Abstract
Introduction:
Emergency responders encounter frequent trauma and myriad occupational hazards, contributing to concerning rates of posttraumatic stress disorder (PTSD) and related mental health symptoms. These symptoms are each strongly linked with neuroticism/negative emotionality (NNE). Thus, an emotion-focused, transdiagnostic, skills-based treatment approach seems to be a strong match for this population. We sought to address barriers to mental health treatment for emergency responders, including stigma, logistical barriers, and lack of provider knowledge regarding emergency response culture by delivering treatment via telehealth by providers trained in emergency response culture.
Methods:
In an uncontrolled pilot trial, we delivered the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders to 30 emergency medical service, police, and fire service personnel.
Results:
The large majority (80.0%) completed treatment. Working Alliance Inventory scores were high. Large improvements occurred at post-treatment and one-month follow-up in PTSD symptom severity (Hedges' g = 1.1 at post-treatment; g = 1.3 at follow-up), depression (g = 1.3; 1.3), anxiety (g = 1.1; 1.0), functional impairment (g = 1.2; 1.1), and quality of life (g = .89; .81). Small-to-medium sized improvements occurred in sleep quality (g = .42; .69) and engagement in values-consistent behavior (g = .34; .77). There were large, theory-consistent improvements during treatment in NNE (g = 1.1), difficulties in emotion regulation (g = .94), and experiential avoidance (g = 1.1), and large associations between changes in these mechanistic variables and improved treatment outcomes.
Discussion:
We summarize our cultural adaptation process aimed at maximizing fit of the UP with emergency responders and recommend additional, controlled research examining the UP in trauma exposed populations.
Clinical Trial Registration:
NCT05357586.
1 Introduction
Emergency response professionals risk their health and well-being to protect the public. Broadly speaking, emergency responders appear to experience elevated risk for developing mental health disorders compared to the general population (1). These elevated risks in emergency responders are linked with myriad occupational stressors (2) including frequent exposure to psychological trauma (3–5) and shift work that interferes with their sleep (6). Level of trauma exposure is associated with suicidal ideation and attempts in emergency responders (7). Moreover, emergency responders were disproportionately impacted by the COVID-19 pandemic and, in turn, experienced an increase in mental health challenges during the pandemic (8–10). While rates vary substantially across studies and disorder categories, estimates of up to one-third of emergency responders develop posttraumatic stress disorder [PTSD; (1, 5, 11–13)]. For the sake of comparison, the estimated lifetime prevalence of posttraumatic stress disorder among people who have been exposed to one or more traumatic event in the general population is 14.5% (14). Other studies report that approximately one-third of emergency responders meet criteria for other common mental health disorders such as depression, anxiety, and sleep disorders (1, 5, 15–18). Published estimates indicate that between one-third and two-thirds of emergency responders report engaging in hazardous alcohol use, which is associated with each of these other mental health challenges and with sleep problems in this population (19–21). Stressors underlying these problems are also linked with elevated rates of occupational burnout, physical health problems such as cardiovascular disease, suicide risk, and greater all-cause mortality, underscoring the need to address the mental health challenges faced by these crucial public safety workers in a holistic manner (2, 7, 22–24). Given that many of the symptoms of these mental health challenges co-occur and overlap across diagnostic categories, treatment for this population should be transdiagnostic in nature (25, 26).
The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders [UP (25, 27, 28);] is a highly structured, empirically supported treatment approach that appears to be a strong match for addressing mental health challenges in emergency responders (26). On a mechanistic level, targeting the negative emotional experiences that underlie and cut across these problems would seem an effective, empirically informed strategy (25, 29). In contrast to disorder-specific treatments that address a single emotional disorder (e.g., depression), the UP engages several evidence-based treatment processes—including mindfulness, cognitive flexibility, and behavioral exposures (30)—and applies them in an integrative manner to address symptoms across diagnostic categories. A growing evidence base supports the utility of the UP for improving emotional and emotion-adjacent symptoms, including anxiety, depression, anger, substance misuse, self-injury, somatization, obsessive-compulsive symptoms, and trauma-related symptoms (26, 31–37). In a meta-analysis of 19 randomized trials (32), there was a medium effect of the UP on pooled anxiety and depression symptoms from pre- to post-treatment (between-groups Hedges' g = .45). Moreover, in this study, findings were substantially stronger at follow-up in the 12 RCTs for which follow-up data were available (between-groups g = 1.13). To date, four pilot studies have examined the UP as a treatment for PTSD, with all four demonstrating that the UP was associated with reductions in PTSD and other mental health symptoms (26, 34, 35, 37). No published RCTs have tested the UP for PTSD to date. One area where there has been virtually no research is on the effect of the UP on sleep problems even though sleep problems are part of the diagnostic criteria for several categories of emotional disorders (38). One case study and one single case experimental design study both reported improvements in sleep onset latency and sleep quality (39, 40), which the latter study also reported concomitant improvements in emotion regulation and negative emotionality/neuroticism (NNE).
On a mechanistic level, the UP was designed to reduce mental health symptoms by targeting negative emotions, including by teaching skills for more effectively responding to and regulating negative emotions (41, 42). Neuroticism, alternately referred to as negative emotionality (NNE), is the core treatment target in the UP. It is one of the Big 5 personality factors that characterizes the frequency and intensity with which people experience emotions that are typically characterized as negative or unwanted [e.g., fear, anger, sadness, guilt (43);]. NNE is linked with multiple forms of maladaptive coping, including inaction, avoidance, and impulsivity (42, 44–46). In a prospective, observational cohort study of fire fighter recruits who did not meet criteria for any mental health disorder upon study entry, higher pre-employment levels of emotionality prospectively predicted (i.e., main effect) and interacted with (i.e., moderated) greater levels of trauma exposure to predict the development of higher levels of PTSD symptom severity over the first three years in fire service (47). Negative alterations in cognition and mood are core features of PTSD, depression, and anxiety (38, 48). NNE is prospectively linked with such a broad range of negative physical and mental health outcomes, including harmful alcohol use, sleep problems, suicide risk, and others that it has been characterized as among the most important risk factors in public health (49–52). Thus, while it is unknown whether emergency response work
Another key factor targeted by the UP is emotion regulation. Extensive research links difficulties in emotion regulation with greater occurrence of negative emotions (53) and symptoms of PTSD, depression, anxiety, and substance use disorders (54–56). We found that fire fighters frequently engage in maladaptive forms of emotion regulation including self-blame and social isolation, which were linked with greater mental health symptoms, particularly when several maladaptive emotion regulation strategies were used in combination (5). In subsequent studies with fire fighters, difficulties in emotion regulation accounted for the link between depression and insomnia and were linked with PTSD symptom severity, sleep difficulties, and alcohol use (16, 17, 57–59). Difficulties in emotion regulation mediated the influence of PTSD symptom severity on relationship satisfaction in fire fighters (60). Conversely, adaptive emotion regulation skills were linked with lower anxiety and depression symptoms in fire fighters (61). Prior research indicates that the UP bolsters adaptive emotion regulation skills and reduces reliance on maladaptive strategies for managing negative emotions (36). The UP also focuses on reducing experiential avoidance, which refers to attempts to avoid, control, or escape from unwanted internal experiences (i.e., cognitions, emotions, physiological sensations), even when doing so interferes with engaging in behaviors that are consistent with one's values and goals (62, 63). The strong associations between experiential avoidance and NNE, along with the negative impact of experiential avoidance on mental health symptoms have been extensively documented (63–68). Several studies have documented decreases in experiential avoidance in diverse client populations receiving the UP (69, 70).
Beyond selecting a treatment approach that addresses the symptoms most commonly experienced by emergency responders, delivering mental health care to this population requires addressing several challenges related to treatment acceptability and feasibility. Emergency responders report stigma and privacy concerns regarding seeking care for mental health symptoms related, at least in part, to occupational stress (16, 71–74). In one study of fire fighters, lack of provider awareness of emergency response culture (53%), fear of breach in confidentiality (51%), and stigma (43%) were rated as the top three barriers to behavioral health care (72). Next, it would be difficult for any clinician to be sufficiently trained in empirically supported treatments for all of the mental health problems commonly found in fire fighters and even less likely that fire fighters would agree to complete each of those protocols sequentially. The UP has the advantage of being transdiagnostic and thus more easily disseminated to and implemented by clinicians who treat fire service personnel. Emergency responders' work schedules often present a challenge related to accessing mental health care (16). Based on our experience working with emergency responders, offering treatment via video conferencing enhances the sense of privacy for many and enhances scheduling convenience, which is important for shift workers. Next, given high levels of trauma exposure in this population, treatment should be trauma informed. Providing treatment that is highly structured and predictable is a core element of trauma informed care. Emergency responders make regular use of manuals and protocols as part of their work; thus, protocol driven treatment may be one way of enhancing predictability and comfort when delivering trauma focused care to this population. Finally, based on our familiarity with emergency response culture, we reasoned that treatment that is active, collaborative, and that emphasizes skill building is a strong fit with emergency response culture.
With these principles in mind, we conducted the first study of the UP in emergency responders, a pilot trial of fire fighters with different combinations of emotional symptoms (26). We began by enlisting the expertise of fire service collaborators in a cultural adaptation process to ensure strong fit between certain elements included in the UP and emergency response culture. Treatment was then delivered via video conferencing by clinicians who were educated in fire service culture. A high proportion (80.3%) of participants completed treatment, underscoring feasibility and acceptability of this highly structured, skills based intervention in this population. We reported medium and large effect size improvements in symptoms of PTSD, depression, anxiety, AUD, and quality of life. Each of these findings was sustained at 1-month follow-up. Thus, receiving the UP was associated with improvements in the types of mental health symptoms most commonly experienced by emergency responders. Moreover, the UP's manualized, skills-based approach seemed to promote treatment acceptability and to be a strong match with emergency response culture.
In the present study, we conducted an uncontrolled pilot trial examining the UP, culturally adapted for use with emergency responders, in a mixed sample of emergency responders. The sample was comprised of emergency medical service professionals (emergency medical technicians and paramedics), fire fighters, law enforcement officers, and emergency room medical personnel. Treatment was delivered individually, either in person or via video conferencing, based on participants' choice in order to maximize access and acceptability. We examined whether emergency responders who received the UP would report improvement in PTSD, depression, anxiety, AUD symptom severity, sleep quality, functional impairment, quality of life, and the extent to which they reported that they were able to consistently engage in behaviors that were consistent with their personal values. We examined treatment outcomes at post-treatment and at 1-month follow-up. Given high rates of trauma exposure in this population and limited data on the utility of the UP for treating posttraumatic stress, we also examined treatment outcomes in the sub-sample of participants who screened positive for PTSD at pre-treatment. We examined the associations between changes in the treatment outcomes and changes in putative treatment mechanisms (NNE, difficulties in emotion regulation, psychological inflexibility). For comparison, we also examined the association between therapeutic working alliance and changes in treatment outcomes. This study expands on our prior study of the UP in fire fighters (26) by examining a mixed sample of emergency responders, examining additional treatment outcomes (functional impairment, sleep quality, values-consistent actions), and exploring the influence of treatment mechanisms. It is the first study to compare the influence of several mechanisms theorized to be targeted in the UP within a trauma exposed sample.
2 Material and methods
2.1 Institutional review board
The University of Pittsburgh IRB approved all procedures (Study 21120152).
2.2 Design
In this uncontrolled pilot trial, all eligible participants received treatment using the UP.
2.3 Participants
Male and female, English-speaking emergency response professionals 18 years of age or older residing in Pennsylvania were eligible to participate. Emergency responders were defined as fire fighters, law enforcement officers, emergency medical service personnel, emergency room medical providers, and emergency dispatchers. Potential participants were excluded if they: (1) were unable or unwilling to complete the study procedures; (2) screened positive for a psychotic or bipolar disorder; (3) were experiencing a current suicidal or homicidal crisis warranting immediate intervention at the time of eligibility screening. Potential participants could participate later once stabilized; (4) evidenced severe organic brain impairment as evidenced by a major apparent disruption of consciousness, cognition, speech, or behavior that would likely interfere with treatment; (5) were awaiting the outcome of litigation involving their employment as an emergency responder or any other reason deemed by the study team to be potentially related to their mental health; (6) were receiving another form of counseling for anxiety, depression, posttraumatic stress, or alcohol use problems. Attendance at self-help programs (e.g., Alcoholics Anonymous) and couples therapy was permitted, though no one in the sample reported attending a self-help program; or (7) endorsed drug use and symptoms consistent with a non-alcohol substance use disorder except nicotine, caffeine, or cannabis.
2.4 Procedure
The study took place between March 2022 and October 2023. Recruitment occurred via social media advertising and community presentations by the first author and staff affiliated with the Pitt Center for Emergency Responder Wellness. Potential participants emailed or called regarding their interest. A post-baccalaureate project coordinator provided study information and determined initial eligibility by phone using a structured screening questionnaire. This telephone screening included screening for the presence of a potential suicidal crisis. Any endorsement of thoughts of suicide in the past month was followed up with an immediate screening by a project clinician. No participants were excluded from the study based on presence of a suicidal crisis. Initially eligible participants were then sent the informed consent form electronically through REDCap. Informed consent and electronic data collection were completed using REDCap. Participants were given sufficient time to review it and were encouraged to reach out with any questions before providing their signature. Study staff then reached out to the participant to verbally confirm that the participant understood the procedures and to offer an additional opportunity to ask questions before the consent form was signed electronically and witnessed by study staff. Participants were sent a link to complete the baseline assessments online. Baseline questionnaires were reviewed to determine final eligibility. Individuals who were deemed ineligible to receive treatment through this project were referred to alternate, appropriate care. Eligible participants were then scheduled for the first treatment session. Participants met with therapists, who were assigned on a rotating basis, either in person at the university or via a secure, HIPAA-compliant online video conferencing platform, depending on the participant's preference. Treatment was delivered as individual (one-on-one) therapy. All treatment sessions were video recorded for training and quality control purposes. One month following the final treatment session, participants were emailed a link to complete the post-treatment assessments and, one month later, the follow-up assessments. Participants were sent reminders to complete these assessments via email as needed. Participants were compensated with a total of $120 for completing all assessments ($30 at baseline, $50 at post-treatment, and $40 at follow-up).
2.4.1 Treatment
The UP (27, 28) is a transdiagnostic form of cognitive behavioral therapy that is empirically supported for treating a range of emotional disorders. In the UP, treatment mechanisms that underlie emotional disorders—NNE, difficulties in emotion regulation, and experiential avoidance—are targeted. These mechanisms are targeted via a series of treatment modules: (1) Assessment/Goal setting/Enhancing motivation, (2) Understanding emotions, (3) Mindful emotion awareness (1–2 sessions), (4) Cognitive flexibility (1–3 sessions), (5) Emotional behaviors (1–3 sessions), (6) Physical sensations (1–2 sessions), (7) Exposures (1–3 sessions), and (8). Recognizing accomplishments/Looking to the future. Standard delivery of the UP occurs across approximately 16 sessions. Treatment duration was tailored based on the individual needs of each participant. Eight sessions was considered the minimum threshold for treatment completion in this study. We arrived at this definition because it was as this was the minimum number of sessions needed to complete all 8 modules and is consistent with the definition of treatment completion used in our prior study of the UP in fire fighters (26). That said, there were instances in which a participant could be deemed a treatment completer by virtue of completing 8 or more sessions even if they did not complete all 8 modules, though this was rare.
2.4.2 Cultural adaptation
Our prior study described in detail the cultural adaptations made to ensure the appropriateness of the UP content for use with fire fighter (26). During that prior study, our collaborators from fire service reviewed the UP materials for possible adaptations in the areas of language (Is terminology used in the UP appropriate and understandable for emergency responders?), concepts (Are concepts/modules likely to be relevant and helpful for emergency responders?), and specific examples (Are examples included in the UP materials likely to resonate? Are different examples needed?). Overall, our adaptation process highlighted the applicability of the standard UP with this population, along with the importance of attending to cultural considerations in certain instances. Specifically, we determined that no adaptations were needed pertaining to language or concepts. We made two adaptations regarding specific examples, both of which were flagged as potential “sticking points” that could interfere with treatment credibility when using the UP with emergency responders. First, we removed “avoiding caffeine” from the “Examples of Emotional Behaviors” worksheet in Module 5: Countering Emotional Behaviors. This example was deemed incongruent with norms among emergency responders, as caffeine intake is prevalent, particularly during overnight shifts. Second, we added an additional “thinking trap” to Module 4: Cognitive Flexibility. We added black-and-white/all-or-nothing thinking to characterize a range of potentially problematic thoughts commonly observed in emergency responders related to “worst case scenario” events to which first responders are likely to be exposed.
In the current study, we completed this same cultural adaptation process, this time with our study therapists from emergency medical service and law enforcement. Thus, across the two studies, the UP was reviewed for potential cultural adaptations by professionals from across fire, police, and emergency medical service who are also mental health professionals. The review during the current study led to one additional adaptation. Namely, given the prevalence of sleep problems in emergency responders, we decided that we would address maladaptive cognitions related to sleep problems (e.g., catastrophizing regarding sleep difficulties), as appropriate, as part of Module 4: Cognitive Flexibility.
2.4.3 Clinicians, training, and supervision
Therapists included five masters-level students in clinical mental health counseling, one clinical social work masters student, one licensed clinical social worker (study author SR), and a licensed clinical psychologist (author EM). Therapist training included both UP-specific training activities as well as a multi-step process to ensure sufficient familiarity with emergency response culture. Study therapists read the UP Therapist Guide and Client Workbook (27, 28), attended a four hour training in using the UP with emergency responders led by a study author (EC), attended a two hour emergency responder cultural awareness training led by a study author (SR), and viewed previously completed videos of treatment sessions from this project. The two hour emergency responder cultural awareness training addressed topics including: training that emergency responders receive and how this could impact their responses to stress and trauma, the most challenging types of critical incidents to deal with emotionally, common reactions to trauma in emergency responders, compassion fatigue, impacts of emergency responder stress on family life, and the importance of relationship and social support for managing stress. Therapists completed a “ride-along” experiential training activity with a local emergency medical service. Throughout the study, the first author provided weekly supervision in groups of 2–3 clinicians during which review of segments of recordings of treatment sessions were reviewed and discussed on a rotating basis. The first author provided written feedback to clinicians on approximately 20% of treatment sessions. The study team benefited from including three therapists who are also emergency responders—two emergency medical technicians and one police officer. This, combined with the first author's experience with these occupational groups, enhanced our ability to focus on how emergency response cultural factors could be influencing the case conceptualization and treatment process during each of our supervision sessions.
2.5 Measures
2.5.1 Eligibility screening measures
We screened for psychosis using the 6-item psychosis scale from the Psychiatric Diagnostic Screening Questionnaire [PDSQ; (75)]. We screened for violence risk using 4 items adapted from the Violence Risk Appraisal Guide (76). We screened for suicide risk using the suicide item from the Patient Health Questionnaire 9 Item- Depression [PHQ-9; (77)]. We used the 11-item Drug Use Disorders Identification Test [DUDIT; (78)] to screen for non-alcohol substance use disorder symptoms. We screened for potential presence of a suicidal crisis based on any endorsement of
2.5.2 Sample characteristics
A self-report questionnaire was administered at baseline to assess demographic characteristics sex, race, age, marital status, education level, and emergency response service characteristics.
2.5.3 Treatment outcome measures
2.5.3.1 PTSD symptoms
The Posttraumatic Stress Disorder Checklist for DSM-5 [PCL-5; (79)] is a 20-item self-report measure of PTSD symptoms over the past month. It assesses the 20 DSM-5 symptom criteria for PTSD with responses rated on a 5-point Likert scale ranging from 0 to 4 (0 = not at all, 4 = extremely). The item scores are summed to creates a total symptom severity score ranging from 0 to 80. The PCL-5 has demonstrated good reliability and validity in emergency responders (26). We identified those who scored above a cutoff score of 41 on the PCL-5 as screening positive for PTSD at baseline (80). Clinically reliable change on this measure is 15–18, and an end-state score of ≤28 indicates clinically significant change (81). In the current study, Cronbach's alpha for the PCL-5 ranged from 0.94 to 0.96 across timepoints (pre-treatment, post-treatment, and one-month follow-up).
2.5.3.2 Depression symptoms
The Patient Health Questionnaire 9 Item- Depression [PHQ-9; (77)] is a 9-item self-report measure that was used to screen for depression symptoms. The PHQ-9 asks patients to report how often- from 0- not at all to 3- nearly every day that they have been bothered by symptoms such as “little interest or pleasure in doing things,” and “feeling down, depressed or hopeless.” Items scores are summed to create a total score ranging from 0 to 27. Scores ranging from 0 to 4 indicate no depressive symptoms; 5–9 indicate mild depressive symptoms; 10–14 moderate; 15–19 moderately severe; 20–27 severe. In the current study, Cronbach's alpha for the PHQ-9 ranged from 0.87 to 0.89 across timepoints (pre-treatment, post-treatment, and 1-month follow-up).
2.5.3.3 Anxiety symptoms
The GAD-7 (82) is a 7-item self-report measure that was used to screen for anxiety symptoms. The GAD-7 asks patients to report how often- from 0- not at all to 3- nearly every day- that they have been bothered by a series of problems such as “feeling nervous, anxious, or on edge,” and “worrying too much about different things.” Item scores are summed to yield a total score ranging from 0 to 21. Scores ranging from 0 to 4 indicate no anxiety symptoms; 5–9 indicate mild anxiety symptoms; 10–14 moderate; 15–21 severe. In the current study, Cronbach's alpha for the GAD-7 ranged from 0.93 to 0.94 across timepoints (pre-treatment, post-treatment, and one-month follow-up).
2.5.3.4 Alcohol use disorder symptoms
The Alcohol Use Disorders Identification Test [AUDIT; (83)] is a widely used, 10-item measure of self-reported AUD symptoms and drinking quantity and frequency. Item response formats vary. Total scores of 10 or greater suggest probable AUD.
2.5.3.5 Drug use disorder symptoms
The Drug Use Disorders Identification Test [DUDIT; (78, 84)] is an 11-item measure of self-reported non-alcohol substance use disorder symptoms that mirrors the AUDIT. Item response formats vary; total scores of 10 or greater suggest probable SUD.
2.5.3.6 Sleep quality
The Pittsburgh Sleep Quality Index [PSQI; (85)] is a widely used, 18-item self-report measure that comprises seven component scores: (1) subjective sleep quality, (2) sleep latency, (3) sleep duration, (4) sleep efficiency, (5) sleep disturbances, (6) sleep medication usage, and (7) daytime dysfunction (85). Item formats vary. We examined the PSQI total score, with higher scores indicating worse overall sleep quality. For exploratory purposes, we also computed a score by summing a subset of PSQI items assessing aspects of sleep quality that may be more likely to change as a result of emotion-focused psychotherapy—these included subjective sleep quality, sleep latency, sleep efficiency, wakefulness after sleep onset, and use of sleep medications—as opposed to items more likely to be linked to sleep problems such as sleep apnea and therefore unlikely to improve via psychotherapy.
2.5.3.7 Functional impairment
The Work and Social Adjustment Scale [WSAS; (86)] is a 5-item measure that was used to assess impairment in work, household tasks, social leisure activities, private recreation, and social relationships. Items are scored on a 0 (no impairment) to 8 (severe impairment) scale, with total scores ranging from 0 to 40. In the current study, Cronbach's alpha ranged from 0.86 to 0.89 across timepoints.
2.5.3.8 Quality of life
The World Health Organization Quality of Life (87) is a 26-item self-report measure designed to assess participant satisfaction in four life domains: physical, psychological, social, and environmental. Items were scored on a 5-point Likert scale (1 = not at all, 5 = extremely). In this study, we used the total score. This measure has shown good reliability and validity in prior research with emergency responders (26). In the current study, Cronbach's alpha ranged from 0.92 to 0.93.
2.5.3.9 Values-consistent actions
The Values Tracker [VT; (88)] is a two-item measure of the extent to which people report behaving in ways that are consistent with their personal values. Each item is rated on a 1–10 scale, with higher scored indicating greater values engagement.
2.5.4 Treatment mechanisms
2.5.4.1 NNE
The negative emotionality scale from the Big Five Inventory-2 (89) is a 12-item scale drawn from this larger personality inventory to assess NNE. In this study, reliability (Cronbach's alpha) ranged from 0.87 to 0.89 across time-points.
2.5.4.2 Emotion regulation
The Difficulties in Emotion Regulation Scale-16 [DERS-16; (90);] is a 16-item self-report measure of frequency of difficulties in emotion regulation that is an abbreviated version of the lengthier DERS. It assesses four types of difficulties: non-acceptance of emotional responses, difficulty engaging in goal-directed behavior amidst emotional distress, difficulty with impulse control, and limited ability to engage in more helpful emotion regulation strategies. Items are scored on a scale of 1–5 with higher scores indicating greater more frequent difficulties in emotion regulation. Scores range from 16 to 80. In the current study, Cronbach's alpha ranged from 0.95 to 0.98.
2.5.4.3 Experiential avoidance
The Acceptance and Action Questionnaire–II [AAQ-II; (63)] is a 7-item self-report measure of unwillingness or perceived inability to remain in contact with difficult internal experiences and efforts to escape, avoid, or modify these experiences. Items are scored on a scale of 1–7 with higher scores indicate greater experiential avoidance. In the current study, Cronbach's alpha ranged from 0.89 to 0.96.
2.5.4.4 Therapeutic alliance
The Working Alliance Inventory—Short Form [WAI-SF; (91)] is a reliable and valid 12-item self-report measure of therapeutic alliance in three domains: agreement on therapy tasks, agreement on goals, and development of a therapist-client bond. Items are rated on a 5-point Likert scale ranging from 1 to 5 (1 = seldom, 5 = always). Item scores are summed to yield a total score ranging from 12 to 60, with higher scores reflecting better therapeutic alliance. The WAI-SF was administered at session 4. Internal consistency was 0.87.
2.6 Data analysis
We compared baseline demographic and clinical characteristics as a function of whether participants completed or dropped out of treatment using t-tests or Chi-square analyses, as appropriate. A series of paired-samples t-tests were conducted on all clinical variables comparing pre-treatment scores with scores on the outcomes at post-treatment and at one-month follow-up, along with repeated measures effect sizes (Hedges' g) where, by convention, values of .3, .5, and .8 are considered small, medium, and large, respectively. Next, because few studies have examined the UP in people with PTSD or AUD, we examined changes across outcomes in participants who screened positive for PTSD and AUD at baseline, respectively. Finally, we explored whether changes in the putative treatment mechanisms (WAI-SR, AAQ-II, DERS-16, BFI-2-N, PSQI) during treatment (i.e., pre- to post-treatment change scores) were associated with changes in the treatment outcomes during treatment and from pre-treatment to follow-up by computing Pearson product-moment correlations. Analyses were conducted using SPSS (v. 28).
3 Results
3.1 Enrollment and participant characteristics
A total of 39 people were screened for eligibility, of whom 36 were deemed eligible. Reasons for ineligibility included having a history of bipolar disorder (2) and not meeting our definition for being an emergency responder (1). Of these 36, 31 provided informed consent and completed the baseline assessment, whereas 5 decided not to participate prior to providing informed consent. One participant who provided informed consent did not complete the baseline assessment and was therefore ineligible. All 30 participants who completed the baseline assessment were deemed eligible and began treatment.
Sample characteristics for treatment completers and non-completers are described in Table 1. Participants were predominantly male (66.7%), Caucasian (93.3%), non-Hispanic (100%), with a mean age of 32.48 years (SD: 11.2 years, range: 19–57 years), 46.7% were single, 43.3% were married. On average, they had completed 14.89 years of education (SD: 1.7), 6.7% were military veterans, and the majority (73.3%) were emergency medical service providers (i.e., emergency medical technicians or paramedics). Emergency response telecommunicators (i.e., 911 dispatchers) were also eligible, though none enrolled in the study. Participants were offered the option of receiving care via video conference, in person, or via a combination of formats. The majority (n = 21; 70.0%) completed treatment via video conference, followed by a combination of formats (n = 5; 16.7%), and in-person only (n = 4; 13.3%). Among the 30 emergency responders who began treatment, 24 (80.0%) completed treatment, defined as attending 8 or more sessions. On average, treatment completers completed 15.41 sessions (range: 8–20), whereas those who dropped out completed an average of 6.17 sessions (range: 4–7). Clinical characteristics are also presented in Table 1. On average, participants scored above the recommended cutoff score for screening positive for PTSD among emergency responders on the PCL-5 (M = 43.10; SD = 19.2). Therapeutic working alliance, as measured by the WAI-SR, was high among treatment completers (M = 52.14 out of 60) as well as those who did not complete treatment (M = 50.0). Treatment completers did not differ from non-completers on any demographic, employment-related, or clinical characteristic. In terms of safety, there were two serious adverse events during the study (medical hospitalizations), neither of which were deemed by the IRB to be study related.
Table 1
| Characteristics | Treatment completers (n = 24) | Non-completers (n = 6) | p-value |
|---|---|---|---|
| Age | 32.74 (11.3) | 31.50 (12.0) | .814 |
| Years of education | 15.00 (1.7) | 14.50 (1.9) | .545 |
| Sex: male; n (%) | 16 (66.7) | 4 (66.7) | .999 |
| Ethnicity: Latinx n (%) | 0 (0) | 0 (0) | – |
| Race n (%) | .272 | ||
| American Indian/Alaska Native | 0 (0) | 0 (0) | |
| Asian/Asian American | 1 (4.1) | 1 (16.7) | |
| Black or African American | 0 (0) | 0 (0) | |
| White | 23 (95.8) | 5 (83.3) | |
| Marital status n (%) | .332 | ||
| Single | 10 (41.6) | 4 (66.7) | |
| Married or cohabitating | 12 (50.0) | 1 (16.7) | |
| Separated, divorced, or widowed | 2 (8.3) | 1 (16.7) | |
| Military veteran n (%) | 2 (8.3) | 0 (0) | .464 |
| Type of emergency responder n (%) | .761 | ||
| Emergency medical service (technician or paramedic) | 17 (70.8) | 5 (83.3) | |
| Fire fighter | 2 (8.3) | 0 (0) | |
| Law enforcement officer | 3 (12.5) | 1 (16.7) | |
| Emergency room medical provider | 2 (8.3) | 0 (0) | |
| Clinical/treatment characteristics | |||
| PCL-5 | 43.25 (18.0) | 42.50 (25.2) | .933 |
| Positive screen for PTSD n (%) | 11 (45.8) | 4 (66.7) | .361 |
| AUDIT | 6.83 (7.2) | 4.33 (5.8) | .437 |
| Positive screen for alcohol use disorder n (%) | 7 (29.2) | 1 (16.7) | .536 |
| PHQ-9 | 14.00 (6.0) | 12.67 (9.5) | .667 |
| GAD-7 | 11.83 (6.1) | 14.17 (9.1) | .454 |
| DUDIT | 0.71 (2.0) | 0 (0) | .397 |
| Positive screen for drug use disorder n (%) | 0 (0) | 0 (0) | – |
| PSQI | 11.33 (3.9) | 8.67 (6.5) | .202 |
| WSAS | 17.63 (8.9) | 19.17 (13.0) | .732 |
| WHOQOL-total | 85.92 (12.8) | 84.33 (24.4) | .825 |
| VT | 11.92 (4.4) | 10.50 (3.9) | .475 |
| WAI-SR at session 4 | 52.14 (6.9)a | 50.00 (7.3)b | .579 |
| AAQ-II | 28.96 (8.3) | 28.83 (15.4) | .985 |
| DERS | 46.96 (15.2) | 50.17 (20.4) | .668 |
| BFI-2-N | 38.13 (9.0) | 40.50 (13.6) | .606 |
Baseline demographic and clinical characteristics by treatment completion status.
Data presented as M (SD) except where otherwise noted; PTSD, posttraumatic stress disorder. PCL-5, posttraumatic stress disorder checklist for DSM-5; PHQ-9, patient health questionnaire 9 Item- depression; GAD-7, generalized anxiety disorder-7; AUDIT, alcohol use disorders identification test; WSAS, work and social adjustment scale; WHOQOL, World Health Organization quality of life; VT, values tracker; PSQI, Pittsburgh sleep quality index; WAI-SR, working alliance inventory-self-report; AAQ-II, acceptance and action questionnaire-II; DERS, difficulties in emotion regulation scale; BFI-2-N, brief five factor inventory negative emotionality scale.
n = 21.
n = 4.
3.2 Main findings
Treatment outcome results are presented in Table 2. Of the 24 treatment completers, 20 (83.3%) completed a post-treatment assessment at the time of the final treatment session, and 15 (62.5%) completed the one-month follow-up assessment. There was a statistically significant reduction in self-reported PTSD symptoms on the PCL-5 at post-treatment, p < .001, g = 1.40 that remained significant at one-month follow-up, p = .002, g = 1.48 (large effects). The change in PCL-5 scores from pre-treatment to post-treatment (22.2 points) and follow-up (23.6 points) exceeded guidelines for determining clinically reliable change (81). There was a statistically significant reduction in depressive symptoms on the PHQ-9 at post-treatment that was sustained at follow-up, p-values <.001, g's = 1.29 and 1.26, respectively (large effects). On average, scores were reduced from the moderate depressive symptoms range at pre-treatment to the mild symptom range at post-treatment and follow-up. There was a significant reduction in anxiety symptoms on the GAD-7 at post-treatment that was sustained at follow-up, p-values <.001, g's = 1.13 and 1.01, respectively (large effects). On average, scores were reduced from the moderate anxiety symptoms range at pre-treatment to the mild symptom range at post-treatment and the no symptoms range at follow-up. There was not a statistically significant reduction in symptoms of alcohol use disorder on the AUDIT at posttreatment or at follow-up (g's = .22 and .23, negligible effects). There was a significant reduction in functional impairment on the WSAS at post-treatment that was sustained at follow-up, p-values <.001, g's = 1.16 and 1.07 (large effects). We observed a significant increase in overall quality of life on the WHOQOL at post-treatment that was sustained at follow-up, p-value =.007, g's = −.89 and −.81 (large effects). The increases in values-consistent actions on the VT were small at post-treatment (p = .333; g = −.34) and medium-to-large at follow-up (p = .050; g = −.77), though these changes were not statistically significantly different from zero. The improvement in sleep quality, assessed using the PSQI total scores during treatment (p = .071; g = .42, small effect) were not statistically significantly different from zero; however, PSQI total scores at follow-up were significantly greater than at pre-treatment (g = .69, medium effect, p = .008). On the subset of PSQI items thought to be more likely to improve among those receiving the UP, the effects were similar in magnitude compared to the PSQI total scores, though the change was statistically significant at both post-treatment (p = .023; g = .51, medium effect) and at follow-up (g = .57, medium effect, p = .011).
Table 2
| Measure | Pre-treatment n = 24 |
Post-treatment n = 20 |
1 month post-treatment n = 15 |
|||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | g 95% CI |
M | SD | g 95% CI |
|
| PCL-5 | 42.00 | 18.7 | 17.85 | 13.9 | 1.40*** .64–2.16 |
16.40 | 14.8 | 1.28** .41–2.16 |
| PHQ-9 | 13.25 | 5.3 | 5.65 | 5.9 | 1.29*** .62–1.96 |
5.20 | 5.1 | 1.26*** .50–2.03 |
| GAD-7 | 11.00 | 5.9 | 4.35 | 5.3 | 1.13*** .56–1.71 |
3.87 | 4.9 | 1.01*** .41–1.62 |
| AUDIT | 6.95 | 7.7 | 5.25 | 7.5 | 0.22 −.03 to .46 |
6.13 | 7.9 | .23 −.05 to .51 |
| WSAS | 17.25 | 9.3 | 7.05 | 7.5 | 1.16*** .45–1.88 |
5.67 | 6.7 | 1.07** .22–1.92 |
| WHOQOL-total | 86.30 | 12.7 | 98.70 | 14.0 | −.89** −1.46 to −.32 |
96.93 | 12.6 | −.81** −1.45 to −.17 |
| VT | 12.35 | 4.5 | 13.90 | 4.3 | −.34 −.99 to −.32 |
14.87 | 2.7 | −.77 −1.59 to .06 |
| PSQI | 10.95 | 3.6 | 9.00 | 5.0 | .42 −.06 to .90 |
8.67 | 3.2 | .69** .14–1.24 |
| AAQ-II | 28.35 | 6.5 | 18.75 | 9.7 | 1.11** .40–1.82 |
17.27 | 9.6 | 1.23*** .42–2.03 |
| DERS | 44.45 | 13.4 | 30.35 | 15.2 | .94*** .38–1.51 |
28.93 | 13.4 | .99*** .35–1.63 |
| BFI-2-N | 38.13 | 9.0 | 26.29 | 11.8 | 1.09*** .46–1.72 |
29.00 | 9.1 | .80** .20–1.39 |
Changes in treatment outcomes and treatment mechanisms between Pre-treatment and 1 month post-treatment in treatment completers.
PCL-5, posttraumatic stress disorder checklist for DSM-5; PHQ-9, patient health questionnaire 9 Item- depression; GAD-7, generalized anxiety disorder-7; AUDIT, alcohol use disorders identification test; WSAS, work and social adjustment scale; WHOQOL, World Health Organization quality of life; VT, values tracker; PSQI, Pittsburgh sleep quality index; AAQ-II, acceptance and action questionnaire-II; DERS, difficulties in emotion regulation scale; BFI-2-N, brief five factor inventory negative emotionality scale.
p < .01; ***p < .001.
Next, we analyzed treatment outcomes for those who screened positive for PTSD at pre-treatment (Table 3). Half of the entire sample (n = 15; 50.0%) screened positive for PTSD at baseline. Nearly half of treatment completers (n = 11; 45.8%) screened positive for PTSD at pre-treatment, of whom 8 (72.7%) provided outcome data at post-treatment and 6 (54.5%) provided data at follow-up. Given the smaller sample, we focus on effect sizes in this summary of the findings, though results pertaining to statistical significance may be found in Table 3. In terms of the overall pattern of findings, the effect sizes at post-treatment and follow-up were larger for those who screened positive for PTSD at pre-treatment compared with the total completers sample on most outcome measures. There were large reductions in PTSD symptoms on the PCL-5 at post-treatment (g = 2.92) and follow-up (g = 3.12). The changes in PCL-5 scores at post-treatment (40.3 points) and follow-up (44.1 points) exceeded guidelines for clinically reliable change. As presented in Figure 1, those who screened positive for PTSD at pre-treatment reported symptom severity equivalent to those who had screened negative for PTSD at both post-treatment and follow-up. There were large reductions in depressive symptoms on the PHQ-9 at post-treatment and follow-up (g = 2.29 and 2.49, respectively). On average, scores were reduced from the moderately severe depressive symptoms range at pre-treatment to the mild symptom range at post-treatment and follow-up. There was a large reduction in anxiety symptoms on the GAD-7 at post-treatment (g = 1.39) that was reduced to a medium effect at follow-up (g = .61). On average, scores were reduced from the moderate anxiety symptoms range at pre-treatment to the no symptom range at post-treatment and follow-up. There was no change in symptoms of alcohol use disorder on the AUDIT at posttreatment or follow-up (g's = .10 and.14, negligible effects). We observed large improvements in functional impairment on the WSAS at post-treatment and follow-up (g = 2.17 and 2.57). We observed large increases in quality of life on the WHOQOL at post-treatment and follow-up (g = −.93 and −1.61) and on values-consistent actions on the VT at post-treatment and follow-up (g = −.88 and −1.81). There was a small-to-medium sized improvement in PSQI total scores at post-treatment (g = .46) and a large effect at follow-up (g = 1.89). On the subset of PSQI items thought to be more likely to improve among those receiving the UP, the effects were similar compared to the PSQI total scores at post-treatment (g = .60, medium effect) and at follow-up (g = 1.02, large effect).
Table 3
| Measure | Pre-treatment n = 8 |
Post-treatment n = 8 |
1 month post-treatment n = 6 |
|||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | g 95% CI |
M | SD | g 95% CI |
|
| PCL-5 | 59.88 | 14.6 | 19.63 | 9.8 | 2.92** .66–5.19 |
15.80 | 6.4 | 3.12** −.33 to 6.56 |
| PHQ-9 | 16.13 | 4.7 | 5.38 | 3.5 | 2.29** .49–4.09 |
5.40 | 2.2 | 2.49* −.45 to 5.42 |
| GAD-7 | 14.00 | 6.9 | 4.75 | 4.4 | 1.39** .16–2.61 |
3.40 | 1.8 | .61* −.23 to 1.46 |
| AUDIT | 6.88 | 11.1 | 5.50 | 9.9 | .10 −.07 to .28 |
8.20 | 11.5 | .14 −.16 to .45 |
| WSAS | 22.13 | 6.3 | 7.25 | 5.9 | 2.17** .37–3.96 |
5.20 | 4.1 | 2.57* −.50 to 5.65 |
| WHOQOL-Total | 80.75 | 10.7 | 95.75 | 16.6 | −.93* −1.95. to .09 |
93.00 | 11.9 | −1.61* −3.82 to .59 |
| VT | 11.38 | 5.2 | 15.25 | 2.6 | −.88 −2.36. to .60 |
14.60 | 2.5 | −1.81 −4.38 to .77 |
| PSQI | 12.25 | 2.6 | 10.38 | 4.5 | .46 −.77 to 1.68 |
9.6 | 2.3 | 1.89* −.30 to 4.08 |
| AAQ-II | 33.63 | 5.0 | 19.50 | 7.9 | 1.92** .22–3.62 |
17.60 | 6.7 | 2.29** −.16 to 4.74 |
| DERS | 52.25 | 6.8 | 30.38 | 11.8 | 1.99** .41–3.57 |
28.20 | 10.1 | 1.94** −.14 to 4.03 |
| BFI-2-N | 42.91 | 8.7 | 26.00 | 13.6 | 1.38** .21–2.55 |
29.40 | 6.8 | 1.14 −.61 to 2.89 |
Changes in treatment outcomes and treatment mechanisms between pre-treatment and 1 month post-treatment in participants who screened positive for posttraumatic stress disorder at baseline.
PCL-5, posttraumatic stress disorder checklist for DSM-5; PHQ-9, patient health questionnaire 9 Item- depression; GAD-7, generalized anxiety disorder-7; AUDIT, alcohol use disorders identification test; WSAS, work and social adjustment scale; WHOQOL, World Health Organization quality of life; VT, values tracker; PSQI, Pittsburgh sleep quality index; AAQ-II, acceptance and action questionnaire-II; DERS, difficulties in emotion regulation scale; BFI-2-N, brief five factor inventory negative emotionality scale.
p < .05. **p < .01.
Figure 1
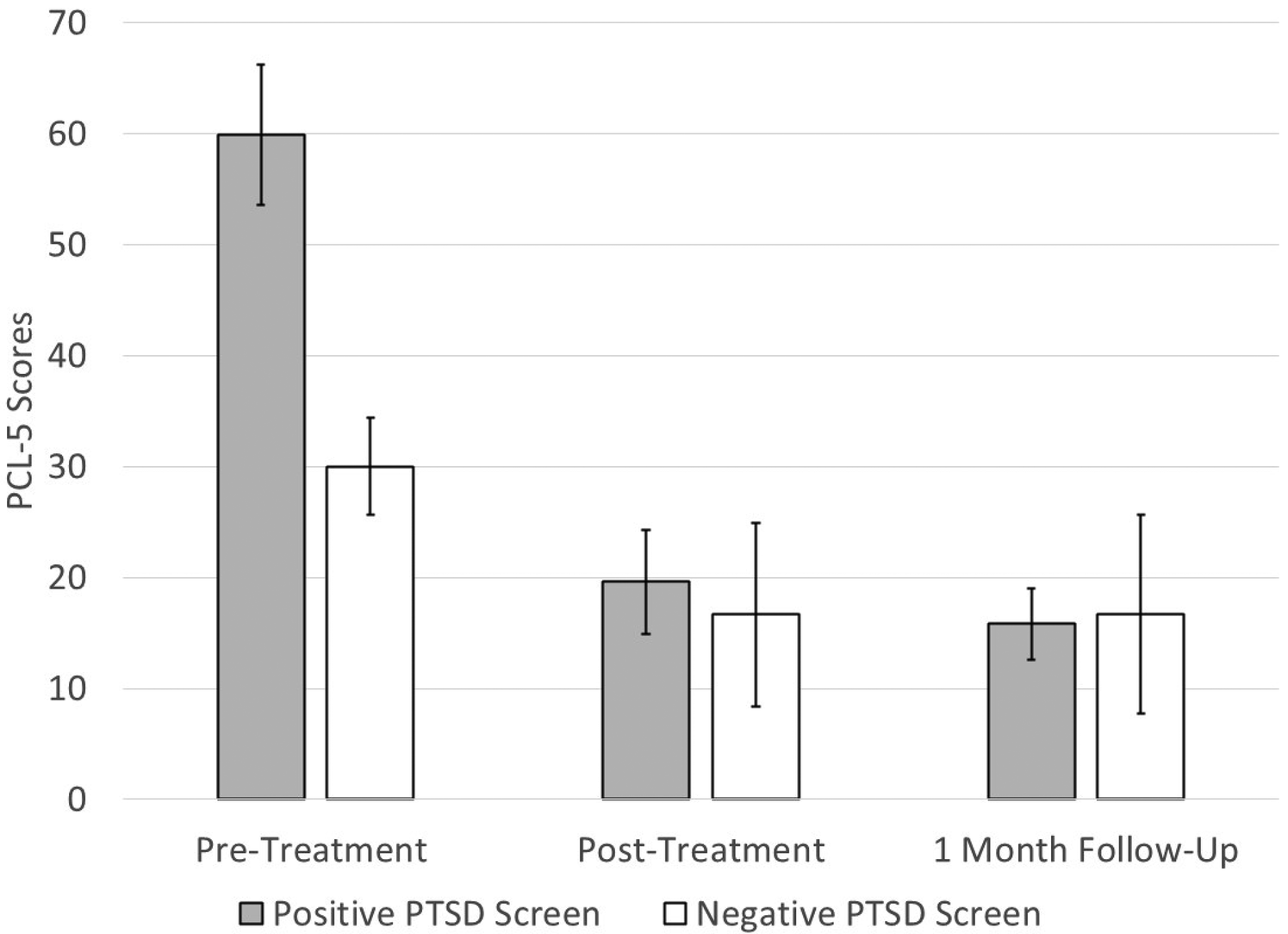
Changes in PCL-5 scores from pre-treatment to post-treatment and 1-month follow-up in those who screened positive and negative for posttraumatic stress disorder (PTSD) at pre-treatment. The error bars represent one standard deviation. The sample sizes are as follows: pre-treatment (n = 8), post-treatment (n = 8), follow-up (n = 6).
Within the total sample, 8 (26.7%) screened positive for AUD. Among treatment completers, 7 (29.2%) screened positive for AUD, of whom 6 completed the post-treatment assessment and 5 provided follow-up data. AUDIT scores decreased from M = 15.3 (SD = 8.8) at pre-treatment to M = 11.5 (SD = 11.2) at post-treatment (g = .32; small effect) and from M = 16.4 (SD = 9.5) at pre-treatment to M = 12.6 (SD = 10.9) at follow-up (g = .30; small effect).
3.3 Treatment mechanisms
Changes in the putative treatment mechanisms are presented in Tables 2, 3. We observed large, statistically significant changes in each of the putative treatment mechanisms (psychological inflexibility on the AAQ-II, difficulties in emotion regulation on the DERS, and NNE on the BFI-2-N) during treatment and at follow-up in the total sample of treatment completers. We observed a similar pattern of large, statistically significant changes in each of the treatment mechanisms at follow-up, with the exception that the change in scores on the BFI-2-N was not statistically significantly different from zero at follow-up despite a large effect (g = 1.14) due to the small sample size.
We explored the associations between changes in the treatment outcomes during treatment and at follow-up and changes in the treatment mechanisms during treatment. These results are presented in Table 4. Correlations between reductions in each of the mechanistic variables and improvements in mental health symptoms (PCL-5, PHQ-9, GAD-7) were uniformly high, with r's ranging from .533 to .866 (p-values .016 to <.001). Correlations between improvements in AUD symptoms on the AUDIT and reductions in the treatment mechanisms during treatment were not significant. At follow-up, improvements in AUDIT at follow-up were associated with reductions in AAQ-II (r = .613, p = .015) and DERS (r = .528, p = .043). There were large associations between improvements in sleep quality on the PSQI and reductions in all three mechanistic variables at post-treatment and at follow-up (r's .549 to .690; p-values .012–.004), with the exception that the correlation with reduction in BFI-2-N was not statistically significant at follow-up (r = .472, p = .076). There were large associations between improvements in functional impairment on the WSAS and reductions in all three mechanistic variables at post-treatment and at follow-up (r's. 711 to .889; p-values.001 to <.001), with the exception that the correlation with reduction in BFI-2-N did not reach statistical significance at post-treatment (r = .408, p = .074). Improvements in quality of life on the WHOQOL were associated with reductions in all three mechanistic variables at post-treatment (r's .588 to. 741; p-values.006 to <.001), whereas none of these correlations were significant at follow-up (r's .217 to .393). At post-treatment, increased engagement in values-consistent behaviors on the VT was associated with reductions in AAQ-II (r = .450, p = .046) and DERS (r = .540, p = .014), whereas the association with changes in BFI-2-N was not statistically significant (r = .442, p = .051). At follow-up, changes in VT scores were not associated with changes in any of the mechanistic variables. For comparison, the association between therapeutic alliance on the WAI-SR and changes in treatment outcomes were much smaller and were not statistically significantly different from zero for any treatment outcome. Overall, there was little difference in the mean correlation between changes in these mechanistic variables and changes across all outcomes: AAQ-II mean r = .60; DERS = .58; BFI-2-N = .49.
Table 4
| Change in outcome |
WAI-SRa | AAQ-II | DERS | BFI-2-N | PSQI |
|---|---|---|---|---|---|
| PCL-5 pre-post | .117 | .858*** | .789*** | .594** | .588** |
| PCL-5 pre-follow-up | .098 | .821*** | .866*** | .687** | .724** |
| PHQ-9 pre-post | .200 | .665** | .539* | .533* | .541* |
| PHQ-9 pre-follow-up | .338 | .711** | .590* | .666** | .574* |
| GAD-7 pre-post | .064 | .655** | .579** | .547* | .576** |
| GAD-7 pre-follow-up | .115 | .665** | .650** | .717** | .675** |
| AUDIT pre-post | -.015 | .336 | .350 | .165 | .272 |
| AUDIT pre-follow-up | .143 | .613* | .528* | .368 | .279 |
| WSAS pre-post | .101 | .711*** | .718*** | .408 | .467* |
| WSAS pre-follow-up | .164 | .889*** | .778*** | .752** | .790*** |
| WHOQOL total pre-post | .336 | .686*** | .588** | .741*** | .600** |
| WHOQOL total pre-Follow-up | .049 | .244 | .217 | .393 | .121 |
| VT pre-post | .162 | .450* | .540* | .442 | .609** |
| VT pre- follow-up | -.276 | -.033 | .257 | -.267 | .476 |
| PSQI pre-post | .152 | .636** | .576** | .549* | – |
| PSQI pre-follow-up | .035 | .690** | .659** | .472 | – |
Correlations between changes in treatment mechanisms during treatment and changes in treatment outcomes at post-treatment and at follow-up and between therapeutic alliance and changes in treatment outcomes.
PCL-5, posttraumatic stress disorder checklist for DSM-5; PHQ-9, patient health questionnaire 9 Item- depression; GAD-7, generalized anxiety disorder-7; AUDIT, alcohol use disorders identification test; WSAS, work and social adjustment scale; WHOQOL, World Health Organization quality of life; VT, values tracker; PSQI, Pittsburgh sleep quality index; WAI-SR, working alliance inventory-self-report; AAQ-II, acceptance and action questionnaire-II; DERS, difficulties in emotion regulation scale; BFI-2-N, brief five factor inventory negative emotionality scale.
p < .05. **p < .01. ***p < .001.
WAI-SR was administered following session 4.
Finally, because improvements in sleep quality may drive improvements in mental health symptoms and related outcomes, we examined the association between changes in PSQI total scores and changes in the other treatment outcomes (Table 4). Improvements in PSQI were associated with reductions in mental health symptoms at post-treatment and at follow-up (r's.541 to.724; p-values .014–.002). Improvements in PSQI were not associated with reductions in AUDIT scores at post-treatment or follow-up. Improvements in PSQI were associated with improvements in WSAS at post-treatment and follow-up (r's.467 and.790, p-values.038 to <.001, respectively). Improvements in PSQI were associated with improvements in WHOQOL at post-treatment (r = .600, p = .005) but not at follow-up. Improvements in PSQI were associated with improvements in VT at post-treatment (r = .609, p = .004), though this correlation did not reach statistical significance at follow-up (r = .476, p = .073).
4 Discussion
Emergency responders are essential public safety workers that experience elevated rates of a number of emotional disorders linked to frequent trauma exposure, shift work and other factors that interfere with quality sleep, and myriad other occupational stressors. Multiple barriers impede treatment seeking in this population including lack of provider knowledge regarding emergency response culture, concerns about receiving treatment for symptoms linked to occupational stress, and scheduling challenges. The UP is an evidence-based approach to addressing inter-connected symptoms of emotional disorders; yet there are few published data on the UP in trauma exposed populations. One prior study examined the UP, culturally adapted for fire fighters, and delivered via video conferencing. That study reported strong feasibility, acceptability, and improvements in mental health symptoms and quality of life in fire fighters (26). The current study built on that prior study by examining a version of the UP that was more broadly culturally adapted for use across emergency response professions. In the current study, the UP was delivered, either in person or via video conferencing, to a mixed sample of emergency responders predominantly comprised of emergency medical professionals.
In terms of treatment feasibility and acceptability, we observed an (80.0%) treatment completion rate, which is comparable to that observed in our prior study of the UP delivered exclusively via video conferencing in fire fighters (80.3%). These treatment completion rates are high for a trauma exposed population (92, 93). Participants in this study reported that their working alliance with their clinician was quite strong, replicating our prior findings regarding therapeutic alliance. In the current study, the majority of treatment (70.0%) was delivered via video conferencing or via a combination of in-person and video (17.3%), indicating that this has become a preferred format within this population. Convenience was cited most often as the reason for this, though alleviation of concerns about stigma and privacy may also have been a factor.
All emergency responders are exposed to potentially traumatic events, and half of the current sample met screening criteria for PTSD. Among treatment completers, we observed large, statistically significant and clinically meaningful reductions in PTSD symptom severity that was maintained at one-month follow-up. These effect sizes closely mirrored—and were slightly larger than—the effects observed in the prior study of the UP in fire fighters. Similarly, we observed large, statistically and clinically significant effect size improvements in symptoms of depression and anxiety at post-treatment that were maintained at follow-up. Again, the magnitude of these improvements closely mirrored but was somewhat larger than the effects observed in the study of the UP with fire fighters. Reductions in symptoms of PTSD, depression, and anxiety were even greater among the subgroup of participants who screened positive for PTSD at pre-treatment. By post-treatment, these participants reported PTSD symptom severity levels that were lower than the pre-treatment PTSD symptom levels for those who screened negative for PTSD. Among participants who screened positive for AUD, we observed small reductions in AUD symptoms. This finding differs from our prior study (26) in which we observed large improvements in AUD symptoms. Of note, the sample size was much smaller in the current study (n = 6), which also used a different measure of AUD than our prior study. Additional research is warranted regarding the effect of the UP on symptoms of AUD in trauma exposed populations.
We also observed strong links between the UP and improvements in several other outcomes. We observed large effect size improvements in quality of life at post-treatment and follow-up, which replicated the finding from the prior study of fire fighters. We also observed large effect size improvements in a measure of impairment in occupational and social functioning at post-treatment and follow-up. We administered a measure of engagement in behaviors that participants view as being consistent with their sense of personal values, meaning, and purpose. On this measure, we observed small effect size improvements at post-treatment and medium-to-large effects at follow-up. This finding, while moderate in magnitude, is noteworthy given that engagement in values-consistent action is not an explicit goal within the UP as in other transdiagnostic treatments such as Acceptance and Commitment Therapy. Next, we examined changes in sleep quality, which is understudied within the broader context of mental health treatment in emergency responders. Moreover, this is a novel area of inquiry, with no published RCTs of the UP for sleep problems to date. At post-treatment, we observed small effect size improvements in sleep quality. However, by follow-up, these improvements represented a medium effect and were statistically significant. Although our adaptation of the UP included greater emphasis on sleep problems than is present in the standard UP, additional modifications may be warranted given the high prevalence of sleep problems in emergency responders. For example, incorporating stimulus control techniques and providing psychoeducation regarding shift work and sleep may confer additional benefits. Next, reductions in alcohol misuse symptoms were small and were not statistically significant. The effect of the UP on alcohol misuse symptoms was somewhat larger in the prior study of the UP in fire fighters in which the proportion of participants who screened positive for AUD was greater than in the current study. The mixed findings across these two studies indicate that the UP has potential for reducing alcohol misuse, though future work should focus on tailoring skills within the UP toward reducing reliance on alcohol as an emotion regulation strategy within the context of co-occurring mental health challenges. Examining whether the UP is associated with reductions in AUD symptoms is also novel, as no published trials have examined this. Overall, these findings, particularly when combined with the prior study in fire fighters, indicates that the UP is a strong match for efficiently addressing the behavioral health needs of emergency responders living with the most common types of challenges observed in this occupational group.
We sought to validate and enhance understanding of treatment mechanisms targeted by the UP, particularly within a trauma exposed sample given the lack of data in this population. We observed large, statistically significant changes in each of these mechanistic variables—NNE, difficulties in emotion regulation, and experiential avoidance—at both post-treatment and follow-up. We observed large associations between reductions in each of these variables during treatment and improvements in mental health symptoms at post-treatment and at follow-up (mean r = .67). Reductions in functional impairment were associated with reductions in each of the mechanistic variables (mean r = .77), with the exception of a medium-sized correlation with reductions in NNE at post-treatment. Changes in each of the mechanistic variables were linked with improved quality of life at post-treatment, though not at follow-up. Interestingly, improved engagement in values-consistent behavior was moderately linked with changes in each of the mechanisms at post-treatment, though not at follow-up. Whereas experiential avoidance has been discussed in the literature as impeding consistent values engagement, these findings suggest that high levels of negative emotion may be more broadly linked with this outcome. We observed similarly large links between changes in these mechanistic variables and improved sleep quality across both measurements (mean r = .60). This finding provides evidence that changes in emotion-related treatment mechanisms are linked with improved sleep and underscores the potential of emotion-focused treatment such as the UP for addressing sleep problems in the context of co-occurring mental health symptoms. Finally, there is no clear consensus in the literature regarding whether it makes sense to target sleep problems as a prelude to addressing trauma related mental health symptoms vs. addressing trauma related symptoms first and then treating any residual sleep problems following treatment for PTSD [see (94) for discussion of this issue]. Therefore, we examined changes in sleep quality during treatment as a mechanistic variable. Improved sleep quality during treatment was associated with most outcome variables at post-treatment and follow-up, indicating that improved sleep quality may help to explain changes—or maintenance of changes—in mental health symptoms and functional outcomes in people receiving the UP.
This study was novel in piloting a culturally adapted version of the UP, which has not yet been extensively tested as a treatment in trauma exposed samples, with emergency responders, an understudied group in relation to the size of this population and the frequency of trauma exposure that they encounter. In terms of clinical implications, our cultural adaptation process, which now includes review by fire, police, and emergency medical personnel across two studies, indicates that only a small number of modifications to the UP were warranted when using the UP with emergency responders. Our adaptations were minor; they consisted of (1) removing a suggestion related to avoiding caffeine because of norms around caffeine use among emergency responders, (2) adding all-or-nothing thinking as a thinking trap to which emergency responders are frequently susceptible, and (3) probing regarding the presence of sleep-related thinking traps given the prevalence of sleep problems in emergency responders. Thus, those who are trained in using the UP but who have little experience working with emergency responders may find that adding these adaptations, along with receiving basic training in emergency response culture, may be sufficient to support them in working with this population.
Strengths of the current study include use of well-validated, widely used self-report measures and broad eligibility criteria, both of which are likely representative of procedures used in clinical practice. The findings of this study should be interpreted in the context of several limitations. The lack of a control group precludes our ability to infer causality regarding the impact of the UP on changes in the outcomes. The racial and ethnic diversity within this sample was low, though it was likely broadly representative of the demographics within emergency response departments—particularly emergency medical services and fire service—in our region. Results pertaining to the subgroup of participants who screened positive for PTSD should be interpreted with particular caution, owing to the small sample size, though these results were consistent with those observed in a subsample that screened positive for PTSD in a prior study of the UP in fire fighters that had a somewhat larger sample (26). Our sample largely consisted of emergency medical service personnel, whereas we had anticipated having a more mixed sample of emergency responders. We received many word-of-mouth referrals to the study within emergency service departments, underscoring the need for services and satisfaction with the treatment received through this project. The generalizability of these findings to other emergency responder professions may be limited, though we again reference the similarity of the current findings to our prior study of fire fighters (26). While we believe that the cultural adaptations enhanced the impact of the UP with this population, our study design did not allow us to empirically evaluate the impact of these adaptations. The small sample in this pilot study precluded examining treatment mechanisms using mediation analyses, which would be preferred for examining these relationships. A larger sample would also allow for more complex modeling analyses that would allow for testing of multiple mediators simultaneously to determine which variables are influencing changes in the outcome while accounting for the other mediators. Finally, although the study therapists received training and ongoing supervision in delivering the UP, the lack of formal fidelity monitoring is a limitation. Overall, the current findings support use of the UP and add to the burgeoning literature on the UP in trauma exposed populations, including emergency responders. The current findings indicate that controlled research is warranted examining the UP in trauma exposed populations. Future, controlled research with a larger, more diverse sample would allow for conclusions to be drawn regarding treatment efficacy, more rigorous examination of treatment mechanisms, and more generalizable findings.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, pending approval of a data use agreement.
Ethics statement
The studies involving humans were approved by University of Pittsburgh Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SR: Investigation, Supervision, Writing – review & editing. EC: Supervision, Writing – review & editing. DT: Conceptualization, Data curation, Formal analysis, Writing – review & editing. SG: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by a grant from the University of Pittsburgh (PI: Eric Meyer). The funding source has or has had no involvement in the study design, the collection, analysis and interpretation of data, the writing of this report, or the decision to submit this article for publication.
Acknowledgments
We thank our participants, the project coordinator Melanie Cherry, Professor Thomas Platt for reviewing the manuscript, and the project clinicians: Amanda Fedunok, Nicole Fuhr, Jackilyn Garces, MeLoni Griffin, Hermione Huo, and Emily Kirschner.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Carleton RN Afifi TO Turner S Taillieu T Duranceau S LeBouthillier DM et al Mental disorder symptoms among public safety personnel in Canada. Can J Psychiatry. (2018) 63:54–64. 10.1177/0706743717723825
2.
Kimbrel NA Steffen LE Meyer EC Kruse MI Knight JA Zimering RT et al A revised measure of occupational stress for fire fighters: psychometric properties and relations with PTSD, depression, and substance abuse. Psychol Serv. (2011) 8:294–306. 10.1037/a0025845
3.
Carleton RN Afifi TO Taillieu T Turner S Mason JE Ricciardelli R et al Assessing the relative impact of diverse stressors among public safety personnel. Int J Environ Res Public Health. (2020) 17:1234. 10.3390/ijerph17041234
4.
Kearney J Muir C Smith K Meadley M . Exploring factors associated with paramedic work-related psychological injury through data linkage. J Saf Res. (2023) 86:213–25. 10.1016/j.jsr.2023.05.012
5.
Meyer EC Zimering R Daly ES Kamholz BW Knight JK Gulliver SB . Predictors of posttraumatic stress disorder and other psychological symptoms in trauma exposed firefighters. Psychol Serv. (2012) 9(1):1–15. 10.1037/a0025414
6.
Billings J Focht W . Firefighter shift schedules affect sleep quality. J Occup Environ Med. (2016) 58(3):294–8. 10.1097/JOM.0000000000000624
7.
Stanley IH Hom MA Joiner TE . A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin Psychol Rev. (2016) 44:25–44. 10.1016/j.cpr.2015.12.002
8.
Heber A Testa V Smith-MacDonald L Brémault-Phillips S Smith-MacDonald L . Rapid response to COVID-19: addressing challenges and increasing the mental readiness of public safety personnel. Health Promot Chronic Dis Prev Can. (2020) 40:350–5. 10.24095/hpcdp.40.11/12.04
9.
Patel H Easterbrook B D’Alessandro-Lowe AM Andrews K Ritchie K Hosseiny F et al Associations between trauma and substance use among healthcare workers and public safety personnel during the SARS-CoV-2 (COVID-19) pandemic: the mediating roles of dissociation and emotion dysregulation. Eur J Psychotraumatol. (2023) 1:2180706. 10.1080/20008066.2023.2180706
10.
Xue Y Lopes J Ritchie K D’Alessandro AM Banfield L McCabe RE et al Potential circumstances associated with moral injury and moral distress in healthcare workers and public safety personnel across the globe during COVID-19: a scoping review. Front Psychiatry. (2022) 13:863232. 10.3389/fpsyt.2022.863232
11.
Iranmanesh S Tirgari B Bardsiri HS . Post-traumatic stress disorder among paramedic and hospital emergency personnel in south-east Iran. World J Emerg Med. (2013) 4:26–31. 10.5847/wjem.j.issn.1920-8642.2013.01.005
12.
Klimley KE Van Hasselt VB Stripling AM . Posttraumatic stress disorder in police, firefighters, and emergency dispatchers. Aggress Violent Behav. (2018) 43:33–44. 10.1016/j.avb.2018.08.005
13.
Maia DB Marmar CR Metzler T Nóbrega A Berger W Mendlowicz MV et al Post-traumatic stress symptoms in an elite unit of Brazilian police officers: prevalence and impact on psychosocial functioning and on physical and mental health. J Affect Disord. (2007) 97:241–5. 10.1016/j.jad.2006.06.004
14.
Kessler RC Sonnega A Bromet E Hughes M Nelson CB . Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. (1995) 52:1048–60. 10.1001/archpsyc.1995.03950240066012
15.
Courtney JA Francis AJP Paxton SJ . Caring for the country: fatigue, sleep and mental health in Australian rural paramedic shiftworkers. J Community Health. (2013) 38:178–86. 10.1007/s10900-012-9599-z
16.
Hom MA Stanley IH Ringer FB Joiner TE . Mental health service use among firefighters with suicidal thoughts and behaviors. Psychiatr Serv. (2016) 67(6):688–91. 10.1176/appi.ps.201500177
17.
Hom MA Stanley IH Rogers ML Tzoneva M Bernert R Joiner TE . The association between sleep disturbances and depression among firefighters: emotion dysregulation as an explanatory factor. J Clin Sleep Med. (2016) 12:235–45. 10.5664/jcsm.5492
18.
Smith EC Burkle FM . Paramedic and emergency medical technician reflections on the ongoing impact of the 9/11 terrorist attacks. Prehosp Disaster Med. (2019) 34:56–61. 10.1017/S1049023X18001255
19.
Davey JD Obst PL Sheehan MC . The use of AUDIT as a screening tool for alcohol use in the police work-place. Drug Alcohol Rev. (2000) 19:49–54. 10.1080/09595230096147
20.
Haddock CK Jahnke SA Poston WSC Jitnarin N Kaipust CM Tuley B et al Alcohol use among firefighters in the central United States. Occup Med (Chic Ill). (2012) 62(8):661–4. 10.1093/occmed/kqs162
21.
Violanti JM Slaven JE Charles LE Burchfiel CM Andrew ME Homish GG . Police and alcohol use: a descriptive analysis and associations with stress outcomes. Am J Crim Justice. (2011) 36:344–56. 10.1007/s12103-011-9121-7
22.
McCarty WP Aldirawi H Dewald S Palacios M . Burnout in blue: an analysis of the extent and primary predictors of burnout among law enforcement officers in the United States. Policy Q. (2019) 22:278–304. 10.1177/1098611119828038
23.
Violanti JM Hartley TA Gu JK Fekedulegn D Andrew ME Burchfiel CM . Life expectancy in police officers: a comparison with the US general population. Int J Emerg Ment Health. (2013) 15(4):217–28.
24.
Violanti JM Owens SL McCanlies E Fekedulegn D Andrew ME . Law enforcement suicide: a review. Policing Int J. (2019) 42:141–64. 10.1108/PIJPSM-05-2017-0061
25.
Barlow DH Harris BA Eustis EH Farchione TJ . The unified protocol for transdiagnostic treatment of emotional disorders. World Psychiatry. (2020) 19:245–6. 10.1002/wps.20748
26.
Meyer EC Coe E Pennington ML Cammarata C Kimbrel NA Ostiguy W et al The unified protocol for transdiagnostic treatment of emotional disorders delivered via video conferencing to firefighters: pilot treatment outcomes highlighting improvements in alcohol use disorder and posttraumatic stress disorder symptoms. Cogn Behav Pract. (2022) 31:215–29. 10.1016/j.cbpra.2022.08.004
27.
Barlow DH Farchione TJ Sauer-Zavala S Latin HM Ellard KK Bullis JR et al Unified Protocol for Transdiagnostic Treatment of Emotional Disorders, Therapist Guide. 2nd ed. Oxford: Oxford Press (2018).
28.
Barlow DH Sauer-Zavala S Farchione TJ Latin HM Ellard KK Bullis JR et al Unified Protocol for Transdiagnostic Treatment of Emotional Disorders, Workbook. 2nd ed. Oxford: Oxford Press (2018).
29.
Gutner CA Galovski T Bovin MJ Schnurr PP . Emergence of transdiagnostic treatments for PTSD and posttraumatic distress. Curr Psychiatry Rep. (2016) 18(10):95. 10.1007/s11920-016-0734-x
30.
Hayes SC Hofmann SG , editors. Process-Based CBT: The Science and Core Competencies of Cognitive-Behavioral Therapy. Oakland, CA: Context Press (2018).
31.
Barlow DH Farchione TJ Bullis JR Gallagher MW Murray-Latin H Sauer-Zavala S et al The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis-specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry. (2017) 74(9):875–84. 10.1001/jamapsychiatry.2017.2164
32.
Carlucci L Saggino A Balsamo M . On the efficacy of the unified protocol for transdiagnostic treatment of emotional disorders: a systematic review and meta-analysis. Clin Psychol Rev. (2021) 87:101999. 10.1016/j.cpr.2021.101999
33.
Cassiello-Robbins C Southward MW Tirpak JW Sauer-Zavala S . A systematic review of unified protocol applications with adult populations: facilitating widespread dissemination via adaptability. Clin Psychol Rev. (2020) 78:101852. 10.1016/j.cpr.2020.101852
34.
Hood CO Southward MW Bugher C Sauer-Zavala S . A preliminary evaluation of the unified protocol among trauma-exposed adults with and without PTSD. Int J Environ Res Public Health. (2021) 18(21):11729. 10.3390/ijerph182111729
35.
O’Donnell ML Lau W Chisholm K Agathos J Little J Terhaag S et al A pilot study of the efficacy of the unified protocol for transdiagnostic treatment of emotional disorders in treating posttraumatic psychopathology: a randomized control study. J Trauma Stress. (2021) 34(3):563–74. 10.1002/jts.22650
36.
Sakiris N Berle D . A systematic review and meta-analysis of the unified protocol as a transdiagnostic emotion regulation based intervention. Clin Psychol Rev. (2019) 72:101751. 10.1016/j.cpr.2019.101751
37.
Varkovitzky RK Sherrill AM Reger GM . Effectiveness of the unified protocol for transdiagnostic treatment of emotional disorders among veterans with posttraumatic stress disorder: a pilot study. Behav Modif. (2018) 42(2):210–30. 10.1177/0145445517724539
38.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Text Revision. Washington, DC: American Psychiatric Association (2022). 10.1176/appi.books.9780890425787
39.
Doos Ali Vand H Gharraee B Asgharnejad Farid AA Ghaleh Bandi MF Habibi M . The effectiveness of transdiagnostic cognitive behavioral therapy for comorbid insomnia: a case report. Iran J Psychiatry. (2018) 13(2):154–9.
40.
Doos Ali Vand H Gharraee B Asgharnejad Farid A Ghaleh Bandi MF Habibi M . Investigating the effects of the unified protocol on common and specific factors in a comorbid insomniac sample: a single-case experimental design. Iran J Psychiatry Behav Sci. (2018) 12(3):e14452. 10.5812/ijpbs.14452
41.
Sauer-Zavala S Fournier JC Steele SJ Woods BK Wang M Farchione TJ et al Does the unified protocol really change neuroticism? Results from a randomized trial. Psychol Med. (2021) 51(14):2378–87. 10.1017/S0033291720000975
42.
Sauer-Zavala S Barlow DH . Neuroticism: A New Framework for Emotional Disorders and Their Treatment. New York: Guilford (2021).
43.
John OP Srivastava S . The big-five trait taxonomy: history, measurement, and theoretical perspectives. In: PervinLAJohnOP, editors. Handbook of Personality: Theory and Research (Vol. 2). New York: Guilford Press (1999). p. 102–38.
44.
Barlow DH Curreri AJ Woodard LS . Neuroticism and disorders of emotion: a new synthesis. Curr Dir Psychol Sci. (2021) 5:410–7. 10.1177/09637214211030253
45.
Connor-Smith JK Flachsbart C . Relations between personality and coping: a meta-analysis. J Pers Soc Psychol. (2007) 93:1080–107. 10.1037/0022-3514.93.6.1080
46.
Ireland ME Hepler J Li H Albarracín D . Neuroticism and attitudes toward action in 19 countries. J Pers. (2015) 83:243–50. 10.1111/jopy.12099
47.
Meyer EC Zimering RT Knight J Carpenter TC Kamholz B Morissette SB et al In firefighters, negative emotionality interacts with trauma exposure to prospectively predict PTSD symptoms during the first three years of service. J Trauma Stress. (2020) 34(2):333–44. 10.1002/jts.22632
48.
Patrick CJ Curtin JJ Tellegen A . Development and validation of a brief form of the multidimensional personality questionnaire. Psychol Assess. (2002) 14(2):150–63. 10.1037/1040-3590.14.2.150
49.
Lahey BB . Public health significance of neuroticism. Am Psychol. (2009) 64(4):241–56. 10.1037/a0015309
50.
Jeronimus BF Kotov R Riese H Ormel J . Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on longitudinal/prospective studies with 443,313 participants. Psychol Med. (2016) 46(14):2883–906. 10.1017/S0033291716001653
51.
Ruiz MA Pincus AL Dickinson KA . NEO PI-R predictors of alcohol use and alcohol-related problems. J Pers Assess. (2003) 81(3):226–36. 10.1207/S15327752JPA8103_05
52.
Settles RE Fischer S Cyders MA Combs JL Gunn RL Smith GT . Negative urgency: a personality predictor of externalizing behavior characterized by neuroticism, low consciousness, and disagreeableness. J Abnorm Psychol. (2012) 121(1):160–72. 10.1037/a0024948
53.
Boemo T Nieto I Vazquez C Sanchez-Lopez A . Relations between emotion regulation strategies and affect in daily life: a systematic review and meta-analysis of studies using ecological momentary assessments. Neurosci Biobehav Rev. (2022) 139:104747. 10.1016/j.neubiorev.2022.104747
54.
Kraiss JT Ten Klooster PM Moskowitz JT Bohlmeijer ET . The relationship between emotion regulation and well-being in patients with mental disorders: a meta-analysis. Compr Psychiatry. (2020) 102:152189. 10.1016/j.comppsych.2020.152189
55.
Seligowski AV Lee DJ Bardeen JR Orcutt HK . Emotion regulation and posttraumatic stress symptoms: a meta-analysis. Cogn Behav Ther. (2015) 44(2):87–102. 10.1080/16506073.2014.980753
56.
Stellern J Xiao KB Grennell E Sanches M Gowin JL Sloan ME . Emotion regulation in substance use disorders: a systematic review and meta-analysis. Addiction. (2022) 118(10):30–47. 10.1111/add.16001
57.
Griffith EL Jin L Contractor AA Slavish DC Vujanovic AA . Heterogeneity in patterns of posttraumatic stress disorder symptoms and sleep disturbances among firefighters: latent profile analyses. J Psychiatr Res. (2022) 153:64–72. 10.1016/j.jpsychires.2022.06.052
58.
Lebeaut A Zegel M Leonard SJ Bartlett BA Vujanovic AA . Examining transdiagnostic factors among firefighters in relation to trauma exposure, probable PTSD, and probable alcohol use disorder. J Dual Diagn. (2021) 17(1):52–63. 10.1080/15504263.2020.1854411
59.
Leonard SJ Vujanovic AA . Thwarted belongingness and PTSD symptom severity among firefighters: the role of emotion regulation difficulties. Behav Modif. (2022) 46(2):352–73. 10.1177/01454455211002105
60.
Godfrey DA Zegel M Babcock JC Vujanovic AA . Posttraumatic stress disorder and relationship satisfaction among firefighters: the role of emotion regulation difficulties. J Aggress Maltreat Trauma. (2022) 31(3):356–69. 10.1080/10926771.2022.2043973
61.
Tao Y Liu X Hou W Niu H Wang S Ma Z et al The mediating role of emotion regulation strategies in the relationship between big five personality traits and anxiety and depression among Chinese firefighters. Front Public Health. (2022) 10:901686. 10.3389/fpubh.2022.901686
62.
Hayes SC Strosahl KD Wilson KG . Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. 2nd ed. New York, NY: Guilford Press (2012).
63.
Bond FW Hayes SC Baer RA Carpenter KM Guenole N Orcutt HK et al Preliminary psychometric properties of the acceptance and action questionnaire–II: a revised measure of psychological flexibility and experiential avoidance. Behav Ther. (2011) 42:676–88. 10.1016/j.beth.2011.03.007
64.
Angelakis I Gooding P . Experiential avoidance in non-suicidal self-injury and suicide experiences: a systematic review and meta-analysis. Suicide Life Threat Behav. (2021) 51(5):978–92. 10.1111/sltb.12784
65.
Gamez W Chmielewski M Kotov R Ruggero C Suzuki N Watson D . The brief experiential avoidance questionnaire: development and initial validation. Psychol Assess. (2014) 26:35–45. 10.1037/a0034473
66.
Ong CW Barthel AL Hofmann SG . The relationship between psychological inflexibility and well-being in adults: a meta-analysis of the acceptance and action questionnaire. Behav Ther. (2024) 55(1):26–41. 10.1016/j.beth.2023.05.007
67.
Meyer EC La Bash H DeBeer BB Kimbrel NA Gulliver SB Morissette SB . Psychological inflexibility predicts PTSD symptom severity in war veterans after accounting for established PTSD risk factors and personality. Psychol Trauma. (2019) 11:383–90. 10.1037/tra0000358
68.
Hayes SC Luoma JB Bond FW Masuda A Lillis J . Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. (2006) 44(1):1–25. 10.1016/j.brat.2005.06.006
69.
Khakpoor S Mohammad BJ Saed O . Reductions in transdiagnostic factors as the potential mechanisms of change in treatment outcomes in the unified protocol: a randomized clinical trial. Res Psychother. (2019) 22(3):379. 10.4081/ripppo.2019.379
70.
Zemestani M Ommati P Rezaei F Gallagher MW . Changes in neuroticism-related constructs over the unified protocol for transdiagnostic treatment of emotional disorders in patients on an optimal dose of SSRI. Personal Disord. (2022) 13(2):171–81. 10.1037/per0000482
71.
Bulala J . The relationship between the utilization of mental health services, coping mechanisms, and reputation in male firefighters (Doctoral dissertation). Alliant International University, San Francisco, CA (2013).
72.
Gulliver SB Pennington ML Torres VA Steffen LE Mardikar A Leto F et al Behavioral health programs in fire service: surveying access and preferences. Psychol Serv. (2019) 16(2):340–5. 10.1037/ser0000222
73.
Halpern J Gurevich M Schwartz B Brazeau P . What makes an incident critical for ambulance workers? Emotional outcomes and implications for intervention. Work Stress. (2009) 23(2):173–89. 10.1080/02678370903057317
74.
Løvseth LT Aasland OG . Confidentiality as a barrier to social support: a cross-sectional study of Norwegian emergency and human service workers. Int J Stress Manag. (2010) 17(3):214–31. 10.1037/a0018904
75.
Zimmerman M Mattia JI . A self-report scale to help make psychiatric diagnoses: the psychiatric diagnostic screening questionnaire. Arch Gen Psychiatry. (2001) 58:787–94. 10.1001/archpsyc.58.8.787
76.
Harris GT Rice ME Camilleri JA . Applying a forensic actuarial assessment (the violence risk appraisal guide) to nonforensic patients. J Interpers Violence. (2004) 19:1063–74. 10.1177/0886260504268004
77.
Kroenke K Spitzer RL Williams JB . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. 10.1046/j.1525-1497.2001.016009606.x
78.
Berman A Bergman H Palmstierna T Schlyter F . Drug Use Disorders Identification Test Manual. Stockholm, Sweden: Karolinska Institutet (2005).
79.
Weathers FW Litz BT Keane TM Palmieri PA Marx BP Schnurr PP . The PTSD checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at:www. ptsd.va.gov (2013).
80.
Morrison K Su S Keck M Beidel DC . Psychometric properties of the PCL-5 in a sample of first responders. J Anxiety Disord. (2021) 77:102339. 10.1016/j.janxdis.2020.102339
81.
Marx BP Lee DJ Norman SB Bovin MJ Sloan DM Weathers FW et al Reliable and clinically significant change in the clinician-administered PTSD scale for DSM-5 and PTSD checklist for DSM-5 among male veterans. Psychol Assess. (2022) 34:197–203. 10.1037/pas0001098
82.
Spitzer RL Kroenke K Williams JB Löwe B . A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. 10.1001/archinte.166.10.1092
83.
Babor TF de la Fuente JR Saunders J Grant M . The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization (1992).
84.
Voluse AC Gioia CJ Sobell LC Dum M Sobell MB Simco ER . Psychometric properties of the drug use disorders identification test (DUDIT) with substance abusers in outpatient and residential treatment. Addict Behav. (2012) 37:36–41. 10.1016/j.addbeh.2011.07.030
85.
Buysse DJ Reynolds CF Monk TH Berman SR Kupfer DJ . The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. 10.1016/0165-1781(89)90047-4
86.
Mundt JC Marks IM Shear MK Greist JM . The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry. (2002) 180:461–4. 10.1192/bjp.180.5.461
87.
WHOQOL Group. Development of the world health organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28:551–8. 10.1017/s0033291798006667
88.
Pielech M Bailey RW McEntee ML Ashworth J Levell J Sowden G et al Preliminary evaluation of the values tracker: a two-item measure of engagement in valued activities in those with chronic pain. Behav Modif. (2016) 40:239–56. 10.1177/0145445515616911
89.
Soto CJ John OP . The next big five inventory (BFI-2): developing and assessing a hierarchical model with 15 facets to enhance bandwidth, fidelity, and predictive power. J Pers Soc Psychol. (2017) 113:117–43. 10.1037/pspp0000096
90.
Bjureberg J Ljótsson B Tull MT Hedman E Sahlin H Lundh LG et al Development and validation of a brief version of the difficulties in emotion regulation scale: the DERS-16. J Psychopathol Behav Assess. (2016) 38:284–96. 10.1007/s10862-015-9514-x
91.
Munder T Wilmers F Leonhard R Linster HW Barth J . Working alliance inventory—short revised (WAI-SR): psychometric properties in outpatients and inpatients. Clin Psychol Psychother. (2010) 17(3):231–9. 10.1002/cpp.658
92.
Edwards-Stewart A Smolenski DJ Bush NE Cyr B-A Beech EH Skopp ,NA et al Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. J Trauma Stress. (2021) 34:808–18. 10.1002/jts.22653
93.
Kehle-Forbes SM Meis LA Spoont MR Polusny MA . Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma. (2016) 8:107–14. 10.1037/tra0000065
94.
Taylor DJ Pruiksma KE Mintz J Slavish DC Wardle-Pinkston S Dietch JR et al Treatment of comorbid sleep disorders and posttraumatic stress disorder in U.S. active duty military personnel: a pilot randomized clinical trial. J Trauma Stress. (2023) 36:712–26. 10.1002/jts.22939
Summary
Keywords
paramedic, fire fighter, police, first responder, PTSD, quality of life, functional impairment, alcohol
Citation
Meyer EC, Roth SG, Coe E, Taylor DJ and Gulliver SB (2025) Pilot outcomes and exploration of treatment mechanisms using a culturally adapted version of the unified protocol for transdiagnostic treatment of emotional disorders to improve mental health symptoms, alcohol misuse, functional outcomes, and sleep quality in emergency responders. Front. Health Serv. 5:1452976. doi: 10.3389/frhs.2025.1452976
Received
21 June 2024
Accepted
28 May 2025
Published
16 June 2025
Volume
5 - 2025
Edited by
Shay-Lee Bolton, University of Manitoba, Canada
Reviewed by
Deborah Beidel, University of Central Florida, United States
Jacqueline Pistorello, University of Nevada, United States
Updates
Copyright
© 2025 Meyer, Roth, Coe, Taylor and Gulliver.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Eric C. Meyer ecm77@pitt.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.