- 1RWTH Aachen University, Faculty of Medicine, Aachen, Germany
- 2Universitatsklinikum Aachen, AcuteCare InnovationHub, Aachen, Germany
Introduction: Providing health care in humanitarian aid missions and conflict settings, such as the ongoing war in Ukraine, presents significant logistical and operational challenges. Telemedicine has emerged as a promising tool to support medical personnel in such environments.
Methods: This study developed a concept for a telemedicine system tailored to humanitarian aid missions. A functioning telemedicine service was implemented and tested under simulated conditions, and its acceptance among medical professionals was assessed through a structured survey.
Results: The survey revealed high levels of interest and acceptance of telemedicine among medical staff, indicating strong potential for practical application. Key barriers and limitations—such as connectivity issues, training needs, and integration challenges—were identified and analyzed.
Conclusions: For effective implementation of telemedicine in humanitarian settings, a detailed needs analysis and close integration with existing health care infrastructure are essential. Strategic recommendations are provided to guide future deployments and improve service delivery in conflict zones.
Introduction
Wars as the current in Ukraine have the potential to create a lasting humanitarian crisis. People are fleeing and no longer have access to public health care (1) as their facilities are also targeted in acts of war. Medical personnel are fleeing, being wounded or being killed (2–9). There are no humanitarian escape corridors, and regular health care for the population cannot be guaranteed due to a lack of material and human resources (6). In the period from the start of the war in February 2022 to the end of that year, 707 attacks on components of the Ukrainian health care system were reported (9). A long-term nationwide shortage in the health system is emerging, which has so far left around 1.5 million people in need of humanitarian health care (1) and will be clearly noticeable for the unforeseeable future. As an important factor in the functioning of a society, the limited availability of the health care system also leads to social destabilization (10).
In light of these challenges, innovative solutions are urgently needed—particularly those that can help maintain or supplement medical services under crisis conditions. One such approach is telemedicine, which has been successfully used in military contexts for several decades (11, 12), but it has also been used to support civilian populations in disaster and war situations (13, 14). In 1985, NASA successfully used modern telecommunications technology to support aid organizations during an earthquake in Mexico City, partially compensating for the collapsed communications infrastructure (13, 15). During the 1988 Armenian earthquake, the U.S. and USSR used the Space Bridge project—originally developed for astronaut telemedicine—to connect local hospitals with counterparts in the U.S. via teleconsultation (13, 16). The U.S. military later applied telemedicine across various specialties—such as radiology, neurosurgery, and dermatology—in both conflicts and civil protection efforts (13, 17).
Beyond military contexts, national studies have shown that the use of telemedicine in emergency services can save scarce physician resources, especially in rural areas (18, 19). Medical expertise can be used remotely to delegate medical interventions to non-medical personnel (18, 19). Despite this great potential, telemedicine is not yet widely used in disaster medicine (20). Initial applications using mobile phones have been tested to guide non-medical personnel in direct patient care and were designed for communication between non-physician and physician medical staff using embed guidelines in addition to the provision of telemedicine (14).
A growing number of humanitarian organizations have also begun to implement telemedicine solutions. For instance, Doctors Without Borders has adopted teleconsultation systems to facilitate physician-to-physician contact in field operations (21, 22). These applications demonstrate that even under extreme conditions, medical support can be delivered remotely.
An illustrative recent example is the conflict in the Gaza Strip, where telemedicine was applied in a low-barrier format using freely accessible messaging platforms, enabling direct physician-to-physician communication in a largely destroyed infrastructure (23).
A critical factor influencing the broader implementation of telemedicine is its cost-effectiveness. Advances in medical and telecommunication technologies have made more portable and affordable solutions widely available (11, 15). While the use of telemedicine in the second half of the 20th century still relied on costly and bulky technology (13), today a smartphone is sufficient to transmit audio and video in real time to almost anywhere in the world at a fraction of the cost. This progress has been helpful for humanitarian aid and civil protection, where the lack of infrastructure requires simple, robust, maintenance-free and fault-tolerant solutions (13). In addition, data security must be ensured, especially when dealing with sensitive patient data. In armed conflicts, there is also the risk of cyber attacks (24) as part of asymmetric warfare.
Given that most existing telemedicine concepts in humanitarian contexts rely on physician-to-physician communication (13, 16, 21–23), this study aims to go one step further. It presents a technical, organizational, and legal telemedicine concept based on an existing application initially developed for civil protection in Germany. While the system has already been evaluated in several simulation studies (14), it is now being adapted for use in actual humanitarian operations in Ukraine.
Methods
Development of a concept
The aim of this project was to develop a telemedicine concept tailored for use in humanitarian aid contexts. To this end, an existing application previously utilized in civil protection scenarios (14) was adapted. The modifications included a reduction in functional complexity to ensure immediate usability without the need for prior training, as well as translation of the interface into English. To facilitate navigation and expedite decision-making, medical queries were categorized into specific domains of expertise. These adaptations were designed to enable use by non-medical personnel in civil protection units, particularly in situations involving non-acute and non-life-threatening medical cases. Use in acute life-threatening situations (e.g., resuscitation) was ruled out, as it would require the implementation of an algorithm-based treatment plan and intensive training for those seeking help.
To ensure data security and mitigate the risk of unauthorized access, the system was secured through multiple measures, including integration with a certified identity provider. The service was designed to be operated by volunteer medical professionals (tele-experts) based in Germany and other European countries (Figure 1).
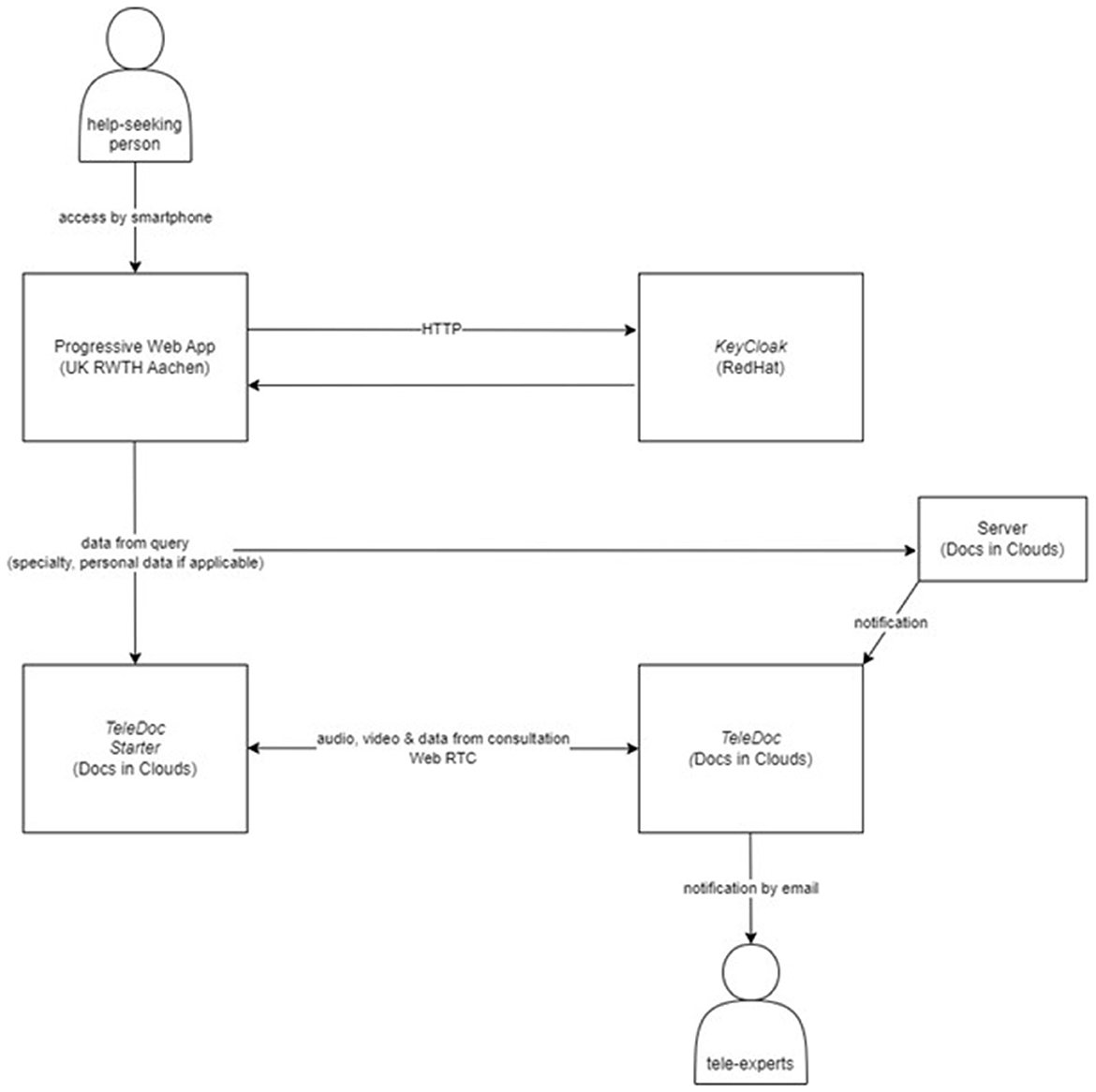
Figure 1. A help-seeker accesses the progressive web application (designed by University Hospital Aachen) via their smartphone. This identifies the person by HTTP using the KeyCloak identity verifier. Data from the query is sent to both the TeleDoc Starter software on the helper side and the tele-experts software (TeleDoc). The tele-experts are notified by e-mail when a consultation is received. The consultation between the help-seeker and the tele-expert is secured by the Web RTC transmission protocol.
To evaluate the acceptance and perceived utility of telemedicine among emergency personnel, several surveys were conducted prior to the project. Participants were asked about their willingness to use telemedicine both in their professional roles and as potential patients.
A feasibility study (n = 11) was carried out during a large-scale event, where a mobile treatment station was established. In this setting, a paramedic trained in the use of telemedical equipment—comprising a tablet, headset, camera, digital devices for measuring vital signs (blood pressure, ECG, and oxygen saturation), and a digital stethoscope—functioned as a “tele-paramedic.” The paramedic received real-time guidance from a remote physician, who provided clinical instructions for triage and treatment.
Building upon the initial findings, a subsequent simulation study (n = 13) further investigated the applicability of telemedicine in a civil protection scenario. During this simulation, ten patients representing various triage categories were managed by multiple response teams within a centralized treatment facility.
The insights obtained from both studies provided the empirical foundation for adapting the telemedicine application to humanitarian aid settings, with an emphasis on operational feasibility, acceptance among users, and integration into existing response structures.
Mission in Ukraine
Project outreach in Ukraine commenced in September 2022, with promotional materials distributed via English-language flyers disseminated through communication channels of various international and local humanitarian aid organizations. Initial contact with these organizations was established via email. In November 2022, promotional efforts were expanded to include smaller, local associations and grassroots initiatives. By March 2023, a Ukrainian-language version of the flier was circulated in multiple cities across the country to further increase visibility and accessibility.
Stakeholder survey
Complementary to the acceptance surveys among end users, a stakeholder survey was designed to assess the usability and perceived value of the telemedicine concept from the perspective of local providers. The aim was to gather feedback to inform real-time adjustments during implementation and support the design of future telemedicine initiatives in similar contexts.
An online search was conducted to identify telemedicine providers actively operating in Ukraine at the time of the study. Relevant stakeholders—including IT professionals and medical personnel—were contacted via email and invited to complete an online questionnaire. Inclusion criteria stipulated that participants must have been involved in the delivery or support of telemedicine services during the survey period.
The survey was administered via SosciSurvey (SosciSurvey GmbH, Munich, Germany) and collected demographic data alongside information on any direct involvement in Ukraine-based deployments or consultations. Respondents were asked to evaluate a series of statements regarding telemedicine use, technical infrastructure, and organizational structures. Responses were recorded using a 5-point Likert scale ranging from “strongly agree” to “strongly disagree,” with an additional option for “no answer.” The data collection period spanned from July to October 2023.
Outcome parameters
The primary outcome of the project was defined as the successful development of a telemedical concept that met the aforementioned functional and operational criteria. As a secondary endpoint, the identification of practical challenges and areas of opportunity was derived from stakeholder evaluations regarding the relevance and feasibility of telemedicine in the context of humanitarian aid delivery.
Statistical analysis
IBM SPSS Statistics version 29.0.0.0 (241) (IBM Corp., Armonk, NY, USA) was used for descriptive statistical analysis and data visualization.
Ethics
The studies were approved by the Ethics Committee of the University Hospital RWTH Aachen (file numbers EK 22-134 and EK 23-233).
Results
Development of a concept
During the adaptation of the “TeleDoc Starter” software (Docs in Cloud TeleCare GmbH, Aachen, Germany) for deployment in international civil protection and humanitarian aid contexts, several key adjustments were made to address the specific needs of users operating in resource-limited and high-stress environments. The system's functionality was deliberately reduced and simplified to ensure that it could be operated by the help-seekers intuitively without prior training.
To ensure accessibility for maximum number of users, English was implemented as the system language. In addition, platform independence was prioritized to allow access from a wide variety of devices. A Progressive Web Application (PWA) was therefore selected, as it eliminates the need for installation and functions across different operating systems. This decision was made to meet the device heterogeneity in the field, especially when systems are accessed by volunteers or local responders using personal devices.
Security considerations played a central role throughout the adaptation process. While the front-end application for field users was designed to be lightweight and easy to access, a Windows-based interface was retained for medical personnel (tele-experts) to ensure compliance with data protection standards. Mechanisms for user authentication and misuse prevention were integrated, including an OpenID Connect-based identity provider (KeyCloak from RedHat Inc, Raleigh, USA) and the option to block new user access in the event of misuse. These additions were made in response to identified risks of cyber attacks in humanitarian operations, particularly in conflict zones.
Furthermore, all components were reviewed for compliance with relevant legal frameworks, including the General Data Protection Regulation (GDPR) and national regulations for telemedical consultations (e.g., §365 (1) SGB V in Germany). This ensured legal deployability of the solution in European-supported humanitarian missions.
Overall, the adaptation process highlighted that telemedicine systems require targeted modifications when transitioning to humanitarian use. Key observations included the need for simplification, legal and linguistic localization, enhanced platform flexibility, and built-in data protection—elements that are essential for safe and effective deployment in disaster and emergency settings.
Acceptance studies
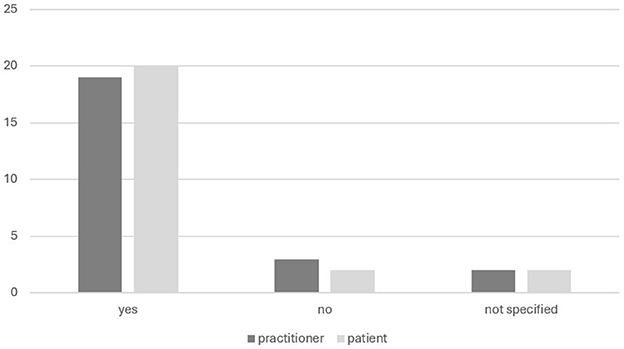
In total, 24 participants from the two associated studies were interviewed to assess their acceptance of telemedicine. The interviews focused on their willingness to engage with telemedical services both as healthcare practitioner and as patient (Figure 2). Willingness to use was high among participants, with 79% (19/24) endorsing its use as practitioners and 83% (20/24) as patients.
Mission in Ukraine
World Health Organization (WHO), International Committee of the Red Cross (ICRC), and Ukrainian Red Cross (URC) were chosen as global/local aid organizations. The Ukrainian-language flyers were translated by native speakers in Germany and distributed by local partners in hospitals in Kiev, Pavlograd, Petropavlivka, and Dnipro.
At this time, the telemedicine system was active and available for use in the field.
Regarding usage patterns, no telemedical consultations were conducted between July 2022 and July 2023. Only a single secondary contact occurred during this period, in which technical expertise was provided to address a question within a highly specialized medical context.
Throughout the period, no technical difficulties were encountered, and simulated consultations proceeded smoothly and without interruption. The system was paused after July 2023. Technically, it could be reactivated at any time, but volunteer tele-experts would first have to be recruited again.
Stakeholder survey
The survey was conducted by 34 respondents, 28 of whom completed the survey in full. A total of 33 respondents indicated their occupation: 57.6%/19 were physicians, 3%/1 chemists, 3%/1 biologists, 18.2%/6 IT specialists, and 18.2%/6 “other.” For better differentiation, respondents were also asked whether they completed the survey as a private individual (82.4%/28) or as a company representative (17.6%/6). The average company size was 1,306 (30–4,500) employees.
Of the 31 responses, 26 (84.4%) were of German nationality, with other nationalities including French, Dutch, Romanian, and Ukrainian (one respondent each). Among the respondents, 12 (35.3%) had been in Ukraine since the beginning of the war in 2022. Of those who had been there, 5 (38.5%) said that they had worked as a physician, another 5 (38.5%) as a civil protection/humanitarian aid worker, 2 (15.4%) as an IT specialist, 2 (15.4%) as a provider of telemedicine solutions, and 2 (15.4%) as a private individual. Multiple responses were possible.
Teleconsultations in Ukraine were conducted by 29.4% of the respondents. These consultations were conducted by third parties using telemedicine platforms other than the system developed in this project. The number of consultations of these respondents varied considerably, ranging from 1 to 175,000. The reported usage data was not linked to a specific period. Among those who actively conducted teleconsultations, the communication formats used included telephone calls (88.9%), e-mail (77.8%), chat (44.4%), and video consultations (88.9%). Multiple formats could be selected.
The primary reasons cited for initiating telemedical contact were the provision of basic or routine care (66.7%), physician-to-physician consultation (22.2%), and other unspecified purposes (11.1%). Notably, none of the respondents selected “acute/emergency care” as a reason for telemedical use.
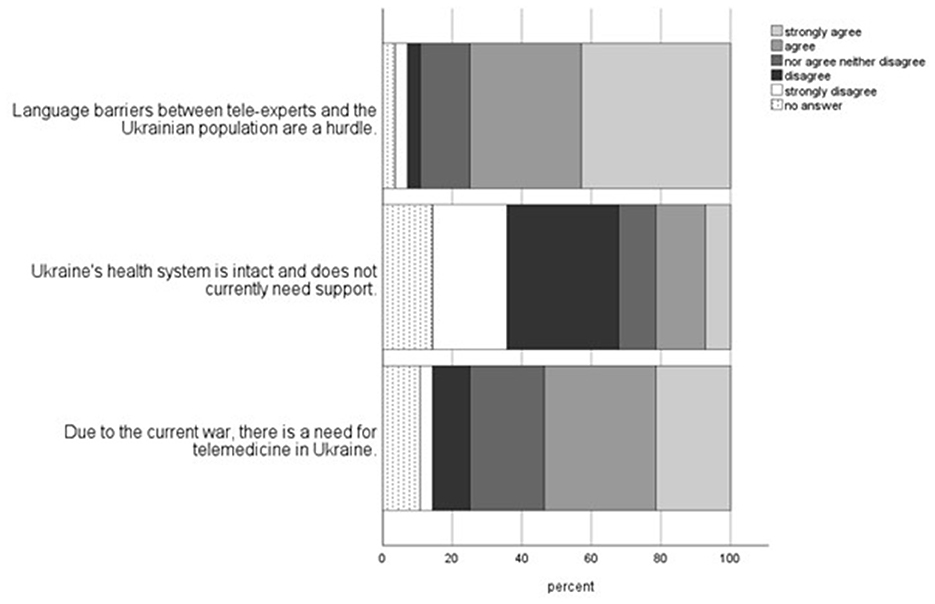
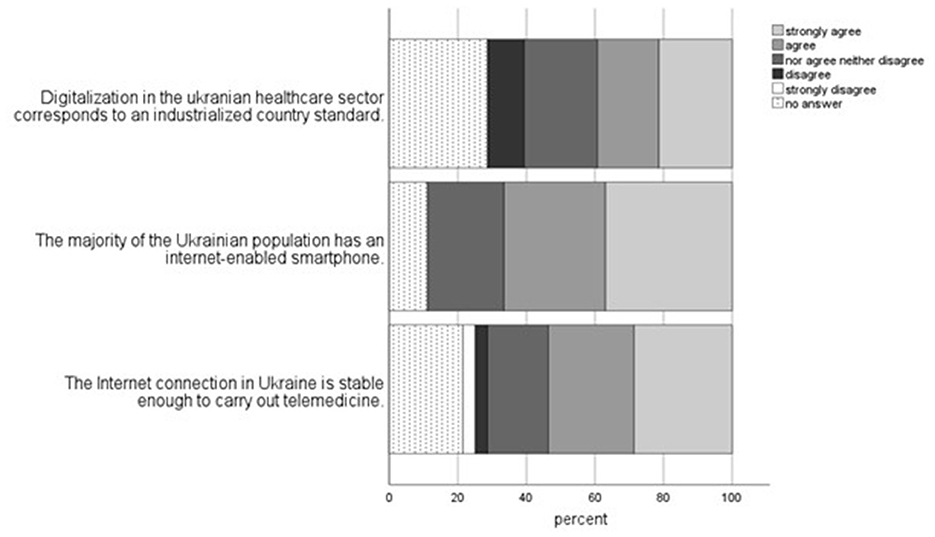
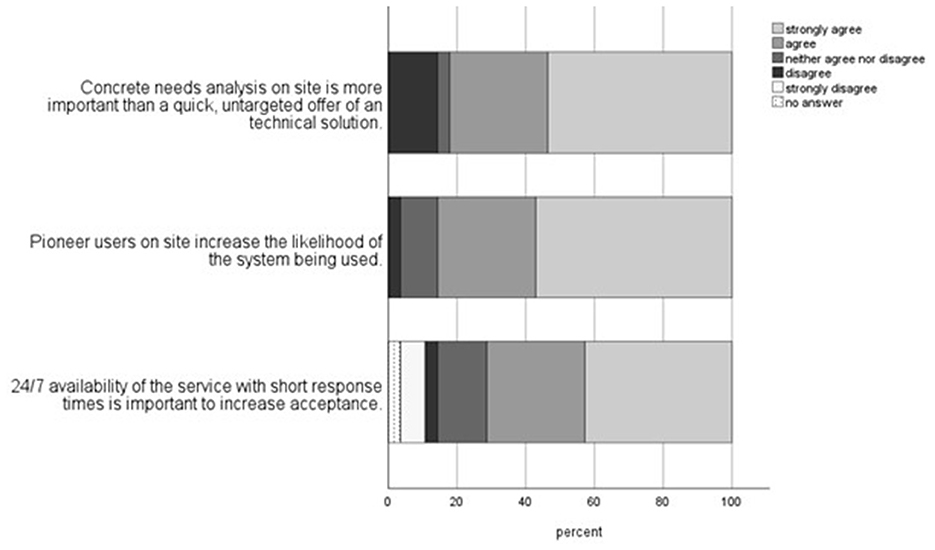
The final topics of telemedicine, technical requirements, and organization were answered by 28 of the 34 respondents (Figures 3–5).
Discussion
A concept of a telemedicine solution to serve in a humanitarian aid mission was successfully developed and evaluated in several acceptance studies. Specific challenges could be identified in a stakeholder survey. A mission in Ukraine did not lead to consultations through the developed system but existing providers successfully offer telemedicine services in Ukraine, especially for basic medical care.
Development of a concept
Providing another physician-to-physician solution did not seem to make much sense given the existing services (13, 16, 21, 22). Focusing on improved collaboration between non-physician and physician medical staff seems more sustainable given the staff shortages. Relevant studies on this interprofessional consultation format have already demonstrated the savings potential of these personnel resources (18, 19). Humanitarian aid could benefit particularly from these savings as it is confronted with a shortage both of personnel and materials.
Acceptance studies
Acceptance of telemedicine by health care professionals and patients has been examined in many ways in our acceptance studies. In the studies presented here (feasibility and simulation study), there was a high willingness to use telemedicine both as medical staff and as a patient after getting to know the application (Figure 2). This suggests that face-to-face contact with telemedicine is critical for trust and acceptance of the technology and thus for its effective use, and that there is an opportunity for improvement by consistently bringing technology and potential users together. Other studies have concluded that although telemedicine has the potential to be used effectively in disaster situations, its use has been very limited (20). This integration must not only take place in the context of telemedicine for civil protection but should also be integrated as multi-dimensionally as possible into everyday areas of medical and non-medical patient care.
Mission in Ukraine
The flier advertising format was the easiest to implement due to the distance between western Europe and Ukraine. Due to the lack of our own communication channels and in order to take advantage of synergies, known and functioning channels of aid organizations were used. Although the system was operational and accessible there were no consultations through the developed system and only one contact by e-mail to provide technical expertise. As no immediate or explicit reasons for the system's non-utilization could be identified during its active phase, a stakeholder survey was initiated in order to gather relevant insights and make them available for the planning and implementation of future similar projects.
Stakeholder survey
The language of counseling was set as English in advance. This could lead to a language barrier for people seeking help from Ukraine but is unavoidable in a setting with volunteers from Germany, as it cannot be assumed that there is a relevant proportion of Ukrainian speakers. Most respondents in the stakeholder survey agreed that the language barrier was a hurdle. One possible improvement here would be the use of free translation applications, as these are already available and would not need to be implemented in a separate program at great expense.
As most of the staff are planned to be volunteers, it is a challenge to provide 24/7 coverage of the telemedicine service with short response times. Depending on the volume of requests, there may be delays in acceptance due to the number of tele-experts recruited. In order to provide a reliable point of contact for those seeking help locally, a response time should be guaranteed within fixed time frames (e.g., Mon-Fri 8–16 h, Sat and Sun 8–20 h) and communicated in advertising. Although implementing a shift model with clearly defined responsibilities would entail greater organizational effort, it should be considered essential, as reliable availability for those seeking help is a fundamental requirement. Most (71.4%) of the respondents to the stakeholder survey shared the need for 24/7 availability with short response times. The number of staff should thus be increased.
The large disparity in the number of reported contacts among surveyed telemedicine providers is likely due to the longstanding presence of certain providers in Ukraine, who became widely recognized during the COVID-19 pandemic. This established visibility has led to sustained high consultation volumes since February 2022. This confirms the assumption that stable demand can be achieved with sufficient awareness and numerous pioneer users. The results from the telemedicine and organization topics are consistent with this: most respondents assumed a need for telemedicine in Ukraine and considered local pioneer users important for a more likely use of telemedicine applications.
The presence of these pioneer users, 24/7 availability of the telemedicine service, and a concrete needs analysis on site were not consistently implemented in the design of our telemedicine service and contributed to the non-use of the system. Coordination with existing local projects, for example, could have created synergies and would have been more effective. This conclusion is supported by the assumption of Chelsom et al. (25) that telemedicine should be integrated into local processes to be used effectively.
The types of formats used—telephone, e-mail, chat, and video consultation—are consistent with the apparently good network coverage and availability of smartphones and other modern communication media in Ukraine. Tsiatsikas et al. (24) point out that combat operations are often accompanied by local cyber-attacks and network outages. A shift to less data-intensive chat and e-mail formats would have been expected in the event of large-scale, prolonged network outages. The results of the survey on the technical requirements for Internet connection stability and the widespread availability of Internet-enabled smartphones in Ukraine are consistent with this.
The fact that the telemedicine contacts were not used for acute/emergency care confirms the assumption according to which the system described in this thesis should be operated. Providing acute/emergency care support would require more intensive training for both the tele-experts and those seeking help, as well as defined standard operating procedures.
The acceptance studies and stakeholder surveys showed that telemedicine is accepted and has the potential to make a decisive contribution to the medical care of the population in humanitarian aid scenarios. Its performance depends directly on technical and organizational challenges that should be addressed in advance by a holistic approach (needs analysis, system availability, pioneer users on site, low threshold, and embedding in existing systems).
The absence of actual consultations, despite targeted and multidimensional dissemination strategies, suggests that the current need for further international telemedicine support may be limited. One possible explanation is that the Ukrainian healthcare system continues to function with sufficient capacity to meet local needs without external assistance. It must also be considered that factors such as lack of awareness, or language barriers may have contributed to the system's non-utilization.
However, this contradicts the results of our stakeholder survey in which only 21.4% of the respondents rated the Ukrainian health care system as intact and not in need of external support. However, Ukraine's digital infrastructure expanded significantly over the past decade: a national eHealth system has been operational since 2017 and provides a nationwide exchange platform for the medical sector (25, 26).
A WHO study examined the availability of primary care in Ukraine in the first 6 months after the start of the war. Most respondents reported being able to see their general practitioner in person, 81% were able to reach them by telephone, 31% by messenger service, and 22% by online consultations (27). Only 7% said they had no access to primary care (27). These results show that, despite the state of war, most of the population still has access to primary care and that there are many channels available for this purpose. This study concluded that the Ukrainian health care system has remained resilient and that access to health care remains fundamentally at a high level (27).
Gostin and Rubenstein (27), on the other hand, concluded that access to health care in Ukraine was significantly restricted or threatened by the war and the resulting attacks on the health care system (6). These sometimes-contradictory findings indicate that the situation is volatile and can vary significantly depending on the time and place studied. In contrast to the WHO study, only 39.3% of the respondents to the stakeholder survey believed that the level of digitalization in the Ukrainian health care system was at the level of an industrialized country. The reasons for this discrepancy could be prejudices against a supposedly “backward” Eastern European post-Soviet region, but also the subjectively better and more modern health care system in the Western world. This assessment must be viewed critically in relation to Germany, which was ranked only 16th out of 17 industrialized countries in a benchmarking study (Digital Health Index) (28).
Of course, a digital system is always a target for new forms of warfare. Concerns about data security may also have led to the system not being used. Location data and information about the wounded could be intercepted and used by the enemy. In view of these data, the need for additional external help from abroad with a telemedicine system that is initially unknown to the users is not necessarily given in this setting.
Limitations and outlook
The effectiveness of the adaptations made to the application for use in international civil protection and humanitarian aid could not be assessed, as the system was not deployed in field.
The acceptance studies were only carried out in a simulated scenario and only in Germany. This may introduce a bias. It is not possible to measure whether the advertising of our system was targeted in Ukraine. Targeted advertising through social media could be an approach to better control advertising here. The very heterogeneous group of respondents in the stakeholder survey makes it difficult to generalize the statements made and the insights gained from the stakeholder survey regarding the system's non-use are not conclusive. The opinions of military experts and actors in the Ukrainian health sector could provide further clarity here. In the future, such systems for telemedicine-supported humanitarian aid must be offered in addition to other services provided by aid organizations in the field. In this way, local structures and contacts can be used to raise awareness and to identify operational obstacles in a timely manner.
Conclusion
Based on a telemedicine application for civil protection, this project developed and evaluated a simplified telemedicine concept intended to support civil protection and humanitarian health operations by connecting international medical experts with local responders. The development process focused on usability, security, and adaptability, resulting in a low-threshold system designed for deployment in resource-constrained and high-stress environments. Under simulated conditions, the system functioned reliably, and no technical difficulties were encountered during testing.
However, despite these promising technical results, the system was not utilized in actual field operations during the pilot phase in Ukraine. As such, the concept remains untested under real-world humanitarian conditions. While stakeholder surveys indicated a generally positive attitude toward the system, the lack of real-life use underscores important challenges related to integration, visibility, and acceptance in complex operational environments. Further qualitative research is necessary to gain a deeper understanding of the contextual and organizational barriers to adoption.
Consequently, while the results support the conceptual and technical feasibility of the system under simulated scenarios, claims about its operational readiness should be made with caution. The findings highlight that digital health tools may face significant implementation barriers if not sufficiently embedded in existing local response structures and workflows.
Nonetheless, this work contributes valuable insights into the design and adaptation of telemedicine systems for humanitarian contexts. It underscores the importance of iterative development, early stakeholder engagement, and thorough needs assessments. Despite these challenges, the feasibility of telemedicine-based humanitarian aid on an international scale remains evident.
The system has potential for future application in both international crisis settings and national civil protection scenarios, such as in Germany. Real-world testing and continuous adaptation will be essential to fully realize this potential.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the University Hospital RWTH Aachen (file numbers EK 22-134 and EK 23-233). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
FH: Conceptualization, Data curation, Formal analysis, Resources, Visualization, Writing – original draft. AM: Conceptualization, Data curation, Writing – review & editing. JK: Conceptualization, Data curation, Writing – review & editing. RR: Resources, Supervision, Writing – review & editing. MC: Conceptualization, Data curation, Resources, Supervision, Writing – review & editing. AF: Conceptualization, Data curation, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The development of the original application, which was subsequently adapted for our purposes within the scope of our project, was funded by the Bundesamt für Bevölkerungsschutz und Katastrophenhilfe under grant ID 41201/425.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PWA, progressive web application; WebRTC, web real time communication; GDPR, general data protection regulation; WHO, World Health Organization; ICRC, International Committee of the Red Cross; URC, Ukrainian Red Cross; CBRN, chemical, biological, radiological, nuclear; DGKM, German Society for Disaster Medicine; ECG, electrocardiogram.
References
1. Devi S. Russia-Ukraine tensions hampering health-care access. Lancet. (2021) 398:2222. doi: 10.1016/S0140-6736(21)02791-4
2. Druce P, Bogatyreva E, Siem FF, Gates S, Kaade H, Sundby J, et al. Approaches to protect and maintain health care services in armed conflict - meeting SDGs 3 and 16. Confl Health. (2019) 13:2. doi: 10.1186/s13031-019-0186-0
3. Fouad FM, Sparrow A, Tarakji A, Alameddine M, El-Jardali F, Coutts AP, et al. Health workers and the weaponisation of health care in Syria: a preliminary inquiry for The Lancet-American University of Beirut Commission on Syria. Lancet. (2017) 390:2516–26. doi: 10.1016/S0140-6736(17)30741-9
4. MSF-Germany. Medizinische Nothilfe im Kreuzfeuer (2017). Available online at: https://www.aerzte-ohne-grenzen.de/sites/default/files/2021-01/2017_mcuf_broschure_final.pdf (Accessed January 10, 2025).
5. Siem FF. Leaving them behind healthcare services in situations of armed conflict. Tidsskr Nor Laegeforen. (2017) 137. doi: 10.4045/tidsskr.17.0524
6. Gostin LO, Rubenstein LS. Attacks on Health Care in the War in Ukraine: International Law and the Need for Accountability. JAMA. (2022) 327:1541–2. doi: 10.1001/jama.2022.6045
7. Jain N, Prasad S, Bordeniuc A, Tanasov A, Shirinskaya AV, Béla B, et al. European Countries Step-up Humanitarian and Medical Assistance to Ukraine as the Conflict Continues. J Prim Care Community Health. (2022) 13:21501319221095358. doi: 10.1177/21501319221095358
8. ICRC. ICRC institutional Health Care in Danger strategy 2020–2022: Protecting Health Care from Violence and Attacks in Situations of Armed Conflict and Other Emergencies (2020).
9. Destruction and Devastation: One Year of Russia's Assault on Ukraine's Health Care System (2023). [press release].
10. Nott E. Ukraine invasion: why I fear for Ukraine's healthcare workers. BMJ. (2022) 376:o605. doi: 10.1136/bmj.o605
11. Weymouth W, Thaut L, Olson N. Point of view telemedicine at point of care. Cureus. (2018) 10:e3662. doi: 10.7759/cureus.3662
12. Meyer F. Funkärztliche Beratung an Bord: Medizinische Unterstützung aus der Heimat. Rettungsdienst (2023) 2:145–7.
13. Garshnek V, Burkle FM Jr. Applications of telemedicine and telecommunications to disaster medicine: historical and future perspectives. J Am Med Inform Assoc. (1999) 6:26–37. doi: 10.1136/jamia.1999.0060026
14. Müller A, Kraus S, Arimond R, Kunczik J, Rossaint R, Czaplik M, et al. Telemedicine in civil protection: a controlled simulation study for the analysis of patient care. Digit Health. (2024) 10:20552076241272662. doi: 10.1177/20552076241272662
15. Andrew T, Simpson CRD, Garber SJ. A Brief History of NASA's Contributions to Telemedicine (2020). Available online at: https://history.nasa.gov/NASAtelemedicine-briefhistory.pdf (Accessed January 10, 2025).
16. Nicogossian AE, Doarn CR. Armenia 1988 earthquake and telemedicine: lessons learned and forgotten. Telemed E-Health. (2011) 17:741–5. doi: 10.1089/tmj.2011.0118
17. Hwang JS, Lappan CM, Sperling LC, Meyerle JH. Utilization of telemedicine in the US military in a deployed setting. Mil Med. (2014) 179:1347–53. doi: 10.7205/MILMED-D-14-00115
18. Follmann A, Schröder H, Neff G, Rossaint R, Hirsch F, Felzen M. When emergency physician and tele-emergency physician save life together: a case description on the application of prehospital telemedicine for ventricular tachycardia with hemodynamic instability. Anaesthesist. (2021) 70:34–9. doi: 10.1007/s00101-020-00872-w
19. Schröder H, Beckers SK, Ogrodzki K, Borgs C, Ziemann S, Follmann A, et al. Tele-EMS physicians improve life-threatening conditions during prehospital emergency missions. Sci Rep. (2021) 11:14366. doi: 10.1038/s41598-021-93287-5
20. Latifi R, Tilley EH. Telemedicine for disaster management: can it transform chaos into an organized, structured care from the distance? Am J Disaster Med. (2014) 9:25–37. doi: 10.5055/ajdm.2014.0139
21. Walji M. Bringing telehealth to humanitarian settings. CMAJ. (2015) 187:E123–e4. doi: 10.1503/cmaj.109-4987
22. MSF-Canada. 'It's about Capacity Building': MSF's Telemedicine Program Brings Advanced Care to Places Where Specialists Can't Always Go (2021). Available online at: https://www.doctorswithoutborders.ca/article/its-about-capacity-building-msfs-telemedicine-program-brings-advanced-care-places-where (Accessed April 22, 2025).
23. Alser K, Mallah SI, El-Oun YRA, Ghayada M, Sammour AA, Gilbert M, et al. Trauma care supported through a global telemedicine initiative during the 2023-24 military assault on the Gaza Strip, occupied Palestinian territory: a case series. Lancet. (2024) 404:874–86. doi: 10.1016/S0140-6736(24)01170-X
24. Tsiatsikas Z, Karopoulos G, Kambourakis G, editors. The Effects of the Russo-Ukrainian War on Network Infrastructures through the Lens of BGP. Cham, Switzerland: Springer International Publishing (2023). doi: 10.1007/978-3-031-25460-4_5
25. Chelsom JJL, Bartnaes CG, Roudsari A. Ukraine - Rural Health and Telemedicine: Telemedicine Implementation Handbook (2020).
26. Gordiichuk P, Kliusov O, Gordiichuk M, Kondratenko A, Ponomarova O, Grushynska T, et al. A view on the problem of providing oncological aid during the war in Ukraine. Contemp Oncol. (2022) 26:191–5. doi: 10.5114/wo.2022.120442
27. The WHO Regional Office for Europe. Health Needs Assessment of the Adult Population in Ukraine: Survey Report: December 2022 (2023). Available online at: https://www.who.int/europe/publications/i/item/WHO-EURO-2023-6904-46670-68538 (Accessed January 10, 2025).
Keywords: telemedicine, tele-paramedic, humanitarian aid, civil protection, Ukraine
Citation: Habers F, Müller A, Kunczik J, Rossaint R, Czaplik M and Follmann A (2025) Telemedicine in humanitarian aid: evaluation of potentials and challenges and an implementation trial in Ukraine. Front. Disaster Emerg. Med. 3:1718877. doi: 10.3389/femer.2025.1718877
Received: 04 October 2025; Accepted: 30 October 2025;
Published: 20 November 2025.
Edited by:
Alexander Muench, University Children's Hospital Tübingen, GermanyReviewed by:
Luca Fontana, World Health Organization, SwitzerlandTina Werringloer, University of Tübingen, Germany
Copyright © 2025 Habers, Müller, Kunczik, Rossaint, Czaplik and Follmann. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Florian Habers, Zmxvcmlhbi5oYWJlcnNAcnd0aC1hYWNoZW4uZGU=
 Florian Habers
Florian Habers Anna Müller2
Anna Müller2 Michael Czaplik
Michael Czaplik Andreas Follmann
Andreas Follmann