- Department of Neurosurgery, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Background: A bibliometric analysis was conducted to understand the current research status and trends in facial nerve injury after cerebellopontine angle (CPA) tumors to identify new perspectives for future research.
Methods: CiteSpace was used to visualize and analyze relevant literature included in the CNKI and WanFang databases, and the Web of Science Core Collection from 2015 to 2024. Chinese literature was deduplicated using NoteExpress.
Results: A total of 7,021 studies was retrieved, showing a pattern of rapid increase in this research area over the past 10 years. Protection and management of the facial nerve in surgery and early recognition of facial nerve injury were the research hotspots and trends.
Conclusion: This study emphasizes the importance of intraoperative protection and management of the facial nerve. Limited research has addressed the postoperative facial nerve injury from the perspective of functional rehabilitation and patient psychology. These areas need more attention and focused research.
1 Introduction
The cerebellopontine angle (CPA) is a triangular three-dimensional area located in the anterolateral aspect of the posterior cranial fossa between the cerebellum, pons, medulla oblongata and the petrous part of the temporal bone. Approximately 10–15% of the intracranial tumors originate in this area (1). Most CPA tumors are benign and patients may present with neurological symptoms such as hearing impairment, vestibular dysfunction, and headaches (2). Treatment options include conservative treatment, radiation therapy, and surgical removal, which should be chosen based on patient preferences and clinical indicators and conditions such as physical status and tumor size (3). About 80% ~ 94% of CPA tumors are vestibular schwannomas, which reinforces surgical resection as the optimal treatment. This procedure carries a 10% ~ 60% chance of damaging the facial nerve (3–5).
Facial nerve injury, and even facial paralysis, can occur in patients because of intraoperative damage to the cranial nerves, especially the facial nerve, secondary to CPA space constraints (6, 7). Expression defects and chewing weakness may occur when patients suffer facial nerve injury (8), potentially triggering adverse emotional states such as anxiety and depression, thereby affecting their social participation (9–12). Patients with impaired or not fully rehabilitated facial nerve function will experience asymmetric facial movements (13). These sequelae significantly compromise their physical and mental health. Kenton et al. (14) conducted qualitative interviews with patients with facial nerve injuries after vestibular schwannoma to understand their distress. They found that the root of the distress was long-term facial paralysis, alteration of self-perception, and social anxiety. Therefore, it is of great significance and necessity to visualize the current status, hotspots, and frontiers of research on patients with postoperative facial nerve injury after CPA tumors.
Bibliometrics is employed to analyze literature in a specific field, aiming to explain the structure of research trends through statistical methods, lexical analysis, and citation analysis, etc. (15). In recent years, CiteSpace has been widely used for bibliometric visualization and analysis, including citations, collaborations, countries, keywords, clusters, and burst terms (16). Currently, the characteristics and management of facial nerve injuries associated with CPA tumors remain inadequately explored. Therefore, this study aimed to employ CiteSpace software and bibliometric methods to conduct a visual analysis of relevant research, to identify the research hotspots and emerging frontiers concerning facial nerve injury following surgical treatment of CPA tumors.
2 Methods
2.1 Literature sources and search strategies
We searched the CNKI and WanFang databases, as well as the Web of Science core collection. Chinese language Database was searched using the terms “lesions of the pontine cerebellar horn region,” “lesions of the pontine cerebellar horn region,” “vestibular nerve sheath tumors,” “acoustic neuromas,” “facial nerves,” “facial nerve injuries,” “facial nerve dysfunction,” “facial paralysis,” “facial nerve palsy,” and more. We also performed searches in English using the terms “cerebellopontine angle,” “neuroma,” “acoustic,” “neurofibromatosis,” “acoustic neuroma,” “vestibular schwannoma,” “facial nerve,” “facial paralysis,” “facial nerve function,” and “facial nerve palsy.” Literature was searched for the last 10 years, from 2015 to 2024. Literatures related to facial nerve injury from cerebellopontine angle tumors was included. While, literature that is grey, duplicate, or published in languages other than English or Chinese was excluded. It’s worth noting that Chinese literature refers to publications in Chinese, not necessarily by Chinese authors. Additionally, Chinese literature was imported into NoteExpress for deduplication and then into CiteSpace software for analysis.
2.2 Data analysis
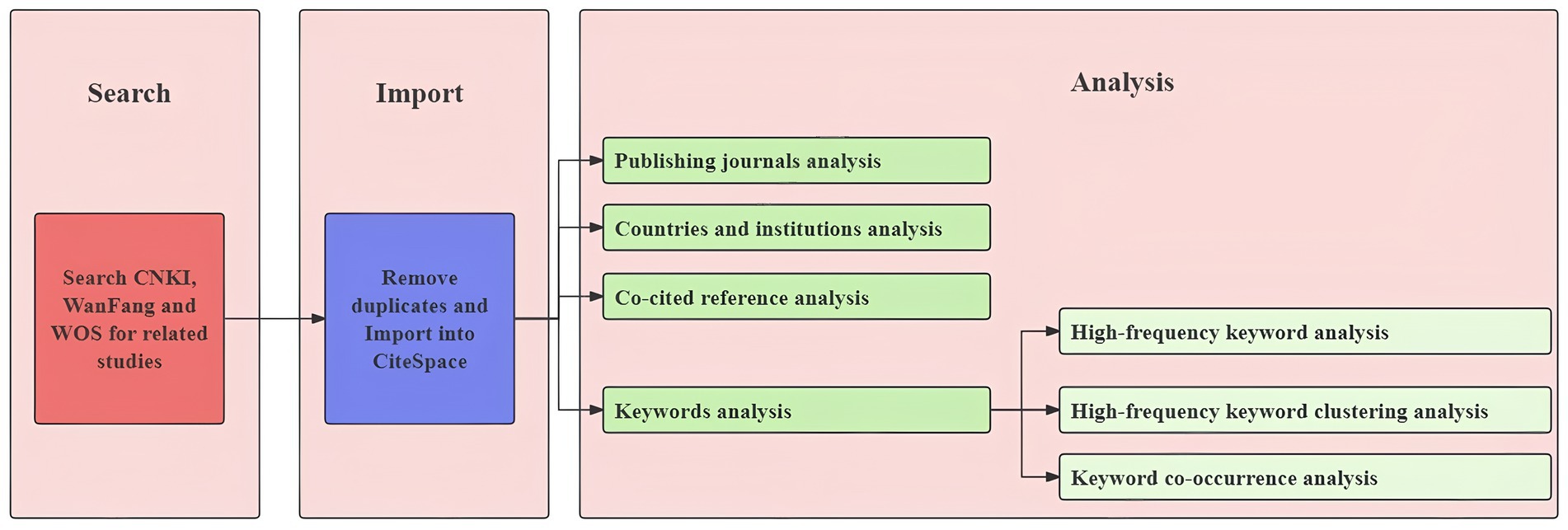
Chinese and English records literature were exported in RefWorks and Plain-text format, respectively, and both were imported into CiteSpace software for format conversion. The time selection used was 2015–2024, and the time slices were set to one-year intervals. Visualization and analysis were performed and plotted after the relevant parameters were set according to the software (Figure 1).
3 Results
3.1 Literature search results, publication trends, and country distribution
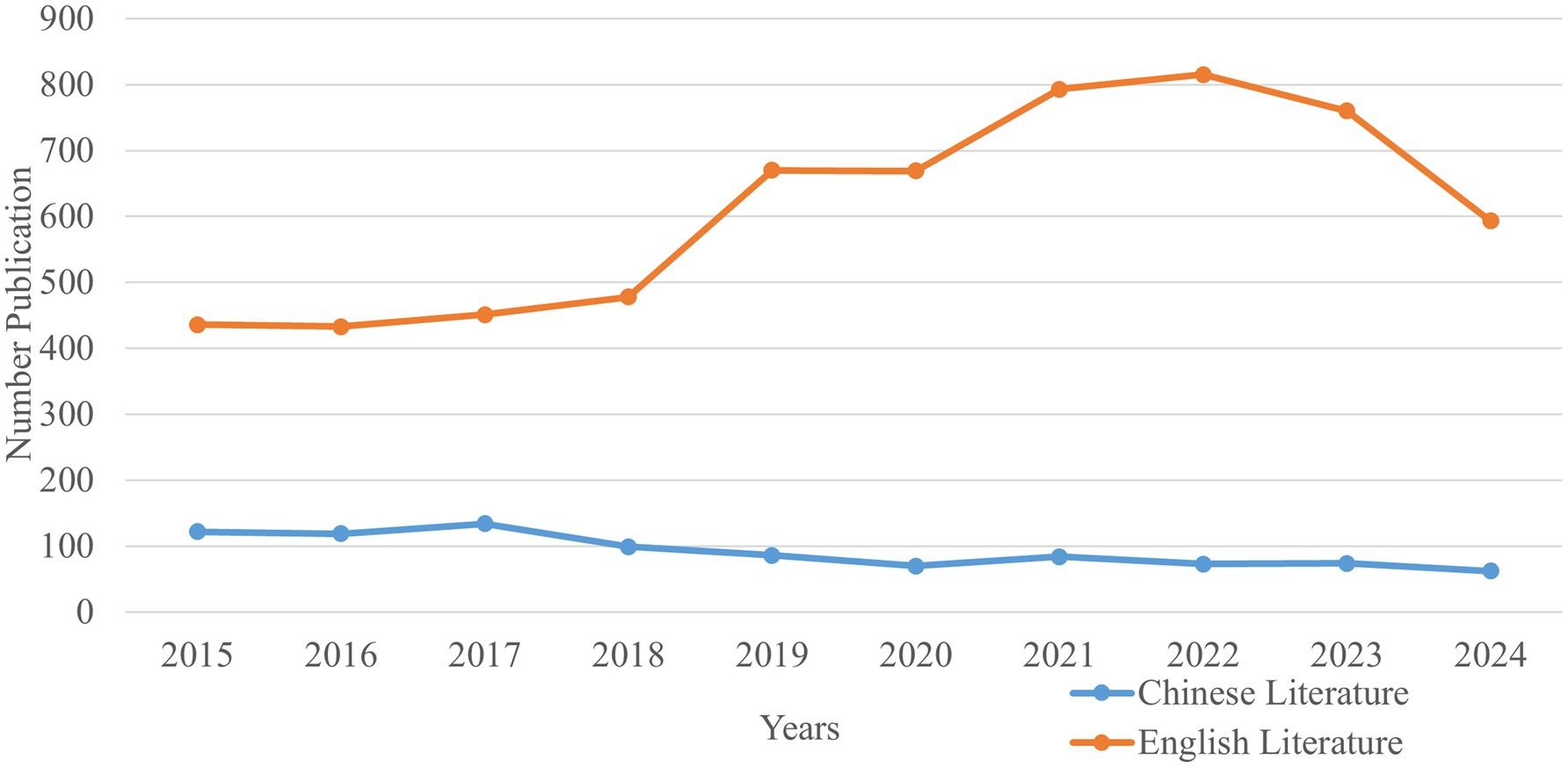
Altogether, 1,227 and 6,098 studies were retrieved in Chinese and English, respectively. A total of 7,021 studies remained after deduplication using NoteExpress. The number of studies related to CPA tumors and facial nerve demonstrated a decreasing trend in Chinese and an increasing trend in English (Figure 2). Furthermore, the number of Chinese studies was significantly lower than that of English. The year 2022 was the peak year for English publications on research related to the CPA and facial nerve, with 815 studies. The top 5 countries for this research, in order of publication volume, were the United States, China, Germany, Japan, and Italy. Among them, the United States ranked first with 1,703 studies, reflecting its research leadership on this field within the academic space.
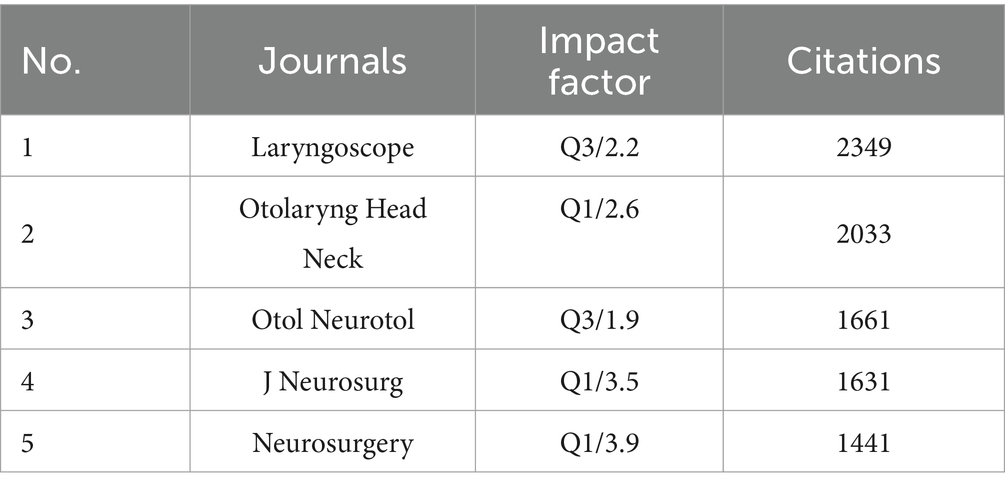
3.2 Publishing journals analysis
Analysis was restricted to English-language journals owing to technical constraints of the bibliometric software. In terms of the number of citations, the journal Laryngoscope was the most cited English journal with a total of 2,349 citations for studies related to the CPA and facial nerve (Table 1).
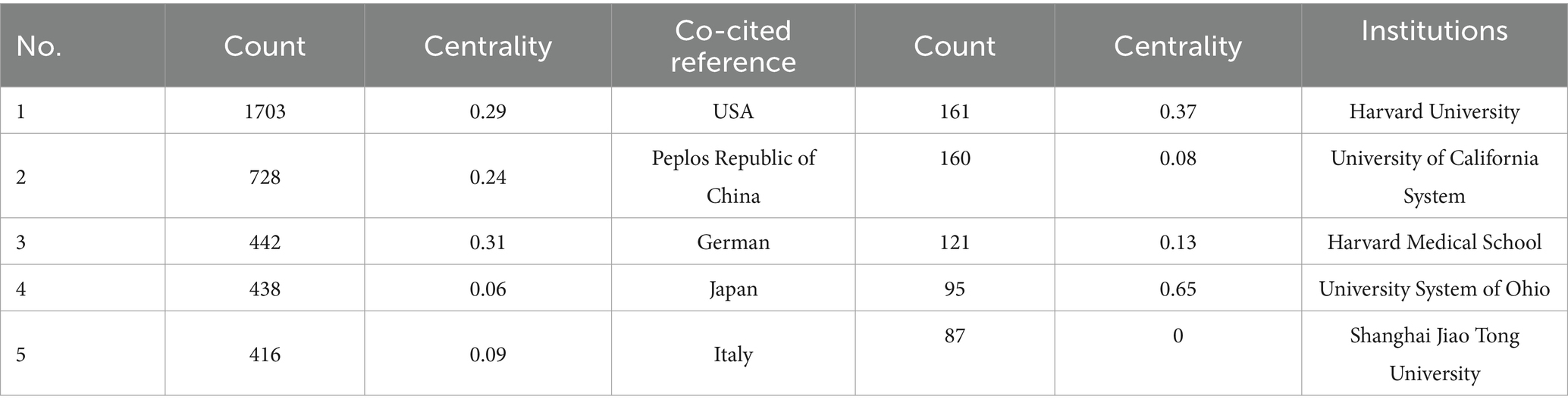
3.3 Countries and institutions analysis
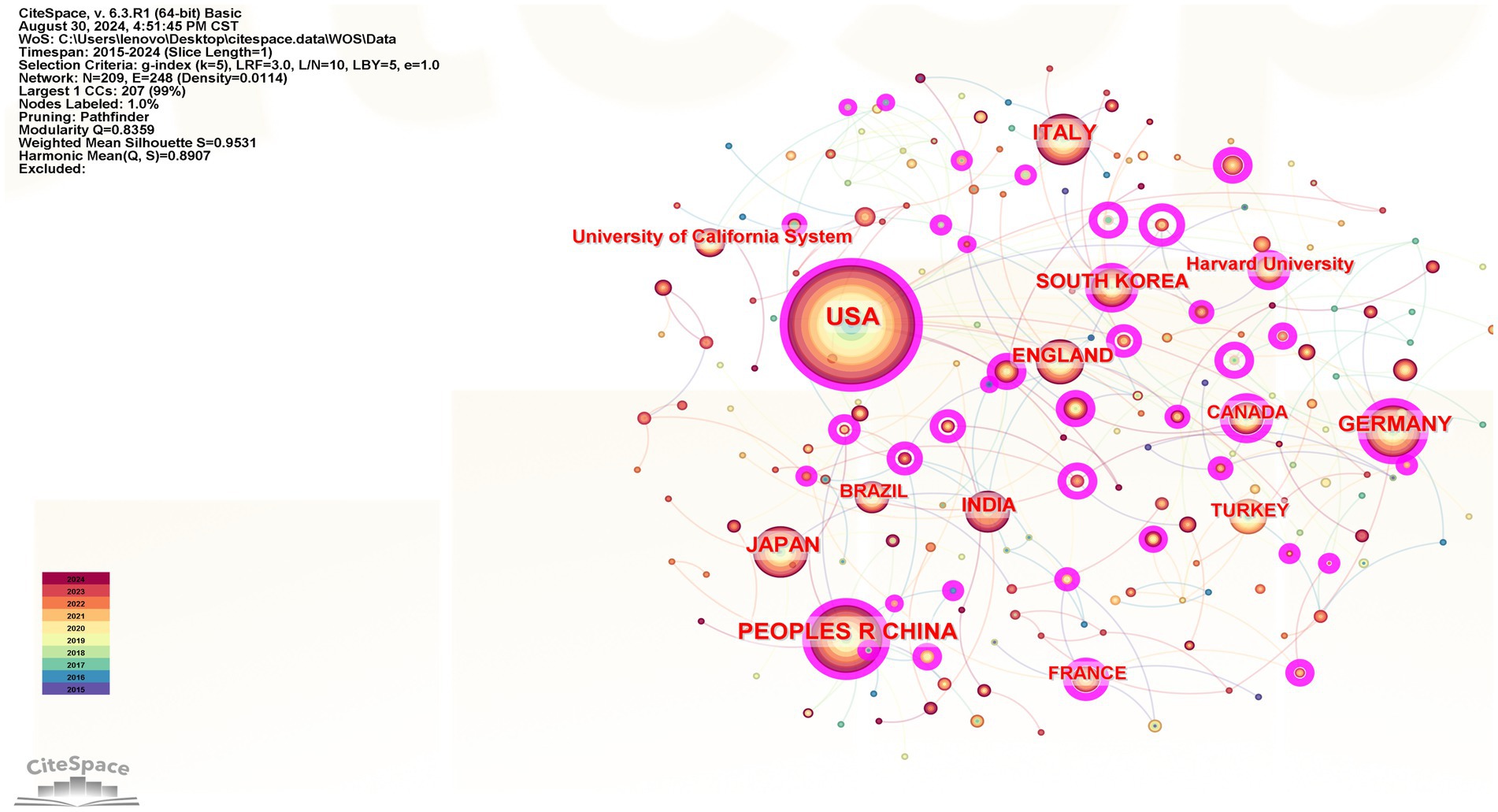
The top 5 countries were the USA, the People’s Republic of China, Germany, Japan, and Italy, while the top 5 institutions were Harvard University, the University of California System, Harvard Medical School, the University of London, and Shanghai Jiao Tong University. For details, see Figure 3 and Table 2.
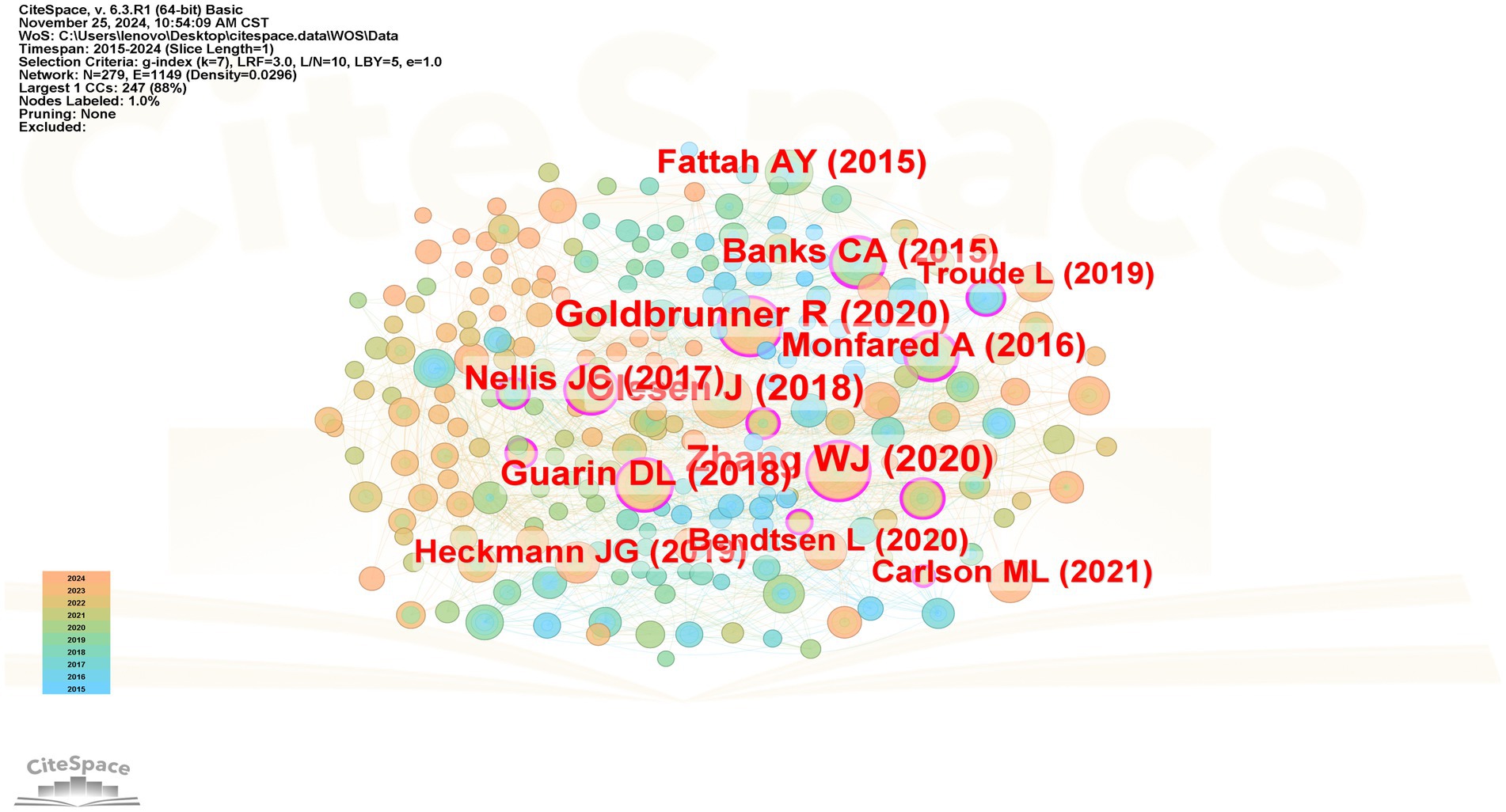
3.4 Co-cited reference analysis
Table 3 presents the top ten co-cited references related to postoperative facial nerve injury in CPA tumors, which have been co-cited more than 400 times. The first co-cited reference was published in 2020 by Goldbrunner et al. (17). This article provided guidelines for the diagnosis and treatment of vestibular schwannoma and laid the foundation for conducting clinically relevant research. The second reviewed the anatomy of the facial nerve (18), and the possible etiology of facial paralysis development. The third article (19) focused on comparing the efficacy different between topiramate and acetazolamide in reducing intracranial pressure. The results showed that Topiramate was more effective. The Figure 4 shows the literature co-citation analysis.
3.5 Keywords analysis
3.5.1 High-frequency keyword analysis
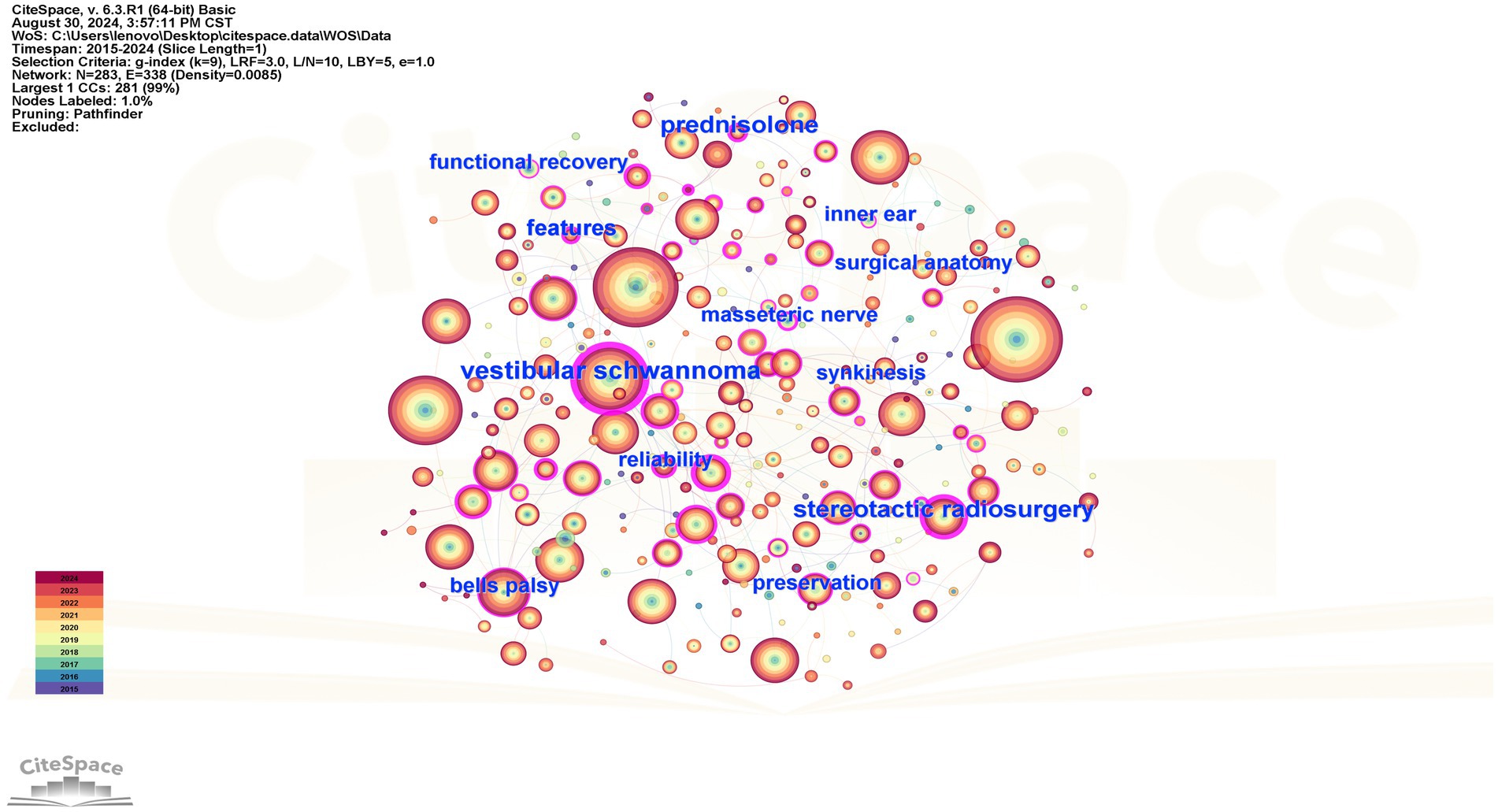
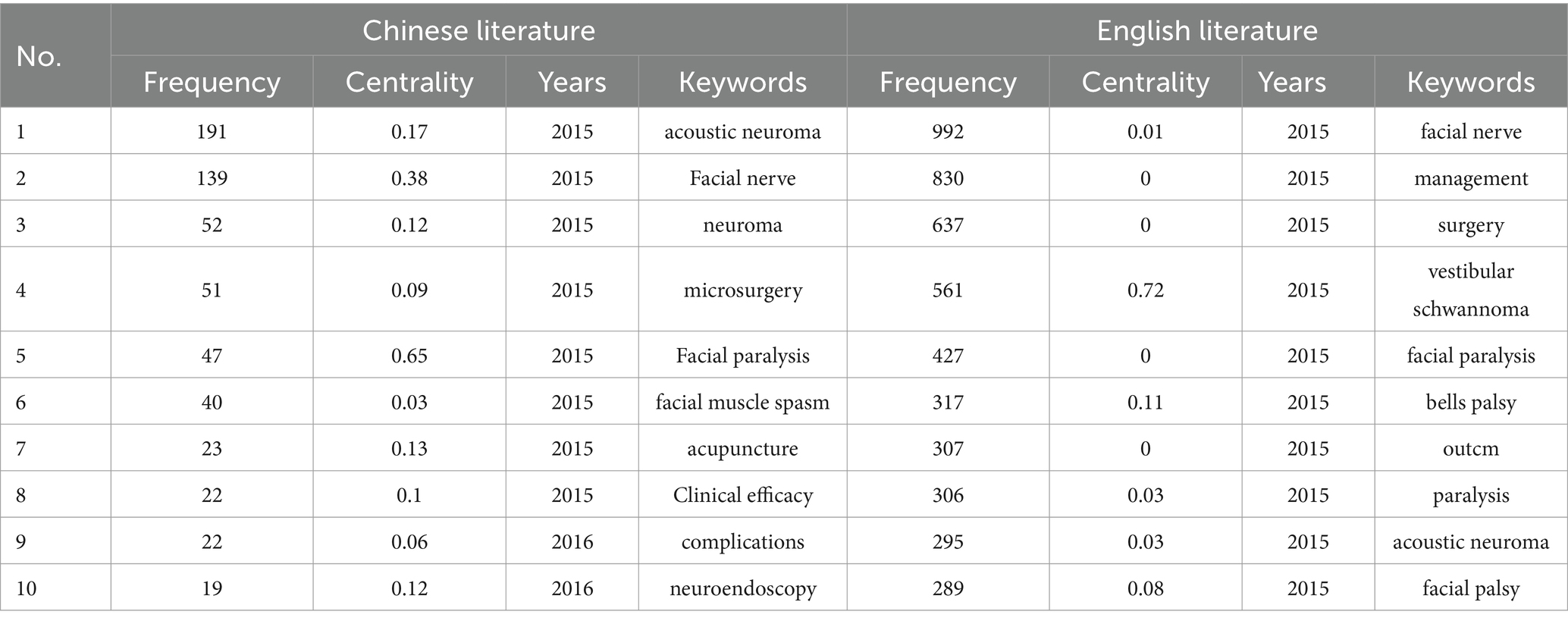
The co-occurrence graph of high-frequency keywords in Chinese and English is shown in Figures 5, 6, after setting the time slice to 1, node type to keyword, and frequency threshold to the Top 50. Both English and Chinese studies focused on acoustic neuroma, facial nerve, facial palsy, and surgery. Table 4 shows the top ten keywords in both English and Chinese.
3.5.2 High-frequency keyword clustering analysis
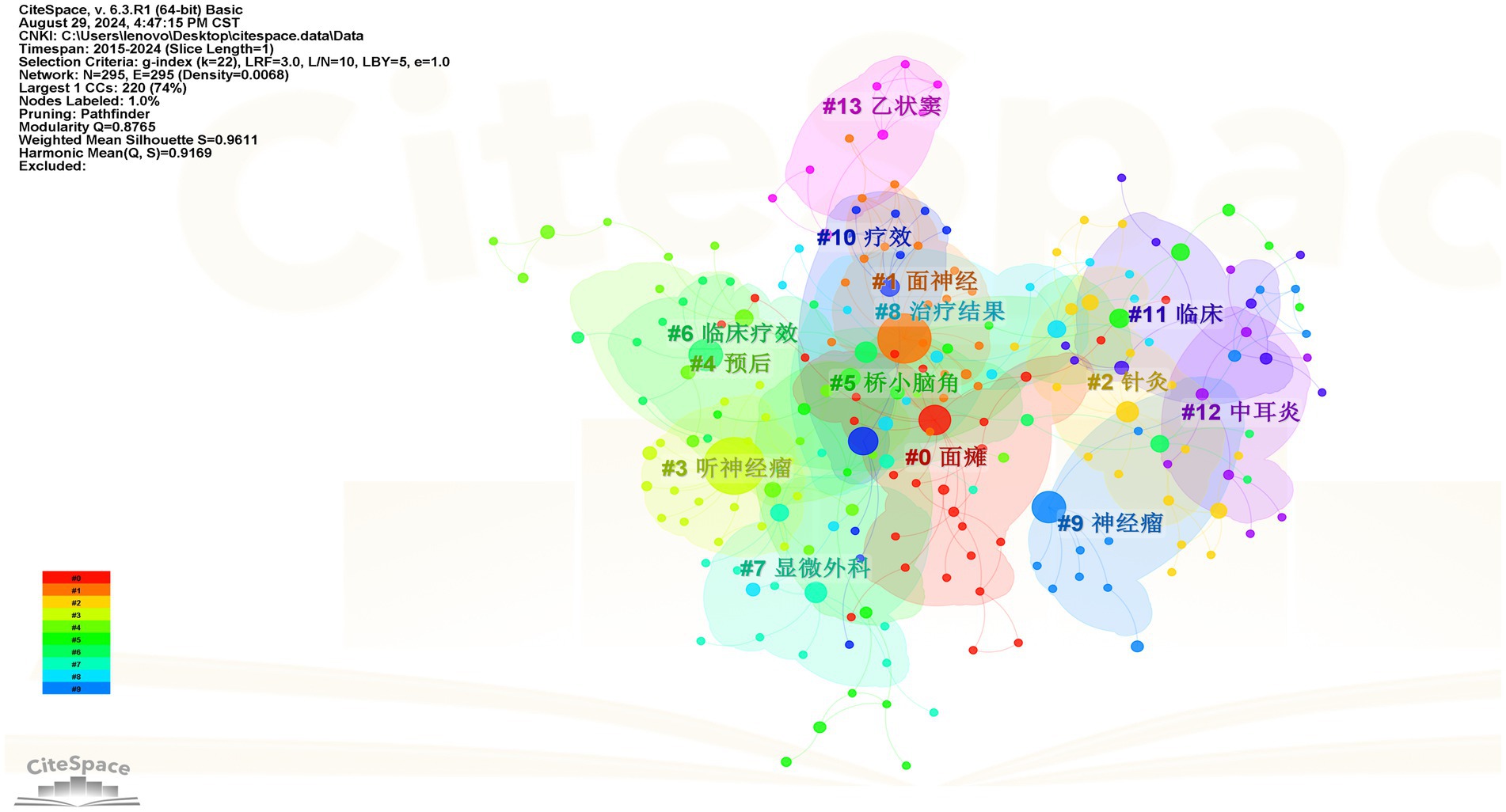
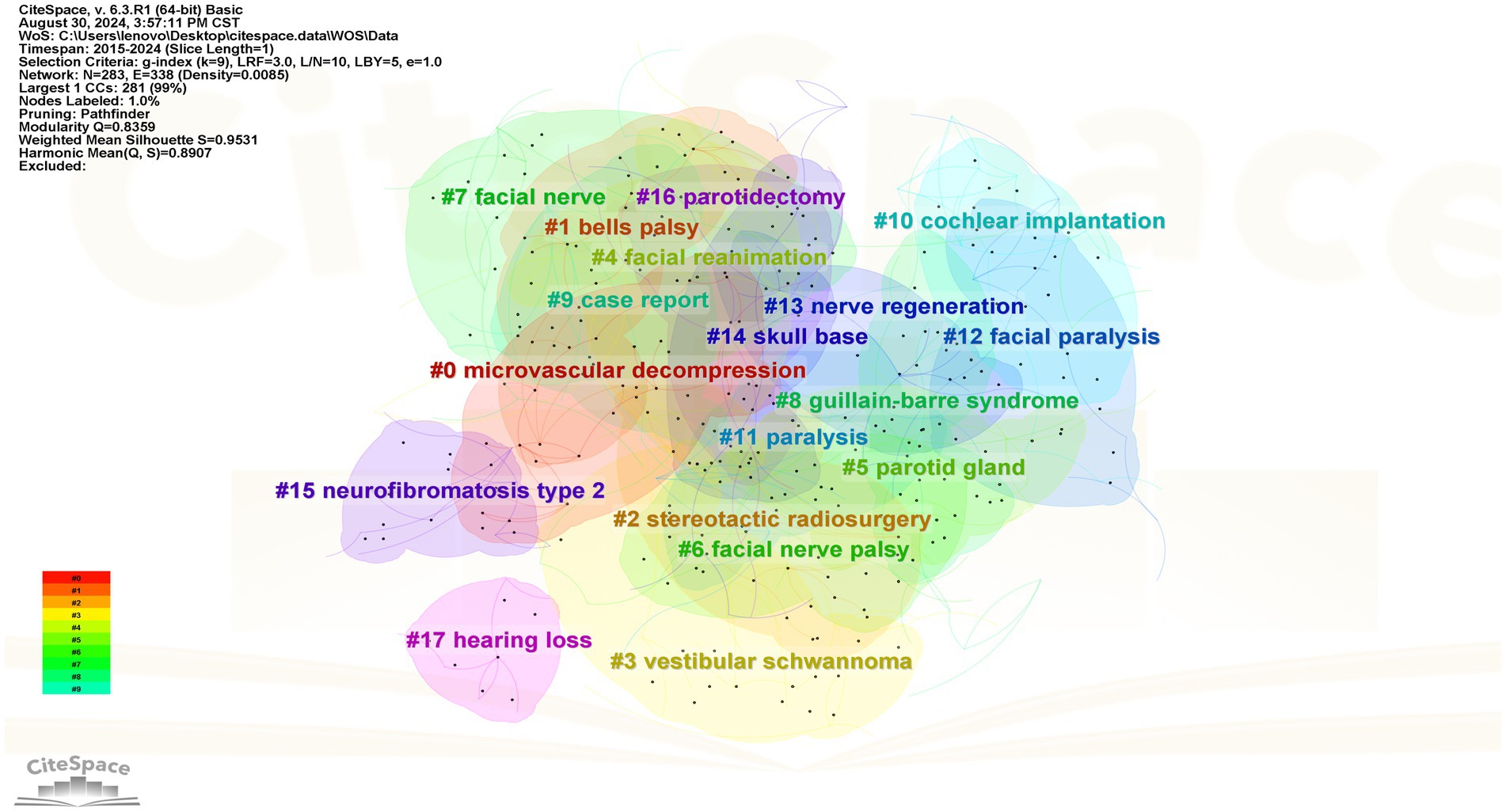
It is generally accepted that a Q value > 0.3 indicates a significant clustering result, while an S value > 0.5 is considered to represent reasonable clustering in keyword analysis. The Q and S values of the Chinese and English studies were 0.877 and 0.961, and 0.836 and 0.953, respectively, indicating that the cluster analysis was efficient and convincing. The smaller the cluster tag value, the more keywords it contains. The cluster analysis mapping of high-frequency keywords related to facial nerve injury and CPA tumors in Chinese and English studies is shown in Figures 7, 8, respectively.
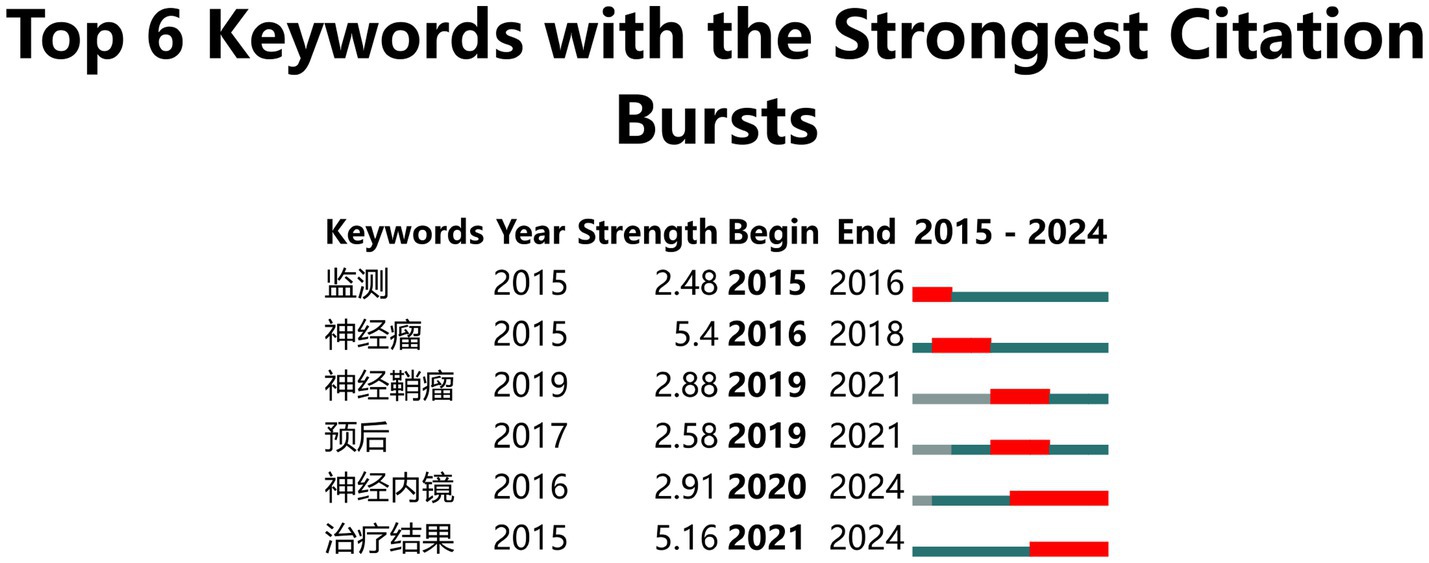
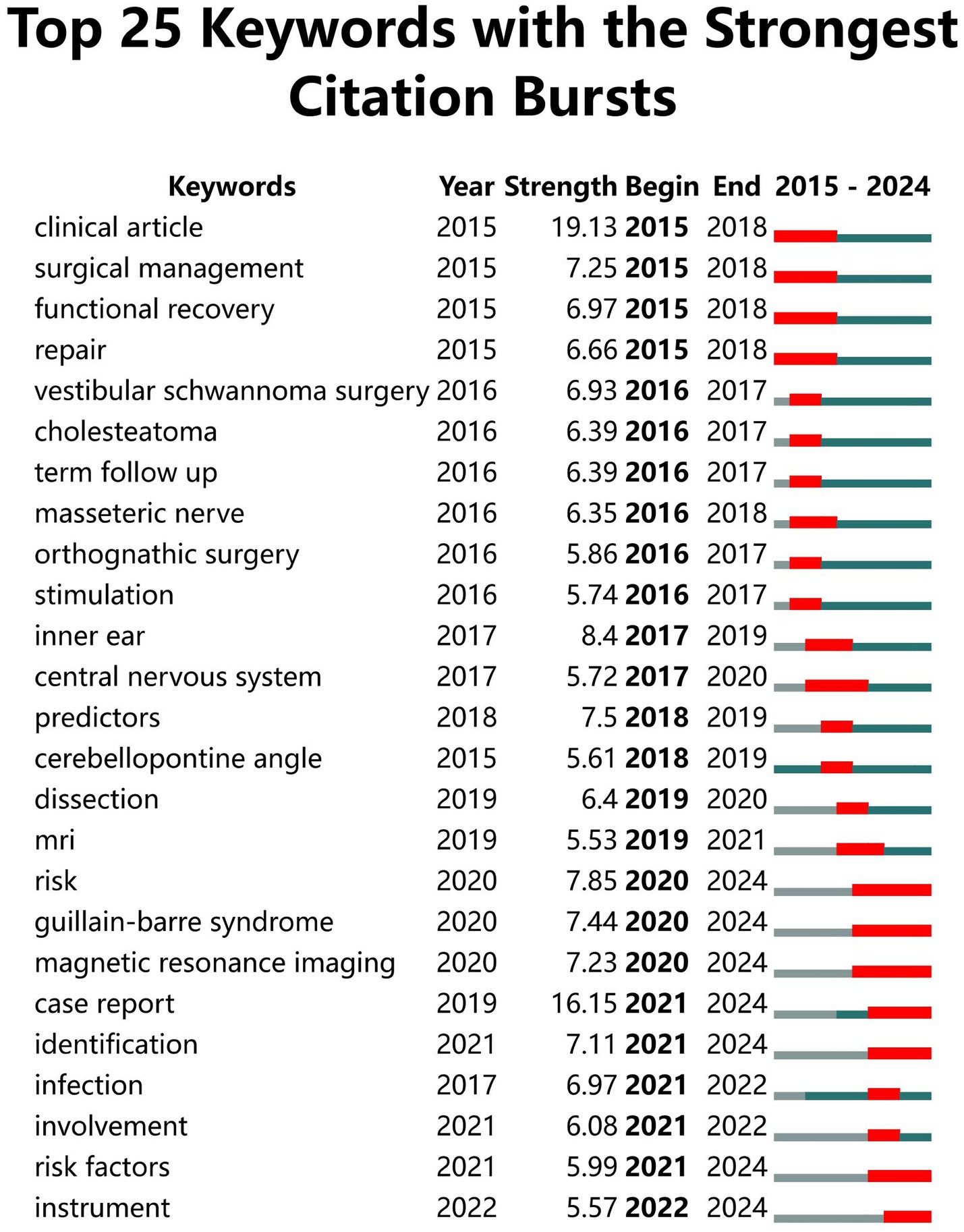
3.5.3 Keyword co-occurrence analysis
CiteSpace uses emerging words to reflect trends in the field (20). There were two breakout terms, “neuroendoscopy” and “treatment outcome,” that persisted to the present when the γ value was set to 1 in Chinese literature. A total of 39 breakout terms appeared, with 7 of the 25 most emergent mutation terms persisting to the present, namely “risk,” “Guillain-Barré syndrome,” “magnetic resonance imaging,” “case report,” “identification,” “risk factors,” and “tools.” Figures 9, 10 present the keyword mutation maps in English and Chinese, respectively.
4 Discussion
4.1 Current status of domestic and international research on facial nerve injury after CPA lesions
The results showed that domestic and international research related to nerve injury after CPA lesion has grown rapidly year by year. The longitudinal development in a specific field is reflected by the number of articles published in different years (21). In this study, the number of English studies showed an upward trend overall, increasing from 436 in 2015 to 593 in 2024. The most obvious increases were in 2019 and 2021, indicating that foreign scholars paid more attention to facial nerve injury after CPA lesions in these 2 years. This is likely due to the increase in the incidence of vestibular schwannoma (22). In addition, with the development of treatment techniques, intraoperative neuroendoscopy (23), electrophysiological monitoring (24), and magnetic imaging technology (25) have improved the identification and management of these lesions, as well as enabled more accurate assessment of facial nerve injury incidence. There has been increasing concern regarding complications, especially facial nerve injury, which is likely the reason for the rapid development and increase in relevant research. Compared with English literature, the number of articles published in Chinese showed a more stable upward trend in 2015–2017. Conversely, there has been a downward trend since 2017, indicating that Chinese research in this field is still in its initial stages.
4.2 Hotspots and frontiers in facial nerve injury after CPA lesions
The results and mediated centrality of high-frequency keywords analyses in domestic and international studies showed that the hotspots focused on the levels of physiological health, clinical efficacy, complications, and management. The emergent terms in national studies included “neuroendoscopy” and “therapeutic outcomes.” Domestic research has paid more attention to improving patients’ physiological health. Risk factors, case reports, early identification, and assessment tools were included in the foreign studies’ emergent words over the last 10 years, indicating that international researchers are more inclined to focus on patients’ health management, preventive measures, and early interventions with the goal of improving patients’ overall health and quality of life. In summary, research on CPA lesion with facial nerve injury is gradually transitioning from a focus on physical health to the management of both the physical and mental health in patients.
4.2.1 Relevant research on assessment tools
The facial nerve is mainly responsible for the movement of facial muscles and some sensory and glandular functions, playing an important role in facial expression, taste, and glandular secretion (26). It is crucial for patients that an appropriate assessment tool be selected to accurately evaluate facial nerve function and extend of damage, which may improve treatment selection and outcomes as well as patient prognosis. The main methods used to assess facial nerve function include the House-Brackmann (H-B) Facial Function Rating Scale (27), Burres-Fisch Facial Nerve Scoring System (28), Sunnybrook Facial Nerve Rating Scale (29), Facial Nerve Function Evaluation System (30), and Quantitative Rating Scale for Facial Palsy Symptoms and Signs and so on (31). All the above scales can be used to easily and quickly assess facial nerve function and recovery in a clinical environment. The H-B Scale can be widely used in the clinic as it allows a rapid assessment and facilitates the comparison of data between different institutions. Despite all these advantages, this scale focuses only on facial muscle movement and does not adequately reflect facial nerve function. The Burres-Fisch Facial Nerve Score encompasses multiple facial movements but is susceptible to user bias. The Sunnybrook Facial Nerve Rating Scale is indicated for evaluating a wide range of facial nerve dysfunctions. The Facial Nerve Function Scoring System includes a statistical and dynamic view, and can be more objective, comprehensive, accurate, and universally applicable than the Sunnybrook System. The Quantitative Facial Palsy Symptoms and Signs Rating Scale, which covers the signs and symptoms of the facial nerve, is more complex than other rating systems and can take longer times and its results are more dependent on the assessor’s experience. With the gradual maturation of artificial intelligence (AI) technology, several AI-based facial nerve function assessment systems have been developed. The eFace, a comprehensive facial function scoring system proposed by American researchers, has been widely used (32). Existing facial nerve function assessment tools primarily focus on the motor function of the facial nerve and pay less attention to sensory and glandular secretory function. Therefore, these tools cannot comprehensively and accurately assess the degree of facial nerve damage in patients. A comprehensive assessment of facial nerve function can be developed and implemented with the help of an AI system when conditions are favorable. Meanwhile, clinical nurses need to closely monitor postoperative facial nerve function in patients with CPA tumors to identify the early occurrence of facial paralysis as a pre-sentinel symptom. This can, in turn, help them carry out functional rehabilitation training through methods such as facial muscle exercises or acupuncture.
4.2.2 Management of postoperative facial paralysis, complications, and related outcomes are an important part of relevant studies
The facial nerve plays a crucial role in various physiological functions, including motor coordination, sensory perception, and parasympathetic control. Additionally, it is more susceptible to irreversible damage or even adverse outcomes, such as facial paralysis, during surgical resection of CPA tumors (26). The consequences of this injury extend beyond the physical realm and into the psychological realm, with patients facing not only a tangible loss of facial activity but also the profound challenge of impaired social expression (33). Therefore, existing studies have shifted from maximizing tumor resection and control to reducing postoperative neurological deficits by introducing intraoperative measures such as electrophysiological monitoring (24) and magnetic resonance imaging (34), especially for the facial and auditory nerves. Zhang et al. (35) used diffusion tensor imaging (DTI) preoperatively to predict the anatomical relationship between the facial nerve and vestibular schwannoma. Moreover, they protected the facial nerve intraoperatively under the guidance of neurophysiological monitoring, which reduced the risk of intraoperative facial nerve injury and improved the preservation of facial nerve function and the patients’ postoperative quality of life. However, 16 to 25% of patients still present with facial paralysis after surgery (14, 36). If patients do not undergo timely rehabilitation during the optimal recovery period following facial paralysis, or fail to regain normal facial nerve function within 12 months, the probability of long-term facial paralysis will remain high (37, 38). In severe cases, facial Synkinesis may emerge. Although there is limited research on how to help patients with facial nerve injuries rehabilitate and promote nerve function recovery. Fortunately, some studies have shown (39) that early rehabilitation can be facilitated by a multidisciplinary team using physical measures such as mirror therapy (40) or virtual reality technology (41) under the guidance of a physical therapist or rehabilitation technician. A quantity of evidences (42–44) suggests that patients with moderate or severe facial injuries exhibit higher levels of social impairment, poorer health ratings, and lower quality of life. This is supported by Keishi Fujiwara et al. (45), whose study showed that the quality of life of nearly half of the facial paralysis patients were severely compromised, particularly in terms of facial comfort and eye comfort. Thus, appropriate referral and systematic follow-up evaluations are essential components of symptom management. However, there are fewer studies on social participation, mental health, and quality of life in facial nerve injury patients in the field of nursing, which have not caused the widespread concern among researchers (8, 46, 47). This suggests that healthcare workers should consider the lower quality of life and poorer mental health of patients while assessing the degree of postoperative facial nerve injury in clinical work and scientific research.
5 Limitations and prospects
This study only searched for relevant literature published in the last 10 years in the CNKI and WanFang databases and Web of Science, and did not include a comprehensive search of domestic and international databases. This may have introduced bias in the reporting of results. The retrieved literature was analyzed only for authors, author institutions, and keywords. Thus, broader research results were not acquired due to the limitations of the CiteSpace software. The results of this study showed that existing studies have focused more on the therapeutic effects of different surgical or therapeutic modalities and on how to protect the facial nerve in the clinical settings. Moreover, most of the studies were predominantly focused on clinical research. The incidence of postoperative facial nerve injury in CPA lesions is high and seriously affects patients’ quality of life and mental health. There is a lack of research on facial nerve injury, particularly in the field of nursing. Moreover, existing research tools are insufficiently comprehensive for assessing facial nerve function. A more comprehensive tool can be developed in the future to identify the cluster of pre-sentinel symptoms, which can help nurses identify and intervene early, promoting the early recovery of facial nerve function. More attention should be paid to the psychological health and functional rehabilitation of patients who develop facial paralysis after CPA surgery. It is necessary to conduct interventional studies at the psychosocial level to explore the patients’ sense of shame and self-esteem, which is likely to help patients better integrate into society.
6 Conclusion
We identified and analyzed studies on facial nerve function related to CPA tumors over the last 10 years by searching Web of Science, as well as the CNKI and WanFang databases, using the CiteSpace 6.3 software. The results showed that existing studies are predominantly focused on clinical research, emphasizing the preservation of intraoperative facial nerve function, with less attention on the psychosocial well-being of patients and functional rehabilitation of their facial nerve in nursing care. In the future, it will be important to focus on managing of patients’ facial nerve function. Simultaneously, the efficiency of early identification and health management can be improved using new technologies such as AI and big data analysis, thereby enhancing the accuracy and effectiveness of assessment tools. Healthcare professionals also need to strengthen patient health education to improve patients participation in their own health management and enhance their understanding and ability to cope with problems.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://pan.baidu.com/s/1s4i1BAbEVc0hVpFVHkaCtw?pwd=erzs.
Author contributions
XL: Visualization, Writing – original draft. BB: Methodology, Supervision, Visualization, Writing – review & editing. BN: Data curation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Zhengzhou University 2023 Education and Teaching Reform Research and Practice Project (2023ZZUJGXM103).
Acknowledgments
I would like to thank Ms. BB for overseeing my whole research process and design. Thank you for your guidance and support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Juan, Z, Chao, Z, and Yumei, Z In: Z Juan, Z Chao, and Z Ym, editors. Effects of different swallowing training modalities on the nursing outcomes of patients with postoperative dysphagia after tumor surgery in the bridge cerebellar horn region : Nursing Research (2020). 580–4.
2. Moussalem, C, Abou-Mrad, Z, El Houcheimy, M, Amine, A, Bsat, S, So, A, et al. Coexisting schwannoma and meningioma simulating a single cerebellopontine angle lesion: Case report and review of the literature. Interdiscip Neurosurg Adv Tech Case Manage. (2021) 25:101169. doi: 10.1016/j.inat.2021.101169
3. Msm, J. Cerebellopontine angle tumors; tumor size and surgical outcome. J Neurol Neurosurg. (2017) 3:46–9. doi: 10.19080/OAJNN.2017.03.555617
4. Rp, V, Yadav, A, Kumar, V, Bk, O, Chandra, A, and Verma, R. Surgical Outcomes and Predictive Factor Analysis for Facial Nerve Preservation in Patients With Cerebellopontine Angle (Cpa) Tumors: A Ten-Year Single Institutional Study. Cureus. (2024) 16:e61756. doi: 10.7759/cureus.61756
5. Grahnke, K, Jr, G, Martin, B, Jp, L, and De, A. Prognostic Indices for Predicting Facial Nerve Outcome following the Resection of Large Acoustic Neuromas. J Neurol Surg Part B-Skull Base. (2017) 78:454–60. doi: 10.1055/s-0037-1604077
6. Sf, A, Terry, C, and Aa, C-G. Surgery for vestibular schwannomas: a systematic review of complications by approach. Neurosurg Focus. (2012) 33:E14. doi: 10.3171/2012.6.FOCUS12163
7. Om, N, Jc, J, Agl, VDM, Rw, K, de Ridder, M, PPG, VB, et al. The impact of vestibular schwannoma and its management on employment. Eur Arch Otorrinolaringol. (2022) 279:2819–26. doi: 10.1007/s00405-021-06977-1
8. Gf, V, Granitzka, T, Kreysa, H, Cm, K, and Guntinas-Lichius, O. Initial severity of motor and non-motor disabilities in patients with facial palsy: an assessment using patient-reported outcome measures. Eur Arch Otorrinolaringol. (2017) 274:45–52. doi: 10.1007/s00405-016-4018-1
9. Pattinson, R, Hm, P, Shorthouse, O, Sa, S, and Bundy, C. Exploring beliefs and distress in patients with facial palsies. Psychol Health Med. (2022) 27:788–802. doi: 10.1080/13548506.2021.1876891
10. Jm, VS, Jf, C, Turnbull, J, Mrzai, T, and Johnson, P. Psychological distress: linking impairment with disability in facial neuromotor disorders. Otolaryngol Head Neck Surg. (1998) 118:790–6. doi: 10.1016/S0194-5998(98)70270-0
11. Saadi, R, Shokri, T, Schaefer, E, Hollenbeak, C, and Jg, L. Depression Rates After Facial Paralysis. Ann Plast Surg. (2019) 83:190–4. doi: 10.1097/SAP.0000000000001908
12. Arslan, F, Mc, G, Binar, M, Aydemir, E, and Durmaz, A. Anxiety, depression, and hopelessness in patients before and after treatment for peripheral facial paralysis. ENT J. (2018) 97:E1–4.
13. Kim, J, Hr, L, Jeong, J, and Ws, L. Features of facial asymmetry following incomplete recovery from facial paralysis. Yonsei Med J. (2010) 51:943–8. doi: 10.3349/ymj.2010.51.6.943
14. Nr, K, Estafanous, M, Itamura, K, Filus, A, Gowrinathan, S, Na, M, et al. Patient Perception of Education, Care Coordination, and Psychological Distress After Developing Facial Paralysis: A Qualitative Study. JAMA Otolaryngol Head Neck Surg. (2023) 149:485–92. doi: 10.1001/jamaoto.2023.0371
15. Rousseau, R. Library science: Forgotten founder of bibliometrics. Nature. (2014) 510:218. doi: 10.1038/510218e
16. Cm, C. CiteSpace Ii: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2006) 57:359–77. doi: 10.1002/asi.20317
17. Goldbrunner, R, Weller, M, Regis, J, Lund-Johansen, M, Stavrinou, P, Reuss, D, et al. Eano guideline on the diagnosis and treatment of vestibular schwannoma. Neuro-Oncology. (2020) 22:31–45. doi: 10.1093/neuonc/noz153
18. Zhang Wj, XL, Luo Tt, WF, Zhao, B, and Xq, L. The etiology of Bell's palsy: a review. J Neurol. (2020) 267:1896–905. doi: 10.1007/s00415-019-09282-4
19. Wj, S, Hf, B, Csj, W, Jl, M, Yiangou, A, Ms, U, et al. Topiramate is more effective than acetazolamide at lowering intracranial pressure. Cephalalgia. (2019) 39:209–18. doi: 10.1177/0333102418776455
20. Chen, C, Hu, Z, Liu, S, and Tseng, H. Emerging trends in regenerative medicine: a scientometric analysis in CiteSpace. Expert Opin Biol Ther. (2012) 12:593–608. doi: 10.1517/14712598.2012.674507
21. Cooper, I. Bibliometrics basics. J Med Libr Assoc. (2015) 103:217–8. doi: 10.3163/1536-5050.103.4.013
22. Jp, M, Br, G, Cm, L, and Ml, C. Prevalence of Sporadic Vestibular Schwannoma: Reconciling Temporal Bone, Radiologic, and Population-based Studies. Otol Neurotol. (2019) 40:384–90. doi: 10.1097/MAO.0000000000002110
23. Yk, B, Yj, N, Gao, D, Qw, Z, Qy, Z, Jj, T, et al. Endoscope-Assisted Retrosigmoid Approach for Vestibular Schwannomas With Intracanalicular Extensions: Facial Nerve Outcomes. Front Oncol. (2022) 11:11. doi: 10.3389/fonc.2021.774462
24. Kang, D, Hong, J, and Rui, Y. Meta-analysis of the role of neurophysiological monitoring in the functional protection of the facial nerve during acoustic neuroma surgery. Nerve Injury Func Recons. (2020) 15:315–9.25. doi: 10.16780/j.cnki.sjssgncj.20190892
25. Ashour, R, Reintjes, S, Ms, P, Sivakanthan, S, van Loveren, H, and Agazzi, S. Intraoperative Magnetic Resonance Imaging in Skull Base Surgery: A Review of 71 Consecutive Cases. World Neurosurg. (2016) 93:183–90. doi: 10.1016/j.wneu.2016.06.045
26. Lou Jw, YH, and Fy, W. A Review on Automated Facial Nerve Function Assessment From Visual Face Capture. IEEE Trans Neural Syst Rehabil Eng. (2020) 28:488–97. doi: 10.1109/TNSRE.2019.2961244
27. Jw, H, and De, B. Facial nerve grading system. Otolaryngol Head Neck Surg. (1985) 93:146–7. doi: 10.1177/019459988509300202
28. Burres, S, and Fisch, U. The Comparison Of Facial Grading Systems. Arch Otolaryngol Head Neck Surg. (1986) 112:755–8.
29. Bg, R, Fradet, G, and Jm, N. Development of a sensitive clinical facial grading system. Otolaryngol Head Neck Surg. (1996) 114:380–6. doi: 10.1016/S0194-59989670206-1
30. Peilian, Sheng. Clinical study of acupuncture combined with thunder fire moxibustion at Shenque acupoint in the treatment of intractable facial paralysis with anxiety state (2021).
31. He, Guan-Heng. Clinical study on the treatment of postoperative facial paralysis after acoustic neuroma by Tongdu Huayu Acupuncture Formula [PhD] (2021).
32. Ca, B, Pk, B, Park, J, Cr, H, and Ta, H. Clinician-Graded Electronic Facial Paralysis Assessment: The eface. Plast Reconstr Surg. (2015) 136:223e–30e. doi: 10.1097/PRS.0000000000001447
33. Mat, I, Mrt, N, Cp, C, Pr, DS, Ci, C, Jm, M, et al. Effectiveness of Hypoglossal-Facial Anastomosis in the Rehabilitation of Facial Paralysis Following Vestibular Schwannoma Surgery: A Systematic Review. Cureus J Med Sci. (2024) 16. doi: 10.7759/cureus.57625
34. Gupta, S, Sa, S, Sinha, U, and Gupta, G. Multimodal Intraoperative Neurophysiological Monitoring in Cranial and Spinal Tumour Surgeries: A Descriptive Observational Study. Cureus. (2023) 15:e49411. doi: 10.7759/cureus.49411
35. Zhang, Y, Ge, H, Xu, M, and Mei, W. Significance of Preoperative Nerve Reconstruction Using Diffusion Tensor Imaging Tractography for Facial Nerve Protection in Vestibular Schwannoma. J Korean Neurosurg Soc. (2023) 66:183–9. doi: 10.3340/jkns.2022.0134
36. Gs, J, Gr, M, Gs, F, Tds, R, and Ramina, R. Facial Nerve Adherence in Vestibular Schwannomas: Classification and Radiological Predictors. J Neurol Surg B Skull Base. (2021) 82:456–60. doi: 10.1055/s-0040-1713103
37. Ma, M, Hendricks, B, Ce, S, Rf, S, Kk, A, and Rw, P. Long-Term Facial Nerve Outcomes after Microsurgical Resection of Vestibular Schwannomas in Patients with Preoperative Facial Nerve Palsy. J Neurol Surgery Part B-Skull Base. (2018) 79:309–13. doi: 10.1055/s-0037-1607320
38. Fei, N, Fei, GF, Bingbing, K, Butterfly, X, Fang, L, and Hongying, P. Correlation analysis of facial paralysis recovery after acoustic neuroma surgery. Chinese J Otol. (2020) 18:287–90. doi: 10.3969/j.issn.1672-2922.2020.02.012
39. Jin, K. Prevention and Treatment of Post-Paralytic Synkinesis: Critical Changes Following Severe Facial Palsy. J Electrodiag Neuromus Dis. (2024) 26:19–24. doi: 10.18214/jend.2024.00038
40. Castaldo, M, Sellitto, G, Ruotolo, I, Berardi, A, and Galeoto, G. The Use of Mirror Therapy in Peripheral Seventh Nerve Palsy: A Systematic Review. Brain Sci. (2024) 14:530–545. doi: 10.3390/brainsci14060530
41. Dl, S, Teixeira, S, Ac, DO, Ldb, L, Moreira, R, Silva, F, et al. Computer-Based Gamified Tools for Facial Rehabilitation: A Scoping Review. Games Health J. (2025) 14:11–20. doi: 10.1089/g4h.2023.0220
42. Tavares-Brito, J, Mm, VV, Jr, D, Bahmad, F Jr, and Ta, H. Facial Palsy-Specific Quality of Life in 920 Patients: Correlation With Clinician-Graded Severity and Predicting Factors. Laryngoscope. (2019) 129:100–4. doi: 10.1002/lary.27481
43. Pouwels, S, Sanches, EE, Chaiet, SR, De Jongh, FW, CHG, B, Monstrey, SJ, et al. Association between duration of peripheral facial palsy, severity, and age of the patient, and psychological distress. J Plast Reconstr Aesthet Surg. (2021) 74:3048–54. doi: 10.1016/j.bjps.2021.03.092
44. Lyford-Pike, S, and Nellis, JC. Perceptions of Patients with Facial Paralysis: Predicting Social Implications and Setting Goals. Facial Plast Surg Clin North Am. (2021) 29:369–74. doi: 10.1016/j.fsc.2021.03.008
45. Fujiwara, K, Morita, S, Fukuda, A, Hoshino, K, Kobayashi, M, Nakamaru, Y, et al. Evaluation of quality of life for patients with resolved facial nerve palsy. Auris Nasus Larynx. (2024) 51:456–9. doi: 10.1016/j.anl.2024.02.002
46. Hamlets, C, Williamson, H, Hotton, M, and Rumsey, N. Your face freezes and so does your life': A qualitative exploration of adults' psychosocial experiences of living with acquired facial palsy. Br J Health Psychol. (2021) 26:977–94. doi: 10.1111/bjhp.12515
Keywords: cerebellopontine angle, tumor, facial nerve, CiteSpace, bibliometric analysis, research trend
Citation: Li X, Bai B and Nie B (2025) Research trends of facial nerve injury after cerebellopontine angle tumor: CiteSpace-based bibliometric analysis. Front. Neurol. 16:1525669. doi: 10.3389/fneur.2025.1525669
Edited by:
Hans Thomeer, Utrecht University, NetherlandsReviewed by:
Essam Mohamed Elmatbouly Saber, Benha University, EgyptJacopo Falco, IRCCS Carlo Besta Neurological Institute Foundation, Italy
Dekun Gao, Shanghai Jiao Tong University, China
Copyright © 2025 Li, Bai and Nie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Bai, YmVsYWJpbmdAMTYzLmNvbQ==
 Xinxin Li
Xinxin Li Bing Bai*
Bing Bai*