- 1Department of Health Policy Management, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
- 2IAE de Paris-Sorbonne Business School, University Paris 1 Pantheon Sorbonne, Paris, France
- 3Physician Group Department, Chinese Non-government Medical Institutions Association, Guangzhou, China
- 4Department of Critical Care Medicine, The First Medical Center of Chinese People’s Liberation Army General Hospital, Beijing, China
- 5Young and Middle-Aged Physicians Department, China Information Association of Traditional Chinese Medicine, Beijing, China
Background: The physician group (PG) model, while well-established in the United States, is a relatively recent healthcare delivery innovation in China. Despite rapid growth in PG registrations, comprehensive understanding of physicians’ perspectives remains limited.
Objective: To investigate Chinese physicians’ perspectives and concerns regarding the PG model and identify factors influencing their support for its implementation.
Methods: A cross-sectional online survey was conducted among 535 Chinese physicians between October-November 2024. The survey assessed participants’ views on PG advantages, concerns, and overall support. Data analysis included descriptive statistics and variance analyses to explore correlations between physicians’ characteristics and their perspectives.
Results: Key facilitators for PG development included “New career direction outside the existing system” (75.1%) and “Improved income levels” (74.4%). Major concerns comprised “Policies restricting physician mobility” (69.7%) and “Lack of support from hospital managers” (57.8%). Overall support for PGs was moderate (3.710 ± 1.241). Administrative position holders showed significantly higher support than non-administrative staff (p = 0.004), and longer work experience correlated positively with support (p = 0.037). Hospital level and specialty area showed no significant influence on support levels.
Conclusion: This first systematic study of Chinese physicians’ perspectives on PGs reveals moderate support driven by career development and income opportunities, while highlighting regulatory and institutional barriers. Results suggest the need for stable policies, enhanced income frameworks, and targeted support for early career physicians-who currently show less support than experienced physicians-to facilitate successful PG implementation in China.
1 Introduction
A physician group is a collective of healthcare professionals collaborating within a common practice, sharing resources to deliver patient care. This model, originating at the Mayo Clinic over a century ago (1), was officially introduced in China in 2014, with more than 1,000 groups registered by 2019 (2). Although the COVID-19 pandemic temporarily hindered growth, physician groups have since resumed activity in the post-pandemic period.
The national policy guideline “Healthy China 2030,” published in 2016, marked the first official mention of the physician group model in a national document, encouraging the exploration of this approach (3). Recent policies have increasingly supported physician mobility and independent practice. These include the implementation of tiered diagnosis systems and medical alliances that facilitate resource sharing between physician groups and hospitals, promoting the distribution of quality healthcare resources across different regions (4). Additionally, digital platforms have enabled the development of “mobile physician groups,” reducing information asymmetry between doctors and patients while enhancing physician brand recognition (5).
Research on physician groups in the United States indicates that group practices enhance physician quality of life and job satisfaction by facilitating knowledge transfer among members and reducing professional isolation. Patients in these group practices typically benefit from improved quality of care, better access to services, and higher satisfaction compared to those in solo practices (1, 6). These advantages of the physician group model are crucial for addressing specific challenges within the Chinese healthcare system.
The purpose of this study is to explore the perspectives and concerns of Chinese physicians regarding the physician group model, as well as to identify the key factors influencing these concerns. By gathering insights directly from healthcare providers, the research aims to highlight the barriers and facilitators associated with the implementation of physician groups in China. Understanding these perspectives is essential for developing effective strategies that support the successful integration of this model into the Chinese healthcare system (7). Ultimately, the study seeks to contribute to the ongoing dialogue about healthcare reform in China and to provide actionable recommendations that can enhance physician collaboration, improve patient outcomes, and foster a more resilient healthcare infrastructure.
2 Methods
2.1 Study design
The questionnaire was developed through a comprehensive literature review, and subsequently revised and expanded based on feedback from a group of 16 experienced pilot physicians who are knowledgeable or experts in this field. Their valuable feedback helped to enhance the questionnaire's content and structure, ensuring its relevance and accuracy in exploring the subject matter.
The inclusion criteria for participating physicians were as follows: (1) currently practicing in China; (2) holding a professional title such as resident, attending physician, associate chief, or chief; (3) possessing experience working in a physician group practice or having a solid understanding of the physician group practice model; and (4) being able to communicate effectively in Mandarin or Cantonese. To ensure that the sample consisted solely of qualified individuals, the exclusion criteria eliminated medical students, nurses, technicians, and those with a medical background who are not currently practicing as physicians. This approach was designed to focus on individuals who could provide meaningful insights and perspectives regarding the physician group model within the Chinese healthcare system.
The survey was distributed using Wenjuan Star, a widely used online questionnaire tool in China, in combination with WeChat, a popular social media platform, to facilitate effective data collection. Conducted from October 31st to November 22nd, 2024. The survey reached a broad audience across China, supported by collaborations with the Chinese Non-government Medical Institutions Association and the China Information Association of Traditional Chinese Medicine. These supports were essential in ensuring the survey was disseminated widely, thereby enhancing the diversity and representativeness of the responses.
The questionnaire is structured into five distinct sections. The first section gathers demographic information, including professional titles, years of experience, and geographical location. The second section assesses respondents' knowledge through a series of yes-or-no questions. The third section further explores practical experiences by employing a similar yes-or-no format. The fourth section utilizes a 5-point Likert scale to evaluate attitudes, allowing participants to indicate their levels of agreement or disagreement with various statements. Finally, the fifth section comprises multiple-choice questions aimed at identifying the factors that facilitate or hinder the implementation of Physician Groups. This comprehensive structure facilitates a thorough collection of data on key aspects related to Physician Groups, encompassing demographics, knowledge, practice experiences, attitudes, and influential factors.
The primary aim of this study is to explore physicians' attitudes toward Physician Groups (PG) and analyze the influencing factors. To achieve this, the research focuses on demographic analysis and the examination of various factors that may affect these attitudes. Additionally, the study will highlight several crucial questions related to attitudes, contributing to a comprehensive understanding of how different elements interplay in shaping physicians' perceptions of PG.
2.2 Ethical considerations
This study was reviewed by the Institutional Review Board Office of Johns Hopkins Bloomberg School of Public Health on January 9th, 2024. The IRB Determination notice (FWA #00000287) stated that the proposed activity does not qualify as human subjects research, as defined by DHHS regulations 45 CFR 46.102, and therefore does not require IRB oversight. The study involved collecting information from individuals about matters unrelated to themselves, without disclosing personal opinions and without exposing respondents to employment or other risks. Additionally, the study ensured participant anonymity and confidentiality by using questionnaires that did not collect names or emails, thus preventing participant tracking. Informed consent was obtained through the questionnaire, and participation was voluntary. The entire study was conducted without any financial burden to the participants.
2.3 Data analysis
The data were analyzed using descriptive statistics to summarize the characteristics of the sample population. Facilitators and barriers associated with physicians' choices to join physician groups (PGs) were ranked based on the frequency of responses. A differential analysis was performed to evaluate attitudes towards PGs across various demographic profiles, including years of experience, education, hospital management roles, hospital level, specialty, and geographic location. A significance level of p < 0.05 was considered indicative of statistical differences. Statistical analyses were conducted using SPSS v24.0 software. Furthermore, we examined the correlation between demographic variables and physicians' attitudes, suggesting avenues for future research to explore additional factors influencing perceptions of PG Model.
3 Results
3.1 Demographic profile
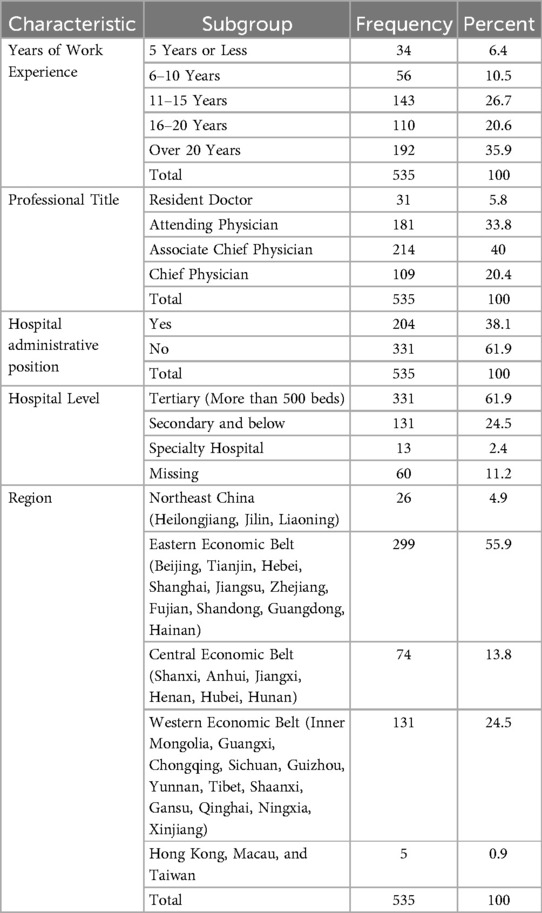
The study population consisted of 535 physicians affiliated with various medical institutions across China. In terms of education, the majority (46.4%) held a bachelor's degree or below, followed by master's degree holders (35.5%), and a smaller proportion (18.1%) possessing a doctorate or higher degree. The doctors' years of work experience ranged from less than five years to more than two decades, with a significant proportion (35.9%) having over 20 years of clinical practice. Their professional titles spanned from resident doctors (5.8%) to chief physicians (20.4%), with associate chief physicians (40%) being the most represented. Specializing in various medical fields, the majority (61.1%) were in surgery, followed by internal medicine (18.7%), traditional Chinese medicine (6.7%), and others (13.5%). Regarding hospital administrative positions, about two-thirds of the doctors did not hold administrative roles within their hospitals. In terms of hospital level, the study population was predominantly from tertiary hospitals with over 500 beds (61.9%), followed by secondary and specialty hospitals. The participants were also geographically diverse, with the eastern economic belt being the most represented (55.9%), followed by the central and western economic belts, as well as Hong Kong, Macau, and Taiwan (Table 1).
3.2 Facilitators of PG model
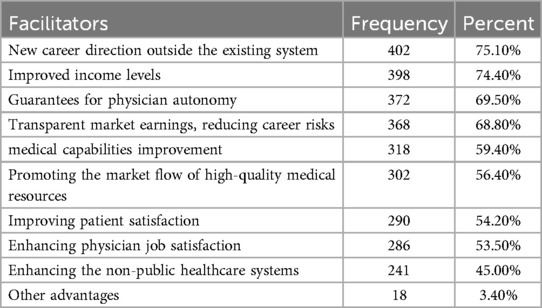
The analysis of facilitators for the development of physician groups (PGs) revealed several key drivers. The most frequently cited facilitator was the opportunity for a new career direction outside the existing system (75.1%), followed by improved income levels (74.4%) and guarantees for physician autonomy (69.5%). Transparent market earnings, reducing career risks (68.8%), and medical capabilities improvement (59.4%) were also prominent factors. Additionally, promoting the market flow of high-quality medical resources (56.4%) and improving patient satisfaction (54.2%) were highlighted. Enhancing physician job satisfaction (53.5%) and strengthening non-public healthcare systems (45.0%) were noted as further advantages (Table 2).
Supplementary analyses were conducted to discern potential variations in the top 3 facilitators based on physicians’ demographic and professional characteristics. Factors such as education, years of work experience, professional title, specialty, administrative roles, and hospital level were evaluated to assess their influence on the perceived significance of these facilitators. These refined analyses aimed to uncover distinct patterns and subgroup differences, facilitating a deeper understanding of how diverse physician profiles align with the development of PGs (Table 3).
3.2.1 New career direction outside the existing system (75.1%)
A new career direction was the most frequently cited facilitator, with 75.1% of respondents identifying this advantage. Although there were no significant differences in responses based on education (p = 0.312), years of work experience (p = 0.668), or other major factors (Table 3), several trends emerge:
Chief physicians (81.7%) rated this facilitator higher compared to attending physicians (71.3%) and associate chief physicians (74.3%). This may suggest that physicians at the pinnacle of their professional journey increasingly seek alternatives to traditional institutional roles.
Surgeons were more likely to emphasize career opportunities (77.1%) compared to internal medicine doctors (72%). This difference, while not statistically significant (p = 0.299), may reflect a higher alignment of surgical fields with entrepreneurial or independent practice opportunities often presented in physician groups (PGs).
Importantly, tertiary hospital physicians, who are typically affiliated with large institutions (78.2%), also saw PGs as a means to step outside the limitations of these systems, compared to those in secondary hospitals (69.5%, p = 0.122). This highlights PGs' potential as a response to the rigidity of traditional practice models, offering flexibility and diversification.
These findings suggest that fostering messaging around “career transformation” and emphasizing independence in marketing or policy campaigns could resonate strongly with certain physician subgroups, especially senior physicians or those engaged in high-demand specialties like surgery.
3.2.2 Improved income levels (74.4%)
Income improvement was the second most popular facilitator, significantly influenced by various demographic factors:
Physicians with 6–10 years of work experience rated this factor highest, with 83.9% selecting it as a facilitator (p = 0.023). In contrast, older physicians (over 20 years of experience) showed lower support (68.2%). Younger and mid-career doctors may view PGs as a means to address financial inequalities earlier in their careers compared to their senior colleagues, who are closer to retirement and may prioritize other factors like stability.
Physicians in tertiary hospitals were significantly more likely to view income improvement as a key facilitator (78.5%) compared to those in secondary hospitals (67.9%, p = 0.042). This reflects the restrictive salary structures of public hospitals, where tertiary-level institutions often impose tighter financial frameworks despite demanding workloads.
Interestingly, the professional title variable showed borderline significance (p = 0.050), with chief physicians (78.9%) and attending physicians (76.2%) slightly more likely to emphasize this factor compared to resident doctors (54.8%). This indicates that targeting salary disparities and creating incentive-based payment frameworks could be an effective strategy for PG implementation. Policies allowing transparent revenue-sharing systems and market-driven earnings may attract wider support from younger and mid-career physicians, particularly in tertiary hospitals.
3.2.3 Guarantees for physician autonomy (69.5%)
Guaranteeing physician autonomy was the third most prominent facilitator, viewed as critical across different demographics. While no statistically significant differences emerged across key factors, several notable trends highlight the importance of autonomy in driving PG adoption:
Chief physicians (73.4%) and associate chief physicians (72.9%) were more inclined to rate autonomy as critical, compared to attending physicians (64.1%). This aligns with the higher expectation among experienced physicians to exercise greater decision-making power over clinical and administrative processes.
Physicians in tertiary hospitals (72.2%) rated autonomy higher than those in secondary hospitals (65.6%); meanwhile, differences across specialties suggested a similar trend, with internal medicine physicians rating it lower (60%) compared to surgeons (72.2%) and practitioners of Traditional Chinese Medicine (66.7%). This suggests that physicians in niche or procedural specialties may perceive more constraints in the current healthcare system compared to others.
3.3 Barriers about PG model
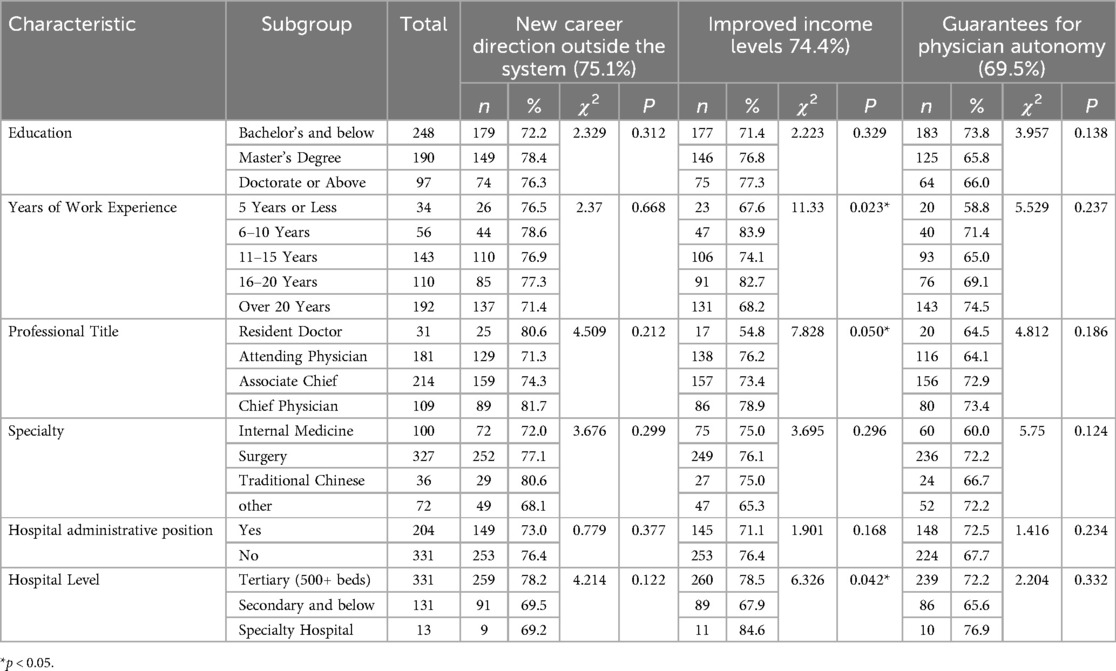
The analysis of barriers to the development of physician groups (PGs) revealed several critical challenges cited by respondents. The most frequently reported barrier was policies restricting physician mobility, identified by 69.7% of participants, reflecting substantial concerns about regulatory constraints within the current healthcare system. This was followed by the lack of support from hospital managers (57.8%) and unstable and unsustainable income (57.2%), both of which highlight organizational and financial difficulties faced by physicians considering the transition to PGs. Additionally, over half of the respondents identified challenges such as limited career development opportunities (53.8%) and insufficient academic resources (53.6%), demonstrating dissatisfaction with institutional barriers hindering professional growth and access to knowledge. Structural and operational obstacles, including a lack of a clear and sustainable business model (50.8%) and limited brand value to attract patients (41.3%), were also noted. Other notable concerns included the shortage of hospitals providing qualified supporting services (40.0%) and limited support from health insurance (39.6%), both of which reflect systemic deficiencies in infrastructure and financial backing. Finally, approximately one-third of respondents highlighted insufficient business operation capabilities (34.2%) as a significant barrier, while only 2.6% selected “Other Challenges,” indicating the primary concerns were well represented (Table 4).
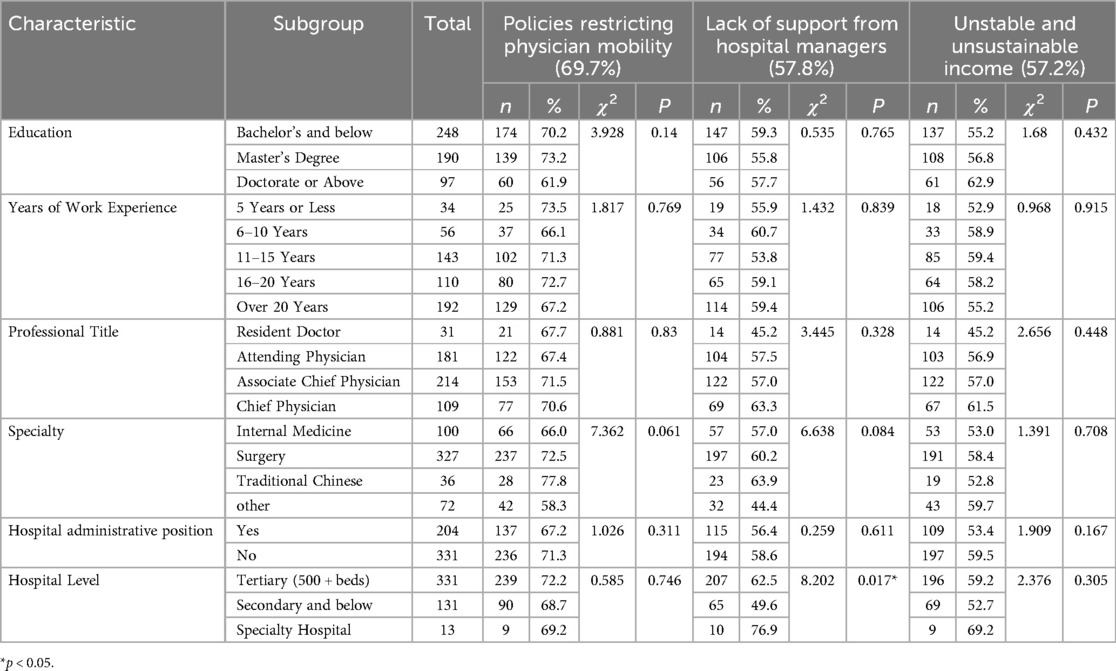
Supplementary analyses were performed to explore potential variations in the top barriers—policies restricting physician mobility, lack of support from hospital managers, and unstable and unsustainable income—based on physicians' demographic and professional characteristics (Table 5).
3.3.1 Policies restricting physician mobility (69.7%)
“Policies restricting physician mobility” was the most frequently cited barrier, chosen by 69.7% of respondents. This reflects a widespread concern regarding the regulatory constraints that limit physicians' ability to transition between institutions or participate in physician groups (PGs). While the chi-square analysis reveals no statistically significant differences across most demographic and professional variables, some trends are noteworthy:
Respondents with a master's degree were slightly more likely to identify this barrier (73.2%) compared to those with a bachelor's or below (70.2%) and those with a doctorate or above (61.9%, p = 0.14). Physicians specializing in Traditional Chinese Medicine (TCM) reported the highest proportion (77.8%) identifying physician mobility restrictions as a barrier, followed by surgical specialists (72.5%) and internal medicine practitioners (66.0%, p = 0.061). The relatively higher percentages in TCM and surgery may suggest these professionals desire greater flexibility for collaborative opportunities or practice expansion.
3.3.2 Lack of support from hospital managers (57.8%)
The second most frequently cited challenge was “lack of support from hospital managers,” chosen by 57.8% of respondents. Unlike the first barrier, this factor showed a statistically significant relationship with hospital level (p = 0.017). Physicians working in tertiary hospitals with over 500 beds were significantly more likely to cite this barrier (62.5%) than those in secondary and below hospitals (49.6%), with a very high proportion seen in specialty hospitals (76.9%). Tertiary hospitals tend to have more rigid hierarchies and managerial systems, which may hinder the flexibility needed for PG participation. While not statistically significant (p = 0.084), TCM practitioners (63.9%) and surgical specialists (60.2%) were slightly more likely than internal medicine specialists (57.0%) and those in “other” specialties (44.4%) to perceive managerial resistance.
3.3.3 Unstable and unsustainable income (57.2%)
The third most frequently noted barrier was “unstable and unsustainable income,” identified by 57.2% of respondents. While this challenge did not present statistically significant differences across most demographics. Interestingly, respondents with a doctorate or higher were more likely to report this barrier (62.9%) than their counterparts with a master's degree (56.8%) or a bachelor's degree or below (55.2%, p = 0.432). This suggests that physicians with higher educational qualifications may experience heightened expectations for financial reliability that are unmet in the PG model. Chief physicians (61.5%) and associate chief physicians (57.0%) expressed greater concerns about income instability compared to attending (56.9%) and resident doctors (45.2%, p = 0.448).
3.4 Physicians' perception on “I support PG to develop in China”
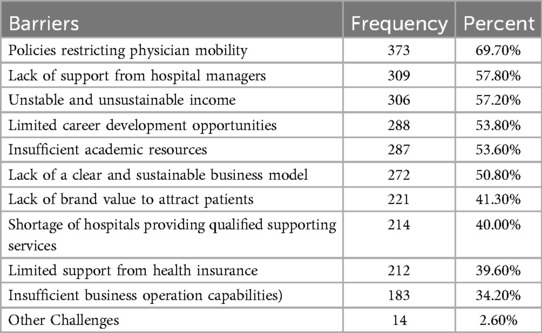
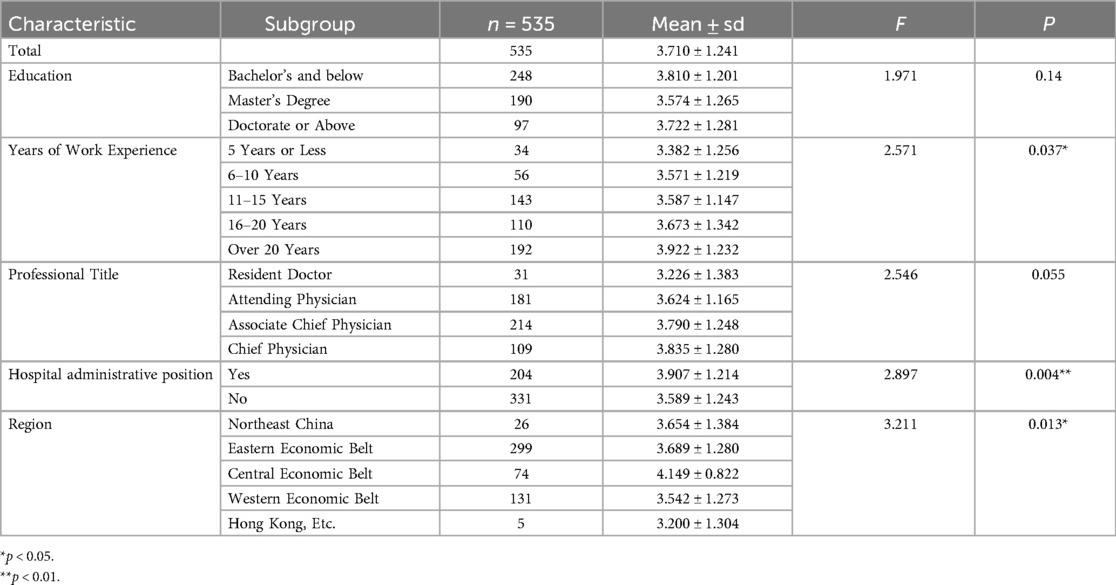
The overall support for the development of physician groups (PGs) in China was positive, with a mean score of 3.710 ± 1.241 among all respondents (n = 535), where a score of 3 indicates neutrality. Further analysis revealed significant variations across several demographic and professional characteristics (Table 6).
Years of Work Experience showed a significant relationship with support levels (F = 2.571, p = 0.037). Notably, physicians with over 20 years of experience demonstrated the strongest support (3.922 ± 1.232), while those with 5 years or less experience showed the lowest support (3.382 ± 1.256). This suggests that more experienced physicians may better recognize the potential benefits of PGs based on their extensive clinical experience.
Hospital Administrative Position emerged as another significant factor (F = 2.897, p = 0.004). Physicians holding administrative positions showed significantly higher support (3.907 ± 1.214) compared to those without administrative roles (3.589 ± 1.243), indicating that healthcare leaders may better understand the strategic value of PGs in addressing systemic challenges.
Regional differences were also significant (F = 3.211, p = 0.013), with physicians in the Central Economic Belt showing the strongest support (4.149 ± 0.822), notably higher than their counterparts in other regions, particularly the Western Economic Belt (3.542 ± 1.273) and Hong Kong, Macau, and Taiwan (3.200 ± 1.304).
While not statistically significant, there were observable trends across other variables. Professional titles showed a marginal effect (F = 2.546, p = 0.055), with chief physicians (3.835 ± 1.280) and associate chief physicians (3.790 ± 1.248) expressing stronger support compared to resident doctors (3.226 ± 1.383). Similarly, specialty hospitals demonstrated the highest mean support (4.077 ± 1.320) among hospital levels, though this difference was not statistically significant (F = 0.972, p = 0.379).
4 Discussion
4.1 Key findings
4.1.1 Overall support with demographic variations
The study shows that Chinese physicians exhibit a generally positive attitude toward the development of physician groups (PGs), with an average support score of 3.710 ± 1.241. This highlights the openness of medical professionals to adopt innovative care models to address systemic issues in China's healthcare system (8, 9) (e.g., uneven resource distribution, lack of autonomy). Previous studies support the conclusion that healthcare restructuring efforts like PGs often receive strong backing from medical professionals willing to improve efficiency and patient outcomes (10). This positive attitude is essential for advancing policy frameworks around PG adoption in China.
Physicians with over 20 years of experience expressed remarkable support (3.922 ± 1.232, p = 0.037), aligning with findings that experience shapes confidence in independent models like PGs. Senior physicians likely recognize the inefficiencies of traditional hospital systems and value PGs' potential to enhance autonomy and income (11). Additionally, physicians in administrative roles demonstrated significantly higher support (3.907 ± 1.214, p = 0.004), as they are more familiar with organizational decision-making and the potential operational efficiencies of PGs (12, 13). This indicates that institutional leaders could act as advocates for PG implementation.
Regional differences highlight a higher readiness for PG adoption in the Central Economic Belt, which showed the strongest support (4.149 ± 0.822, p = 0.013). These regions often experience a unique balance of resource availability, greater medical competition, and economic advancements, contributing to stronger acceptance of innovative models. In contrast, lower support in the Western Economic Belt (3.542 ± 1.273) correlates with systemic resource and infrastructure limitations. Tailored strategies recognizing these regional disparities should direct implementation efforts toward regions with higher readiness, while addressing barriers in under-resourced areas (14, 15).
4.1.2 Career development and financial incentives as primary facilitators
The opportunity for new career directions emerged as the most cited facilitator (75.1%), highlighting physicians' growing desire for alternatives to traditional institutional roles. Many physicians, especially senior specialists, view physician groups (PGs) as a solution to rigid institutional hierarchies and limited professional growth opportunities. This finding is consistent with the Diffusion of Innovations theory, which posits that adoption of new organizational models such as PGs is influenced by perceived advantages—including autonomy and professional advancement—over existing systems. This aligns with broader global trends, where healthcare professionals increasingly prioritize entrepreneurial ventures and independent practice models for career satisfaction (1, 16). By enabling greater flexibility, PGs offer physicians a platform to redefine their professional track while meeting the evolving demands of healthcare services.
Improved income levels (74.4%) were identified as the second most important facilitator, indicating strong financial expectations from joining PGs. Physicians in mid-career stages (6–10 years) and those in tertiary hospitals, who often experience restrictive salary structures, were particularly motivated by income improvement. Transparent revenue-sharing systems and opportunities for market-driven earnings make PGs attractive for physicians seeking to bridge wage disparities. These financial incentives represent a critical driver, especially for healthcare providers who are overburdened yet undercompensated within traditional employment frameworks (17, 18).
4.1.3 Systemic and institutional barriers
Policy restrictions on physician mobility emerged as the most significant barrier, with 69.7% of participants identifying this issue. Regulatory constraints hinder physicians from transitioning between institutions or joining physician groups (PGs), limiting opportunities for professional growth or alternative employment. Simplifying inter-institutional approval system and promoting multi-site licensing could help alleviate this challenge and enable greater mobility within the healthcare system (8, 19).
Lacking institutional support from hospital managers was reported by 57.8% of respondents, with the issue being more acute in tertiary hospitals (62.5%, p = 0.017). Large, hierarchical institutions often display resistance to external frameworks like PGs, as managers prioritize maintaining control over talent networks. Addressing these barriers requires targeted engagement with hospital leaders, promoting options like co-management models that align PG goals with institutional objectives (20–22).
Concerns about unstable and unsustainable income were highlighted by 57.2% of participants. Notably, this issue was more prominent among highly educated physicians (e.g., those with doctoral degrees, 62.9%). Higher expectations for financial security, derived from their advanced qualifications, may explain greater sensitivity to income risks compared with less educated peers. Transparent revenue-sharing mechanisms and government-backed financial incentives for PG participants could address these concerns while ensuring economic stability (23). Furthermore, tailoring financial structures for PGs to meet the needs of senior and highly educated physicians could enhance engagement (24, 25).
4.2 Implications and suggestions
4.2.1 Policy reform priorities
Policy reform to enhance physician mobility is critical for the successful development of PGs. Current regulatory constraints limit physicians' ability to explore opportunities outside traditional systems. To address this, comprehensive reforms should introduce flexible mobility structures that facilitate inter-institutional transitions (26). For example, designing transferable contracts or creating inter-regional licensing systems can enable physicians to engage in collaborative, multi-site practices without bureaucratic hurdles (27). Enhanced flexibility will ensure optimal utilization of medical expertise across regions while reducing professional waste (28–30).
International experience, particularly from the United States, offers valuable insights. In the US, physicians often hold state-specific licenses, but mechanisms such as the Interstate Medical Licensure Compact (IMLC) have been developed to facilitate multi-state practice and physician mobility (31). This compact allows eligible physicians to obtain expedited licensure in multiple participating states, thereby reducing administrative barriers and enabling greater workforce flexibility—especially important for large physician groups and telemedicine practices (32, 33). Similarly, models from other low- and middle-income countries (LMICs), such as India's Apollo Group, demonstrate how adaptable policy environments and innovative contracting can support the growth of physician groups despite resource constraints (34). Comparisons with these international models highlight both the potential and the challenges of implementing cross-regional practice frameworks in China's unique healthcare context.
Clear legal protections for physicians participating in PGs are paramount to overcome risks associated with independent practice. Without robust legal frameworks, physicians face uncertainties regarding income stability, liability, and intellectual property. Policymakers should establish legal safeguards addressing these issues to create a supportive ecosystem for PG members.
Reforms must be tailored to address regional disparities in healthcare infrastructure and willingness to adopt PGs. For example, to advance physician group (PG) integration and operational effectiveness, pilot programs for multi-site licensing reforms can be initiated in regions such as the Central Economic Belt, which already demonstrates an active physician group landscape and physician mobility. These pilots would test streamlined licensing processes that allow qualified physicians to practice across multiple institutions and regions, reducing administrative barriers and broadening access to high-quality clinical expertise. Conversely, less prepared areas such as the Western Economic Belt may need capacity-building initiatives to strengthen institutional cooperation before implementing large-scale reforms. These targeted approaches can bridge gaps, ensuring equitable development and expanding healthcare access nationwide (35).
4.2.2 Institutional support mechanisms
To foster the integration of Physician Groups (PGs) into the broader healthcare ecosystem, it is crucial to establish collaborative models between PGs and hospitals. Many hospitals, particularly tertiary institutions, demonstrate resistance to PGs due to the perceived threat of losing skilled medical professionals. Addressing this requires co-management models that align the objectives of both parties. For example, hospitals can collaborate with PGs through shared service platforms, resource pooling, and coordinated patient care pathways. Such collaborations improve patient outcomes while reducing inter-institutional conflicts, paving the way for successful PG adoption (36, 37).
Transparent revenue-sharing systems are essential for encouraging physician participation in PGs and lightening financial concerns. A fair and standardized revenue-sharing framework can provide clarity on how profits are distributed among participating physicians and affiliated hospitals. These systems should also ensure that financial incentives align with performance metrics, fostering a culture of accountability and trust while improving physician satisfaction and operational sustainability (38, 39).
Creating structured professional development pathways within PGs can further enhance their appeal. Physicians often identify limited career growth opportunities in traditional hospital systems. As such, PGs should offer tailored career trajectories, including specialized training programs, leadership development courses, and research initiatives (40). By fostering an environment that prioritizes educational advancement and skill-building, PGs can attract top-tier talent and empower their members to achieve long-term professional success (41, 42). These development pathways could also address regional and institutional disparities by nurturing more skilled physicians in underserved areas.
4.3 Limitations
This study has several limitations that deserve attention. First, the sample distribution reveals notable regional imbalances, with overrepresentation from the Eastern and Central Economic Belts, and disproportionate representation from certain areas such as the Central Economic Belt. These disparities may limit the generalizability of the findings to all regions of China. While we did not apply statistical weighting to adjust for these differences, we explicitly acknowledge this as a limitation and recommend the use of stratified or weighted sampling designs in future research to improve representativeness.
Second, our reliance on self-reported data introduces potential bias, as respondents may overstate or misrepresent their knowledge, attitudes, or practices regarding physician group (PG) development. The anonymous, voluntary nature of the survey may have resulted in nonresponse bias, with individuals more interested in or supportive of PGs being more likely to participate. This could further skew the results and limit their applicability to the broader population of healthcare professionals.
Third, the cross-sectional design of the study restricts our ability to draw causal inferences about the factors influencing support for PGs. Longitudinal research would be beneficial to track changes in knowledge, attitudes, and practices over time.
Finally, our analysis was limited to descriptive statistics, as sample constraints precluded multivariate regression. Consequently, we could not fully assess the influence of potential confounders such as hospital funding models, regional GDP, and institutional policy variations. These unmeasured factors may have impacted our results. We recommend that future studies use multivariate analyses and more comprehensive data collection to better clarify the interplay of institutional, economic, and regional variables, as well as to enhance generalizability through more balanced samples and longitudinal approaches.
5 Conclusion
The findings highlight the widespread support among Chinese physicians for the development of PGs, with senior practitioners and those in administrative roles exhibiting the strongest advocacy. Facilitators such as career development, financial incentives, and autonomy emerge as key motivators, while barriers including restrictive mobility policies and income stability concerns underscore systemic challenges. To succeed, PGs need policy reforms enabling flexibility, institutional support through collaborative models, and tailored financial and professional growth systems. Addressing these challenges holistically can maximize the potential of PGs, enabling them to transform healthcare delivery and improve patient outcomes throughout China.
Institutional review board statement
This study was reviewed by the Institutional Review Board Office of Johns Hopkins Bloomberg School of Public Health on January 9th, 2024. The IRB Determination notice (FWA #00000287) stated that the proposed activity does not qualify as human subjects research, as defined by DHHS regulations 45 CFR 46.102, and therefore does not require IRB oversight.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study of human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants OR patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
RF: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. QM: Investigation, Project administration, Resources, Writing – review & editing. LZ: Investigation, Resources, Writing – review & editing. CL: Investigation, Methodology, Resources, Writing – review & editing. LH: Investigation, Resources, Writing – review & editing. ML: Investigation, Resources, Writing – review & editing. LS: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors thank the Chinese Non-government Medical Institutions Association and the China Information Association of Traditional Chinese Medicine for helping to publish the survey questionnaire.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tan B, Kash D. Physician group practice trends: a comprehensive review. J Hosp Med Manage. (2016) 2(1):1–7. doi: 10.4172/2471-9781.100008
2. Zhang S, Guo J. Physician Group development status. Chin Physician Group Dev Rep. (2021) 2021:1–8.
4. Xu L, Zhang M. Regulated multi-sited practice for physicians in China: incentives and barriers. Global Health J. (2018) 2(1):14–31. doi: 10.1016/S2414-6447(19)30117-4
5. Pan Z, Linqi X, Yun T, Weiqi W, Yong H. Analysis and thought of the development path of medical group in China. Chin J Hosp Manage. (2021) 41(12):5.
6. Zwiep T, Ahn S, Brehaut J, Balaa F, McIsaac DI, Rich S, et al. Group practice impacts on patients, physicians and healthcare systems: a scoping review. BMJ Open. (2021) 11(1):e041579. doi: 10.1136/bmjopen-2020-041579
7. Lin J, Zhou J, Wang L. Health care reform in China from the perspective of physicians. Biosci Trends. (2020) 14(2):151–5. doi: 10.5582/bst.2020.01015
8. Chen C, Liu M. Achievements and challenges of the healthcare system in China. Cureus. (2023) 15(5):e39030. doi: 10.7759/cureus.39030
9. Zheng L, Zhang L, Chen K, He Q. Unmasking unexpected health care inequalities in China using urban big data: service-rich and service-poor communities. PLoS One. (2022) 17(2):e0263577. doi: 10.1371/journal.pone.0263577
10. Federman AD, Woodward M, Keyhani S. Physicians’ opinions about reforming reimbursement. Arch Intern Med. (2010) 170(19):1735–42. doi: 10.1001/archinternmed.2010.369
11. Zhang X, Shen KN, Xu B. Double-edged sword of knowledge inertia: overcoming healthcare professionals’ resistance in innovation adoption. Technovation. (2024) 133:103011. doi: 10.1016/j.technovation.2024.103011
12. Singh PK, Kumari V, Tiwari M. Navigating healthcare leadership: theories, challenges, and practical insights for the future. J Postgrad Med. (2024) 70(4):232–41. doi: 10.4103/jpgm.jpgm_533_24
13. Nilsen P, Seing I, Ericsson C, Birken SA, Schildmeijer K. Characteristics of successful changes in health care organizations: an interview study with physicians, registered nurses and assistant nurses. BMC Health Serv Res. (2020) 20(1):147. doi: 10.1186/s12913-020-4999-8
14. Yuan L, Cao J, Wang D, Yu D, Liu G, Qian Z. Regional disparities and influencing factors of high quality medical resources distribution in China. Int J Equity Health. (2023) 22(1):8. doi: 10.1186/s12939-023-01825-6
15. Liu W, Liu Y, Twum P, Li S. National equity of health resource allocation in China: data from 2009 to 2013. Int J Equity Health. (2016) 15(1):68. doi: 10.1186/s12939-016-0357-1
16. Rao S, Ferris TG, Hidrue MK, Lehrhoff SR, Lenz S, Heffernan J, et al. Physician burnout, engagement and career satisfaction in a large academic medical practice. Clin Med Res. (2020) 18(1):3–10. doi: 10.3121/cmr.2019.1516
17. Auer EM, Behrend TS, Collmus AB, Landers RN, Miles AF. Pay for performance, satisfaction and retention in longitudinal crowdsourced research. PLoS One. (2021) 16(1):e0245460. doi: 10.1371/journal.pone.0245460
18. Seathu Raman SS, McDonnell A, Beck M. Hospital doctor turnover and retention: a systematic review and new research pathway. J Health Organ Manag. (2024) 38(9):45–71. doi: 10.1108/JHOM-04-2023-0129
19. Concha-Amin M, Trindade CS, Zen PRG, Giergowicz BB. Supply and demand in the physician workforce: an integrative review. Rev Bras Med Trab. (2024) 22(2):01. doi: 10.47626/1679-4435-2022-1022
20. Kozlowska O, Lumb A, Tan GD, Rea R. Barriers and facilitators to integrating primary and specialist healthcare in the United Kingdom: a narrative literature review. Future Healthcare J. (2018) 5(1):64–80. doi: 10.7861/futurehosp.5-1-64
21. Moreno-Domínguez M-J, Escobar-Rodríguez T, Pelayo-Díaz Y-M, Tovar-García I. Organizational culture and leadership style in Spanish hospitals: effects on knowledge management and efficiency. Heliyon. (2024) 10(20):e39216. doi: 10.1016/j.heliyon.2024.e39216
22. Karamat J, Shurong T, Ahmad N, Afridi S, Khan S, Khan N. Developing sustainable healthcare systems in developing countries: examining the role of barriers, enablers and drivers on knowledge management adoption. Sustainability. (2019) 11(4):954. doi: 10.3390/su11040954
23. Roberts WC. The importance of acquiring financial security for physicians. Am J Med. (2020) 133(12):1403–5. doi: 10.1016/j.amjmed.2020.06.019
24. Eltorai AEM, Eltorai AS, Fuentes C, Durand WM, Daniels AH, Ali S. Financial implications of physician specialty choice. R I Med J. (2018) 101(8):50–5.
25. Rosenthal MP, Diamond JJ, Rabinowitz HK, Bauer LC, Jones RL, Kearl GW, et al. Influence of income, hours worked, and loan repayment on medical students’ decision to pursue a primary care career. JAMA: J Am Med Assoc. (1994) 271(12):914–7. doi: 10.1001/jama.1994.03510360040033
26. Xierali IM. Physician multisite practicing: impact on access to care. J Am Board Fam Med. (2018) 31(2):260–9. doi: 10.3122/jabfm.2018.02.170287
27. Xiao Y, Wu X-H, Chen J, Xie F-F. Challenges in establishing a graded diagnosis and treatment system in China. Fam Pract. (2022) 39(1):214–6. doi: 10.1093/fampra/cmab089
28. Guo J, Kilby AE, Marks MS. The impact of scope-of-practice restrictions on access to medical care. J Health Econ. (2024) 94:102844. doi: 10.1016/j.jhealeco.2023.102844
29. Markowitz S, Adams EK, Lewitt MJ, Dunlop AL. Competitive effects of scope of practice restrictions: public health or public harm? J Health Econ. (2017) 55:201–18. doi: 10.1016/j.jhealeco.2017.07.004
30. Silver JK, Bean AC, Slocum C, Poorman JA, Tenforde A, Blauwet CA, et al. Physician workforce disparities and patient care: a narrative review. Health Equity. (2019) 3(1):360–77. doi: 10.1089/heq.2019.0040
31. Adashi EY, Cohen IG, McCormick WL. The interstate medical licensure compact. JAMA: J Am Med Assoc. (2021) 325(16):1607–8. doi: 10.1001/jama.2021.1085
32. Pariser DM. Building a group practice and going big. Dermatol Clin. (2023) 41(4):635–41. doi: 10.1016/j.det.2023.05.002
33. Nunes FC, Sousa JM, Pinho ES, Caixeta CC, Barbosa MA, Costa AP. Driving and restrictive factors of group practice in community psychosocial care services. Cien Saude Colet. (2022) 27(1):183–92. doi: 10.1590/1413-81232022271.19992021
34. Rao KD, Shahrawat R, Bhatnagar A. Composition and distribution of the health workforce in India: estimates based on data from the national sample survey. WHO South East Asia J Public Health. (2016) 5(2):133–40. doi: 10.4103/2224-3151.206250
35. Berenson J, Li Y, Lynch J, Pagán JA. Identifying policy levers and opportunities for action across states to achieve health equity. Health Aff. (2017) 36(6):1048–56. doi: 10.1377/hlthaff.2017.0004
36. Goes JB, Zhan C. The effects of hospital-physician integration strategies on hospital financial performance. Health Serv Res. (1995) 30(4):507–30.7591779
37. Duberman T, Hemker B, Solomon L. Innovative strategies for physician partnerships. One health system shares the steps it took to strengthen physician engagement. Healthc Exec. (2015) 30(3):84–6.26742349
38. Doerr T, Olsen L, Zimmerman D. The collaborative payer provider model enhances primary care, producing triple aim plus one outcomes: a cohort study. Healthcare (Basel). (2017) 5(3):84–6.29099742
39. Schnackenberg A, Tomlinson E. Organizational transparency: a new perspective on managing trust in organization-stakeholder relationships. J Manage. (2014) 42:1–35. doi: 10.1177/0149206314525202
40. Parsons M, Caldwell M, Alvarez A, Davenport D, Gallegos M, Landry A. Physician pipeline and pathway programs: an evidence-based guide to best practices for diversity, equity, and inclusion from the council of residency directors in emergency medicine. West J Emerg Med. (2022) 23(4):514–24. doi: 10.5811/westjem.2022.2.54875
41. Smith SG, Nsiah-Kumi PA, Jones PR, Pamies RJ. Pipeline programs in the health professions, part 1: preserving diversity and reducing health disparities. J Natl Med Assoc. (2009) 101(9):836–40, 845–51. doi: 10.1016/s0027-9684(15)31030-0
Keywords: physician group practice, healthcare reform, health policy, Chinese healthcare system, medical workforce management
Citation: Fan R, Meng Q, Zhang L, Liu C, Han L, Liu M and Shi L (2025) Physician group practice in China's healthcare reform: a national survey on physicians' perspectives and implementation challenges. Front. Health Serv. 5:1574388. doi: 10.3389/frhs.2025.1574388
Received: 11 February 2025; Accepted: 16 June 2025;
Published: 30 June 2025.
Edited by:
Liaqat Ali Khan, Ministry of Health, Saudi ArabiaReviewed by:
Yu Xiao, Chengdu No. 4 People’s Hospital, ChinaOthman M. Gatar, Universiti Putra Malaysia, Malaysia
Copyright: © 2025 Fan, Meng, Zhang, Liu, Han, Liu and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leiyu Shi, bHNoaTJAamh1LmVkdQ==
 Rui Fan
Rui Fan Qing Meng2
Qing Meng2 Chao Liu
Chao Liu Leiyu Shi
Leiyu Shi