be fully representative of the general population of pilgrims. The patient sample likely overrepresented older adults, who are more likely to experience health complications during the pilgrimage. Additionally, factors such as socioeconomic status, which could influence access to medical care and health outcomes, were not directly assessed in this study. These limitations in sample representation may introduce a selection bias that affects the generalizability of our findings to the entire population of pilgrims. To clarify this, we have added a discussion on the potential impact of sample bias and have highlighted the need for future research that incorporates a more comprehensive demographic profile of all pilgrims to better understand the health needs and care outcomes of this diverse group. Overall, the strengths and limitations should be considered in interpreting the results.
Conclusion
This study offers valuable insights into the demographic diversity, comorbidities, transfer characteristics, and risk factors among patients transferred during the Hajj season, highlighting the complexities of managing high-risk populations during transport. The association between higher RSTP and factors such as older age, arrhythmias, and the need for respiratory support points to the need for targeted risk mitigation strategies. These findings underscore the importance of enhancing transport protocols to improve patient safety and outcomes.
Future recommendations
Based on the findings, several recommendations are proposed. Implementing comprehensive pre-transport assessments that include patients' medical histories, comorbidities, and clinical parameters can help identify those at elevated risk and tailor transport protocols accordingly. Specific monitoring protocols should be established for patients with high-risk features, such as arrhythmias or respiratory support needs, to enable timely interventions during transport. Training healthcare professionals involved in patient transfers to recognize and manage transport-related risks can further improve patient safety. Additionally, refining risk assessment tools like the RSTP to enhance their predictive accuracy and practical use is essential. We also recommend enhancing the medical convoy systems by incorporating comprehensive pre-transfer assessments, advanced training for healthcare teams, and improving communication protocols, including multilingual support. Upgrading equipment and introducing real-time monitoring can further optimize patient care during transport. Moreover, systematic data analysis should be implemented to continuously assess and improve the quality and effectiveness of the medical convoy operations. Continued research into the long-term outcomes of transported patients will provide further insights to guide policy and protocol development. Overall, this study highlights the need for improved patient transport practices and adaptive healthcare strategies to meet the challenges of high-demand periods, such as the Hajj season, ensuring safer and higher-quality care.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the King Fahad Medical City Research Ethics Committee (log number 23-452E). This study was performed in line with the principles of the Declaration of Helsinki. The ethics committee waived the requirement for written informed consent.
Author contributions
GA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AK: Writing – review & editing. LA: Writing – review & editing. JA: Writing – review & editing. AA: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Alqathama AA, Ahmad R. Muslim pilgrims' knowledge, attitudes, and practices regarding complementary and alternative medicine (CAM); a study conducted during Hajj season. Saudi Pharm J. (2024) 32:101988. doi: 10.1016/j.jsps.2024.101988
2. Aldossari M, Aljoudi A, Celentano D. Health issues in the Hajj pilgrimage: a literature review. East Mediterr Health J. (2019) 25:744–53. doi: 10.26719/2019.25.10.744
3. Almehmadi M, Alqahtani JS. Healthcare research in mass religious gatherings and emergency management: a comprehensive narrative review. Healthcare. (2023) 11:244. doi: 10.3390/healthcare11020244
4. Ahmed QA, Memish ZA. Hajj 2022 and the post pandemic mass gathering: epidemiological data and decision making. New Microbes New Infect. (2022) 49–50:101033. doi: 10.1016/j.nmni.2022.101033
5. Moulaei K, Bastaminejad S, Haghdoost A. Health challenges and facilitators of arbaeen pilgrimage: a scoping review. BMC Public Health. (2024) 24:132. doi: 10.1186/s12889-024-17640-9
6. Ahmed QA, Arabi YM, Memish ZA. Health risks at the Hajj. Lancet. (2006) 367:1008–15. doi: 10.1016/S0140-6736(06)68429-8
7. Yezli S, Ehaideb S, Yassin Y, Alotaibi B, Bouchama A. Escalating climate-related health risks for Hajj pilgrims to Mecca. J Travel Med. (2024) 31:taae042. doi: 10.1093/jtm/taae042
8. Yezli S. The threat of meningococcal disease during the Hajj and Umrah mass gatherings: a comprehensive review. Travel Med Infect Dis. (2018) 24:51–8. doi: 10.1016/j.tmaid.2018.05.003
9. Ardiana M, Utami ER, Al Farabi MJ, Azmi Y. The impact of classical cardiovascular risk factors on hospitalization and mortality among Hajj pilgrims. ScientificWorldJournal. (2023) 2023:9037159. doi: 10.1155/2023/9037159
10. Alrashdi MM, Al Thobaity A. Exploring the experiences, motivations, and skillsets of nurse volunteers during Hajj: implications for enhancing volunteer programs. BMC Nurs. (2024) 23:44. doi: 10.1186/s12912-024-01712-7
11. Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: kingdom's vision 2030. J Med Life. (2021) 14:347–54. doi: 10.25122/jml-2021-0070
12. Sindy AI, Baljoon MJ, Zubairi NA, Dhafar KO, Gazzaz ZJ, Deiab BA, et al. Pattern of patients and diseases during mass transit: the day of Arafat experience. Pak J Med Sci. (2015) 31:1099–103. doi: 10.12669/pjms.315.8017
13. Ministry of Health (MOH) Kingdom of Saudi Arabia. MOH Medical Convoy Transports Hospitalized Pilgrims from Madinah to Mount Arafat (2022). Available at: https://www.moh.gov.sa/en/HealthAwareness/Pilgrims_Health/News/Pages/News-2022-07-05-009.aspx (accessed October 11, 2024).
14. Nashwan AJ, Aldosari N, Hendy A. Hajj 2024 heatwave: addressing health risks and safety. Lancet. (2024) 404:427–8. doi: 10.1016/S0140-6736(24)01440-5
15. Alotaibi BM, Yezli S, Bin Saeed AA, Turkestani A, Alawam AH, Bieh KL. Strengthening health security at the Hajj mass gatherings: characteristics of the infectious diseases surveillance systems operational during the 2015 Hajj. J Travel Med. (2017) 24:taw087. doi: 10.1093/jtm/taw087
16. Taibah H, Arlikatti S, Andrew SA, Maghelal P, DelGrosso B. Health information, attitudes and actions at religious venues: evidence from Hajj pilgrims. Int J Disaster Risk Reduct. (2020) 51:101886. doi: 10.1016/j.ijdrr.2020.101886
17. Gosadi IM, BinSaeed A, Al-Hazmi AM, Fadl AA, Alharbi KH, Swarelzahab MM. Evaluation of applied public health emergency system at prince mohammed international airport in Almedinah during Hajj season 2014: a qualitative case study. BMC Res Notes. (2015) 8:435. doi: 10.1186/s13104-015-1415-2
18. Alzahrani F, Kyratsis Y. Emergency nurse disaster preparedness during mass gatherings: a cross-sectional survey of emergency nurses' perceptions in hospitals in Mecca Saudi Arabia. BMJ Open. (2017) 7:e013563. doi: 10.1136/bmjopen-2016-013563
19. Almuzaini Y, Abdulmalek N, Ghallab S, Mushi A, Yassin Y, Yezli S, et al. Adherence of healthcare workers to Saudi management guidelines of heat-related illnesses during Hajj pilgrimage. Int J Environ Res Public Health. (2021) 18:1156. doi: 10.3390/ijerph18031156
20. Alrufaidi KM, Nouh RM, Alkhalaf AA, AlGhamdi NM, Alshehri HZ, Alotaibi AM, et al. Prevalence of emergency cases among pilgrims presenting at king abdulaziz international airport health care center at Hajj terminal, Jeddah. Saudi Arabia during Hajj Season, 1440 H-−2019. Dialogues Health. (2023) 2:100099. doi: 10.1016/j.dialog.2023.100099
21. Khan AA, Sheerah HA, Alamri FA, Alsaleh G, Almuzaini Y, Alahmari AA, et al. Medical convoy: interfacility transfer of hospitalized patients during Hajj season 2019. SJEMed. (2024) 5:182–9. doi: 10.24911/SJEMed.72-1704795659
22. Yezli S, Mushi A, Almuzaini Y, Balkhi B, Yassin Y, Khan A. Prevalence of diabetes and hypertension among Hajj pilgrims: a systematic review. Int J Environ Res Public Health. (2021) 18:1155. doi: 10.3390/ijerph18031155
23. Alzahrani AG, Choudhry AJ, Al Mazroa MA, Turkistani AH, Nouman GS, Memish ZA. Pattern of diseases among visitors to Mina health centers during the Hajj season. (1429) H (2008 G). J Infect Public Health. (2012) 5:22–34. doi: 10.1016/j.jiph.2011.10.003
24. Markakis C, Dalezios M, Chatzicostas C, Chalkiadaki A, Politi K, Agouridakis PJ. Evaluation of a risk score for interhospital transport of critically ill patients. Emerg Med J. (2006) 23:313–7. doi: 10.1136/emj.2005.026435
25. Srithong K, Sindhu S, Wanitkun N, Viwatwongkasem C. Incidence and risk factors of clinical deterioration during inter-facility transfer of critically ill patients; a cohort study. Arch Acad Emerg Med. (2020) 8:e65.
26. Khan ID, Khan SA, Asima B, Hussaini SB, Zakiuddin M, Faisal FA. Morbidity and mortality amongst Indian Hajj pilgrims: a 3-year experience of Indian Hajj medical mission in mass-gathering medicine. J Infect Public Health. (2018) 11:165–70. doi: 10.1016/j.jiph.2017.06.004
27. Madani TA, Ghabrah TM, Albarrak AM, Alhazmi MA, Alazraqi TA, Althaqafi AO, et al. Causes of admission to intensive care units in the Hajj period of the islamic year 1424 (2004). Ann Saudi Med. (2007) 27:101–5. doi: 10.5144/0256-4947.2007.101
28. Razavi S, Ardakani HZ, Rajai S, Hollisaz M, Sadeghipoor H, Farshad A, et al. Trends in prevalent injuries among Iranian pilgrims in Hajj. Iran J Public Health. (2011) 40:110–5.
Keywords: Hajj, medical convoy, patient transfer, Risk Score for Transported Patients (RSTP), pilgrimage healthcare, Saudi Arabia, healthcare challenges
Citation: Alsaleh G, Khan A, Alabdulatif L, Alhazmi J and Althobaiti A (2025) Quality of care and challenges in medical convoy transfers during Hajj season 2023: a cross-sectional study. Front. Disaster Emerg. Med. 3:1534361. doi: 10.3389/femer.2025.1534361
Received: 25 November 2024; Accepted: 17 January 2025;
Published: 25 February 2025.
Edited by:
Doğaç Niyazi Özüçelik, Istanbul University-Cerrahpasa, TürkiyeReviewed by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeTamorish Kole, University of South Wales, United Kingdom
Copyright © 2025 Alsaleh, Khan, Alabdulatif, Alhazmi and Althobaiti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ghadah Alsaleh, R2hhbHNhbGVoQG1vaC5nb3Yuc2E=
 Ghadah Alsaleh
Ghadah Alsaleh Anas Khan
Anas Khan Lamis Alabdulatif
Lamis Alabdulatif Jumana Alhazmi
Jumana Alhazmi