Abstract
Background:
Implementation science in public health has facilitated the translation of research findings into effective public health programming and evidence-based policy decision-making. One of the most prominent implementation science methodologies is intervention mapping, briefly defined as a rigorous protocol that guides the design of multi-level health promotion interventions and implementation strategies. In this manuscript, we describe our use and adaption of intervention mapping in Medical-Legal Partnerships, which are an integration of comprehensive legal services within primary health care and social service spaces working to mitigate the effects of negative social determinants of health for persons with HIV (PWH).
Methods:
Intervention mapping in this study was modified from a six-step to a five-step approach by integrating Step 4 and Step 5 of the original version of intervention mapping. The rationale for combining Step 4 and 5 into one step was that coherent, independent intervention packages existed for the provision of legal and HIV services, and it was determined through Step 1 of intervention mapping that these two existing intervention approaches can be integrated at the organizational level but should remain collocated at the patient level. Thus, our modified intervention mapping steps consisted of: (1) conducted needs assessments among medical legal partnerships (MLP) programs (providers and patients) serving PWH in order to identify the current landscape of MLP adoption and implementation in HIV care contexts and common components of those programs; (2) generated organizational and practice-level implementation outcomes and objectives, determinants and change objectives matrices to guide each strategy; (3) chose methods and mechanisms of change of the overarching implementation strategy; (4) produced implementation protocols and materials; and (5) developed a plan to evaluate implementation outcomes.
Results:
Following intervention mapping author recommendations that not every step is needed in intervention mapping, using our modified intervention mapping approach resulted in a comprehensive organizational level intervention. Applying our adapted intervention mapping process resulted in the intervention package, OPAHL (Organizational Partnerships for Healthy Living), which currently is being tested for feasibility and preliminary effectiveness in a hybrid, randomized cluster trial in Philadelphia, Pennsylvania.
Conclusions:
The work presented here provides a practical framework that can be replicated by other researchers and practitioners working on the social epidemiology of chronic illness, communicable disease, and access to and engagement with care.
Introduction
Intervention mapping is a six-step approach that specifies processes for integrating empirical evidence and contextual-practical considerations within health intervention planning (1, 2). The standard intervention mapping approach has been demonstrated to be efficient in developing evidence-based interventions in areas of chronic illness, communicable disease, and behavioral change interventions (1–8). Implementation science analyses of intervention mapping suggest that, as a methodology, it increases the cultural relevance of intervention tools, proper adaptability, and effective target population uptake of interventions. Despite the multilevel features of intervention mapping, it has been mostly used for individual- and interpersonal-level interventions, with limited application to organizational level interventions (1–8). In response to these gaps, we intentionally used intervention mapping to develop an organizational level intervention to address the health-harming legal needs (HHLN) of PWH. This article describes our adapted version of intervention mapping to integrate the MLP approach into HIV care. Our learning offers an initial blueprint for communities seeking to strengthen HIV care through developing organizational level interventions to address socio-legal barriers to care—and health—through legal services.
Background
Since 2018, our investigative team has worked on examining the potential of integrating legal services into HIV care as a mechanism for addressing disparities in HIV care. Medical-legal partnerships (MLP) offer such a potential intervention opportunity. MLP is a healthcare delivery approach that integrates legal services into clinical, behavioral, and social services (9–15). MLPs were developed in order for medical providers to better identify and meet underrepresented patients’ legal needs (16, 17). Though MLPs typically show improved patient outcomes (18), some studies have shown mixed results (19).
From 1993 to 2017, 294 healthcare institutions across 41 states in the U.S. established Medical-Legal Partnership (MLP) programs, offering a multifaceted approach to healthcare delivery by integrating legal advocacy into medicine and health care practices (17, 20, 21). Following the Preferred Reporting Items for Systematic Review, Martinez and colleagues systematically reviewed studies published from January 1993-August 2015 to investigate the capacity of MLP programs to address health disparities and access to justice challenges (13). Thirteen relevant studies from an initial pool of 355 records were identified. Only four studies addressed the effect of MLP interventions on patient health outcomes (22–24, 59). Among these empirical studies, MLPs improved patients' environmental conditions by meeting legal needs and increasing their access to, and retention in, both health services and health-promoting resources such as SNAP (22, 25–27). There also was clear evidence that MLP programs can financially benefit not only patients—through medical debt relief and mitigation—but also the partnering healthcare organizations in the form of reduced organizational costs (24, 28, 29).
MLPs have the potential to improve HIV continuity of care (30–33). Yet MLPs are underutilized in systems of care serving people with HIV or to specifically address their legal needs (34, 35). Implementation science methodologies, such as intervention mapping, can facilitate the adoption and integration of existing intervention packages into health and social services organizations (36–38).
To advance the growing field of implementation science in public health, this manuscript presents a practical application and adaptation of intervention mapping to support the integration of MLPs into HIV care settings. Specifically, we outline a modified five-step intervention mapping process used to design and implement OPAHL (Organizational Partnerships for Healthy Living), an organizational-level intervention aiming to mitigate the impact of negative social determinants of health on persons with HIV. The objectives of this manuscript are to (1) describe the rationale and methodology behind adapting the traditional six-step intervention mapping protocol, (2) detail the steps used to co-develop and tailor MLP implementation strategies in HIV care settings, and (3) present the resulting intervention framework currently being evaluated for feasibility and preliminary effectiveness.
Methods
Participants and recruitment
We identified programs with existing or planned services for persons with HIV (PWH) and invited MLP staff (e.g., attorneys, case managers, paralegals) and affiliated HIV care providers (e.g., clinicians, social workers, administrators) to participate. Participants were recruited via email and direct outreach from project collaborators.
Data collection
To inform Step 1 of intervention mapping, we conducted a mixed-methods implementation needs assessment using both survey instruments and semi-structured interviews. Surveys included both closed- and open-ended questions on current MLP activities, perceived barriers and facilitators to integration with HIV services, training needs, and organizational readiness. Interview questions further explored program structure, collaborative practices, staff roles, communication processes, and observed legal needs among PWH. We also collected relevant documentation from MLPs (e.g., intake forms, training materials, workflows) for supplemental content analysis.
Thematic analysis
We applied thematic analysis (39) to the open-ended narrative responses from interviews and survey instruments, following Braun and Clarke's six-phase framework: (1) familiarization with data, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes, and (6) producing the report. Data were coded independently by two members of the research team using both deductive codes derived from constructs and inductive codes that emerged from the data. Discrepancies were resolved through consensus meetings, and coding consistency was assessed through inter-rater reliability checks. Emergent themes were mapped to provide a structured understanding of MLP implementation in HIV settings. In addition to thematic analysis, content analysis of program materials was conducted to identify the most common components and workflows in use across sites. This dual approach enabled us to triangulate findings and identify key implementation barriers and facilitators, which informed the development of logic models, performance objectives, and strategy selection in subsequent intervention mapping steps.
Application to intervention mapping steps
Empirical evidence exists supporting the use of intervention mapping as an innovative methodological approach for building intervention models that can be implemented and tested (40, 41). The design of sustainable interventions that achieve desired outcomes requires transparent, rigorous processes (5). For these reasons, we used the intervention mapping approach, as opposed to PRECEDE-PROCEED, ADAPT-ITT, colocation or other intervention design methodologies to design our MLP integration into HIV care services intervention package.
Figure 1 illustrates our adapted five-step intervention mapping process. While we retained the core principles of the original intervention mapping framework, our most significant methodological adaptation was the integration of Step 4 (program production) into Step 5 (adoption and implementation). Step 4 traditionally focuses on organizing intervention components into a coherent program, but through our initial needs assessment (Step 1), we identified that robust, independent intervention packages already exist for both legal services (via Medical-Legal Partnerships) and HIV care. These interventions are implemented by trained professionals in their respective domains—attorneys and medical providers—following established protocols. Rather than reconfigure these interventions at the patient level, our analysis revealed the greater opportunity and need to integrate them at the organizational level while maintaining their separate identities during patient service delivery. This strategic decision ensures that patients benefit from co-located but distinct services that preserve professional boundaries while fostering collaborative care.
Figure 1
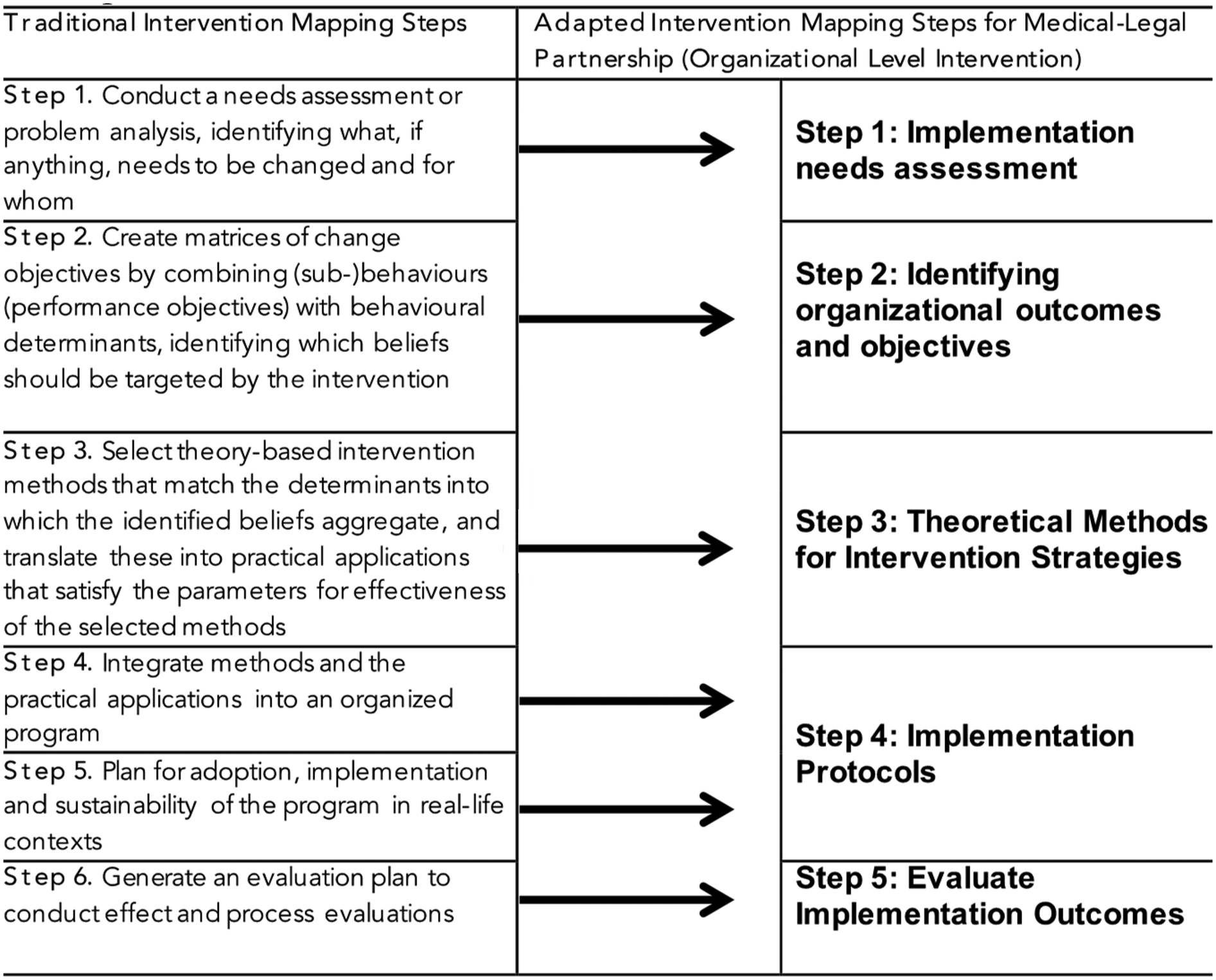
Adapted intervention mapping steps for development of an intervention to integrate a medical-legal partnership approach to HIV care services.
This shift in focus required an enhanced emphasis on the systems-level integration, implementation logistics, and sustainability planning typically housed in Step 5. We prioritized understanding how to embed MLPs within existing HIV care infrastructure in ways that are feasible, acceptable, and effective. This aligns with the flexibility endorsed by the developers of intervention mapping, who recognize that certain steps may be modified or omitted based on the intervention context and readiness. As such, our adapted five-step model includes: (1) conducting an implementation needs assessment, (2) identifying multi-level outcomes and objectives, (3) selecting theoretical methods and change strategies, (4) developing site-specific implementation protocols, and (5) evaluating implementation outcomes. This tailored approach allowed us to create an integrated yet scalable intervention grounded in real-world conditions and informed by community and provider perspectives.
Results
The first step of our intervention design was to convene a planning advisory working group consisting of two collaborative boards (scientific and community), drawing on Pinto et al. (42) approaches to community engagement in HIV research. The community collaborative board met in person at Temple University College of Public Health with an attendance of 30 individuals in that initial meeting. The scientific advisory board first meeting was online to discuss the project. From the community and scientific collaborative board we created a subgroup, the planning advisory working group which included: (1) investigators, (2) a core group of eight MLP practitioners who are experts in their fields, including clinical care, legal services, health care administration, behavioural and social services (3) four health services researchers with expertise in the HIV care continuum; and (4) twenty people with HIV, adults, residents of Philadelphia, Pennsylvania. We organized ten planning advisory working group meetings around the intervention mapping steps.
Adapted intervention mapping step 1: implementation needs and assets assessment
The planning advisory group provided feedback to the investigative team in designing the needs and assets assessment. We decided to conduct and need and assets assessment that consisted of three components: (1) online survey with existing MLP practices that may serve PWH; (2) online survey with PWH who have received legal services to address their HHLN; (3) open-ended interviews with MLP practitioners; and (4) content analysis of secondary information provided by MLPs. The list of MLPs was obtained from the National Center of Medical Legal Partnerships. To participate in the assessment, individuals had to verify that (1) they were part of an operational MLP program with integrated legal services, on-site or off-site; (2) the program had been operating for at least one year and they had been part of the program's service delivery for at least one year; and (3) at least fifty percent of the patients served by the program, during the six months prior to our research communication, were PWH.
The objectives of the needs/assets assessment were: (1) to identify existing best practices among current MLP programs to address legal barriers to care and health for clients/patients with HIV; and (2) to assess the effects of current MLP programming and practices on HIV care continuum indicators. The online survey and open-ended interview instruments were designed using the EPIS framework for examining inner and outer factors in adopting innovations (43). In this case, the potential innovation is the integration through colocation of legal services in HIV services facilities. Recruitment for the online survey was a challenge, with close to 20% response from all MLPs nationwide, and 15% meeting our organizational eligibility criteria. A subsample of the survey participants was selected to participate in the open-ended interviews. Selection was based on availability and willingness to participate in the interviews. Open-ended, informal interviews were conducted in person with 6 providers at The Philadelphia AIDS Consortium (Philadelphia, PA- 1 participant), Betances (New York, NY-1 participant), Us Helping Us (Washington, DC-1 participant), and Whitman Walker (Washington, DC-3 participants) Further, in Step 1 we were able to recruit n = 111 MLP practitioners who participated in the online survey with existing MLP practices that may serve PWH, including providers from for-profit (0.9%) and non-profit organizations (62.2%) as well as some unknown (36.9%). Providers who completed the surveys were Administrators (15.3%), Clinicians (22.5%), Lawyers (36%), and Social Service providers (26.1%) (44).
The investigative team conducted tabulated the online survey findings and conducted basic descriptive statistics. We also conducted thematic analysis of the open-ended interview narrative materials and content analysis of the reports and materials provided by the MLPs to determine the common themes in barriers and facilitators to addressing HHLN for PWH.
A majority of providers (76.9%) identified the need for better tools to screen for HHLN, while 39.1% reported limited collaboration with legal partners. Organizational capacity was a major concern, with one administrator stating, “We have only been operating for 2 years, and we are a staff of two—one MLP attorney and one program coordinator. We could already use another attorney”. Structural limitations were also noted: “Coordinating the logistics of all the services we provide with limited staff” (social/behavioral health provider), and “Funding. Funding. Funding”. (lawyer) were common refrains. Legal providers also highlighted the burden of being under-resourced, especially in time-intensive cases: “Legal cases take time and one lawyer cannot handle as many cases as one doctor sees patients”. Systemic misalignment between healthcare and legal domains was another theme: “Medical providers’ policies aren’t always clear… we get sent back and forth between supervisors”, and “Hospital partners don’t always respect attorney-client confidentiality or how time sensitive fixing problems can be” (lawyers). These concerns reflected deeper interprofessional tensions and challenges in establishing effective interdisciplinary workflows.
Despite these barriers, the assessment also documented important facilitators and benefits. Providers praised the model's ability to reach clients who otherwise would not seek legal help: “One-stop shop for patients who need services. we feel we are able to address a population who does not actively seek out legal aid” (lawyer). Integration into clinical workflows enabled more holistic care: “It's so nice to work as a team with social workers and providers to give the best service to patients” and “Working in a health setting and in collaboration with a healthcare provider improves patient care” (lawyers). Several lawyers emphasized the health impact of legal services: “The help of a lawyer can improve patient health”, and “An MLP is able to identify and address root legal issues before they reach a crisis point and cause health crises”.
Thematic findings from this assessment were triangulated with survey results and presented to the planning advisory group, which used them to inform two logic models: (1) a logic model of risk focused on unaddressed HHLN for PWH, and (2) a logic model of change outlining necessary organizational and system-level shifts to detect and mitigate HHLN. From these, we established our primary health outcome: reducing HIV viral load to undetectable levels within six months of care engagement through the resolution of legal and social barriers.
Five key stakeholder groups were identified to operationalize this intervention: (1) PWH with unsuppressed viral loads and HHLN; (2) healthcare and social service providers in community health centers; (3) administrators and organizational leaders; (4) legal aid organizations geographically proximal to HIV service sites; and (5) attorneys providing direct legal services.
Adapted intervention mapping step 2: identifying stakeholders' outcomes and performance objectives
In this step 2, we develop matrices that combine the desired behaviors identified in the logic model of change and the hypothesized environmental conditions, factors, and determinants that lead to those desired behaviors, thus creating measurable competencies (defined here as objectives that will result in the desired change). Below we list the desired behaviors by type of stakeholder:
- •
Administrators of partnering community health centers and legal aid organizations: (1) facilitating the implementation of MLP programming meetings with internal operations and external collaborators; and (2) providing ongoing support for the effectiveness and sustainability of the MLP program.
- •
Medical, health, and social services providers: (1) identifying HHLN within clinical, behavioural, and social services encounters; (2) screening and referring patients with identified HHLN to MLP legal services providers; (3) alerting legal services colleagues to any health conditions that may impact efforts to address HHLN (assuming patients have authorizing this transmission of protected health information); and (4) coordinating communications between medical and legal providers as part of ongoing, sound case management for PWH.
- •
Legal services providers: (1) managing the consent/authorization process with legal clients that can enable the legal team to transmit case update information to the patient's medical and/or social services teams, as appropriate and necessary; (2) reinforcing, as part of that consent/authorization process, that a patient/client still can receive legal services even if they decline to permit communication between legal advocates and medical or social services staff, without any negative impact on the attorney-client relationship (although the lack of information-sharing sometimes can impact the strength of advocacy in certain contexts); (3) confirming the specific legal needs as to which the attorney will provide legal representation to the client; (4) confirming the specific legal needs for which the patient/client will be offered referral to other organizations with aligned expertise and capacity; and (5) providing regular workshops for patients and collaborating medical sites on recurring legal concerns.
In our step 2, we used the matrices to operationalize each of the above desired behaviors further into sub-tasks, or performance objectives. After each performance objective was identified, the investigative team, conducted a literature review of behavioral change among providers and consulted with the planning advisory working group to identify determinants of change, i.e., what cognitive resources, material resources, and affective resources would be needed to motivate the stakeholder to achieve the task. We selected determinants from the Diffusion of Innovations Theory and from Organizational Innovations Change Theory (
45–
48) and identified six core determinants with various degrees of applicability to each of the performance objectives: (1) awareness knowledge; (2) procedural knowledge; (3) motivation for innovation; (4) outcomes expectations; (5) organizational culture; and (6) reinforcements. Following, Fernandez, et al. (
49), we asked what members of the planning advisory group what resources were needed to change in the determinants listed above to accomplish the performance objective. Those responses became the competencies guiding the intervention that was being developed.
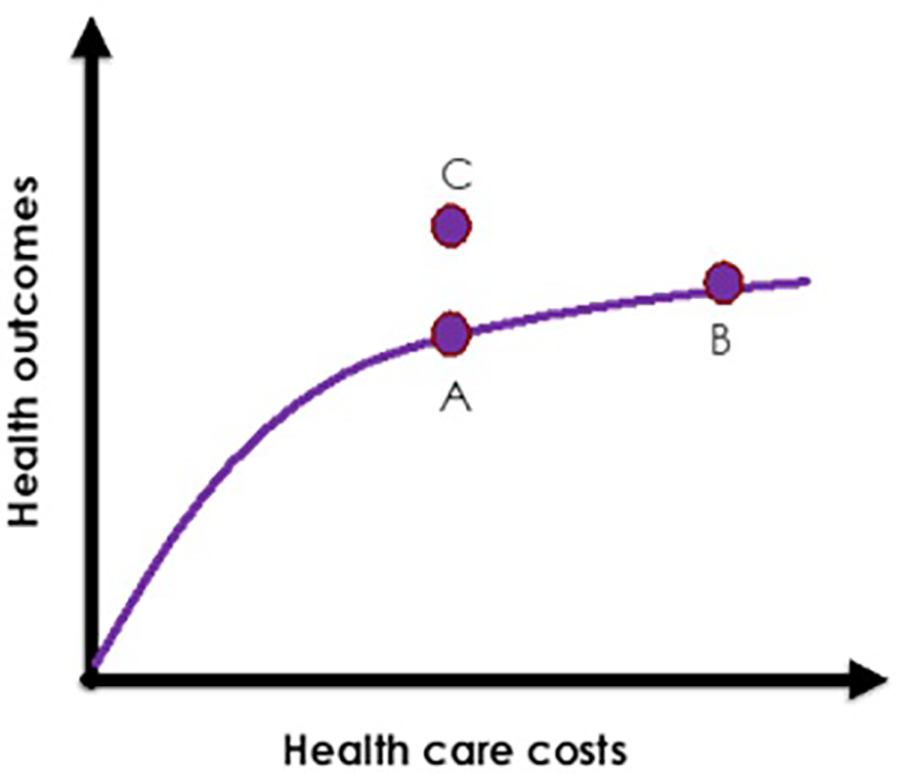
Conceptual basis of intervention
As a result of Step 1 and 2 exercises and discussions with the planning advisory group, the investigative team developed the conceptual basis of the intervention. Building on the literature of integrative care (50, 51), the conceptual basis of our proposed intervention is two folds: (1) in order to provide comprehensive HIV care, we first must identify the HHLN that reduce or prevent access to care in the first place; and, (2) integration of legal and HIV services should be grounded in a basic economic model of integration and co-location of healthcare services. Thus, we selected the Evans Health Economic model illustrated in Figure 2 to achieve better health outcomes without a significant cost increase (52). In Figure 2, Point B represents higher health care costs for slightly better health outcomes (point A). Point C represents achievement of a better health outcome (than point A) without increased costs (such as in Point B). This conceptual basis was based on discussions of the planning advisory group and would need to be tested empirically to be further validated. The planning advisory group agreed that an MLP PWH who have undetectable viral loads cannot transmit HIV, therefore, increasing the number of PWH who are virally suppressed is a national priority (53). For every person not infected with HIV, there is a lifetime cost savings of $367,134 per person in potential lifetime HIV treatment costs (54).
Figure 2
OPAHL synergistic continua of care for people with HIV (PWH).
Adapted intervention mapping step 3: theoretical methods for intervention strategies
We grouped the competencies created in Step 2 according to their respective determinants. We brainstormed and conducted additional literature reviews of the most effective learning constructs and concrete strategies to achieve the designated competencies. For example, in Step 2 we identified the key competencies for medical, health and social services providers to achieve both individual- and organization-level impacts: (1) Explain the importance of MLP services for PWH; (2) Explain the MLP program structure for PWH; (3) List the problem-solving strategies to connect and participate in MLP from the perspectives of providers and patients; (4) Express positive disposition towards innovative, holistic services for PWH; (5) Express positive disposition towards screening for health-harming legal needs; (6) Express support for integration of legal services into HIV care; and (7) Understand that MLP program implementation will reduce health care costs for out of care PWH. This intervention should increase awareness, knowledge, motivation for innovation, and outcome expectations (briefly defined as subjective estimates of how likely it is that a specific behaviour will be followed by consequences) through the following educational methods: (1) consciousness raising, (2) chunking of information, (3) information transfer, (4) persuasive communication, and (5) constructive argument.
Strategies for effective implementation included tailoring of best-practice communication and information- sharing protocols, anchored in patient autonomy and choice. Through this design step, we decided on using the following educational-intervention strategies by: (1) person-to-person meetings with administrators of health centers and legal aid organizations; (2) in-person training on HHLN for medical, health and social services providers; (3) in-person training on the HIV continuum of care for legal services providers.
At the end of this Step, we collected all the educational strategies together and identified five stages for education of stakeholders: identification of health-harming legal need(s); offering of, and referral to, legal services; engagement in legal services; resolution of legal concern(s); and ongoing access to legal support (see Figure 3).
Figure 3
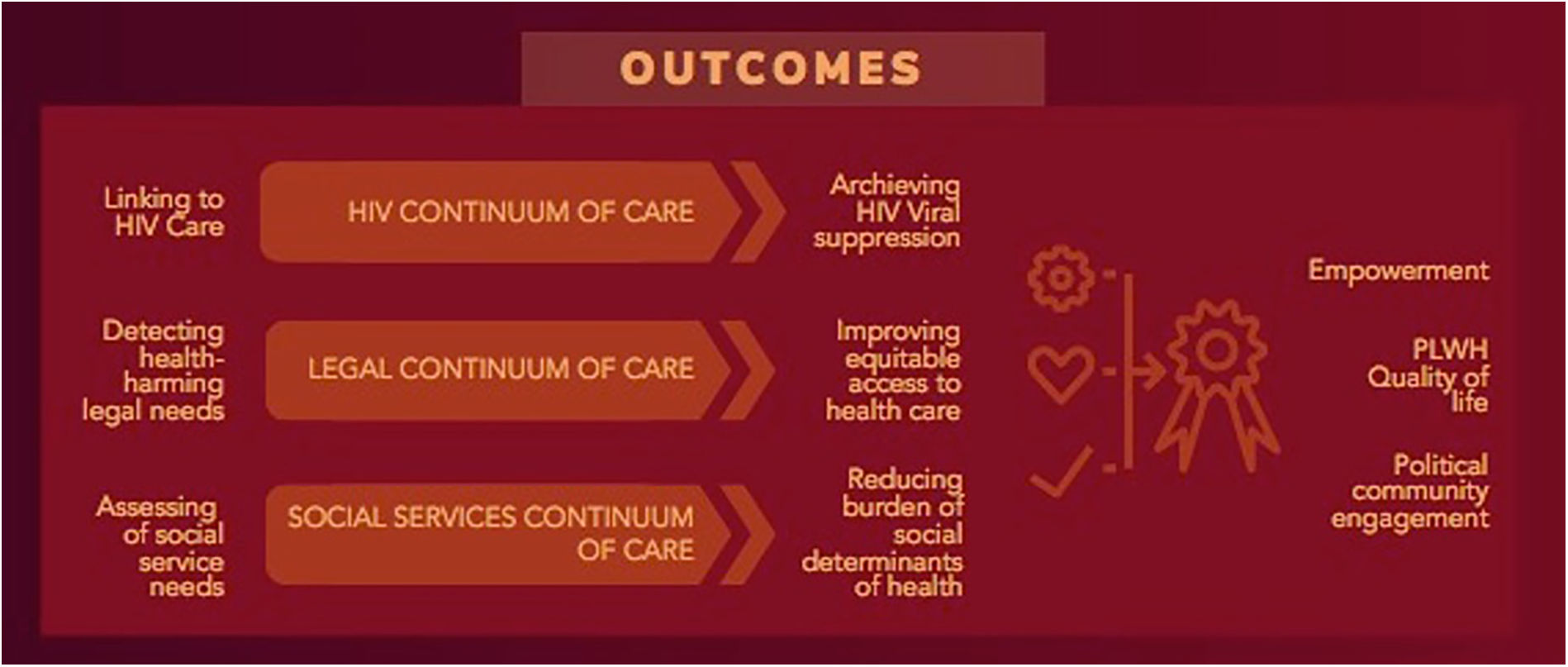
Illustration of Evan's Health Economic model.
Adapted intervention mapping step 4: implementation protocols
This step focuses on building a plan for building and implementing the intervention.
Generating the name of the intervention
A member of the team suggested the name, Organizational Partnerships for Healthy Living, OPAHL, because of the importance of building interorganizational partnerships. The name was adopted for our MLP intervention package.
Development of program materials
In Steps 2 and 3, we developed and cross-checked all the content for each component of the intervention. Because of the high level of prior training and education of our intervention targets (e.g., licensed attorneys, licensed physicians and nurses) at the organizational level, all materials geared to organization-level impact were developed at a high level of literacy. Lawyers, physicians, psychologists, health educators, and social workers of the advisory planning group were asked to provide feedback in the review of intervention materials to identify and simplify professional jargon.
Program overview
Our intervention leverages medical care expertise to enable access to legal support, potentially increasing the benefits to detecting and addressing HIV patients experiencing HHLN. Three factors were identified by the advisory planning group as necessary for a feasible MLP program implementation: (1) coordination of clinical, behavioural, social, and legal services; (2) an effective protocol to identify HHLN and offer/refer patients for legal support; and (3) siting of legal services on-site at the health clinic. Against this backdrop, the OPAHL intervention package consists of three components.
Component 1 is a comprehensive training for all MLP care providers delivered to clinical, behavioural, social, and legal staff together to establish a collaborative environment and relationship. This training is to be delivered by an expert team experienced in MLP implementation.
Component 2 consists of the screening tool and screening protocol to identify health-harming legal needs of PWH patients. The screening tool, based on a screening tool developed by the National Center for Medical-Legal Partnership, provides a comprehensive guide to identify potential legal concerns of PWH patients (55). This screening, administered by a member of the clinic's staff, offers the initial point of entry to potential legal services. This is a core node of the OPAHL intervention, as a positive screening (a screening is positive if at least one legal need is identified) triggers the initial offer of connection to legal support.
Component 3 includes the provision of legal services by legal advocates. Upon a positive legal needs screening, a case manager or social services provider connects the patient to the co-located lawyer, giving the patient the option to engage the services of the attorney and address the identified legal concern(s) with legal representation.
The OPAHL training curriculum is a combination of readings and in-person training that provides the knowledge and skills needed to integrate legal and HIV services. The content covers a variety of topics, including social determinants of health; HHLN and their impact on PWH; legal aid as health care; HIV synergistic continua of care; and MLP in action. The training is designed to be conducted in collaboration with organizations and/or experts experienced in MLP implementation.
We piloted the OPAHL training manual in a two day in-person sessions with members of an HIV services and a legal aid organization in Philadelphia. We modified the training based on the sessions feedback resulting in three pre-training readings (approximately 2 h) slide-animated presentations (approximately 1 h), and two-day sessions of interactive discussions delivered in-person (approximately 7 h, exclusive of breaks). The OPAHL training focus is not on the practices of law, medicine, nursing or social work, but rather how systems thinking with regards to the detection of HHLN and the linkage and retention in legal care.
In addition to the implementation characteristics noted above, this Step of the intervention mapping process helped to clarify important features of the scope and limitations of OPAHL. OPAHL will offer direct legal services for a broad range of civil law (as opposed to criminal law-based) needs that impact health. Most legal aid organizations are funded by the Legal Services Corporation (LSC), a publicly funded non-profit corporation established by the U.S. Congress in 1974. LSC funding prohibits the use of its funds for representation of people in several contexts, including criminal cases and several categories of people who are not U.S. citizens; limited exceptions exist. Thus, OPAHL likely will not directly enhance patient access to criminal law defense resources; and depending on the funding of the legal partner characteristics, OPAHL may bolster access to immigration law resources for PWH.
Ideal site for implementation
The planning advisory group decided that to most effectively monitor the implementation of OPAHL in achieving its health outcomes, it is best to be implemented in federally qualified health centers (FQHC). FQHC have the infrastructure and capacity of maintaining health and social services records for patients; provide on-site medical care; and conduct a comprehensive evaluation of the OPAHL implementation (see Step 5).
Planning for sustainability
Potential participating FQHCs will sign letters of support. The OPAHL planning advisory group designed a “pitch” one-to-one intervention activity with administrators consisting of three in-person meetings with the OPAHL team and the leadership of at least one local legal aid organization. As part of this step, the intervention team works with the selected FQHC and legal aid collaborators to create a Memorandum of Understanding (MOU). This MOU outlines the mission and goals of the partnership(s), designates roles and responsibilities between FQHC and legal services, and identify the organizational contributions of all partner organizations. The initial expectation is that the FQHC will provide legal colleagues with office space, computer, phone, and necessary access to patient files and records. The legal aid organization(s), in coordination with the intervention team, will minimally designate protected time of an attorney licensed to practice in the state as well as protected time of paralegal resources, and will provide to that legal team office space as well as telephones and computer systems at the legal aid office. Within 4–6 months of executing the Memorandum of Understanding, it is expected that the components described above under Step 3 will begin.
Two tasks are critical for the adoption-implementation step: (1) the internal collection of data on exposure to the intervention components, and (2) the monitoring of patients'/clients' progress along the HIV continuum of care and the phases of MLP-enabled legal advocacy. For the first task, OPAHL requires the OPAHL staff paralegal, in collaboration with FQHC staff, to collect health and social services exposure data, following an OPAHL- designated protocol (assuming patients have consented to this information transmission). For the second task, attorneys will coordinate with FQHC administrators to integrate de-identified MLP program observations and trends into regular clinic dialogues.
Adapted intervention mapping step 5: evaluate implementation outcomes
Guided by the adapted intervention mapping steps 1 through 4, we specified the desired intervention outcomes, predictors, mediating variables, and process evaluation indicators (see Table 1). The intervention mapping process also enabled us to identify the most appropriate evaluation models. We utilized the RE-AIM (Reach, Effectiveness, Adoption, Implementation, and Maintenance) and the EPIS frameworks to design an evaluation plan. In this Step, we develop a feasibility trial proposal to examine the implementation and preliminary efficacy of OPAHL. Together with the planning advisory group, and other collaborative organizations, we were externally funded to evaluate OPAHL in Philadelphia, PA. In Step 5, we added additional members to the planning advisory group, including epidemiologists, health economists and statisticians. Completing Step 5 of intervention mapping was critical in developing an evaluation plan that was realistic and feasible to be implemented in three-way organizational partnership: health care center (FQHC), legal aid services organization, and investigative-research organization.
Table 1
| Objectives | Measures (Indicator of success) |
|---|---|
| (1) To assess the feasibility of the processes that are critical to the success of the subsequent efficacy trial. |
|
| (2) To identify the time and resource problems that can occur during the subsequent trial. |
|
| (3) To forecast potential management problems. |
|
Implementation indicators guided by Re-AIM (56).
Discussion
Epidemics driven by structural factors, such as HIV, require multi-level interventions that account for individual, organizational, and structural variables. Intervention mapping allowed the planners, through iterative processes, to identify key domains of intervention, leverage important assets, and design a multilevel, evidence-based intervention. Intervention mapping facilitates planning and design for dissemination, implementation, and maintenance of evidence-based interventions in practice. Given the promise of ecological approaches, we implemented intervention mapping methodology identified by Fernandez, et al. (5, 36) including the application of theory, evidence, and incorporation of care and service providers and community stakeholders into the intervention design process (36).
We identified four challenges in the process of designing OPAHL using intervention mapping. First, most intervention design methodologies are geared to individual-level (patient-level) interventions and outcomes. To overcome this challenge, we drew heavily on the qualitative data collected during Step 1 of our adapted intervention mapping process. This qualitative data reflected important inputs from MLP program delivery actors (largely professionals and paraprofessionals) who could offer observations of how their organizations' operational and cultural characteristics can impact successful MLP program implementation, impact, and sustainability. Second, there are inherent epistemological differences between the fields of medicine, behavioral health, social services, law and public heath that can affect their frameworks for intervention planning. However, integration of services aligned with each of these fields (and likely additional fields) is essential to tackle the growing HIV epidemic in the U.S.; particularly among subgroups including immigrants, sexual and gender minorities, and racial/ethnic minorities. Preliminary research has documented the positive impacts of care integration approaches, including legal services integration, on individual-level health outcomes (11, 57). Third, the study findings revealed that diverse systems of care deploy a range of documentation systems (e.g., electronic health records, legal case management databases, mental health records that are subject to a higher level of confidentiality and privacy, etc.) and are subject to a range of professional responsibility obligations relating to confidentiality and mandated reporting of suspected neglect or abuse. However, recent literature has shed light on potential strategies to address confidentiality navigation and management challenges (58), including the creation of comprehensive data-sharing standard agreements (for organizations) and informed consent forms (for patients) that clearly explain allowable data usage and access. Fourth, in the healthcare ecosystem, which occupied 17.3% of U.S. Gross Domestic Product in 2022, there is profound concern about the economic sustainability of integrated approaches to care; especially those perceived to require large, ongoing funding streams to be sustainable. We urge researchers to promote the importance of multi-level, sequenced implementation steps to iteratively design for sustainability. In addition, research studies should be conducted to assess the cost-effectiveness of MLP program interventions.
Using intervention mapping was time consuming. The time and effort dedicated to assembling, organizing, and facilitating working meetings with the planning advisory working group was significant, but relatively negligible compared to the time and effort expended “behind the scenes” preparing materials for each meeting and completing deliverables stipulated by the planning advisory working group. We completed Step 1 in 12 months. A total of 616 salaried hours of intervention designers' time, and 1,400 salaried hours of staff time, were dedicated to Step 1. We completed Steps 2 through 5 in approximately 6 months, with an estimated total of 403 salaried hours of salaried intervention designers' time, and 840 salaried hours of staff time were dedicated to these steps. We found the use of intervention mapping critical to supporting design rigor and intervention quality for the OPAHL package; this presents a major advantage in designing a multi-level intervention that has high potential for adoption and sustainability. After the development of the OPAHL intervention package, OPAHL was funded by the National Institute of Mental Health (NIMH) to be tested for large scale feasibility and preliminary effects in randomized cluster trial in the city of Philadelphia, Pennsylvania, United States (grant # 1R34 MH125718-01A1; 2021–2024).
An important implication of this work lies in its alignment with the shifting priorities of the National Institutes of Health (NIH), particularly amid recent funding cuts to HIV prevention and care. Rather than retreating from structural interventions, federal agencies should expand investment in community-informed, multi-level strategies that address the root causes of health inequities. Our findings offer a timely, evidence-based framework for integrating MLPs into HIV service delivery. Developed through a rigorous, participatory process, the OPAHL intervention exemplifies a sustainable and scalable approach that embeds social determinants of health into care models. This work underscores the urgent need for stable, long-term funding mechanisms that support complex, structural interventions beyond short-term demonstration projects.
Limitations
This study has several limitations. Firstly, the modification of the intervention mapping process from a six-step to a five-step approach may have led to oversimplification or omission of critical components, potentially impacting the comprehensiveness and effectiveness of the intervention design. Additionally, the needs assessments conducted among Medical-Legal Partnership (MLP) programs may not fully capture the diverse perspectives and experiences of all stakeholders involved, including providers, patients, and community members. This could introduce biases or overlook important contextual factors that influence the implementation of comprehensive legal services in HIV care settings. Furthermore, while intervention mapping emphasizes iterative processes and stakeholder engagement, the extent to which these principles were effectively implemented in our study may vary, potentially impacting the fidelity and sustainability of the intervention. Lastly, the feasibility and preliminary effectiveness testing of the intervention package, OPAHL, in a hybrid, randomized cluster trial in Philadelphia, Pennsylvania, may not fully generalize to other settings or populations, limiting the external validity of our findings. These limitations underscore the need for further research and refinement of intervention mapping methodologies to address complex public health challenges comprehensively and effectively.
Conclusion
Adapting intervention mapping enabled the development of a multi-level MLP intervention package with the potential to strengthen HIV care continuum outcomes by addressing health-harming legal needs and underlying social determinants of health. Aligning legal services with emerging patient needs is essential to advancing national HIV treatment priorities. This study provides a replicable framework for researchers and practitioners designing structural interventions in contexts where care access and treatment engagement are shaped by complex social and systemic factors—particularly in chronic and communicable disease settings like HIV. Importantly, this work is especially relevant amid recent shifts in NIH priorities and reductions in federal HIV funding. Rather than moving away from structural approaches, sustained investment in scalable, community-informed solutions like OPAHL is urgently needed. Our findings highlight the importance of long-term funding mechanisms that support real-world implementation of equity-driven, multi-sector interventions.
Statements
Data availability statement
The datasets presented in this article are not readily available due to the nature and sensitivity of the qualitative data presented. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
Ethical approval was obtained from Temple University's Institutional Review Board. Participants provided informed consent prior to participation. As the study was deemed minimal risk, written consent was not required. All procedures were conducted in accordance with local regulations and institutional guidelines.
Author contributions
MM-L: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Formal analysis, Methodology, Visualization. AF: Writing – review & editing. RD: Writing – review & editing, Data curation. SM: Writing – review & editing, Data curation, Formal analysis. EA: Writing – review & editing. AR: Writing – review & editing. RJ: Writing – review & editing. MF: Writing – review & editing. OM: Data curation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study is funded by U.S. National Institute of Mental Health, NIMH (Grant # 1R21MH115820–01, 2018–2020). The research design, protocol, and implementation were not influenced by the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgments
We would like to thank study participants for their contribution to research and the broader membership of the community-engaged research partnership that the authors are part of, including community stakeholders living with and impacted by HIV. Communities are the key to ending the epidemic; affected and impacted communities should assume a major role in planning, developing and implementing HIV prevention and treatment initiatives.
Conflict of interest
SM was employed by Samantha Morton Consulting.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MLP, medical-legal partnership; HHLN, health-harming legal needs; PWH, persons with HIV; FQHC, federally qualified health center; OPAHL, organizational partnerships for healthy living; LSC, legal services corporation.
References
1.
Bartholomew Eldredge LK Parcel GS Kok G . Planning Health Promotion Programs: An Intervention Mapping Approach. 3rd ed.San Francisco, CA: John Wiley & Sons (2011).
2.
Bartholomew LK Parcel GS Kok G . Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav. (1998) 25(5):545–63. 10.1177/109019819802500502
3.
Draper CE Micklesfield LK Kahn K Tollman SM Pettifor JM Dunger DB et al Application of intervention mapping to develop a community-based health promotion pre-pregnancy intervention for adolescent girls in rural South Africa: Project Ntshembo (Hope). BMC Public Health. (2014) 14(Suppl 2):S5. 10.1186/1471-2458-14-S2-S5
4.
Fernández ME Allen JD Mistry R Kahn JA . Integrating clinical, community, and policy perspectives on human papillomavirus vaccination. Annu Rev Public Health. (2010) 31:235–52. 10.1146/annurev.publhealth.012809.103609
5.
Fernandez ME Ruiter RAC Markham CM Kok G . Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. (2019) 7:209. 10.3389/fpubh.2019.00209
6.
Hou S-I Fernandez ME Parcel GS . Development of a cervical cancer educational program for Chinese women using intervention mapping. Health Promot Pract. (2004) 5(1):80–7. 10.1177/1524839903257311
7.
Miranda J Côté J . The use of intervention mapping to develop a tailored web-based intervention, condom-HIM. JMIR Public Health and Surveill. (2017) 3(2):e20. 10.2196/publichealth.7052
8.
Wolfers MEG van den Hoek C Brug J de Zwart O . Using intervention mapping to develop a programme to prevent sexually transmittable infections, including HIV, among heterosexual migrant men. BMC Public Health. (2007) 7(1):141. 10.1186/1471-2458-7-141
9.
Anderson-Carpenter KD Collie-Akers V Colvin JD Cronin K . The role of advocacy in occasioning community and organizational change in a medical–legal partnership. J Prev Interv Community. (2013) 41(3):167–75. 10.1080/10852352.2013.788343
10.
Edward JS Northrip KD Welker A Costich JF . Medical-legal partnerships facilitate patient-provider cost of care conversations: a multisite qualitative study in the U.S. Clin Nurs Res. (2022) 31(8):1500–9. 10.1177/10547738221120339
11.
Hall EC Current JJ Sava JA Rosen JE . The case for integrating medical-legal partnerships into trauma care. J Surg Res. (2022) 274:153–9. 10.1016/j.jss.2021.12.043
12.
Mapp AM Moore C Booker E Santiago C Baker D Salvatore AL . Legal needs, health, and health care utilization among patients participating in the Delaware medical legal partnership. J Public Health Manag Pract. (2022) 28(6):E815–24. 10.1097/PHH.0000000000001597
13.
Martinez O Boles J Muñoz-Laboy M Levine EC Ayamele C Eisenberg R et al Bridging health disparity gaps through the use of medical legal partnerships in patient care: a systematic review. J Law Med Ethics. (2017) 45(2):260–73. 10.1177/1073110517720654
14.
Murphy JS Lawton EM Sandel M . Legal care as part of health care the benefits of medical-legal partnership. Pediatr Clin N Am. (2015) 62(5):1263. 10.1016/j.pcl.2015.06.001
15.
Regenstein M Trott J Williamson A Theiss J . Addressing social determinants of health through medical-legal partnerships. Health Aff. (2018) 37(3):378–85. 10.1377/hlthaff.2017.1264
16.
Malik FS Yi-Frazier JP Taplin CE Roth CL Whitlock KB Howard W et al Improving the care of youth with type 1 diabetes with a novel medical-legal community intervention: the diabetes community care ambassador program. Diabetes Educ. (2018) 44(2):168–77. 10.1177/0145721717750346
17.
Zuckerman B Sandel M Lawton E Morton S . Medical-legal partnerships: transforming health care. Lancet. (2008) 372(9650):1615–7. 10.1016/S0140-6736(08)61670-0
18.
Tobin-Tyler E Teitelbaum JB . Medical-legal partnership: a powerful tool for public health and health justice. Public Health Rep. (2019) 134(2):201–5. 10.1177/0033354918824328
19.
Liaw W Northrup TF Stotts AL Bakos-Block C Suchting R Chen A et al Medical-legal partnership effects on mental health, health care use, and quality of life in primary care: a randomized clinical trial. J Am Board Fam Med. (2023) 36(3):414–24. 10.3122/jabfm.2022.220349R1
20.
Regenstein M Trott J Williamson A . The State of the Medical-Legal Partnership Field: Findings from the 2016 National Center for Medical-Legal Partnership Surveys. Washington, DC: National Center for Medical-Legal Partnership (2017). Available at: https://medical-legalpartnership.org/wp-content/uploads/2017/07/2016-MLP-Survey-Report.pdf (Accessed November 1, 2023).
21.
Williams DR Costa MV Odunlami AO Mohammed SA . Moving upstream. J Public Health Manag Pract. (2008) 14(6):S8–S17. 10.1097/01.PHH.0000338382.36695.42
22.
Sege R Preer G Morton SJ Cabral H Morakinyo O Lee V et al Medical-legal strategies to improve infant health care: a randomized trial. Pediatrics. (2015) 136(1):97–106. 10.1542/peds.2014-2955
23.
O’Sullivan MM Brandfield J Hoskote SS Segal SN Chug L Modrykamien A et al Environmental improvements brought by the legal interventions in the homes of poorly controlled inner-city adult asthmatic patients: a proof-of-concept study. J Asthma. (2012) 49(9):911–7. 10.3109/02770903.2012.724131
24.
Ryan AM Kutob RM Suther E Hansen M Sandel M . Pilot study of impact of medical-legal partnership services on Patients’ perceived stress and wellbeing. J Health Care Poor Underserved. (2012) 23(4):1536–46. 10.1353/hpu.2012.0179
25.
Klein MD Beck AF Henize AW Parrish DS Fink EE Kahn RS . Doctors and lawyers collaborating to HeLP children—: outcomes from a successful partnership between professions. J Health Care Poor Underserved. (2013) 24(3):1063–73. 10.1353/hpu.2013.0147
26.
Beck AF Klein MD Schaffzin JK Tallent V Gillam M Kahn RS . Identifying and treating a substandard housing cluster using a medical-legal partnership. Pediatrics. (2012) 130(5):831–8. 10.1542/peds.2012-0769
27.
Taylor DR Bernstein BA Carroll E Oquendo E Peyton L Pachter LM . Keeping the heat on for Children’s health: a successful medical–legal partnership initiative to prevent utility shutoffs in vulnerable children. J Health Care Poor Underserved. (2015) 26(3):676–85. 10.1353/hpu.2015.0074
28.
Teufel JA Werner D Goffinet D Thorne W Brown SL Gettinger L . Rural medical-legal partnership and advocacy: a three-year follow-up study. J Health Care Poor Underserved. (2012) 23(2):705–14. 10.1353/hpu.2012.0038
29.
Rodabaugh KJ Hammond M Myszka D Sandel M . A medical–legal partnership as a component of a palliative care model. J Palliat Med. (2010) 13(1):15–8. 10.1089/jpm.2009.0203
30.
Fuller SM Steward WT Martinez O Arnold EA . Medical-legal partnerships to support continuity of care for immigrants impacted by HIV: lessons learned from California. J Immigr Minor Health. (2020) 22(1):212–5. 10.1007/s10903-019-00919-0
31.
Killelea A . Collaborative lawyering meets collaborative doctoring: how a multidisciplinary partnership for HIV/AIDS services can improve outcomes for the marginalized sick. Geo J Poverty Law Poly. (2009) 16(2/3):413–59. Available at:https://search.ebscohost.com/login.aspx?direct=true&AuthType=cookie,shib&db=aph&AN=47838402&authtype=shib&site=ehost-live&scope=site&custid=current&groupid=main&authtype=shib
32.
Muñoz-Laboy M Martinez O Davison R Fernandez I . Examining the impact of medical legal partnerships in improving outcomes on the HIV care continuum: rationale, design and methods. BMC Health Serv Res. (2019) 19(1):N.PAG-N.PAG. 10.1186/s12913-019-4632-x
33.
Yamanis TJ Zea MC Ramé Montiel AK Barker SL Díaz-Ramirez MJ Page KR et al Immigration legal services as a structural HIV intervention for latinx sexual and gender minorities. J Immigr Minor Health. (2019) 21(6):1365–72. 10.1007/s10903-018-0838-y
34.
Atkins Ddhgc Heller S DeBartolo E Sandel M . Medical-legal partnership and healthy start: integrating civil legal aid services into public health advocacy. J Leg Med. (2014) 35(1):195–209. 10.1080/01947648.2014.885333
35.
Hagins S Loubier E . Medical-legal partnership 101: an introduction to the benefits of integrated care. National Center for Medical Legal Partnership (2019). Available at: https://nchph.org/wp-content/uploads/2015/10/Medical-Legal-Partnership-101.pdf(Accessed December 1, 2024).
36.
Fernandez ME Ten Hoor GA van Lieshout S Rodriguez SA Beidas RS Parcel G et al Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. (2019) 7:158. 10.3389/fpubh.2019.00158
37.
McNett M Tucker S Melnyk BM . Implementation science: a critical strategy necessary to advance and sustain evidence-based practice. Worldviews Evid Based Nurs. (2019) 16(3):174–5. 10.1111/wvn.12368
38.
Waltz TJ Powell BJ Fernández ME Abadie B Damschroder LJ . Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci. (2019) 14(1):42. 10.1186/s13012-019-0892-4
39.
Braun V Clarke V . One size fits all? What counts as quality practice in (reflexive) thematic analysis?Qual Res Psychol. (2021) 18(3):328–52. 10.1080/14780887.2020.1769238
40.
Bartholomew LK Parcel GS Kok G Gottlieb NH Schaalma H Markham C et al Planning Health Promotion Programs: An Intervention Mapping Approach. 2nd ed.San Francisco, CA: Jossey-Bass (2006).
41.
Intervention Mapping. Intervention Mapping (2020).
42.
Pinto RM Park SE Miles R Ong PN . Community engagement in dissemination and implementation models: a narrative review. Implement Res Pract. (2021) 2:2633489520985305. 10.1177/2633489520985305
43.
Aarons GA Hurlburt M Horwitz SM . Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health. (2011) 38(1):4–23. 10.1007/s10488-010-0327-7
44.
Jaen JF French AA Davison R Munoz-Laboy M Martinez O . Medical-legal partnerships: a promising approach for addressing health-harming legal needs among people with HIV. Front Sociol. (2024) 9:1422783. 10.3389/fsoc.2024.1422783
45.
Backer TE Rogers EM . Diffusion of innovations theory and work-site AIDS programs. J Health Commun. (1998) 3(1):17–28. 10.1080/108107398127481
46.
Damanpour F . Innovation effectiveness, adoption and organizational performance. In: WestMAFarrJL, editors. Innovation and Creativity at Work: Psychological and Organizational Strategies. Oxford: John Wiley & Sons (1990). p. 125–41.
47.
Damanpour F . Organizational complexity and innovation: developing and testing multiple contingency models. Manage Sci. (1996) 42(5):693. 10.1287/mnsc.42.5.693
48.
Ramseyer Winter V . Diffusion of innovations theory: a unifying framework for HIV peer education. Am J Sex Educ. (2013) 8(4):228–45. 10.1080/15546128.2013.838512
49.
Fernández ME Gonzales A Tortolero-Luna G Partida S Bartholomew LK . Using intervention mapping to develop a breast and cervical cancer screening program for Hispanic farmworkers: Cultivando La Salud. Health Promot Pract. (2005) 6(4):394–404. 10.1177/1524839905278810
50.
Campo JV Geist R Kolko DJ . Integration of pediatric behavioral health services in primary care: improving access and outcomes with collaborative care. Can J Psychiatry. (2018) 63(7):432–8. 10.1177/0706743717751668
51.
Colvin JDjce Nelson B Cronin K . Integrating social workers into medical-legal partnerships: comprehensive problem solving for patients. Soc Work. (2012) 57(4):333–41. 10.1093/sw/sws012
52.
Bonciani M Schäfer W Barsanti S Heinemann S Groenewegen PP . The benefits of co-location in primary care practices: the perspectives of general practitioners and patients in 34 countries. BMC Health Serv Res. (2018) 18:1–22. 10.1186/s12913-018-2913-4
53.
Jain KMkje Maulsby C Kinsky S Charles V Holtgrave DR . 2015–2020 National HIV/AIDS strategy goals for HIV linkage and retention in care: recommendations from program implementers. Am J Public Health. (2016) 106(3):399–401. 10.2105/AJPH.2015.302995
54.
Schackman BR Fleishman JA Su AE Berkowitz BK Moore RD Walensky RP et al The lifetime medical cost savings from preventing HIV in the United States. Med Care. (2015) 53(4):293–301. 10.1097/MLR.0000000000000308
55.
Tool: Screening for MLP legal needs in health care settings (2015).
56.
Glasgow RE Klesges LM Dzewaltowski DA Estabrooks PA Vogt TM . Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. (2006) 21(5):688–94. 10.1093/her/cyl081
57.
Sege R Kaplan-Sanoff M Morton SJ Velasco-Hodgson MC Preer G Morakinyo G et al Project DULCE: strengthening families through enhanced primary care. Zero Three. (2014) 35(1):10–8. Available at:http://libproxy.temple.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=eue&AN=98485014&site=ehost-live&scope=site
58.
Mantel J Fowler L . Thinking outside the silos: information sharing in medical-legal partnerships. J Leg Med. (2020) 40(3–4):369–89. 10.1080/01947648.2020.1854135
59.
Weintraub D Rodgers MA Botcheva L Loeb A Knight R Ortega K et al Pilot study of medical-legal partnership to address social and legal needs of patients. J Health Care Poor Underserved. (2010) 21(2 Suppl):157–68. 10.1353/hpu.0.0311
Summary
Keywords
medical-legal partnership, legal services, health-harming legal needs, HIV, people with HIV, implementation science, intervention mapping, health services research
Citation
Muñoz-Laboy M, French A, Davison R, Morton SJ, Arnold EA, Rudolph AE, Jones RM, Fernandez MI and Martinez O (2025) Adapting and applying intervention mapping to integrate medical-legal partnership into organizations providing HIV care: an implementation methodology study. Front. Health Serv. 5:1435663. doi: 10.3389/frhs.2025.1435663
Received
20 May 2024
Accepted
02 April 2025
Published
01 May 2025
Volume
5 - 2025
Edited by
Bo Kim, VA HSR&D Center for Healthcare Organization and Implementation Research, United States
Reviewed by
Meagen Rosenthal, University of Mississippi, United States
Ida Griesemer, White River Junction VA Medical Center, United States Department of Veterans Affairs, United States
Updates
Copyright
© 2025 Muñoz-Laboy, French, Davison, Morton, Arnold, Rudolph, Jones, Fernandez and Martinez.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Omar Martinez omar.martinez@ucf.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.