- 1College of Clinical Medicine, North China University of Science and Technology, Tangshan, Hebei, China
- 2Cangzhou Center for Disease Control and Prevention, Cangzhou, Hebei, China
- 3College of Psychology and Mental Health of North China University of Science and Technology, Tangshan, Hebei, China
- 4Department of Neurology, Tangshan Gongren Hospital, Tangshan, Hebei, China
Background: The levels of anxiety and depression among patients with restless leg syndrome (RLS) are controversial. The aim of this systematic review and meta-analysis was to compare the levels of depression and anxiety among individuals with RLS with those of healthy controls.
Methods: We conducted an extensive electronic search of the PubMed, Web of Science, EMBASE, and Cochrane Library databases from their inception dates to 20 June 2023. Studies presenting data on depression and anxiety in individuals with RLS were included, and a comprehensive meta-analysis was performed.
Results: Twenty-one studies matched the inclusion criteria. Significantly more depressive symptoms were present in the individuals with RLS than in those without RLS, as measured by the Beck Depression Inventory [mean difference (MD) = 6.58, 95% confidence interval (CI) = 5.54–7.62, p < 0.01; heterogeneity I2 = 0%, p = 0.99]. Similarly, the results from the Beck Anxiety Inventory indicated that there were significantly more pronounced anxiety symptoms in the individuals with RLS than in those without RLS (MD = 9.30, 95%CI = 7.65–10.94, p < 0.01; heterogeneity I2 = 0%, p = 0.92). The other anxiety and depression scales also yielded statistically significant results. Significant heterogeneity was observed in the Hamilton Depression Rating Scale and Hamilton Anxiety Rating Scale, with the primary contributing factor probably being the scoring criteria of the scales.
Conclusion: This meta-analysis found that the levels of depression and anxiety symptoms were significantly higher in individuals with RLS than in their healthy counterparts.
Systematic review registration:https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023410364, (identifier CRD42023410364).
1 Introduction
Restless Legs Syndrome (RLS) is the most common sleep-related sensorimotor disorder characterized by an irresistible urge to move the legs, with typical worsening of symptoms at night during periods of immobility. In the general population, the prevalence is approximately 5–15%, with female predominance (1–3). The prevalence also increases with age in European and North American countries, but not in Asian countries (4). The disease is divided into two types: primary RLS, also known as idiopathic RLS, and secondary RLS, which may be linked to various factors, such as pregnancy, iron deficiency, end-stage renal disease, or neuropathy. Both types share the same symptoms and diagnostic criteria (5). The pathogenesis of primary RLS has not been fully established; however, genetic factors, impaired dopaminergic neuron function, and brain iron deficiency are recognized as contributors to its development (6).
Symptoms of anxiety and depression are consistently associated with RLS. Previous studies have reported that major depressive disorders, anxiety, and abnormal personality traits, such as neuroticism, are common in RLS (7, 8). Compared with their nonaffected counterparts, individuals with RLS are more likely to suffer from anxiety, depression, chronic pain, and cognitive difficulties. Individuals with RLS exhibit cognitive deficits in the domains of short-term attention, verbal fluency, visuospatial functions, and executive function (9–11). Furthermore, RLS, with its high prevalence, significantly affects emotional well-being and elevates the risk of cardiovascular diseases, ultimately affecting overall quality of life (12). Epidemiological studies have reported a two-to fourfold higher risk of depressive disorders in individuals with RLS than in healthy controls (13, 14). Consequently, RLS has become a nervous system disorder that is closely related to sleep, mood, cognition, and productivity in individuals’ daily lives. Furthermore, as the understanding of RLS continues to expand, comprehensive evidence regarding mental health outcomes will have an impact on mental health care (15, 16).
Although a previous narrative review provided an overview of RLS diagnosis and reported epidemiological evidence for an association between RLS and mood disorders (17), the association between RLS and depression/anxiety has been less well studied. Therefore, our study aim was to conduct a systematic review and meta-analysis to compare the levels of depression and anxiety between individuals with RLS and healthy controls.
2 Methods
2.1 Registration
This meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42023410364) and was conducted in accordance with the Cochrane guidelines.
2.2 Study search
We searched the PubMed, Web of Science, EMBASE and Cochrane Library, from inception date through 20 April 2023, and further updated the search on 20 June 2023. We utilized the Medical Subject Headings (MeSH) term “restless legs syndrome” combined with the following free text terms: “anxiety” and “depression.” No restrictions were placed on geographic location, language, or availability of the full text. To extend the scope of the search, we also meticulously reviewed the references of relevant review and meta-analysis studies to find additional articles of interest. The references were managed using Endnote software.
2.3 Study selection (inclusion and exclusion criteria)
Search results were imported into Endnote, where duplicates were removed automatically. Two authors (Tianyang An and Haiyang Sun) conducted a two-stage review process. Titles and abstracts were evaluated at the first stage and peer-reviewed full-length studies that met the following predefined criteria were considered for inclusion at the second stage. These criteria included: (1) observational study (cross-sectional, case–control, cohort); (2) the study’s population should have been stratified into at least two groups: cases (with RLS) and controls (without RLS); (3) the exposure of interest was depression or anxiety symptoms, or both; and (4) separately reported mean values (M) with their standard deviations (SD) for depression or anxiety symptoms, or both, using a validated quantitative scale for both cases (with RLS) and controls (without RLS). We excluded studies as follows: (1) RLS studies with multiple simultaneous groups; (2) studies that did not have a control group; and (3) conference abstracts, meta-analysis and reviews, animal studies, case series, case reports, or letters; and (4) studies that did not compare across groups or failed to address the primary research question.
2.4 Data extraction
Two authors (Tianyang An and Haiyang Sun) independently extracted the following data to a customized data extraction form eligible studies: publication year, first author, country of origin, study type, mean age pf participants, percentage of female participants, sample size, data resources, and depression/anxiety scores. In cases where certain data were not readily available in the included studies, we contacted the corresponding author of the original study to request unavailable data.
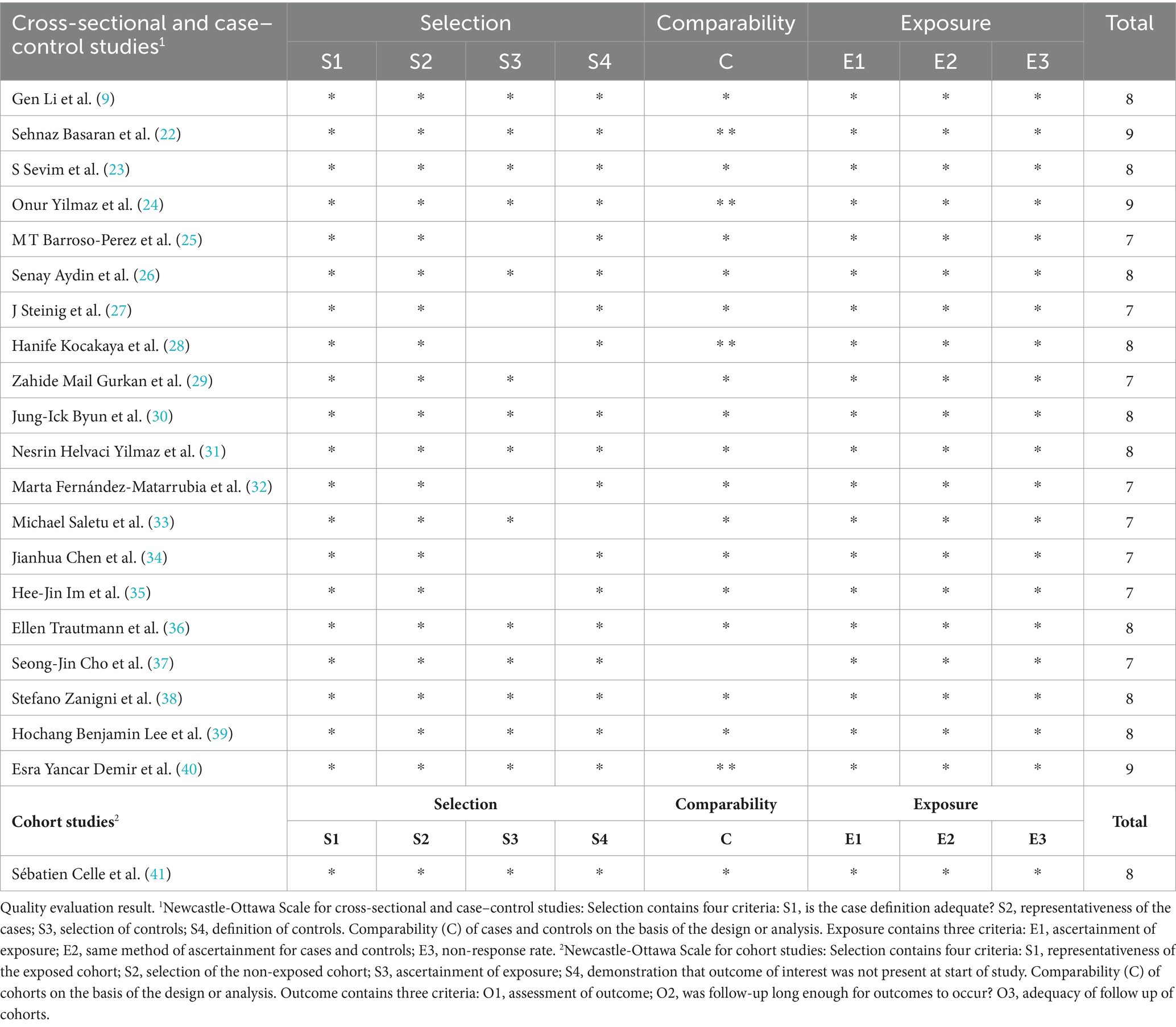
2.5 Study quality assessment
Using the Newcastle–Ottawa Scale, two authors (Tianyang An and Haiyang Sun) independently evaluated the quality of each eligible study, considering case–control, cross-sectional, and cohort study designs, into high quality (7–9), moderate quality (4–6), or low quality (0–3) (18). Any discrepancies were resolved through an objective discussion with the third author (Lu Yuan).
2.6 Statistical analyses
Review Manager software 5.4.1was used to analyze the data. Mean (M), SD, and mean difference (MD) with corresponding 95% confidence interval (CI) were used to compare depression and anxiety symptoms between individuals with RLS and those without RLS. The pooled point estimates of the MDs of the average scores of depression and anxiety, with 95%CIs, were calculated using forest plots, where the size of the square represents the weight of each study and the horizontal lines represent the 95%CI. We considered a statistically significant difference to be present when the 95%CI did not encompass zero. The heterogeneity of the studies was assessed graphically with forest plots and statistically via a chi-square-based Q statistic and I2 value. p < 0.05 was considered statistically significant (19). To investigate and mitigate sources of heterogeneity or inconsistency, we conducted subgroup analyses and several sensitivity analyses. All sensitivity analyses were carried out using STATA v.12.0 (Stata, College Station, TX, United States). In addition, funnel plots and Egger’s test were used to explore the potential publication bias in this meta-analysis (20, 21).
3 Results
3.1 Search results
As shown in Figure 1, our search strategy resulted in a total of 666 original studies. After the removal of reviews, conference abstracts, meta-analysis, other types of records, and duplicates, we identified 290 articles that appeared relevant to the study question. Following the subsequent title and abstract screening, 38 articles remained for full-text review. Articles that were excluded during full-text review were: study designs that did not match inclusion criteria (n = 5); experimental designs meet criteria but without extractable data (n = 8); and lack of a control group (n = 4). In total, we included 21 studies in the meta-analysis.
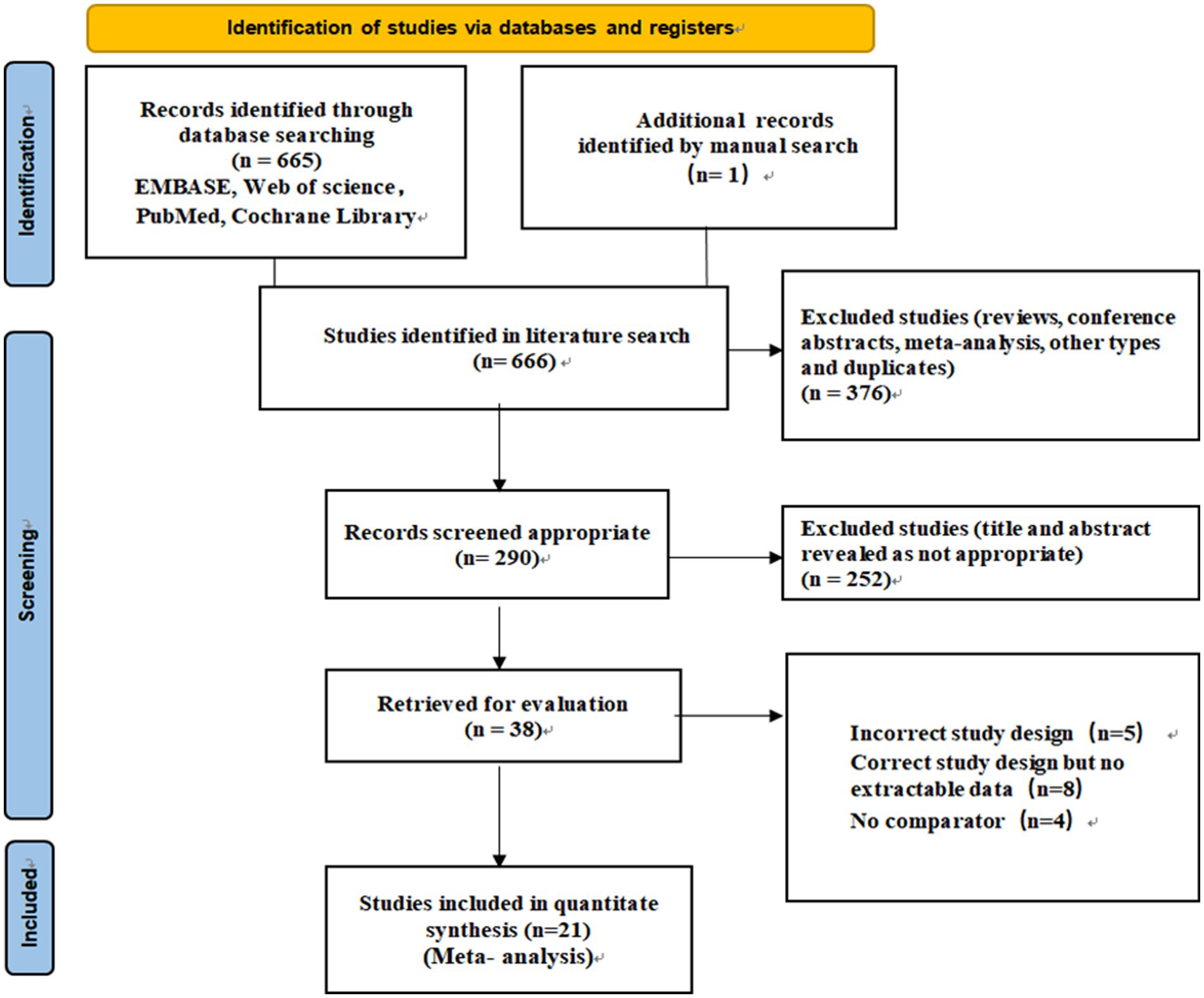
Figure 1. PRISMA flow diagram of identification, screening, and selection process for the meta-analysis on depression, anxiety, and Restless Legs Syndrome.
3.2 Study characteristics
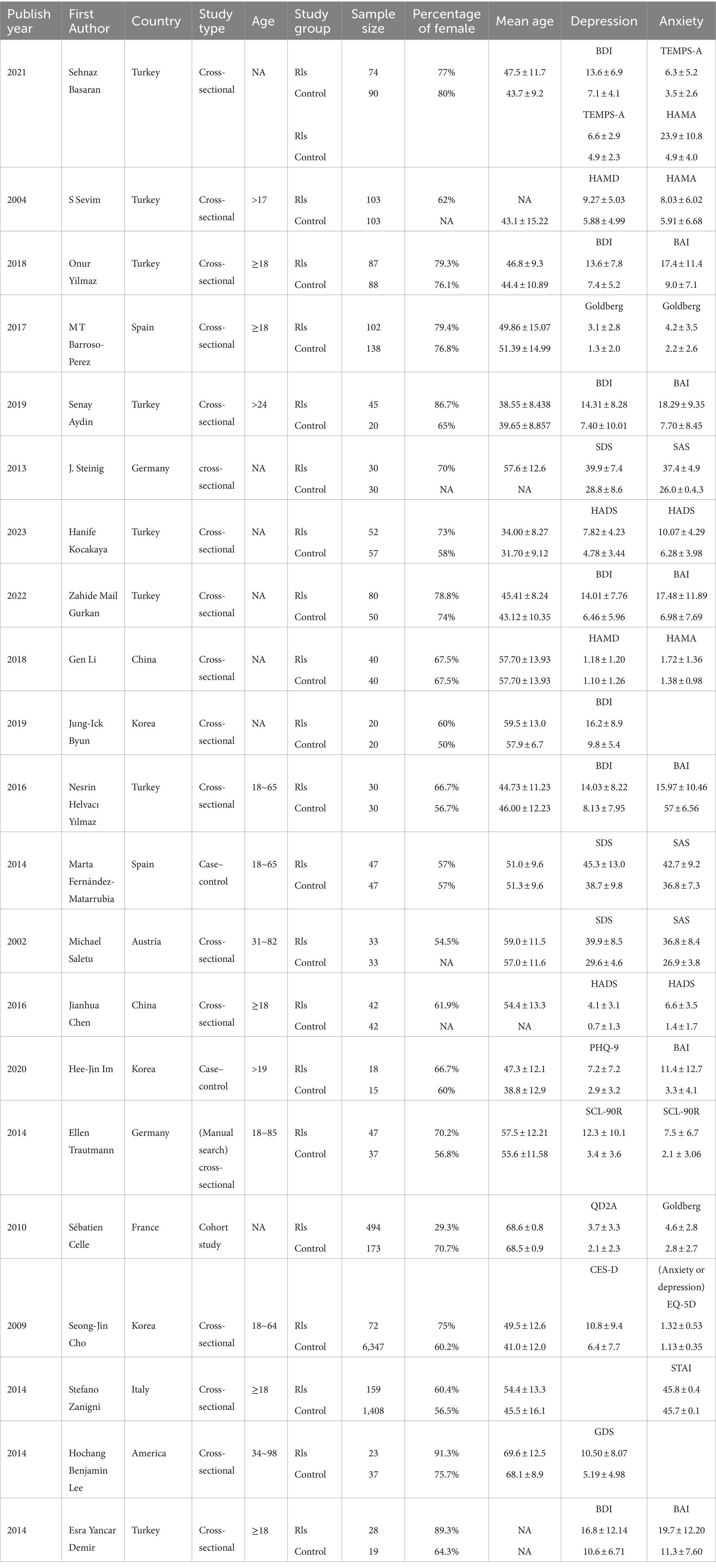
A summary of the 21 included study characteristics was shown in Table 1. The studies included a total of 1,626 individuals with RLS and 8,824 individuals without RLS. Table 2 summarized the study qualities where all studies received a rating of high quality.
Of the included studies, eight were conducted in Turkey (22–24, 26, 28, 29, 31, 40), three in Korea (30, 35, 38), two in Spain (25, 32), two in Germany (27, 36), two in China (9, 34), one in Austria (33), one in France (37), one in Italy (39), and one in America (41).
To assess depression, seven studies used the Beck Depression Inventory (BDI); three articles used the Zung Self-Rating Depression Scale (SDS); two studies used the Hamilton Depression Rating Scale (HAMD), two studies used the Hospital Anxiety And Depression Scale (HADS); and the remaining eight studies used screening tools including Goldberg scale, The Symptom Checklist-90-Revised (SCL-90-R), Center for Epidemiologic Studies for Depression (CES-D), QD2A, EuroQol five-dimensional questionnaire (EQ-5D), Patient Health Questionnaire-9 m (PHQ-9), Temperament Evaluation of Memphis, Pisa, Paris, and San Diego-Auto questionnaire (TEMPS-A) and Geriatric Depression Scale (GDS).
For the assessment of anxiety, six studies used the Beck Anxiety Inventory (BAI); three articles used the Zung Self-Rating Anxiety Scale (SAS); three used the Hamilton Anxiety Rating Scale (HAMA); two used the Hospital Anxiety and Depression Scale (HADS); two used Goldberg scale; and the remaining four studies used screening tools including SCL-90-R, State–Trait Anxiety Inventory (STAI), EQ-5D, and TEMPS-A.
3.3 Association of RLS with depression
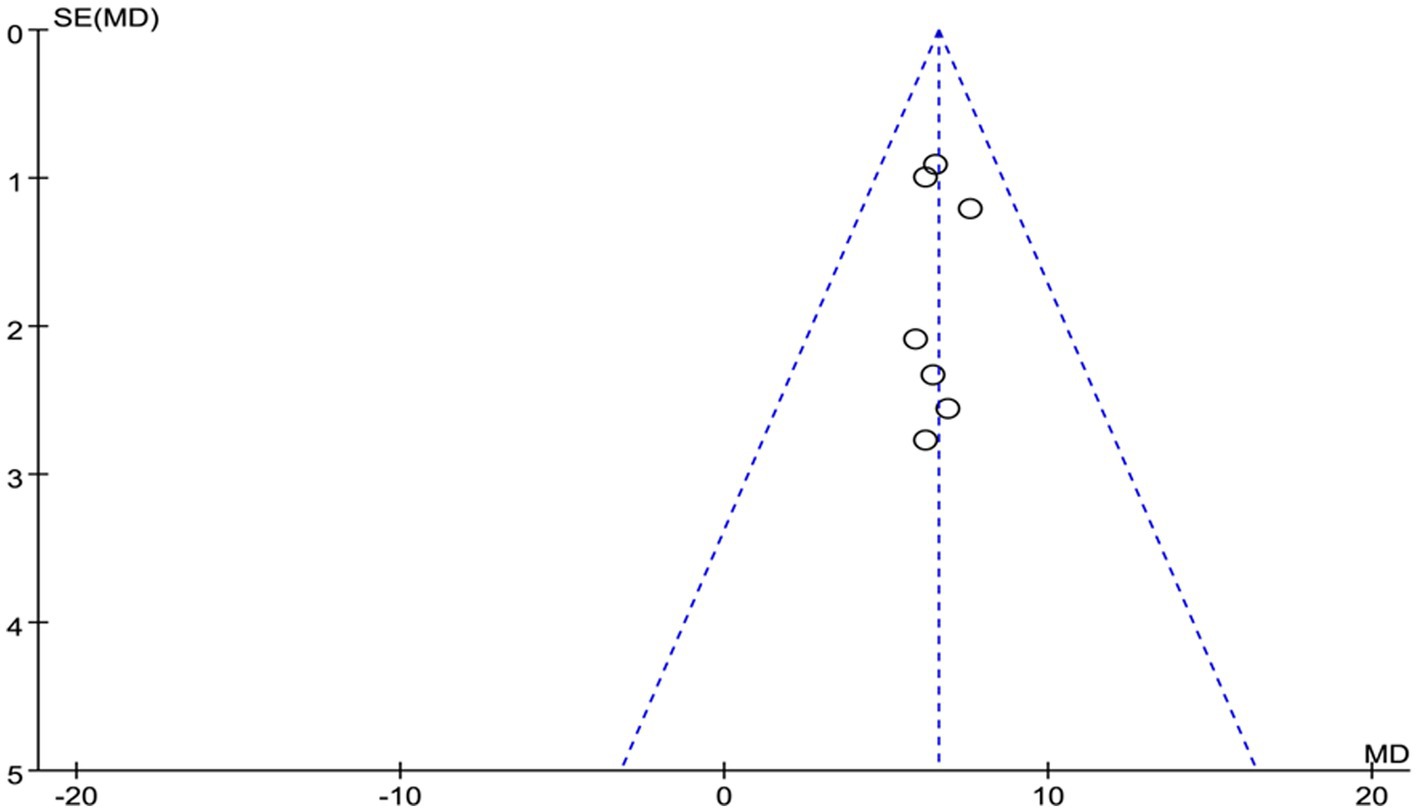
As shown in Figure 2, a meta-analysis of cross-sectional, case–control, and cohort studies revealed a significant association of RLS with depression. Compared with healthy individuals (n = 317), individuals with RLS (n = 364) had higher scores on the BDI, based on the fixed model (MD 6.58, 95% CI 5.54, 7.62, Z = 12.45, p < 0.01, Heterogeneity: I2 = 0%; p = 0.99), which suggests they have more severe depression. In addition, SDS and HADS were also significantly higher in individuals with RLS compared to healthy controls (for SDS, MD 9.68, 95% CI 7.44, 11.93, Z = 8.46, p < 0.01; Heterogeneity: I2 = 13%; p = 0.32; and for HADS, MD 3.28, 95% CI 2.45, 4.12, Z = 7.72, p < 0.01, Heterogeneity: I2 = 0%, p = 0.69). However, based on the random model, HAMD did not show a significant difference in depression between individuals with RLS those without RLS (MD 1.67, 95% CI −1.57, 4.91, Z = 1.01, p = 0.31, Heterogeneity: I2 = 95%, p < 0.01).
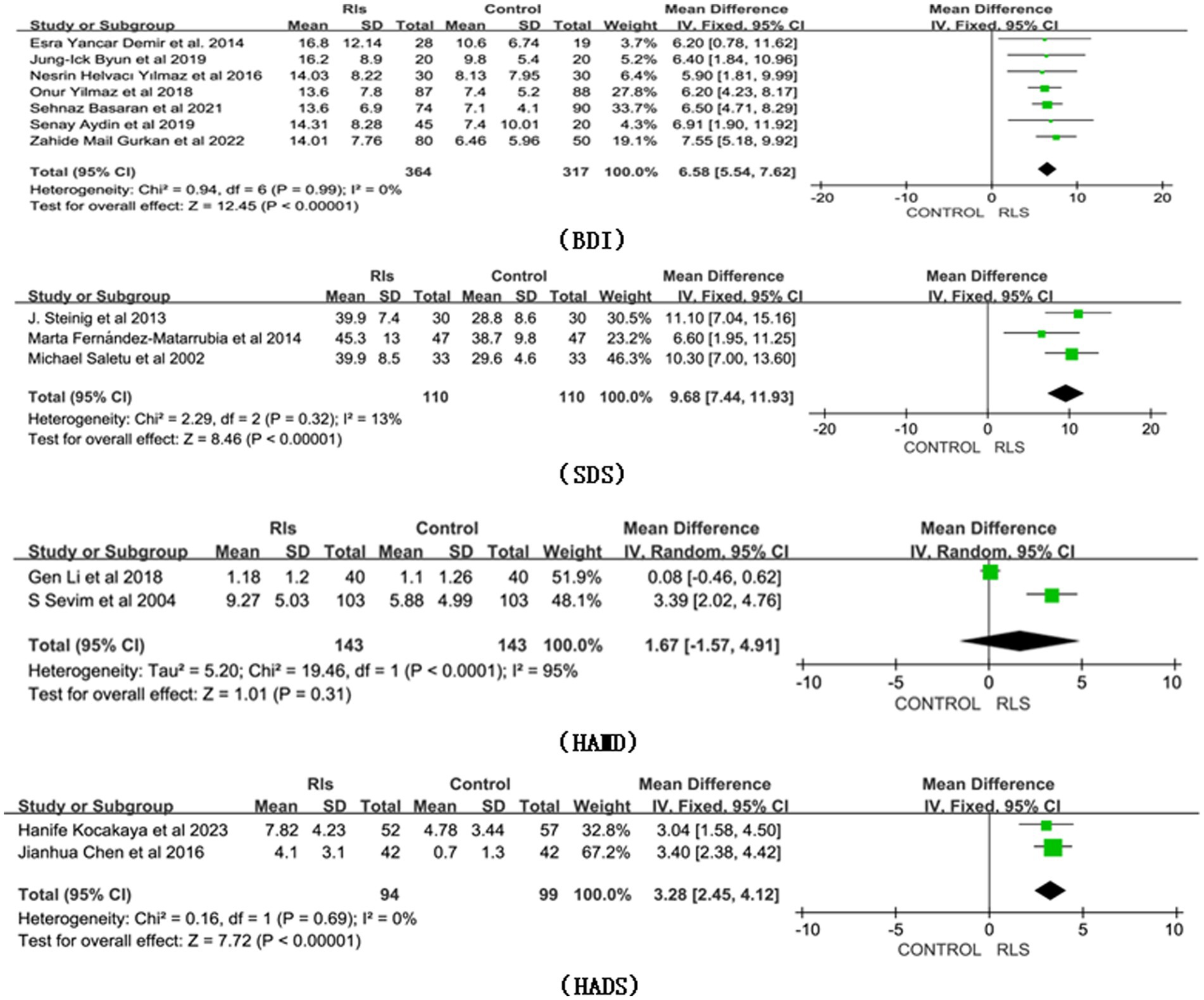
Figure 2. Forest plot of RLS and risk of depression symptoms. CI, Confidence interval; RLS, Restless Legs Syndrome.
3.4 Association of RLS with anxiety
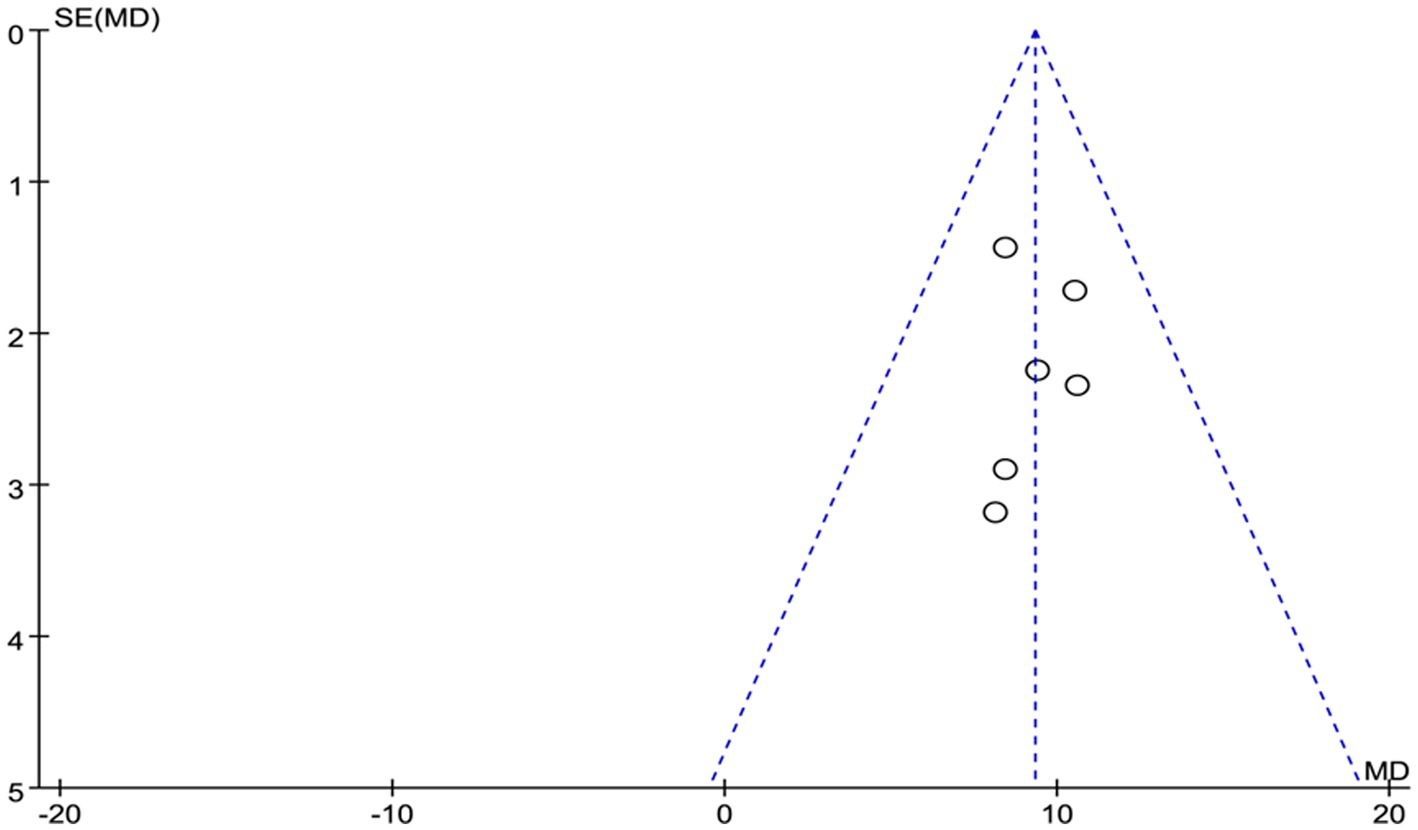
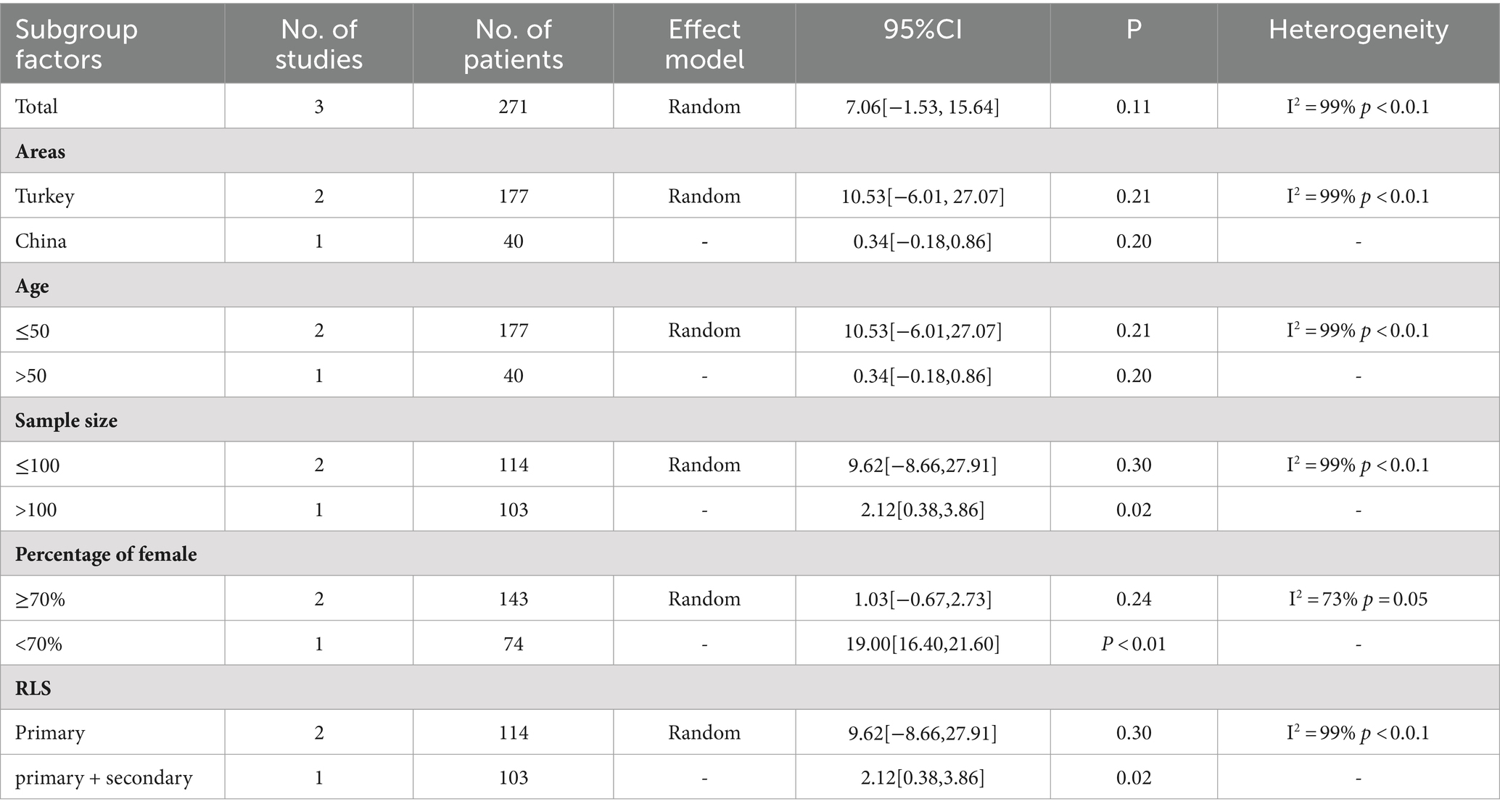
Compared with healthy controls (n = 222), individuals with RLS (n = 288) had higher scores on the BAI, based on the fixed model (Figure 3: MD 9.30, 95% CI 7.65 10.94, Z = 11.08, p < 0.01, Heterogeneity: I2 = 0%, p = 0.92). Moreover, SAS, HADS, and Goldberg scores were all significantly higher in individuals with RLS compared to healthy controls (respectively, MD 9.23, 95% CI 6.08, 12.39, Z = 5.74, p < 0.01, Heterogeneity: I2 = 71%, p = 0.03, MD 4.69; 95% CI 3.75, 5.63, Z = 9.78 p < 0.01, Heterogeneity: I2 = 50%; p = 0.16, and MD 1.85; 95% CI 1.44, 2.26, Z = 8.91 p < 0.01, Heterogeneity: I2 = 0%, p = 0.67). However, based on the random model, HAMA did not show a significant difference in anxiety scores for RLS (MD 7.06, 95% CI -1.53, 15.64, Z = 1.61, p = 0.11, Heterogeneity: I2 = 99%, p < 0.01).
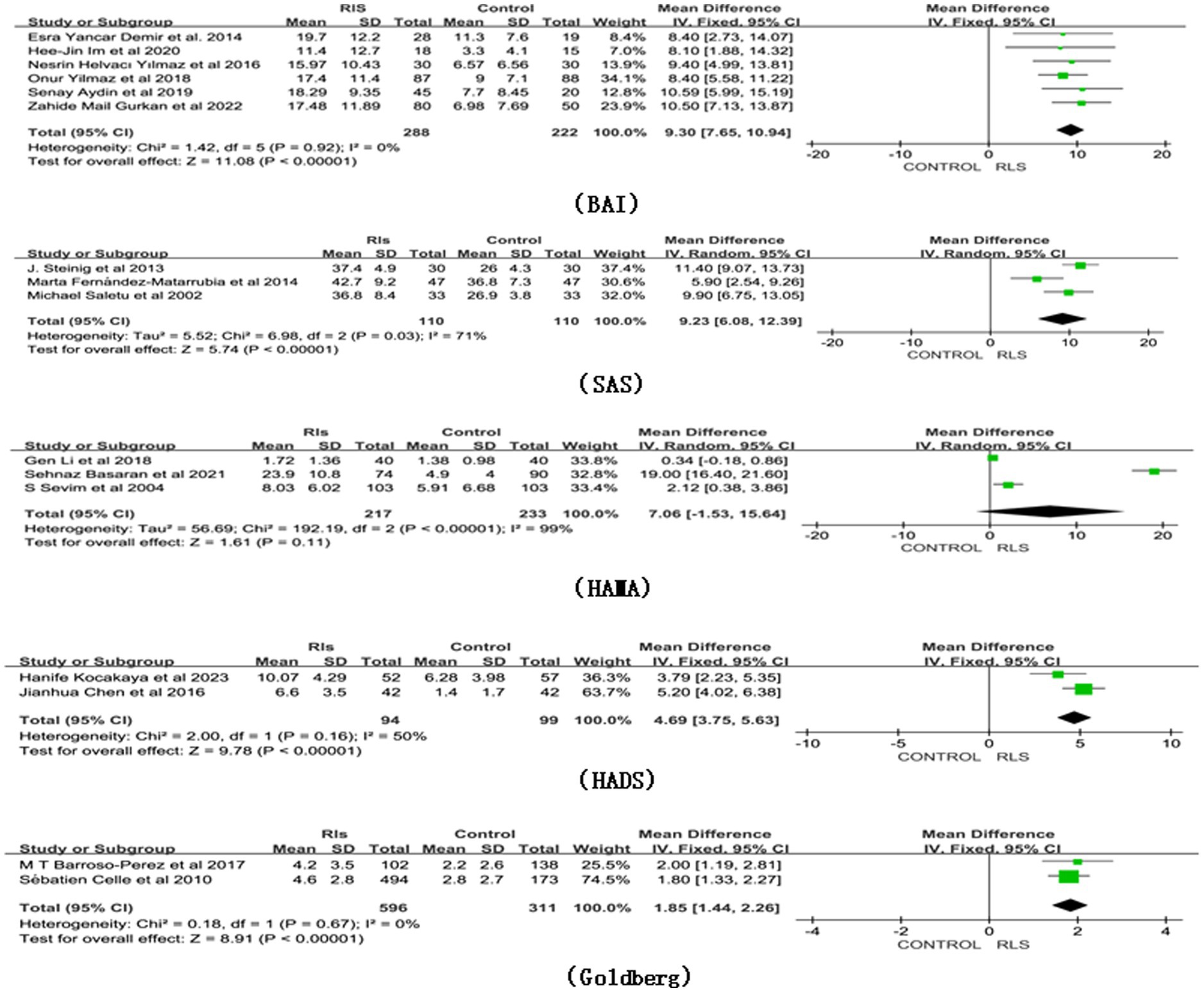
Figure 3. Forest plot of RLS and risk of anxiety symptoms. CI, Confidence interval; RLS, Restless Legs Syndrome.
3.5 Heterogeneity across studies, publication bias, subgroup analysis, and sensitivity analysis
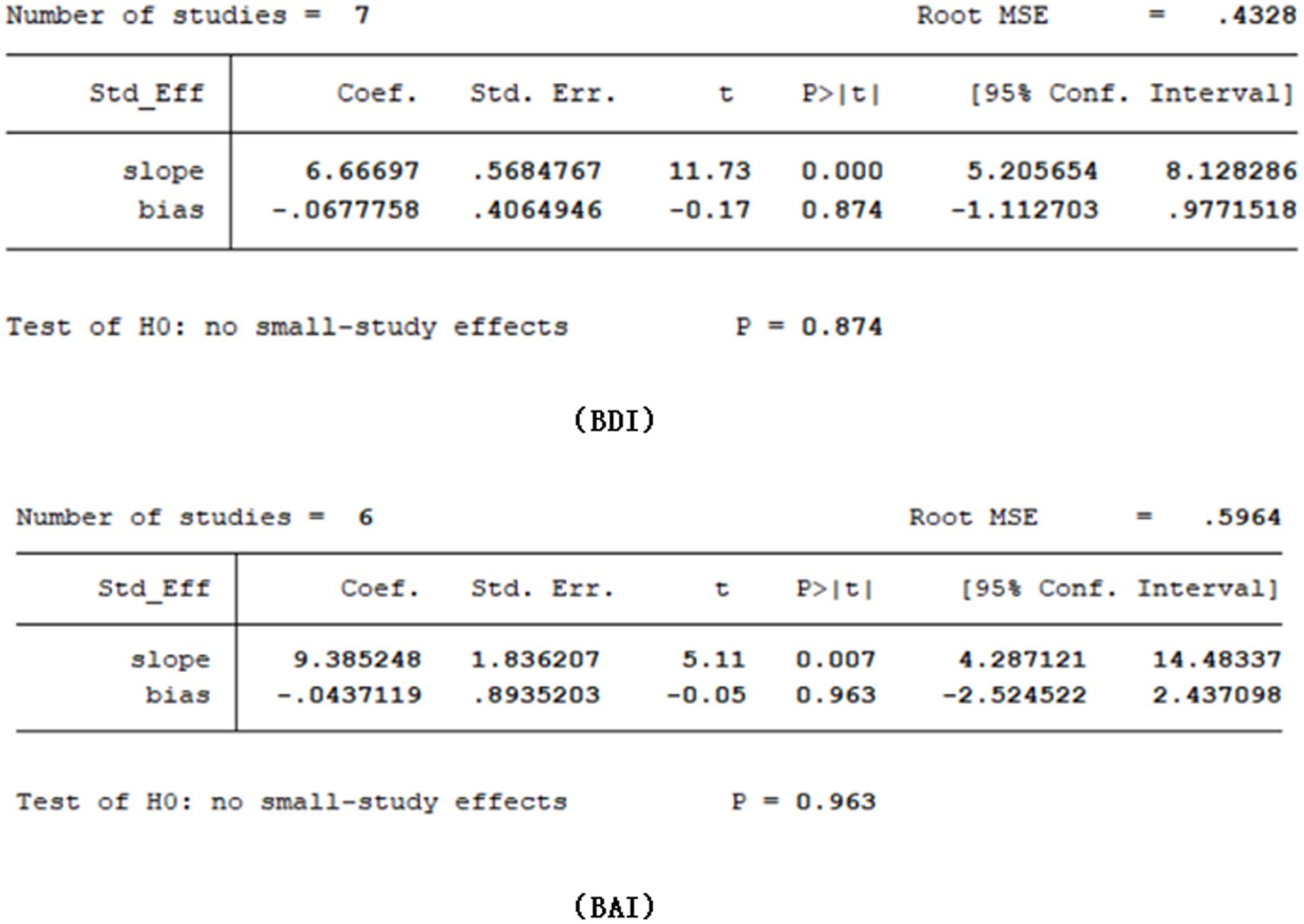
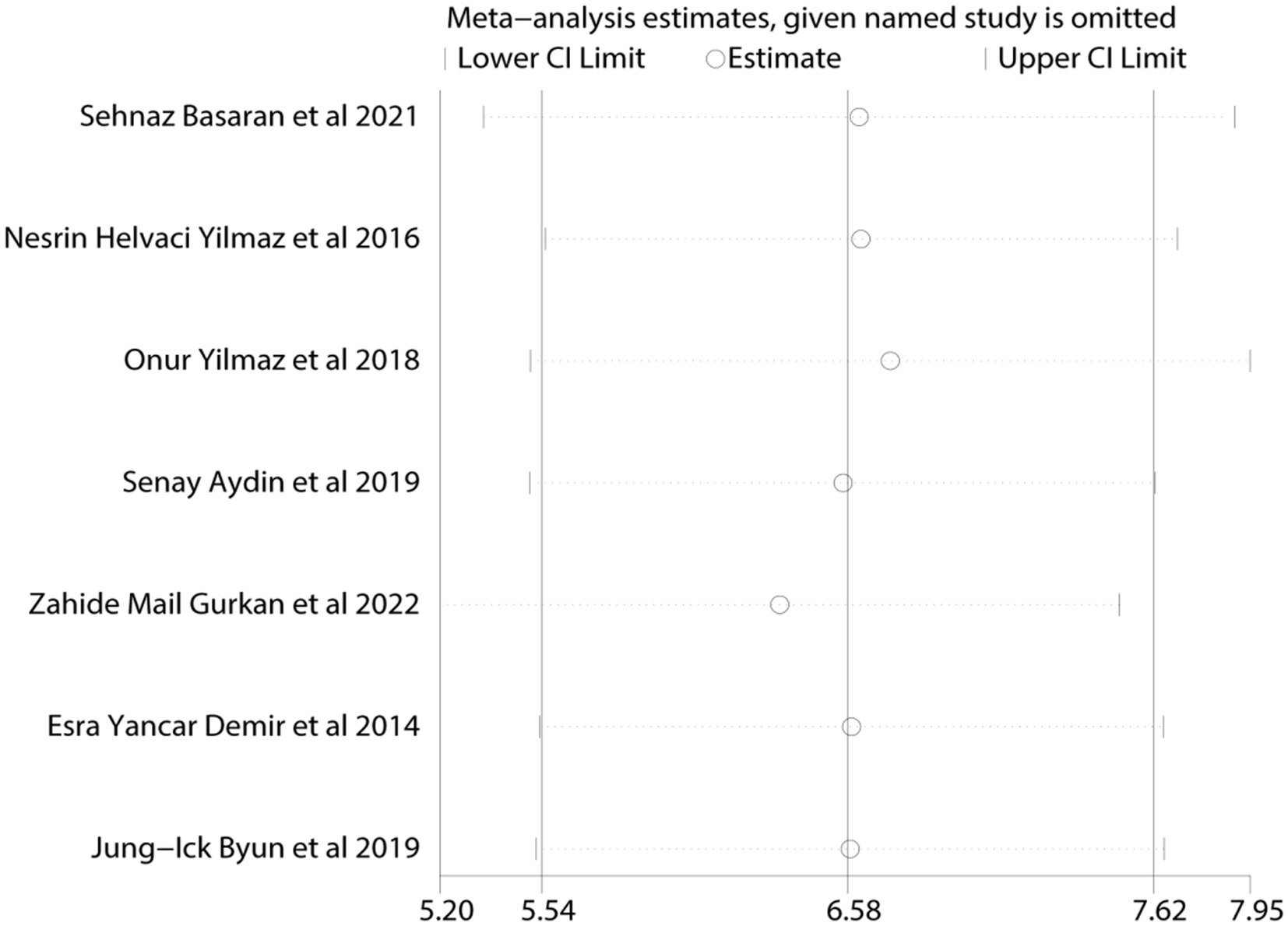
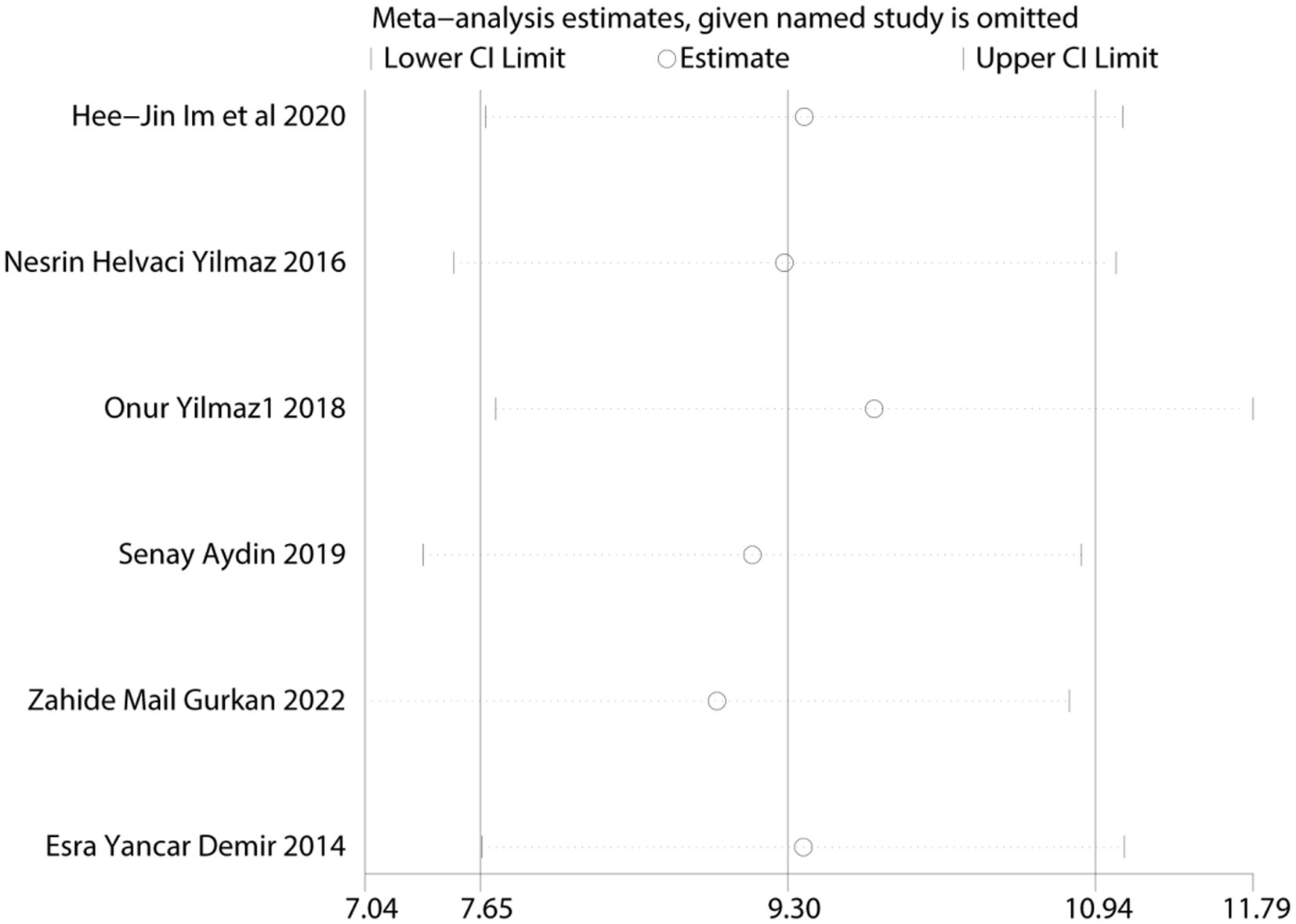
Given the limited inclusion of literature, we focused our primary analysis on the two scales that featured the most comprehensive literature, namely BDI and BAI. Because no statistically significant heterogeneity (defined as a p value of X2 < 0.1 or I2 > 50%) across studies was detected, we opted for the fixed model for BDI and BAI. Visual inspection of the funnel plots indicated a low publication bias (Figures 4, 5). The Egger’s test results for BDI (p = 0.874) and BAI (p = 0.963) were non-significant, suggesting no publication bias (Figure 6) (42). Sensitivity analyses were performed by excluding one study each time and rerunning the analysis to verify the robustness of the overall results. A sensitivity analysis confirmed the robustness of our significant findings of the result from BDI and BAI (Figures 7, 8). Subgroup analysis of RLS and healthy controls was used for HAMA was shown in Table 3.
4 Discussion
This study summarized and compared the current evidence of depression and anxiety symptoms between two group: a group with RLS and a group without RLS. A total of 21 studies were systematically reviewed and subjected to meta-analysis. Despite variations in sample sizes and the diagnostic scales used for depression, anxiety, or both, the selected studies demonstrated high overall methodological quality. However, certain results exhibited significant heterogeneity. We found that the levels of depressive or anxious symptoms were significantly higher in individuals with RLS than in those without RLS. To the best of our knowledge, this is the first meta-analysis to quantitatively compare levels of anxiety and depression between adults with RLS and healthy controls.
The association between RLS and anxiety or depression levels in individuals with other medical conditions has previously shown mixed results. Some studies found that RLS in conjunction with other medical conditions was associated with higher anxiety or depression levels. Recent studies based on large cross-sectional survey data suggested that RLS in individuals with multiple sclerosis (MS) may contribute to heightened anxiety and depression symptoms. The effects of RLS on patients with MS included negative effects on functional ability, anxiety levels, sleep quality, and health-related quality of life (43, 44). Rana et al. showed that individuals with Parkinson’s disease combined with RLS had the highest incidence of anxiety and depression (45). Lee et al. found that untreated patients with idiopathic RLS and periodic limb movement during sleep had high levels of anxiety and depression (46). Recent studies in patients with cancer have suggested a significant increase in anxiety and depression levels, as evidenced by higher total HADS scores in those with RLS (47, 48). However, RLS in other diseases does not consistently correlate with anxiety and depression. There was no significant difference in anxiety and depression levels observed in adults with attention-deficit hyperactivity disorder or inflammatory bowel disease who also had RLS (49, 50). The use of varying scales of measures to compare the anxiety and depression levels of individuals with RLS with healthy controls may lay the groundwork for understanding complex associations. Building on this knowledge gap, we conducted a meta-analysis focusing on RLS-related anxiety and depression. By comparing the results from various depression and anxiety scales, our analysis demonstrated that the symptoms of depression or anxiety were more pronounced in individuals with RLS than in individuals without RLS.
In addition, data related to the interaction between RLS severity and anxiety and depression in patients with RLS are conflicting. One study from Korea evaluated anxiety and insomnia as factors that affected RLS severity (51). Other studies have shown no relationship between RLS severity and differences in depression and anxiety. Depressive symptoms in patients with RLS seem to be related to sleep impairment. Subjects with chronic insomnia were at a high risk of developing major depressive disorder (52–54). Perhaps more severe RLS symptoms associated with sleep disturbance would have had an effect on cognitive performance if left untreated (39, 55). A future meta-analysis could continue to examine the contribution of RLS severity to the increased risk of anxiety and depressive symptoms.
In the meta-analysis, the HAMD and HAMA did not show statistically significant differences between the individuals with RLS and the controls. First, it is important to note that the HAMD was only used in the studies reported in two articles; therefore, the number of articles was too small to confer certainty to the results. Second, significant heterogeneity was observed in the HAMA scores. Heterogeneity remained after subgroup analysis, and differences in age range, study design (including psychological assessment), scoring criteria, and sample size may have contributed to this heterogeneity.
Our findings highlight the positive associations between RLS and depression and anxiety. The precise mechanisms underlying these associations have not been elucidated. Nonetheless, certain evidence might help explain this phenomenon. The patients with RLS experienced night-time sensations characterized by an irresistible urge to move their legs. These sensations intensified during periods of rest, particularly at night, leading the patients to engage in movements or massage their limbs for relief. Prolonged occurrences of these symptoms significantly diminished the sleep quality of individuals with RLS, potentially triggering the onset of depression and anxiety (56). Dopamine is a neurotransmitter involved in muscle control and behavior and has a crucial role in the functioning of the central nervous system. When dopamine-pathway dysfunction occurs, involuntary movement can occur, which could lead to RLS (57–59). Our review showed that dopamine levels followed a circadian pattern, with the highest levels observed at 8 a.m. In the evening, between 20:00 and 22:00, dopamine levels dropped to approximately 60% of their peak levels. The lowest point occurred at 3 am (60). Therefore, the patients had mild RLS symptoms during the day and severe symptoms at night. Decreased levels of monoamine neurotransmitters, such as dopamine, could lead to anxiety and depression (61, 62). At night, dopamine levels were low, which may have caused anxiety and depression. Meanwhile, the patients with RLS had symptoms of severe physical discomfort, and their uncomfortable symptoms might aggravate anxiety and depression. RLS may have a substantial psychological effect on the affected individuals. Our study revealed a need in the clinical setting for physicians to evaluate psychological symptoms when diagnosing RLS and consider incorporating psychological counseling for patients as part of the treatment.
The current study had some limitations. First, not all depression and anxiety scales were analyzed, with some scales having too few associated literature articles for a comprehensive analysis, such as the STAI, PHQ-9, GDS, and SCL-90-R. Second, although we conducted subgroup analyses, the identified heterogeneity remained high, which made it challenging to pinpoint the exact source. Future studies with larger sample sizes are warranted to clearly identify the sources of heterogeneity.
5 Conclusion
This systematic review and meta-analysis of cross-sectional, case–control, and cohort studies revealed a higher risk of depression and anxiety among individuals with RLS than among their healthy counterparts. Efforts should be made by organizations to increase awareness of the psychological health of individuals affected by RLS.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
TA: Formal analysis, Methodology, Software, Writing – original draft. HS: Formal analysis, Methodology, Software, Writing – review & editing. LY: Methodology, Software, Writing – review & editing. XW: Formal analysis, Methodology, Writing – review & editing. BL: Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Hebei province administration of traditional Chinese medicine scientific research project (2023204) and North China University of Science and Technology doctoral starting fund (28432299).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Trotti, LM. Restless legs syndrome and sleep-related movement disorders. Continuum (Minneap Minn). Sleep Neurol. (2017) 23:1005–16. doi: 10.1212/CON.0000000000000488
2. Allen, RP, Picchietti, DL, Garcia-Borreguero, D, Ondo, WG, Walters, AS, Winkelman, JW, et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated international restless legs syndrome study group (IRLSSG) consensus criteria-history, rationale, description, and significance. Sleep Med. (2014) 15:860–73. doi: 10.1016/j.sleep.2014.03.025
3. Wijemanne, S, and Ondo, W. Restless legs syndrome: clinical features, diagnosis and a practical approach to management. Pract Neurol. (2017) 17:444–52. doi: 10.1136/practneurol-2017-001762
4. Ohayon, MM, O'Hara, R, and Vitiello, MV. Epidemiology of restless legs syndrome: a synthesis of the literature. Sleep Med Rev. (2012) 16:283–95. doi: 10.1016/j.smrv.2011.05.002
5. Bjorvatn, B, Leissner, L, Ulfberg, J, Gyring, J, Karlsborg, M, Regeur, L, et al. Prevalence, severity and risk factors of restless legs syndrome in the general adult population in two Scandinavian countries. Sleep Med. (2005) 6:307–12. doi: 10.1016/j.sleep.2005.03.008
6. Nagandla, K, and De, S. Restless legs syndrome: pathophysiology and modern management. Postgrad Med J. (2013) 89:402–10. doi: 10.1136/postgradmedj-2012-131634
7. Kalaydjian, A, Bienvenu, OJ, Hening, WA, Allen, RP, Eaton, WW, and Lee, HB. Restless legs syndrome and the five-factor model of personality: results from a community sample. Sleep Med. (2009) 10:672–5. doi: 10.1016/j.sleep.2008.07.004
8. Winkelman, JW, Finn, L, and Young, T. Prevalence and correlates of restless legs syndrome symptoms in the Wisconsin sleep cohort. Sleep Med. (2006) 7:545–52. doi: 10.1016/j.sleep.2006.01.004
9. Li, G, Tang, H, Chen, J, Qi, X, Chen, S, and Ma, J. Executive and visuospatial dysfunction in patients with primary restless legs syndrome/Willis-Ekbom disease: study of a Chinese population. J Clin Sleep Med. (2018) 14:785–90. doi: 10.5664/jcsm.7106
10. Pearson, VE, Allen, RP, Dean, T, Gamaldo, CE, Lesage, SR, and Earley, CJ. Cognitive deficits associated with restless legs syndrome (RLS). Sleep Med. (2006) 7:25–30. doi: 10.1016/j.sleep.2005.05.006
11. Fulda, S, Beitinger, ME, Reppermund, S, Winkelmann, J, and Wetter, TC. Short-term attention and verbal fluency is decreased in restless legs syndrome patients. Mov Disord. (2010) 25:2641–8. doi: 10.1002/mds.23353
12. Zhang, LY, Ma, XY, Lin, J, Liu, WH, Guo, W, Yin, L, et al. Prevalence and risk factors of restless legs syndrome in hemodialysis patients. Nat Sci Sleep. (2020) 12:19–27. doi: 10.2147/NSS.S236393
13. Hornyak, M. Depressive disorders in restless legs syndrome: epidemiology, pathophysiology and management. CNS Drugs. (2010) 24:89–98. doi: 10.2165/11317500-000000000-00000
14. Happe, S, Baune, BT, Lanz, M, Berger, K, and Hornyak, M. Restless legs syndrome in patients with depressive disorders. Somnologie. (2012) 16:183–8. doi: 10.1007/s11818-012-0568-7
15. Cederberg, KLJ, Jeng, B, Sasaki, JE, and Motl, RW. Restless legs syndrome, sleep quality, and perceived cognitive impairment in adults with multiple sclerosis. Mult Scler Relat Disord. (2020) 43:102176. doi: 10.1016/j.msard.2020.102176
16. Stevens, MS. Restless legs syndrome/Willis-Ekbom disease morbidity: burden, quality of life, cardiovascular aspects, and sleep. Sleep Med Clin. (2015) 10:369–73. doi: 10.1016/j.jsmc.2015.05.017
17. Becker, PM, and Sharon, D. Mood disorders in restless legs syndrome (Willis-Ekbom disease). Clin Psychiatry. (2014) 75:e679–94. doi: 10.4088/JCP.13r08692
18. Wells, GA, Shea, B, O’Connell, D, Peterson, J, Welch, V, Losos, M, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. (2009). Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
19. Hamilton, M. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
20. Egger, M, Davey Smith, G, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
21. Sterne, JA, and Egger, M. Funnel plots for detecting bias in meta-analysis:guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/s0895-4356(01)00377-8
22. Basaran, S, and Tas, Hİ. Evaluation of affective temperament profile and levels of depressive symptoms and anxiety in patients with restless legs syndrome. Sleep Breath. (2022) 26:381–8. doi: 10.1007/s11325-021-02375-3
23. Sevim, S, Dogu, O, Kaleagasi, H, Aral, M, Metin, O, and Camdeviren, H. Correlation of anxiety and depression symptoms in patients with restless legs syndrome: a population based survey. J Neurol Neurosurg Psychiatry. (2004) 75:226–30. doi: 10.1007/BFb0026701
24. Yilmaz, O, Şengül, Y, Şengül, HS, Parlakkaya, FB, and Öztürk, A. Investigation of alexithymia and levels of anxiety and depression among patients with restless legs syndrome. Neuropsychiatr Dis Treat. (2018) 14:2207–14. doi: 10.2147/NDT.S174552
25. Barroso-Perez, MT, Cubo, E, Cordero-Guevara, J, Poza-Maure, E, and Checa-Diez, L. Calidad de Vida y caracteristicas asociadas del sindrome de piernas inquietas en la poblacion adulta de Burgos, España quality of life and associated characteristics of restless legs syndrome in the adult population of Burgos, Spain. Rev Neurol. (2017) 65:257–62. doi: 10.33588/rn.6506.2016576
26. Aydin, S. Huzursuz Bacaklar Sendromu ve Bilişsel Fonksiyonlar; restless legs syndrome and cognitive functions. J Turk Sleep Med. (2019) 6:22–8. doi: 10.4274/jtsm.galenos.2019.92485
27. Steinig, J, Reess, T, Klösch, G, Sauter, C, Zeitlhofer, J, and Happe, S. Personality traits in patients with restless legs syndrome. Somnologie. (2013) 17:281–3. doi: 10.1007/s11818-013-0623-z
28. Kocakaya, H, and Say, B. Evaluation of emotional dysregulation in patients with restless legs syndrome. Sleep Biol Rhythms. (2023) 21:447–54. doi: 10.1007/s41105-023-00467-z
29. Mail Gurkan, Z, Tantik Pak, A, Parlakkaya, FB, Kilicarslan, T, Yilmaz, O, and Sengul, Y. Recognition of emotional face expressions in patients with restless legs syndrome. Appl Neuropsychol Adult. (2022):1–6. doi: 10.1080/23279095.2022.2043326
30. Byun, JI, Kim, JS, Shin, YY, Hwang, KJ, Jung, YJ, and Shin, WC. Difference in psychological distress between patients with periodic limb movement disorder and restless legs syndrome. Sleep Med Res. (2019) 10:25–30. doi: 10.17241/smr.2019.00339
31. Ylmaz, NH, Cantürk, E, Arc Düz, ZGE, Parlakolu, B, and Zer, FF. The prevalence of fibromyalgia in patients with restless legs syndrome. Turk Noroloji Dergisi. (2016) 22:161–6. doi: 10.4274/tnd.04764
32. Fernández-Matarrubia, M, Cuadrado, ML, Sánchez-Barros, CM, Martínez-Orozco, FJ, Fernández-Pérez, C, Villalibre, I, et al. Prevalence of migraine in patients with restless legs syndrome: a case-control study. Headache. (2014) 54:1337–46. doi: 10.1111/head.12382
33. Saletu, M, Anderer, P, Saletu, B, Lindeck-Pozza, L, Hauer, C, and Saletu-Zyhlarz, G. EEG mapping in patients with restless legs syndrome as compared with normal controls. Psychiatry Res. (2002) 115:49–61. doi: 10.1016/s0925-4927(02)00023-9
34. Chen, JH, Huang, R, Luo, JM, Xiao, Y, Zhong, X, and Liu, XQ. Restless legs syndrome in adults in Peking union medical college hospital. Zhongguo Yi Xue Ke Xue Yuan Xue Ba. (2016) 38:548–53. doi: 10.3881/j.issn.1000-503X.2016.05.010
35. Im, HJ, Kim, JH, Yun, CH, Kim, DW, and Oh, J. Changes in Hepcidin serum levels correlate with clinical improvement in idiopathic restless legs syndrome patients. J Clin Med. (2020) 9:4115. doi: 10.3390/jcm9124115
36. Trautmann, E, Barke, A, Frisch, JU, Schmidt, AL, Kunert, F, Canelo, M, et al. Restless legs syndrome: psychiatric comorbidities are more important than neuroticism. Behav Sleep Med. (2015) 13:375–86. doi: 10.1080/15402002.2014.919917
37. Cho, SJ, Hong, JP, Hahm, BJ, Jeon, HJ, Chang, SM, Cho, MJ, et al. Restless legs syndrome in a community sample of Korean adults: prevalence, impact on quality of life, and association with DSM-IV psychiatric disorders. Sleep. (2009) 32:1069–76.
38. Zanigni, S, Giannini, G, Melotti, R, Pattaro, C, Provini, F, Cevoli, S, et al. Association between restless legs syndrome and migraine: a population-based study. Eur J Neurol. (2014) 21:1205–10. doi: 10.1111/ene.12462
39. Lee, HB, Ramsey, CM, Spira, AP, Vachon, J, Allen, R, and Munro, CA. Comparison of cognitive functioning among individuals with treated restless legs syndrome (RLS), untreated RLS, and no RLS. J Neuropsychiatry Clin Neurosci. (2014) 26:87–91. doi: 10.1176/appi.neuropsych.12120394
40. Demir, EY, Zcan, T, Zer, F, Parlakolu, BA, Enginyurt, Z, and Ankaya, S. Restless legs syndrome and depression-anxiety disorder association in iron deficiency anemia patients. J Exp Clin Med. (2014) 31:225–9. doi: 10.5835/jecm.omu.31.04.005
41. Celle, S, Roche, F, Kerleroux, J, Thomas-Anterion, C, Laurent, B, Rouch, I, et al. Prevalence and clinical correlates of restless legs syndrome in an elderly French population: the synapse study. J Gerontol A Biol Sci Med Sci. (2010) 65:167–73. doi: 10.1093/gerona/glp161
42. Dalton, JE, Bolen, SD, and Mascha, EJ. Publication Bias: the elephant in the review. Anesth Analg. (2016) 123:812–3. doi: 10.1213/ANE.0000000000001596
43. Sevim, S, Demirkiran, M, Terzi, M, Yüceyar, N, Taşdelen, B, Idiman, E, et al. Coexistence of restless legs syndrome and multiple sclerosis aggravates anxiety and depression. Arq Neuropsiquiatr. (2022) 80:168–72. doi: 10.1590/0004-282X-ANP-2020-0400
44. Seferoğlu, M, Sivaci, AÖ, and Tunç, A. Restless legs syndrome/Willis-Ekbom disease in multiple sclerosis: a contributing factor for anxiety, disability, sleep disorder, and quality of life. Arq Neuropsiquiatr. (2020) 78:708–12. doi: 10.1590/0004-282X20200084
45. Rana, AQ, Mosabbir, AA, Qureshi, AR, Abbas, M, and Rana, MA. Restless leg syndrome: a risk factor of higher prevalence of anxiety and depression in Parkinson's disease patients. Neurol Res. (2016) 38:309–12. doi: 10.1080/01616412.2016.1147682
46. Lee, HB, Song, ML, Koo, BB, and Cho, YW. Mood symptoms and restless legs syndrome without periodic limb movements during sleep: is it a clinical subtype? J Neuropsychiatry Clin Neurosci. (2017) 29:52–9. doi: 10.1176/appi.neuropsych.15090228
47. Saini, A, Berruti, A, Ferini-Strambi, L, Castronovo, V, Rametti, E, Giuliano, PL, et al. Restless legs syndrome as a cause of sleep disturbances in cancer patients receiving chemotherapy. J Pain Symptom Manag. (2013) 46:56–64. doi: 10.1016/j.jpainsymman.2012.06.018
48. Ostacoli, L, Saini, A, Ferini-Strambi, L, Castronovo, V, Sguazzotti, E, Picci, RL, et al. Restless legs syndrome and its relationship with anxiety, depression, and quality of life in cancer patients undergoing chemotherapy. Qual Life Res. (2010) 19:531–7. doi: 10.1007/s11136-010-9614-8
49. Wagner, ML, Walters, AS, and Fisher, BC. Symptoms of attention-deficit/hyperactivity disorder in adults with restless legs syndrome. Sleep. (2004) 27:1499–504. doi: 10.1093/sleep/27.8.1499
50. Schindlbeck, KA, Becker, J, Berger, F, Mehl, A, Rewitzer, C, Geffe, S, et al. Impact of restless legs syndrome in patients with inflammatory bowel disease on sleep, fatigue, and quality of life. Int J Color Dis. (2017) 32:125–30. doi: 10.1007/s00384-016-2681-8
51. Kim, JB, Koo, YS, Eun, MY, Park, KW, and Jung, KY. Psychosomatic symptom profiles in patients with restless legs syndrome. Sleep Breath. (2013) 17:1055–61. doi: 10.1007/s11325-013-0800-0
52. Hornyak, M, Kopasz, M, Berger, M, Riemann, D, and Voderholzer, U. Impact of sleep-related complaints on depressive symptoms in patients with restless legs syndrome. J Clin Psychiatry. (2005) 66:1139–45. doi: 10.4088/jcp.v66n0909
53. Ford, DE, and Kamerow, DB. Epidemiologic study of sleep disturbances and psychiatric disorders: an opportunity for prevention? JAMA. (1989) 262:1479–84. doi: 10.1001/jama.262.11.1479
54. Riemann, D, and Voderholzer, U. Primary insomnia: a risk factor to develop depression? J Affect Disord. (2003) 76:255–9. doi: 10.1016/s0165-0327(02)00072-1
55. Galbiati, A, Marelli, S, Giora, E, Zucconi, M, Oldani, A, and Ferini-Strambi, L. Neurocognitive function in patients with idiopathic restless legs syndrome before and after treatment with dopamine-agonist. Int J Psychophysiol. (2015) 95:304–9. doi: 10.1016/j.ijpsycho.2014.12.005
56. Geng, C, Yang, Z, Kong, X, Xu, P, and Zhang, H. Correlation between vitamin D and poor sleep status in restless legs syndrome. Front Endocrinol. (2022) 13:994545. doi: 10.3389/fendo.2022.994545
57. Earley, CJ, Connor, J, Garcia-Borreguero, D, Jenner, P, Winkelman, J, Zee, PC, et al. Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis–Ekbom disease). Sleep Med. (2014) 15:1288–301. doi: 10.1016/j.sleep.2014.05.009
58. Gossard, TR, Trotti, LM, Videnovic, A, and St Louis, EK. Restless legs syndrome: contemporary diagnosis and treatment. Neurotherapeutics. (2021) 18:140–55. doi: 10.1007/s13311-021-01019-4
59. Turjanski, N, Lees, AJ, and Brooks, DJ. Striatal dopaminergic function in restless legs syndrome: 18F-dopa and 11C-raclopride PET studies. Neurology. (1999) 52:932–7. doi: 10.1212/wnl.52.5.932
60. Sowers, JR, and Vlachakis, N. Circadian variation in plasma dopamine levels in man. J Endocrinol Investig. (1984) 7:341–5. doi: 10.1007/BF03351014
61. Qi, G, Zhang, P, Li, T, Li, M, Zhang, Q, He, F, et al. NAc-VTA circuit underlies emotional stress-induced anxiety-like behavior in the three-chamber vicarious social defeat stress mouse model. Nat Commun. (2022) 13:577. doi: 10.1038/s41467-022-28190-2
Keywords: depression, anxiety, restless legs syndrome, meta-analysis, mental health
Citation: An T, Sun H, Yuan L, Wu X and Lu B (2024) Associations of anxiety and depression with restless leg syndrome: a systematic review and meta-analysis. Front. Neurol. 15:1366839. doi: 10.3389/fneur.2024.1366839
Edited by:
Keisuke Suzuki, Dokkyo Medical University, JapanReviewed by:
Jung Bin Kim, Korea University Anam Hospital, Republic of KoreaCornelius Bachmann, Independent Researcher, Osnabrück, Germany
Copyright © 2024 An, Sun, Yuan, Wu and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiuling Wu, d3V4aXVsaW5nMjAxMkAxMjYuY29t; Baoquan Lu, YmFvcXVhbmx1QDE2My5jb20=
 Tianyang An1
Tianyang An1 Baoquan Lu
Baoquan Lu