Abstract
Introduction:
The Introduction, Situation, Background, Assessment, and Recommendation (ISBAR) approach to clinical handovers assists healthcare providers in sharing information about patients within clinical teams and across health sectors while reducing information gaps and medical errors. However, despite its significance, uncertainties remain about the clear outcomes of applying ISBAR and training, especially in settings managing COVID-19 and those not dealing with the pandemic.
Methods:
This review was conducted following the PRISMA guidelines. All the selected articles underwent a progressive check for bias and validity using GRADEpro GDT and RoB-2 as per Cochrane guidelines. This review utilized a meta-analysis of 29 studies and a critical narrative review of seminal articles to condense the non-numerical findings. All articles were checked for heterogeneity with the I2 coefficient. The extracted effect size was the common language effect size (CLES), with 95% confidence intervals.
Results:
ISBAR strengthens communication skills in clinical teams, increases self-confidence and efficacy among healthcare practitioners, improves interprofessional communication, reduces medical errors, and enhances patient safety.
Conclusions:
Our systematic review confirms that ISBAR handover improved the quality of care during the COVID-19 pandemic and non-COVID clinical practice. The limitation of this study is related to the lack of randomized controlled trials and blinding. Almost all studies were cross-sectional, which only provides information regarding associations but not causation.
Introduction
Coronavirus disease (COVID-19), caused by the SARS-CoV-2 virus, typically results in moderate to severe respiratory illness in most people infected with this virus, who recover without requiring special care. However, certain individuals may develop a severe infection and require medical attention. Older adults and those with underlying health conditions—such as cancer, diabetes, cardiovascular disease, or chronic respiratory disorders—are more likely to experience severe illness when infected. Additionally, COVID-19 can infect people of any age (1). The COVID-19 cases in the UK have followed the global pandemic's trend—there have been 20,629,892 cases since the pandemic was declared in the UK in 2020, with 5,911 admissions in a week and 981,596 people hospitalized as of 27 February 2023 (2). The pandemic also impacted all surgical and medical specialties. Hospitalization and intensive care are required for moderate to severe cases, including non-invasive and invasive ventilation, antipyretics, antivirals, antibiotics, and steroids (3). During a COVID-19 emergency, the clinical teams working with the patient must coordinate their handovers to develop a unified strategy for a pathology affecting multiple organs (3).
Clinical handovers (CHs) involve transferring, whether temporarily or permanently, professional accountability and responsibility for part or all of a patient's or group of patients' care to another individual, family member, legal guardian, or professional organization through verbal, written, or electronic exchanges of patient information and duty among healthcare providers (HCPs) (4, 5). CHs include verbal, face-to-face, written, email, video, or electronic notes on a patient's current clinical conditions, treatment plans, and any assessment and clinical results produced by the professionals developing the handovers (4, 5). A handover involves transferring accountability from the sender to the receiver to reduce confusion about patients' conditions. It clarifies the patients' current state, presentation, diagnosis, and treatment and explains the necessary care management in a specific context and setting through verbal or electronic communication (6). During handovers, data and information about a patient are shared among caregivers, within a team of caregivers, and between the hospital and the patient's family or the patient himself (5).
In more detail, CHs involve transferring responsibility for assessment and treatment, sharing information about clinical conditions, and reviewing patient cases. This process enables continuity of care, shared care plans, and the transfer of duties for patient care and assessment to another team member or different teams to whom the handover is directed or who have equal responsibility for the patient (7–9). In hospitals, handovers usually happen after a shift (in the UK, there are about three handovers each day on average) (7) Thus, CHs (or “clinical handoffs” in the USA) are the temporary (e.g., daily clinical notes, patient progress, and liaison assessment) or final (e.g., discharge from hospital and referral to another team or structure) transfer of information and responsibility for care to another professional team member or group from a different setting, hospital, or community (10). CHs are conducted in various ways during routine daily practice: (a) during verbal handovers, healthcare professionals discuss patients; (b) occasionally, nurses talk about patients while reading notes from family members about the patient's presentation, assessment, or clinical conditions; (c) sometimes, handovers occur at the patient's bedside so that the patient's current presentation, symptoms, and conditions can help fill out the necessary information during CHs (10).
Information refers to any data communicated between people via a shared system of representations, symbols, or behavior (11). The main information communicated during handovers is clinical data about patients. Despite the importance of structured communication through CHs, between 25% and 40% of adverse patient care events, 27% of instances of medical misconduct, and over 70% of warning clinical occurrences are caused by breakdowns in verbal and written CHs regarding patients and among healthcare personnel (12). A review of about 23,000 medical malpractice cases found that over 7,000 cases—nearly 2,000 avoidable deaths and 80% of serious medical errors—were connected to caregiver miscommunication during patient handovers (13). Based on research analyzing 16,165 electronic records in Michigan, interprofessional communication has notable flaws, such as missing essential messages, omitted communication goals, distorted physical or temporal message contexts, absent key participants, and unclear or lost information (14).
Interprofessional communication can be either synchronous or asynchronous; synchronous channels include meetings, ward rounds, handoffs, and spontaneous conversations (
15). Asynchronous communication and CHs may also happen through prescription orders, written progress reports, computerized patient notes, and whiteboards (
15). The four or five steps of patient CHs form the basis for the situation, background, assessment, and suggestion (SBAR) approach and its variations, which include Introduction, Situation, Background, Assessment, Recommendation, and Suggestion (ISBARS) and SBAR plus Kindness (K-SBAR) (
16–
19):
- •
An introduction briefly describes the individual or professional providing the evidence; healthcare practitioners (HCPs) who write the handover notes disclose their identity, role, and motivation for creating the document. It also includes biographical data about the patients, such as their name, age, gender, social circumstances, housing, address, ethnic background, and other personal details, such as how the patient came into contact with the healthcare provider providing the handover.
- •
Situation details the patient's condition and summarizes any current issues the team needs to know about; the healthcare providers share and communicate the patient's relevant background information regarding his or her current situation.
- •
Background summarizes the patient's medical and psychiatric history; the HCPs list the significant events that the interprofessional team believes have contributed to the current issue.
- •
Assessment is the clinical evaluation of a patient; healthcare providers share their perspective on the issues, describe what they believe is happening, complete their specialized assessment, and suggest one or more potential solutions.
- •
Recommendation emphasizes what the patient's future care plan should include; the HCPs propose a course of action to address the issue under review and within their area of expertise.
The theoretical framework of this study is based on the Donabedian model, which divides care into three distinct areas: the structure in which care is provided; the process through which interactions between patients and caregivers take place; and the impact of care on the health status of the patient or population, referred to as outcomes (
20,
21). Structure or input measures evaluate the attributes of the service provided, such as promoting data sharing during handovers and ensuring their completeness (
20,
21). Process measures are the parts of the service operation that influence the intended outcome, such as training healthcare providers to ensure proper transfer of patient communication (
20,
21). The impact of the service on patient health outcomes and the extent to which the desired outcomes have been achieved are reflected in outcome measures, such as a reduction in the number of incidents involving missing patient data during handovers (
20,
21).
The primary aim of this systematic review is to comprehensively identify and synthesize salient literature examining the implementation of the Identify, Situation, Background, Assessment, Recommendation (ISBAR) handover protocol within diverse healthcare contexts. This review aims to compare and critically assess the reported outcomes associated with ISBAR adoption, focusing on both clinical effectiveness and the implications for patients’ biopsychological and relational well-being. Specifically, the review evaluates ISBAR's role in enhancing communication accuracy, reducing adverse events, fostering interprofessional collaboration, and improving patient engagement and safety. By integrating quantitative and qualitative findings, the study aims to generate an evidence-informed understanding of how ISBAR contributes to systemic improvements in healthcare delivery and nurtures compassionate, patient-centered care. The review also explores contextual factors influencing ISBAR's efficacy, such as training modalities, setting-specific adaptations, and cultural determinants, with a view to guiding future implementation and policy development.
Methods
Review questions
-
1.
What are the key characteristics and documented outcomes of the SBAR/ISBAR handover framework in both COVID-19 and non-COVID clinical settings? This question aims to identify the structural components, contextual adaptations, and measurable effects of the SBAR/ISBAR protocol across various healthcare environments. Emphasis is on comparing its operational effectiveness in high-stress settings—such as pandemic response units, emergency departments, and ICUs—with routine care settings. The review seeks to evaluate how ISBAR impacts clinical handover accuracy, decision-making processes, interdisciplinary communication, and patient safety. Special attention is paid to differences in outcome reporting, including decreases in adverse events, improvements in workflow continuity, and enhancements in biopsychosocial aspects of patient care during both pandemic and non-pandemic conditions.
-
2.
What are the perceived barriers and enabling factors for implementing the SBAR/ISBAR handover framework in diverse healthcare systems? This question explores the practical and contextual factors that influence the adoption and ongoing use of SBAR/ISBAR. It considers organizational, cultural, and interpersonal challenges such as resistance to change, differences in training effectiveness, hierarchical dynamics, and digital interoperability issues. Facilitators examined include institutional support, integration into professional education, standardization efforts, and leadership backing. The aim is to highlight the complex conditions that either hinder or promote ISBAR's implementation—helping to develop strategies that are culturally adaptable, ethically sound, and resilient during systemic disruptions like public health emergencies.
Inclusion criteria
We selected studies focusing on handovers based on the SBAR/ISBAR framework that are applicable across all clinical settings. The systematic review (SR) included qualitative, quantitative, and mixed-method studies from peer-reviewed journals. We also included policy papers and other reviews on the topic. Additionally, we only used sources published in English or accessible in English. We included policy papers and national guidelines from UK professional regulatory organizations. Studies presenting meta-analyses were excluded. We also considered results from handover training. To broaden our research, we included quantitative, qualitative, and policy papers, as well as policy articles on SBAR/ISBAR in mental and medical settings to expand the review's scope. We used the population, intervention, comparison, outcomes, and settings (PICOS) framework for selection analysis.
Exclusion criteria
We excluded studies on handovers when using the ISBAR framework. We also omitted gray literature, Internet sources, opinion papers, and government reports. Other exclusion criteria included studies where SBAR/ISBAR was only a minor finding and the main focus of the investigation was not on it. Additionally, we excluded other meta-analyses.
Population of interest
This review focused on a population of healthcare professionals (HCPs) at various levels of clinical practice, training, or education. These included physicians, nurses, pharmacists, surgeons, psychiatrists, and allied health professionals such as radiographers and occupational therapists. Eligible individuals were either actively employed in healthcare settings or involved in formal educational programs, ranging from undergraduate coursework to postgraduate clinical training and ongoing professional development.
To be included, studies needed to examine the application or evaluative outcomes of SBAR or ISBAR handover protocols within clinical or educational healthcare settings. Studies were required to involve one or more of the aforementioned professional groups and report empirical findings—whether derived from quantitative, qualitative, or mixed-methods designs—pertaining to communication processes, implementation outcomes, patient safety, or clinical efficacy. Only articles published in peer-reviewed journals and available in full-text English were considered. Relevance to both COVID-19 and non-COVID clinical contexts was also a prerequisite to ensure broader applicability across healthcare conditions.
Conversely, studies were excluded if they involved non-healthcare populations, such as administrative personnel or patient cohorts lacking relevant clinical or communication outcome data. Works that did not explicitly address SBAR/ISBAR frameworks or only mentioned them peripherally without analysis were excluded. Studies lacking outcome data related to handover quality, patient impact, or operational implementation were also omitted. Editorials, opinion pieces, conference abstracts, and gray literature that were not peer-reviewed were considered ineligible, as were publications in languages other than English without available translations.
Interventions
This review included studies that examined the application, training, or knowledge development related to the SBAR/ISBAR communication framework within healthcare settings. Interventions were eligible if conducted in clinical or educational environments under both COVID-19 and non-COVID-19 circumstances. Studies were considered relevant if they involved healthcare professionals or trainees from health services, acute and community care, or other clinical specialties. Eligible research encompassed structured communication programs, simulation exercises, curriculum integration, and protocol use in real-world practice, as long as they provided data on feasibility, impact, or knowledge outcomes.
Studies were excluded if they did not focus on SBAR/ISBAR frameworks as a central intervention or if they lacked empirical evaluation of training, implementation, or communication-related outcomes. Research conducted outside healthcare contexts or involving non-clinical populations was considered irrelevant. Interventions that did not relate to clinical handover or interdisciplinary exchange or those that merely mentioned SBAR/ISBAR without a methodological focus were excluded. Studies not available in English or not peer-reviewed, including opinion pieces, editorials, and conference abstracts, were omitted.
Comparisons
This review included studies that used comparative methods to evaluate the effectiveness, acceptability, and clinical impact of SBAR/ISBAR communication frameworks. Eligible comparisons involved assessing participants' performance before and after receiving structured SBAR/ISBAR training, focusing on changes in handover accuracy, confidence, and communication clarity. Studies were also included if they compared respondent groups based on experience, professional role, or engagement with handover protocols—especially regarding ISBAR usage fidelity and quality. Additional criteria extended to research comparing participant satisfaction before and after implementing clinical handover systems (CHs), as well as comparing clinical outcomes related to SBAR/ISBAR implementation in both COVID-19 and non-COVID-19 healthcare settings.
Studies were excluded if they lacked a clear comparative component or did not report outcome-based contrasts attributable to SBAR/ISBAR interventions. Research that did not involve pre-/post-intervention designs, intergroup comparisons, or assessment of clinical handover efficacy was considered ineligible. Additionally, studies that reported only descriptive or anecdotal accounts without analytical comparison—such as narrative summaries or editorial commentaries—were excluded. Comparative studies conducted in non-healthcare domains or involving tools unrelated to SBAR/ISBAR were also omitted.
Outcomes
Studies were included if they assessed the impact of the ISBAR communication framework on healthcare-related outcomes. Specifically, eligible studies examined ISBAR's effect on nurses' clinical skills and the quality of care provided. Research focusing on carers' confidence, self-efficacy, and readiness to engage in effective handover communication was also included. Studies reporting on interprofessional collaboration and communication improvements among healthcare teams using ISBAR, especially within multidisciplinary settings, were considered relevant. Additionally, investigations evaluating ISBAR's influence on patient safety—including the reduction of adverse events, improvements in handover continuity, and enhanced risk identification—were included, as long as outcomes were empirically measured.
Studies were excluded if they did not evaluate the outcomes of ISBAR implementation or training related to healthcare delivery or professional development. Research lacking empirical data on nursing performance, caregivers' confidence, interprofessional communication, or patient safety was deemed ineligible. Studies that mentioned ISBAR without assessing its impact, as well as those limited to conceptual discussions without reporting outcomes, were excluded. Research conducted outside clinical or educational healthcare settings and publications not peer-reviewed or unavailable in English were also omitted.
Settings
This review included studies conducted in various healthcare and educational settings where SBAR/ISBAR protocols were applied or assessed. Eligible settings included both public and private hospitals, covering primary and secondary care facilities. Studies from academic institutions—such as medical, nursing, and pharmacy schools—were considered, especially when the framework was incorporated into curricula or training simulations. Research from acute and chronic care environments, as well as medical and surgical units, was included. To ensure comprehensive coverage, studies conducted in COVID-19-affected health facilities and those in non-COVID clinical settings were both eligible.
Studies were excluded if they were conducted outside recognized healthcare or health education settings. Research from purely administrative, corporate, or non-clinical environments was deemed ineligible. Studies not relevant to patient care, clinical handovers, or professional training within the specified medical domains were excluded. Additionally, settings unrelated to hospital systems, formal care structures, or health education programs—such as community organizations without clinical components—were omitted.
Types of sources
Data extraction
The Centers for Disease Control and Prevention (CDC) at McMaster University in Canada has guidelines for extracting the following information from selected articles: (1) study details, authors, title, year published, and year of research; (2) place and time; (3) study design; (4) intervention component; (5) description: what is proposed, how it is delivered, who is targeted, where it is delivered; (6) theory described; (7) setting; (8) population, sampling, and sample; (9) characteristics; (10) comparison groups; (11) primary outcomes and how and where they are assessed; and (12) secondary outcomes (22). The author (CL) evaluated all studies, and any disagreements with the second researcher (MR) were discussed between them. In case of any dispute, the opinion of a more experienced person or a third party was considered. Study quality was not a factor in the inclusion or exclusion criteria, which aligns with the Arksey and O'Malley scoping review framework (23).
Search strategy
In the search strategy, the core terms included “handover,” “handoff,” “SBAR,” “ISBAR,” and “COVID-19” connected by the Boolean operators “AND, OR, NOT.” During the search, thesaurus terms were organized in a tree structure, with more specific and narrower terms on the lower branches; all thesaurus terms were searched and “exploded” when we used MEDLINE Search (24). To implement the multidatabase search, the review had a focused query, a detailed description of the selected articles, a definition of central ideas, and documentation of the search process with friendly syntaxes and Boolean search (24). The primary search databases were (1) health sciences and medicine (PubMed/MEDLINE, Embase, Web of Science); (2) nursing (CINAHL); (3) psychology (PsycINFO); and (4) education (ERIC) (25). Additional sources included Google Scholar and Google. The PRISMA flowchart presented in Figure 1 summarizes the results.
Figure 1
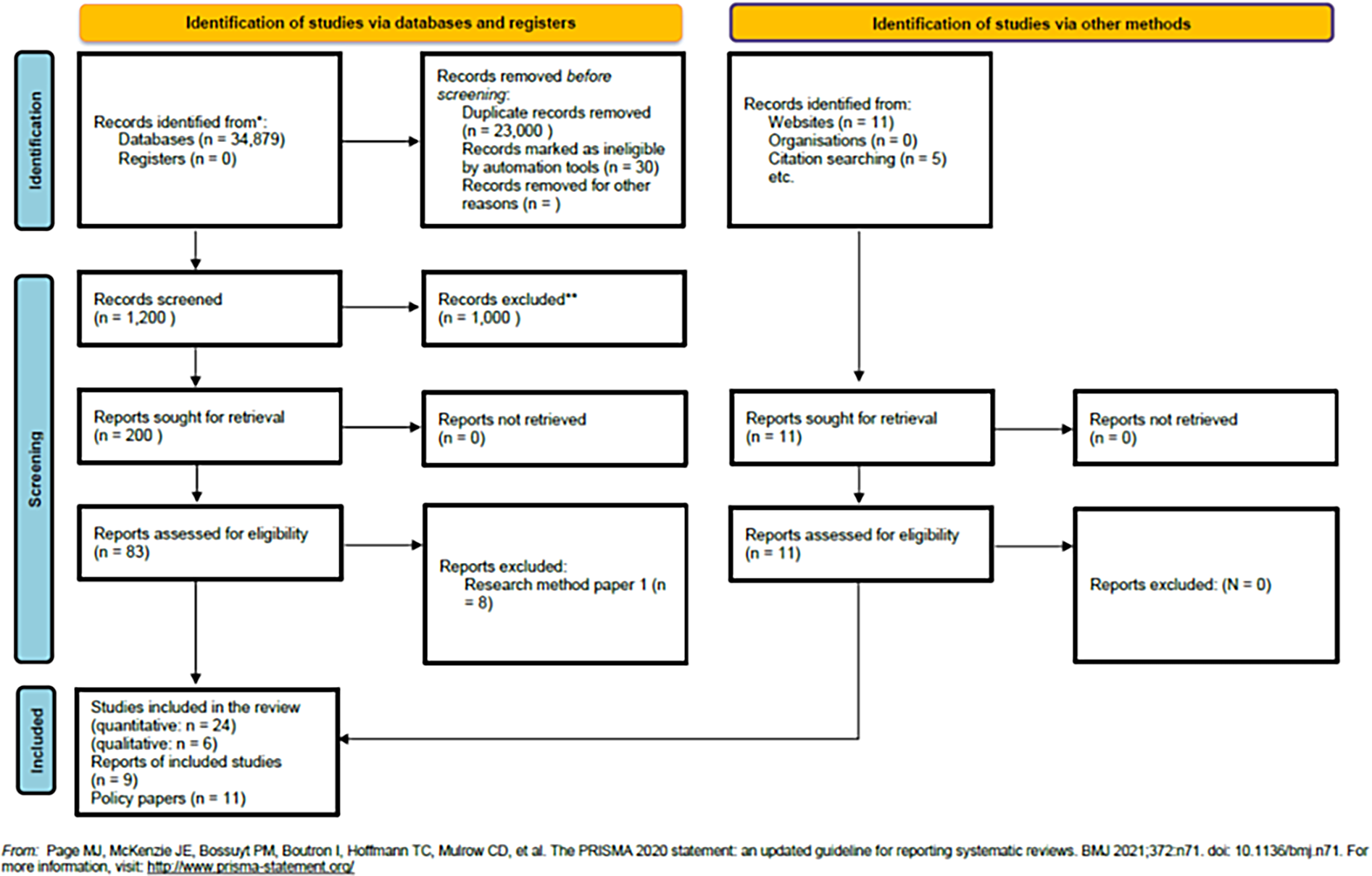
PRISMA flowchart.
Basic keywords
“ISBAR handover”; “clinical communication”; “structured handover”; “COVID-19 pandemic”; “non-COVID settings”; “healthcare handover”; “systematic review”; “meta-analysis”; “patient safety”; “interprofessional communication”
Grouped keywords with Boolean
(“ISBAR” OR “SBAR” OR “structured handover” OR “communication protocol”) AND
(“COVID-19” OR “coronavirus pandemic” OR “non-COVID” OR “general wards”) AND
(“patient safety” OR “communication quality” OR “clinical outcomes”) AND (“systematic review” OR “meta-analysis” OR “literature review”)
Truncated keywords
The search terms were developed to balance specificity with broad retrieval across major databases. Keywords related to the ISBAR framework included terms such as ISBAR, SBAR, handover*, hand-off*, communicat*, transfer*, shift chang*, and clinical handover. These were used to capture variations in terminology and spelling across international literature. Contextual terms addressed the clinical setting, including both COVID-19 and non-COVID environments. Relevant truncations and phrases were COVID-19, coronavirus, SARS-CoV-2, pandemic*, non-COVID, routine care, acute care, chronic care, emergenc*, hospital*, ward*, unit*, and setting. These allowed the retrieval of studies across diverse health system structures and care models. Population-based keywords targeted healthcare professionals, using nurse*, physician*, doctor*, clinician*, healthcare professional*, HCP*, student*, and trainee. This ensured the inclusion of studies involving varied clinical roles and levels of expertise. Outcome-related keywords included terms such as outcome*, effect*, impact*, efficac*, safety, error*, adverse event*, patient care, patient safety, interprofessional, collaborat*, team*, self-efficac*, and confidenc*, enabling capture of articles reporting both clinical and professional development measures. Finally, methodological terms focused on review and synthesis approaches: systematic review, meta-analys*, scoping review, integrative review, literature review, and evidence synthesis. These were critical for identifying eligible sources aligned with the study's design.
Combined search keywords with truncation
The search keywords combined yielded: (ISBAR OR SBAR OR handover* OR hand-off* OR communicat* OR transfer* OR “clinical handover”) AND (COVID-19 OR coronavirus OR SARS-CoV-2 OR pandemic* OR non-COVID OR “routine care” OR “acute care” OR “chronic care” OR emergenc* OR hospital* OR ward* OR unit*) AND (nurse* OR physician* OR doctor* OR clinician* OR “healthcare professional*” OR HCP* OR student* OR trainee*) AND (outcome* OR effect* OR impact* OR efficac* OR safety OR error* OR “adverse event*” OR “patient care” OR “patient safety” OR interprofessional OR collaborat* OR team* OR self-efficac* OR confidenc*) AND (“systematic review” OR meta-analys* OR “scoping review” OR “integrative review” OR “literature review” OR “evidence synthesis”).
PRISMA flowchart
During the identification stage, we extracted 34,979 records from the databases. Afterwards, 23,000 records were excluded due to duplication, while 30 records were marked as ineligible by automation tools. We found 11 records from websites and retrieved 5 additional records through citation searching. During the screening process, we reviewed 1,200 records; 1,000 were excluded based on the titles and abstracts. This resulted in 200 records being retrieved from databases and 11 others identified through alternative methods, such as hand searching or selecting from references of the studied articles. At the end of the screening, 58 records were initially deemed eligible, and 8 were excluded because they did not meet the inclusion criteria. The final sample included 24 quantitative studies, 6 qualitative studies, 9 reports, and 11 policy papers (Figure 1).
Statistical analysis
We converted the numerical results from each study (such as t-test, ANOVA F, correlation coefficients, and percentages) to extract their effect sizes (ES) and 95% confidence intervals (CIs) from the outcomes. They mainly used Cohen's d, which estimates the magnitude of an intervention (ISBAR) on the relative outcomes on a scale from 0 (nil) to 1 (huge) and transforms it into a common language effect size (CLES) (26). For calculating Cohen's d and CLES, we used the Psychometrica online calculator (https://www.psychometrica.de/effect_size.html) (27). The CLES is typically expressed as a percentage that indicates the effect of the independent variable on the dependent variable (28). The CLES indicates the likelihood (ratio) that a score randomly chosen from the intervention group would differ from a score randomly chosen from the control group when testing an intervention's effectiveness (29). Given the importance of sharing research findings in applied psychology, it is crucial to identify the most effective way to communicate ESs to general audiences is crucial (30).
The final step of the analysis was to find the 95% CIs of the CLES using an online calculator (31). Although CLES' simplicity of interpretation is its main advantage over other impact measures, it also has other appealing qualities; for example, it can be used regardless of the number of groups being compared, the degree of relatedness between the groups' scores, or the accuracy of the scores (29). Then, we calculated the fit of the CLES results using the Chi-square goodness of fit, Kolmogorov–Smirnov, and Shapiro–Wilk tests for normality. The CLES values and their 95% CI were the numerical values included in the meta-analysis. Alpha's rejection level for statistical significance in all tests was p ≤ 0.05, while the null hypothesis (Ho) was that the observed data distribution of data did not differ from a normally distributed one.
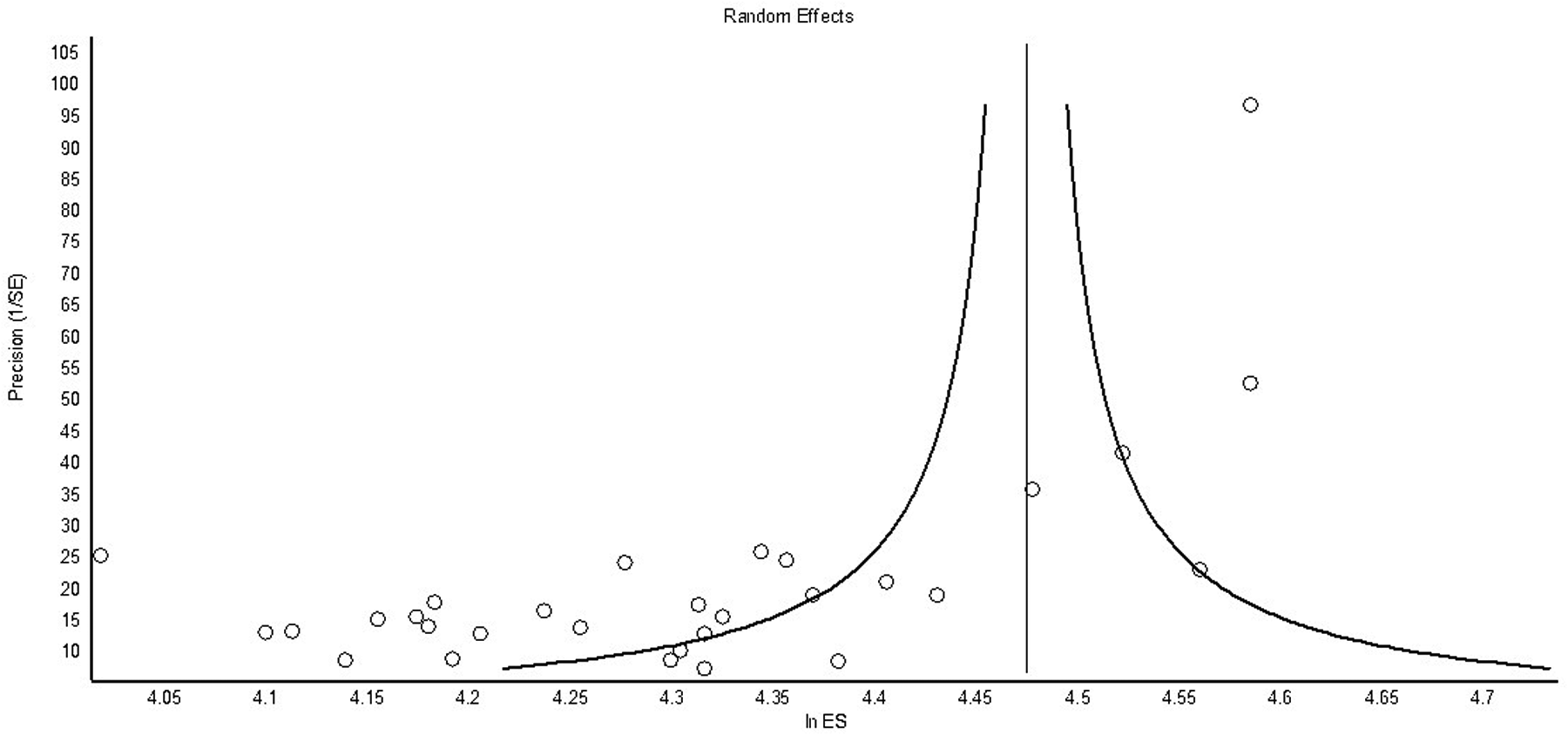
A meta-analysis of the subpopulation computed the global effect size (ES) and the coefficient of heterogeneity (I2) for the selected outcomes. We used the OpenMeta-Analyst of Brown University to perform a multistrata meta-analysis (32). Since the extracted data came from diverse populations and studies, we anticipated an asymmetrical funnel plot distribution explaining variations among the studies that could result in potential selection bias. Cochrane RoB-2 assessed the risk of bias for the studies included in the meta-analysis (https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials). The outcomes of SBAR/ISBAR implementation included effects on communication quality, team performance, and care quality. The outcome data were continuous, dichotomous, ordinal event history, and counts (33). Moreover, further reviews resulted in increasing the number of studies deemed suitable for inclusion in this systematic review (SR) (34).
Ethical considerations
The current SR did not require local and university ethical approval because it is a literature review with no intervention. However, the authors are aware of the ethical considerations of SRs. They referenced the general ethical guidelines for SRs, recognizing that (1) an SR may include studies with ethical inconsistencies and diversity; (2) an SR may report unethical studies; (3) in theory, a meta-analysis of extracted data might serve a different purpose than some of the original research it includes; and (4) there is an inherent subjective element in the process of conducting an SR and meta-analysis that can produce outcomes not originally intended in the screened research screened (35). Using SRs of biased research to guide policy decisions under the assumption that review findings represent the whole population raises serious ethical issues. Therefore, systematic reviewers must carefully assess the impact of potential publishing and search biases when developing an appropriate sample and search strategy (36).
Data summary
The present systematic review summarized the results from the extracted articles using quantitative meta-analysis and a narrative review of qualitative outcomes. The PICOS framework was used to summarize the studies (37). The qualitative outcomes were combined based on a Setting, Perspective, Intervention, Comparison, and Evaluation (SPICE) framework that allowed for clear recommendations at the end of the scoping review; using these findings in policies, program development, and research is a method of synthesizing bibliographic searches (38). The SPICE framework aided the summary by including questions related to the (1) setting, where? (2) perspective, for whom? (3) intervention, what? (4) comparison, compared with what? and (5) evaluation, with what outcomes? (39). One step in a meta-synthesis is to compare studies and produce a final summary of the results (39). Incorporating these findings into policy, program development, and research completed the synthesis of the literature search (40).
Meta-synthesis is a qualitative interpretive method used in systematic reviews to combine findings from multiple studies that employ different methodologies, especially those of a qualitative or mixed-methods approach. Unlike meta-analysis, which statistically combines numerical data, meta-synthesis aims to identify overall patterns, themes, and theoretical insights from detailed textual data such as participant stories, thematic codes, or interpretive frameworks. This process involves systematically selecting and evaluating relevant literature, extracting findings that represent shared or different perspectives, and integrating these insights into a cohesive conceptual model that goes beyond individual study contexts (41).
Meta-synthesis is especially suited to examining phenomena that are context-dependent, nuanced, and emotionally or relationally complex—such as the experience of implementing communication frameworks such as ISBAR in healthcare environments. Through interpretive layering and thematic integration, meta-synthesis enables reviewers to identify convergence in experiential knowledge, articulate latent meanings across professional narratives, and generate evidence-informed theories that contribute to best practice in clinical communication, interprofessional collaboration, and patient-centered care. Its value lies in the ability to generate novel understandings that enrich policy development, educational interventions, and compassionate clinical practice (42).
Relevance
Before any critical assessment, the selected publications were examined to determine their relevance; therefore, a complete version of each study was evaluated using the inclusion and exclusion criteria (43). We followed Saracevic's Manifestations of Relevance for the selected studies, which can be described as follows: (1) system/algorithmic relevance, how well a query resembles the retrieved document, its adequacy, usefulness, and value in use; (2) topical relevance, the semantic match between the query and the retrieved articles, including thematic richness, breadth, value, and approach; (3) cognitive relevance, the novelty, usefulness, reliability, verifiability, and quality of information; (4) motivational relevance, how well a document aligns with a user's objectives, goals, and reasons for seeking information, including personal trust and confidence in the information; and (5) situational relevance, how the retrieved articles help the reviewer achieve the review's goal (44, 45).
Summary of findings
To summarize the findings, we used the summary of findings GRADEpro GDT Cochrane table, which allows the extraction of evidence certainty, effect sizes (ES), and their confidence intervals (CIs) (46). GRADEpro GDT assessment enables the analysis of bias risks in search results and studies, extracts outcomes, and determines the grade of certainty in the evidence. The domains that can be extracted using GRADEpro include (1) risk of bias at both the study and outcome levels; (2) inconsistency, with a focus on clinical heterogeneity; (3) indirectness, assessed through direct comparisons between treatments in populations and settings similar to those for which the recommendations are intended; (4) imprecision, related to the accuracy of the population estimate based on the sample; and (5) publication bias, which considers the likelihood that results have influenced published outcomes (47–49). We also conducted a narrative review of the outcomes. A narrative review enables researchers to describe what is currently known about a topic, while also providing a subjective analysis and critique of the existing literature (50). The goal was to create a meaningful synthesis of research that involves a detailed description and interpretation (50).
Heterogeneity
The authors assessed the statistical heterogeneity of outcomes (CLES) with the following (51, 52): (1) visual inspection of the (forest) plots of confidence intervals of CLES; (2) I2 coefficient of heterogeneity (from 0% to 100%); the Cochrane's Q and χ2 statistics were used to detect statistical heterogeneity, where p < 0.05 indicates a high level of statistical heterogeneity between studies; I2 statistic is employed to quantify the statistical heterogeneity between studies, where I2 of 30%–50% represents moderate and I2 of 50%–90% characterizes substantial heterogeneity (53). A random-effects meta-analysis was used, as preliminary results from our pilot study showed high heterogeneity in the direction of the outcomes. We also calculated the 95% CI for all the CLES scores (54). Statistical software for meta-analysis was OpenMeta-Analyst by Brown University to complete a multilevel analysis (http://www.cebm.brown.edu/openmeta/). Risk of bias was calculated using Cochrane RoB-2 software (https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials).
Results
We extracted 29 studies or outcomes for the preliminary meta-analysis. The review began in January 2023 and ended in July 2025. The selected studies employed various implementation strategies and analyzed ISBAR/SBAR. Therefore, we found significant variability in the global extracted CLES (74.24%; 95% CI = 69.49%–79.31%), with
I2= 94.89% (
p< 0.001),
τ2= 0.30, and Cochrane's
Q= 567.224 (df = 29). The major subpopulations clustered around the following subpopulation outcomes of SBAR/ISBAR, with the extracted degree of certainty of the results as generated by the GRADEpro table and software (
Figures 2,
3):
- •
Increased communication and handover skills and quality (13 studies), with CLES = 76.19% (95% CI = 69.85%–83.10%) and high heterogeneity in the outcomes (I2 = 94.55%); in GRADEpro, this outcome had a moderate certainty in the results, with critical importance for the study.
- •
Increased confidence, preparedness, and self-efficacy in handover communication (eight studies), with CLES = 73.72% (95% CI = 62.57%–86.86%) and high heterogeneity (I2 = 95.7%); in GRADEpro, this outcome had a moderate certainty, with an important impact on the study.
- •
Increased interprofessional communication skills and confidence (six studies), with CLES = 75.53% (95% CI = 72.01%–79.24%) and minor heterogeneity (I2 = 19.3%); in GRADEpro, this outcome had a moderate certainty and was critical for the study, with a low heterogeneity of the results.
- •
Registered nurses were more frequently senders than receivers in interprofessional communication (one study), with CLES = 74.00% (95% CI = 61.39%–89.20%); in GRADEpro, this study had a very low certainty and had an unimportant impact on the results.
- •
Increased patient safety (two studies) with CLES = 65.32% (95% CI = 56.11%–76.05%) with high heterogeneity (I2 = 94.14%); in GRADEpro, this reached a very low certainty, although it was important for the study.
Figure 2
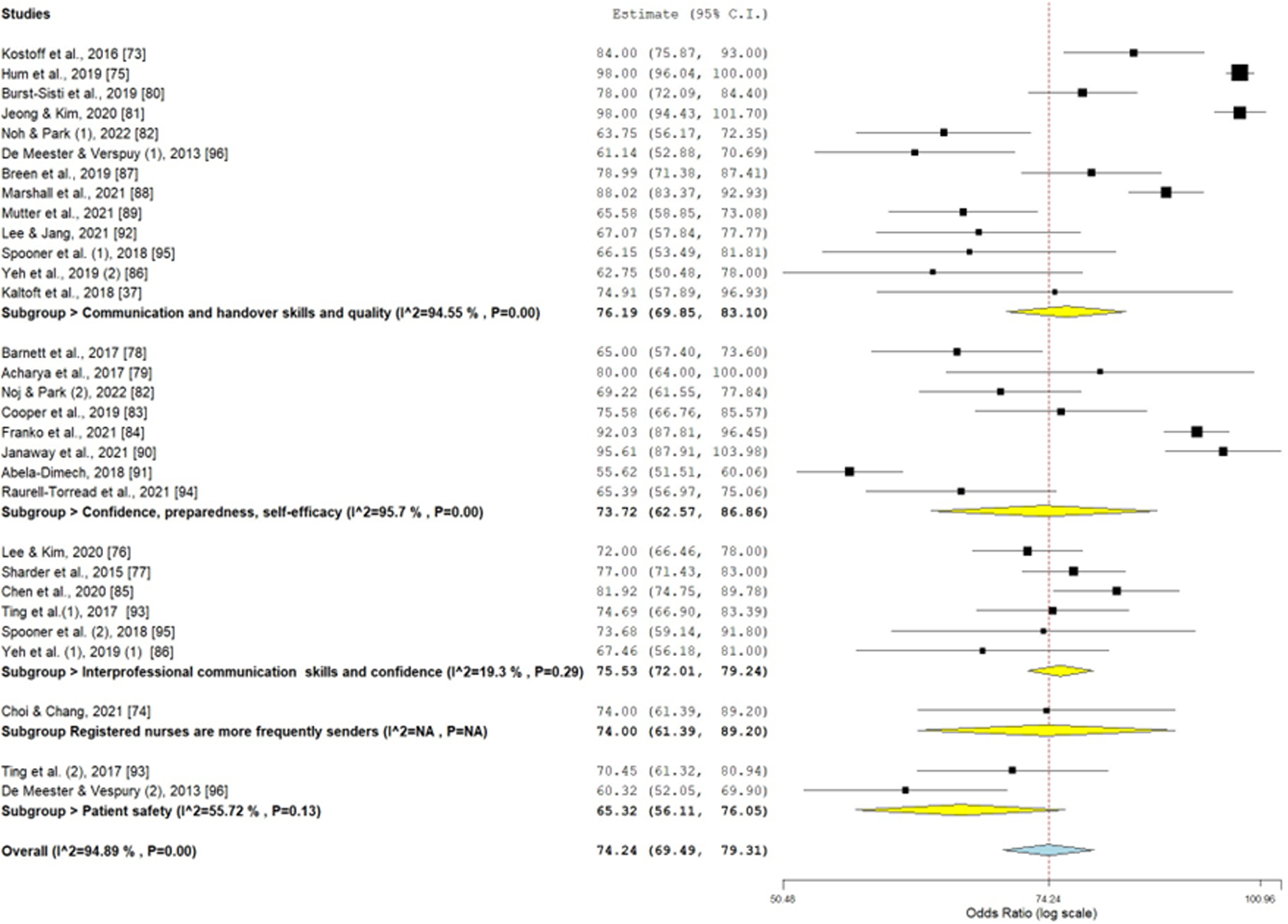
Forest plot.
Figure 3
Funnel plot.
The Kolmogorov–Smirnov test of CLES normality was D = 0.10 and accepted the normal distribution of the CLES (p > 0.10). The overall bias for all studies was low, although very few were randomized controlled studies (Tables 1–3; Figures 2, 3).
Table 1
| Authors | Country | Setting | Study design | Sample size | Population | Intervention | Comparison and measurements | Outcome | Cohen's d | Magnitude ES | CLES (low) (%) | CLES (%) | CLES high (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kostoff et al. (55) | USA | School of Pharmacy | BASa | 58 | Pharmacy students (PharmD): | Simulation based on SBAR where pharmacy students and nursing students were, respectively, sender and receiver | Collaborative Competency Attainment Survey (ICCAS) | ↑communication skills | 1.39 | ⊕⊕⊕b | 74.0 | 84.0 | 93.4 |
| Choi and Chang (56) | South Korea | Nursing home emergency | Survey, mixed-method | 50 | Nursing home personnel | Interviews on SBAR application and network analysis on data from semi-structured, face-to-face interviews | Comparing information flow between care worker, occupational therapist, physical therapist, registered nurse, and social worker | Registered nurses are more frequent senders | 0.5 | ⊕⊕⊕ | 58.8 | 74.0 | 89.2 |
| Hum et al. (57) | South Korea | Nursing school | BAS | 83 | Pediatric nurses | Impact of an SBAR communication program on communication performance, perception, and practicum-related outcomes in senior-year nursing students | Intervention vs. control group | ↑communication clarity and handover confidence | 3.02 | ⊕⊕⊕ | 95.0 | 98.0 | 100 |
| Lee and Kim (58) | South Korea | Nursing school | BAS, prospective observational | 194 | Nursing students | Team task performance was categorized into two phases: the initial team performance before a call to a mock doctor and the team task performance after receiving verbal instructions from a doctor via phone | Team performance correlation with SBAR and read-back communication in a simulated emergency | ↑team performance | 0.81 | ⊕⊕⊕ | 65.0 | 72.0 | 78.0 |
| Shrader et al. (59) | USA | PharmD Fourth year | BAS | 171 | Pharmacy students | Simulation with standardized colleagues | Within sample; inpatient and outpatient settings | ↑interprofessional communication skills and confidence | 1.06 | ⊕⊕⊕ | 70.0 | 77.0 | 83.0 |
| Barnett et al. (60) | USA | PharmD students | BAS | 118 | Pharmacy students | Simulated interactions with healthcare providers | Before–after SBAR preparedness to medication recommendation using the SBAR tool | ↑preparedness | 0.55 | ⊕⊕c | 56.4 | 65.0 | 73.6 |
| Acharya et al. (61) | USA | School of Psychiatry | BAS | 11 | Trainees in psychiatry | 3 h sessions in simulation education | Before–after SBAR confidence in giving and receiving information | ↑confidence | 1.20 | ⊕⊕⊕ | 53.1 | 80 | 100 |
| Brust-Sisti et al. (62) | USA | Pharmacy school | BAS | 197 | Third-year pharmacy students | Simulated telephone intervention | Before–after SBAR confidence in delivering pharmacotherapy-related intervention | ↑communication skills | 1.12 | ⊕⊕⊕ | 71.5 | 78.0 | 84.4 |
| Jeong and Kim (63) | South Korea | Nursing college | BAS | 54 | Third-semester nursing students | Handover skills | Clarity in handover | ↑clarity | 3.01 | ⊕⊕⊕ | 92.7 | 98 | 101.7 |
| Noh and Park (64) | South Korea | Nursing college | BAS | 120 | Fourth-year students | Simulation with 200 min sessions for 15 sessions | Comparison in communication flow timing | ↑communication flow ↑self-efficacy |
0.46 0.71 |
⊕d ⊕⊕ |
55.15 60.96 |
63.75 69.22 |
72.35 77.84 |
| Cooper et al. (65) | USA | Doctor of Nursing Practice programs (DNP) and Doctor of Physical Therapy (DPT) | BAS | 71 | First-year DPT and second-year DNP students | Educational intervention on SBAR and IPE using an online audio-conferencing tool | Comparison in the levels of communication confidence | ↑confidence | 0.98 | ⊕⊕⊕ | 65.59 | 75.58 | 85.57 |
| Franko et al. (66) | USA | Nursing and medical school | BAS | 144 | Pharmacy, medicine, and nursing students | Education in the use of SBAR | Comparison in the use of SBAR components | ↑appropriate use | 1.99 | ⊕⊕⊕ | 87.61 | 92.03 | 96.45 |
| Chen et al. (67) | China | First Affiliated Hospital of Xi’an Jiaotong University | BAS | 92 | General practitioners | Impact of the ISBAR communication training on residents’ interpersonal communication and teamwork in general practice standardized training | Doctor-to-nurse communication ability | ↑interpersonal communication ability, doctor-to nurse ↑interpersonal communication, doctor-to-doctor |
1.29 0.97 |
⊕⊕⊕ ⊕⊕⊕ |
74.06 67.5 |
81.92 75.36 |
89.78 84.17 |
| Yeh et al. (68) | USA | Nursing school | BAS | 46 | Pre-licensure nursing students | Communication performance; voluntary participants must complete two deliberate practice sessions over 2 weeks with a small incentive | Comparison of participant evaluation on components of the online deliberate practice session | ↑performamce ↑confidence |
0.46 0.64 |
⊕ ⊕⊕ |
62.75 67.46 |
0.46 0.53 |
0.78 0.81 |
| Breen et al. (19) | Ireland | Nursing and medical school | RCTd + BAS | 90 | Third-year nursing students and final-year medical undergraduates | Proficiency-based progression (PBP) training approach to clinical communication in the context of a clinically deteriorating patients | PBP vs. e-learning alone or in combination with standard simulation | ↑communication skills | 1.14 | ⊕⊕⊕ | 70.57 | 78.99 | 87.41 |
| Marshall et al. (69) | Australia | Medical school | RCT + BAS | 168 | Medical students | Communication during telephone referral in a simulated clinical setting | Clarity of delivery on a five-point Likert scale | ↑clarity | 5.06 | ⊕⊕⊕ | 83.11 | 88.02 | 92.93 |
| Mutter et al. (70) | USA | Schools of Medicine and Nursing | BAS | 154 | Fourth-year medical students and master's nursing students | Mock-paging interprofessional education | Immediate vs. delayed feedback | ↑SBAR scores in the immediate feedback group | 0.56 | ⊕⊕ | 58.08 | 65.58 | 73.08 |
| Janaway et al. (71) | UK | Mental health settings | Survey | 23 | Psychiatric nurses and doctors | Survey about awareness of SBAR through its use and benefits | Objective data were collected, looking at handover gathered during the survey period. Data were collected via phone from the duty physician over a 5-day period, twice daily | ↑self-efficacy ↑understanding of patients |
2.58 | ⊕⊕⊕ | 87.24 | 95.61 | 103.98 |
| Abela-Dimec (72) | Canada | Mental health settings | BAS survey | 481 | Psychiatric nurses | Impact of SBAR on 122 handovers | Comparing the degree of satisfaction in the information received during handovers | ↑satisfaction | 0.20 | ⊕ | 51.18 | 55.62 | 60.06 |
| Lee and Jang (73) | South Korea | Mental health settings | BAS | 74 | Psychiatric nurses | SBAR simulation to improve communication skills | SBAR vs. communication as usual | ↑communication skills | 0.47 | ⊕ | 56.99 | 67.07 | 77.77 |
| Ting et al. (74) | Taiwan | Obstetric wards | BAS | 96 | Obstetric nurses | 1 h session during monthly meetings | Nurses’ scores on the Chinese version of the Safety Attitudes Questionnaire (SAQ) | ↑teamwork climate/communication ↑safety climate, |
0.94 0.76 |
⊕⊕⊕ ⊕⊕ |
65.99 61.32 |
74.69 70.45 |
83.39 79.58 |
| Raurell-Torredà et al. (75) | Spain | Nursing school | BAS RCT |
93 | Undergraduate nurse students | The intervention group was trained in teamwork skills, role and task assignment skills, and the use of the SBAR worksheet in a 1 h role-play training session | Intervention + control group measured on the KidSIM Team Performance Scale (teamwork skills) and the Clinical Simulation Evaluation Tool (non-technical skills) | ↑confidence | 0.56 | ⊕⊕ | 55.72 | 65.39 | 75.06 |
| Spooner et al. (76) | Australia | Public hospital | BAS | 35 | Junior medical officers (JMO) | Following ISBAR, there is an increase in core categories that are completed | Measuring subjective responses by survey and completeness of ISBAR items | ↑confidence and skills ↑quality of handovers |
0.89 0.58 |
⊕⊕⊕ ⊕ |
55.5 50.5 |
73.68 66.15 |
91.8 81.8 |
| Kaltoft et al. (39) | Denmark | Public hospital | BAS survey | 50 observations | Both certified registered nurse anesthetists and registered nurses (RNs) from postanesthesia care unit | Nurses were interviewed about their satisfaction with the handover via an electronic survey | Comparing satisfaction in the handover before and after exposure to SBAR | ↑quality of handovers | 0.95 | ⊕⊕⊕ | 62.89 | 74.91 | 86.93 |
| De Meester and Vespury (77) | Belgium | Public hospital | BAS | 425 | Nurses were taught to interact with doctors in 16 hospital wards using SBAR when patients were worsening | SBAR training of intensive care unit (ICU) nurses | Comparing perception of teamwork and efficient communication; comparing ICU admissions; comparing patient fatalities | ↑communication skills and quality ↓ expected deaths |
0.40 0.37 |
⊕ ⊕ |
61.14 60.32 |
52.88 50.60 |
70.69 69.90 |
Summary of findings (PICO).
BAS, before–after study.
Large ES.
Intermediate ES.
Small ES.
Table 2
| Certainty assessment | No of patients | Effect size CLES | Certainty | Importance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | SBAR handover + routine handover | (95% CI) | ||
| Increased communication and handover skills (assessed with: I/SBAR) | ||||||||||
| 13 | Observational studies | Serious | Serious | Not serious | Not serious | Publication bias strongly suspected Strong association All plausible residual confounding would reduce the demonstrated effect |
14,433 | 76.19 (69.85–83.10) | ⊕⊕⊕◯ Moderate |
Critical |
| Registered nurses are more frequently senders (assessed with: I/SBAR) | ||||||||||
| 1 | Observational studies | Serious | Serious | Not serious | Very serious | Publication bias strongly suspected Strong association All plausible residual confounding would suggest spurious effect, while no effect was observed |
50 | 74.00 (61.39–89.20) | ⊕◯◯◯ Very low |
Not important |
| Increased interprofessional communication skills and confidence (assessed with: I/SBAR) | ||||||||||
| 6 | Observational studies | Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected Strong association All plausible residual confounding would reduce the demonstrated effect |
500 | 75.53 (72.01–79.24) | ⊕⊕⊕◯ Moderate |
Critical |
| Increased confidence, preparedness, and self-efficacy (assessed with: I/SBAR) | ||||||||||
| 8 | Observational studies | Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected Strong association All plausible residual confounding would reduce the demonstrated effect |
1,104 | 73.72 (62.57–86.86) | ⊕⊕⊕◯ Moderate |
Important |
| Patient safety (assessed with: I/SBAR) | ||||||||||
| 2 | Observational studies | Not serious | Not serious | Not serious | Not serious | Publication bias strongly suspected Strong association All plausible residual confounding would reduce the demonstrated effect |
518 | 65.32 (51.11–76.05) | ⊕◯◯◯ Very low |
Important |
GRADEpro GDT summary of findings.
Question: What are the I/SBAR handover outcomes compared with routine handover for communication in healthcare?
Setting: Schools of medicine and nursing; pharmacy schools; psychiatric settings; Doctor of Pharmacy school; Doctor of Physical therapy school; nursing home.
Bibliography: Kostoff et al. (78), Choi and Chang (79), Hum et al. (80), Lee and Kim (81), Shrader et al. (82), Barnett et al. (83), Acharya et al. (84), Brust-Sisti et al. (85), Jeong and Kim (86), Noh and Park (16), Cooper et al. (87), Franko et al. (88), Chen et al. (89), Yeh et al. (90), Breen et al. (91), Marshall et al. (92), Mutter et al. (93), Janaway et al. (55), Abela-Dimec (56), Lee and Jang (57), Ting et al. (58), Raurell-Torredà et al. (59), Spooner et al. (60), Kaltoft et al. (28), De Meester and Vespury (61). [Table adapted from Schünemann et al. (47)].
Table 3
| Authors | RoB-2 quality assessmentb Low risk:  Some concerns: Some concerns:  High risk: High risk:  |
||||||
|---|---|---|---|---|---|---|---|
| Outcomesa | D1 | D2 | D3 | D4 | D5 | OA | |
| Kostoff et al. (55) | O1 |

|

|

|

|

|

|
| Choi nd Chang (56) | O4 |

|

|

|

|

|

|
| Hum et al. (57) | O1 |

|

|

|

|

|

|
| Lee and Kim (58) | O3 |

|

|

|

|

|

|
| Shrader et al. (59) | O3 |

|

|

|

|

|

|
| Barnett et al. (60) | O2 |

|

|

|

|

|

|
| Acharya et al. (61) | O2 |

|

|

|

|

|

|
| Brust-Sisti et al. (62) | O1 |

|

|

|

|

|

|
| Jeong and Kim (63) | O1 |

|

|

|

|

|

|
| Noh and Park (64) | O1, O2 |

|

|

|

|

|

|
| Cooper et al. (65) | O2 |

|

|

|

|

|

|
| Franko et al. (66) | O2 |

|

|

|

|

|

|
| Chen et al. (67) | O3 |

|

|

|

|

|

|
| Yeh et al. (68) | O1, O2 |

|

|

|

|

|

|
| Breen et al. (19) | O1 |

|

|

|

|

|

|
| Marshall et al. (69) | O1 |

|

|

|

|

|

|
| Mutter et al. (70) | O1 |

|

|

|

|

|

|
| Janaway et al. (71) | O2 |

|

|

|

|

|

|
| Abela-Dimech (72) | O2 |

|

|

|

|

|

|
| Lee and Jang (73) | O1 |

|

|

|

|

|

|
| Ting et al. (74) | O2, O5 |

|

|

|

|

|

|
| Raurell-Torredà et al. (75) | O2 |

|

|

|

|

|

|
| Spooner et al. (76) | O1, O3 |

|

|

|

|

|

|
| Kaltoft et al. (39) | O1 |

|

|

|

|

|

|
| De Meester and Vespury (77) | O1, O5 |

|

|

|

|

|

|
Summary of findings, outcomes, and RoB-2 quality assessment.
O1, increased communication and handover skills and quality; O2, increased confidence, preparedness, and self-efficacy; O3, increased interprofessional communication skills and confidence; O4, registered nurses are more frequent senders in communication exchanges; O5, increased patient safety.
D1, randomization process; D2, deviations from the intended interventions; D3, missing outcome data; D4, measurement of the outcome; D5, selection of the reported results; OA, overall.
Qualitative critical analysis
Handover during COVID-19
ISBAR was used during the COVID-19 pandemic to extract patient identification, analyze current scenarios, summarize background information, convey assessment, and provide recommendations; it also included identification, diagnosis, admission information, symptoms, treatments, medical background, past exposure, allergies, assessment, and nursing consensus (94). Perioperative nurses use ISBAR to summarize critical data for quick, structured handovers in COVID-19 patients, including patient names, operations, anesthesia, airway status, heat and moisture exchanger (HME) filter usage, and intraoperative issues (95). We utilized an ISBAR format for liaison psychiatric teams during COVID-19 emergencies in mental health settings; ISBAR involved recording mental symptoms and hallucinations to confirm or exclude a delirium diagnosis. The recommendation focused on psychopharmacological input—such as antipsychotics, benzodiazepines, or antihistamines—to reduce recurrent agitation in organic and agitated COVID-19 delirium (96, 97). CHs can relieve the pressure on junior doctors as well as reduce their anxiety and depression (when this generated by the medical handover); therefore, including kindness in CHs led to the coinage of the term “K-ISBAR” to emphasize the importance of delivering CHs kindly, particularly during stressful clinics during the COVID-19 pandemics (98, 99).
Other research supports the value of adopting an SBAR/ISBAR handover in the treatment of COVID-19 patients who are severely unwell (100). We suggest improving interprofessional education and handover for COVID-19 patients by providing undergraduate healthcare students with mobile technology apps for continuous ecological momentary assessment, online surveys, and mentoring (101). To address the general healthcare needs of COVID-19 patients who could not see their providers in person, students collaborated remotely with attending doctors in a multispecialty clinic using SBAR (102). During infectious disease outbreaks, online handovers using video conferencing software could be used in addition to traditional face-to-face handovers for intensive care unit patients to adhere to pandemic restrictions (78). Education improves handover completion rates for patients in an acute stage of COVID-19 but can increase workloads and staffing demands, thereby reducing handover quality (79).
Previous systematic reviews
The first SR analyzed 18 studies and found communication training differences in ISBAR between nurses and physicians; however, it found simulation and standardized tools effective in improving CH skills (80). The second SR analyzed 18 studies and identified barriers and facilitators to communication in handover outcomes in interprofessional teams; understanding reciprocal roles and appreciating unique contributions facilitated CH, while a hostile hospital atmosphere hindered successful CHs (81). The third SR examined 28 studies and found that a lack of coordination and interprofessional communication were obstacles to patients' rehabilitation, thereby resulting in poor adherence and engagement with the clinical team (82). The fourth SR analyzed 16 studies and found that innovative mobile technology enhances accessibility, sharing, and handover communication (83). The fifth SR of 73 studies found that effective interprofessional learning strategies for CH include workshops, discussions, simulated patient training, and experiential learning (84). However, despite efforts to design communication programs around competency-based stages, we found that most programs lack a longitudinal perspective and effective means of appraising competency and self-perceived improvement in teamwork (85). The sixth SR analyzed 91 articles and found that the facilitators of effective communication include standardization, team integration, shared values, stability, and open culture; barriers include professional hierarchies, environmental factors, and irrelevant details (86). The seventh SR analyzed eight studies and found that CH reduces adverse events in patient care and improves patient safety when studies focused on team communication, with a reduction in adverse drug effects and communication breakdown in interprofessional teams (16). The eighth SR analyzed 34 studies on the SBAR technique and found significant improvements in communication clarity in classroom and clinical settings (87).
Policy papers on SBAR implementation in the UK
The NHS Institute for Innovation and Improvement suggests learning outcomes in SBAR scenarios involve participants understanding how SBAR can improve communication, using a structured technique, discussing strategies, listing practical communication situations, simulating situations, and describing successful practice areas using SBAR (88). The Royal College of Nursing in the UK has sponsored two articles that suggest the link between team communication and clinical outcomes in patient care (89–91). The Royal College of Physicians in the UK emphasizes that using structured communication tools, such as SBAR handover, improves patient safety and that senior staff should promote a good handover culture (92). Further, the National Institute for Health and Care Excellence (NICE) in the UK encourages HCPs (such as doctors, nurses, advanced clinical practitioners, physiotherapists, mental health teams, and pharmacists) to work together to provide a planned handover of care (verbal, written, or electronic) to patients who have been hospitalized with a medical emergency (93).
Discussion
The current review reveals that CHs are crucial for patient safety and quality of life in healthcare settings, but gaps in SBAR/ISBAR handover implementation are also reported. The COVID-19 pandemic underscored the importance of coordinated communication and prompt measures to mitigate the virus (103). In emergency rooms, electronic handovers were employed to decrease crowded multidisciplinary meetings, enhance patient safety, and minimize information governance violations, while also helping to maintain social distancing during the COVID-19 pandemic (103). Electronic handovers improve quality and efficiency, reduce clinical errors, shorten time in sharing crucial data, and enhance patient safety in intensive care units (104). Furthermore, distance and electronic handovers facilitate information sharing during COVID-19 isolation or routine multidisciplinary team meetings (MDT), thereby enabling integrated and rapid care for community patients (105). Teams can use the Internet and intranet for questions, opinions, and management changes during CHs which expedites the sharing of vital data about patients with professionals virtually and synchronously participating from different geographical areas linked to the same healthcare settings and patients (105).
One of the significant aspects that emerged in the international literature was the need to implement SBAR/ISBAR handover in clinical practice, medical education, and community health. Implementation research is crucial in global health, as it addresses the gaps and logistics of achieving national and international health objectives (106). Moreover, implementation research emphasizes partnerships among the community, people, implementers, researchers, and policymakers, focusing on strategies to improve equality, efficiency, scale-up, and sustainability (106). Implementing SBAR/ISBAR has thus a positive effect, with increased job satisfaction among healthcare professionals and teams (107). However, hospitals, units, and nurses use various delivery techniques for shift reports; therefore, narrative, repetitive, or irrelevant information may occasionally make communication difficult. Additionally, shift reports are more likely to include errors since nurse handovers occur during busy periods of the day when there are several distractions and time restrictions (108).
Therefore, implementation strategies should include daily safety-critical handovers, standardized training, structured patient handovers, uniform handover information and reception, participation of all parties, contribution of each team member, team endorsement, and professional exchanges (109). For example, ISBAR implementation reduced sepsis and operative time in a urological department compared with the non-ISBAR control group (110). In a study in nursing homes in the USA, the application of ISBAR improved communication and collaboration between home providers and nursing staff (111). In another study, nursing students found that the ISBAR has high usability, providing opportunities for active contribution and increased self-motivation (112). The findings from this systematic review also establish a strong basis for promoting wider adoption of the ISBAR communication protocol across healthcare settings. The consistent pattern observed in the reviewed studies highlights ISBAR's ability to enhance clarity, reduce cognitive load during high-pressure situations, and support a structured approach to information exchange in patient care. Importantly, these advantages translate into measurable improvements in clinical outcomes and patient safety. For instance, using ISBAR for handovers has been shown to decrease adverse events and omissions in information transfer, especially in emergency departments and intensive care units (113, 114).
From an educational perspective, ISBAR also promotes the development of communication skills among healthcare trainees. By offering a structured framework, it helps learners to understand clinical reasoning and focus on important information during interprofessional interactions (12). This organized communication training improves not only technical accuracy but also builds confidence and accountability, which are essential for delivering safe patient care (115). Furthermore, in increasingly complex and fragmented healthcare systems, ISBAR may act as a unifying tool to connect professional and disciplinary boundaries. The evidence reviewed indicates that when used consistently, ISBAR fosters a culture of standardization that encourages relational responsibility among practitioners—an idea that aligns with broader objectives of compassionate and ethically responsible healthcare delivery (116). ISBAR's role in fostering relational accountability is especially important in high-stakes environments such as pandemic response teams or community-based multidisciplinary care, where effective communication is directly linked to outcomes (117).
Future research should examine ISBAR's adaptability in culturally diverse and digitally connected healthcare settings, as well as its integration with emerging communication technologies. This will provide insights into how ISBAR can be used to promote inclusive patient engagement and support fair care delivery. Overall, the evidence reviewed in this study confirms that ISBAR is more than just a communication tool; it is a vital part of safe, collaborative, and compassionate clinical practice. Increasing its use across different systems and training programs offers a strategic way to improve patient care outcomes and should be a top priority for healthcare educators and policymakers. With the use of a structured ISBAR handover, patients reported that their interprofessional team effectively coordinated care and shared relevant information, helping to prevent communication gaps among team members (118). This approach also enhanced patient satisfaction with the healthcare team and reduced complaints related to the provision of missed or inconsistent information across providers (118).
Conclusion
We have seen that SBAR/ISBAR handovers improve collaborative healthcare practices and communication exchanges, reduce patient risk, and increase staff satisfaction. They also enhance clinical practice by clarifying roles, reducing information gaps, and minimizing clinical and surgical risks. Therefore, structured CHs reduce medical errors, improve the quality of care, and enhance patient safety, while also reducing the global time allocated to understanding and resolving clinical cases. However, implementation and regular application remain a challenge due to high turnover and the need to address primary and secondary care emergencies. National and international policies promote the use of the SBAR/ISBAR for improved care quality, patient safety, and team performance. At other times, professionals from different backgrounds and seniority add to the same electronic notes linked to the same patient, thereby causing some interprofessional misunderstanding due to the technical language used that is unique to each HCP. Occasionally, CHs are not comprehensive and do not incorporate the ISBAR algorithm, thereby comprising bits of globally inapplicable information (119, 120).
Limitations
This SR has several limitations. Although we conducted a comprehensive extraction of significant studies, the outcomes were heterogeneous, and we restricted the numerical analysis to span different outcomes. A more comprehensive and extended study selection would have yielded different results. SBAR/ISBAR is not the only technique used for handovers in clinical practice; overall, the study may have had a positive bias toward this approach and its use. The scrutinized studies also did not provide evidence that the proposed use of the clinical handovers had long-term effects, and whether, if adopted, the teams continued to perform well long after the training. Furthermore, almost all studies were cross-sectional, lacking randomization and blinding, which limits the conclusions regarding the association of variables but does not allow for further conclusions about the impact of biases in the selected studies.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
CL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MR: Conceptualization, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
COVID-19, the SARS-CoV-2 virus infectious illness known as coronavirus disease; ISBAR, Introduction, Situation, Background, Assessment, and Recommendation; SBAR, Situation, Background, Assessment, and Recommendation; K-SBAR, SBAR plus Kindness; CH, clinical handover; NHS, National Health Service; HCP, healthcare professional (nurses, doctors, allied healthcare professionals, pharmacists, and other health professionals); SR, systematic review.
References
1.
World Health Organization (WHO). Coronavirus, World Health Organization. (not dated). Available online at:https://www.who.int/health-topics/coronavirus/coronavirus(Accessed May 29, 2023).
2.
UK Government. England summary | Coronavirus (COVID-19) in the UK (not dated). Available online at:https://coronavirus.data.gov.uk/details/cases?areaType=nation&areaName=(Accessed May 29, 2023).
3.
Parasher A . COVID-19: current understanding of its pathophysiology, clinical presentation and treatment. Postgrad Med J. (2020) 97:312–20. 10.1136/postgradmedj-2020-138577
4.
The Royal Children’s Hospital Melbourne. Nursing clinical handover. (2024). Available online at:https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Nursing_clinical_handover/(Accessed December 22, 2023).
5.
World Health Organization (WHO). Communicating during patients handovers. (2007). Available online at:https://cdn.who.int/media/docs/default-source/patient-safety/patient-safety-solutions/ps-solution3-communication-during-patient-handovers.pdf(Accessed December 23, 2022).
6.
Kim EJ Seomun G . Handover in nursing: a concept analysis. Res Theory Nurs Pract. (2020) 34:297–20. 10.1891/rtnp-d-19-00089
7.
Smeulers M Lucas C Vermeulen H. What is the best nursing handover style to ensure continuity of information for hospital patients? (2014). Available online at:https://www.cochrane.org/CD009979/EPOC_what-best-nursing-handover-style-ensure-continuity-information-hospital-patients(Accessed December 23, 2022).
8.
Government of Western Australia Department of Health. Clinical handover (not dated). Available online at:https://ww2.health.wa.gov.au/Articles/A_E/Clinical-handover(Accessed December 23, 2022).
9.
Rickard F Lu F Gustafsson L MacArthur C Cummins C Coker I et al Clinical handover communication at maternity shift changes and women’s safety in Banjul, the Gambia: a mixed-methods study. BMC Pregnancy Childbirth. (2022) 22:784. 10.1186/s12884-022-05052-9
10.
Australian Medical Association. Guidance on clinical handover. (2020). Available online at:https://www.ama.com.au/article/guidance-clinical-handover(Accessed February 6, 2023).
11.
Merriam-Webster Dictionary Online. Communicate definition & meaning. Available online at:https://www.merriam-webster.com/dictionary/communicate(Accessed February 6, 2023).
12.
Eggins S Slade D . Communication in clinical handover: improving the safety and quality of the patient experience. J Public Health Res. (2015) 4:666. 10.4081/jphr.2015.666
13.
The Joint Commission. Patient safety. Available online at:https://www.jointcommission.org/resources/patient-safety(Accessed February 6, 2023).
14.
Umberfield E Ghaferi AA Krein SL Manojlovich M . Using incident reports to assess communication failures and patient outcomes. Jt Comm J Qual Patient Saf. (2019) 45:406–13. 10.1016/j.jcjq.2019.02.006
15.
Conn LG Lingard L Reeves S Miller KL Russell A Zwarenstein M . Communication channels in general internal medicine: a description of baseline patterns for improved interprofessional collaboration. Qual Health Res. (2009) 19:943–53. 10.1177/1049732309338282
16.
Müller M Jürgens J Redaèlli M Klingberg K Hautz WE Stock S . Impact of the communication and patient handoff tool SBAR on patient safety: a systematic review. BMJ Open. (2018) 8:e022202. 10.1136/bmjopen-2018-022202
17.
Institute for Healthcare Improvement. Sbar tool: Situation-background-assessment-recommendation: IHI (2023). Available online at:https://www.ihi.org/resources/Pages/Tools/sbartoolkit.aspx(Accessed February 21, 2023).
18.
Burgess A van Diggele C Roberts C Mellis C . Teaching clinical handover with ISBAR. BMC Med Educ. (2020) 20:459. 10.1186/s12909-020-02285-0
19.
Breen D O’Brien S McCarthy N Gallagher A Walshe N . Effect of a proficiency-based progression simulation program on clinical communication for the deteriorating patient: a randomized controlled trial. BMJ Open. (2019) 9(7):e025992. 10.1136/bmjopen-2018-025992
20.
McCullogh K Andrew L Genoni A Dunham M Whitehead L Pock D . An examination of primary care nursing service evaluation using the Donabedian model: a systematic review. Res Nurs Health. (2023) 46(1):159–76. 10.1002/nur.22291
21.
Donabedian A . Evaluating the quality of medical care. Milbank Quarterly. (2005) 83(4):691–729. 10.1111/j.1468-0009.2005.00397.x
22.
National Collaborating Centre for Methods and Tools. McMaster University. Guide to Community Preventive Services Data Abstraction Form. (2021). Available online at:https://www.thecommunityguide.org/sites/default/files/assets/abstractionform.pdf(Accessed December 20, 2021).
23.
Arskey H O’Malley L . Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. 10.1080/1364557032000119616
24.
Bramer WM de Jonge GB Rethlefsen ML Mast F Kleijnen J . A systematic approach to searching: an efficient and complete method to develop literature searches. J Med Libr Assoc. (2018) 106:531–41. 10.5195/jmla.2018.283
25.
University of Florida. FIU libraries: How to find and conduct systematic reviews: Step 4: Choose your databases. (2023). Available online at:https://library.fiu.edu/systematicreviews/step4(Accessed May 20, 2023).
26.
Bowling A . Research Methods in Health. McGraw-Hill: Open University Press (2009).
27.
Lenhard W Lenhard A. Computation of effect sizes. Psychometrica. (2016). Available online at:https://www.psychometrica.de/effect_size.html(Accessed May 23, 2023).
28.
Mastrich Z Hernandez I . Results everyone can understand: a review of common language effect size indicators to bridge the research-practice gap. Health Psychol. (2021) 40(10):727–36. 10.1037/hea0001112
29.
McGraw KO Wong SP . A common language effect size statistic. Psychol Bull. (1992) 111(2):361–5. 10.1037/0033-2909.111.2.361
30.
Brooks ME Dalal DK Nolan KP . Are common language effect sizes easier to understand than traditional effect sizes?J Appl Psychol. (2014) 99(2):332–40. 10.1037/a0034745
31.
Bobbitt Z. Confidence Interval Calculator. Calculating the 95% confidence interval of a percentage. Available online at:https://www.statology.org/confidence-intervals/(Accessed April 23, 2023).
32.
Wallace BC Schmid CH Lau J Trikalinos TA . Meta-analyst: software for meta-analysis of binary, continuous, and diagnostic data. BMC Med Res Methodol. (2009) 9:80. 10.1186/1471-2288-9-80
33.
Thomas J O’Mara-Eves Kneale D Shemilt I . Chapter 8: synthesis methods for combining and configuring quantitative data. In: GoughDOliverSThomasJ, editors. An Introduction to Systematic Reviews. 2nd ed.London: SAGE (2017). p. 182–209.
34.
Stoll C Izadi S Fowler S Gree P Suls J Colditz G . The value of a second reviewer for study selection in systematic reviews. Res Synth Methods. (2019) 10(4):539–45. 10.1002/jrsm.1369
35.
Vergnes JN Marchal-Sixou C Nabet C Maret D Hamel O . Ethics in systematic reviews. J Med Ethics. (2010) 36(12):771–4. 10.1136/jme.2010.039941
36.
Suri H . Ethical considerations of conducting systematic reviews in educational research. In: Zawacki-RichterOKerresMBedenlierSBondMBuntisK, editors. Systematic Reviews in Educational Research: Methodology, Perspectives and Application. Wiesbaden, Germany: Springer (2020). p. 41–54. Available online at:https://link.springer.com/chapter/10.1007/978-3-658-27602-7_3
37.
Amir-Behghadami M Janati A . Population, intervention, comparison, outcomes, and study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. (2020) 37(6):387. 10.1136/emermed-2020-209567
38.
Marshall AP Tobiano G Murphy N Comadira G Willis N Gardiner T et al Handover from operating theatre to the intensive care unit: a quality improvement study. Aust Crit Care. (2019) 32(3):229–36. 10.1016/j.aucc.2018.03.009
39.
France EF Uny I Ring N Turley RL Maxwell M Duncan EAS et al A methodological systematic review of meta-ethnography conduct to articulate the complex analytical phases. BMC Med Res Methodol. (2019) 19(1):35. 10.1186/s12874-019-0670-7
40.
Noblit GW Hare RD . Meta-ethnography: Synthesizing Qualitative Studies. Newbury Park, California: Sage Publications, Inc (1988). p. 1–88.
41.
Campbell M McKenzie JE Sowden A Katikireddi SV Brennan SE Ellis S et al Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. Br Med J. (2020) 368:l6890. 10.1136/bmj.l6890
42.
Nicolas. What is Meta Synthesis in Literature Review. ResearchProspect Canada (2024). Available online at:https://researchprospect.ca/resources/meta-synthesis-literature-review/(Accessed July 12, 2025).
43.
Aveyard H Payne S Preston N . A Post-graduate’s Guide to Doing a Literature Review in Health and Social Care. Maidenhead: Open University Press (2021). p. 1–188.
44.
Toms EG O’Brien HL Kopak R Freund L . Searching for relevance in the relevance of search. In: CrestaniFRuthvenI, editors. Context: Nature, Impact, and Role. Berlin: Springer (2005). p. 59–78. Available online at:https://link.springer.com/chapter/10.1007/11495222_7
45.
Saracevic T . Relevance: a review of the literature and a framework for thinking on the notion in information science. Part III: behavior and effects of relevance. J Am Soc Inf Sci Technol. (2007) 58:2126–44. 10.1002/asi.20681
46.
Higgins JPT Thomas J Chandler J Cumpston M Li T Page MJ et al , editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 6.2. Chichester: John Wiley & Sons (2021). Available online at: https://training.cochrane.org/handbook (Accessed November 16, 2023).
47.
Schünemann H Brożek J Guyatt G Oxman A . editors. GRADE handbook for grading quality of evidence and strength of recommendations. Updated. The GRADE Working Group, guidelinedevelopment.org/handbook (Accessed April 13, 2023).
48.
GRADEpro GDT. GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime (2024). Available online at:gradepro.org(Accessed April 13, 2023).
49.
Guyatt GH Oxman AD Schünemann HJ Tugwell P Knottnerus A . GRADE Guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. (2011) 64(4):380–2. 10.1016/j.jclinepi.2010.09.011
50.
Sukhera J . Narrative reviews: flexible, rigorous, and practical. J Grad Med Educ. (2022) 14(4):414–7. 10.4300/JGME-D-22-00480.1
51.
Ryan R . Cochrane Consumers and Communication Review Group. Heterogeneity and Subgroup Analyses in Cochrane Consumers and Communication Group Reviews: Planning the Analysis at Protocol Stage. Cochrane (2021). Available online at:http://cccrg.cochrane.org (Accessed October 03, 2023).
52.
Higgins JPT López-López JA Becker BJ Davies SR Dawson S Grimshaw JM et al Synthesizing quantitative evidence in systematic reviews of complex health interventions. BMJ Glob Health. (2019) 4(1):e000858. 10.1136/bmjgh-2018-000858
53.
McMaster University. Home—McMaster evidence review & synthesis team. (not dated). Available online at:https://merst.healthsci.mcmaster.ca/(Accessed March 1, 2023).
54.
Statology. Confidence Interval Calculator for Proportions. Statology (2023). Available online at:https://www.statology.org/confidence-interval-proportion-calculator/(Accessed April 23, 2023).
55.
Kostoff M Burkhardt C Winter A Shrader S . An interprofessional simulation using the SBAR communication tool. Am J Pharm Educ. (2016) 80(9):157. 10.5688/ajpe809157
56.
Choi YR Chang SO . Exploring interprofessional communication during nursing home emergencies using the SBAR framework. J Interprof Care. (2023) 37:83–90. 10.1080/13561820.2021
57.
Hum RS . Cognitive disconnect and information overload: electronic health record use for rounding and handover communications in a pediatric intensive care unit. In: ZhengKWestbrookJKannampallilTPatelV, editors. Cognitive Informatics. Health Informatics. Cham.: Springer (2019). p. 297–306. 10.1007/978-3-030-16916-9_18
58.
Lee KR Kim EJ . Relationship between interprofessional communication and team task performance. Clinical Simulation in Nursing. (2020) 43:44–50. 10.1016/j.ecns.2020.02.002
59.
Shrader S Dunn B Blake E Phillips C . Incorporating standardized colleague simulations in a clinical assessment course and evaluating the impact on interprofessional communication. Am J Pharm Educ. (2015) 79:57. 10.5688/ajpe79457
60.
Barnett S Nagy MW Hakim RC . Integration and assessment of the situation-background-assessment-recommendation framework into a pharmacotherapy skills laboratory for interprofessional communication and documentation. Curr Pharm Teach Learn. (2017) 9:794–801. 10.1016/j.cptl.2017.05.023
61.
Acharya R Thomas G Hellaby M . Evaluation of a clinical handover simulation training session for junior doctors in psychiatry. BMJ Simul Technol Enhanc Learn. (2016) 3:23–7. 10.1136/bmjstel-2016-000114
62.
Brust-Sisti LA Sturgill M Volino LR . Situation, background, assessment, recommendation (SBAR) technique education enhances pharmacy student communication ability and confidence. Curr Pharm Teach Learn. (2019) 11(4):409–16. 10.1016/j.cptl.2019.01.006
63.
Jeong JH Kim EJ . Development and evaluation of an SBAR-based fall simulation program for nursing students. Asian Nurs Res. (Korean Soc Nurs Sci). (2020) 14(2):114–21. 10.1016/j.anr.2020.04.004
64.
Noh GO Park MJ . Effectiveness of incorporating situation-background-assessment-recommendation (SBAR) methods into simulation-based education for nursing students: a quasi-experimental study. Nurse Educ Today. (2022) 109:105252. 10.1016/j.nedt.2021.105252
65.
Cooper D Keiser M Berg K Sherman E . Improving interprofessional communication confidence among physical therapy and nurse practitioner students. Journal of Physical Therapy Education. (2019) 33:177–84. 10.1097/JTE.0000000000000092
66.
Franko TS 2nd Shah V Hong KL Bommareddy A . Evaluation of long term retention and utilization of the situation, background, assessment, recommendation (SBAR) communication technique. Curr Pharm Teach Learn. (2021) 13:122–6. 10.1016/j.cptl.2020.09.001
67.
Chen M Yin J Jia R Zhang H Yan R Zhang Y . Impact of ISBAR communication training on interpersonal communication and teamwork of residents in general practice standardized training. Technium Social Sciences Journal. (2020) 11:76–83. 10.47577/tssj.v11i1.1609
68.
Yeh V Sherwood G Durham C Kardong-Edgren S Schwartz T Beeber L . Online simulation-based mastery learning with deliberate practice: developing interprofessional communication skills. Clin Simul Nurs. (2019) 32:27–38. 10.1016/j.ecns.2019.04.005
69.
Marshall S Harrison J Flanagan B . The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care. (2009) 18:137–40. 10.1136/qshc.2007.025247
70.
Mutter MK Pedersen K Cunningham T Martindale JR . Feedback methods in an interprofessional mock paging program. Med Sci Educ. (2021) 31:2001–5. 10.1007/s40670-021-01445-1
71.
Janaway B Zinchenko R Anwar L Wadlow C Soda E Cove K . Using SBAR in psychiatry: findings from two London hospitals. BJ Psych Open. (2021) 7(1):S197. 10.1192/bjo.2021.530
72.
Abela-Dimech F Vuksic O . Improving the practice of handover for psychiatric inpatient nursing staff. Arch Psychiatr Nurs. (2018) 32:729–36. 10.1016/j.apnu.2018.04.004
73.
Lee H Jang SJ . Effects of flipped-learning-based simulation for nursing students: a retrospective survey. Int J Ment Health Nurs. (2021) 30:1263–73. 10.1111/inm.12885
74.
Ting WH Peng FS Lin HH Hsiao SM . The impact of situation-background-assessment-recommendation (SBAR) on safety attitudes in the obstetrics department. Taiwan J Obstet Gynecol. (2017) 56:171–4. 10.1016/j.tjog.2016.06.021
75.
Raurell-Torredà M Rascón-Hernán C Malagón-Aguilera C Bonmatí-Tomás A Bosch-Farré C Gelabert-Vilella S et al Effectiveness of a training intervention to improve communication between/awareness of team roles: a randomized clinical trial. J Prof Nurs. (2021) 37:479–87. 10.1016/j.profnurs.2020.11.003
76.
Spooner AJ Aitken LM Corley A Chaboyer W . Developing a minimum dataset for nursing team leader handover in the intensive care unit: a focus group study. Aust Crit Care. (2018) 31:47–52. 10.1016/j.aucc.2017.01.005
77.
De Meester K Verspuy M Monsieurs KG Van Bogaert P . SBAR improves nurse-physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation. (2013) 84:1192–6. 10.1016/j.resuscitation.2013.03.016
78.
Temsah MH Abouammoh N Ashry A Al-Eyadhy A Alhaboob A Alsohime F et al Virtual handover of patients in the pediatric intensive care unit during the COVID-19 crisis. J Multidiscip Health. (2021) 14:1571–81. 10.2147/JMDH.S310028
79.
Tan XL Park H Patel J Murden M . Improving clinical handover on an electronic communication platform: a quality improvement project. Cureus. (2021) 13(10):e19156. 10.7759/cureus.19156
80.
Foronda C MacWilliams B McArthur E . Interprofessional communication in health care: an integrative review. Nurse Educ Pract. (2016) 19:36–40. 10.1016/j.nepr.2016.04.005
81.
Gleeson L O’Brien GL O’Mahony D Byrne S . Interprofessional communication in the hospital setting: a systematic review of the qualitative literature. J Interprof Care. (2023) 37:203–13. 10.1080/13561820.2022.2028746
82.
Land V Parry R Seymour J . Communication practices that encourage and constrain shared decision-making in healthcare encounters: systematic review of conversation analytic research. Health Expect. (2017) 20:1228–47. 10.1111/hex.12557
83.
Aungst TD Belliveau P . Leveraging mobile smart devices to improve interprofessional communications in inpatient practice setting: a literature review. J Interprof Care. (2015) 29:570–8. 10.3109/13561820.2015
84.
Ong ZH Tan LHE Ghazali HZB Ong YT Koh JWH Ang RZE et al A systematic scoping review on pedagogical strategies of interprofessional communication for physicians in emergency medicine. J Med Educ Curric Dev. (2021) 8:23821205211041794. 10.1177/23821205211041794
85.
Bok C Ng CH Koh JWH Ong ZH Ghazali HZB Tan LHE et al Interprofessional communication (IPC) for medical students: a scoping review. BMC Med Educ. (2020) 20(1):372. 10.1186/s12909-020-02296-x
86.
Etherington C Wu M Cheng-Boivin O Larrigan S Boet S . Interprofessional communication in the operating room: a narrative review to advance research and practice. Can J Anaesth. (2019) 66:1251–60. 10.1007/s12630-019-01413-9
87.
Lo L Rotteau L Shojania K . Can SBAR be implemented with high fidelity and does it improve communication between healthcare workers? A systematic review. BMJ Open. (2021) 11:e055247. 10.1136/bmjopen-2021-055247
88.
NHS England. SBAR implementation and training guide. Available online at:https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/SBAR-Implementation-and-Training-Guide.pdf(Accessed February 22, 2023).
89.
Rabøl LI Andersen ML Østergaard D Bjørn B Lilja B Mogensen T . Descriptions of verbal communication errors between staff. An analysis of 84 root cause analysis-reports from Danish hospitals. BMJ Qual Saf. (2011) 20:268–74. 10.1136/bmjqs.2010.040238
90.
Nadzam DM . Nurses’ role in communication and patient safety. J Nurs Care Qual. (2009) 24:184–8. 10.1097/01.NCQ.0000356905.87452.62
91.
Park LJ . Using the SBAR handover tool. Br J Nurs. (2020) 29:812–3. 10.12968/bjon.2020.29.14.812
92.
Ruhomauly Z Betts K Jayne-Coupe K Karanfilian L Szekely M Relwani A et al Improving the quality of handover: implementing SBAR. Future Health J. (2019) 6(2):54. 10.7861/futurehosp.6-2s-s54
93.
NICE [National Institute for Health and Care Excellence]. Quality Statement 4: Structure patient handovers. (2018). Available online at:https://www.nice.org.uk/guidance/qs174/chapter/Quality-statement-4-Structured-patient-handovers(Accessed May 30, 2023).
94.
Lu YL Zhu L Hou GH Gao XD Chen WX Liu HF et al Expert consensus on nursing management for patients undergoing primary percutaneous coronary intervention during the COVID-19 pandemic. Cardiol Plus. (2020) 5:81–8. 10.4103/cp.cp_9_20
95.
Stapleton HJ . COVID changes to post-anesthesia care unit nursing practices. J Perioper Nurs. (2021) 34(2):3. 10.26550/2209-1092.1113
96.
Lazzari C Shoka A Nusair A Rabottini M . Psychiatry in time of COVID-19 pandemic. Psychiatr Danub. (2020) 32:229–35. 10.24869/psyd.2020.22
97.
Lazzari C Nusair A Shoka A Hein SM Rabottini M . Case reports of first psychiatric presentations during CoViD-19 pandemic. Riv Psichiatr. (2020) 55:319–21. 10.1708/3457.34465
98.
de Senneville LL Brewin A Thomas A Calvert K . A qualitative analysis of adding kindness into the ISBAR handover tool. Aust N Z J Obstet Gynaecol. (2022) 62:901–5. 10.1111/ajo.13607
99.
Kaltoft A Jacobsen YI Tangsgaard M Jensen HI . ISBAR as a structured tool for patient handover during postoperative recovery. J Perianesth Nurs. (2022) 37:34–9. 10.1016/j.jopan.2021.01.002
100.
Neto JM Viana RA Franco AS Prado PR Gonçalves FA Nóbrega MM . Nursing diagnosis/outcomes and interventions for critically ill patients affected by COVID-19 and sepsis. Texto Contexto Enfermagem. (2020) 29:e20200160. 10.1590/1980-265X-TCE-2020-0160
101.
Lazzari C McAleer S Nusair A Rabottini M . Psychiatric training during COVID-19 pandemic benefits from integrated practice in interprofessional teams and ecological momentary e-assessment. Riv Psichiatr. (2021) 56:74–84. 10.1708/3594.35765
102.
Wees I Murtuza MI Mathisen D Zhang H Roy M Phelps E et al Improving the care of patients with COVID-19 with a medical student-run telemedicine clinic. BMJ Open Qual. ((2022)1) 1(1):e001646. 10.1136/bmjoq-2021-001646
103.
Jacob N Chaudhary O Darwish NM Vijay V Pardoe H . E-handover in surgery improves clinical efficiency and adherence to COVID-19 infection control measures. Cureus. (2021) 13:e13967. 10.7759/cureus.13967
104.
Tataei A Rahimi B Afshar HL Alinejad V Jafarizadeh H Parizad N . The effects of electronic nursing handover on patient safety in the general (non-COVID-19) and COVID-19 intensive care units: a quasi-experimental study. BMC Health Serv Res. (2023) 23:527. 10.1186/s12913-023-09502-8
105.
Wasserteil N Nun AB Mimouni FB Kasirer Y . Handover of patients: the challenges of COVID-19. J Perinatol. (2020) 40:1453–4. 10.1038/s41372-020-00792-y
106.
Theobald S Brandes N Gyapong M El-Saharty S Proctor E Diaz T et al Implementation research: new imperatives and opportunities in global health. Lancet. (2018) 392(10160):2214–28. 10.1016/S0140-6
107.
Martínez-Fernández MC Castiñeiras-Martín S Liébana-Presa C Fernández-Martínez E Gomes L Marques-Sanchez P . SBAR method for improving well-being in the internal medicine unit: quasi-experimental research. Int J Environ Res Public Health. (2022) 19(24):16813. 10.3390/ijerph192416813
108.
Ghosh S Ramamoorthy L Pottakat B . Impact of structured clinical handover protocol on communication and patient satisfaction. J Patient Exp. (2021) 8:2374373521997733. 10.1177/2374373521997733
109.
Fliegenschmidt J Merkel MJ von Dossow V Zwißler B . Strukturierte patientenübergabe in hochrisikobereichen: evidenz und empfehlungen für die praktische implementierung [structured patient handover in high-risk areas: evidence and recommendations for the practical implementation]. Anaesthesiologie. (2023) 72(3):183–88. (In German). 10.1007/s00101-022-01249-x
110.
Gadea-Company P Casal Angulo C Hurtado Navarro C . Impact of the implementation of identification-situation-background-assessment-recommendation (ISBAR) tool to improve quality and safety measure in a lithotripsy and endourological unit. PLoS One. (2023) 18(6):e0286565. 10.1371/journal.pone.0286565
111.
Kay S Unroe KT Lieb KM Kaehr EW Blackburn J Stump TE et al Improving communication in nursing homes using plan-do-study-act cycles of an SBAR training program. J Appl Gerontol. (2023) 42(2):194–204. 10.1177/07334648221131469
112.
Andreasen EM Høigaard R Berg H Steinsbekk A Haraldstad K . Usability evaluation of the preoperative isbar (identification, situation, background, assessment, and recommendation) desktop virtual reality application: qualitative observational study. JMIR Hum Factors. (2022) 9(4):e40400. 10.2196/40400
113.
Foster S Manser T . The effects of patient handoff characteristics on subsequent care: a systematic review and areas for future research. Acad Med. (2012) 87(8):1105–24. 10.1097/ACM.0b013e31825cfa69
114.
Moore M Roberts C Newbury J Crossley J . Am I getting an accurate picture: a tool to assess clinical handover in remote settings?BMC Med Educ. (2017) 17:213. 10.1186/s12909-017-1067-0
115.
Gordon M Hill E Stojan JN Daniel M . Educational interventions to improve handover in health care: an updated systematic review. Acad Med. (2018) 93(8):1234–44. 10.1097/ACM.0000000000002236
116.
Hales BM Pronovost PJ . The checklist—a tool for error management and performance improvement. J Crit Care. (2006) 21(3):231–5. 10.1016/j.jcrc.2006.06.002
117.
Platis C Theodoros A Psomiadi ME Theodorou P . Interdisciplinary collaboration and communication among doctors and nurses in ICUs during the COVID-19 pandemic and their importance in professional life quality improvement. In: VlamosP, editor. GeNeDis 2022. GeNeDis 2022. Advances in Experimental Medicine and Biology, vol 1425. Cham: Springer (2023). p. 331–43. 10.1007/978-3-031-31986-0_32
118.
Lazzari C Costley C Nikolou-Walker E . Interprofessional and Intraprofessional Teamwork and Handovers in Healthcare: Challenges and Recommendations from Work-based Learning. Faringdon: Libri (2024).
119.
Lazzari C . Theoretical frameworks of clinical handovers in healthcare settings. In: ItoS, editor. Research Highlights in Disease and Health Research, Vol. 4. London: BP International (2023). p. 125–47. 10.9734/bpi/rhdhr/v4/5177E
120.
Lazzari C . Implementing the verbal and electronic handover in general and psychiatric nursing using the introduction, situation, background, assessment, and recommendation framework: a systematic review. Iran J Nurs Midwifery Res. (2024) 29(1):23–32. 10.4103/ijnmr.ijnmr_24_23
Summary
Keywords
handover, handoff, ISBAR, SBAR, COVID-19, outcome, systematic review, meta-analysis
Citation
Lazzari C and Rabottini M (2025) The use of Introduction, Situation, Background, Assessment, and Recommendation handover in the COVID-19 pandemic and non-COVID clinical settings: a systematic review and meta-analysis. Front. Health Serv. 5:1380948. doi: 10.3389/frhs.2025.1380948
Received
02 February 2024
Accepted
22 July 2025
Published
07 August 2025
Volume
5 - 2025
Edited by
Rui Medeiros, Portuguese Oncology Institute of Porto (IPO Porto)/Porto Comprehensive Cancer Centre (Porto.CCC), Portugal
Reviewed by
Alexandre Morais Nunes, University of Lisbon, Portugal
Keith Ruskin, The University of Chicago, United States
Updates
Copyright
© 2025 Lazzari and Rabottini.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Carlo Lazzari carlolazzari2015@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.