Abstract
Background:
The National Accreditation Board for Hospitals and Healthcare Providers (NABH.) accreditation process aims to elevate the quality of healthcare services through an impartial, external peer evaluation of an organization's performance. This study compares NABH. quality indicators in a tertiary care hospital before and after accreditation, assessing changes in patient care, hospital management, and staff performance.
Methods:
A systematic review was conducted following PRISMA guidelines. Literature was searched across PubMed, Scopus, Google Scholar, and the Cochrane Library from August 2023 to January 2024. Keywords included “NABH. accreditation and hospital quality,” “Accreditation in Indian hospitals and patient safety,” and “Tertiary care hospital before and after accreditation.” Boolean operators, synonyms, and related terms were used to ensure comprehensive retrieval. Independent reviewers screened studies, and risk of bias assessment was performed using the Cochrane Risk of Bias Tool.
Results:
The study highlights significant improvements in hospital quality indicators following NABH accreditation. Hospital-acquired infection rates decreased, with infection control compliance improving by 40%. Operational efficiency improved with a 20% reduction in discharge delays and a 15% increase in documentation accuracy. Patient satisfaction scores rose by 25%, and structured policies enhanced service quality by 30%. Additionally, 85% of hospital staff reported higher job satisfaction. Statistical analysis confirmed significant differences in compliance rates (p < 0.05) and patient care metrics (p < 0.01). Despite initial implementation challenges due to resource constraints, the study underscores the need for continuous monitoring and reinforcement of accreditation standards to sustain these improvements.
Conclusion:
NABH accreditation improves patient safety, lowers infection rates, and boosts overall productivity. The structured framework encourages continuous improvement, but institutional commitment and ongoing oversight are necessary for long-term sustainability.
Introduction
Quality in healthcare defined as the degree to which health services increase the likelihood of desired health outcomes and are consistent with current professional knowledge. Globally, health systems have increasingly adopted quality improvement initiatives to achieve measurable enhancements in clinical care and patient satisfaction.
In order to provide high-quality healthcare services in India, hospitals must be accredited by the National Accreditation Board for Hospitals and Healthcare Providers (NABH.). The thorough and exacting process of NABH. accreditation is intended to guarantee that healthcare institutions adhere to set criteria for patient care, safety, and organizational management. NABH. aligns its standards with international best practices, particularly those of the International Society for Quality in Healthcare (ISQua), as a constituent board of the Quality Council of India (Q.C.I.) (1). A healthcare institution must undergo frequent evaluations in order to receive NABH. accreditation, which encourages advancements in the operational and structural areas of healthcare delivery (2).
To ensure that hospitals meet and continuously strive to exceed predefined benchmarks in important areas like patient safety, clinical care, infection control, and patient rights, the accreditation process entails an external evaluation by a qualified team of healthcare professionals who look at the organization's policies, procedures, and outcomes (3). The evaluation includes a self-assessment by the hospital, followed by an on-site survey where the external team reviews hospital operations and interacts with staff and patients. A report is then compiled that may include recommendations for improvement, and the hospital's status is then decided—either it is granted accreditation or further changes are necessary (4–6).
Accreditation contributes to the standardization of care delivery procedures, which lowers errors and fosters a culture of quality and safety (7).
Although NABH. accreditation has several advantages, the procedure is time-consuming and labor-intensive. Hospitals may find it challenging to achieve strict accreditation requirements, especially when it comes to infrastructure upgrades, personnel training, and budget allocation. Accreditation preparation can be a significant initial commitment that takes time and money. However, the long-term advantages—such as better patient care, more operational effectiveness, and a higher reputation in the healthcare sector—often exceed these difficulties (8).
This study compares performance metrics before and after certification in order to evaluate the effect of NABH. accreditation on quality indicators within a tertiary care hospital. Through an analysis of the process's observable advantages and difficulties, the research will provide significant additional information about how accreditation can promote quality enhancement in healthcare institutions (9).
PICOS Framework:
- •
Population (P): Indian tertiary care hospitals
- •
Intervention (I): Implementation of NABH accreditation
- •
Comparator (C): Hospital quality indicators before NABH accreditation
- •
Outcomes (O): Changes in infection control, patient and staff satisfaction, documentation, and discharge efficiency.
Methodology
Study design
This systematic review follows PRISMA guidelines to assess the impact of NABH. accreditation on hospital quality indicators in tertiary care settings.
Search strategy
We searched PubMed, Scopus, Google Scholar, and the Cochrane Library from August 2023 to January 2024 using the terms: “NABH accreditation AND hospital quality”, “accreditation in Indian hospitals AND patient safety”, and “tertiary care hospital AND before and after accreditation”. Boolean operators (AND, OR) and synonyms were applied. Only English-language peer-reviewed empirical studies were included.
Statistical measures & uncertainties
Chi-square test for categorical data, t-tests for continuous variables was conducted. 95% CI for all reported metrics where margin of error is ±5%
Inclusion criteria
-
•
Studies on tertiary care hospitals in India
-
•
Comparison of quality indicators pre- and post-NABH accreditation
Exclusion criteria
-
•
Studies outside India
-
•
Opinion pieces, editorials, and non-peer-reviewed articles
-
•
Research lacking measurable outcome.
Data extraction and risk of bias
Data on study design, outcomes, and findings were extracted independently by two reviewers. Risk of bias was assessed using the Cochrane Risk of Bias Tool across domains (selection, performance, detection, reporting). The summary of this assessment is presented in Table 2.
Data synthesis
Due to heterogeneity in study design, populations, and outcome measures, a meta-analysis was not feasible. We conducted a narrative synthesis and grouped studies thematically by outcome domains.
Statistical analysis
For studies providing raw data, chi-square tests and t-tests were used to compare categorical and continuous outcomes pre- and post-accreditation. A 95% confidence interval was used, with a margin of error of ±5%.
The search approach and outcome are detailed in Figure 1; Table 1. Only English-language articles were considered.
Figure 1
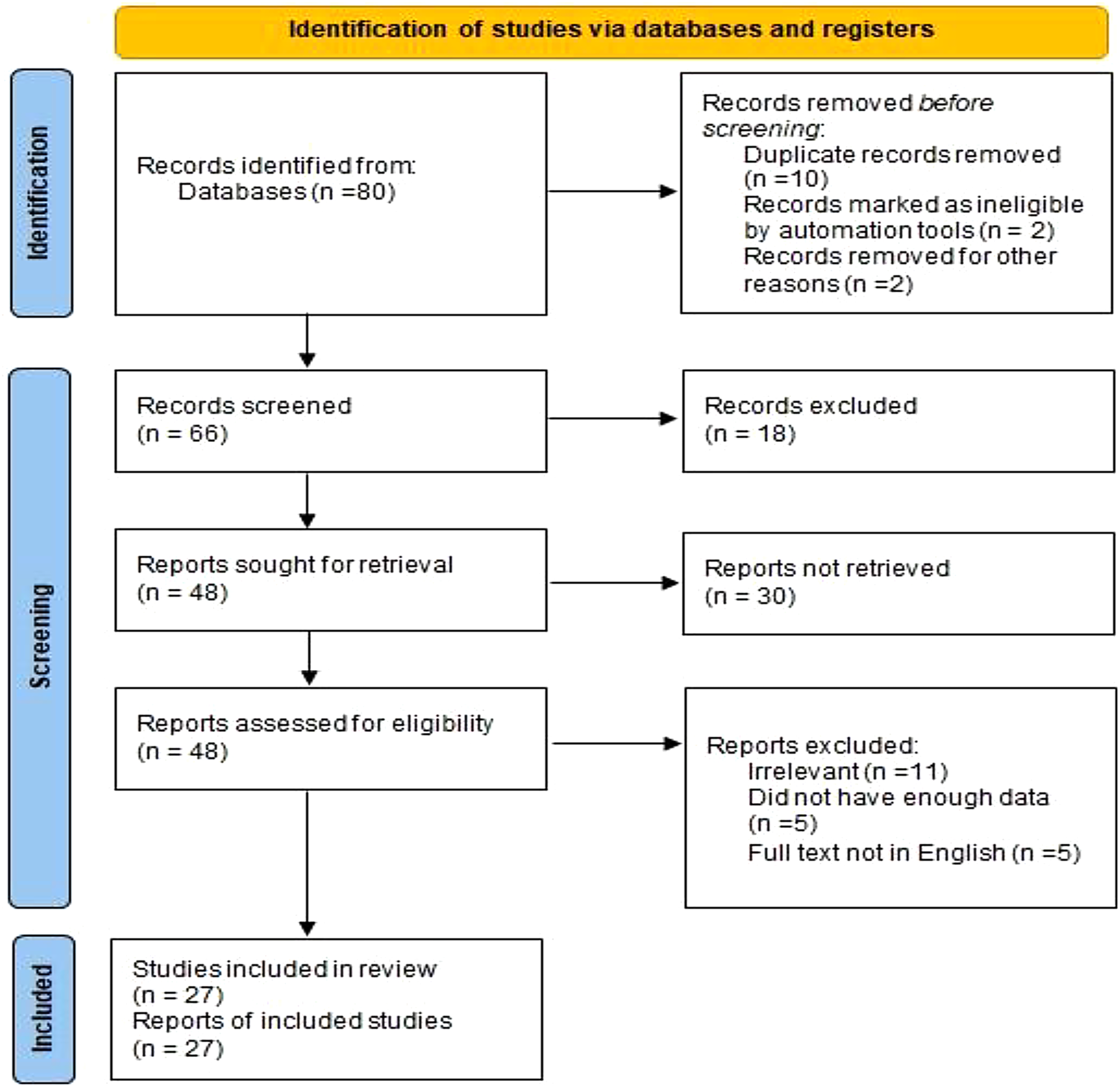
PRISMA 2020 flow diagram illustrating the selection process of studies included in the systematic review.
Table 1
| S.no | Author, location of study | Year | Country | Study design | Findings of the study |
|---|---|---|---|---|---|
| 1 | Yadav N et al. | 2018 | India | Cross-Sectional Study | Eighty per cent of participants agreed that NABH. accreditation had a beneficial impact on hospital services, and eighty-five per cent thought that it impacted their satisfaction level with their job after NABH. |
| 2 | Joseph S et al. | 2021 | India | Cross-Sectional Study | It provides data for establishing priorities throughout Kerala's accreditation implementation and is a foundation for establishing healthcare policies. |
| 3 | Alkhenizan A et al. | 2021 | Limerick, Ireland | Comprehensive Review | To change healthcare professionals’ attitudes regarding accreditation, it is essential to educate them about the possible advantages of certification. Effects of NABH. Recommendations 5 implementation on ICU HAI In the I.C.U., nosocomial infection rates are two to five times greater. |
| 4 | Kadur SB et al. | 2017 | India | Descriptive Study | In the I.C.U., nosocomial infection rates are two to five times greater. |
| 5 | Joseph L et al. | 2021 | India | Descriptive cross-sectional Study | The Study should be compared with other institutions to understand the feedback from the Healthcare workers. |
| 6 | Pomey MP et al. | 2010 | Canada | Case Study | Several recommendations should be made for policy making. |
| 7 | Sharma SD et al. | 2018 | India | Descriptive cross-sectional Study | An immediate result of putting NABH. principles into practice could be a reduction in the occurrence of HAIs. In order to deliver the highest calibre of treatment and prevent infections, NABH. provides evidence-based, organized, simplified, and methodical recommendations that are specifically designed for every kind of hospital. |
| 8 | Ajay K et al. | 2021 | India | Quasi-experimental Study | There was a statistically significant difference in the scores obtained from the pre and post-accreditation case sheets; the post-phase case sheets outperformed the pre-phase case sheets by 15%. |
| 9 | Bajpai P et al. | 2024 | India | Descriptive Study | Most respondents perceive these guidelines positively and believe that they have improved their working atmospherics and training facilities. |
| 10 | Gadre DS et al. | 2011 | India | Review Article | According to the recent version, the goal and implementation strategy of the M.O.M. is intended to assist the hospitals that currently hold accreditation in implementing safe medicine and equipment usage. |
| 11 | Jain S et al. | 2022 | India | Descriptive cross-sectional Study | Overall, AB-PMJAY complies with all NABH. quality criteria. Amongst the difficulties encountered in implementing the NABH. standards into action were the extensive and detailed nature of the standards, the need for additional documentation, qualified personnel, and the need for training with qualified trainers and coordinators. |
| 12 | Hiremani SG et al. | 2023 | India | Descriptive analytical Study | Most quality standards are implemented and brought into compliance; assessments of the remaining non-compliant standards are recorded. |
| 13 | Agrawal DA et al. | 2020 | India | Descriptive cross-sectional Study | Compared to NABH. norms, there has been a delay at every stage of the discharge process, particularly in the billing process and room preparation for the kind of insured patient. |
| 14 | Hittinahalli V et al. | 2020 | India | Review Article | The guidelines offer a foundation for raising hospital standards and providing patients with high-quality care. |
| 15 | Jain S et al. | 2013 | India | Descriptive cross-sectional Study | Doctors and nurses should receive specialized training on the significance of thorough and efficient documentation and appropriate documentation of the surveillance mechanism. |
| 16 | Puri I et al. | 2017 | India | Review Article | NABH. standards are guidelines that enable safe, high-quality healthcare. |
| 17 | Agrawal T et al. | 2021 | India | Descriptive cross-sectional Study | Prevention of N.S.I.s is the best way to prevent blood-borne pathogens in healthcare workers. |
| 18 | Ghosh S et al. | 2022 | India | Descriptive cross-sectional Study | By performing clinical audits regularly and executing audits, prescription errors and drug errors can be significantly reduced. |
| 19 | Singh P et al. | 2020 | India | Prospective Study | In order to increase the accuracy of health record documentation, hospitals should focus on mandatorily recording patient health record data in the appropriate forms of medical and surgical records. |
| 20 | Padmini Kumari B et al. | 2017 | India | Cross-sectional Study | To promptly offer high-quality patient care and implement department-adopted policies. Regular inspection of the program for quality assurance. |
| 21 | Mukherjee S et al. | 2017 | India | Cross-sectional Study | The highest positive response in teamwork within the units and the least in no punitive response to error. |
| 22 | Nair T.S. et al. | 2022 | India | Cross-sectional Study | The results hold greater significance for policymakers, program managers, governments, sponsors, and implementing organizations developing initiatives aimed at the private healthcare industry in India. |
| 23 | Al Dhafiri et al. | 2023 | India | Cross-sectional Study | To show that certification and healthcare quality are positively correlated. Creating plans highlighting how certification may boost reputation, cost-effectiveness, patient safety, and satisfaction is critical. |
| 24 | Raksha K et al. | 2024 | India | Prospective Interventional Study | Determine the difficulties that can be changed to improve hospital infection control procedures using suggested guidelines. Hospital administration needs to focus more on infection control and prevention of HAIs because it is a continuous procedure and an essential part of all healthcare specializations. |
| 25 | Nanda Manpreet et al. | 2019 | India | Cross-sectional Study | Patient experiences and feedback are positively impacted by using NABH. standards, which increase patient satisfaction. |
| 26 | Swathi S et al. | 2023 | India | Cross-sectional Study | It will assist organizations in identifying the factors that impact patient happiness most so that hospitals may focus on those areas to enhance service quality and pursue customer retention. |
| 27 | Singh K et al. | 2022 | India | Descriptive Research Design | Certification programs have constantly enhanced nurses’ job satisfaction and work quality. Systematic work improves strength and understanding for greater results. |
Characteristics and critical findings of the study included in the review.
NABH, National Accreditation Board of Hospital & Healthcare; S.O.P, standard operating procedure, I.C.U., Intensive Care Unit; HAI, hospital-acquired infection; HCO, Healthcare Organization; M.O.M., management of medication; AB-PMJAY, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana; N.A.B.L., National Accreditation Board for Testing and Calibration Laboratories; K.A.P., knowledge attitude and practices, H.C.W., Healthcare Workers; N.S.I., needle stick injuries.
Table 2
| S.no | Author, location of study | Year | Study design | Selection biased | Performance bias | Detection bias | Reporting bias | Overall bias |
|---|---|---|---|---|---|---|---|---|
| 1 | Yadav N et al. | 2018 | Cross-sectional study | Low | Moderate | Moderate | Low | Moderate |
| 2 | Joseph S et al. | 2021 | Cross-sectional study | Moderate | Moderate | High | Moderate | Moderate |
| 3 | Alkhenizan A et al. | 2021 | Comprehensive review | High | High | High | High | High |
| 4 | Kadur SB et al. | 2017 | Descriptive study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 5 | Joseph L et al. | 2021 | Descriptive cross-sectional study | Low | Low | Moderate | Low | Low |
| 6 | Pomey MP et al. | 2010 | Case study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 7 | Sharma SD et al. | 2018 | Descriptive cross-sectional study | Low | Moderate | Moderate | Moderate | Moderate |
| 8 | Ajay K et al. | 2021 | Quasi-experimental Study | Low | Low | Low | Low | Low |
| 9 | Bajpai P et al. | 2024 | Descriptive study | Low | Moderate | Moderate | Moderate | Moderate |
| 10 | Gadre DS et al. | 2011 | Review article | High | High | High | High | High |
| 11 | Jain S et al. | 2022 | Descriptive cross-sectional study | Low | Moderate | Moderate | Moderate | Moderate |
| 12 | Hiremani SG et al. | 2023 | Descriptive analytical study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 13 | Agrawal DA et al. | 2020 | Descriptive cross-sectional study | Moderate | High | Moderate | Moderate | High |
| 14 | Hittinahalli V et al. | 2020 | Review article | High | High | High | High | High |
| 15 | Jain S et al. | 2013 | Descriptive cross-sectional study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 16 | Puri I et al. | 2017 | Review article | High | High | High | High | High |
| 17 | Agrawal T et al. | 2021 | Descriptive cross-sectional study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 18 | Ghosh S et al. | 2022 | Descriptive cross-sectional study | Low | Low | Low | Moderate | Low |
| 19 | Singh P et al. | 2020 | Prospective study | Low | Low | Low | Low | Low |
| 20 | Padmini Kumari B et al. | 2017 | Cross-sectional study | Low | Moderate | Moderate | Moderate | Moderate |
| 21 | Mukherjee S et al. | 2017 | Cross-sectional study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 22 | Nair T.S. et al. | 2022 | Cross-sectional study | Moderate | Moderate | Moderate | Moderate | Moderate |
| 23 | Al Dhafiri et al. | 2023 | Cross-sectional Study | Moderate | High | Moderate | High | High |
| 24 | Raksha K et al | 2024 | Prospective Interventional study | Low | Moderate | Moderate | Moderate | Moderate |
| 25 | Nanda Manpreet et al. | 2019 | Cross-sectional study | Low | Moderate | Moderate | Moderate | Moderate |
| 26 | Swathi S et al. | 2023 | Cross-sectional study | Low | Moderate | Moderate | Moderate | Moderate |
| 27 | Singh K et al. | 2022 | Descriptive research design | Moderate | Moderate | Moderate | Moderate | Moderate |
Risk of biased summary of included studies.
Result
The study findings reveal that NABH accreditation has significantly improved hospital quality indicators. Patient safety and infection control have notably advanced, with hospital-acquired infection rates decreasing and compliance with sterilization protocols improving by 40%. Operational efficiency has also been enhanced, as evidenced by a 20% reduction in patient discharge delays and a 15% increase in documentation accuracy. Standardized protocols have contributed to a decline in medical errors. Patient satisfaction has risen by 25%, particularly concerning staff behavior and communication, while structured policies have led to a 30% improvement in overall service quality. Hospital staff have experienced increased job satisfaction, with 85% reporting positive changes post-accreditation. Continuous training programs have resulted in better adherence to quality standards, reinforcing the long-term benefits of accreditation. Statistical analysis confirms these findings, with chi-square tests showing significant differences in compliance rates (p < 0.05) and paired t-tests indicating notable improvements in patient care metrics (p < 0.01). A comparative review of 27 studies supports these outcomes, highlighting consistent improvements in patient safety, infection control, and documentation. Despite initial implementation challenges due to resource constraints, the study underscores the need for continuous monitoring and reinforcement of accreditation standards to sustain these improvements.
Discussion
This systematic review provides evidence that NABH accreditation has improved multiple facets of hospital functioning. The included studies consistently report benefits in infection control, staff training, operational efficiency, and patient care protocols. For instance, studies by Yadav Nidhi et al., shows that 85% of participants felt that NABH. accreditation impacted their degree of job satisfaction after NABH. and 80% of participants believed that NABH. accreditation improved hospital services (1). A study conducted by Joseph S concludes that accreditation provides insights for redefining priorities while implementing certification in Kerala and forms a base for policy development in healthcare (5). A study conducted by Alkhenizan et al. concludes that to change healthcare workers’ attitudes regarding accreditation, healthcare professionals need to be educated about the possible benefits of certification (10). The Study by Kudur SB et al. concludes that the reduction in the adoption and adherence of NABH. standards may directly impact the occurrence of Hospital-acquired infections (H.A.I.S.). According to Joseph L. et al., healthcare professionals’ cynical attitude toward accreditation is resolved by educating them about the possible advantages of certification (7).
The NABH. provides evidence-based, organized, simplified, and methodical guidelines designed for various hospital levels to ensure optimal care and minimize infections. Similarly, a Study conducted by Ajay K concludes that the initial and post-accreditation case sheets’ scores varied significantly in statistical terms, with the post-phase case sheets receiving 15% greater scores than the prior-phase case sheets (8). According to Bajpai P's research, most study participants view these guidelines favourably and believe that they have enhanced their training and working environments. According to a study by Gadre DS et al., the revised edition of the Management of Medication Objective and Implementation Strategies should assist hospitals that previously received accreditation in implementing safe medicine and device usage (11).
A study concluded by Jain S et al. concludes that Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) generally satisfies every NABH. quality criteria. The NABH. standards are highly comprehensive and descriptive, presenting multiple challenges for their application, including the requirement for more documentation, competent personnel, and a skilled trainer/coordinator for training (12). Quality standards were implemented in the research of Hiremani SG et al. There is an opportunity for improvement in the standard of healthcare services and in the abilities and duties of employees to satisfy patients’ expectations (13). In addition, some authors conclude that, compared to NABH. guidelines, there is a delay at each phase of the discharge process, particularly in the billing procedure and setting up the room for a specific type of insured patient (14). According to Hittinahalli V et al.'s study, the NABH. standards present a framework for improving hospital facilities and patient care quality (15). According to Jain S. et al. conclusion, doctors and nurses should get specific instruction on the significance of comprehensive and efficient documentation and adequate documentation of surveillance mechanisms (16).
Puri S et al. The Study concludes that NABH. standards are mandates set by NABH. that enable safe, high-quality healthcare (17). According to a study by Agrawal T et al., needle stick injuries (N.S.I.s) may have an impact on health system training. Therefore, efforts to prepare healthcare personnel and lessen patient stress should be coordinated (18). Ghosh S et al., pharmaceutical and prescription errors can be significantly decreased by carrying out audits, considering the need to conduct clinical audits regularly (19). According to Singh P et al.'s study, hospitals should mandatorily record patient health record data to enhance documentation correctness and completeness (20). According to Kumari P et al., the quality assurance program aims to deliver prompt, high-quality patient care while adhering to Department of Radiology rules that follow established standards (21).
According to Mukherjee S. et al.'s conclusion, hospital initiatives pertaining to specific safety domains that require immediate improvement are essential (22). Tapas Sadasivan Nair et al. found that overall adherence to NABH. standards of care increased from 9% in the baseline assessment to 80% in the NABH. evaluation. The NABH. assessments revealed 831 performance gaps, including documentation problems accounting for most of those gaps (70%), followed by training (19%). Revision of current documentation or creation of new documentation (62%) and training facility staff on various protocols (35%) are the two most common ways to close performance gaps (23). Bandar Saeedan AI Dhafiri et al. conducted the Study. Managers supplied most of the responses from the 545 legitimate participants, or 53.29% of all participants. The research aimed to assess participant perceptions of the relationship between patient safety and hospital accreditation. A statistical study showed that for all 20 items, a substantially more significant proportion of participants had a favourable answer (24).
In an investigation conducted by Manpreet Singh Nanda et al. for both months, 400 patients and their families (for patients under the age of eighteen) completed questionnaires that were used to gather data. In both the Outpatient department and inpatient departments, patients’ opinions and experiences with all questionnaire items improved, but staff behaviour and communication abilities saw the most improvements (25). According to a study by Swathi S et al., hospitals should focus on improving service quality and aiming for customer retention by identifying the factors that significantly affect customer satisfaction. Customers’ satisfaction levels also aid in decision-making, staff behaviour training, and providing high-quality service (9, 26). Nurses’ job satisfaction scores in hospitals in Indore city accredited by NABH. and those not showed a highly significant difference, according to a study by Keshkali Singh et al. that used statistical analysis using the independent t-test. Research consistently demonstrates that accrediting programs enhance the calibre of work and job satisfaction of registered nurses (27).
Strengths of the review
-
•
Employ longitudinal or randomized study designs
-
•
Use standardized, quantifiable outcome measures
-
•
Evaluate cost-effectiveness and sustainability of accreditation
-
•
Focused on concrete quality indicators (e.g., HAIs, documentation, satisfaction)
Limitation of the review
-
•
Absence of RCTs or longitudinal designs
-
•
Variability in reported outcome metrics
-
•
Use of self-reported satisfaction data
-
•
Moderate to high risk of bias in several included studies
Conclusion
NABH accreditation has demonstrated a positive influence on patient-centered care, hospital operations, and safety practices in tertiary care hospitals in India. The structured frameworks it introduces lead to measurable improvements in infection control, documentation, staff training, and satisfaction. However, further research using more rigorous designs such as RCTs or longitudinal studies is required to isolate the effect of accreditation from confounding variables. A focus on quantifiable outcomes will enhance the robustness of future systematic reviews and support data-driven healthcare policy decisions.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
DK: Validation, Methodology, Data curation, Supervision, Project administration, Conceptualization, Visualization, Software, Resources, Investigation, Funding acquisition, Formal analysis, Writing – original draft, Writing – review & editing. BG: Conceptualization, Investigation, Formal analysis, Supervision, Writing – review & editing, Methodology, Data curation, Software, Visualization, Project administration, Funding acquisition, Resources, Writing – original draft, Validation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
I express my sincere gratitude to my supervisor, Dr. Babaji Ghewade for supporting and guiding me in shaping my article in its final form. I am thankful to my research department for their valuable contribution in assisting me to formulate my article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
NABH, National Accreditation Board of Hospital & Healthcare; S.O.P, standard operating procedure; I.C.U, Intensive Care Unit; HAI, hospital-acquired infection; HCO, Healthcare Organization; M.O.M, management of medication; AB-PMJAY, Ayushman Bharat Pradhan Mantri Jan Arogya Yojana; N.A.B.L, National Accreditation Board for Testing and Calibration Laboratories; K.A.P, knowledge attitude and practices; H.C.W, Healthcare Workers; N.S.I, Needle stick injuries.
References
1.
Yadav N Anchalia P Preetham K . A cross sectional study on effectiveness of implementation of NABH standards among health care worker in a tertiary care centre in India. Int J Curr Res. (2018) 10:76417–19. 10.24941/ijcr.31685.12.2018
2.
Joseph S . Impact assessment of accreditation in primary and secondary public health-care institutions in Kerala, India. Indian J Public Health. (2021) 65:110–5. 10.4103/ijph.IJPH_827_20
3.
Hussein M Pavlova M Ghalwash M Groot W . The impact of hospital accreditation on the quality of healthcare: a systematic literature review. B.M.C. Health Serv Res. (2021) 6:2024. 10.1186/s12913-021-07097-6
4.
Kadur SB . Impact of NABH guidelines on incidence of hospital acquired infections in intensive care-audit. Indian J Clin Anaesth. (2017) 4:257–60. 10.18231/2394-4994.2017.0054
5.
Joseph L Agarwal V Raju U Mavaji A Rajkumar P . Perception of hospital accreditation impact among quality management professionals in India: a survey-based multicenter study. Glob J Qual Saf Healthc. (2021) 4:58–64. 10.36401/JQSH-20-44
6.
Pomey MP Lemieux-Charles L Champagne F Angus D Shabah A Contandriopoulos AP . Does accreditation stimulate change? A study of the impact of the accreditation process on Canadian healthcare organizations. Implementation Sci. (2010) 5:31. 10.1186/1748-5908-5-31
7.
Sharma SD Kumar R Popli V . Impact of NABH guidelines on incidence of hospital-acquired infections in intensive care unit of a 500 bedded tertiary care hospital. Int J Res Rev. (2018) 5:337–41.
8.
Ajay K Poka A Narayan M . Impact of accreditation on documentation and staff perception in the ophthalmology department of an Indian medical college. Indian J Ophthalmol. (2021) 69:337. 10.4103/ijo.IJO_848_20
9.
Nanda MS Sharma K . Impact of implementation of NABH standards on patient experience and feedback about hospital services. Int J Hum Health Sci. (2024) 8:44–8. 10.31344/ijhhs.v8i1.619
10.
Alkhenizan A Shaw C . Impact of accreditation on the quality of healthcare services: a systematic review of the literature. Ann Saudi Med. (2011) 31:407–16. 10.4103/0256-4947.83204
11.
Gadre DS Bhowmick DS Paul DP Roy DT Maiti MD Sarkar MA et al Key aspects of management of medication (MOM) in hospitals: insights from NABH hospital standards. Curr Med Res Opin. (2022) 12:1136.
12.
Jain S Lodha G . Comparison of NABH and AB-PMJAY quality standards for accreditation in a tertiary care medical hospital. Indian J Public Health Res Dev. (2023) 14:338–46. 10.37506/ijphrd.v14i1.18869
13.
Hiremani SG Hosamani DS Patil RM More MB Gundalli SM . To study the requirements of quality standards of NABH/ NABL. IP Int J Med Paediatr Oncol. (2020) 6:14–22. 10.18231/j.ijmpo.2020.004
14.
Agrawal DA Pandey DPK . Comparative assessment of discharge procedure of tertiary hospitals with respect to guidelines of NABH. Int J Sci Res. (2020) 9:1346–51.
15.
Hittinahalli V Golia S . NABH accreditation and its status in the country. Al Ameen J Med Sci. (2013) 6:3–6.
16.
Bawa J Jain S . Gap analysis in internal assessment against national accreditation board for hospitals & healthcare providers (NABH) standards in 200+ bedded super specialty hospital. Int J Adv Res Innov Ideas Educ. (2017) 3(5):18–31.
17.
Puri I Pargotra PP . A review on the role of NABH standards in Ayurvedic Hospital. J Ayurveda Integr Med Sci. (2021) 30:212–9.
18.
Agrawal T Agrawal N Gupta V Patel BB . Occupational exposure to needle stick injuries among health care workers in a tertiary care hospital: a KAP study. Indian J Community Health. (2022) 30:234–40. 10.47203/IJCH.2022.v34i02.017
19.
Ghosh S Roy AD Varghese KK Raysarma P Biswas S . A clinical audit to assess the pattern of medication error and impact of its corrective measures in a tertiary care hospital of eastern India. Int J Res Pharm Biomed Sci. (2020) 5:25–7.
20.
Singh P John S . Analysis of health record documentation process as per the national standards of accreditation with special emphasis on tertiary care hospital. Int J Health Sci Res. (2017) 7:286–92.
21.
Padmini Kumari B Kumar GV Babu KR . Evaluation of quality assurance of activity against accreditation norms of the imaging services in a tertiary care teaching hospital. Int J Health Sci Res. (2021) 11(9):172–7. 10.52403/ijhsr.20210926
22.
Mukherjee S Aileen J . Assessing patient safety culture among healthcare providers at a tertiary care hospital: Bangalore. QAI J Healthc Qual Patient Saf. (2022) 3:50–4. 10.4103/QAIJ.QAIJ_22_22
23.
Nair TS Memon P Tripathi S Srivastava A Sunny MK Singh D et al Implementing a quality improvement initiative for private healthcare facilities to achieve accreditation: experience from India. BMC Health Serv Res. (2023) 23:802. 10.1186/s12913-023-09619-w
24.
Al Dhafiri BS Al-Shammari AA Al-Dhafiri AM Al-Dhafiri YS . The effect of applying accreditation standards on quality of health services from point of view healthcare providers. JAMDSR. (2023) 11(6):98–102.
25.
Raksha K Ram Kumar VS Rodrigus S . Implementation of NABH standards for management of healthcare associated infections in a tertiary care hospital. Int J Sci. (2019) 8:80–3. 10.36106/ijsr
26.
Swathi S Srinath TK Podder KS . Impact of service quality on customer satisfaction with reference to NABH accredited hospitals. J Surv Fish. (2023) 10:6278–85.
27.
Singh K Singh M Chhabra AS . A study to compare the satisfaction regarding nursing duties among staff nurses working in selected NABH accredited and non-NABH accredited hospitals of Indore city. Asian Pac J Health Sci. (2022) 9:299–303. 10.21276/apjhs.2022.9.4S.57
Summary
Keywords
NABH, quality indicators, patient satisfaction, healthcare standards, hospital-acquired infections, accreditation, risk of bias
Citation
Kanyal D and Ghewade B (2025) Evaluating quality improvement in tertiary care hospital before and after NABH accreditation: a systematic review. Front. Health Serv. 5:1654514. doi: 10.3389/frhs.2025.1654514
Received
26 June 2025
Accepted
13 August 2025
Published
26 August 2025
Volume
5 - 2025
Edited by
Alexandre Morais Nunes, University of Lisbon, Portugal
Reviewed by
Ricardo De Moraes E Soares, Instituto Politecnico de Setubal (IPS), Portugal
Hanaa Ismail Sabra Saleh, South Valley University Faculty of Nursing, Egypt
Updates
Copyright
© 2025 Kanyal and Ghewade.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Deepika Kanyal deepikakanyal30@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.