Abstract
Extracellular vesicles (EVs), natural membrane-bound structures released by cells, offer a promising platform for precise and targeted delivery of therapeutic payloads, including drugs and nanoparticles. This comprehensive review explores the integration of engineered nanomaterials with EVs to advance drug delivery systems. It covers various aspects of this integration, including techniques for synthesizing, loading, characterizing, and applying nanomaterials within EVs. Methodologies for integrating diverse nanocarriers like nanoparticles, liposomes, and quantum dots into EVs are discussed, along with characterization methods such as electron microscopy and light scattering. Attention is also given to considerations of biological compatibility, safety assessments, and strategies for surface modification to enhance targeting precision. Highlighting various applications, including targeted drug delivery, cancer therapy, and vaccine development, the review underscores the potential of EV-nanomaterial hybrids to leverage EVs’ innate targeting capabilities and the versatility of nanomaterials. However, it also addresses challenges such as scalability, standardization, and safety that must be overcome to facilitate the clinical translation of these promising biomedical solutions.
1 Introduction
Extracellular vesicles (EVs) are gaining considerable attention in advanced biomedical applications due to their pivotal role in intercellular communication. EVs are naturally occurring nanoscale vesicles, secreted by various cell types and provide a unique platform for transporting bioactive cargo, such as proteins, nucleic acids, and lipids, across biological barriers (Song et al., 2022). However, realizing the full therapeutic potential of EVs presents challenges like limited cargo capacity, rapid clearance from circulation, and difficulties in achieving targeted delivery. This is where nanomaterials come into play a versatile class of engineered nanoparticles and structures at the nanoscale, designed with specific properties and functions (Xu M. et al., 2023). Integrating nanomaterials with EVs forms a synergistic partnership that offers promising solutions to these challenges, unlocking advanced possibilities in biomedical applications (Tian et al., 2022).
Understanding the fundamental characteristics of nanomaterials and EVs are essential before exploring their synergistic integration. An EV is a membrane-bound structure released by a cell, such as an exosome, nanovesicles, or apoptotic bodies. Physiological processes rely on them for transporting biologically active molecules (Zinger et al., 2020). Furthermore to the endosomal sorting complex required for transport (ESCRT) machinery, lipid rafts, and protein sorting pathways play a significant role in their formation and cargo loading (Rani et al., 2023). Meanwhile, nanomaterials have different physical and chemical properties, including nanoparticles, liposomes, and polymers. Size, shape, surface chemistry, and cargo-loading capacity can all be precisely controlled using top-down and bottom-up manufacturing methods (Gong et al., 2023). The integration of nanomaterials with EVs addresses the challenge of enhancing their cargo capacity. The increased cargo capacity of EVs is one of the key advantages of this integration (Liu C. et al., 2022). A more substantial cargo of drugs, nucleic acids, or imaging agents can be delivered to target cells or tissues using EVs loaded with nanomaterials that contain therapeutic agents. As cancer therapy requires high drug doses, systemic toxicity is often a concern, which makes this feature particularly valuable. Integration of EVs and nanomaterials can be used to enhance drug delivery efficiency while minimizing off-target effects (Zhang et al., 2021).
Additionally, the incorporation of nanomaterials into EVs enhances the vesicles’ stability. The EVs may be degraded by enzymes or cleared by the immune system if administered directly. By extending the circulation time of EVs and ensuring a more sustained therapeutic effect, nanomaterials can protect them against external factors (Manandhar et al., 2022). Furthermore, nanomaterials can be customized with targeting ligands to enable precise site-specific delivery. This active targeting capability addresses the challenge of achieving precision medicine by directing therapeutic cargo exclusively to the intended cells or tissues while sparing healthy ones. This develops particularly significant in the context of diseases like cancer, where the precise delivery of drugs to tumor sites is crucial (Luo et al., 2020). Besides, nanomaterials combined with EVs present novel opportunities for regenerative medicine. A substantial amount of attention has been paid to EVs derived from stem cells because of their regenerative potential. It is possible to engineer these EVs to repair and regenerate tissues by combining them with nanomaterials. The nanomaterials not only offer structural support but can also be designed to mimic the extracellular matrix, facilitating cell adhesion and tissue regeneration. This approach holds promise in various applications, such as repairing damaged cardiac tissue, addressing neural injuries, and treating musculoskeletal disorders (Beetler et al., 2023).
In this review, we explore the transformative synergy between nanomaterials and EVs, including implications for diagnostics, drug delivery, and regenerative medicine. EVs, once overlooked, have now come to the forefront as crucial mediators of intercellular communication, proficient in transporting biomolecules across biological barriers. Nanomaterials, engineered on the nanoscale, effectively address the limitations of EVs, enhancing their cargo capacity, stability, and targeted delivery capabilities. This comprehensive review navigates through various sources of EVs, elucidates their biogenesis, and outlines the regulatory mechanisms involved. Subsequently, it explores the multifaceted advantages and innovative strategies associated with the integration of nanomaterials and EVs, unveiling advanced biomedical applications. Therefore, this review aims to provide a comprehensive analysis of the synergistic potential between extracellular vesicles and nanomaterials for advanced biomedical applications.
In this review, we conducted a systematic literature search across PubMed, Scopus, Web of Science, and Google Scholar to identify studies on integrating extracellular vesicles with nanomaterials for targeted drug delivery and biomedical applications. Using keywords like “extracellular vesicles,” “nanomaterials,” and “targeted therapy,” we included peer-reviewed articles in English published within the last decade, prioritizing those that directly addressed EV-nanomaterial hybrids in therapeutic or diagnostic applications. Studies were selected based on relevance, methodological quality, and robustness of findings, with exclusions applied to non-medical uses, opinion pieces, and theoretical-only models. This approach ensures a focused and comprehensive review of recent advances in EV-nanomaterial integration for biomedical applications.
2 Extracellular vesicles (EVs)
EVs signify a fascinating and diverse class of biological nanoparticles that have garnered substantial attention in the fields of cell biology, immunology, and biomedical research (Mansoori et al., 2022). These small membranous structures are buried by virtually all cell types and play pivotal roles in intercellular communication, both in physiological and pathological contexts (Patil and Soekmadji, 2021).
2.1 Diverse sources of EVs
Extracellular vesicles (EVs) are tiny structures secreted by various cell types, serving as crucial messengers in intercellular communication. In animals, diverse sources of EVs (Figure 1). On the other hand, in plants (Figure 2), EVs are produced by variety of cells which are described in Table 1. Both animal and plant-derived EVs carry diverse cargo and play crucial roles in physiology, health, and disease. Research into EVs continues to expand, offering promising applications in various fields (Silachev, 2023).
FIGURE 1

Sources of EVs from the different animal cells. This figure visually bears the concept that EVs are released by animal cells, originating from various cellular sources, and they could play various roles in the advanced biomedical applications.
FIGURE 2

Sources of EVs from plant cells. This figure visually conveys the concept that EVs are released by plant cells, originating from several cellular sources within the plant cells, and they could play diverse roles in biomedical applications.
TABLE 1
| Sources | Description | References | |
|---|---|---|---|
| Animal-derived Evs | Mesenchymal Stem Cells (MSCs) | Release regenerative EVs with growth factors and immune-modulatory molecules | Allan et al. (2020) |
| Immune Cells | Dendritic cells, macrophages, T cells, and B cells produce EVs influencing immune responses and antigen presentation | Zhou et al. (2022b) | |
| Cancer Cells | Cancer cells emit tumor-derived EVs, aiding tumor growth and metastasis | Xu et al. (2022) | |
| Neurons and Glial Cells | Central nervous system cells release EVs for synaptic signaling, neuroprotection, and neurodegenerative disease spread | Shaimardanova et al. (2020) | |
| Endothelial Cells | EVs from these cells affect vascular homeostasis, inflammation, and endothelial dysfunction | Song et al. (2020) | |
| Cardiomyocytes | Cardiac EVs (exosomes, microvesicles) play roles in cardiac health and regeneration | Wagner et al. (2021) | |
| Epithelial Cells | They release EVs involved in tissue repair, immune responses, and intercellular signaling | Zonneveld et al. (2021) | |
| Adipocytes | Adipose tissue-derived EVs affect metabolic regulation and obesity-related issues | Li et al. (2023c) | |
| Platelets | Platelet EVs, called microparticles, participate in hemostasis, thrombosis, and inflammation | Boilard and Bellio (2022) | |
| Hepatocytes | Liver cells release EVs relevant to liver diseases | Li et al. (2022c) | |
| Sperm Cells | Epididymosomes from sperm cells assist in sperm maturation and fertilization | Ali et al. (2023) | |
| Placental Cells | Syncytiotrophoblast-derived exosomes play roles in fetal development and maternal-fetal communication | Nair and Salomon (2020) | |
| Stem Cells | Various stem cell types release EVs with regenerative potential | Haque et al. (2022) | |
| Adipose Tissue-Derived Stromal Cells (ASCs) | A subtype of stem cells, ASCs release therapeutic EVs | Ritter et al. (2022) | |
| Circulating Blood Cells | Red and white blood cells release EVs affecting immune responses, clotting, and vascular health | Thangaraju et al. (2020) | |
| Ciliated Cells | Respiratory tract ciliated cells release EVs with roles in mucociliary clearance and respiratory defense | Kalininskiy et al. (2021) | |
| Plant-derived EVs | Plant Cells | Nearly all plant cells release EVs, facilitating cell-to-cell communication, nutrient transport, and defense responses | Borniego and Innes (2023) |
| Leaf Cells | They emit EVs crucial for transporting phytohormones, nutrients, and secondary metabolites | Song et al. (2023) | |
| Root Cells | Root cell-derived EVs participate in nutrient uptake, transport, and signaling during symbiotic interactions | Cai et al. (2021) | |
| Pollen Cells | Pollen cell EVs are involved in pollen tube growth and fertilization | Yu et al. (2023) | |
| Seed Cells | Seed cell EVs transport nutrients and information during seed development and germination | Girija et al. (2023) | |
| Phloem Sieve Elements | These cells produce EVs contributing to systemic signaling and stress responses | Notaguchi et al. (2022) | |
| Root Nodules | In leguminous plants, nodule cells release EVs involved in nutrient exchange with nitrogen-fixing bacteria | Dicenzo et al. (2020) | |
| Pathogen-Infected Cells | Infected plant cells release EVs as part of their defense, potentially carrying antimicrobial compounds | Zhou et al. (2022a) | |
| Stress-Induced EVs | Plants produce EVs in response to environmental stresses, aiding in stress adaptation | Bhattacharya and Kundu (2020) | |
| Xylem Cells | Xylem cell EVs play roles in long-distance signaling | Rogo et al. (2023) | |
| Reproductive Tissues | Ovules, embryos, and pollen cells release EVs during reproduction | Bayat et al. (2021) | |
| Algal Cells | Some algae also produce EVs, likely involved in communication and responses to environmental conditions | Silachev (2023) | |
Different sources of EVs.
2.2 Biogenesis of extracellular vesicles
EVs are produced through a complex biogenesis process, involving budding from the plasma membrane or intracellular compartments. They come in three types (Table 2): exosomes, originating from the endosomal system; microvesicles, budding directly from the cell membrane; and apoptotic bodies formed during cell apoptosis. EV biogenesis is tightly regulated and includes the sorting of cargo molecules like proteins and nucleic acids, facilitating their vital roles in intercellular communication and physiology (Kang et al., 2021).
TABLE 2
|
Type |
Description | Size range | Biogenesis mechanism |
|---|---|---|---|
| Exosomes | Exosomes are the smallest of the three major EV types, typically ranging from 30 to 150 nm in diameter. They are produced by endosomes. The process begins with the formation of early endosomes, which mature into multivesicular bodies (MVBs) containing intraluminal vesicles (ILVs). These ILVs are ultimately released as exosomes when MVBs fuse with the cell’s plasma membrane | 30–150 nm | Endosomal pathway: Formation of early endosomes, maturation into MVBs, and release of ILVs as exosomes upon fusion with the cell’s plasma membrane |
| Microvesicles (Microparticles or Shedding Vesicles) | Microvesicles are larger than exosomes, typically ranging from 100 to 1,000 nm. They are produced by direct outward budding and fission of the cell’s plasma membrane. This process is triggered by various cellular stimuli, including calcium influx, cytoskeletal rearrangements, and activation of certain enzymes | 100–1,000 nm | Plasma membrane budding and fission: Direct outward budding and fission of the cell’s plasma membrane, triggered by various cellular stimuli |
| Apoptotic Bodies | Apoptotic bodies are the largest among the three types, with diameters exceeding 1,000 nm. They are produced during programmed cell death (apoptosis). As a dying cell undergoes apoptosis, it fragments into apoptotic bodies, which contain various cellular components, including organelles and deoxyribonucleic acid (DNA) fragments. These apoptotic bodies are subsequently engulfed and cleared by phagocytic cells | >1,000 nm | Programmed cell death (apoptosis): Formation of apoptotic bodies as dying cells undergo apoptosis, containing a variety of cellular components and DNA fragments. These bodies are subsequently engulfed and cleared by phagocytic cells |
The key characteristics and biogenesis mechanisms of EVs.
2.3 Classification of extracellular vesicles
Extracellular vesicles (EVs) are small, membrane-bound particles secreted by cells into the extracellular environment, serving as key mediators of intercellular communication. Based on characteristics such as size, biogenesis pathways, and molecular composition, EVs are generally classified into three main types: exosomes, microvesicles, and apoptotic bodies.
2.3.1 Exosomes
Exosomes are the smallest type of EVs, typically ranging from 30 to 150 nm in diameter. They are formed within endosomal compartments called multivesicular bodies (MVBs), which fuse with the plasma membrane to release exosomes into the extracellular space. Exosomes carry a diverse array of bioactive molecules, including proteins, lipids, and nucleic acids (e.g., miRNAs, mRNAs), which play essential roles in cellular signaling and immune modulation. Key surface markers for exosomes include tetraspanins such as CD63, CD81, and CD9. Exosomes are involved in processes such as immune responses, tissue regeneration, and tumor progression, and can originate from various cell types like dendritic cells, mesenchymal stem cells, and cancer cells.
2.3.2 Microvesicles
Microvesicles, also known as ectosomes or microparticles, vary widely in size, generally ranging from 100 to 1,000 nm. Unlike exosomes, microvesicles are formed through the outward budding and fission of the plasma membrane. Their molecular composition is highly dependent on the originating cell type, encompassing surface markers and cargos that reflect the cell’s physiological state. They often express phosphatidylserine on their surface, which serves as a distinguishing marker. Microvesicles are implicated in hemostasis, inflammation, and cellular repair processes and are commonly secreted by platelets, endothelial cells, and immune cells.
2.3.3 Apoptotic bodies
Apoptotic bodies are the largest type of EVs, typically ranging from 1 to 5 µm in diameter. These vesicles are produced during apoptosis, a regulated form of cell death, and contain fragments of the parent cell, including DNA, cytoplasmic components, and intact organelles. Apoptotic bodies are cleared by phagocytic cells, contributing to immune tolerance and inflammation regulation. Their composition often includes phosphatidylserine and markers like histones, which are indicative of their apoptotic origin.
Beyond these primary classifications, EVs can also be categorized into subpopulations based on specific markers, cargo contents, and the cell types from which they originate. For example, EVs derived from cancer cells often contain oncogenic proteins and nucleic acids that support tumor growth and metastasis, while EVs from mesenchymal stem cells are rich in regenerative factors that aid in tissue repair. Additionally, EVs secreted under different physiological conditions, such as oxidative stress or hypoxia, display unique molecular profiles that reflect these environmental cues. (Palanisamy et al., 2023).
2.4 Physiological roles of extracellular vesicles
EVs serve diverse physiological roles in intercellular communication (Table 3). They transport bioactive molecules, including proteins, lipids, and nucleic acids, influencing processes like immune regulation, tissue repair, and cell signaling. EVs are also implicated in disease pathogenesis and hold promise as diagnostic and therapeutic tools in various medical fields. There are several physiological processes to be understood and novel biomedical applications to be developed, which depend on EVs, and these vesicles represent a versatile and dynamic way to communicate between cells. Their biogenesis, classification, and roles continue to be areas of intense research, represents promising avenues for future discoveries and therapeutic interferences (Cheng and Hill, 2022).
TABLE 3
| Roles of EVs | Description | References |
|---|---|---|
| Intercellular Communication | EVs serve as messengers that transport bioactive molecules such as proteins, lipids, nucleic acids (DNA, ribonucleic acid (RNA), and microRNAs), and metabolites between cells. They facilitate the exchange of information and regulatory signals, influencing recipient cell behavior | Li et al. (2023a) |
| Immune Regulation | EVs derived from immune cells, such as dendritic cells and T cells, play a significant role in immune responses. They can either stimulate or suppress immune reactions, depending on their cargo and context | Mittal et al. (2020) |
| Tissue Homeostasis | EVs contribute to tissue repair and regeneration by delivering growth factors and signaling molecules to target cells. Stem cell-produced EVs, for instance, have regenerative potential | Jia et al. (2023) |
| Pathogen Defense | Certain EVs comprise antimicrobial factors and can be intricately involved in the immune response against infections | Buzas (2023) |
| Cancer Progression | In cancer, EVs are involved in tumor growth, metastasis, and immune evasion. Furthermore, they are capable of carrying oncogenic cargo, promoting angiogenesis, and altering the tumor microenvironment | Schubert and Boutros (2021) |
| Neurological Functions | EVs are involved in neuronal signaling, synaptic plasticity, and the spread of pathological proteins in neurodegenerative diseases and disorders | Natale et al. (2022) |
| Diagnostic and Therapeutic Targets | Various diseases, including cancer and neurodegenerative disorders, have been linked to EVs as potential biomarkers. Hence, they are also being explored as drug delivery vehicles for targeted therapy | Cheng and Hill (2022) |
The physiological roles of EVs in both health and disease, highlighting their functions.
2.5 Mechanisms governing EVs formation and secretion
The formation and secretion of EVs are complex processes regulated by numerous cellular mechanisms (Table 4). These pathways vary by cell type and are tailored to meet specific cellular needs. Key pathways, such as those mediated by the Endosomal Sorting Complex Required for Transport (ESCRT) machinery, lipid rafts, and calcium signaling, orchestrate EV biogenesis, ensuring the correct cargo is sorted, enclosed, and released. Below, we outline the principal mechanisms that regulate EV formation and secretion, with examples of their roles in producing different EV types, including exosomes, microvesicles, and apoptotic bodies (Zhang et al., 2023).
TABLE 4
| Mechanisms governing EVs formation and secretion | Description | References |
|---|---|---|
| Endosomal Sorting Complexes Required for Transport (ESCRT) | ESCRT is critical for EVs biogenesis in many cell types. It comprises various protein complexes (ESCRT-0, -I, -II, and -III) that recognize and sequester specific cargo into intraluminal vesicles (ILVs) within multivesicular bodies (MVBs). ESCRT-III is responsible for vesicle scission and release of ILVs as exosomes into the MVB lumen | Cruz Camacho et al. (2023) |
| Lipid Rafts and Tetraspanins | Lipid rafts, cholesterol-rich membrane microdomains, and tetraspanins (e.g., CD9, CD63, CD81) are involved in EV biogenesis, particularly exosomes. They assist in sorting specific cargo into EVs and the budding process | Dixson et al. (2023) |
| Ceramide and Sphingolipids | Ceramide-enriched membrane domains and sphingolipids contribute to EV budding. The generation of ceramide in the plasma membrane induces membrane curvature, facilitating vesicle budding | Peeters et al. (2022) |
| Small GTPases | Proteins like Rho GTPases (e.g., RhoA, Cdc42, ARF6) regulate cytoskeletal dynamics and membrane remodeling for EV biogenesis. They influence vesicle budding and release | Hu et al. (2020) |
| Calcium Signaling | Intracellular calcium levels can modulate EV secretion. Calcium-dependent enzymes, such as calpain and scramblase, play roles in membrane remodeling and vesicle shedding | Catalano and O’Driscoll (2020) |
| Phospholipids and Phosphoinositides | Specific phospholipids and phosphoinositides (e.g., PS, PI3P) contribute to membrane curvature and EV formation | Skotland et al. (2020) |
| Tetraspanin-Enriched Microdomains (TEMs) | TEMs serve as platforms for the assembly of protein complexes involved in EV biogenesis, cargo sorting, and membrane scission | Teng and Fussenegger (2021) |
| Protein Sorting Machinery | Proteins involved in cargo sorting, such as the endosomal protein ALIX and the syndecan-syntenin-ALIX pathway, select specific cargo for incorporation into EVs | Bennett et al. (2020) |
| Regulation by Cellular Stress and Signaling | Cellular stressors like hypoxia, oxidative stress, and inflammation can stimulate or modulate EV production. Signaling pathways like mTOR, p53, and HIF-1α influence EV formation in response to cellular stress | Kuo et al. (2022) |
| Autophagy Machinery | Autophagy-related proteins, particularly during microautophagy, contribute to the formation of EVs containing specific cargo targeted for degradation | Leidal and Debnath (2021) |
| pH and Ion Channels | Changes in intracellular pH and ion channel activity can influence EV formation and secretion | Sheth and Esfandiari (2022) |
The various cellular pathways and processes involved in the formation and secretion of EVs.
3 Nanomaterials
Nanomaterials are engineered or naturally occurring substances with structures at the nanoscale, typically ranging from 1 to 100 nm. Their unique and enhanced physical, chemical, and biological properties arise from their small size, high surface area, and quantum effects, making them ideal for diverse applications (Han and Choi, 2021). Broadly, nanomaterials can be classified into four primary types based on their morphology and composition: Nanoparticles: These are the most commonly studied nanomaterials and include metallic (e.g., gold, silver), metal oxide (e.g., titanium dioxide, zinc oxide), polymeric, and carbon-based particles. Nanoparticles are widely applied in drug delivery, imaging, and antibacterial treatments due to their capacity for targeted delivery and surface functionalization. Nanotubes: Carbon nanotubes (CNTs) are a prominent example, known for their mechanical strength and electrical conductivity. They are utilized in electronic devices, as well as in tissue engineering and biosensing due to their flexibility and biocompatibility. Nanowires: Metallic and semiconducting nanowires, such as those made from silicon or gold, find applications in nanoelectronics, sensors, and photodetectors. Their ability to conduct electrons efficiently makes them valuable in energy storage and conversion devices. Quantum Dots: These are semiconductor nanocrystals that exhibit unique optical properties, such as fluorescence, which vary with their size. They are used in imaging, drug delivery, and as fluorescent markers in biological research and diagnostics.
In terms of contextual applications, nanomaterials are pivotal in medicine, particularly for targeted drug delivery and regenerative medicine, where their controlled release and interaction with biological systems can enhance therapeutic efficacy. In materials science, they improve the properties of composites, making them stronger, lighter, or more flexible. In electronics, nanomaterials facilitate advancements in microelectronics, energy storage, and solar cells. Environmental applications include water treatment, air purification, and environmental sensing. However, their small size also raises concerns regarding toxicity and environmental persistence, making it critical to evaluate their safety and regulatory requirements (Albalawi et al., 2021).
3.1 Classification of nanomaterials
Nanomaterials can be classified into several categories based on their composition, structure, and properties, each with distinct applications and characteristics that make them valuable across various fields.
3.1.1 Nanoparticles
These are solid particles with at least one dimension within the nanoscale (1–100 nm). Examples include: Gold nanoparticles (AuNPs), commonly used in diagnostics and drug delivery due to their biocompatibility and ease of functionalization. Silver nanoparticles (AgNPs), known for their antimicrobial properties and widely used in medical devices and coatings. Titanium dioxide (TiO₂) nanoparticles, frequently used in sunscreens, cosmetics, and photocatalysis applications for environmental remediation.
3.1.2 Nanocomposites
These materials consist of a bulk matrix embedded with nanoscale inclusions to enhance their mechanical, thermal, or electrical properties. Polymer-matrix nanocomposites, where polymers are reinforced with nanoparticles like clay, carbon nanotubes, or graphene, are used in automotive and aerospace components for their strength and light weight. Metal-matrix nanocomposites, such as aluminum reinforced with silicon carbide nanoparticles, are applied in structural materials needing high strength and durability.
3.1.3 Nanoporous materials
These materials contain nanoscale pores, which make them suitable for applications in adsorption, catalysis, and filtration. Zeolites, microporous aluminosilicate minerals used in catalysis, adsorption, and ion-exchange processes. Metal-organic frameworks (MOFs), a class of nanoporous materials with high surface area and tunable pore sizes, are used in gas storage, separation, and drug delivery. Mesoporous silica (MCM-41), which is utilized in catalysis and as a drug delivery vehicle due to its high surface area and stability.
3.1.4 Nanostructured materials
Bulk materials with nanoscale features throughout the structure exhibit enhanced mechanical, optical, and electrical properties. Nanostructured metals, like nanocrystalline copper, are used in wear-resistant coatings and conductive films due to their enhanced hardness and ductility. Nanostructured ceramics, such as nanocrystalline zirconia, are used in dental and orthopedic implants for their strength and biocompatibility. Graphene, a single layer of carbon atoms with a two-dimensional nanostructure, is applied in flexible electronics, sensors, and composite materials due to its high conductivity and strength.
3.1.5 Nanomaterials by composition
These materials are categorized based on their chemical makeup. Carbon-based nanomaterials, including carbon nanotubes and fullerenes, are valued in electronics and composite materials for their electrical conductivity and tensile strength. Metal nanoparticles, like silver, gold, and iron oxide nanoparticles, are used in biomedical applications for imaging, drug delivery, and hyperthermia treatment. Semiconductor nanocrystals, such as quantum dots made from cadmium selenide (CdSe), are utilized in displays, solar cells, and bioimaging for their tunable optical properties.
3.1.6 Nanomaterials by application
Nanomaterials can also be grouped based on their primary applications, facilitating targeted research and development. Medical applications: Gold nanoparticles and iron oxide nanoparticles are used in diagnostics, drug delivery, and imaging. Electronics: Carbon nanotubes and graphene are key in creating flexible electronics, transistors, and sensors. Energy storage and conversion: Nanostructured silicon and lithium iron phosphate nanoparticles are utilized in batteries and fuel cells for improved energy capacity and efficiency. Environmental applications: Titanium dioxide nanoparticles and silver nanoparticles are used in water treatment, antimicrobial coatings, and air purification.
These classifications help to understand and leverage the unique properties of nanomaterials, enabling their tailored use across disciplines, including medicine, electronics, materials science, and environmental sustainability (Han et al., 2020).
3.2 Nanomaterials in therapeutic innovations
This section highlights the significant impact of nanomaterials on medical advancements. It possess unique properties that make them highly advantageous for diverse medical applications. In the realm of drug delivery, nanomaterials serve as carriers for pharmaceutical compounds, safeguarding them from degradation and enabling precise targeting. This enhances therapeutic efficacy while reducing side effects, as drugs can be delivered directly to affected tissues or cells while sparing healthy ones (Lai et al., 2022). Examples of drug delivery platforms employing nanomaterials include liposomes, polymer nanoparticles, and lipid-based nanocarriers (Nasrollahzadeh et al., 2020).
Cancer therapy, in particular, has benefited significantly from nanomaterials, allowing the targeted delivery of chemotherapy drugs to cancer cells while sparing healthy tissue. Additionally, nanoparticles can be engineered to release drugs in response to specific triggers within tumor microenvironments (Meng et al., 2021). Targeted therapies like photodynamic therapy and hyperthermia, where nanomaterials generate heat or light to destroy cancer cells, have shown promise. The field of vaccines has also been revolutionized by nanomaterials, as they can effectively carry antigens to enhance immune responses, potentially leading to more effective vaccines against infectious diseases (Makabenta et al., 2021).
Nanomaterials have made substantial contributions to medical imaging, serving as contrast agents in various imaging modalities such as magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound. Their ability to enhance image quality aids in early and accurate disease detection, assisting clinicians in making informed decisions (Chen et al., 2021).
In regenerative medicine, nanomaterials offer scaffolds that mimic the extracellular matrix, supporting tissue rejuvenation. They can also carry growth factors and bioactive molecules, promoting tissue repair in applications ranging from bone regeneration to wound healing (Tan et al., 2023). Nanomaterials have shown promise in delivering therapeutic agents to the brain, potentially offering new avenues for treating neurodegenerative diseases like Alzheimer’s and Parkinson’s disease, which are notoriously difficult to address due to the blood-brain barrier (Soufi and Iravani, 2020).
Nanomaterials with antibacterial properties have emerged as promising tools in the fight against antibiotic-resistant bacteria and infections (Meng et al., 2023). They can be incorporated into wound dressings, medical implants, or device coatings to prevent infections and improve patient outcomes (Naskar and Kim, 2019). Cardiovascular therapies have also benefited from nanomaterials in the development of drug-eluting stents and as carriers for medications targeting heart diseases (Cassani et al., 2020).
Furthermore, nanomaterials have played a crucial role in gene therapy by facilitating the delivery of nucleic acids for the treatment of genetic disorders, offering hope for previously untreatable conditions (Ma et al., 2021). They have also advanced the field of personalized medicine, enabling therapies tailored to an individual’s genetic or disease profile, maximizing treatment effectiveness (dos Santos et al., 2021).
While the potential of nanomaterials in therapeutics is undeniable, challenges related to safety, scalability, and cost-effectiveness need to be addressed through rigorous testing and regulation (Mundekkad and Cho, 2022). Despite these challenges, nanomaterials have ushered in a new era of therapeutic innovation, offering precision, versatility, and efficiency in the treatment of a wide range of medical conditions. Continued research and development in this field hold great promise for improving patient outcomes and reshaping the healthcare landscape (Pusta et al., 2023).
4 Synergistic integration of nanomaterials with EVs
This section explores the emerging area of research that combines nanomaterials with EVs for potential therapeutic applications in medicine, drug delivery, and diagnostics. EVs are small membranous structures released by cells, which play a crucial role in intercellular communication by carrying bioactive molecules like proteins, nucleic acids, and lipids (Rani et al., 2023). In contrast, nanomaterials are engineered materials with unique properties at the nanoscale that can be tailored for various applications. The integration of nanomaterials with EVs aims to merge the properties and functions of both entities to enhance their therapeutic or diagnostic potential (Niu et al., 2021). This integration holds several promising aspects.
4.1 Enhanced drug delivery
The integration of nanomaterials with EVs significantly enhances drug delivery systems by providing a robust platform for improved precision and efficiency in targeting specific cells or tissues. Nanomaterials can serve as ideal carriers for EVs, protecting them from enzymatic degradation and environmental factors that may compromise their therapeutic efficacy. The surface properties of nanomaterials can also be engineered to facilitate the binding of EVs to target receptors, ensuring that therapeutic molecules are delivered directly to disease sites.
For example, in cancer treatment, EVs loaded with therapeutic molecules, such as small interfering RNAs (siRNAs) or proteins, can be delivered precisely to tumor cells. Nanomaterials like liposomes, gold nanoparticles, and carbon nanotubes can be employed to enhance the stability and drug-loading capacity of EVs, facilitating the co-delivery of multiple therapeutic agents. This ability to co-load various drugs or biomolecules allows for synergistic effects, improving the efficacy of treatment regimens, minimizing the risk of drug resistance, and enabling the treatment of multifactorial diseases. As shown in studies by Meng et al. (2020) and Mondal et al. (2023), the use of nanomaterials for loading EVs can help target hard-to-reach areas and improve overall bioavailability (Meng et al., 2020; Mondal et al., 2023).
4.2 Therapeutic cargo loading
One of the key advantages of integrating nanomaterials with EVs is the ability to control the loading of specific therapeutic cargo during EV biogenesis. This can be achieved by incorporating nanomaterials into the EV membrane or internalizing them within the EV lumen, allowing for the targeted delivery of nucleic acids (such as mRNAs or small RNAs), proteins, and other bioactive compounds. By precisely engineering nanomaterials to interact with EVs, researchers can enhance the specificity and efficiency of therapeutic cargo delivery.
For example, gold nanoparticles and magnetic nanoparticles can be used to guide the EVs to desired locations within the body, ensuring that they carry out their therapeutic function only at the target site. Moreover, the use of nanomaterials in the engineering of EVs allows for the co-delivery of several different therapeutic agents, providing a multi-pronged approach to therapy. This method not only enhances the efficacy of treatments but also reduces off-target effects, as shown by Yom-Tov et al. (2022) and Tripathi et al. (2023), where custom-engineered EVs facilitated controlled drug release and minimized systemic toxicity (Yom-Tov et al., 2022; Tripathi et al., 2023).
4.3 Stability and longevity
A major limitation of EV-based therapeutics is their susceptibility to degradation during storage, transport, and in vivo circulation. Nanomaterials can address this challenge by providing protective barriers for EVs, enhancing their stability and longevity. By coating or encapsulating EVs with nanomaterials, it is possible to shield them from harsh environmental conditions such as high temperatures, enzymatic degradation, and oxidative stress.
Nanomaterials, such as silica nanoparticles, lipid nanoparticles, and polymeric nanocarriers, have been shown to enhance the shelf life and stability of EVs, ensuring that they retain their therapeutic cargo’s integrity until they reach their target site. Additionally, nanomaterials help to prevent aggregation, which can occur when EVs are exposed to external stresses, improving their therapeutic efficacy upon delivery. As reported by Paolillo et al. (2021) and Yaraki et al. (2022), this integration significantly extends the shelf-life of EVs and ensures that their therapeutic potential remains intact over time (Paolillo et al., 2021; Yaraki et al., 2022).
4.4 Imaging and diagnostics
Nanomaterials offer powerful tools for the imaging and tracking of EVs in vivo, enabling real-time monitoring of their distribution and therapeutic effects. By integrating nanomaterials such as quantum dots, gold nanoparticles, or superparamagnetic iron oxide nanoparticles (SPIONs) into EVs, researchers can enhance the visualization and detectability of EVs using various imaging modalities, including fluorescence imaging, magnetic resonance imaging (MRI), and computed tomography (CT).
This capability is especially valuable in clinical diagnostics and biomedical research, where tracking the biodistribution of EVs can provide insights into their therapeutic efficacy and potential side effects. For instance, Liu Q. et al. (2022) demonstrated the use of fluorescent nanomaterials to track EVs in cancer models, offering a non-invasive approach to monitor EV delivery in real-time. The ability to visualize EVs can also aid in determining the best time and dosage for EV-based therapies, improving treatment outcomes (Liu Q. et al., 2022).
4.5 Immunomodulation
Nanomaterials integrated with EVs can be utilized to modulate the immune system’s response, offering a potential strategy for therapeutic interventions in autoimmune diseases, inflammation, and cancer immunotherapy. Nanomaterials can be engineered to enhance the immunomodulatory properties of EVs, such as boosting the ability of EVs to interact with immune cells or modulating their immunosuppressive effects.
For example, the incorporation of gold nanoparticles or lipid-based nanomaterials into EVs has been shown to enhance their ability to stimulate immune responses, thereby promoting antitumor immunity or enhancing vaccine efficacy. Conversely, EVs can be engineered with nanomaterials to carry immunosuppressive cargo, which could be beneficial in conditions where dampening the immune response is desired, such as in autoimmune diseases. Cheng et al. (2021) and Liu Z. et al. (2023) demonstrated how the combination of nanomaterials and EVs could be used to control immune responses with high precision, opening up new avenues for immunotherapies (Cheng et al., 2021; Liu Z. et al., 2023).
4.6 Tissue engineering
The integration of nanomaterials with EVs has significant potential in tissue engineering and regenerative medicine, particularly for promoting tissue repair and regeneration. Nanomaterials can serve as scaffolds or delivery systems for EVs, ensuring that bioactive molecules are efficiently delivered to damaged tissues, thereby accelerating the healing process. For example, the combination of nanomaterials such as hydrogels, nanofibers, and nanoparticles with EVs can provide both structural support and bioactive cues for cell proliferation and tissue regeneration.
Trubiani et al. (2019) and Ju et al. (2022) have explored how EV-loaded nanomaterials can be used in bone and cartilage regeneration, where nanomaterials help to direct the EVs to the site of injury, enhancing the regenerative potential of EVs. This synergistic approach not only promotes tissue repair but also improves the overall efficacy of regenerative therapies (Trubiani et al., 2019; Ju et al., 2022).
4.7 Safety and toxicity considerations
While the integration of nanomaterials with EVs holds great promise, it is essential to thoroughly assess the safety and biocompatibility of these systems. The long-term effects of nanomaterials on human health and the environment must be carefully evaluated to mitigate potential risks. Toxicological studies are needed to understand the potential cytotoxicity, immunogenicity, and biodistribution of the nanomaterials when integrated with EVs.
Researchers are exploring methods to design biocompatible nanomaterials that are easily excreted from the body and do not accumulate in vital organs. In addition, the impact of these integrated systems on immune function, organ health, and overall system toxicity should be systematically studied. Cheng et al. (2018), El Nahrawy et al. (2021), and Herrmann et al. (2021) highlight the importance of safety profiles in nanomaterial-EV therapeutics, which will be essential for translating these systems into clinical applications (Cheng et al., 2018; El Nahrawy et al., 2021; Herrmann et al., 2021).
The synergistic integration of nanomaterials with EVs represents an exciting frontier in biomedical research, with the potential to revolutionize various aspects of medicine and healthcare. However, further research and development are needed to fully unlock the clinical potential of this approach (Rufino-Ramos et al., 2017).
5 Characterization methods for integration of nanomaterials with EVs
Characterizing the integration of nanomaterials with EVs is essential for understanding their properties, behaviour, and potential applications in various fields. Numerous characterization approaches could be employed to assess these integrated systems which are given below.
5.1 Transmission electron microscopy (TEM)
TEM is an authoritative imaging technique for characterizing nanomaterial-EVs complexes with exceptional detail. By using a attentive beam of electrons, TEM gives the ultra-high resolution images that unveil the intricate features of these integrated structures. Researchers could exactly determine the size, shape, and arrangement of nanomaterials within EVs, shedding light on their morphology and distribution. This microscopic vision is precious for understanding how nanomaterials and EVs interact at the nanoscale, providing crucial information that underpins the development of novel therapeutic strategies and biomedical applications (Murugesan, 2021).
5.2 Scanning electron microscopy (SEM)
SEM is a valuable tool for characterizing EVs-nanomaterial complexes, particularly when it comes to assessing their surface properties. SEM produces high-resolution images by scanning an electron beam across a sample’s surface. Nanomaterial-EV complexes can be characterized based on their surface morphology, texture, and features by this technique. Scientists can gain a deeper understanding of EV stability and cellular uptake by studying their surface characteristics. In a variety of biomedical applications, SEM’s ability to provide detailed surface information is crucial for optimizing design and functionality. (Noble et al., 2020).
5.3 Dynamic light scattering (DLS)
In solution, DLS is an effective technique for characterizing nanomaterial-EV complexes. DLS provides crucial information about particle size distribution and hydrodynamic diameter by analysing the fluctuations in scattered light caused by Brownian motion. As nanomaterials are integrated with EVs, DLS assists researchers in determining the dimensions of these integrated structures. Physiological and experimental settings require dynamic data to understand their stability, dispersibility, and interactions. DLS enables precise size measurements and aids in optimizing the design of these complexes for targeted therapeutic delivery and other biomedical applications (Tiwari et al., 2021).
5.4 Zeta potential analysis
Zeta Potential Analysis is a valuable method for assessing the surface charge properties of nanomaterial-EVs complexes. By quantifying the electrical charge at the particle’s surface when suspended in a solution, it exposes vibrant information about their stability and propensity for aggregation. A high positive or negative zeta potential proposes repulsion between particles, hindering aggregation and promoting stability. Equally, a low zeta potential can indicate the potential for particles to aggregate or clump together. This characterization method is precious for forecasting the behaviour of nanomaterial-EVs complexes in various environments, aiding researchers in optimizing their design for targeted drug delivery, imaging, and other biomedical applications (Midekessa et al., 2020).
5.5 Fourier transform infrared spectroscopy (FTIR)
Fourier Transform Infrared Spectroscopy (FTIR) is a prevailing analytical technique used to find the chemical composition of nanomaterial-EVs complexes. By subjecting these complexes to infrared radiation, FTIR perceives the specific vibrational frequencies of chemical bonds and functional groups existing in the sample. It provides a complete molecular fingerprint, allowing researchers to identify and quantify the numerous constituents within the nanomaterial-EVs complexes. FTIR aids in discriminating critical information about the structural modifications, surface functionalization, or chemical interactions which may occur during the integration of nanomaterials with EVs (Di Santo et al., 2022).
5.6 X-ray diffraction (XRD)
X-ray Diffraction (XRD) is a powerful technique for probing the crystallographic characteristics of nanomaterials encapsulated EVs. By exposing the sample to X-rays and analysing the resultant diffraction pattern, XRD could precisely determine the arrangement and spacing of atoms within crystalline structures. This information is precious in understanding the structural integrity and phase composition of nanomaterial-EVs complexes. Researchers could assess whether nanomaterials maintain their crystalline properties post-integration, which is critical for predicting their stability and functionality in various applications, from drug delivery to catalysis and beyond. XRD contributes crucial insights into the behaviour of nanomaterial-EVs complexes at the atomic and molecular level (Paisrisarn et al., 2022).
5.7 Nuclear magnetic resonance (NMR) spectroscopy
NMR Spectroscopy is a adaptable analytical technique employed to gain perceptions into the chemical structure, dynamics, and interactions within nanomaterial-EVs complexes. NMR exploits the magnetic properties of certain atomic nuclei, exposing their specific environments within a sample. In the integration of nanomaterials with EVs, NMR could identify and characterize the chemical constituents of both components. It could elucidate how nanomaterials and EVs interrelate on a molecular level, provides data on binding affinities, conformational changes, and intermolecular forces. NMR is essential for considerate the intricacies of these integrated systems, aiding researchers in enhancing their design for diverse applications in biomedicine, materials science, and beyond (Nielsen et al., 2021).
5.8 Fluorescence and confocal microscopy
Fluorescence and Confocal Microscopy are essential tools for examining the behaviour of nanomaterial-EVs complexes within biological systems. These techniques control the intrinsic or fluorescently labelled properties of the nanomaterials or EVs to visualize their uptake and intracellular localization in real-time. By enlightening the interactions between these complexes and living cells or tissues, researchers could track their journey by cellular compartments, discerning how they are internalized, trafficked, and whether they reach specific target sites. This information is essential for optimizing the design of nanomaterial-EV systems for drug delivery, imaging, or therapeutic applications, eventually enhancing our understanding of their behaviour within complex biological environments (Shimomura et al., 2021).
5.9 Mass spectrometry (MS)
MS is a vital analytical technique hired to delve into the cargo content of EVs and monitor any alterations resulting from their integration with nanomaterials. Through ionizing and separating molecules based on their mass-to-charge ratios, MS could precisely identify and quantify the proteins, lipids, nucleic acids, and metabolites carried by EVs. This technique allows researchers to examine the cargo composition and assess whether nanomaterial integration induces any changes, shedding light on potential modifications or cargo loading efficiency. MS plays a vital role in interpreting the functional and therapeutic potential of nanomaterial-EVs complexes, guiding their optimization for various biomedical applications (Jalaludin et al., 2023).
5.10 Biological assays
Biological assays are crucial for assessing the functional aspects and safety profile of nanomaterial-EVs complexes within biologically relevant contexts. Cell viability assays provides critical insights into the biological activity and possible toxicity of these integrated systems. By exposing cells to nanomaterial-EVs complexes and measuring their impact on cell viability and proliferation, researchers could assess whether these complexes encourage cytotoxicity or adversely affect cellular health. Such assays are essential for defining the biocompatibility of these complexes and guiding their safe use in various biomedical applications, from drug delivery to regenerative medicine, confirming that they have a positive impact on biological systems (Nguyen et al., 2020).
5.11 Spectroscopic techniques
Spectroscopic techniques, together with ultra violet -visible (UV-Vis) spectroscopy, Raman spectroscopy, and fluorescence spectroscopy, provides valuable insights into the optical properties and interactions of nanomaterial with EVs. UV-Vis spectroscopy dealings the absorption of light by these complexes, exposing the information about their electronic structure and composition. On the other hand, Raman spectroscopy provides information about molecular vibrations within complexes, allowing chemical bonds and structural changes to be identified. After excitation, fluorescence spectroscopy utilizes the emitted light to determine fluorescence properties and biomolecular interactions. A variety of biomedical and materials science applications demand the use of these spectroscopic methods to characterize and optimize nanomaterial-EV systems (Imanbekova et al., 2022).
5.12 Electrophoretic techniques
In order to evaluate the stability and electrophoretic mobility of nanomaterial-EV complexes, electrophoretic techniques, with gel electrophoresis, are indispensable. When subjected to an electric field, gel electrophoresis separates these complexes according to their size and charge, providing vital information about their structure and dispersion. Researchers could determine whether nanomaterial-EVs complexes have aggregated or degraded by analyzing their migration patterns in a gel matrix. Nanomaterial-EV complexes are essential for targeted drug delivery, diagnostics, and other biomedical applications (Yang et al., 2020).
5.13 Quantitative PCR (qPCR)
qPCR is a powerful molecular biology technique used to investigate how nanomaterial-EV complexes alter gene expression. Through the measurement of gene levels, qPCR provides valuable insight into the biological effects of these integrated systems. Nanomaterial-EV complexes are shown to influence cellular processes, including signaling pathways, immune responses, and other essential functions. Using this information, we can develop tailored biomedical interventions and advance our understanding of their interactions with biological systems as well as understand the therapeutic or regulatory impact of these complexes (Fauth et al., 2019).
5.14 Proteomic and lipidomic analysis
A proteomic and lipidomic analysis is a sophisticated method of dissecting EVs molecular composition and examining the changes caused by nanomaterial integration. To conduct proteomics, it is necessary to identify and quantify the proteins present in EVs. Additionally, lipidomics focuses on determining the lipid content of these vesicles. By encapsulating nanomaterials with EVs, these techniques can detect changes in protein and lipid compositions. In order to understand what effects nanomaterial integration may have on therapeutic potential, EV stability, or functionality, this is crucial. Our understanding of the complex interactions between nanomaterials and EVs is improved by proteomic and lipidomic analyses, which guide the optimization of EVs for various biomedical applications (Wang T. et al., 2023).
5.15 Characterization methods of EVs proteins
Characterizing EVs proteins is crucial for understanding their composition and functions. Common methods include Western Blotting, which uses specific antibodies to detect proteins; Enzyme-Linked Immunosorbent Assay (ELISA) for quantification; Mass Spectrometry, which identifies and quantifies proteins through mass analysis of peptides; Flow Cytometry, allowing analysis of EVs based on size and surface proteins; Immunoelectron Microscopy for nanoscale visualization of EVs and their protein content; Nanoparticle Tracking Analysis (NTA) for measuring size and concentration; Transmission Electron Microscopy (TEM) for high-resolution imaging; Protein Arrays for simultaneous screening of multiple proteins; Immunoprecipitation (IP) for isolating target proteins; Size-Exclusion Chromatography (SEC) for EV subpopulation separation; Surface Plasmon Resonance (SPR) for analyzing protein interactions; and Proteomic Analysis (e.g., LC-MS) for comprehensive proteome identification. Researchers often combine these techniques based on research goals and equipment availability to comprehensively characterize EV protein composition.
6 Integration of nanomaterials with EVs for advanced biomedical applications
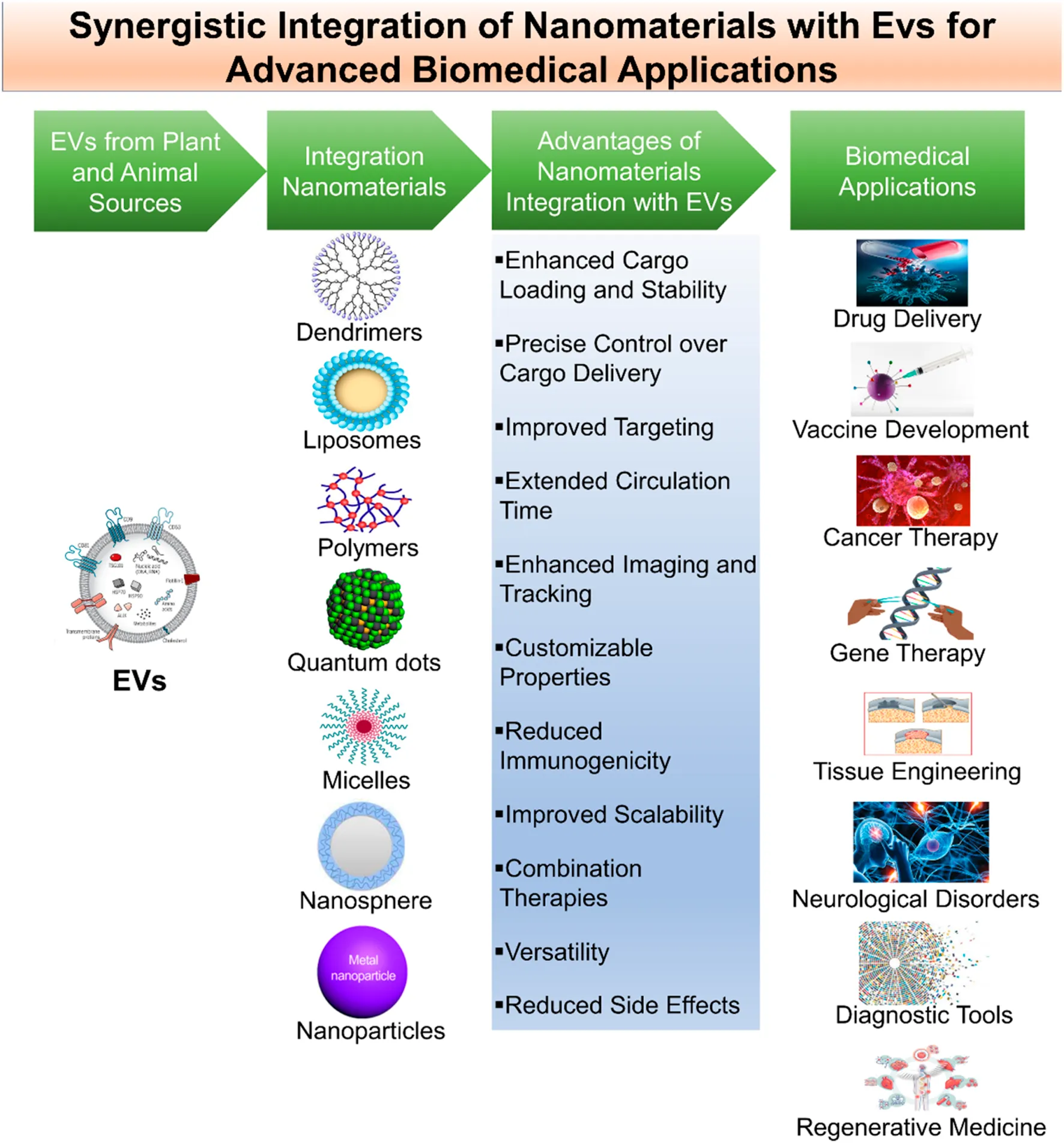
The synergistic integration of nanomaterials with EVs are emerging as an innovative and dynamic approach that has been profound implications for advanced biomedical application (Table 5) (Figure 3) (Yang et al., 2022). This synergistic integration epitomizes a growing field at the intersection of biomedicine, drug delivery, and nanotechnology, promising transformative solutions to a variety of healthcare challenges (Li et al., 2021). Accordingly, this approach harnesses their combined potential. Nanomaterials, including nanoparticles, liposomes, quantum dots, and other engineered carriers offers multifunctionality and versatility, while EVs provides natural targeting competences and a biocompatible delivery system. Moreover, this approach amplifies therapeutic and diagnostic potential of both components, leading to improved consequences in the advanced biomedical applications (Wang et al., 2021).
TABLE 5
| S. No. | EVs Sources | Materials | Preparation methods | Disease | Study done | Applications | References |
|---|---|---|---|---|---|---|---|
| 1 | MSC | Gelatin-based hydrogels | Embedding hybrid EVs-liposome (hEL) NVs in gelatin-based hydrogels | Tissue regeneration | In vitro | Efficient delivery of microRNAs (miRNAs) for gene expression regulation in 3D bioprinted tissues | (Elkhoury et al., 2022) |
| 2 | Natural grapefruit | Heparin-based nanoparticles (DNs) with doxorubicin | Patching DNs onto the surface of EVs | Glioma | In vitro and in vivo | Drug delivery and antiglioma efficacy enhancement | (Niu et al., 2021) |
| 3 | Genetically engineered mammalian cells | Gold nanoparticles (AuNPs) | Surface modification of AuNPs using mechanical method or extrusion with brain-targeted exosomes | Brain targeting | In vitro and in vivo | Targeted delivery to brain cells for theranostic applications | (Khongkow et al., 2019) |
| 4 | Macrophages | Superparamagnetic iron oxide nanoparticles (SPIONs) and curcumin (Cur) | Loading SPIONs and Cur into exosomes, followed by conjugation with neuropilin-1-targeted peptide (RGERPPR, RGE) using click chemistry | Glioma | In vitro and in vivo | Glioma-targeted exosomes with imaging and therapeutic functions for diagnostic and therapeutic purposes | (Jia et al., 2018) |
| 5 | Neuro2A cells | Nanobodies specific for epidermal growth factor receptor (EGFR) conjugated to phospholipid (DMPE)-PEG derivatives | Decorating EVs with nanobody-PEG-lipids to confer targeting specificity | Tumor cells | In vitro and in vivo | Improved cell-specific drug delivery and prolonged circulation time for EVs | (Kooijmans et al., 2016) |
| 6 | Leaf extract of Phyllanthus niruri-apoplastic fluid | Leaf extract of Phyllanthus niruri (GS-AgNP-LEPN) | Green synthesis method using LEPN as a reducing and capping agent; Encapsulation of GS-AgNP-LEPN in EVs (nanovesicles) from apoplastic fluid (APF) | Citrus canker | In vitro | Potential treatment for citrus canker | (Gaurav et al., 2023) |
| 7 | SCC9 cells | Chrysin and gold nanoparticles (AuNPs) | Synthesis of EVs containing chrysin; Carrying AuNPs by EVs (Au-EVs) | Tongue squamous cell carcinoma (TSCC) | In vitro and in vivo | Potential TSCC treatment with Au-EVs | (Yang et al., 2021b) |
| 8 | MSC | Heat shock proteins 70 (HSP70) highly expressed EVs encapsulated with Te nanoparticles (Te@EVsHSP70) | Tumor cells used as bioreactors for intracellular synthesis of Te nanoparticles; NIR irradiation to upregulate HSP70 expression and exocytosis for engineered Te@EVsHSP70 | Tumor photothermal therapy triggering improved immunotherapy | In vitro and in vivo | Multifunctional EVs-based drug delivery system for photothermal-triggered tumor immunotherapy | (Li et al., 2023b) |
| 9 | Bacterial cultures | PEGylated MoS2-ZnO (MZ) nanocomposite cloaked with Lactobacillus paracasei-derived extracellular vesicle (LPEV) | Characterization of MZ nanocomposite; Coating of MZ with LPEV; Antibacterial activity against Staphylococcus aureus; Mechanisms of action; Biocompatibility and selectivity | Antibacterial activity against Staphylococcus aureus | In vitro | Development of synergistic nanoantibiotics | (Naskar et al., 2022) |
| 10 | MDA-MB-231 cells | Biomimetic nanoparticle platform for systemic and intracellular delivery of proteins | Caging guest proteins in metal-organic frameworks (MOFs); Decoration with EV membrane; In vitro and in vivo studies; Tumor growth inhibition | Intracellular delivery of biofunctional enzymes or therapeutic proteins | In vitro and in vivo | Systemic and intracellular delivery of proteins | (Cheng et al., 2018) |
| 11 | Ginger | Electrodynamic Pd-Pt nanosheets | Integration of Pd-Pt nanosheets and ginger-derived EVs; Prolonged blood circulation and accumulation at infection sites; EV lipid-dependent entry into bacteria; Sustainable ROS generation; Synergistic electrodynamic and photothermal therapy | Anti-infective therapy | In vitro and in vivo | Biomimetic nanoparticles for anti-infective therapy | (Qiao et al., 2022) |
| 12 | Macrophage | Tumor-targeting folate (FA)-modified EVs with protoporphyrin X (PpIX) and doxorubicin (DOX) | In situ biosynthetic approach for drug encapsulation in EVs; High drug-loading efficiency with minimal perturbations; Enhanced accumulation and penetration in tumors; Strengthened immune response | Photochemotherapy | In vitro and in vivo | Biomedicine applications of biosynthetic EVs | (Li et al., 2021) |
| 13 | KB cell line | Zinc oxide (ZnO) nanocrystals | Encapsulation of ZnO nanocrystals in extracellular vesicles; Biomimetic and stable Trojan nano-horses (TNHs) | Cancer theranostics | In vitro and in vivo | Biomimetic platform for nanotheranostics | (Dumontel et al., 2019) |
| 14 | 4T1 cells | Cationic polymer nanoparticles (cNPs) | Formation of cNP@EVs through exocytosis; Autophagy-mediated exocytosis; Intercellular transportation of nanoparticles; Enhanced penetration and antitumor activity | Nanoparticle-cell interactions | In vitro and in vivo | Clinical application of EV-mediated nanoparticle transportation | (Shang et al., 2023) |
| 15 | Breast cancer cells | Quercetin-iron complex nanoparticle-loaded EVs | Preparation of nanoparticle-loaded EVs using direct flow filtration; Characterization of loaded EVs; Protein marker analysis; Cellular uptake studies | Drug delivery and tracking after delivery | In vitro and in vivo | Production of nanoparticle-loaded EVs and cellular uptake studies | (Mansur et al., 2023) |
| 16 | Engineered cancer cells | Gold-polydopamine (PDA) core–shell nanoparticles decorated with doxorubicin (Dox), glucose oxidase (GOx), and miR-21-indicative DNA tags | Extraction of EVs with surface N-glycans cut and intracellular microRNA-21 (miR-21) silenced from engineered cancer cells; Coating of gold-PDA nanoparticles with EVs; Loading of Dox, GOx, and miR-21-indicative DNA tags | Cancer cell targeting and killing | In vitro | Targeted and cascaded cancer cell killing | (Wu et al., 2023a) |
| 17 | MSC | Iron oxide nanoparticle (IONP)-incorporated exosome-mimetic nanovesicles (NV-IONP) | Fabrication of NV-IONP from IONP-treated hMSCs; Increased therapeutic growth factor content; In vivo systemic injection with magnetic guidance | Spinal cord injury treatment | In vitro and in vivo | Repairing injured spinal cord | (Kim et al., 2018) |
| 18 | Engineered lipid-hybridized EVs | Layer-by-layer (LbL) assembly for incorporation of doxorubicin (DOX) | Loading of siRNA into eEVs; Incorporation of DOX via LbL assembly | Cancer therapy | In vitro and in vivo | Targeted delivery of multiple therapeutics for cancer treatment | (Jhan et al., 2021) |
| 19 | iRGD-modified EVs | siS100A4-loaded iRGD-modified EVs (siS100A4-iRGD-EVs) | Engineering of siS100A4-iRGD-EVs nanoparticles; Protection of siRNA from RNase degradation; Enhanced cellular uptake; Attenuation of lung metastases in breast cancer model | Postoperative breast cancer metastasis prevention | In vitro and in vivo | Preventing postoperative breast cancer metastasis | (Pan et al., 2023) |
| 20 | Hepatocellular carcinoma cells | Gold oxide nanoparticles (GOD-ESIONs@EVs) | Surface engineering of EVs for sequential nanocatalysts; Active targeting with arginine-glycine-aspartic acid (RGD); Intracellular endocytosis; Stimulation of apoptosis and necrosis via ROS generation | Hepatocellular carcinoma treatment | In vitro and in vivo | Therapeutic nanocatalytic treatment of hepatocellular carcinoma | (Wu et al., 2021) |
| 21 | MSC | GMNPs decorated with poly(ethylene glycol) (PEG)-aldehyde (CHO) | Construction of GMNPs; Isolation of BMSC-EVs; Selection of miR-150-5p; DO rat model; Preparation of GMNPE; Co-culture with osteoblasts; Promotion of osteogenesis; Enhanced delivery of miR-150-5p to osteoblasts | Diabetic osteoporosis (DO) | In vitro | Drug delivery for diabetic osteoporosis prevention | (Xu et al., 2023a) |
| 22 | Non-small cell lung carcinoma cells | Doxorubicin (DOX) and lonidamine (LND) | Loading of DOX and LND into EVs; Enhanced cytotoxicity and reduced drug dose; Direct fusion of EVs with cancer cell membranes; Synergistic effects on cancer cell proliferation inhibition | Lung cancer | In vitro and in vivo | Enhanced lung cancer treatment | (Li et al., 2022b) |
| 23 | MSC | Iron oxide nanoparticles (IONP)-harboring MSC | Preparation of MNV from IONP-treated MSC; Enhanced therapeutic growth factor content; Targeting to ischemic lesion; Promotion of anti-inflammatory response, angiogenesis, and anti-apoptosis; Improved therapeutic outcome | Ischemic stroke | In vitro and in vivo | Improved treatment for ischemic stroke | (Kim et al., 2020) |
| 24 | MSC | Diels-Alder crosslinked hyaluronic acid/PEG (DAHP) hydrogel | Development of injectable DAHP hydrogel; Sustained release of MSC-sEVs; Enhanced therapeutic functions of sEVs; Improved efficacy for osteoarthritis (OA) treatment | Osteoarthritis (OA) | In vitro and in vivo | Sustained delivery for OA therapy | (Yang et al., 2021a) |
| 25 | Non-small cell lung carcinoma cells | Palladium (Pd) catalysts | Loading of Pd nanosheets into cancer-derived exosomes; Pd-triggered dealkylation reactions; Preferential tropism for cancer cells | Cancer | In vitro and in vivo | Targeted therapy for cancer using exosome-directed catalyst prodrug therapy | (Sancho-Albero et al., 2019) |
| 26 | Broccoli | Poly (lactic-co-glycolic acid) (PLGA) encapsulated astaxanthin (AST@PLGA) nanoparticles | Preparation of AST@PLGA nanoparticles; Coating with BEVs; Optimization of drug loading (DL); Characterization of AST@PLGA@BEVs nanoparticles; In vitro anticancer activity evaluation | Anticancer | In vitro and in vivo | Drug delivery for anticancer therapy | (Li et al., 2022a) |
| 27 | Bone marrow cells | Ureido-pyrimidinone (UPy) units coupled to poly(ethylene glycol) chains (UPy-hydrogel) | Use of UPy-hydrogel as a delivery platform for EVs; Measurement of sustained EV release; Functional capacity of released EVs; In vivo administration and EV retention evaluation | Regenerative medicine | In vitro and in vivo | Local delivery of EVs for regenerative medicine | (Mol et al., 2019) |
| 28 | Platelet cells | Resveratrol (RES)-loaded MSNs | Synthesis of GelMA/SFMA composite hydrogels; Loading of RES into MSNs; Combination with PDEVs; In vitro biocompatibility and functional studies; Diabetic mouse wound model and therapeutic evaluation | Diabetic wounds | In vitro and in vivo | Wound dressings for diabetic wound treatment | (Zhu et al., 2022) |
| 29 | MSC | Not specified | Identification of aging-induced vascular dysfunction mechanism; Therapeutic effect of miR-675; Encapsulation of exosomes in silk fibroin hydrogel; In vitro and in vivo studies for functional evaluation | Aging-induced vascular dysfunction (Mouse model) | In vitro and in vivo | Local delivery of exosomes to prevent aging-induced vascular dysfunction | (Han et al., 2019) |
| 30 | MSC | Not specified | Enhancement of stability and retention of exosomes in chitosan hydrogel; Evaluation of endothelium-protective and proangiogenesis abilities in vitro; Therapeutic effects in a murine hindlimb ischemia model | Hindlimb ischemia | In vitro and in vivo | Local delivery of exosomes for hindlimb ischemia treatment | (Zhang et al., 2018) |
| 31 | MSC | Poly(lactide) (3D-PLA) | 3D printing of PLA with hGMSCs and EVs; Evaluation of osteogenic and angiogenic marker expression in vitro; Implantation in rat calvaria defects; Histological and MicroCT analysis | Osteoangiogenesis commitment | In vitro and in vivo | Bone tissue regeneration | (Pizzicannella et al., 2019) |
| 32 | Human adipose-derived stem cells | Poly(lactic-co-glycolic acid) (PLGA) scaffolds | Immobilization of exosomes on PLGA/pDA scaffolds; In vitro assessment of effects on osteogenic, proliferation, and migration capabilities; In vivo evaluation in a mouse calvarial defect model | Bone regeneration | In vitro and in vivo | Bone tissue engineering | (Li et al., 2018) |
| 33 | Human Induced Pluripotent Stem Cells | Poly(glycerol sebacate) acrylate-based polymers | Design of a controlled release system for EVs delivery to the cardiac tissue; Evaluation of polymer biocompatibility and release kinetics; Development of freeze-dried EV formulations for controlled release; Release of bioactive EVs for an extended period of time | Chronic heart failure | In vitro and in vivo | Cardiac repair | (Hamada et al., 2020) |
| 34 | MSC | Sodium alginate hydrogel | Determination of optimal alginate hydrogel for sEVs release and rheology; Evaluation of sEVs retention in the heart ex vivo; Analysis of immunoregulation and angiogenesis effects; Assessment of cardiac function and infarct size after myocardial infarction | Myocardial infarction | In vitro | Cell-free therapy for myocardial infarction | (Lv et al., 2019) |
| 35 | MSC | Clickable polyethylene glycol (PEG) macromeres | Formation of EV-encapsulated PEG hydrogels via click reaction; In vivo tracking of labeled EVs; Evaluation of antifibrosis, anti-apoptosis, and regenerative effects in rat model of chronic liver fibrosis | Chronic Liver Failure | In vitro and in vivo | Hepatic Regeneration | (Mardpour et al., 2019) |
| 36 | MSC | Collagen matrix | Encapsulation of EVs in collagen matrix; Evaluation of EV stability and release; Assessment of EV retention in AKI model; Investigation of therapeutic effects in AKI model | Acute Kidney Injury (AKI) | In vitro and in vivo | Experimental AKI Treatment | (Liu et al., 2020) |
| 37 | MSC | RGD hydrogels | Development of RGD hydrogels to enhance EV efficacy; In vivo tracking of labeled EVs; Assessment of EV-hydrogel interaction; Evaluation of therapeutic effects in AKI models | Acute Kidney Injury (AKI) | In vitro and in vivo | Kidney Repair | (Zhang et al., 2020) |
Integration of Nanomaterials with EVs for advanced biomedical applications.
FIGURE 3

Synergistic of integration of nanomaterials with EVs. This figure depicts the integration of nanomaterials with EVs for advanced biomedical applications. It illustrates the synergy between these two components to achieve various biomedical and therapeutic applications.
Research and development (R&D) in this field encompass various stages, starting with the isolation of EVs from various cell sources (both animal and plant cells) and biological fluids. Numerous techniques employed to obtain pure and functional EVs which includes ultracentrifugation, filtration, size exclusion chromatography, and immunoaffinity capture (Sidhom et al., 2020). Consequently, the loading of nanomaterials into EVs is an essential step, involving several strategies to professionally encapsulate these carriers within EVs. This process confirms that the therapeutic payloads are safely loaded into EVs and ready for targeted delivery. Evaluation of integration success, researchers utilized several characterization methods such as transmission electron microscopy, dynamic light scattering, and Western blotting which techniques are enabling the validation of nanomaterial integration with EVs and offer insights into their structure and stability. Besides, biological compatibility and safety considerations are supreme, necessitating comprehensive assessments of toxicity, immunogenicity, and stability in relevant biological environments (Wang Z. et al., 2023).
Surface modification approaches are also discovered to improve the targeting specificity of EVs-nanomaterial complexes for various biomedical applications. By engineering the surface properties of these hybrids, researchers can tailor their interactions with specific cell types or tissues, thereby enhancing their therapeutic efficacy and reducing off-target effects (Tian et al., 2022). The applications of EV-nanomaterial hybrids are extensive and continue to expand. They encompass targeted drug delivery, in vivo imaging, regenerative medicine, cancer therapy, and vaccine development. By leveraging the natural targeting abilities of EVs and the multifunctionality of nanomaterials, these hybrid systems hold the potential to revolutionize the treatment and diagnosis of various diseases (Liu R. et al., 2023). Nonetheless, several challenges, such as scalability, standardization, and safety, must be addressed for the clinical translation of these promising innovations. Despite these hurdles, the synergistic integration of nanomaterials with EVs represents a rapidly evolving and highly promising field in biomedical research, offering new avenues for precision medicine and improved healthcare outcomes (Table 1) (Wu Q. et al., 2023).
The research by Elkhoury et al. (2022) explores a groundbreaking approach to enhance the potential of additive manufacturing for tissue engineering. Traditional 3D-printed tissues have limitations when it comes to influencing the behavior of the cells they contain, especially in terms of delivering crucial gene expression regulators like microRNAs (miRNAs). To overcome this challenge, the researchers incorporated extracellular vesicles (EVs), which are naturally occurring nanovesicles, into bioinks used in 3D bioprinting. miRNA could be delivered to cells without impairment through EVs due to their excellent biocompatibility, rapid endocytosis capabilities, and low immunogenicity. In order to improve the control and release of these EVs, liposomes combined with them. EV-liposome hybrid nanovesicles (hEL) compressed in gelatin-based hydrogels molded bioinks that effectively encapsulated and delivered miRNA to their target sites. This breakthrough permissible for the accurate regulation of gene expression within a 3D bioprinted matrix, confirming not only excellent shape fidelity but also high cell viability in the engineered tissues.
The integration of these innovative regulatory factor-loaded bioinks has the possibilities to intensify the development of new bioprinting applications in the field of tissue engineering. It describes an synergistic integration of nanomaterials, such as EVs and liposomes, with bioinks to overcome venerable challenges in delivering gene expression regulators, eventually advancing the possibilities for effective tissue regeneration and biomedical applications. In 2021, Niu et al. (2021) established an advanced glioma therapy drug delivery approach. They integrated grapefruit EVs with doxorubicin-loaded heparin-based nanoparticles (DNs) to create biomimetic EV-DNs. This strategy, known as “patching,” improved drug loading capability by four-fold compared to conventional methods. Biomimetic EV-DNs effectively crossed the blood-brain barrier (BBB) and penetrated glioma tissues, thanks to receptor-mediated transcytosis and membrane fusion. This approach improved cellular uptake, anti-proliferative effects, and circulation time. In vivo results demonstrated significant accumulation in glioma tissues, promising a breakthrough in challenging glioma therapy by overcoming critical delivery barriers.
Khongkow et al. (2019) introduced an innovative biomedical approach focusing on enhancing gold nanoparticles’ (AuNPs) ability to breach the blood-brain barrier for precise brain cell targeting. They combined the unique characteristics of extracellular vesicle-derived membranes with synthetic AuNPs, creating a novel nanomaterial for brain cell delivery. Brain-targeted exosomes, obtained from genetically engineered mammalian cells, were integrated onto synthetic AuNPs’ surfaces using mechanical or extrusion methods. This led to specialized nanomaterial development with enhanced targeting capabilities, as demonstrated by binding to brain cells under laminar flow conditions. The modified AuNPs also showed improved blood-brain barrier transport, signifying a significant achievement in brain drug delivery. In vivo imaging confirmed their brain accumulation, promising advanced neurological therapies and diagnostics through brain-targeted exosome-coated AuNPs. This research offers an effective and innovative strategy for efficient brain targeting in biomedical applications (Khongkow et al., 2019).
Jia et al. (2018) tackled glioma treatment challenges by introducing engineered EVs as targeted drug delivery carriers. Early glioma detection and overcoming the blood-brain barrier (BBB) for drug delivery are critical issues. Exosomes, with their cargo capacity and BBB-crossing ability, serve as ideal candidates. Researchers loaded superparamagnetic iron oxide nanoparticles (SPIONs) and curcumin into EVs, modifying their membrane with a neuropilin-1-targeted peptide. This engineered EV system effectively crossed the BBB, providing targeted imaging and therapy for glioma. Combining SPION-mediated magnetic flow hyperthermia and Cur therapy demonstrated potent synergistic antitumor effects, improving glioma management while minimizing side effects. This innovative approach offers promise for glioma diagnosis and treatment enhancement (Jia et al., 2018).
Kooijmans et al. (2016) tackled the limitations of using extracellular vesicles (EVs) for drug delivery by developing a method to modify EVs with targeting ligands. They used nanobodies specific for the epidermal growth factor receptor (EGFR) conjugated to polyethylene glycol (PEG) and introduced them to EVs through 'post-insertion.’ This process didn't alter EV characteristics but enhanced their cell specificity. Unmodified EVs cleared rapidly from the bloodstream, while modified EVs remained detectable for over 60 min post-injection. This innovation offers improved EV targeting and extended circulation times, promising enhanced drug delivery for biomedical applications without the need to modify EV-secreting cells (Kooijmans et al., 2016).
Gaurav et al. (2023) combat citrus canker, caused by Xanthomonas axonopodis, using an eco-friendly approach. They synthesized silver nanoparticles with Phyllanthus niruri leaf extract (GS-AgNP-LEPN), eliminating the need for toxic reagents. To enhance their efficacy, these nanoparticles were encapsulated in extracellular vesicles (EVs) from leaf apoplastic fluid (APF-EV-GS-AgNP-LEPN). This hybrid was tested against Xanthomonas axonopodis pv., outperforming ampicillin. The treatment works by inhibiting flavin adenine dinucleotide-flavodoxin NADP(H) reductase (FAD-FNR) and Xanthomonas outer protein AI (XopAI) through nirurinetin. This eco-friendly approach offers a promising solution to combat citrus canker, a significant threat to the citrus industry (Gaurav et al., 2023).
Yang Y. et al. (2021) address tongue squamous cell carcinoma (TSCC) treatment challenges by using extracellular vesicles (EVs) loaded with chrysin, a flavonoid with anti-tumor properties. They combine this with gold nanoparticles (AuNPs) for photothermal therapy. EVs enhance specificity for TSCC cells. Au-EVs, with near-infrared irradiation, induce TSCC cell apoptosis. RNA sequencing reveals upregulated tumor suppressor miRNAs, particularly let-7a-3p, in EVs-chrysin. Au-EVs combined with near-infrared radiation (NIR) irradiation inhibit tumor growth in vivo by increasing let-7a-3p expression, offering a promising nanomaterial-based approach for TSCC treatment (Yang Z. et al., 2021).
Li J. et al. (2023) enhance tumor immunotherapy using engineered extracellular vesicles (EVs), addressing limitations in tumor antigen presentation to dendritic cells (DCs). They create Te@EVsHSP70 by upregulating heat shock protein 70 (HSP70) expression in tumor cells, leading to engineered EVs with tellurium nanoparticles (Te) for photothermal therapy. Te@EVsHSP70 induce immunogenic cell death and DC maturation, resulting in superior antitumor efficacy in vitro and in vivo. This study offers a practical method to boost tumor immunotherapy by combining photothermal therapy with engineered EVs for enhanced antigen presentation, highlighting an innovative approach in oncology (Li X. et al., 2023).
Naskar et al. (2022) developed an innovative approach to combat Staphylococcus aureus using a nanocomposite coated with EVs from Lactobacillus paracasei (MZ-LPEV). This bioinspired nanoantibiotic exposed considerably progressive antibacterial activity against S. aureus, outperforming other nanoparticles. Its mechanisms included reactive oxygen species production and bacterial membrane disruption. MZ-LPEV also demonstrated enhanced biocompatibility and selectivity for S. aureus. This innovative approach offers promise in addressing antibiotic-resistant strains and represents a novel strategy in the battle against infectious diseases (Naskar et al., 2022).
Cheng et al. (2018) developed a biomimetic nanoparticle platform for efficient systemic and intracellular protein delivery. Guest proteins with high loading content are encapsulated in metal-organic framework (MOF) nanoparticles and protected from degradation. These nanoparticles, coated with an EVs membrane, selectively target tumors, avoid the immune system’s detection, and improve cellular uptake. By using therapeutic protein gelonin, the platform accomplished a 14-fold advances in therapeutic efficacy, inhibiting tumor growth in vivo. This novel approach provides promise in enhanced protein delivery for therapeutic interventions in various diseases, overcoming critical obstacles in current strategies (Cheng et al., 2018).
Qiao et al. (2022) developed EV-Pd-Pt, a biomimetic nanoplatform for synergetic anti-infective therapy. The integration of Pd-Pt nanosheets with ginger-derived EVs, this nanoplatform shows prolonged circulation, exact accumulation at infection sites, and the capability to enter bacteria cells. It also generates sustainable reactive oxygen species (ROS) for enhanced therapy. Notably, EV-Pd-Pt employs both electrodynamic and photothermal therapy, enhancing its anti-infective efficacy. With excellent biocompatibility and biosafety, this nanoplatform presents a promising approach for combating infections in complex biological environments (Qiao et al., 2022).
Li et al. (2021) explored an novel photochemotherapy nanoplatform through macrophage-derived EVs. These EVs were altered with folate for boosted tumor targeting and employed an in situ biosynthetic approach to produce photosensitizer protoporphyrin X (PpIX) and chemotherapy drug doxorubicin (DOX) within the EVs. This approach accomplished high drug-loading efficiency, enhanced tumor accumulation and penetration, and triggered a strengthened immune response for efficacious cancer treatment. The smart nanoplatform’s versatility permits for possible applications in numerous biomedical contexts. This research highlights an well-organized strategy for EVs-based drug delivery, mainly in photochemotherapy, providing potential biomedicine for cancer (Li et al., 2021).
Dumonte et al. (2019) established Trojan nano-horses (TNHs) as a nanotherapeutic approach by encapsulating zinc oxide (ZnO) nanocrystals within EVs. In cancer theranostics, TNHs address issues such as aggregation, degradation, and clearance. In this study, ZnO nanocrystals were carried in EVs, which are known to be stable and biocompatible. Researchers demonstrated TNHs’ biomimetic nanotheranostic potential in this study by verifying their efficient encapsulation, biostability, and cytotoxicity in cells. TNHs are a promising avenue for cancer therapy due to their biomimetic nature and cellular uptake of ZnO nanocrystals (Dumontel et al., 2019).
Shang et al. (2023) investigated into the communications between cationic polymer nanoparticles (cNPs) and cells, converging on their transport mechanisms and possible as biomimetic drug delivery systems. Their study exposed that cNPs could be excreted as cNP@EVs, enveloped by EVs, and travel across several cellular compartments, assisted by autophagy. Nanoparticles can be efficiently transported between cells via EVs, enhancing deep penetration and the effectiveness of antitumor therapies. These results provide insights into nanoparticle transport within and between cells, accenting the role of EVs in facilitating this process. This knowledge possess potential for the advancement of EVs-based drug delivery systems in cancer therapy (Shang et al., 2023).
Mansur et al. (2023) developed a scalable approach for producing EVs loaded with quercetin-iron complex nanoparticles. This novel method was done by direct flow filtration, resulted in improved EVs yield compared to conventional ultracentrifugation. Characterization studies confirmed EVs morphology and standard protein markers, including ALIX, tumor susceptibility gene 101 (TSG101), CD63, and CD81. Cellular uptake experiments specified that, nanoparticle-loaded EVs had greater internalization and uniform distribution in MDA-MB-231br cells when compared with free nanoparticles. In this study, researcher’s, demonstrated the potential of direct flow filtration for scalable nanoparticle-loaded EVs production and suggests their efficiency in targeted drug delivery for advanced biomedical applications, mainly in cancer therapy (Mansur et al., 2023).
Wu M.-S. et al. (2023) delved an novel strategy to improve the therapeutic potential of nanomaterials for cancer treatment. In this study, researchers engineered EVs from modified cancer cells, changing their surface properties and microRNA-21 (miR-21) expression to improve the cancer targeting. These improved EVs encapsulated with gold-polydopamine (PDA) core-shell nanoparticles loaded with doxorubicin (Dox), glucose oxidase (GOx), and miR-21-indicative DNA tags. Upon cellular uptake, the nanoreactors released Dox, triggered GOx-catalyzed hydrogen peroxide (H2O2) generation, and consumed glucose due to the acidic pH and photothermal effect. This cascade treatment strategy, facilitated by EV-assisted delivery, offers a promising approach for improving cancer therapy, addressing biocompatibility and targeting challenges associated with nanomaterial-based treatments (Wu M.-S. et al., 2023).
In their 2018 study, Kim et al. addressed limitations in using human mesenchymal stem cell (hMSC)-derived exosomes for spinal cord injury treatment. To enhance their therapeutic potential, researchers created exosome-mimetic nanovesicles (NV-IONP) by incorporating iron oxide nanoparticles (IONPs) into exosomes from hMSCs treated with IONPs. NV-IONP acted as magnet-guided navigation tools, containing higher therapeutic growth factor levels than exosomes without IONPs. Systemic injection with magnetic guidance increased NV-IONP accumulation in the injured spinal cord, promoting blood vessel formation, reducing inflammation, and improving spinal cord function. This study represents progress in enhancing therapeutic extracellular nanovesicles for spinal cord injury therapy (Kim et al., 2018).
In their 2021 study, Jhan et al. address the challenge of creating effective combination therapies for cancer treatment. They use extracellular vesicles (EVs) as a delivery platform, engineering lipid-hybridized EVs (eEVs) to load small-interfering RNA (siRNA) and then creating an outer polyelectrolyte shell incorporating the chemotherapeutic agent doxorubicin (DOX) through layer-by-layer (LbL) assembly. These findings exposed that, stable EVs-polymer complexes (LbL-eEVs) that efficiently enters cancer cells, delivering siRNA into the cytoplasm and DOX into the cell nuclei, inducing cell death. In addition to being selective for cancer cells, LbL-eEVs minimized harm to normal tissues, making them a auspicious platform for accurate cancer treatment (Jhan et al., 2021).
Pan et al. (2023) developed siS100A4-loaded EVs modified with internalizing arginylglycylaspartic acid (iRGD), a tumor-penetrating peptide, to target S100A4 and inhibit postoperative breast cancer metastasis. These integrated nanoparticles confirmed the protection of siRNA, improved cellular uptake, and compatibility in vitro. In the in vivo model, iRGD-modified EVs exposed enhanced siRNA accumulation in lung metastatic sites, leading to a significant reduction in lung metastases and improved survival rates. In this study, researchers highlights the potential of siS100A4-iRGD-EV nanoparticles as a compelling approach to combat postoperative breast cancer metastasis, provides the hope for better treatment outcomes in breast cancer patients at risk of metastasis after surgery (Pan et al., 2023).
Wu et al. (2021) investigated the hepatocellular carcinoma (HCC)-derived EVs as nanocarriers for sequential nanocatalysts, creating glucose oxidase (GOD)-extremely small-sized iron oxide nanoparticles (ESIONs)@EVs (GE@EVs) for targeted nanocatalytic therapy against HCC. GE@EVs exploited RGD targeting for efficient intracellular delivery. These nanocatalysts encouraged a cascade of reactions in the tumor microenvironment, producing toxic hydroxyl radicals that triggered HCC cell death. In this study, researchers effectively suppressed HCC in vitro and in vivo and doubled as a contrast agent for MRI, offering valuable imaging capabilities. The study highlights the possible of EVs-based nanocatalytic therapy for HCC and validates the versatility of EVs in advanced biomedical applications (Wu et al., 2021).
Xu C. et al. (2023) examined the bone marrow mesenchymal stem cell-derived EVs (BMSC-EVs) loaded on magnetic nanoparticles for diabetic osteoporosis (DO). They identify miR-150-5p as a key player in osteoporosis and use gold-coated magnetic nanoparticles (GMNPs) to enhance BMSC-EV isolation. GMNPs combined with anti-CD63, known as GMNPE, enrich EVs in DO rat bone tissues. BMSC-EVs deliver miR-150-5p to osteoblasts, targeting MMP14 and activating the Wnt/β-catenin pathway. This activation enhances osteoblast proliferation and maturation, making GMNP-BMSC-EVs a promising strategy for diabetic osteoporosis treatment (Xu C. et al., 2023).
In their 2022 study, Li et al. tackle chemotherapy challenges in lung cancer treatment by utilizing EVs for simultaneous delivery of the anticancer drug doxorubicin (DOX) and the chemosensitizer lonidamine (LND). Two types of EVs, 16k EVs and 120k EVs, were prepared and co-delivered DOX and LND, leading to enhanced cytotoxicity and reduced drug doses in vitro. The direct fusion of EVs with cancer cell membranes enabled efficient drug delivery. In vivo studies in a mouse lung cancer model exhibited substantial anticancer activity, with smaller EVs representing improved efficiency. This co-delivery strategy possess efficiency lung cancer chemotherapy outcomes (Li H. et al., 2022).
Kim et al. (2020) addressed the challenge of targeting ischemic brain lesions in stroke treatment by emerging magnetic nanovesicles (MNVs) derived from mesenchymal stem cells (MSCs). These MNVs, carrying iron oxide nanoparticles (IONPs), were exposed to prompt developed levels of therapeutic growth factors when compared with untreated nanovesicles. MNVs are 5.1 times more effective when delivered systemically and guided to the lesion using magnetic navigation in rats with ischemic stroke. This targeted method encouraged an anti-inflammatory response, angiogenesis, and anti-apoptosis, reducing infarction volume and enhanced motor function. MNVs provides a promising strategy for attractive stroke treatment efficacy (Kim et al., 2020).
Yang Y. et al. (2021) addressed a significant challenge in osteoarthritis (OA) therapy through mesenchymal stem cell-derived small EVs (MSC-sEVs). DAHP (Diels-Alder crosslinked hyaluronic acid/PEG) hydrogel was developed as a delivery platform for MSC-sEVs, in order to improve the bioavailability and therapeutic effectiveness. The DAHP hydrogel was exposed to sustain the release of MSC-sEVs without compromising their therapeutic function in vitro and in vivo. This approach provides a promising solution for improving OA treatment by gorgeous the delivery and efficacy of MSC-sEVs, potentially advancing cell-free therapies in regenerative medicine (Yang Y. et al., 2021).
Sancho-Albero et al. (2019) discovered an novel approach in bioorthogonal catalysis, leveraging cancer-derived EVs as carriers for ultrathin palladium (Pd) nanosheets. Bioorthogonal chemistries permit the non-natural synthesis of bioactive compounds in vivo, with Pd catalysts playing a important role. In this study researchers addressed the challenge of selectively delivering catalysts to specific cell types by developing a bio-artificial device consisting of exosomes loaded with Pd catalysts. These EVs enable the controlled assembly of Pd nanosheets inside EVs. This integrated system facilitates Pd-triggered reactions in vitro and within specific cancer cells, opening new possibilities for targeted therapy, including “EVs-directed catalyst prodrug therapy” for accurate and effective cancer treatment (Sancho-Albero et al., 2019).
Li C. et al. (2022) examined the stability and bioavailability challenges of astaxanthin (AST), a potent antioxidant and anticancer compound. They developed AST@PLGA@BEVs by using broccoli-derived extracellular vesicles (BEVs) to coat AST-loaded poly (lactic-co-glycolic acid) (PLGA) nanoparticles. The optimized AST@PLGA@BEVs had a size of 191.60 ± 2.23 nm, a polydispersity index of 0.166, and a zeta potential of −15.85 ± 0.92 mV. Importantly, in vitro experiments demonstrated significantly enhanced anticancer activity compared to AST alone. This innovative approach offers improved stability and bioavailability for astaxanthin, making it a potential functional food with enhanced health benefits (Li C. et al., 2022).
In their 2019 study, Mol et al. explored the potential of injectable supramolecular ureidopyrimidinone (UPy) hydrogels as a delivery platform for extracellular vesicles (EVs). EVs, small vesicles secreted by cells, have garnered interest as promising vehicles for drug delivery and cell-free therapeutics in regenerative medicine. One challenge is achieving optimal therapeutic effects by prolonging EV exposure to target organs, and this study investigates the use of UPy-based hydrogels to address this challenge. The UPy-hydrogel is designed to undergo a solution-to-gel transition when transitioning from a high to neutral pH, enabling rapid gelation upon administration into physiological systems. The researchers demonstrate sustained release of EVs from the UPy-hydrogel over a period of 4 days, during which EVs retain their functional capacity. Importantly, in an in vivo experiment involving the local administration of fluorescently labeled EVs incorporated into a UPy-hydrogel, the EVs are still detected within the hydrogel after 3 days. In contrast, when administered without a hydrogel, the EVs are internalized by surrounding fat and skin tissue near the injection site. These findings highlight the potential of UPy-hydrogels for providing sustained release of EVs and enhancing local retention in vivo. This approach has the potential to improve therapeutic efficacy when using local delivery methods and may open up new applications in the field of regenerative medicine (Mol et al., 2019).
In their 2022 study, Zhu et al. developed a composite hydrogel-based approach for diabetic wound healing. They used gelatin methacrylate (GelMA) and silk fibroin glycidyl methacrylate (SFMA) to create a versatile hydrogel with suitable properties for sustained drug release. Resveratrol (RES) was loaded into mesoporous silica nanoparticles (MSNs) to enhance drug release, and platelet-derived extracellular vesicles (PDEVs) were added to promote cell proliferation and angiogenesis. These hydrogels demonstrated low toxicity, excellent biocompatibility, and the ability to inhibit inflammation and enhance tube formation in vitro. In diabetic mice, they reduced pro-inflammatory factors, boosted anti-inflammatory factors, stimulated angiogenesis, and accelerated wound healing. This approach shows promise for diabetic wound healing by addressing both inflammation and angiogenesis synergistically (Zhu et al., 2022).
In their 2019 study, Han et al. tackled aging-related vascular dysfunction, a complex problem with limited solutions. They uncovered microRNA-675 (miR-675) as a key player in aging-induced vascular issues. MiR-675 levels were reduced in aging muscle tissue, and its mimic reduced markers of aging in senescent cells. They confirmed miR-675’s role by targeting transforming growth factor-β1 (TGF-β1) through dual-luciferase assays. EVs from umbilical cord stem cells loaded with miR-675 were effective in rejuvenating senescent cells. These EVs were embedded in a silk fibroin hydrogel for controlled release. This approach improved blood flow in ischemic limbs and extended EVs retention. It offers promise for addressing aging-related vascular problems and other age-related complications (Han et al., 2019).
In their 2018 study, Zhang et al. aimed to boost the therapeutic potential of MSC-derived EVs for hindlimb ischemia, a condition characterized by reduced blood flow to the legs. They integrated human placenta-derived MSC-derived EVs into a chitosan hydrogel to enhance their stability, retention, and therapeutic impact. The chitosan hydrogel significantly improved EVs stability, crucial for maintaining therapeutic cargo. It also extended EVs retention in target tissues, potentially prolonging their therapeutic effects. In vitro, these EVs showed endothelium-protective and proangiogenic properties. In a murine model, the hydrogel-incorporated exosomes improved angiogenesis. This strategy may advance cell-free treatments for ischemic conditions and other diseases by enhancing EVs stability, retention, and efficacy (Zhang et al., 2018).
In their 2019 study, Pizzicannella et al. explored bone tissue regeneration through 3D printing and biomaterials enriched with gingival stem cells (GSCs) and extracellular vesicles (EVs). They used poly (lactide) (PLA) for 3D printing, creating a scaffold (3D-PLA) enriched with human gingival mesenchymal stem cells (hGMSCs) and their EVs. In vitro, they found increased expression of osteogenic and angiogenic markers in the living construct. In rats, implantation of 3D-PLA/hGMSCs/EVs stimulated bone regeneration and vascularization, confirmed by histology and microCT imaging. Upregulation of miR-2861 and miR-210, associated with osteoangiogenesis, was observed. This approach offers promise for bone tissue regeneration, driven by specific microRNAs and regenerative biomaterials (Pizzicannella et al., 2019).
In their 2018 study, Li et al. developed a novel approach to accelerate bone regeneration by creating cell-free tissue-engineered bone. They immobilized EVs from human adipose-derived stem cells (hASCs) onto poly (lactic-co-glycolic acid) (PLGA) scaffolds coated with polydopamine (pDA). These EVs, nanoscale vesicles crucial for cell communication, enhanced osteogenesis, cell proliferation, and migration of mesenchymal stem cells in vitro. Optimizing their osteoinductive effects further boosted bone formation. In mouse calvarial defects, this cell-free system significantly improved bone regeneration, attributed to EVs-induced osteoinduction and enhanced mesenchymal stem cell migration. This research offers a promising therapeutic avenue for bone tissue engineering and defect repair (Li et al., 2018).
In their 2020 study, Hamada et al. tackled the challenges of cardiac repair in chronic heart failure by developing a controlled release system using a photocurable adhesive polymer called poly (glycerol-co-sebacate) acrylate ethylene glycol (PGSA-g-EG). This polymer adheres to the heart’s surface, enabling local and sustained delivery of EVs, which play a crucial role in tissue regeneration. Importantly, the study showed that the polymer didn't compromise EV bioactivity. In rat experiments, the polymer proved biocompatible and stayed attached to the heart surface for over a month. The release kinetics of EVs from the polymer were improved, confirming the sustained delivery of bioactive EVs for at least 14 days. This novel approach provides a promising solution for controlled EVs delivery in cardiac repair, potentially improving therapy for chronic heart failure (Hamada et al., 2020).
Lv et al. (2019) introduced an innovative therapeutic approach for myocardial infarction (MI) using sEVs derived from bone marrow MSCs. In this study, researchers developed a sodium alginate hydrogel system with sEVs incorporated into it (sEVs-Gel) in order to overcome the challenges of limited retention and short-term effects of MSC-derived sEVs in the heart. This optimized system improved sEV release and rheological properties. Ex vivo imaging confirmed enhanced sEV retention in heart tissue. Functional analysis revealed reduced cardiac cell apoptosis, improved macrophage polarization, increased scar thickness, and enhanced angiogenesis after MI. Cardiac function and infarct size assessments showed superior outcomes compared to sEV treatment alone. This approach represents a promising cell-free therapy for MI (Lv et al., 2019).
In their 2019 research, Mardpour and colleagues aimed to improve hepatic regeneration in chronic liver failure using MSC-EVs. These EVs hold therapeutic potential but are rapidly cleared when systemically administered, reducing their efficacy. To address this, they developed a novel approach involving sustained EV release into the peritoneum. Clickable polyethylene glycol (PEG) macromeres were mixed with MSC-EVs to form EV-encapsulated PEG hydrogels. These hydrogels gradually released EVs as they biodegraded, extending EV accumulation in the liver over a month. In a rat model of liver fibrosis, Gel-EV treatment outperformed Free-EV, reducing fibrosis, inflammation, apoptosis, and improving liver regeneration. This study suggests that sustained EV delivery through hydrogel-mediated release could enhance their therapeutic potential for chronic liver failure (Mardpour et al., 2019).
In their 2020 study, Liu et al. investigated the enhanced therapeutic potential of MSC-EVs for acute kidney injury (AKI). They encapsulated EVs from human placental MSCs (hP-MSC-EVs) in a collagen matrix to address retention and stability issues post-transplantation. The collagen matrix significantly improved EV stability, promoted sustained release, and extended EV retention in an AKI model, as shown by Gaussia luciferase imaging. It also stimulated renal tubular epithelial cell proliferation and enhanced therapeutic effects, including angiogenesis, reduced fibrosis, and apoptosis. The study revealed that EVs partly exerted their therapeutic effects by inhibiting endoplasmic reticulum stress. This strategy holds promise for advancing cell-free regenerative medicine in AKI treatment (Liu et al., 2020).
In their 2020 study, Zhang et al. sought to enhance the therapeutic effectiveness of MSC-EVs for treating acute kidney injury (AKI). MSC-EVs offer a cell-free AKI therapy, but their limited stability and retention have been obstacles. To address this, researchers developed hydrogels with Arg-Gly-Asp (RGD) peptides, which bind to MSC-EV membranes’ integrins. RGD hydrogels improved EV retention and stability, confirmed through in vivo tracking and integrin gene knockdown experiments. When EV-RGD hydrogels were injected intrarenal into mouse models with AKI, enhanced kidney function, damage was reduced, and cell proliferation was improved. MicroRNA let-7a-5p also improved the MSC-EV’s antifibrotic effects during chronic AKI phases when RGD hydrogels were applied. Cell-free renal repair is conceivable with MSC-EVs and insights into regenerative medicine are exposed in this study (Zhang et al., 2020).
7 Limitations
The integration of nanomaterials with EVs for biomedical applications, while promising, faces several significant limitations that need to be addressed before clinical translation can be achieved. These limitations span issues related to standardization, scalability, safety, understanding of underlying mechanisms, regulatory hurdles, and ethical considerations. Addressing these challenges is essential for optimizing the efficacy of EV-nanomaterial hybrids and advancing their use in various therapeutic and diagnostic applications.
7.1 Lack of standardization and reproducibility
A fundamental challenge in the integration of EVs with nanomaterials is the lack of standardized protocols. There is no consensus on optimal methods for isolating EVs or selecting nanomaterials, and differences in experimental protocols—ranging from EV extraction methods to nanomaterial properties—result in considerable variability across studies. EVs are derived from various sources such as stem cells, tumor cells, and platelets, each with distinct biological compositions and functionalities. Nanomaterials, including liposomes, nanoparticles, and polymers, also vary widely in size, surface charge, and chemical composition, further complicating the integration process. This diversity in both EVs and nanomaterials leads to inconsistent results in terms of loading efficiency, stability, and therapeutic outcomes. Without uniform protocols for EV-nanomaterial hybridization, comparing results across different studies becomes challenging, making it difficult to establish reliable conclusions about the most effective combinations and methods (Nieuwland et al., 2022).
7.2 Scalability and large-scale production
One of the most significant barriers to the clinical translation of EV-nanomaterial hybrids is scaling up production. While small-scale studies have demonstrated the potential of these systems, there are challenges in translating these findings to clinical settings. The large-scale production of EVs with consistent quality is still in its nascent stages. The isolation of EVs from biological fluids often involves ultracentrifugation or filtration methods, which can be time-consuming, costly, and not easily scaled for clinical use. Moreover, the therapeutic properties of EVs—such as their ability to efficiently deliver cargo and maintain functionality—can degrade during large-scale production processes. Ensuring that the high yield of EVs retains its therapeutic properties is critical for maintaining their efficacy in clinical applications. Furthermore, maintaining the functionality of the hybrid system during large-scale manufacturing, particularly the stability of the nanomaterials integrated with EVs, remains a significant challenge. This makes the standardization of large-scale production methods essential for the successful clinical translation of these therapies (Paganini et al., 2019).
7.3 Safety concerns:- toxicity and immunogenicity
The safety of EV-nanomaterial hybrids is a major concern that needs to be addressed before their clinical application. While EVs are generally considered biocompatible due to their natural origin, the incorporation of nanomaterials can introduce risks related to toxicity, immune responses, and long-term side effects. Nanomaterials, particularly metallic nanoparticles, have been shown to elicit immune responses, cause oxidative stress, and potentially lead to tissue toxicity. The combination of nanomaterials with EVs could exacerbate these effects, as the nanomaterials may induce inflammation, alter cell signaling, or affect the stability of the EVs themselves. Moreover, the potential for accumulation of nanomaterials in non-target organs over time raises concerns about chronic toxicity. Understanding the dose-response relationships, tissue distribution, and long-term effects of these hybrid systems is crucial to assess their safety. Additionally, ensuring that the hybrid systems do not provoke unwanted immune responses, such as hypersensitivity or autoimmune reactions, is critical for their clinical success (Worthington and Hagood, 2020).
7.4 Incomplete understanding of EV-nanomaterial interactions
Another limitation is the incomplete understanding of the mechanisms underlying EV-nanomaterial interactions. The efficiency with which nanomaterials are loaded into EVs, their stability within the vesicles, and the ability of the hybrid system to efficiently deliver therapeutic cargo to target tissues depend on a complex interplay of biochemical and physical factors. For example, the surface properties of nanomaterials, such as charge and size, play a significant role in determining the efficiency of cargo loading into EVs and their cellular uptake. However, the molecular mechanisms governing these interactions remain poorly understood. Factors such as the affinity between the nanomaterial and the EV membrane, the loading capacity of different nanomaterials, and the potential for disrupting the native properties of EVs are areas that require further investigation. A deeper understanding of these mechanisms will allow for better design and optimization of EV-nanomaterial hybrids, improving their therapeutic efficacy (van Niel et al., 2022).
7.5 Regulatory challenges
The lack of clear regulatory guidelines for EV-nanomaterial hybrids remains a major obstacle to their clinical translation. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have yet to establish comprehensive frameworks for the approval of nanomaterial-based therapies. This creates uncertainty regarding the requirements for preclinical and clinical testing, safety evaluations, and manufacturing standards. The complexity of EV-nanomaterial hybrids—being a combination of biologically derived materials and engineered nanomaterials—adds an extra layer of complexity to the regulatory process. Regulatory agencies must determine the appropriate criteria for assessing the quality, safety, and efficacy of these systems, considering both their biological and engineered components. Furthermore, ensuring consistency in batch production, controlling for variability in both EVs and nanomaterials, and establishing reproducible safety profiles are essential for obtaining regulatory approval. As the field progresses, there is an urgent need for clear, standardized guidelines for the clinical development of EV-nanomaterial hybrid therapies (Chua et al., 2022).
7.6 Limited therapeutic persistence
While EV-nanomaterial hybrids show great promise for targeted drug delivery, their therapeutic potential is often limited by the short half-life of EVs in circulation. EVs are naturally cleared from the body quickly, primarily through interactions with the mononuclear phagocyte system (MPS), which reduces their efficacy for systemic drug delivery. Although surface modifications, such as PEGylation or the incorporation of stabilizing nanomaterials, can prolong the circulation time of EVs, achieving sustained therapeutic efficacy remains challenging. Strategies to enhance the persistence of EVs in circulation, such as modifying their surface properties to reduce immune recognition or designing nanomaterial-based carriers to shield EVs from clearance, are actively being explored. However, these strategies are still in early stages, and the long-term effects of such modifications need thorough investigation to ensure that they do not compromise the EVs’ natural properties or induce adverse immune reactions (Pirisinu et al., 2022).
7.7 Ethical and privacy concerns
As with any novel therapeutic approach, ethical considerations must be carefully addressed when developing EV-nanomaterial hybrid therapies. These therapies involve modifying biological materials, which raises questions about informed consent, patient privacy, and the long-term implications of using genetically modified or engineered materials in humans. Ethical concerns also extend to the collection and use of human-derived EVs, particularly in terms of privacy and consent for their use in research or clinical applications. Additionally, the introduction of nanomaterials into the body, particularly those that may accumulate over time, raises potential concerns about unintended consequences. Regulatory bodies will need to consider these ethical issues in developing frameworks that ensure the responsible use of EV-nanomaterial hybrids in clinical settings (Hagey and El Andaloussi, 2023).
These limitations underscore the complexity of integrating nanomaterials with EVs for advanced biomedical applications and highlight areas requiring further research and collaboration to overcome these challenges.
8 Emerging trends in EV-nanomaterial research
Emerging trends in EV-nanomaterial research indicate significant advancements in the integration of AI and machine learning (ML) to accelerate the design and optimization of hybrid systems. AI-driven computational models are increasingly being used to predict the behavior of EVs and nanomaterials at the molecular level, enabling more efficient selection of nanomaterials based on specific properties such as size, surface charge, and targeting capacity. Machine learning algorithms can analyze large datasets to identify patterns that may not be immediately apparent, helping to streamline the discovery of novel nanomaterial-EV combinations.
Furthermore, AI has the potential to revolutionize the customization of EV-based drug delivery systems. By combining AI with high-throughput screening techniques, researchers can rapidly identify the most effective formulations for therapeutic delivery, based on factors like cargo loading efficiency, stability, and cellular uptake. In addition, AI can assist in predicting and mitigating the potential toxicity or immunogenicity of these hybrid systems, which is a major concern in their clinical translation.
Additionally, the future of EV-nanomaterial hybrids may involve the incorporation of advanced nanofabrication techniques, such as 3D printing, to create more complex, multifunctional systems. These advances could pave the way for more personalized and scalable therapeutic options, particularly in areas such as cancer treatment, regenerative medicine, and gene therapy.
By integrating AI and other cutting-edge technologies, the future of EV-nanomaterial hybrids looks promising, offering enhanced efficiency, precision, and safety in drug delivery and biomedical applications. We believe this addition significantly enriches the manuscript by providing insight into the exciting potential of AI in shaping the next-generation of EV-based therapies.
9 Future perspectives
The integration of nanomaterials with EVs offers exhilarating potentials for advanced biomedical applications. As a result of this synergy, healthcare can be transformed and innovative advances made. One of the most promising future prospects is the expansion of highly targeted therapies using EVs-nanomaterial hybrids. Researchers are actively developing the engineered EVs to carry specific cargo molecules, like drugs or nucleic acids, and functionalizing nanomaterials to enhance targeting. This innovative approach could be transformed into cancer treatment, delivering drugs precisely to tumors while minimizing side effects. It may also possess efficacy treatments for other diseases, such as neurodegenerative disorders and cardiovascular conditions. Personalized medicine is another boulevard that, this integration could unlock. By leveraging the diversity of EVs and tailoring nanomaterials properties, clinicians might create modified therapies for individual patients. This could involve selecting EVs from specific cell sources, engineering them with patient-specific cargo, and optimizing nanomaterials for improved targeting, resulting in more operative and safer treatments.
EVs have exposed promise as vehicles for vaccines. In the future, EVs-based vaccines using nanomaterials to enhance the stability and immune responses. EVs could carry viral antigens, making them ideal for vaccine delivery. Nanomaterials could optimize the vaccine formulation and delivery, possibly leading to more operative and easily administered immunization strategies. Regenerative medicine can be benefited significantly from EVs-nanomaterial hybrids. Researchers are discovering these hybrids to excite tissue repair and regeneration. By designing nanomaterials that mimic the extracellular matrix and loading EVs with regenerative cargo, this method could encourage the healing of damaged tissues, such as cartilage, bone, and nerves, providing new hope for treating injuries and degenerative diseases. The integration of nanomaterials with EVs also provides new potentials in diagnostics and medical imaging. Researchers are emerging the EVs-based biosensors and imaging agents for real-time disease monitoring. This innovative approach revolutionize early disease detection, leading to more effective and personalized healthcare.
Future research will likely focus on refining the use of EV-nanomaterial hybrids for drug delivery. Improving cargo loading efficiency, extending EV circulation time, and enhancing stability are key objectives. Nanomaterials can play a pivotal role in achieving these goals through various approaches, ultimately leading to more efficient and safer drug delivery systems for a wide range of diseases. Combining the unique properties of EVs and nanomaterials may enable the development of multimodal therapies. These therapies could incorporate various treatment strategies into a single platform. EVs, as versatile carriers, and engineered nanomaterials could facilitate multiple therapeutic approaches simultaneously, particularly valuable for complex diseases requiring a multifaceted approach. Addressing scalability is a crucial future perspective for this field. Researchers are actively exploring innovative manufacturing techniques to produce EVs and nanomaterials at larger scales while maintaining quality and reproducibility. Scalable production methods are essential to translating EV-nanomaterial therapies from the lab to clinical practice effectively. As EV-nanomaterial-based therapies progress toward clinical use, regulatory and ethical considerations will become increasingly important. Regulatory agencies will need to establish clear guidelines for evaluating the safety and efficacy of these novel treatments. Ethical discussions should continue to ensure responsible development and equitable access to these advanced biomedical applications.
The synergistic integration of nanomaterials with extracellular vesicles represents a promising frontier in biomedical research and applications. Future prospects include highly targeted therapies, personalized medicine, EV-based vaccines, regenerative medicine, diagnostics, drug delivery optimization, multimodal therapies, advancements in manufacturing, and regulatory and ethical considerations. Collaborative research energies among researchers, clinicians, industry partners, and regulatory bodies are essential to realizing the full potential of this novel field. With continued research and innovation, EVs-nanomaterials hybrids possess the promise of revolutionizing healthcare and improving patients’ lives worldwide.
10 Conclusion
The integration of nanomaterials with EVs signifies a highly promising frontier in advanced biomedical research. This synergistic approach provides exciting prospects, including highly targeted therapies, personalized medicine, regenerative medicine, improved diagnostics, efficient drug delivery, multimodal therapies, scalable production methods, and ethical regulatory considerations. The possible impact of EVs-nanomaterials hybrids on healthcare is substantial. They have the capability to revolutionize treatment strategies, efficacy patient outcomes, and allow the tailored therapies for a range of diseases. Nevertheless, addressing existing limitations such as scalability, cargo loading efficiency, and regulatory challenges is crucial to realizing these probabilities. Research collaboration among researchers, clinicians, industry partners, and regulatory bodies will be crucial for the responsible development and equitable access to these innovative biomedical applications. With ongoing research and innovation, EVs-nanomaterials hybrids possess the promise of transforming the landscape of healthcare, enlightening patient wellbeing, and advancing the field of medicine.
Statements
Author contributions
HJ: Conceptualization, Investigation, Writing–original draft. RK: Conceptualization, Investigation, Writing–original draft. JP: Formal Analysis, Investigation, Resources, Validation, Writing–original draft. KR: Formal Analysis, Investigation, Resources, Validation, Writing–original draft. GV: Conceptualization, Supervision, Validation, Writing–review and editing. CP: Conceptualization, Formal Analysis, Investigation, Supervision, Writing–review and editing. IDM: Conceptualization, Formal Analysis, Investigation, Supervision, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by Lucian Blaga University of Sibiu & Hasso Plattner Foundation research grants LBUS-IRG-2021-07.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
Albalawi F. Hussein M. Z. Fakurazi S. Masarudin M. J. (2021). Engineered nanomaterials: the challenges and opportunities for nanomedicines. Int. J. nanomedicine16, 161–184. 10.2147/ijn.s288236
2
Ali W. Deng K. Bian Y. Liu Z. Zou H. (2023). Spectacular role of epididymis and bio-active cargo of nano-scale exosome in sperm maturation: a review. Biomed. and Pharmacother.164, 114889. 10.1016/j.biopha.2023.114889
3
Allan D. Tieu A. Lalu M. Burger D. (2020). Mesenchymal stromal cell-derived extracellular vesicles for regenerative therapy and immune modulation: progress and challenges toward clinical application. Stem Cells Transl. Med.9, 39–46. 10.1002/sctm.19-0114
4
Bayat F. Afshar A. Baghban N. (2021). Algal cells-derived extracellular vesicles: a review with special emphasis on their antimicrobial effects. Front. Microbiol.12, 785716. 10.3389/fmicb.2021.785716
5
Beetler D. J. Di Florio D. N. Law E. W. Groen C. M. Windebank A. J. Peterson Q. P. et al (2023). The evolving regulatory landscape in regenerative medicine. Mol. Aspects Med.91, 101138. 10.1016/j.mam.2022.101138
6
Bennett A. P. De La Torre-Escudero E. Robinson M. W. (2020). Helminth genome analysis reveals conservation of extracellular vesicle biogenesis pathways but divergence of RNA loading machinery between phyla. Int. J. Parasitol.50, 655–661. 10.1016/j.ijpara.2020.04.004
7
Bhattacharya S. Kundu A. (2020). “Sugars and sugar polyols in overcoming environmental stresses,” in Protective chemical agents in the amelioration of plant abiotic stress: biochemical and molecular perspectives, 71–101.
8
Boilard E. Bellio M. (2022). Platelet extracellular vesicles and the secretory interactome join forces in health and disease. Immunol. Rev.312, 38–51. 10.1111/imr.13119
9
Borniego M. L. Innes R. W. (2023). Extracellular RNA: mechanisms of secretion and potential functions. J. Exp. Bot.74, 2389–2404. 10.1093/jxb/erac512
10
Buzas E. I. (2023). The roles of extracellular vesicles in the immune system. Nat. Rev. Immunol.23, 236–250. 10.1038/s41577-022-00763-8
11
Cai Q. He B. Wang S. Fletcher S. Niu D. Mitter N. et al (2021). Message in a bubble: shuttling small RNAs and proteins between cells and interacting organisms using extracellular vesicles. Annu. Rev. plant Biol.72, 497–524. 10.1146/annurev-arplant-081720-010616
12
Cassani M. Fernandes S. Vrbsky J. Ergir E. Cavalieri F. Forte G. (2020). Combining nanomaterials and developmental pathways to design new treatments for cardiac regeneration: the pulsing heart of advanced therapies. Front. Bioeng. Biotechnol.8, 323. 10.3389/fbioe.2020.00323
13
Catalano M. O’driscoll L. (2020). Inhibiting extracellular vesicles formation and release: a review of EV inhibitors. J. Extracell. vesicles9, 1703244. 10.1080/20013078.2019.1703244
14
Chen J. Zhang X. Millican R. Sherwood J. Martin S. Jo H. et al (2021). Recent advances in nanomaterials for therapy and diagnosis for atherosclerosis. Adv. drug Deliv. Rev.170, 142–199. 10.1016/j.addr.2021.01.005
15
Cheng G. Li W. Ha L. Han X. Hao S. Wan Y. et al (2018). Self-assembly of extracellular vesicle-like metal–organic framework nanoparticles for protection and intracellular delivery of biofunctional proteins. J. Am. Chem. Soc.140, 7282–7291. 10.1021/jacs.8b03584
16
Cheng H. W. Tsao H. Y. Chiang C. S. Chen S. Y. (2021). Advances in magnetic nanoparticle‐mediated cancer immune‐theranostics. Adv. Healthc. Mater.10, 2001451. 10.1002/adhm.202001451
17
Cheng L. Hill A. F. (2022). Therapeutically harnessing extracellular vesicles. Nat. Rev. Drug Discov.21, 379–399. 10.1038/s41573-022-00410-w
18
Chua J. K. E. Lim J. Foong L. H. Mok C. Y. Tan H. Y. Tung X. Y. et al (2022). Mesenchymal stem cell-derived extracellular vesicles: progress and remaining hurdles in developing regulatory compliant quality control assays. Cell Biol. Transl. Med.17, 191–211. 10.1007/5584_2022_728
19
Cruz Camacho A. Alfandari D. Kozela E. Regev-Rudzki N. (2023). Biogenesis of extracellular vesicles in protozoan parasites: the ESCRT complex in the trafficking fast lane?PLoS Pathog.19, e1011140. 10.1371/journal.ppat.1011140
20
Dicenzo G. C. Tesi M. Pfau T. Mengoni A. Fondi M. (2020). Genome-scale metabolic reconstruction of the symbiosis between a leguminous plant and a nitrogen-fixing bacterium. Nat. Commun.11, 2574. 10.1038/s41467-020-16484-2
21
Di Santo R. Vaccaro M. Romanò S. Di Giacinto F. Papi M. Rapaccini G. L. et al (2022). Machine learning-assisted FTIR analysis of circulating extracellular vesicles for cancer liquid biopsy. J. Personalized Med.12, 949. 10.3390/jpm12060949
22
Dixson A. C. Dawson T. R. Di Vizio D. Weaver A. M. (2023). Context-specific regulation of extracellular vesicle biogenesis and cargo selection. Nat. Rev. Mol. Cell Biol.24, 454–476. 10.1038/s41580-023-00576-0
23
Dos Santos J. De Oliveira R. S. De Oliveira T. V. Velho M. C. Konrad M. V. Da Silva G. S. et al (2021). 3D printing and nanotechnology: a multiscale alliance in personalized medicine. Adv. Funct. Mater.31, 2009691. 10.1002/adfm.202009691
24
Dumontel B. Susa F. Limongi T. Canta M. Racca L. Chiodoni A. et al (2019). ZnO nanocrystals shuttled by extracellular vesicles as effective Trojan nano-horses against cancer cells. Nanomedicine14, 2815–2833. 10.2217/nnm-2019-0231
25
Elkhoury K. Chen M. Koçak P. Enciso-Martínez E. Bassous N. J. Lee M. C. et al (2022). Hybrid extracellular vesicles-liposome incorporated advanced bioink to deliver microRNA. Biofabrication14, 045008. 10.1088/1758-5090/ac8621
26
El Nahrawy A. M. Hemdan B. A. Mansour A. Elzwawy A. Abou Hammad A. B. (2021). Integrated use of nickel cobalt aluminoferrite/Ni2+ nano-crystallites supported with SiO2 for optomagnetic and biomedical applications. Mater. Sci. Eng. B274, 115491. 10.1016/j.mseb.2021.115491
27
Fauth M. Hegewald A. B. Schmitz L. Krone D. J. Saul M. J. (2019). Validation of extracellular miRNA quantification in blood samples using RT‐qPCR. FASEB bioAdvances1, 481–492. 10.1096/fba.2019-00018
28
Gaurav I. Thakur A. Kumar G. Long Q. Zhang K. Sidu R. K. et al (2023). Delivery of apoplastic extracellular vesicles encapsulating Green-synthesized silver nanoparticles to treat citrus canker. Nanomaterials13, 1306. 10.3390/nano13081306
29
Girija A. Hacham Y. Dvir S. Panda S. Lieberman-Lazarovich M. Amir R. (2023). Cystathionine γ-synthase expression in seeds alters metabolic and DNA methylation profiles in Arabidopsis. Plant Physiol.193, 595–610. 10.1093/plphys/kiad330
30
Gong D. Sun L. Li X. Zhang W. Zhang D. Cai J. (2023). Micro/nanofabrication, assembly, and actuation based on microorganisms: recent advances and perspectives. Small Struct.4, 2200356. 10.1002/sstr.202370026
31
Hagey D. W. El Andaloussi S. (2023). “The promise and challenges of extracellular vesicles in the diagnosis of neurodegenerative diseases,” in Handbook of clinical neurology (Elsevier), 227–241.
32
Hamada T. Dubois J. L. Bellamy V. Pidial L. Hagège A. Pereira M. N. et al (2020). In vitro controlled release of extracellular vesicles for cardiac repair from poly (glycerol sebacate) acrylate-based polymers. Acta Biomater.115, 92–103. 10.1016/j.actbio.2020.08.015
33
Han C. Zhou J. Liu B. Liang C. Pan X. Zhang Y. et al (2019). Delivery of miR-675 by stem cell-derived exosomes encapsulated in silk fibroin hydrogel prevents aging-induced vascular dysfunction in mouse hindlimb. Mater. Sci. Eng. C99, 322–332. 10.1016/j.msec.2019.01.122
34
Han H. S. Choi K. Y. (2021). Advances in nanomaterial-mediated photothermal cancer therapies: toward clinical applications. Biomedicines9, 305. 10.3390/biomedicines9030305
35
Han X. Mitchell M. J. Nie G. (2020). Nanomaterials for therapeutic RNA delivery. Matter3, 1948–1975. 10.1016/j.matt.2020.09.020
36
Haque N. Widera D. Govindasamy V. Soesilawati P. Abu Kasim N. H. (2022). Extracellular vesicles from stem and progenitor cells for cell-free regenerative therapy. Curr. Mol. Med.22, 120–131. 10.2174/1566524021666210125114828
37
Herrmann I. K. Wood M. J. A. Fuhrmann G. (2021). Extracellular vesicles as a next-generation drug delivery platform. Nat. Nanotechnol.16, 748–759. 10.1038/s41565-021-00931-2
38
Hu W. Liu C. Bi Z.-Y. Zhou Q. Zhang H. Li L.-L. et al (2020). Comprehensive landscape of extracellular vesicle-derived RNAs in cancer initiation, progression, metastasis and cancer immunology. Mol. Cancer19, 102–123. 10.1186/s12943-020-01199-1
39
Imanbekova M. Suarasan S. Lu Y. Jurchuk S. Wachsmann-Hogiu S. (2022). Recent advances in optical label-free characterization of extracellular vesicles. Nanophotonics11, 2827–2863. 10.1515/nanoph-2022-0057
40
Jalaludin I. Lubman D. M. Kim J. (2023). A guide to mass spectrometric analysis of extracellular vesicle proteins for biomarker discovery. Mass Spectrom. Rev.42, 844–872. 10.1002/mas.21749
41
Jhan Y.-Y. Palou Zuniga G. Singh K. A. Gaharwar A. K. Alge D. L. Bishop C. J. (2021). Polymer-coated extracellular vesicles for selective codelivery of chemotherapeutics and siRNA to cancer cells. ACS Appl. Bio Mater.4, 1294–1306. 10.1021/acsabm.0c01153
42
Jia G. Han Y. An Y. Ding Y. He C. Wang X. et al (2018). NRP-1 targeted and cargo-loaded exosomes facilitate simultaneous imaging and therapy of glioma in vitro and in vivo. Biomaterials178, 302–316. 10.1016/j.biomaterials.2018.06.029
43
Jia Z. Zhang S. Li W. (2023). Harnessing stem cell-derived extracellular vesicles for the regeneration of degenerative bone conditions. Int. J. NanomedicineVol. 18, 5561–5578. 10.2147/ijn.s424731
44
Ju Y. Hu Y. Yang P. Xie X. Fang B. (2022). Extracellular vesicle-loaded hydrogels for tissue repair and regeneration. Mater. Today Bio18, 100522. 10.1016/j.mtbio.2022.100522
45
Kalininskiy A. Kittel J. Nacca N. E. Misra R. S. Croft D. P. Mcgraw M. D. (2021). E-cigarette exposures, respiratory tract infections, and impaired innate immunity: a narrative review. Pediatr. Med. Hong. Kong, China4, 5. 10.21037/pm-20-97
46
Kang T. Atukorala I. Mathivanan S. (2021). Biogenesis of extracellular vesicles. New Front. Extracell. Vesicles97, 19–43. 10.1007/978-3-030-67171-6_2
47
Khongkow M. Yata T. Boonrungsiman S. Ruktanonchai U. R. Graham D. Namdee K. (2019). Surface modification of gold nanoparticles with neuron-targeted exosome for enhanced blood–brain barrier penetration. Sci. Rep.9, 8278. 10.1038/s41598-019-44569-6
48
Kim H. Y. Kim T. J. Kang L. Kim Y.-J. Kang M. K. Kim J. et al (2020). Mesenchymal stem cell-derived magnetic extracellular nanovesicles for targeting and treatment of ischemic stroke. Biomaterials243, 119942. 10.1016/j.biomaterials.2020.119942
49
Kim H. Y. Kumar H. Jo M.-J. Kim J. Yoon J.-K. Lee J.-R. et al (2018). Therapeutic efficacy-potentiated and diseased organ-targeting nanovesicles derived from mesenchymal stem cells for spinal cord injury treatment. Nano Lett.18, 4965–4975. 10.1021/acs.nanolett.8b01816
50
Kooijmans S. Fliervoet L. Van Der Meel R. Fens M. Heijnen H. En Henegouwen P. V. B. et al (2016). PEGylated and targeted extracellular vesicles display enhanced cell specificity and circulation time. J. Control. Release224, 77–85. 10.1016/j.jconrel.2016.01.009
51
Kuo C.-L. Ponneri Babuharisankar A. Lin Y.-C. Lien H.-W. Lo Y. K. Chou H.-Y. et al (2022). Mitochondrial oxidative stress in the tumor microenvironment and cancer immunoescape: foe or friend?J. Biomed. Sci.29, 74. 10.1186/s12929-022-00859-2
52
Lai J. Meng Q.-F. Tian M. Zhuang X. Pan P. Du L. et al (2022). A decoy microrobot that removes SARS-CoV-2 and its variants in wastewater. Cell Rep. Phys. Sci.3, 101061. 10.1016/j.xcrp.2022.101061
53
Leidal A. M. Debnath J. (2021). Emerging roles for the autophagy machinery in extracellular vesicle biogenesis and secretion. FASEB BioAdvances3, 377–386. 10.1096/fba.2020-00138
54
Li C. Song Q. Yin X. Song R. Chen G. (2022a). Preparation, characterization, and in vitro anticancer activity evaluation of broccoli-derived extracellular vesicle-coated astaxanthin nanoparticles. Molecules27, 3955. 10.3390/molecules27123955
55
Li H. Xu W. Li F. Zeng R. Zhang X. Wang X. et al (2022b). Amplification of anticancer efficacy by co-delivery of doxorubicin and lonidamine with extracellular vesicles. Drug Deliv.29, 192–202. 10.1080/10717544.2021.2023697
56
Li J. Zhang Y. Dong P.-Y. Yang G.-M. Gurunathan S. (2023a). A comprehensive review on the composition, biogenesis, purification, and multifunctional role of exosome as delivery vehicles for cancer therapy. Biomed. and Pharmacother.165, 115087. 10.1016/j.biopha.2023.115087
57
Li R. Gong X. Hong C. Wang H. Chen Y. Tan K. et al (2021). An efficient photochemotherapy nanoplatform based on the endogenous biosynthesis of photosensitizer in macrophage-derived extracellular vesicles. Biomaterials279, 121234. 10.1016/j.biomaterials.2021.121234
58
Li W. Liu Y. Zhang P. Tang Y. Zhou M. Jiang W. et al (2018). Tissue-engineered bone immobilized with human adipose stem cells-derived exosomes promotes bone regeneration. ACS Appl. Mater. and interfaces10, 5240–5254. 10.1021/acsami.7b17620
59
Li X. He S. Luo B. Li P. Chen X. Wu M. et al (2023b). Engineered extracellular vesicles to enhance antigen presentation for boosting light‐driven tumor immunotherapy. Small19, 2303541. 10.1002/smll.202303541
60
Li Y. Tang X. Gu Y. Zhou G. (2023c). Adipocyte-derived extracellular vesicles: small vesicles with big impact. Front. Bioscience-Landmark28, 149. 10.31083/j.fbl2807149
61
Li Y. Wu J. Liu R. Zhang Y. Li X. (2022c). Extracellular vesicles: catching the light of intercellular communication in fibrotic liver diseases. Theranostics12, 6955–6971. 10.7150/thno.77256
62
Liu C. Wang Y. Li L. He D. Chi J. Li Q. et al (2022a). Engineered extracellular vesicles and their mimetics for cancer immunotherapy. J. Control. Release349, 679–698. 10.1016/j.jconrel.2022.05.062
63
Liu Q. Huang J. Xia J. Liang Y. Li G. (2022b). Tracking tools of extracellular vesicles for biomedical research. Front. Bioeng. Biotechnol.10, 943712. 10.3389/fbioe.2022.943712
64
Liu R. Luo C. Pang Z. Zhang J. Ruan S. Wu M. et al (2023a). Advances of nanoparticles as drug delivery systems for disease diagnosis and treatment. Chin. Chem. Lett.34, 107518. 10.1016/j.cclet.2022.05.032
65
Liu Y. Cui J. Wang H. Hezam K. Zhao X. Huang H. et al (2020). Enhanced therapeutic effects of MSC-derived extracellular vesicles with an injectable collagen matrix for experimental acute kidney injury treatment. Stem cell Res. and Ther.11, 161. 10.1186/s13287-020-01668-w
66
Liu Z. Zhuang Y. Fang L. Yuan C. Wang X. Lin K. (2023b). Breakthrough of extracellular vesicles in pathogenesis, diagnosis and treatment of osteoarthritis. Bioact. Mater.22, 423–452. 10.1016/j.bioactmat.2022.10.012
67
Luo Y. Yang H. Zhou Y.-F. Hu B. (2020). Dual and multi-targeted nanoparticles for site-specific brain drug delivery. J. Control. Release317, 195–215. 10.1016/j.jconrel.2019.11.037
68
Lv K. Li Q. Zhang L. Wang Y. Zhong Z. Zhao J. et al (2019). Incorporation of small extracellular vesicles in sodium alginate hydrogel as a novel therapeutic strategy for myocardial infarction. Theranostics9, 7403–7416. 10.7150/thno.32637
69
Ma W. Zhan Y. Zhang Y. Mao C. Xie X. Lin Y. (2021). The biological applications of DNA nanomaterials: current challenges and future directions. Signal Transduct. Target. Ther.6, 351. 10.1038/s41392-021-00727-9
70
Makabenta J. M. V. Nabawy A. Li C.-H. Schmidt-Malan S. Patel R. Rotello V. M. (2021). Nanomaterial-based therapeutics for antibiotic-resistant bacterial infections. Nat. Rev. Microbiol.19, 23–36. 10.1038/s41579-020-0420-1
71
Manandhar B. Paudel K. R. Panth N. Hansbro P. Oliver B. G. Dua K. (2022). Applications of extracellular vesicles as a drug-delivery system for chronic respiratory diseases. Future Med.17, 817–820. 10.2217/nnm-2021-0384
72
Mansoori B. Baradaran B. Nazari A. Gaballu F. A. Cho W.C.-S. Mansoori B. (2022). MicroRNAs in the cancer cell-to-cell communication: an insight into biological vehicles. Biomed. and Pharmacother.153, 113449. 10.1016/j.biopha.2022.113449
73
Mansur S. Habib S. Hawkins M. Brown S. R. Weinman S. T. Bao Y. (2023). Preparation of nanoparticle-loaded extracellular vesicles using direct flow filtration. Pharmaceutics15, 1551. 10.3390/pharmaceutics15051551
74
Mardpour S. Ghanian M. H. Sadeghi-Abandansari H. Mardpour S. Nazari A. Shekari F. et al (2019). Hydrogel-mediated sustained systemic delivery of mesenchymal stem cell-derived extracellular vesicles improves hepatic regeneration in chronic liver failure. ACS Appl. Mater. and interfaces11, 37421–37433. 10.1021/acsami.9b10126
75
Meng Q.-F. Tai W. Tian M. Zhuang X. Pan Y. Lai J. et al (2023). Inhalation delivery of dexamethasone with iSEND nanoparticles attenuates the COVID-19 cytokine storm in mice and nonhuman primates. Sci. Adv.9, eadg3277. 10.1126/sciadv.adg3277
76
Meng Q. F. Zhao Y. Dong C. Liu L. Pan Y. Lai J. et al (2021). Genetically programmable fusion cellular vesicles for cancer immunotherapy. Angew. Chem. Int. Ed.60, 26320–26326. 10.1002/anie.202108342
77
Meng W. He C. Hao Y. Wang L. Li L. Zhu G. (2020). Prospects and challenges of extracellular vesicle-based drug delivery system: considering cell source. Drug Deliv.27, 585–598. 10.1080/10717544.2020.1748758
78
Midekessa G. Godakumara K. Ord J. Viil J. LäTtekivi F. Dissanayake K. et al (2020). Zeta potential of extracellular vesicles: toward understanding the attributes that determine colloidal stability. ACS omega5, 16701–16710. 10.1021/acsomega.0c01582
79
Mittal S. Gupta P. Chaluvally-Raghavan P. Pradeep S. (2020). Emerging role of extracellular vesicles in immune regulation and cancer progression. Cancers12, 3563. 10.3390/cancers12123563
80
Mol E. A. Lei Z. Roefs M. T. Bakker M. H. Goumans M. J. Doevendans P. A. et al (2019). Injectable supramolecular ureidopyrimidinone hydrogels provide sustained release of extracellular vesicle therapeutics. Adv. Healthc. Mater.8, 1900847. 10.1002/adhm.201900847
81
Mondal J. Pillarisetti S. Junnuthula V. Saha M. Hwang S. R. Park I.-K. et al (2023). Hybrid exosomes, exosome-like nanovesicles and engineered exosomes for therapeutic applications. J. Control. Release353, 1127–1149. 10.1016/j.jconrel.2022.12.027
82
Mundekkad D. Cho W. C. (2022). Nanoparticles in clinical translation for cancer therapy. Int. J. Mol. Sci.23, 1685. 10.3390/ijms23031685
83
Murugesan R. (2021). “Advanced characterization and techniques,” in 2D functional nanomaterials: synthesis, characterization and applications, 141–156.
84
Nair S. Salomon C. (2020). Extracellular vesicles as critical mediators of maternal-fetal communication during pregnancy and their potential role in maternal metabolism. Placenta98, 60–68. 10.1016/j.placenta.2020.06.011
85
Naskar A. Cho H. Kim K.-S. (2022). A nanocomposite with extracellular vesicles from Lactobacillus paracasei as a bioinspired nanoantibiotic targeting Staphylococcus aureus. Pharmaceutics14, 2273. 10.3390/pharmaceutics14112273
86
Naskar A. Kim K.-S. (2019). Nanomaterials as delivery vehicles and components of new strategies to combat bacterial infections: advantages and limitations. Microorganisms7, 356. 10.3390/microorganisms7090356
87
Nasrollahzadeh M. Sajjadi M. Soufi G. J. Iravani S. Varma R. S. (2020). Nanomaterials and nanotechnology-associated innovations against viral infections with a focus on coronaviruses. Nanomaterials10, 1072. 10.3390/nano10061072
88
Natale F. Fusco S. Grassi C. (2022). Dual role of brain-derived extracellular vesicles in dementia-related neurodegenerative disorders: cargo of disease spreading signals and diagnostic-therapeutic molecules. Transl. Neurodegener.11, 50. 10.1186/s40035-022-00326-w
89
Nguyen V. V. Witwer K. W. Verhaar M. C. Strunk D. Van Balkom B. W. (2020). Functional assays to assess the therapeutic potential of extracellular vesicles. J. Extracell. vesicles10, e12033. 10.1002/jev2.12033
90
Nielsen J. E. Maltesen R. G. Havelund J. F. Færgeman N. J. Gotfredsen C. H. Vestergård K. et al (2021). Characterising Alzheimer's disease through integrative NMR-and LC-MS-based metabolomics. Metab. open12, 100125. 10.1016/j.metop.2021.100125
91
Nieuwland R. Siljander P.R.-M. Falcón-Pérez J. M. Witwer K. W. (2022). Reproducibility of extracellular vesicle research. Eur. J. cell Biol.101, 151226. 10.1016/j.ejcb.2022.151226
92
Niu W. Xiao Q. Wang X. Zhu J. Li J. Liang X. et al (2021). A biomimetic drug delivery system by integrating grapefruit extracellular vesicles and doxorubicin-loaded heparin-based nanoparticles for glioma therapy. Nano Lett.21, 1484–1492. 10.1021/acs.nanolett.0c04753
93
Noble J. M. Roberts L. M. Vidavsky N. Chiou A. E. Fischbach C. Paszek M. J. et al (2020). Direct comparison of optical and electron microscopy methods for structural characterization of extracellular vesicles. J. Struct. Biol.210, 107474. 10.1016/j.jsb.2020.107474
94
Notaguchi M. Pallas V. Qiu J. Wang X. (2022). Editorial: systemic RNA signalling in plants. Front. plant Sci.13, 878728. 10.3389/fpls.2022.878728
95
Paganini C. Capasso Palmiero U. Pocsfalvi G. Touzet N. Bongiovanni A. Arosio P. (2019). Scalable production and isolation of extracellular vesicles: available sources and lessons from current industrial bioprocesses. Biotechnol. J.14, 1800528. 10.1002/biot.201800528
96
Paisrisarn P. Yasui T. Zhu Z. Klamchuen A. Kasamechonchung P. Wutikhun T. et al (2022). Tailoring ZnO nanowire crystallinity and morphology for label-free capturing of extracellular vesicles. Nanoscale14, 4484–4494. 10.1039/d1nr07237d
97
Palanisamy C. P. Pei J. Alugoju P. Anthikapalli N. V. A. Jayaraman S. Veeraraghavan V. P. et al (2023). New strategies of neurodegenerative disease treatment with extracellular vesicles (EVs) derived from mesenchymal stem cells (MSCs). Theranostics13, 4138–4165. 10.7150/thno.83066
98
Pan R. He T. Zhang K. Zhu L. Lin J. Chen P. et al (2023). “Tumor-targeting extracellular vesicles loaded with siS100A4 for suppressing postoperative breast cancer metastasis,” in Cellular and molecular bioengineering, 1–9.
99
Paolillo M. Comincini S. Schinelli S. (2021). Fostering “education”: do extracellular vesicles exploit their own delivery code?Cells10, 1741. 10.3390/cells10071741
100
Patil K. C. Soekmadji C. (2021). Extracellular vesicle-mediated bone remodeling and bone metastasis: implications in prostate cancer. New Front. Extracell. Vesicles97, 297–361. 10.1007/978-3-030-67171-6_12
101
Peeters B. W. Piët A. C. Fornerod M. (2022). Generating membrane curvature at the nuclear pore: a lipid point of view. Cells11, 469. 10.3390/cells11030469
102
Pirisinu M. Pham T. C. Zhang D. X. Hong T. N. Nguyen L. T. Le M. T. (2022). “Extracellular vesicles as natural therapeutic agents and innate drug delivery systems for cancer treatment: recent advances, current obstacles, and challenges for clinical translation,” in Seminars in cancer biology (Elsevier), 340–355.
103
Pizzicannella J. Diomede F. Gugliandolo A. Chiricosta L. Bramanti P. Merciaro I. et al (2019). 3D printing PLA/gingival stem cells/EVs upregulate miR-2861 and-210 during osteoangiogenesis commitment. Int. J. Mol. Sci.20, 3256. 10.3390/ijms20133256
104
Pusta A. Tertis M. Crăciunescu I. Turcu R. Mirel S. Cristea C. (2023). Recent advances in the development of drug delivery applications of magnetic nanomaterials. Pharmaceutics15, 1872. 10.3390/pharmaceutics15071872
105
Qiao Z. Zhang K. Liu J. Cheng D. Yu B. Zhao N. et al (2022). Biomimetic electrodynamic nanoparticles comprising ginger-derived extracellular vesicles for synergistic anti-infective therapy. Nat. Commun.13, 7164. 10.1038/s41467-022-34883-5
106
Rani S. Lai A. Nair S. Sharma S. Handberg A. Carrion F. et al (2023). Extracellular vesicles as mediators of cell-cell communication in ovarian cancer and beyond–A lipids focus. Cytokine and Growth Factor Rev.73, 52–68. 10.1016/j.cytogfr.2023.06.004
107
Ritter A. Kreis N.-N. Hoock S. C. Solbach C. Louwen F. Yuan J. (2022). Adipose tissue-derived mesenchymal stromal/stem cells, obesity and the tumor microenvironment of breast cancer. Cancers14, 3908. 10.3390/cancers14163908
108
Rogo U. Fambrini M. Pugliesi C. (2023). Embryo rescue in plant breeding. Plants12, 3106. 10.3390/plants12173106
109
Rufino-Ramos D. Albuquerque P. R. Carmona V. Perfeito R. Nobre R. J. De Almeida L. P. (2017). Extracellular vesicles: novel promising delivery systems for therapy of brain diseases. J. Control. Release262, 247–258. 10.1016/j.jconrel.2017.07.001
110
Sancho-Albero M. Rubio-Ruiz B. Pérez-López A. M. Sebastián V. Martín-Duque P. Arruebo M. et al (2019). Cancer-derived exosomes loaded with ultrathin palladium nanosheets for targeted bioorthogonal catalysis. Nat. Catal.2, 864–872. 10.1038/s41929-019-0333-4
111
Schubert A. Boutros M. (2021). Extracellular vesicles and oncogenic signaling. Mol. Oncol.15, 3–26. 10.1002/1878-0261.12855
112
Shaimardanova A. A. Solovyeva V. V. Chulpanova D. S. James V. Kitaeva K. V. Rizvanov A. A. (2020). Extracellular vesicles in the diagnosis and treatment of central nervous system diseases. Neural Regen. Res.15, 586. 10.4103/1673-5374.266908
113
Shang L. Xie Q. Yang C. Kong L. Zhang Z. (2023). Extracellular vesicles facilitate the transportation of nanoparticles within and between cells for enhanced tumor therapy. ACS Appl. Mater. and Interfaces15, 42378–42394. 10.1021/acsami.3c10237
114
Sheth M. Esfandiari L. (2022). Bioelectric dysregulation in cancer initiation, promotion, and progression. Front. Oncol.12, 846917. 10.3389/fonc.2022.846917
115
Shimomura T. Seino R. Umezaki K. Shimoda A. Ezoe T. Ishiyama M. et al (2021). New lipophilic fluorescent dyes for labeling extracellular vesicles: characterization and monitoring of cellular uptake. Bioconjugate Chem.32, 680–684. 10.1021/acs.bioconjchem.1c00068
116
Sidhom K. Obi P. O. Saleem A. (2020). A review of exosomal isolation methods: is size exclusion chromatography the best option?Int. J. Mol. Sci.21, 6466. 10.3390/ijms21186466
117
Silachev D. N. (2023). Study of the molecular mechanisms of the therapeutic properties of extracellular vesiclesInt. J. Mol. Sci.24 (8), 7093. 10.3390/ijms24087093
118
Skotland T. Sagini K. Sandvig K. Llorente A. (2020). An emerging focus on lipids in extracellular vesicles. Adv. drug Deliv. Rev.159, 308–321. 10.1016/j.addr.2020.03.002
119
Song J. Yu S. Yang R. Xiao J. Liu J. (2023). Opportunities for the use of selenium nanoparticles in agriculture. NanoImpact31, 100478. 10.1016/j.impact.2023.100478
120
Song M. Cui M. Fang Z. Liu K. (2022). Advanced research on extracellular vesicles based oral drug delivery systems. J. Control. Release351, 560–572. 10.1016/j.jconrel.2022.09.043
121
Song T. Lv M. Zhang L. Zhang X. Song G. Huang M. et al (2020). The protective effects of tripeptides VPP and IPP against small extracellular vesicles from angiotensin II-induced vascular smooth muscle cells mediating endothelial dysfunction in human umbilical vein endothelial cells. J. Agric. Food Chem.68, 13730–13741. 10.1021/acs.jafc.0c05698
122
Soufi G. J. Iravani S. (2020). Eco-friendly and sustainable synthesis of biocompatible nanomaterials for diagnostic imaging: current challenges and future perspectives. Green Chem.22, 2662–2687. 10.1039/d0gc00734j
123
Tan D. Zhu W. Liu L. Pan Y. Xu Y. Huang Q. et al (2023). In situ formed scaffold with royal jelly-derived extracellular vesicles for wound healing. Theranostics13, 2811–2824. 10.7150/thno.84665
124
Teng F. Fussenegger M. (2021). Shedding light on extracellular vesicle biogenesis and bioengineering. Adv. Sci.8, 2003505. 10.1002/advs.202003505
125
Thangaraju K. Neerukonda S. N. Katneni U. Buehler P. W. (2020). Extracellular vesicles from red blood cells and their evolving roles in health, coagulopathy and therapy. Int. J. Mol. Sci.22, 153. 10.3390/ijms22010153
126
Tian T. Qiao S. Tannous B. A. (2022). Nanotechnology-inspired extracellular vesicles theranostics for diagnosis and therapy of central nervous system diseases. ACS Appl. Mater. and Interfaces15, 182–199. 10.1021/acsami.2c07981
127
Tiwari S. Kumar V. Randhawa S. Verma S. K. (2021). Preparation and characterization of extracellular vesicles. Am. J. Reproductive Immunol.85, e13367. 10.1111/aji.13367
128
Tripathi D. Hajra K. Maity D. (2023). Recent advancement of bio-inspired nanoparticles in cancer theragnostic. J. Nanotheranostics4, 299–322. 10.3390/jnt4030014
129
Trubiani O. Marconi G. D. Pierdomenico S. D. Piattelli A. Diomede F. Pizzicannella J. (2019). Human oral stem cells, biomaterials and extracellular vesicles: a promising tool in bone tissue repair. Int. J. Mol. Sci.20, 4987. 10.3390/ijms20204987
130
Van Niel G. Carter D. R. Clayton A. Lambert D. W. Raposo G. Vader P. (2022). Challenges and directions in studying cell–cell communication by extracellular vesicles. Nat. Rev. Mol. Cell Biol.23, 369–382. 10.1038/s41580-022-00460-3
131
Wagner K. T. Nash T. R. Liu B. Vunjak-Novakovic G. Radisic M. (2021). Extracellular vesicles in cardiac regeneration: potential applications for tissues-on-a-chip. Trends Biotechnol.39, 755–773. 10.1016/j.tibtech.2020.08.005
132
Wang J. Zhu M. Nie G. (2021). Biomembrane-based nanostructures for cancer targeting and therapy: from synthetic liposomes to natural biomembranes and membrane-vesicles. Adv. drug Deliv. Rev.178, 113974. 10.1016/j.addr.2021.113974
133
Wang T. Koukoulis T. F. Vella L. J. Su H. Purnianto A. Nie S. et al (2023a). The proteome and lipidome of extracellular vesicles from Haemonchus contortus to underpin explorations of host–parasite cross–talk. Int. J. Mol. Sci.24, 10955. 10.3390/ijms241310955
134
Wang Z. Wang X. Xu W. Li Y. Lai R. Qiu X. et al (2023b). Translational challenges and prospective solutions in the implementation of biomimetic delivery systems. Pharmaceutics15, 2623. 10.3390/pharmaceutics15112623
135
Worthington E. N. Hagood J. S. (2020). Therapeutic use of extracellular vesicles for acute and chronic lung disease. Int. J. Mol. Sci.21, 2318. 10.3390/ijms21072318
136
Wu H. Xing H. Wu M.-C. Shen F. Chen Y. Yang T. (2021). Extracellular-vesicles delivered tumor-specific sequential nanocatalysts can be used for MRI-informed nanocatalytic Therapy of hepatocellular carcinoma. Theranostics11, 64–78. 10.7150/thno.46124
137
Wu M.-S. Zhou Z.-R. Wang X.-Y. Lv J. Li D.-W. Qian R.-C. (2023a). Engineered extracellular vesicle-encapsuled nanoreactors for effective targeting and cascade killing of cancer cells. ACS Appl. Bio Mater.6, 1479–1487. 10.1021/acsabm.2c01019
138
Wu Q. Fu S. Xiao H. Du J. Cheng F. Wan S. et al (2023b). Advances in extracellular vesicle nanotechnology for precision theranostics. Adv. Sci.10, 2204814. 10.1002/advs.202204814
139
Xu C. Wang Z. Liu Y. Wei B. Liu X. Duan K. et al (2023a). Extracellular vesicles derived from bone marrow mesenchymal stem cells loaded on magnetic nanoparticles delay the progression of diabetic osteoporosis via delivery of miR-150-5p. Cell Biol. Toxicol.39, 1257–1274. 10.1007/s10565-022-09744-y
140
Xu M. Han X. Xiong H. Gao Y. Xu B. Zhu G. et al (2023b). Cancer nanomedicine: emerging strategies and therapeutic potentials. Molecules28, 5145. 10.3390/molecules28135145
141
Xu Y. Feng K. Zhao H. Di L. Wang L. Wang R. (2022). Tumor-derived extracellular vesicles as messengers of natural products in cancer treatment. Theranostics12, 1683–1714. 10.7150/thno.67775
142
Yang L. Patel K. D. Rathnam C. Thangam R. Hou Y. Kang H. et al (2022). Harnessing the therapeutic potential of extracellular vesicles for biomedical applications using multifunctional magnetic nanomaterials. Small18, 2104783. 10.1002/smll.202104783
143
Yang M. Liu X. Luo Q. Xu L. Chen F. (2020). An efficient method to isolate lemon derived extracellular vesicles for gastric cancer therapy. J. nanobiotechnology18, 100–112. 10.1186/s12951-020-00656-9
144
Yang Y. Zhu Z. Gao R. Yuan J. Zhang J. Li H. et al (2021a). Controlled release of MSC-derived small extracellular vesicles by an injectable Diels-Alder crosslinked hyaluronic acid/PEG hydrogel for osteoarthritis improvement. Acta biomater.128, 163–174. 10.1016/j.actbio.2021.04.003
145
Yang Z. Liu D. Zhou H. Tao B. Chang L. Liu H. et al (2021b). A new nanomaterial based on extracellular vesicles containing chrysin-induced cell apoptosis through let-7a in tongue squamous cell carcinoma. Front. Bioeng. Biotechnol.9, 766380. 10.3389/fbioe.2021.766380
146
Yaraki M. T. Tukova A. Wang Y. (2022). Emerging SERS biosensors for the analysis of cells and extracellular vesicles. Nanoscale14, 15242–15268. 10.1039/d2nr03005e
147
Yom-Tov N. Guy R. Offen D. (2022). Extracellular vesicles over adeno-associated viruses: advantages and limitations as drug delivery platforms in precision medicine. Adv. drug Deliv. Rev.190, 114535. 10.1016/j.addr.2022.114535
148
Yu T.-Y. Xu C.-X. Li W.-J. Wang B. Cai G. Takeuchi H. et al (2023). SPECIALTY SECTION this article was submitted to plant cell biology, a section of the journal frontiers in plant science, II. Regulation of Pollen Tube Growth, 59.
149
Zhang C. Shang Y. Chen X. Midgley A. C. Wang Z. Zhu D. et al (2020). Supramolecular nanofibers containing arginine-glycine-aspartate (RGD) peptides boost therapeutic efficacy of extracellular vesicles in kidney repair. ACS nano14, 12133–12147. 10.1021/acsnano.0c05681
150
Zhang K. Zhao X. Chen X. Wei Y. Du W. Wang Y. et al (2018). Enhanced therapeutic effects of mesenchymal stem cell-derived exosomes with an injectable hydrogel for hindlimb ischemia treatment. ACS Appl. Mater. and interfaces10, 30081–30091. 10.1021/acsami.8b08449
151
Zhang L. Liu J. Zhou C. (2023). Current aspects of small extracellular vesicles in pain process and relief. Biomaterials Res.27, 78. 10.1186/s40824-023-00417-3
152
Zhang X. Zhang H. Gu J. Zhang J. Shi H. Qian H. et al (2021). Engineered extracellular vesicles for cancer therapy. Adv. Mater.33, 2005709. 10.1002/adma.202005709
153
Zhou Q. Ma K. Hu H. Xing X. Huang X. Gao H. (2022a). Extracellular vesicles: their functions in plant–pathogen interactions. Mol. Plant Pathol.23, 760–771. 10.1111/mpp.13170
154
Zhou Q. Yan Y. Li Y. Fu H. Lu D. Li Z. et al (2022b). Tumor-derived extracellular vesicles in melanoma immune response and immunotherapy. Biomed. and Pharmacother.156, 113790. 10.1016/j.biopha.2022.113790
155
Zhu W. Dong Y. Xu P. Pan Q. Jia K. Jin P. et al (2022). A composite hydrogel containing resveratrol-laden nanoparticles and platelet-derived extracellular vesicles promotes wound healing in diabetic mice. Acta Biomater.154, 212–230. 10.1016/j.actbio.2022.10.038
156
Zinger A. Brozovich A. Pasto A. Sushnitha M. Martinez J. O. Evangelopoulos M. et al (2020). Bioinspired extracellular vesicles: lessons learned from nature for biomedicine and bioengineering. Nanomaterials10, 2172. 10.3390/nano10112172
157
Zonneveld M. I. Van Herwijnen M. J. Fernandez‐Gutierrez M. M. Giovanazzi A. De Groot A. M. Kleinjan M. et al (2021). Human milk extracellular vesicles target nodes in interconnected signalling pathways that enhance oral epithelial barrier function and dampen immune responses. J. Extracell. Vesicles10, e12071. 10.1002/jev2.12071
Summary
Keywords
engineered nanomaterials, extracellular vesicles, characterization, targeted drug delivery, biomedical applications
Citation
Jiang H, Kumarasamy RV, Pei J, Raju K, Kanniappan GV, Palanisamy CP and Mironescu ID (2025) Integrating engineered nanomaterials with extracellular vesicles: advancing targeted drug delivery and biomedical applications. Front. Nanotechnol. 6:1513683. doi: 10.3389/fnano.2024.1513683
Received
18 October 2024
Accepted
11 December 2024
Published
22 January 2025
Volume
6 - 2024
Edited by
Mona Khafaji, Sharif University of Technology, Iran
Reviewed by
Gopal Niraula, Iowa State University, United States
Nishtha Lukhmana, University of Georgia, United States
Updates
Copyright
© 2025 Jiang, Kumarasamy, Pei, Raju, Kanniappan, Palanisamy and Mironescu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gopalakrishnan Velliyur Kanniappan, vkgopalakrishnan@gmail.com; Chella Perumal Palanisamy, perumalbioinfo@gmail.com; Ion Dan Mironescu, ion.mironescu@ulbsibiu.ro
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.