Abstract
Objective:
This study aimed to evaluate the effectiveness and safety of auricular acupuncture (AA) on postoperative analgesia, the degree of postoperative nausea, and the effect of inflammation after total knee arthroplasty (TKA).
Methods:
This was a single-center, placebo-controlled, randomized clinical trial. In total, 96 patients were randomly divided into an AA group with an indwelling intradermal needle (n = 48) and a sham auricular acupuncture (SAA) group with a non-penetrating placebo needle (n = 48). Intra-spinal anesthesia was adopted in both groups during surgery, and an epidural analgesic pump was implanted after surgery for 48 h. The primary outcome was the post-surgery visual analog score (VAS) of resting and movement states (at 6, 12 h and 1, 2, 3, 5, and 7 days). The secondary outcomes included additional doses of analgesic injection during the treatment, C-reactive protein (CRP) levels, erythrocyte sedimentation rate (ESR), and white blood cell (WBC) count on the 1st, 3rd, and 7th day after the operation, nausea on the 1st, 2nd, and 3rd day after the operation, the Hospital for Special Surgery Knee Score (HSS) on the 2nd and 12th week after the operation, and adverse events.
Results:
The VAS in the AA group at 6 h, 12 h, 2, 3, and 5 days after surgery were lower than those of the SAA group (p < 0.05). Among the secondary outcomes, the total dose of additional analgesic injection after surgery in the AA group was lower than that in the SAA group (p < 0.05). The serum CRP on the 1st day after operation in the AA group was lower than that in the SAA group (p < 0.05). The degree of nausea on 2nd day after surgery in the AA group was lower than that in the SAA group (p < 0.05). There was no significant difference in other outcomes (p > 0.05).
Conclusion:
In this study, AA was shown to be an effective and safe complementary and alternative therapy for pain relief after TKA, which was able to reduce the total postoperative dose of additional painkillers, decrease serum CRP 1 day after surgery, and improve the degree of postoperative nausea.
Clinical trial registration:
www.chictr.org.cn, ChiCTR2100054403.
Introduction
Knee osteoarthritis (KOA) is a chronic degenerative disease characterized by articular cartilage damage and involves the whole joint tissue (1). KOA is very common in elderly patients. Knee deformity and swelling can directly affect the function of the lower limbs, cause a series of complications, and seriously affect the quality of life of elderly patients (2).
Patients suffering from KOA are mainly treated by surgery and analgesic drugs, while total knee arthroplasty (TKA) is mostly used for patients with advanced KOA. However, TKA is often accompanied by varying degrees of persistent pain, which causes physiological and psychological adverse effects, reducing the efficacy of surgery to a certain extent (3, 4). The use of analgesics during and after surgery is associated with numerous side effects, including nausea and vomiting, respiratory depression (5), liver and kidney injury, depression (6), and adverse cardiovascular events (7). Therefore, it is particularly important to explore a method that can effectively control pain and reduce the use of analgesics.
Previous studies have found that acupuncture is primarily used to treat pain, and acupuncture has significant effects on pain relief, with high safety and few side effects (8, 9). A previous meta-analysis demonstrated that auricular point pressing, a traditional acupuncture therapy, combined with conventional analgesia can effectively relieve postoperative pain and reduce the consumption of different types of analgesic drugs (10). According to the theory of bioholography, the auricle forms a holographic reflex path from the homologically connected neurons in the brain and acts through the holographic connection of neurons in the brain (11). Therefore, abnormalities in various parts of the body cause corresponding changes in the ear through the holographic reflex path. Similarly, in the case of pain, the stimulation of ear points will also be transmitted to the corresponding organs of the body through the holographic reflex path to achieve the purpose of analgesia, while intervention away from the surgical incision site can avoid infection.
Two non-TKA randomized controlled trials (RCTs) (12, 13) have compared the use of indwelling intradermal needles in postoperative analgesia, with the results demonstrating that indwelling intradermal needles are effective in postoperative analgesia. The needles (14–17) used in previous postoperative analgesia studies were 0.2–0.22 mm in diameter and 1.2–1.5 mm in length, but the needle used in this study was 0.4 mm in diameter and 2.1 mm in length, which is larger in diameter and longer in the body than the conventional needles; thus, it is hoped that the needle will also provide better analgesia. However, there has been no previous RCT to evaluate the analgesic effect of an indwelling intradermal needle after TKA.
The underlying cause of postoperative pain is the stimulation of inflammatory factors. Serum C-reactive protein (CRP) level, erythrocyte sedimentation rate (ESR), and white blood cell (WBC) count are routine blood indicators used to assess postoperative infection as they represent inflammatory and anti-inflammatory factors in the serum of postoperative trauma (18). When an infection occurs after surgery, these indicators rise significantly. However, due to factors such as their short half-life, these indicators alone cannot be used as inflammation indicators to determine postoperative infection. Therefore, a combination of more than two indicators should be used to improve the accuracy of predicting postoperative infection after TKA (19). Additionally, numerous studies have demonstrated a positive correlation between CRP and postoperative visual analog score (VAS), suggesting that CRP may serve as an objective indicator for evaluating the postoperative analgesic effect of TKA (20–22).
Therefore, we designed a prospective sham-RCT to provide a clinical basis for the efficacy and safety of auricular indwelling intradermal needles as adjuvant analgesia to reduce the use of analgesic drugs.
Materials and methods
Study design and participants
This study was a single-center placebo-controlled RCT. The patients in the AA group received an indwelling intradermal needle and were covered by a disposable opaque circular Band-Aid, whereas the patients in the SAA group only received the Band-Aid to cover five auricular acupoints. All eligible participants provided written informed consent before the trial. This study strictly followed the Declaration of Helsinki and SPIRIT guidelines. The study was approved by the Ethics Committee of Shijiazhuang West Medical Center (No. JXXYYLL006) and registered in the Chinese Clinical Trial Registry (ChiCTR2100054403). Patients who underwent TKA in the Department of Joint Surgery of the center from November 2021 to October 2022 were recruited by conversation.
This trial was based on the Guidelines for the Diagnosis and Treatment of Osteoarthritis (2018 edition) (23) issued by the Orthopaedic Branch of the Chinese Medical Association as the criteria for the diagnosis of KOA, including (1) recurrent knee pain within the last month; (2) X-ray films (standing or weight-bearing position) showed narrowing of the joint space, sclerosis and/or cystic degeneration of the subchondral bone, and osteophyte formation at the joint edge; (3) age ≥ 50 years old; (4) morning stiffness time ≤ 30 min; and (5) a bone rub (feeling) during activity.
The inclusion criteria were as follows: patients diagnosed with KOA; conservative treatment was ineffective and met the surgical indications of TKA (24); patients undergoing primary TKA; patients and their families were fully informed, and informed consent was obtained; and patients with clear consciousness who possessed the capacity to communicate.
The exclusion criteria were as follows: strong resistance to acupuncture therapy or a history of seasickness; accompanied by pain in other parts of the body; serious medical diseases such as severe cardiovascular and cerebrovascular diseases or liver and kidney dysfunction; and dependent on or allergic to narcotic drugs.
Interventions
The patients were anesthetized by spinal anesthesia during surgery and implanted with an epidural analgesia pump after surgery. The specific equation of the analgesia pump included sufentanil citrate injection (No. H20054171, Yichang Renfu Pharmaceutical Co., Ltd.), ketorolac tropanol injection (No. H20052634, Shandong New Times Pharmaceutical Co., Ltd.), and granisetron hydrochloride injection (No. H20093415, Hebei Yipin Pharmaceutical Co., Ltd.) in 96 mL of 0.9% sodium chloride solution (the specific content of the injections was determined according to the patient’s weight, age, sex, and other factors). The conventional drug administration rate was 2 mL/h, the patient-controlled dose was 0.5 mL/15 min, and the analgesia time after operation was 48 h. Celecoxib capsules (No. H20203297, Shiyao Group Ouyi Pharmaceutical Co., Ltd.) were taken orally for 7 days after surgery at a dosage of 200 mg/capsule twice a day, 1 capsule once after breakfast and dinner.
In the AA group, on the basis of the conventional treatments, the indwelling intradermal needles (type C, specification: 0.4 mm, 2.1 mm; Yushang Zhuzhun 20,202,200,203, Henan Kangjiulai Medical Technology Co., Ltd.; Figure 1) were inserted into five auricular acupoints, including those at the shenmen (TF4), adrenal gland (TG2p), knee (AH4), subcortex (AT4), and stomach (CO4) (25) (Figure 2, this right ear in the figure was provided by the first author). The needles were used on the operated side 1 day before the operation and on the contralateral side 3 days after the operation, lasting for 5 days. The treatment was performed under strict aseptic conditions by the same acupuncturist who had obtained the doctor’s certificate. After the needle was directly pricked into the selected auricular acupoints, a disposable opaque round Band-Aid was applied to cover the site. In the SAA group, a disposable opaque circular Band-Aid was applied to patch these acupoints (26, 27).
Figure 1

Indwelling intradermal needles.
Figure 2
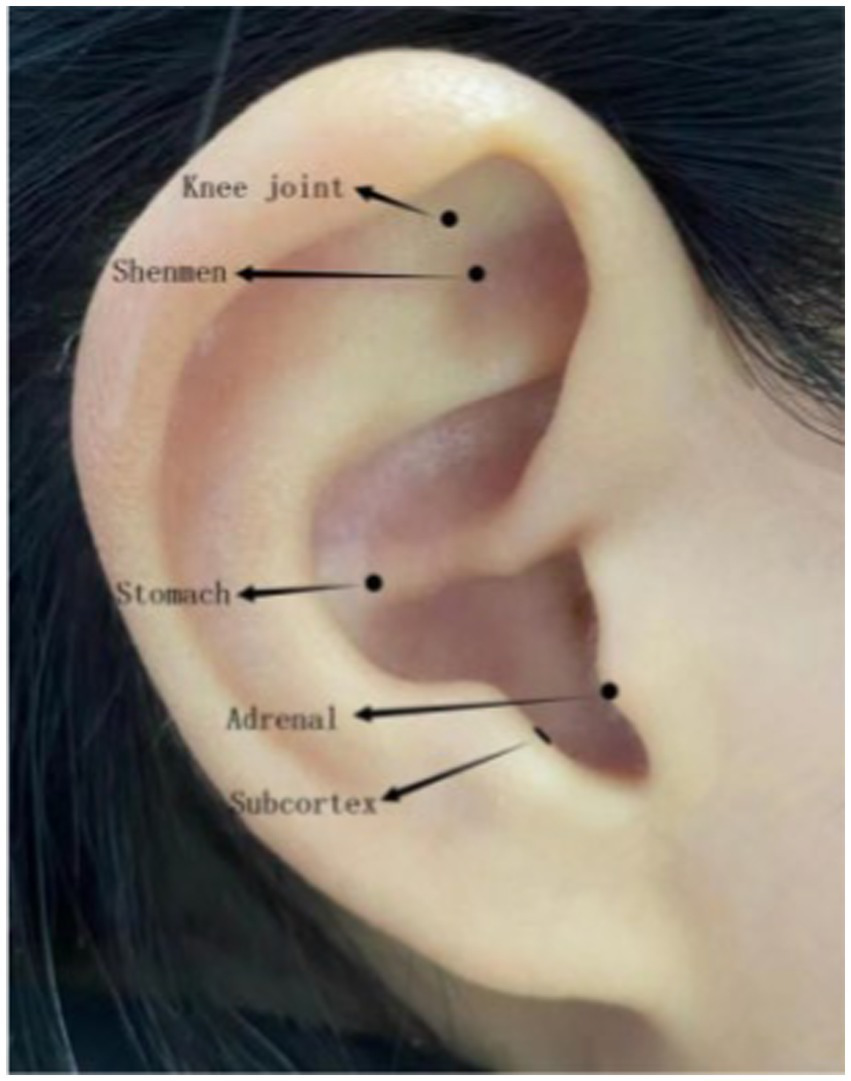
Selected auricular acupoints.
Outcome measures
Primary outcome
The primary outcome was the VAS (28, 29) of resting and movement states at 6 h, 12 h, and 1, 2, 3, 5, and 7 days after surgery. The evaluation was conducted face to face by the evaluator and the patient using a VAS of 0–10 points. At the time of evaluation, the patient was shown a ruler with a scale of 10 cm, where 0 cm on one end indicated no pain, and 10 cm on the other end indicated the most pain. At each time point of the evaluation, the patient outlined the point that best represented the degree of pain, and this point was taken as the patient’s score.
Secondary outcomes
Additional analgesic injections
Parecoxib sodium for injection (No. H20193217, Hunan Cylon Pharmaceutical Co., Ltd., 40 mg/dose) was added when the pain score was greater than 6, and the total additional dose during the treatment period was recorded.
Hospital for special surgery knee score
The hospital for special surgery knee score (HSS) (30) was recorded when the patients were followed up by telephone or outpatient visits at 2 and 12 weeks postoperatively.
Serum examination
The CRP level, ESR, and WBC count in the two groups were detected at 1, 3, and 7 days after the operation. CRP was detected by immunoturbidimetry, ESR by Wei’s method, and WBC by semiconductor laser flow cytometry.
Degree of postoperative nausea
The VAS was used to record nausea at 1, 2, and 3 days after surgery (31, 32) when the evaluator was face to face with the patient. The VAS scale ranged from 0 to 10 points. At each time point of the evaluation, the point that best represented the degree of nausea was outlined by the patient, and this point was recorded as the patient’s score.
Safety assessments
The adverse reactions of the two groups during the treatment were observed and recorded; these included whether skin allergy, subcutaneous hematoma, local infection, and fainting occurred during acupuncture in the AA group and whether skin allergy occurred in the SAA group.
Sample size calculation
Sample size calculations were determined from known literature (33, 34). The ratio between the two groups was 1:1 according to the following equation:
where n is the required number of cases in each group, P1 and P2 represent the estimated values of the AA group and SAA group, respectively (represented by decimal points), and P is the combined rate. If the number of the two groups is equal (i.e., k = 1), P = (P1 + P2)/2. Type I error probability was set to α = 0.05, and type II error probability was set to β = 0.10; therefore, according to our clinical experience and the literature, Zβ = 1.645, Zα = 1.282, P1 = 95.18%, and P2 = 70.22%. n ≈ 40 can be calculated using Equation 1. As the patient required two treatments and a follow-up after discharge, we considered a dropout rate of 20%. A total of 96 patients were needed, 48 patients in each group.
Randomization, allocation concealment, and blinding
The enrolled patients were randomly assigned at a 1:1 ratio to the AA or SAA group using a random number table method generated by IBM SPSS 25.0 software, with treatments fixed in sequentially numbered opaque envelopes. When a patient was admitted for elective surgery, a physician who was not involved in the assessment opened the envelope to identify the patient group and informed the nurse to arrange the corresponding ward. The day before surgery, the patients were informed that they would receive auricular acupuncture at specific acupoints in addition to standard postoperative analgesia. After obtaining informed consent from the patient, the acupuncturist began the intervention. The acupuncturist had no further personal contact with the included patients at the end of each intervention. A professional orthopedics clinician, who had received training before the trial, was selected as the evaluator. The evaluators did not intervene and were unaware of the grouping of the patients. Similarly, the patients were also unaware of their grouping. Case collectors, acupuncturists, and data analysts were kept separate.
Statistical analysis
Data were analyzed using IBM SPSS 25.0 software analysis. Measurement data were first analyzed to determine whether they followed a normal distribution using a Shapiro–Wilk normality test. If the data had a normal distribution, they were expressed as the mean ± standard deviation ( ± s), and if they did not, then they were expressed as the median (upper quartile, lower quartile) [M (P25, P75)]. Comparisons between the two groups were performed using the Kruskal–Wallis test; intra-group comparisons were conducted using the Wilcoxon signed-rank test or Friedman test; and different time points were compared through repeated-measures analysis of variance between groups. Count data are described by the number of cases and percentage, and the chi-square test was used to compare the differences between the two groups. Two-sided p-values <0.05 were considered statistically significant.
Results
Baseline characteristics
A total of 112 patients were recruited, and 16 were excluded due to meeting the exclusion criteria. The flow chart of the study is shown in Figure 3. Because the patients were hospitalized during the treatment period and the later follow-up was in the form of re-consultation, there were no cases of dropout. The two groups were comparable, with no significant differences at baseline. All baseline demographic characteristics are shown in Table 1.
Figure 3
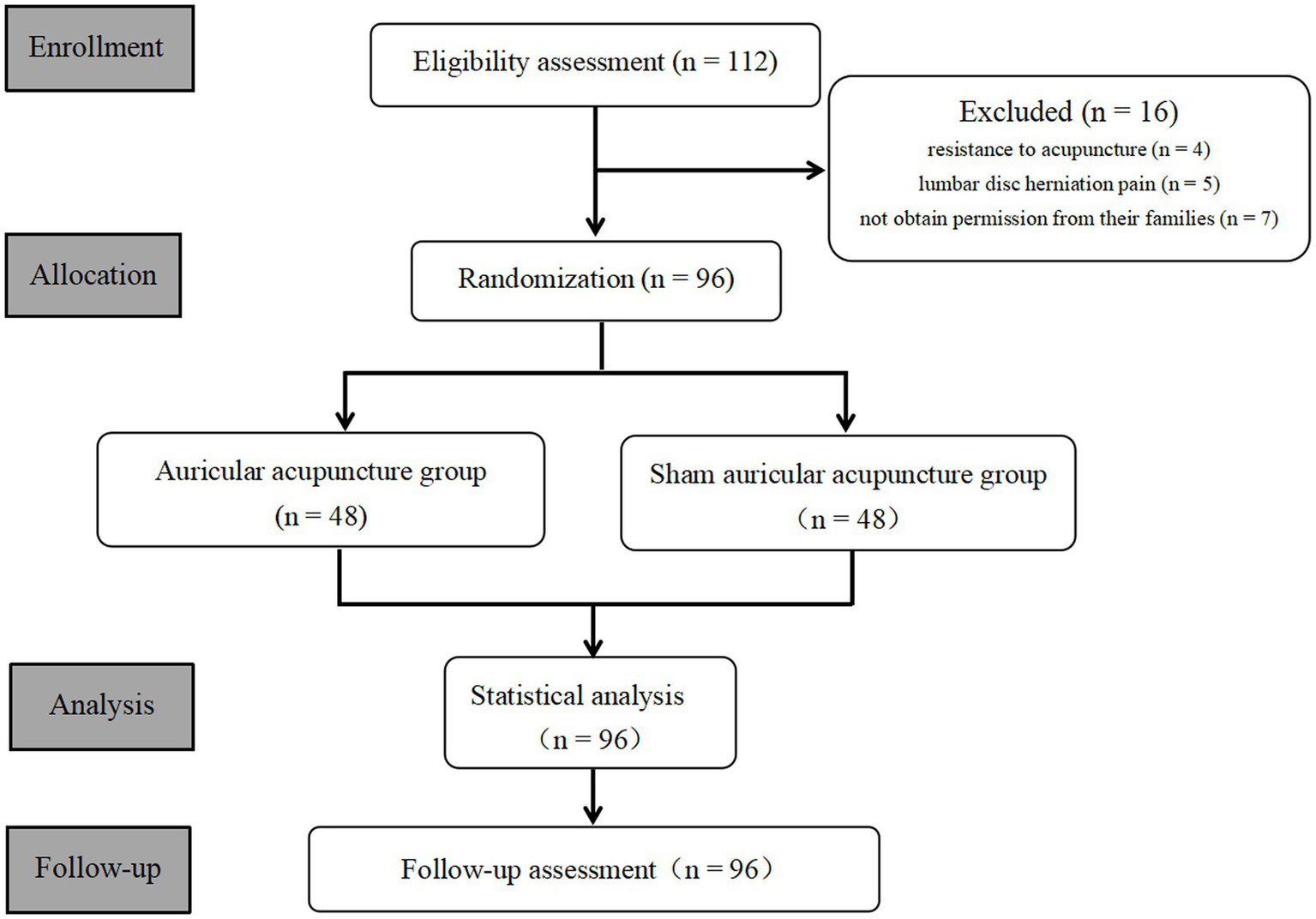
Flow chart of this trial.
Table 1
| Characteristics | Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) |
|---|---|---|
| Age, year | 67.9 ± 6.6 | 66.5 ± 7.5 |
| Sex (male/female) | 20/28 | 9/39 |
| Weight, kg | 71.69 ± 12.02 | 71.89 ± 12.12 |
| Height, cm | 163.02 ± 7.24 | 160.13 ± 5.54 |
| Course of disease, year | 10.5 (6.58, 15) | 10.75 (7.25, 16) |
| Hypertension | 19 (19.8%) | 14 (14.6%) |
| Type 2 diabetes | 4 (4%) | 3 (3%) |
| Hypertension and type 2 diabetes | 3 (3%) | 2 (2%) |
| None | 21 (21.9%) | 29 (30.2%) |
| Initial pain, visual analog scale score | 6.36 ± 1.77 | 6.50 ± 1.60 |
| Left | 29 (30%) | 25 (26%) |
| Right | 19 (20%) | 23 (24%) |
| C-reactive protein, mg/L | 1.82 (0.98, 2.66) | 2.14 (0.88, 4.23) |
| Erythrocyte sedimentation rate, mm/h | 17 (10, 26.75) | 16.5 (11, 34.5) |
| White blood cell count, cell/μL | 5.70 ± 1.65 | 5.95 ± 1.72 |
Baseline characteristics of the population.
Primary outcome
The VAS values of the resting and movement states were significantly different between the two groups at 6 h, 12 h, 2 days, 3 days, and 5 days after the operation. The VAS values of patients who received AA were lower than those of the SAA group (p < 0.05, Figure 4), but there was no significant difference between the two groups at 1 day and 7 days after the operation (p > 0.05, Table 2).
Figure 4
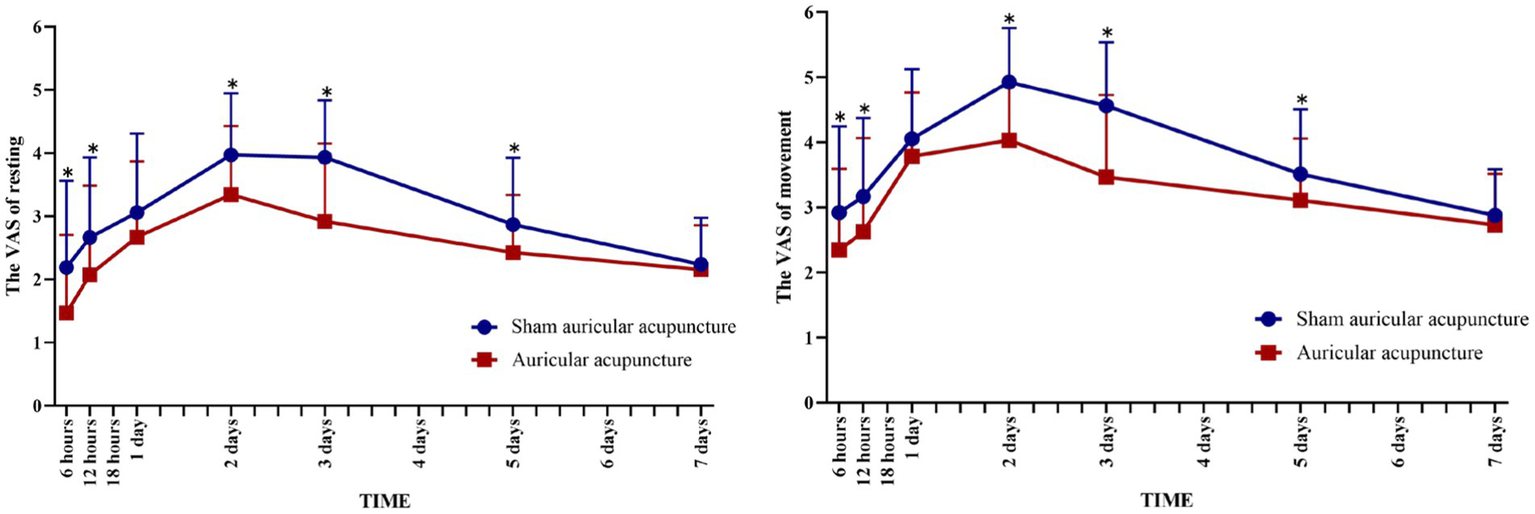
Visual analog scale scores over time in the AA and SAA groups. *Compared with sham auricular acupuncture, *P < 0.05.
Table 2
| Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) | p-value | |
|---|---|---|---|
| Post-operative VAS value at resting state, score | |||
| 6 h | 1.47 ± 1.24 | 2.19 ± 1.37 | 0.008 |
| 12 h | 2.08 ± 1.41 | 2.67 ± 1.27 | 0.034 |
| 1 day | 2.68 ± 1.20 | 3.06 ± 1.26 | 0.125 |
| 2 days | 3.34 ± 1.09 | 3.98 ± 0.98 | 0.004 |
| 3 days | 2.92 ± 1.23 | 3.94 ± 0.90 | 0.000 |
| 5 days | 2.43 ± 0.91 | 2.87 ± 1.06 | 0.030 |
| 7 days | 2.16 ± 0.70 | 2.24 ± 0.74 | 0.581 |
| Post-operative VAS value at movement state, score | |||
| 6 h | 2.35 ± 1.24 | 2.92 ± 1.32 | 0.031 |
| 12 h | 2.63 ± 1.44 | 3.17 ± 1.20 | 0.048 |
| 1 day | 3.79 ± 0.98 | 4.05 ± 1.07 | 0.203 |
| 2 days | 4.03 ± 0.90 | 4.93 ± 0.83 | 0.000 |
| 3 days | 3.47 ± 1.26 | 4.56 ± 0.98 | 0.000 |
| 5 days | 3.11 ± 0.95 | 3.51 ± 0.99 | 0.045 |
| 7 days | 2.73 ± 0.78 | 2.89 ± 0.70 | 0.326 |
Comparison of the postoperative VAS values during resting and movement states at each time point between the two groups.
Secondary outcomes
The total dosage of analgesic requirement after the operation in the AA group was lower than that in the SAA group (p < 0.05), and the additional dosage at each time point in the AA group was also lower than that in the SAA group postoperative days 1 and 2 (p < 0.05) as shown in Table 3.
Table 3
| Additional dosage at each time point | Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) | P-value |
|---|---|---|---|
| 6 h | 1 (0, 1) | 1 (1, 1) | 0.348 |
| 12 h | 0 (0, 1) | 0 (0, 1) | 0.943 |
| 1 day | 0 (0, 1) | 0 (0, 1) | 0.044 |
| 2 days | 0 (0, 0) | 0 (0, 1) | 0.019 |
| 3 days | 0 (0, 0) | 0 (0, 0) | 0.103 |
| 5 days | 0 (0, 0) | 0 (0, 0) | 0.313 |
| 7 days | 0 (0, 0) | 0 (0, 0) | 0.058 |
| Total additional injections | 3 (1, 4) | 1 (1, 2.5) | 0.004 |
Comparison of the postoperative dose of additional analgesic injections between the two groups.
The level of CRP in the AA group was lower than that in the SAA group on the 1st day after the operation (P < 0.05), while there was no significant difference in CRP between the two groups on the 3rd and 7th days after the operation (P > 0.05). In addition, there was no significant difference in ESR and WBC between the two groups at 1, 3, and 7 days after the operation (p > 0.05, Table 4).
Table 4
| C-reactive protein | Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) | P-value |
|---|---|---|---|
| 1 day | 67.25 ± 32.20 | 80.79 ± 34.43 | 0.049 |
| 3 days | 147.53 ± 52.95 | 155.36 ± 52.95 | 0.446 |
| 7 days | 64.39 ± 33.18 | 62.08 ± 28.38 | 0.715 |
| Erythrocyte sedimentation rate | |||
| 1 day | 25 (15, 35.75) | 20 (15.25, 30) | 0.359 |
| 3 days | 93.50 ± 29.28 | 92.56 ± 24.07 | 0.864 |
| 7 days | 93.38 ± 26.53 | 99.29 ± 30.60 | 0.314 |
| White blood cell count | |||
| 1 day | 11.47 ± 3.33 | 11.98 ± 3.38 | 0.459 |
| 3 days | 9.30 ± 2.73 | 9.34 ± 2.30 | 0.955 |
| 7 days | 7.38 ± 1.87 | 7.74 ± 2.17 | 0.381 |
Comparison of the postoperative serum CRP, ESR, and WBC between the two groups.
The degree of nausea in the AA group was lower than that in the SAA group on the 2nd day after the operation (p < 0.05), but there was no significant difference on the 1st and 3rd days after the operation (p > 0.05, Table 5).
Table 5
| Degree of postoperative nausea | Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) | P-value |
|---|---|---|---|
| 1 day | 1 (0, 2.5) | 2.3 (0, 4.08) | 0.062 |
| 2 days | 1.25 (0, 2.3) | 1.7 (0.08, 3.38) | 0.046 |
| 3 days | 0 (0, 1) | 1 (0, 1.73) | 0.081 |
Comparison of postoperative nausea between the two groups.
The HSS was not significantly different between the two groups (p > 0.05, Table 6).
Table 6
| Postoperative HSS score | Auricular acupuncture group (n = 48) | Sham auricular acupuncture group (n = 48) | P-value |
|---|---|---|---|
| 2 weeks | 95.5 (88, 100) | 98 (90, 100) | 0.348 |
| 12 weeks | 100 (100, 100) | 100 (100, 100) | 0.095 |
Follow-up results of HSS scores in the two groups.
Adverse events
During the treatment, none of the patients suffered any adverse events (e.g., infection). The safety was not significantly different between the two groups (p > 0.05).
Discussion
Approximately 10–34% of patients with TKA have poor acute pain control, leading to chronic pain (35), which seriously affects the postoperative rehabilitation and quality of life of the patients and increases their reliance on analgesics. However, the drug-related side effects of analgesics limit their application in daily clinical practice (36). Therefore, it is particularly important to explore an analgesic method with the characteristics of green therapy (37).
As a kind of green complementary and alternative therapy, auricular acupuncture therapy has a good analgesic effect during the perioperative period and has been widely used in gynecology, orthopedics, anorectal, and other fields (10). According to the theory of bioholography, the close association between auricular acupoints and zangfu-meridians is the basis for the clinical treatment of pain (11).
The pain mechanism of TKA can be attributed to peripheral sensitization and central sensitization (38). Peripheral sensitization is caused by injury to the body, resulting in inflammation and local organ pain. On the other hand, central sensitization occurs due to pain stimulation, leading to increased neuronal excitability in the dorsal horn of the spinal cord and resulting in pain. Research has demonstrated that the application of auricular acupuncture can activate the descending pain inhibition pathway along the dorsal side of the spinal cord, specifically where the dorsal horn cells are located. This activation plays an analgesic role and effectively relieves pain after TKA (39). In addition, the analgesic effect of auricular acupuncture also works by stimulating specific acupoints on the ear to activate the nociceptin receptors, which release endogenous morphine-like substances such as endorphins and enkephalins, thereby enhancing the pain threshold and reducing the degree of pain (40). Our results demonstrated that an indwelling intradermal needle, as an auricular acupuncture device, could provide effective postoperative analgesia after TKA. The best analgesic effect was achieved 2 days after the operation, which reduced moderate pain (VAS score 4–6 points) to mild pain (VAS score 0–3 points), as well as the dose of analgesic needling.
Based on previous literature, textbooks, and clinical practice experience of acupuncture, the auricular acupoints stimulated in this study included the TF4, TG2p, AH4, AT4, and CO4. First, according to the results of literature data mining (41, 42), TF4 and AT4 were the two most commonly used in perioperative analgesia. The TG2p can effectively regulate the patient’s autonomic nerve with sedative and analgesic effects (43). Second, after the operation, the vital qi of the body is consumed and the qi of the spleen and stomach is gradually weakened, causing the stomach qi to be out of balance. At the same time, the usage of analgesics stimulates the stomach organ, which leads to nausea and vomiting. The CO4 was selected to control nausea and vomiting based on clinical experience. Third, according to the location of the lesion, the AH4 was directly stimulated to relieve the pain, which is a type of acupoint selection method based on traditional Chinese medicine. All in all, the combination of five acupoints can regulate the meridians and collateralis to reduce pain.
It is found that CRP, ESR, and WBC are the primary inflammatory and anti-inflammatory factors in the serum of patients who have suffered postoperative trauma. Those blood indicators may be an objective index for the evaluation of postoperative analgesia after TKA. Our results showed that AA could reduce the CRP level over a certain period of time, which showed that the analgesic effect of intradermal needling may be the result of an anti-inflammation effect; however, ESR and WBC did not decrease significantly. The reason for this could be that the diagnostic advantage of CRP is significantly higher than that of the ESR and WBC count (44). The ESR and WBC are often used as monitoring indices to evaluate postoperative infection; however, as the specificity of these indices is relatively low and easily affected by many factors (45), this result still needs to be verified by a larger sample size.
The degree of postoperative nausea in the AA group was lower than that in the SAA group at 2 days after the operation, partly because fewer analgesic needles were added in the AA group, especially at 2 days after the operation. According to the perspective of Chinese medicine, the pathogenesis of vomiting is a “stomach disorder causing qi inverse to the upper.” Patients with TKA have a deficiency of both qi and blood of the body, which impairs the function of the spleen and stomach qi and the occurrence and aggravation of nausea induced by qi inverse (46). In addition, the risk of nausea is increased due to the aggravation of postoperative pain in patients. Simultaneously, the use of analgesics stimulates the vomiting center of the brain, which will also induce the generation and aggravation of nausea (47). Modern research has proved that auricular acupoint therapy can effectively alleviate the degree of postoperative nausea (47). Moreover, it has been verified that CO4, one of the five acupoints selected in this study, can reduce regurgitation and stop vomiting.
Limitations
First, the population of this trial was taken from a single center, which may cause population bias. In future, our research team will conduct a multicenter RCT with a large sample size. Second, this pilot study only examined the visual analog score as the primary outcome measure of postoperative pain but did not consider the possible influencing factors such as perioperative patients’ emotional state and cognitive function on pain assessment. The effect of these factors on the results is unknown. Third, this study was invasive and may not have been double-blind. Despite the implementation of the principle of three separations, the effect of blind implementation was not assessed, which is an important point for future consideration of sham control settings. Fourth, the study should be conducted in experienced institutions to obtain more rigorous data. Fifth, the research team will consider how to assess the analgesia-related effects of indwelling intradermal needles independently of the use of analgesics. In parallel, we will seek to provide more reliable and effective clinical methods for postoperative analgesia in TKA based on this study in the future.
Conclusion
Auricular acupuncture is effective for adjuvant analgesia after TKA and functions by reducing CRP on the first day after the operation, the use of analgesic needles, and the occurrence of postoperative nausea.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Shijiazhuang West Medical Center. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XZ: Writing – original draft. HC: Writing – original draft. JQL: Data curation, Visualization, Writing – review & editing. XL: Funding acquisition, Resources, Writing – review & editing. PX: Conceptualization, Methodology, Writing – review & editing. ML: Formal analysis, Writing – review & editing. JDL: Funding acquisition, Resources, Supervision, Writing – review & editing. YS: Conceptualization, Funding acquisition, Methodology, Resources, Visualization, Writing – review & editing. XW: Methodology, Software.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This trial was supported by grant 81973755 from the National Natural Science Foundation of China.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1275192/full#supplementary-material
References
1.
Sharma L . Osteoarthritis of the knee. N Engl J Med. (2021) 384:51–9. doi: 10.1056/NEJMcp1903768
2.
Kan HS Chan PK Chiu KY Yan CH Yeung SS Ng YL et al . Non-surgical treatment of knee osteoarthritis. Hong Kong Med J. (2019) 25:127–33. doi: 10.12809/hkmj187600
3.
Corbett MS Rice SJ Madurasinghe V Slack R Fayter DA Harden M et al . Acupuncture and other physical treatments for the relief of pain due to osteoarthritis of the knee: network meta-analysis. Osteoarthr Cartil. (2013) 21:1290–8. doi: 10.1016/j.joca.2013.05.007
4.
Lin Z Zheng J Chen M Chen J Lin J . The efficacy and safety of Chinese herbal medicine in the treatment of knee osteoarthritis: An updated systematic review and meta-analysis of 56 randomized controlled trials. Oxidative Med Cell Longev. (2022) 2022:1–28. doi: 10.1155/2022/6887988
5.
Yang F Chen Y Lu Z Xie W Yan S Yang J et al . Treatment of knee osteoarthritis with acupuncture combined with Chinese herbal medicine: a systematic review and meta-analysis. Ann Palliat Med. (2021) 10:11430–44. doi: 10.21037/apm-21-2565
6.
Joint surgery Group of Beijing Medical Association Orthopaedic Society, Joint Surgery Group of Chinese Medical Association Orthopaedic Society . Chinese guidelines for perioperative pain management of total knee arthroplasty (2022). Chin Med J. (2021) 13:965–85. doi: 10.12290/xhyxzz.2022-0642
7.
Moucha CS Weiser MC Levin EJ . Current strategies in anesthesia and analgesia for total knee arthroplasty. J Am Acad Orthop Surg. (2016) 24:60–73. doi: 10.5435/JAAOS-D-14-00259
8.
Lin JG Kotha P Chen YH . Understandings of acupuncture application and mechanisms. Am J Transl Res. (2022) 14:1469–81. PMID:
9.
Lee S Jo DH . Acupuncture for reduction of opioid consumption in chronic pain: a systematic review and meta-analysis protocol. Medicine (Baltimore). (2019) 98:e18237. doi: 10.1097/MD.0000000000018237
10.
Yin Z Zhang W Zeng Y Su X . Effect of auricular point pressing therapy on postoperative pain of fracture: a protocol for systematic review and meta-analysis. Medicine (Baltimore). (2020) 99:e23696. doi: 10.1097/MD.0000000000023696
11.
Shuyi X Hongron M . The theoretical basis of bioholography on the therapeutic effect of acupuncture and Acupoints. Asia-Pacific Trad Med. (2016) 16:204–7. doi: 10.11954/ytctyy.202011061
12.
Collinsworth KM Goss DL . Battlefield acupuncture and physical therapy versus physical therapy alone after shoulder surgery. Med Acupunct. (2019) 31:228–38. doi: 10.1089/acu.2019.1372
13.
Kim H Markert R Burtson K . Battlefield acupuncture appears to be an effective therapy for pain management. Acupunct Med. (2022) 40:43–9. doi: 10.1177/09645284211050648
14.
Usichenko TI Henkel BJ Klausenitz C Hesse T Pierdant G Cummings M et al . Effectiveness of acupuncture for pain control after cesarean delivery: a randomized clinical trial. JAMA Netw Open. (2022) 5:e220517. doi: 10.1001/jamanetworkopen.2022.0517
15.
Rongyuan ZHANG Xinrong ZHANG Caifeng GUO Ying ZENG Zhaoxin LI . Clinical random trial of thumbtack needling therapy for analgesia after cesarean section. Acupunct Res. (2022) 47:719–23. doi: 10.13702/j.1000-0607.20210959
16.
Xiaoyan HUANG Huan ZHOU . The effect of thumb-tack Neede-embedding therapy on analgesia during artificial abortion. Shanghai J Acumox. (2021) 40:315–8. doi: 10.13460/j.issn.1005-0957.2021.03.0315
17.
Haixia XU Haixia LUO . Clinical observation of acupuncture at Neiguan and Hegu points with ring-headed thumb-tack needle on postoperative pain and nausea and vomiting in patients undergoing orthopedic surgery. Henan Trad Chin Med. (2021) 41:271–4. doi: 10.16367/j.issn.1003-5028.2021.02.0062
18.
Yue Y Diao HL Nan D Chen SR Cheng WX Li X et al . Analgesic mechanism of traditional Chinese medicine comprehensive external treatment on anal fistula model rats based on SP/NK1R interaction pathway. Lishizhen medicine and Materia Medica. Research. (2019) 30:2555–8. doi: 10.3969/j.issn.1008-0805.2019.10.082
19.
Kayani B Tahmassebi J Ayuob A Konan S Oussedik S Haddad FS . A prospective randomized controlled trial comparing the systemic inflammatory response in conventional jig-based total knee arthroplasty versus robotic-arm assisted total knee arthroplasty. Bone Joint J. (2021) 103-B:113–22. doi: 10.1302/0301-620X.103B1.BJJ-2020-0602.R2
20.
Du X Wang W . C-reactive protein as marker of post-operative analgesic quality after primary total knee arthroplasty: several questions. Int Orthop. (2020) 44:1443–4. doi: 10.1007/s00264-020-04603-z
21.
Jianda X Yuxing Q Yi G Hong Z Libo P Jianning Z . Impact of preemptive analgesia on inflammatory responses and rehabilitation after primary Total knee arthroplasty: a controlled clinical study. Sci Rep. (2016) 6:30354. doi: 10.1038/srep30354
22.
Tarasov DA Lychagin AV Yavorovkiy AG Lipina MM Tarasova IA . C-reactive protein as marker of post-operative analgesic quality after primary total knee arthroplasty. Int Orthop. (2020) 44:1727–35. doi: 10.1007/s00264-020-04551-8
23.
Osteoporosis Group of Chinese Orthopaedic Association . Guideline for diagnosis and treatment of osteoarthritis. Chin J Orthop. (2018) 38:705–15. doi: 10.3760/cma.j.issn.0253-2352.2018.12.001
24.
Xu ST Ge BF Xu YK . Practical orthopedics. 3rdBeijing: People’s Military Medical Press. (2005) 2112–2124.
25.
General Administration of Quality Supervision . Inspection and quarantine of the People’s republic of China, standardization Administration of the People’s republic of China, GB/T 13734–2008, Nomenclature and location of auricular points. Beijing: China Standards Press (2008).
26.
Favre-Félix J Laurent V Branche P Huissoud C Raffin M Pradat P et al . Auricular acupuncture for preoperative anxiety in parturient women with scheduled cesarean section: a randomized placebo-controlled blind study. J Integr Complement Med. (2022) 28:569–78. doi: 10.1089/jicm.2021.0346
27.
Ma J Zhang Y Ge Q Wu K . The effect of auricular acupuncture on preoperative blood pressure across age groups: a prospective randomized controlled trial. Clin Exp Hypertens. (2023) 45:2169452. doi: 10.1080/10641963.2023.2169452
28.
Brozovich AA Incavo SJ Lambert BS Sullivan TC Wininger AE Clyburn TA et al . Intraosseous morphine decreases postoperative pain and pain medication use in total knee arthroplasty: a double-blind, randomized controlled. Trial J Arthroplasty. (2022) 37:S139–46. doi: 10.1016/j.arth.2021.10.009
29.
Li Y An M Ding Y Wang C Qiu Y . Oxycodone-acetaminophen versus celecoxib for postoperative pain in knee osteoarthritis patients after total knee arthroplasty: a randomized, controlled study. Arch Orthop Trauma Surg. (2023) 143:6753–62. doi: 10.1007/s00402-023-04943-6
30.
Huang H Tang K Song X Zhao L Liang Y Xu H et al . Effects of contralateral versus ipsilateral electroacupuncture for analgesia and rehabilitation after unilateral total knee arthroplasty: a randomized controlled trial. Acupunct Med. (2023) 27:9645284231211601. doi: 10.1177/09645284231211601
31.
Adib-Hajbaghery M Hosseini FS . Investigating the effects of inhaling ginger essence on post-nephrectomy nausea and vomiting. Complement Ther Med. (2015) 23:827–31. doi: 10.1016/j.ctim.2015.10.002
32.
Lu C Chen X Yan X He J Nie Z . The preventive and relieving effects of ginger on postoperative nausea and vomiting: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. (2022) 125:104094. doi: 10.1016/j.ijnurstu.2021.104094
33.
Kong WW JL LI Liu F An LL Zhang JH Tian JQ et al . Clinical effects of auricular plaster therapy in improving acute pain after Total knee arthroplasty and early recovery. Western. J Tradit Chin Med. (2020) 33:109–12. doi: 10.12174/j.issn.1004-6852.2020.12.30
34.
He BJ Tong PJ Li J Jing HT Yao XM . Auricular acupressure for analgesia in perioperative period of total knee arthroplasty. Pain Med. (2013) 14:1608–13. doi: 10.1111/pme.12197
35.
Beswick AD Dennis J Gooberman-Hill R Blom AW Wylde V . Are perioperative interventions effective in preventing chronic pain after primary total knee replacement? A systematic review. BMJ Open. (2019) 9:e028093. doi: 10.1136/bmjopen-2018-028093
36.
Chen Z Shen Z Ye X Xu Y Liu J Shi X et al . Acupuncture for rehabilitation after total knee arthroplasty: a systematic review and Meta-analysis of randomized controlled trials. Front Med (Lausanne). (2021) 7:602564. doi: 10.3389/fmed.2020.602564
37.
Xiang J Zhang Y Wu J Shui Y Zhu Y . Electroacupuncture combined with continuous adductor canal block for postoperative analgesia in patients undergoing total knee arthroplasty. Chin Acupuncture. Moxibust. (2023) 44:57–61. doi: 10.13703/j.0255-2930.20230418-00
38.
Yanan L Huaijing H Jianjun X Yalan M Huaipeng H . Research Progress of the mechanism of pain after TKA and acupuncture analgesia. Western J Trad Chin Med. (2020) 33:146–50. doi: 10.12174/j.issn.1004-6852.2020.04.45
39.
Hou PW Hsu HC Lin YW Tang NY Cheng CY Hsieh CL . The history, mechanism, and clinical application of auricular therapy in traditional Chinese medicine. Evid Based Complement Alternat Med. (2015) 2015:495684. doi: 10.1155/2015/495684
40.
Ying L Du JL Hao PL Zhang MX Jiang YB Man S et al . Effect of auricular point sticking therapy on perioperative pain in patients with partial lung resection. Chin Acupunct. Moxibust. (2021) 41:603–7. doi: 10.13703/j.0255-2930.20200505-k0003
41.
He XY Tao H Hu LY . Analysis of ear acupoint application in perioperative period based on data mining. Clin J Trad Chin Med. (2021) 33:714–8.
42.
Peng S Wang Y Zhang SQ Sun YQ . Acupoint selection rules of auricular plaster therapy for postoperative pain based on data mining. J Nurs. (2021) 28:21–5. doi: 10.16448/j.cjtcm.2021.0430
43.
Liao BS Li LH Hong FM Rao XZ Li CY . Application and curative effect of ear acupoint bean-pressing therapy in perioperative analgesia of cesarean section. Chin J Basic Med Trad Chin Med. (2013) 19:1078–80. doi: 10.16460/j.issn1008-9969.2021.05.021
44.
Xie Q Lei GH . Blood inflammatory markers for the diagnosis of joint prosthesis infection. Chin J Tissue Engin Res. (2012) 16:8271–8. doi: 10.19945/j.cnki.issn.1006-3250.2013.09.041
45.
Li GD . Changes in serum C-reactive protein level and erythrocyte sedimentation rate in patients after use of orthopedic metal implants. Chin J Tissue Engin Res. (2015) 19:3967–71. doi: 10.3969/j.issn.2095-4344.2012.44.020
46.
Liu X Fang R . A study on the prevention and treatment of nausea and vomiting after knee joint replacement by acupuncture and moxibustion. Clin J Chin Med. (2020) 12:146–8. doi: 10.3969/j.issn.2095-4344.2015.25.007
47.
Liu Y Huang L Xu G Tian H Zhou Z Huang F et al . The application of acupuncture therapy for postoperative pain over the past 20 years: a bibliometric analysis. J Pain Res. (2022) 15:2085–104. doi: 10.2147/JPR.S371399
Summary
Keywords
total knee arthroplasty, adjuvant analgesia, auricular acupuncture, randomized clinical trial, pain management
Citation
Zhang X, Chen H, Li J, Liu X, Wang X, Xue P, Lin M, Li J and She Y (2024) Effectiveness and safety of auricular acupuncture on adjuvant analgesia in patients with total knee arthroplasty: a randomized sham-controlled trial. Front. Neurol. 15:1275192. doi: 10.3389/fneur.2024.1275192
Received
09 August 2023
Accepted
25 January 2024
Published
16 February 2024
Volume
15 - 2024
Edited by
Shiyan Yan, Beijing University of Chinese Medicine, China
Reviewed by
Zhifang Xu, Tianjin University of Traditional Chinese Medicine, China
Xuli Ren, Jilin University, China
Updates
Copyright
© 2024 Zhang, Chen, Li, Liu, Wang, Xue, Lin, Li and She.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jidong Li, jidongli1966@sina.comYanfen She, sheyanfen@163.com
†These authors have contributed equally to this work and share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.