- 1Department of Hepatobiliary and Pancreatic Surgery, University Medical Center at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 2Department of Surgery, Faculty of Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 3Helios Klinikum Schwelm, Department of Orthopedics and Trauma Surgery, Schwelm, Germany
- 4Online Research Club, Nagasaki, Japan
- 5Faculty of Medicine Delta University for Science and Technology, Gamasa, Egypt
- 6Cardiology Department, Ha Nam General Hospital, Ninh Binh, Vietnam
- 7Institute of Research and Development, Duy Tan University, Da Nang, Vietnam
- 8School of Medicine and Pharmacy, Duy Tan University, Da Nang, Vietnam
- 9Department of Surgery, AKFA Medline University Hospital, Tashkent, Uzbekistan
- 10School of Medicine, Central Asian University, Tashkent, Uzbekistan
- 11Invasive Cardiology Nam Can Tho University, Can Tho, Vietnam
- 12School of Tropical Medicine and Global Health (TMGH), Nagasaki University, Sakamoto, Nagasaki, Japan
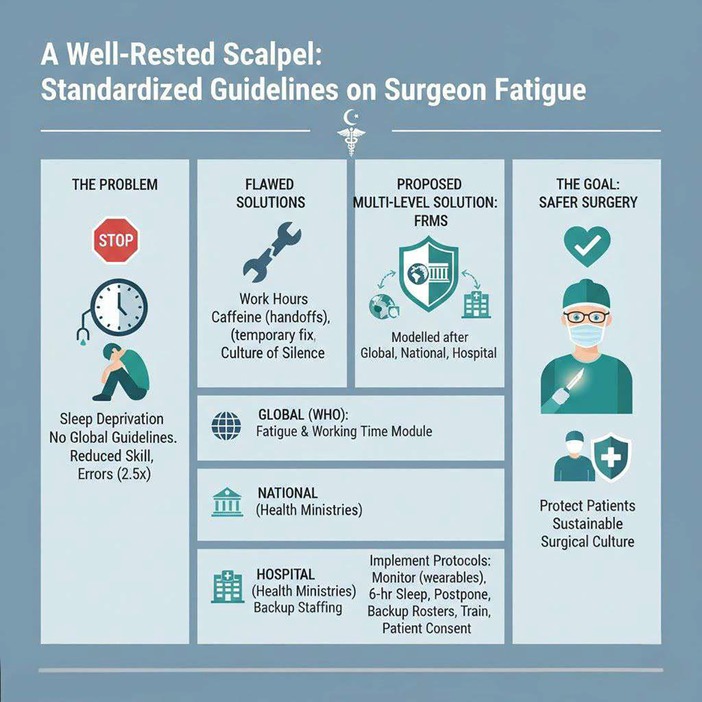
A significant gap in perioperative safety persists due to the absence of internationally recognized guidelines for managing surgeon fatigue. While other high-risk fields utilize robust fatigue management systems, surgical institutions frequently rely on fragmented coping strategies and inconsistent local policies. This oversight is concerning, as evidence confirms that sleep deprivation compromises surgical performance, with simulator studies reporting technical skill reductions of up to 32%. Current countermeasures, such as work-hour limits or caffeine use, are insufficient substitutes for restorative sleep and have an inconclusive impact on patient care. This paper proposes a systemic solution, urging global, national, and hospital-level collaboration to establish a standardized framework for fatigue risk management. Key recommendations include the use of fatigue-monitoring tools, mandating rest periods that allow for at least six hours of sleep before elective procedures, creating backup on-call rosters, and making fatigue management a part of surgical training. Adopting these evidence-based protocols is an essential step toward protecting patients and fostering a sustainable, safer surgical culture.
1 Introduction
Sleep deprivation among surgeons represents a critical and preventable threat to patient safety and physician well-being. Surgical practice is inherently demanding, involving long hours, night shifts, unpredictable emergencies, and high cognitive load, which often results in inadequate rest. Evidence from both military and medical domains demonstrates that within 48 h of sustained wakefulness, individuals may become functionally “combat-ineffective” (1). Fatigue reduces attention, memory, and decision-making, while also impairing dexterity and prolonging operative times (2, 3).
Despite decades of evidence on the risks of surgeon fatigue, there remains no internationally recognized guideline to systematically address sleep deprivation in surgery. Instead, institutions continue to rely on fragmented, ad hoc coping strategies and inconsistent local policies.
This lack of consensus suggests an important gap in perioperative safety, which can lead to bad outcomes. We urge the World Health Organization (WHO), national health ministries, and hospitals to collaborate to develop standardized fatigue management guidelines to protect both patients and surgical teams.
2 The impact of sleep deprivation on surgical performance
Multiple lines of evidence underscore that sleep deprivation compromises surgical performance. Simulator studies report reductions of 11%–32% in technical performance, with more errors, longer operative times, and diminished motion economy (4). Sleep loss further impairs decision-making, multitasking (5), and higher-order functions such as attention, while more basic functions like simple working memory and cognitive flexibility may remain intact (6). Real-world outcomes remain mixed: about one-third of clinical studies report increased complication rates among fatigued surgeons, while others find no significant differences in mortality or complication rates (3). However, large-scale data indicate that surgeons experiencing high burnout had a 2.5-fold greater odds of being involved in a medical error, while emotional exhaustion alone increased this risk by 1.7-fold (7). These inconsistencies may partly reflect methodological challenges, such as reliance on crude outcome measures that overlook subtle cognitive deficits or behavioral deficits. Experience matters, as junior surgeons and residents are more susceptible to fatigue-related impairments (8). Senior surgeons may partially compensate through experience and structured preparation (9), though often at the cost of their long-term well-being (10). The overall consensus remains clear: fatigue impairs performance in ways that are ethically and professionally indefensible if left unaddressed (11).
3 Current coping mechanisms and their limitations
There are many techniques to combat fatigue used by surgeons, and these techniques are mostly incomplete. The limitations on work hours set by the ACGME and the EWTD reduce fatigue; however, their impact on patient care is inconclusive. Patient care may actually be worsened by these policies because handoffs are more frequent and less continuous (12). The above methods, as well as individual strategies such as coffee, bright light, and microbreaks, are improvements. However, these strategies are not replacements for sleep (13). Caffeine may improve wakefulness but also can lead to performance detriment in highly skilled tasks at higher doses (14). Sleep banking is a method where there is sleep extension prior to a period of anticipated deprivation. This method is used in the military and in aviation, but in healthcare, its potential is vastly ignored (15). The aim of this paper is to argue that incorporating structured sleep banking schedules into surgical routines will assist in alleviating fatigue and its associated risks. Pharmacologic stimulants, such as modafinil and amphetamines, can increase alertness; however, the user may become overconfident and believe there is no room for further lethargy (16). There is a lack of cultural awareness regarding the surgical field. This culture, which encourages lack of endurance and silence surrounding fatigue, socially constructs fatigue in a very dangerous manner (17). The gaps in this approach, which is remaining underdeveloped at the moment, are very important.
4 The case for standardized guidelines
In line with practices from aviation and other high-risk industries, fatigue management in surgery should encompass several key components (18). These include the establishment of Fatigue Risk Management Systems (FRMS), that integrate structured rostering rules—such as limiting consecutive night shifts, ensuring ≥11 h of rest between duties, and avoiding “quick returns”—as successfully applied by Transport Canada and the FAA/NASA Fatigue Countermeasures Program (19, 20). Surgeons’ sleep deficits should be assessed and monitored using validated self-assessment tools and/or worn monitoring devices (21, 22). Evidence shows that surgeons obtaining fewer than six hours of sleep before elective procedures are 2.7 times more likely to experience intraoperative complications, whereas those who are sleep-deprived despite achieving at least six hours of rest still face a 170% increased risk of adverse events (23, 24). Accordingly, elective procedures should be postponed when fatigue thresholds are exceeded, and hospitals should maintain on-call rosters of qualified surgeons to fill in for overworked and exhausted colleagues. Additional countermeasures proven effective in other high-risk sectors include controlled 20-minute rest breaks (25), moderate caffeine doses (approximately 32–300 mg) administered early in a shift may enhance alertness and vigilance (26), and fatigue-awareness training such as the UK Association of Anaesthetists’ Fight Fatigue campaign and NHS Fatigue Pack (27). Lastly, in the graduate training, fatigue management and recognition should be imbibed into the curricula, and patients should be informed if their operating surgeon is significantly sleep-deprived, supporting informed consent and, when appropriate, the option to reschedule the procedure.
4.1 Implementation considerations
When talking about fatigue management from an organizational perspective, it is crucial to look at fatigue management within a global, national, and hospital context simultaneously and in a coordinated manner. The World Health Organization needs to take the Global Patient Safety Action Plan 2021–2030 and augment it with a fatigue and working time module, developing a first model incorporating FRMS principles (28) successfully used in aviation and now adapted to healthcare. At the national level, Ministries of Health must customize and implement these frameworks to the local context, mandating adherence, providing backup staffing, on-call system resources, and alignment with the WHO/ILO occupational health and safety standards (29). At the hospital level, institutions ought to incorporate Fatigue Risk Management Systems, monitor the impact of schedule reforms, and promote the rest of the surgical culture as protective to patients (30). Furthermore, the fundamental barriers, like culture, pushback from senior surgical staff, and lack of health workforce and resources in low- and middle-income and developing countries, make the execution of such plans difficult. High-volume centers can be the starting point and support pilot programs to test the refinement of resistance evidence, sustainability, and feasibility to promote the surge for evidence-based practice.
5 Conclusion
For sure, sleep deprivation on the part of the surgeon is an epic risk when it comes to the safety of patients and the doctor himself/herself, both of whom are put in danger and are in dire need of safety and protection, all of which are not in any way an illusion. While the results, when analyzed in the context of certain outcome studies, might not be as straightforward, any simulator-based studies and cognitive or clinical trials show consistent results affirming that performance is impaired in one way or another. Current and existing coping mechanisms for this problem, such as the use of caffeine, short naps, and all peer casual and informal support, are not and have never been effective. It is only the clear and present danger that is resulting from sleep deprivation on the part of the surgeon that is leading to the emergence of global guidelines. Healthcare systems have the power, thanks to the existing fatigue assessment methods, mandatory rest and lap periods, active avoidance of procedures, replacement staffing systems, educational initiatives, and openness, that can lead to safer surgical procedures along with longer sustainable working periods in the field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
DL: Writing – original draft, Writing – review & editing. MD: Conceptualization, Writing – original draft, Writing – review & editing. ES: Conceptualization, Writing – original draft, Writing – review & editing. DT: Writing – original draft, Writing – review & editing. MK: Writing – original draft, Writing – review & editing. PT: Writing – original draft, Writing – review & editing. NH: Writing – original draft, Writing – review & editing. TL: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Howard SK, Gaba DM, Rosekind MR, Zarcone VP. The risks and implications of excessive daytime sleepiness in resident physicians. Acad Med. (2002) 77(10):1019–25. doi: 10.1097/00001888-200210000-00015
2. Parker RS, Parker P. The impact of sleep deprivation in military surgical teams: a systematic review. J R Army Med Corps. (2017) 163(3):158–63. doi: 10.1136/jramc-2016-000640
3. Reijmerink IM, van der Laan M, Wietasch JKG, Hooft L, Cnossen F. Impact of fatigue in surgeons on performance and patient outcome: systematic review. Br J Surg. (2023) 111(1):znad397. doi: 10.1093/bjs/znad397
4. Eastridge BJ, Hamilton EC, O’Keefe GE, Rege RV, Valentine RJ, Jones DJ, et al. Effect of sleep deprivation on the performance of simulated laparoscopic surgical skill. Am J Surg. (2003) 186(2):169–74. doi: 10.1016/S0002-9610(03)00183-1
5. Lim JYL, Killgore WDS, Bennett D, Drummond SPA. The impact of sleep loss on decision making: opening the cognitive black box. Sleep Med Rev. (2025) 82:102114. doi: 10.1016/j.smrv.2025.102114
6. García A, Del Angel J, Borrani J, Ramirez C, Valdez P. Sleep deprivation effects on basic cognitive processes: which components of attention, working memory, and executive functions are more susceptible to the lack of sleep? Sleep Sci. (2021) 14(2):107–18. doi: 10.5935/1984-0063.20200049
7. Al-Ghunaim TA, Johnson J, Biyani CS, Alshahrani KM, Dunning A, O'Connor DB. Surgeon burnout, impact on patient safety and professionalism: a systematic review and meta-analysis. Am J Surg. (2022) 224(1, Part A):228–38. doi: 10.1016/j.amjsurg.2021.12.027
8. Gander P, Purnell H, Garden A, Woodward A. Work patterns and fatigue-related risk among junior doctors. Occup Environ Med. (2007) 64(11):733–8. doi: 10.1136/oem.2006.030916
9. Banfi T, Coletto E, d'Ascanio P, Dario P, Menciassi A, Faraguna U, et al. Effects of sleep deprivation on surgeons dexterity. Front Neurol. (2019) 10:595. doi: 10.3389/fneur.2019.00595
10. Vitous CA, Dinh DQ, Jafri SM, Bennett OM, MacEachern M, Suwanabol PA. Optimizing surgeon well-being: a review and synthesis of best practices. Ann Surg Open. (2021) 2(1):e029. doi: 10.1097/as9.0000000000000029
11. Weinger MB, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. (2002) 287(8):955–7. doi: 10.1001/jama.287.8.955
12. Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. (2014) 259(6):1041–53. doi: 10.1097/sla.0000000000000595
13. Hayashi M, Masuda A, Hori T. The alerting effects of caffeine, bright light and face washing after a short daytime nap. Clin Neurophysiol. (2003) 114(12):2268–78. doi: 10.1016/S1388-2457(03)00255-4
14. Wilk M, Krzysztofik M, Filip A, Zajac A, Del Coso J. The effects of high doses of caffeine on maximal strength and muscular endurance in athletes habituated to caffeine. Nutrients. (2019) 11(8):1912. doi: 10.3390/nu11081912
15. Patterson PD, Ghen JD, Antoon SF, Martin-Gill C, Guyette FX, Weiss PM, et al. Does evidence support “banking/extending sleep” by shift workers to mitigate fatigue, and/or to improve health, safety, or performance? A systematic review. Sleep Health. (2019) 5(4):359–69. doi: 10.1016/j.sleh.2019.03.001
16. Caldwell JL, Schroeder VM, Kunkle CL, Stephenson HG. Differential effects of modafinil on performance of low-performing and high-performing individuals during total sleep deprivation. Pharmacol Biochem Behav. (2020) 196:172968. doi: 10.1016/j.pbb.2020.172968
17. Coverdill JE, Bittner JGI, Park MA, Pipkin WL, Mellinger JD. Fatigue as impairment or educational necessity? Insights into surgical culture. Acad Med. (2011) 86(10):S69–72. doi: 10.1097/ACM.0b013e31822a6b40
18. Cumber E, Greig PR. Can a tool developed for industry be used to assess fatigue risk in medical rotas? A pilot study of foundation doctors’ rotas in a tertiary centre. BMJ Open. (2019) 9(2):e023470. doi: 10.1136/bmjopen-2018-023470
19. Transport Canada. Flight Crew Member Fatigue Management – Prescriptive Regulations. Government of Canada (2024). Available online at: https://tc.canada.ca/en/aviation/reference-centre/advisory-circulars/advisory-circular-ac-no-700-047 (Accessed October 26, 2025).
20. Hilditch CJ. The Benefits of Napping for Safety & How Quickly Can the Brain Wake-Up from Sleep? Nasa.gov. (2019). Available online at: https://ntrs.nasa.gov/citations/20190033981 (Accessed November 2, 2025).
21. Kakhi K, Jagatheesaperumal SK, Khosravi A, Alizadehsani R, Acharya UR. Fatigue monitoring using wearables and AI: trends, challenges, and future opportunities. Comput Biol Med. (2025) 195:110461. doi: 10.1016/j.compbiomed.2025.110461
22. Whelehan DF, Alexander M, Connelly TM, McEvoy C, Ridgway PF. Sleepy surgeons: a multi-method assessment of sleep deprivation and performance in surgery. J Surg Res. (2021) 268:145–57. doi: 10.1016/j.jss.2021.06.047
23. Czeisler CA, Pellegrini CA, Sade RM. Should sleep-deprived surgeons be prohibited from operating without Patients’ consent? Ann Thorac Surg. (2013) 95(2):757–66. doi: 10.1016/j.athoracsur.2012.11.052
24. Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. (2009) 302(14):1565–72. doi: 10.1001/jama.2009.1423
25. Konya I, Shishido I, Watanabe K, Ikebuchi M, Tanaka T, Kataoka H, et al. Effects of taking a nap or break immediately after night shift on nurses’ fatigue recovery and sleep episodes: a quasi-experimental study. J Physiol Anthropol. (2025) 44(1):21. doi: 10.1186/s40101-025-00399-2
26. McLellan TM, Caldwell JA, Lieberman HR. A review of caffeine’s effects on cognitive, physical and occupational performance. Neurosci Biobehav Rev. (2016) 71:294–312. doi: 10.1016/j.neubiorev.2016.09.001
27. Anaesthetists, T.A.O. Fight Fatigue resources (NHS Trust). (2020). Available online at: https://anaesthetists.org/Portals/0/PDFs/Wellbeing/Fatigue%20Pack_Scotland.pdf?ver=2020-10-15-133930-043 (Accessed October 26, 2025).
28. Stewart S, Koornneef F, Akselsson R. Establishment of the global international fatigue risk management forum. Aviat Psychol Appl Hum Fact. (2011) 1(2):103–9. doi: 10.1027/2192-0923/a000017
29. WHO, ILO. HealthWISE Work Improvement in Health Services: Action Manual. 1st ed. International Labour Organization and World Health Organization (2014). Available online at: https://www.who.int/publications/m/item/health-wise-action-manual (Accessed October 26, 2025).
30. Rosen M, Kilcullen MP, Zhang A, Sharma R, Xiao C, Bass EB. Fatigue and Sleepiness of Clinicians Due to Hours of Service: Rapid Response, in Making Healthcare Safer IV: A Continuous Updating of Patient Safety Harms and Practices. Rockville, MD: Agency for Healthcare Research and Quality (US) (2023).
Keywords: surgeon fatigue, burnout, patients safety, fatigue countermeasures, perioperative safety, surgical performance
Citation: Le DT, Dadam MN, Shaaban E, Thang DX, Khaydarov M, Tran P, Huy NT and Long TCD (2025) A well-rested scalpel: a proposal for standardized guidelines on surgeon fatigue. Front. Health Serv. 5:1713346. doi: 10.3389/frhs.2025.1713346
Received: 2 October 2025; Accepted: 27 October 2025;
Published: 20 November 2025.
Edited by:
Melissa Baysari, The University of Sydney, AustraliaReviewed by:
Abdulmueen Alotaibi, University of Almaarefa, Saudi ArabiaCopyright: © 2025 Le, Dadam, Shaaban, Thang, Khaydarov, Tran, Huy and Long. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nguyen Tien Huy, bmd1eWVudGllbmh1eTRAZHV5dGFuLmVkdS52bg==; Tran Cong Duy Long, bG9uZy50Y2RAdW1jLmVkdS52bg==
†These authors have contributed equally to this work
‡ORCID:
Dat Tien Le
orcid.org/0000-0002-5623-9737
Mohammad Najm Dadam
orcid.org/0000-0002-8814-0205
Ethar Shaaban
orcid.org/0009-0002-2818-6065
Dang Xuan Thang
orcid.org/0000-0002-7973-2858
Mukhammadbektosh Khaydarov
orcid.org/0009-0006-2554-7987
Phillip Tran
orcid.org/0000-0003-3329-2276
Nguyen Tien Huy
orcid.org/0000-0002-9543-9440
Tran Cong Duy Long
orcid.org/0000-0002-3994-4864
 Dat Tien Le
Dat Tien Le Mohammad Najm Dadam
Mohammad Najm Dadam Ethar Shaaban5,‡
Ethar Shaaban5,‡ Dang Xuan Thang
Dang Xuan Thang Mukhammadbektosh Khaydarov
Mukhammadbektosh Khaydarov Nguyen Tien Huy
Nguyen Tien Huy