- 1Department of Neurosurgery, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 2Department of Obstetrics and Gynecology, TCM Hospital Affiliated of Southwest Medical University, Luzhou, China
- 3Neurosurgery Clinical Medical Research Center of Sichuan Province, Luzhou, China
- 4Academician (Expert) Workstation of Sichuan Province, The Affiliated Hospital of Southwest Medical University, Luzhou, China
- 5Laboratory of Neurological Diseases and Brain Functions, The Affiliated Hospital of Southwest Medical University, Luzhou, China
Background: While studies have confirmed that flow diversion (FD) can treat intracranial aneurysms via transradial approach (TRA), it remains unclear whether their treatment ultimately impacts safety and feasibility. We aim to conduct a systematic review and meta-analysis assessing the safety and feasibility after FD treatment of intracranial aneurysms via TRA.
Methods: PubMed, EMBASE, and Web of Science were systematically reviewed. The primary outcomes were the success rate and the access-related complications of deploying FD via TRA. Meta-analysis was performed using a random or fixed effect model based on heterogeneity. And the publication bias was evaluated using a funnel plot. This study was registered with PROSPERO, number CRD42021244448.
Results: Data from 8 studies met inclusion criteria (250 non-duplicated patients). The success rate was 93% (95% confidence interval [CI] 0.86–0.98; I2 = 61.05%; p = 0.01). The access-related complications rate was 1% (95% CI 0–0.03; I2 = 0.00%; p < 0.01). The mainly access-related complications included radial artery spasm (85.7%) and radial artery occlusion (14.3%). The TRA convert to transfemoral approach (TFA) was 7% (95% CI 0.02–0.14; I2 = 61.05%; p = 0.01).
Conclusions: Although TFA is still the main access for FD in the treatment of intracranial aneurysms, the TRA also has a higher success rate and lower access-related complications rate. With the improvement of future experience and equipment, the TRA may become the main access for FD which has more advantages. Future studies should design prospective, multicenter randomized controlled studies for long-term follow-up.
Introduction
In interventional cardiology, the advantages of the TRA are more and more obvious than that of the TFA (1, 2). Meanwhile, TRA gradually began to pay attention to the field of neurointervention (3–5).
With the development of Interventional Neurology, flowdiversion (FD) has become an important complementary treatment for coils and stents (6). Although some studies have shown that FD is effective and safe for the treatment of intracranial aneurysms via TRA, its data are limited. There were only some meta-analyses of diagnostic cerebral angiography and mechanical embolectomy (7, 8). Therefore, we conducted the first meta-analysis to illustrate the feasibility and safety of FD in the treatment of intracranial aneurysms via TRA. This study may be helpful to provide benchmark numbers to guide surgeons choose the appropriate access when using FD to treat intracranial aneurysms.
Methods
This study was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (9).
Search Strategy
We conducted a comprehensive literature search of the PubMed, EMBASE, and Web of Science databases for studies published from their dates of inception to May 2021. The title and abstract were searched using combinations of the following search terms: (divert OR diverts OR diversion OR flow-diverter OR flow diversion OR pipeline embolization device OR PED OR pipeline OR flow diverters OR diverters) AND (Intracranial Aneurysm OR Aneurysms, Intracranial OR Intracranial Aneurysms OR Aneurysm, Intracranial OR Brain Aneurysm OR Aneurysm, Brain OR Aneurysms, Brain OR Brain Aneurysms OR Cerebral Aneurysm OR Aneurysms, Cerebral OR Cerebral Aneurysms OR Aneurysm, Cerebral) AND (Radial Artery OR Arteries, Radial OR Artery, Radial OR Radial Arteries OR transradial OR radial OR transradial access OR transradial approach).
Selection Criteria
The inclusion criteria were (1) treatment of aneurysms with FD via TRA; (2) ≥5 patients with an aneurysm; (3) and the clinical or angiographic outcomes of aneurysms reported. The exclusion criteria were as follows: (1) unextractable or unclear data; (2) duplicated reports; (3) meta-analyses, reviews, comments, letters, and non-English language studies.
Data Extraction and Item Definition
The following information was extracted from the included studies: first author, publication year, the number of procedures treated by FD via TRA, baseline patient information, the number of stents successfully placed via the TRA, the access-related complications, and the number of the conversion from the TRA to the TFA. Data extraction was performed by Xiang Liu and Wenzhang Luo. Any disagreement during article selection was resolved by a discussion with a third author (Changren Huang). The success rate refers to the successful placement of FD via TRA rather than via TFA. The access-related complications include radial artery spasm, radial artery occlusion, forearm hematoma, and forearm osteofascial space syndrome.
Critical Appraisal
The study quality was assessed using the modified Newcastle–Ottawa scale for case series (10). It mainly includes selection, ascertainment, causality, and reporting.
Statistical Analysis
This meta-analysis was performed using Stata, version 14.0 (StataCorp, College Station, Texas, USA). The main outcome was the success rate of procedures and the access-related complications. The secondary result was the conversion rate of TRA. Continuous variables are presented as mean values. Dichotomous variables are presented as efficient with 95% confidence intervals (CI). The statistical heterogeneity was assessed using I2. A fixed-effects model was used if I2 < 50% and a random-effects model was used if I2 > 50%. An alpha level of significance was set to 0.05 and 95% CI.
Results
Search Results
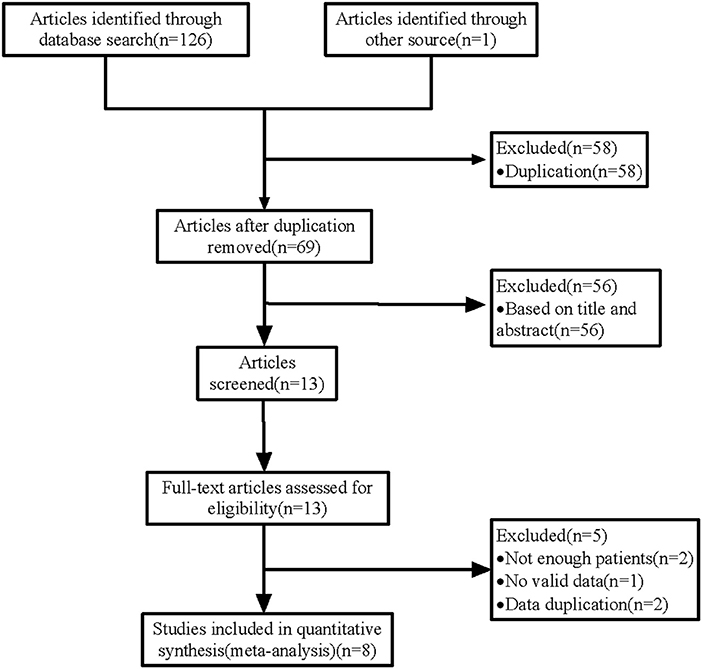
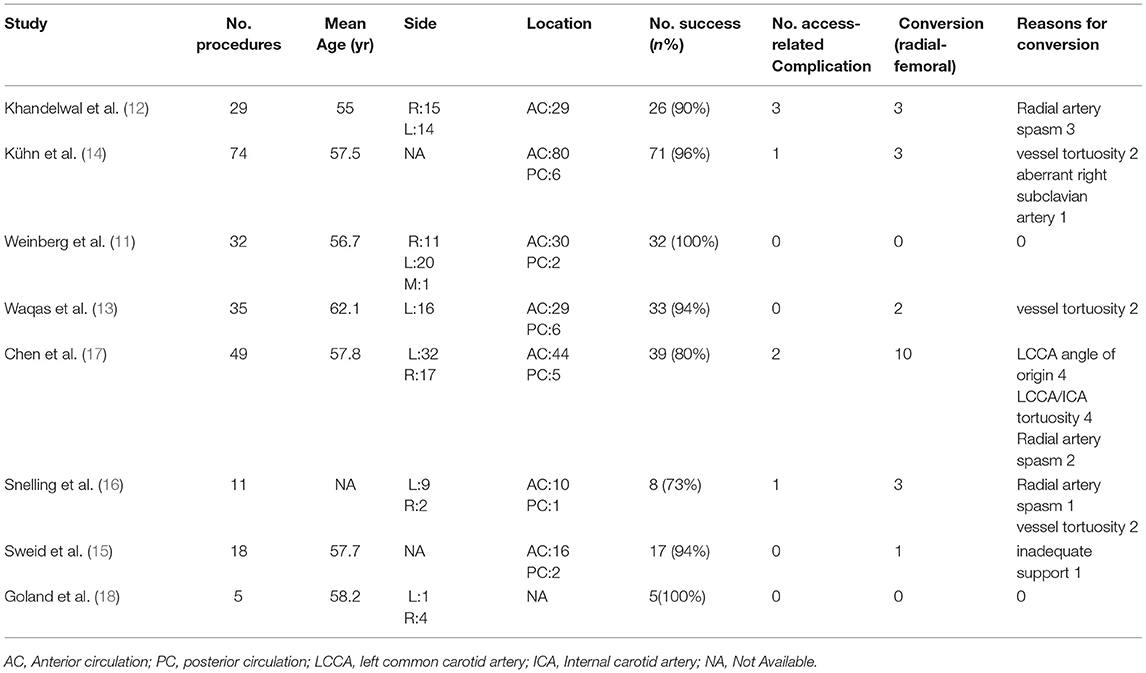
Our search rendered 127 studies (Figure 1). After duplicate removal and abstract screening, 13 studies remained for full-text screening. After reading the full text, we included 8 studies (11–18) in the meta-analysis. The 8 studies involved 265 FD-treated aneurysms via TRA in 250 patients. All studies were single- or multi-center retrospective analyses. Table 1 shows the quality evaluation of 8 studies and their characteristics are summarized in Table 2.
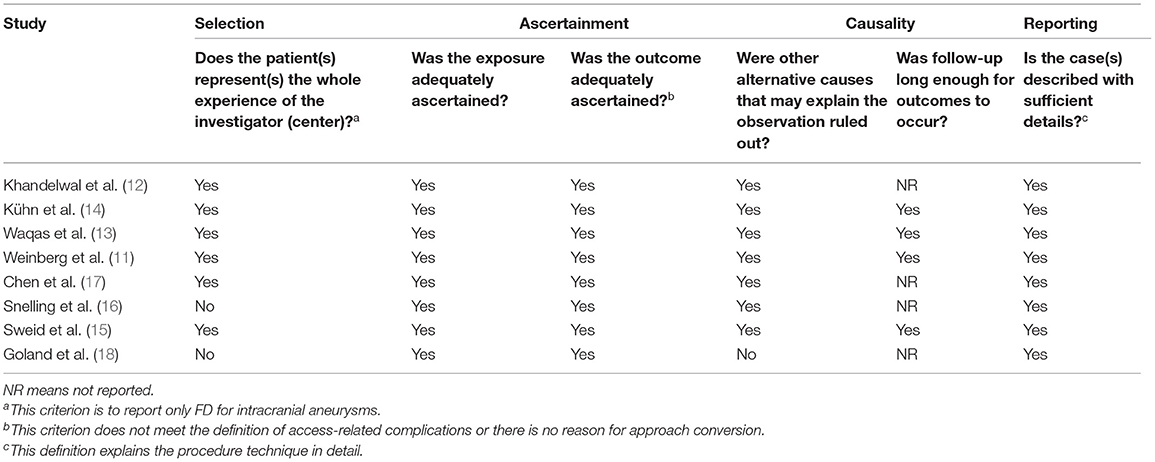
Table 1. Evaluation of the included studies using the criteria described by Murad et al. (10).
Clinical Characteristics
The average age of the 8 studies included was 55–62.1 years. Six studies (11–13, 16–18) reported the laterality of aneurysms, 57.1% (92/161) of which were located on the left side and 7 studies (11–17) reported that 91.5% (238/260) of aneurysms were located in the anterior circulation. The 8 studies described in detail the use of drugs and operative procedures before operation.
Procedural Success
In this meta-analysis, 253 cases of intracranial aneurysms were treated with FD via TRA, of which 231 cases were successful. Based on the meta-analysis of random effects, the total effect amount of 8 studies was 93% (95% CI 0.86–0.98; I2 = 61.05%; p = 0.01; Figure 2). The funnel plot showed there was no significant publication bias.
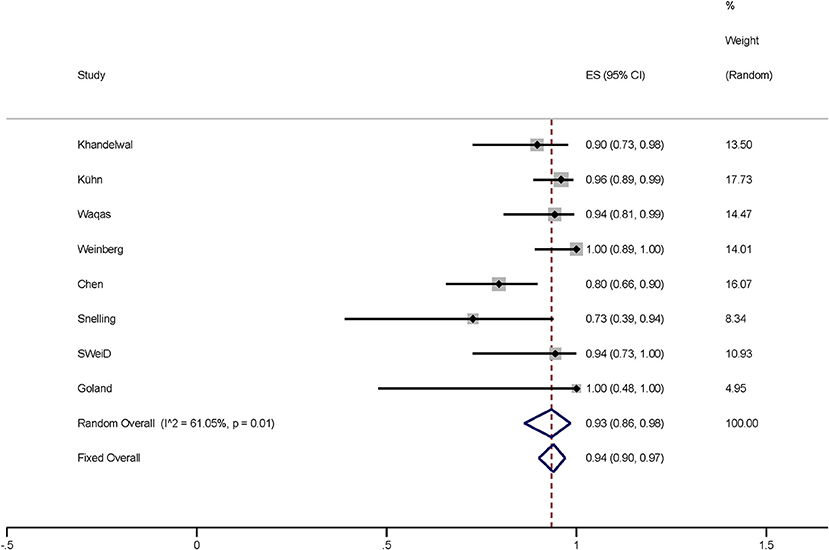
Figure 2. Plot showing the success rate of 265 FD-treated intracranial aneurysms via TRA, reported by eight studies. FD, flow diversion; TRA, transradial approach; CI, confidence interval.
Complications
The access-related complications include radial artery spasm and radial artery occlusion. Complications occurred in four of these studies (12, 14, 16, 17). Based on the meta-analysis of fixed effects, the access-related complications rate was 1% (95% CI 0–0.03; I2 = 0.00%; p < 0.01; Figure 3). These complications included radial artery spasm (85.7%, 6/7) and radial artery occlusion (14.3%, 1/7). The funnel plot showed there was no significant publication bias.
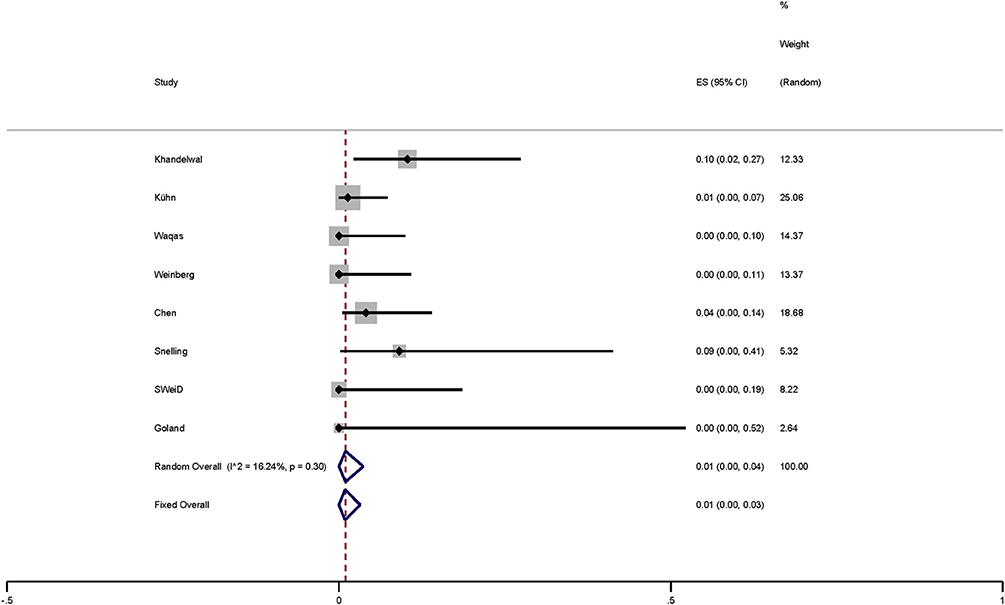
Figure 3. Plot showing the access-related complications of FD-treated intracranial aneurysms via TRA.
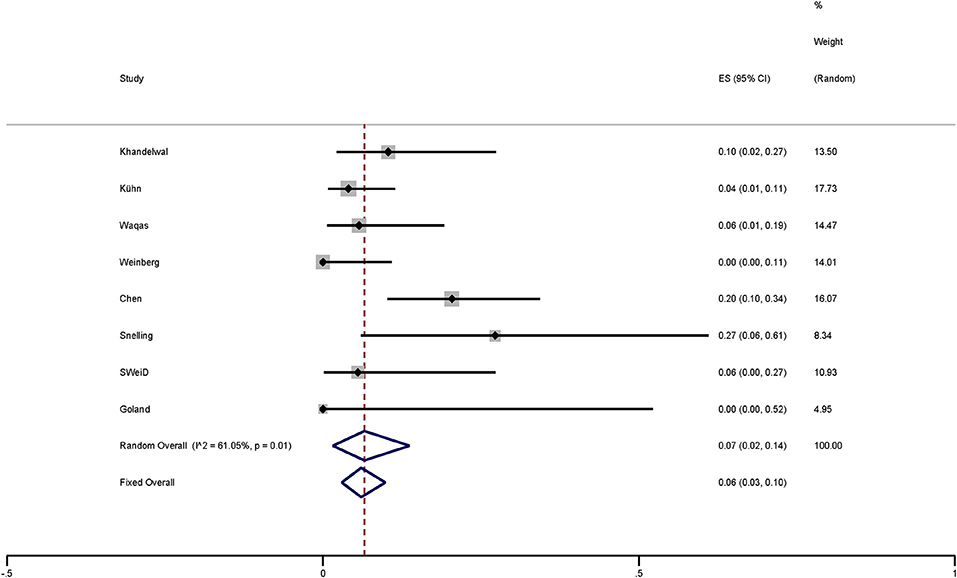
Conversion (Radial-Femoral)
Based on the meta-analysis of random effects, the conversion rate is 7% (95% CI 0.02–0.14; I2 = 61.05%; p = 0.01; Figure 4). The vessel tortuosity was the most common reason (45.5%), followed by radial artery spasm (27.3%), left common carotid artery (LCCA) angle of origin (18.2%), and inadequate support (4.5%) and aberrant right subclavian artery (4.5%). In one study (14), two cases were converted to femoral artery pathway because of vascular tortuosity and insufficient support. We think that it was caused by vascular tortuosity.
Discussion
We present the first meta-analysis demonstrating the success rate and the access-related complications rate of FD via TRA for the treatment of intracranial aneurysms. Our results demonstrate that the success rate was 93% (95% CI 0.86–0.98; I2 = 61.05%; p = 0.01) and the access-related complications rate was 1% (95% CI 0–0.03; I2 = 0.00%; p < 0.01).
The concept of “endovascular flow diversion” was proposed on the assumption that the stent can block the blood flow in the aneurysm while preserving the flow into the parent vessel and adjacent branches (19). This device has higher surface coverage and lower porosity, which can slow down the blood flow to the aneurysm, gradually form thrombosis and promote the formation of new endothelium at the neck of the aneurysm (20). With the development of materials, FD has not only been confined to the original indications, but also has been applied to acutely rupture aneurysms, posterior circulation aneurysms, carotid-cavernous fistulas, distal anterior circulation aneurysms, and blister aneurysms (21, 22). At present, FD is the most commonly used access for the treatment of intracranial aneurysms via TFA. However, with the advantages of TRA becoming more and more prominent, some studies began to treat intracranial aneurysms with FD via TRA.
Dietrich et al. (23) first reported that a large cavernous internal carotid artery aneurysm was treated with Pipeline Embolization Device (PED) via TRA due to a complex aortic arch. Other previous studies had also reported that FD in the treatment of intracranial aneurysms via TRA was mainly suitable for type III aortic arch or bovine arch configurations (24, 25). At present, it has been the preferred access in some institutions with rich experience in the treatment of intracranial aneurysms with FD via TRA (11, 13, 15). When the radial artery is less than 2.0–2.5 mm on ultrasound, some studies suggest that TFA should be chosen. Even if you want to use TRA, 071″ systems (Envoy DA with 058″ Navien or 044″ DAC) or triaxial system should be selected (17, 23). In terms of materials, the research had shown that the system suitable for TFA is also suitable for radial artery (16). At the same time, some studies suggested Barbeau testing to evaluate palm blood circulation before operation and exclude patients with a D-shape of Barbeau testing when deploying FD via TRA (16, 17). However, some studies suggested that there was no additional benefit of preoperative Barbeau testing or Allen testing for hand ischemic complications (26, 27). In our meta-analysis, only 1 case had an access-related complication of asymptomatic radial artery occlusion. In addition, all researchers performed radial artery punctures under the guidance of ultrasound in the literature we included, which significantly improved the success rate of punctures. The TRA with Ultrasound Trial (RAUST) confirmed that ultrasound guidance was helpful for the success rate and efficiency of radial artery catheterization. Compared with palpation, fewer attempts for successful puncture with the guidance of ultrasound (mean: 1.65 ± 1.2 vs. 3.05 ± 3.4, p < 0.0001) (28). After a puncture, immediately 2.5–5 mg verapamil and 200 μg nitroglycerin will be paid to prevent radial artery spasm, and some studies will also be given 5 mg nicardipine (11, 15). In our meta-analysis, the incidence of radial artery spasm was 85.7% and 27.3% turned to TFA because of radial artery spasm. Therefore, how to prevent radial artery spasm is also one of the problems that TRA will become the main access for the treatment of aneurysms with FD in the future. There are also reports of forearm hematoma and forearm osteofascial space syndrome during interventional operation via TRA (29, 30). A short sheath of 6F was routinely inserted after the puncture, and the target artery was entered through Simmons-II. An appropriate multiaxial system was supposed to place FD according to the diameter of the radial artery. Because the deployment of FD requires a larger vessel diameter, it not only increases the risk of radial artery spasm but also makes surgeons reluctant to deploy FD via TRA. The triaxial system was utilized for patients with radial artery diameter > 2.5 mm and the biaxial or triaxial system was used for patients with radial artery diameter <2.5 mm in a multicenter study. The overall success rate was 91% (122/134) and compared with TFA, which has higher access-related complications (2.48 vs. 0%, p = 0.039) (30). Their research also believed that the deployment of FD via TRA is safe and feasible. Patel et al. (31) believed that the biaxial systems could replace the triaxial systems to place FD. In our meta-analysis, the incidence of access-related complications is only 1% (95% CI 0–0.03; I2 = 0.00%; p < 0.01). On the other hand, the most important reason is that the access conversion is 63.7% owing to the vessel tortuosity and LCCA angle of origin. In the future, the development of neurointervention materials and the progress of technology may improve this situation.
Deploying FD needs to take a large dose of dual antiplatelet therapy, which increases the risk of femoral artery bleeding, prolonged compression time, and pseudoaneurysm via TFA (32). The radial artery is shallow, which is easier to stop bleeding by compression. At the same time, the TRA will not lead to the patient's bed for a long time, and will also reduce the incidence of lower extremity deep venous thrombosis (15, 33, 34). Secondly, several studies had shown that neurointerventional via TRA can reduce the discomfort of patients after interventional surgery, and reduce the cost of surgery, and length of hospital stay compared to TFA (3, 11, 35–37). Especially for patients taking anticoagulants, pregnant women, patients with severe iliac atherosclerosis, bovine arch, type II/III aortic arch, the TRA should be the main access for FD in the treatment of intracranial aneurysms (11, 38, 39).
Although the deployment of FD via TRA has more benefits for patients with intracranial aneurysms, it also has a high success rate in our meta-analysis. However, we cannot ignore the causes of his conversion to TFA and its complications. We should choose the appropriate access based on maximizing the interests of patients.
Limitations
Our study has some limitations. We only included a small number of cases without a control group which lead to selection bias, and this result is not suitable for comprehensive promotion. Further, we were unable to analyze the location of the failed aneurysm, aortic arch angles, and catheter system because of the lack of stratification. Moreover, given the lack of long-term follow-up in the included studies, we were not able to consider the cases of access-related complications that may have been missed.
Conclusions
Although TFA is still the main access for FD in the treatment of intracranial aneurysms, the TRA also has a higher success rate and lower access-related complications rate. With the improvement of future experience and equipment, the TRA may become the main access for FD which has more advantages. Future studies should design prospective, multicenter randomized controlled studies for long-term follow-up.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
Guarantor of integrity of entire study, manuscript revision and review, manuscript final version approval, and manuscript definition of intellectual content: KB and CH. Study concepts: XL and MW. Study design and data acquisition: XL and WL. Literature research: MW. Data analysis/interpretation and statistical analysis: XL, WL, and KB. Manuscript preparation: XL. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Scientific Research Project of Sichuan Provincial Health Committee, 19PJ296; Luzhou Science and Technology Plan Project, 2020-SYF-29.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
FD, flow diversion; CI, confidence interval; TRA, transradial approach; TFA, transfemoral approach; LCCA, left common carotid artery; AC, anterior circulation; PC, posterior circulation; ICA, internal carotid artery; NA, not available.
References
1. Ferrante G, Rao SV, Jüni P, Da Costa BR, Reimers B, Condorelli G, et al. Radial versus femoral access for coronary interventions across the entire spectrum of patients with coronary artery disease: a meta-analysis of randomized trials. JACC Cardiovasc Interv. (2016) 9:1419–34. doi: 10.1016/j.jcin.2016.04.014
2. Mitchell MD, Hong JA, Lee BY, Umscheid CA, Bartsch SM, Don CW. Systematic review and cost-benefit analysis of radial artery access for coronary angiography and intervention. Circ Cardiovasc Qual Outcomes. (2012) 5:454–62. doi: 10.1161/CIRCOUTCOMES.112.965269
3. Khanna O, Sweid A, Mouchtouris N, Shivashankar K, Xu V, Velagapudi L, et al. Radial artery catheterization for neuroendovascular procedures. Stroke. (2019) 50:2587–90. doi: 10.1161/STROKEAHA.119.025811
4. Chen SH, Snelling BM, Sur S, Shah SS, McCarthy DJ, Luther E, et al. Transradial versus transfemoral access for anterior circulation mechanical thrombectomy: comparison of technical and clinical outcomes. J Neurointerv Surg. (2019) 11:874–8. doi: 10.1136/neurintsurg-2018-014485
5. Snelling BM, Sur S, Shah SS, Khandelwal P, Caplan J, Haniff R, et al. Transradial cerebral angiography: techniques and outcomes. J Neurointerv Surg. (2018) 10:874–81. doi: 10.1136/neurintsurg-2017-013584
6. Wang CB, Shi WW, Zhang GX, Lu HC, Ma J. Flow diverter treatment of posterior circulation aneurysms. a meta-analysis. Neuroradiology. (2016) 58:391–400. doi: 10.1007/s00234-016-1649-2
7. Peterson C, Waldau B. Transradial access for thrombectomy in acute stroke: a systematic review and meta-analysis. Clin Neurol Neurosurg. (2020) 198:106235. doi: 10.1016/j.clineuro.2020.106235
8. Hoffman H, Jalal MS, Masoud HE, Pons RB, Rodriguez Caamaño I, Khandelwal P, et al. Distal transradial access for diagnostic cerebral angiography and neurointervention: systematic review and meta-analysis. AJNR Am J Neuroradiol. (2021) 42:888–95. doi: 10.3174/ajnr.A7074
9. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. BMJ (Clinical Research ed). (2009) 339:b2535. doi: 10.1136/bmj.b2535
10. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. (2018) 23:60–3. doi: 10.1136/bmjebm-2017-110853
11. Weinberg JH, Sweid A, Hammoud B, Asada A, Greco-Hiranaka C, Piper K, et al. A comparative study of transradial versus transfemoral approach for flow diversion. Neuroradiology. (2021) 63:1335–43. doi: 10.1007/s00234-021-02672-4
12. Khandelwal P, Majmundar N, Rodriguez GJ, Patel P, Dodson V, Singla A, et al. Dual-Center study comparing transradial and transfemoral approaches for flow diversion treatment of intracranial aneurysms. Brain Circ. (2021) 7:65–70. doi: 10.4103/bc.bc_38_20
13. Waqas M, Vakharia K, Dossani RH, Rajah GB, Tso MK, Gong AD, et al. Transradial access for flow diversion of intracranial aneurysms: case series Interv Neuroradiol. (2021) 27:68–74. doi: 10.1177/1591019920938961
14. Kühn AL, Satti SR Eden T, de Macedo Rodrigues K, Singh J, Massari F, et al. Anatomic snuffbox (Distal Radial Artery) and radial artery access for treatment of intracranial aneurysms with fda-approved flow diverters. AJNR Am J Neuroradiol. (2021) 42:487–92. doi: 10.3174/ajnr.A6953
15. Sweid A, Starke RM, Herial N, Chalouhi N, Xu V, Shivashankar K, et al. Transradial approach for the treatment of brain aneurysms using flow diversion: feasibility, safety, and outcomes. J Neurosurg Sci. (2019) 63:509–17. doi: 10.23736/S0390-5616.19.04761-1
16. Snelling BM, Sur S, Shah SS, Caplan J, Khandelwal P, Yavagal DR, et al. Transradial approach for complex anterior and posterior circulation interventions: technical nuances and feasibility of using current devices. Oper Neurosurg (Hagerstown). (2019) 17:293–302. doi: 10.1093/ons/opy352
17. Chen SH, Snelling BM, Shah SS, Sur S, Brunet MC, Starke RM, et al. Transradial approach for flow diversion treatment of cerebral aneurysms: a multicenter study. J Neurointerv Surg. (2019) 11:796–800. doi: 10.1136/neurintsurg-2018-014620
18. Goland J, Doroszuk GF, Garbugino SL, Ypa MP. Transradial approach to treating endovascular cerebral aneurysms: case series and technical note. Surg Neurol Int. (2017) 8:73. doi: 10.4103/sni.sni_393_16
19. D'Urso PI, Lanzino G, Cloft HJ, Kallmes DF. Flow diversion for intracranial aneurysms: a review. Stroke. (2011) 42:2363–8. doi: 10.1161/STROKEAHA.111.620328
20. Walcott BP, Stapleton CJ, Choudhri O, Patel AB. Flow diversion for the treatment of intracranial aneurysms. JAMA Neurol. (2016) 73:1002–8. doi: 10.1001/jamaneurol.2016.0609
21. Dandapat S, Mendez-Ruiz A, Martínez-Galdámez M, Macho J, Derakhshani S, Foa Torres G, et al. Review of current intracranial aneurysm flow diversion technology and clinical use. J Neurointerv Surg. (2021) 13:54–62. doi: 10.1136/neurintsurg-2020-015877
22. Brouillard AM, Sun X, Siddiqui AH, Lin N. The use of flow diversion for the treatment of intracranial aneurysms: expansion of indications. Cureus. (2016) 8:e472. doi: 10.7759/cureus.472
23. Dietrich C, Hauck GH, Valvassori L, Hauck EF. Transradial access or simmons shaped 8f guide enables delivery of flow diverters in patients with large intracranial aneurysms and type iii aortic arch: technical case report. Neurosurgery. (2013) 73 (Suppl. 1):5–6. doi: 10.1227/NEU.0b013e31827e0d67
24. Peitz GW, Kura B, Johnson JN, Grandhi R. Transradial approach for deployment of a flow diverter for an intracranial aneurysm in a patient with a type-3 aortic arch. J Vasc Interv Neurol. (2017) 9:42–4.
25. Daou B, Chalouhi N, Tjoumakaris S, Hasan D, Barros G, Rosenwasser RH, et al. Alternative access for endovascular treatment of cerebrovascular diseases. Clin Neurol Neurosurg. (2016) 145:89–95. doi: 10.1016/j.clineuro.2016.04.015
26. van Leeuwen MAH, Hollander MR, van der Heijden DJ, van de Ven PM, Opmeer KHM, Taverne Y, et al. The acra anatomy study (assessment of disability after coronary procedures using radial access): a comprehensive anatomic and functional assessment of the vasculature of the hand and relation to outcome after transradial catheterization. Circ Cardiovasc Interv. (2017) 10:e005753. doi: 10.1161/CIRCINTERVENTIONS.117.005753
27. Barbeau GR, Arsenault F, Dugas L, Simard S, Larivière MM. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: comparison with the Allen's test in 1010 patients. Am Heart J. (2004) 147:489–93. doi: 10.1016/j.ahj.2003.10.038
28. Seto AH, Roberts JS, Abu-Fadel MS, Czak SJ, Latif F, Jain SP, et al. Real-Time ultrasound guidance facilitates transradial access: raust (radial artery access with ultrasound trial). JACC Cardiovasc Interv. (2015) 8:283–91. doi: 10.1016/j.jcin.2014.05.036
29. Rashid M, Kwok CS, Pancholy S, Chugh S, Kedev SA, Bernat I, et al. Radial artery occlusion after transradial interventions: a systematic review and meta-analysis. J Am Heart Assoc. (2016) 5:e002686. doi: 10.1161/JAHA.115.002686
30. Li Y, Chen SH, Spiotta AM, Jabbour P, Levitt MR, Kan P, et al. Lower complication rates associated with transradial versus transfemoral flow diverting stent placement. J Neurointerv Surg. (2021) 13:91–5. doi: 10.1136/neurintsurg-2020-015992
31. Patel AS, Griessenauer CJ, Ogilvy CS, Thomas AJ. Biaxial system using the benchmark intracranial guide catheter for placement of a pipeline embolization device for intracranial aneurysms. Interv Neuroradiol. (2016) 22:402–6. doi: 10.1177/1591019916632490
32. Starke RM, Snelling B, Al-Mufti F, Gandhi CD, Lee SK, Dabus G, et al. Transarterial and transvenous access for neurointerventional surgery: report of the snis standards and guidelines committee. J Neurointerv Surg. (2020) 12:733–41. doi: 10.1136/neurintsurg-2019-015573
33. Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. (2004) 44:349–56. doi: 10.1016/j.jacc.2004.04.034
34. Almallouhi E, Al Kasab S, Sattur MG, Lena J, Jabbour PM, Sweid A, et al. Incorporation of transradial approach in neuroendovascular procedures: defining benchmarks for rates of complications and conversion to femoral access. J Neurointerv Surg. (2020) 12:1122–6. doi: 10.1136/neurintsurg-2020-015893
35. Sur S, Snelling B, Khandelwal P, Caplan JM, Peterson EC, Starke RM, et al. Transradial approach for mechanical thrombectomy in anterior circulation large-vessel occlusion. Neurosurg Focus. (2017) 42:E13. doi: 10.3171/2017.1.FOCUS16525
36. Haussen DC, Nogueira RG, DeSousa KG, Pafford RN, Janjua N, Ramdas KN, et al. Transradial access in acute ischemic stroke intervention. J Neurointerv Surg. (2016) 8:247–50. doi: 10.1136/neurintsurg-2014-011519
37. Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (rival): a randomised, parallel group, multicentre trial. Lancet (London, England). (2011) 377:1409–20. doi: 10.1016/S0140-6736(11)60404-2
38. Kedev S, Zafirovska B, Antov S, Kostov J, Spiroski I, Boshev M, et al. Total wrist access for angiography and interventions: procedural success and access site crossover in a high volume transradial center. Cardiovasc Revasc Med. (2018) 19(5 Pt B):570-4. doi: 10.1016/j.carrev.2017.12.009
39. Qi G, Sun Q, Xia Y, Wei L. Emergency percutaneous coronary intervention through the left radial artery is associated with less vascular complications than emergency percutaneous coronary intervention through the femoral artery. Clinics (São Paulo, Brazil). (2017) 72:1–4. doi: 10.6061/clinics/2017(01)01
Keywords: endovascular procedures, flow diversion, transradial approach, intracranial aneurysms, meta-analysis
Citation: Liu X, Luo W, Wang M, Huang C and Bao K (2022) Feasibility and Safety of Flow Diversion in the Treatment of Intracranial Aneurysms via Transradial Approach: A Single-Arm Meta-Analysis. Front. Neurol. 13:892938. doi: 10.3389/fneur.2022.892938
Received: 09 March 2022; Accepted: 20 June 2022;
Published: 15 July 2022.
Edited by:
Jianmin Liu, Second Military Medical University, ChinaReviewed by:
Li Li, Henan Provincial People's Hospital, ChinaXiaoxi Zhang, Naval Medical University, China
Copyright © 2022 Liu, Luo, Wang, Huang and Bao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changren Huang, Y2hhbmdyZW5odWFuZzFAc3dtdS5lZHUuY24=; Kunyang Bao, Ymt5bHpzcm15eUAxNjMuY29t
†These authors have contributed equally to this work
 Xiang Liu1
Xiang Liu1 Wenzhang Luo
Wenzhang Luo Changren Huang
Changren Huang