- 1Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China
- 2Beijing University of Chinese Medicine, Beijing, China
Background: Post-stroke thalamic pain (PS-TP), a common form of central pain, is characterized by hyperalgesia and abnormal sensations in the contralateral affected area. Acupuncture treatment has shown increasing promise in treating PS-TP in recent years. This systematic review and meta-analysis aimed to evaluate the efficacy and safety of acupuncture treatment for PS-TP.
Methods: According to the established search strategy, randomized controlled trials (RCTs) of acupuncture therapy for PS-TP were retrieved from eight Chinese and English databases as well as two clinical trial registration platforms, up to February 2024. Outcome measures included the total efficacy rate, visual analogue scale (VAS), present pain intensity score (PPI), pain rating index (PRI), β-endorphin (β-EP), substance P (SP) and adverse reactions. Sensitivity analysis and subgroup analysis were conducted to identify the sources of heterogeneity. We evaluated the evidence quality of outcomes via the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) rating system and performed trial sequential analyses using TSA software.
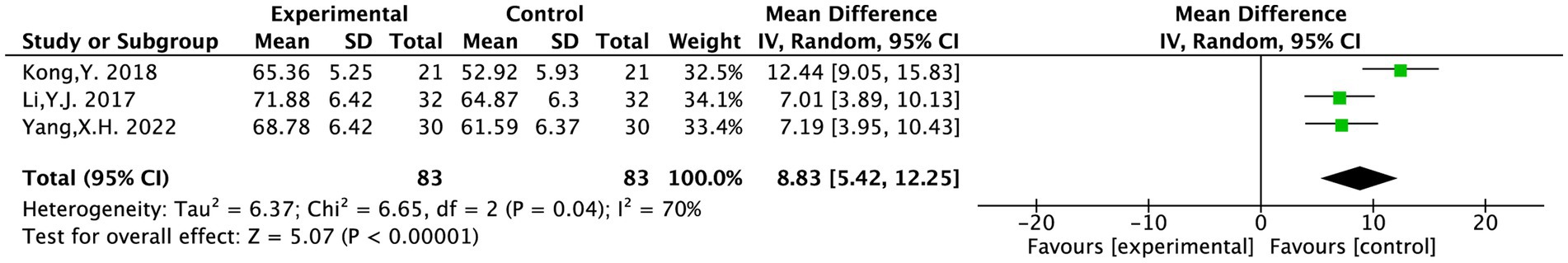
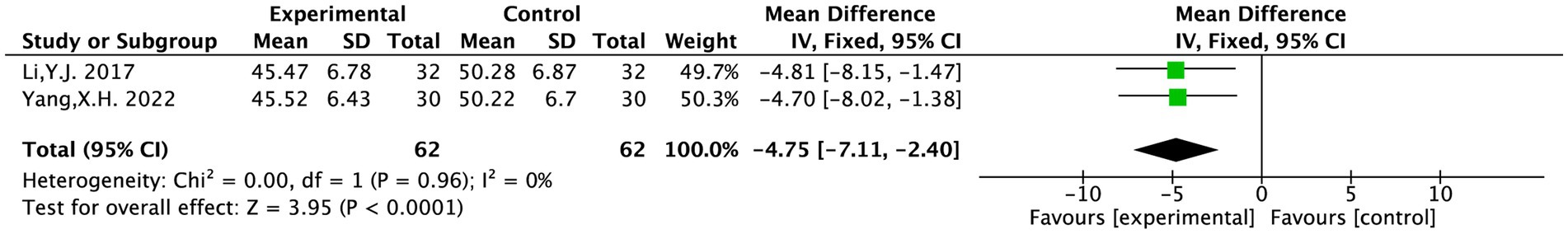
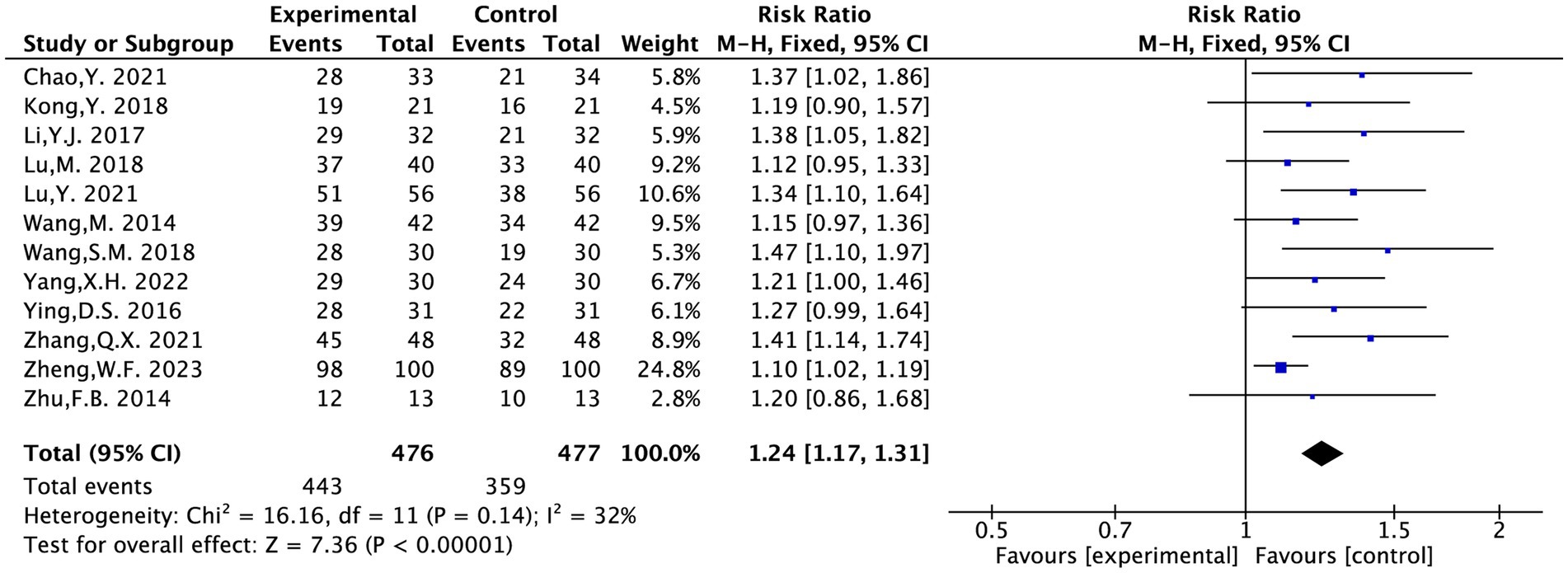
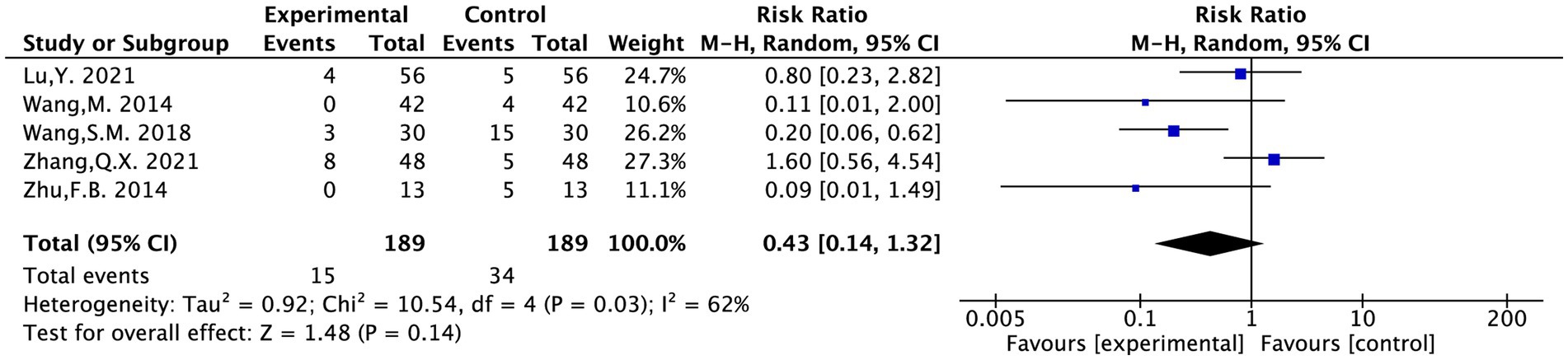
Results: The final inclusion comprised 12 articles, which involved 953 patients. Meta-analysis results indicated that acupuncture treatment for PS-TP was more effective than conventional medical treatment in reducing VAS scores [MD = −1.11, 95% CI (−1.33, −0.88), p = 0.002], PPI scores [MD = −0.65, 95% CI (−1.13, −0.16), p = 0.009], and PRI scores [MD = −1.02, 95% CI (−1.41, −0.63), p < 0.00001]. Additionally, acupuncture treatment for PS-TP was superior to the conventional medical treatment in increasing plasma β-EP levels [MD = 8.83, 95% CI (5.42, 12.25), p < 0.00001], and reducing SP levels [MD = −4.75, 95% CI (−7.11, −2.40), p < 0.0001]. Regarding the total efficacy rate, acupuncture treatment was superior to the conventional medical treatment in treating PS-TP [RR = 1.24, 95% CI (1.17, 1.31), p < 0.00001]. The incidence of adverse events was lower in acupuncture treatment than in conventional medical treatment [RR = 0.43, 95% CI (0.14, 1.32), p = 0.03]. The GRADE assessment indicated that the quality of evidence for all outcome measures ranged from moderate to very low. Trial sequential analysis (TSA) results provided compelling evidence for the efficacy of acupuncture in treating PS-TP.
Conclusion: Acupuncture treatment emerges as a potentially efficacious and safe treatment option for PS-TP. In the future, more large-sample, high-quality RCTs are needed to provide primarily high-level evidence in evidence-based medicine regarding the safety and sustained effects of acupuncture treatment for PS-TP.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024498698, identifier CRD42024498698.
1 Introduction
Post-stroke thalamic pain (PS-TP), a common form of central pain, is characterized by hyperalgesia and abnormal sensations in the contralateral affected area. In many patients, this pain tends to progressively worsen, significantly affecting their quality of life and psychological well-being (1). Modern medicine recognizes that pain, along with the anxiety and depression it induced, constitutes a cycle of negative emotions that can intensify the perception of pain (2). In some cases, these psychological states may further aggravate the pain. The pathogenesis of PS-TP involves spinothalamic tract dysfunction and neuroinflammatory cascades. Central sensitization arises from loss of inhibitory regulation in the lateral tract and hyperexcitability in the medial tract, driven by compensatory neural hyperactivity post-stroke (3). Neuroglial remodeling further exacerbates pain through microglial activation, which releases signaling molecules (e.g., SDF1, ITC) to trigger cytokine cascades and pro-inflammatory mediators (IL-1β, IL-6β), disrupting central pain modulation and sustaining nociception (4).
Despite these advances in understanding its pathophysiology, there are currently few effective medications available that directly target the underlying causes of PS-TP. Some domestic and international treatment guidelines recommend antidepressants, antiepileptic drugs, opioid analgesics, and other medications to alleviate symptoms. Non-pharmacological interventions, such as repetitive transcranial magnetic stimulation, electrical stimulation, and deep brain stimulation, are also suggested (5). However, these approaches often fall short in efficacy and fail to achieve the desired therapeutic outcomes (6).
In contrast to these conventional approaches, traditional Chinese medicine (TCM) has shown increasing promise in treating PS-TP in recent years. Multiple clinical trials have validated that TCM, particularly acupuncture, offers more significant therapeutic effects and higher safety than conventional drugs and non-pharmacological interventions (7–9). Acupuncture, a cornerstone of TCM, is valued for its ability to address multiple symptoms, targets, and mechanisms. Beyond pain modulation, TCM also posits that acupuncture can help regulate emotions and alleviate the negative psychological states associated with PS-TP.
Despite accumulating empirical support, existing evidence remains fragmented due to small sample sizes, heterogeneous methodologies, and insufficient attention to long-term efficacy. Moreover, existing systematic reviews have not adequately assessed the methodological quality of evidence and robustness of the findings. To address this gap, we conducted this study to systematically evaluate the efficacy and safety of acupuncture therapy compared to conventional medical treatment for PS-TP. The aim of the study was to generate evidence-based recommendations and inform future clinical guideline development for PS-TP management.
2 Subject/materials and methods
2.1 Method
The PROSPERO International Prospective Register of Systematic Reviews had an agreement for this meta-analysis registered under registration number CRD42024498698. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards were adhered to in the preparation of the report (10).
2.1.1 Search strategy
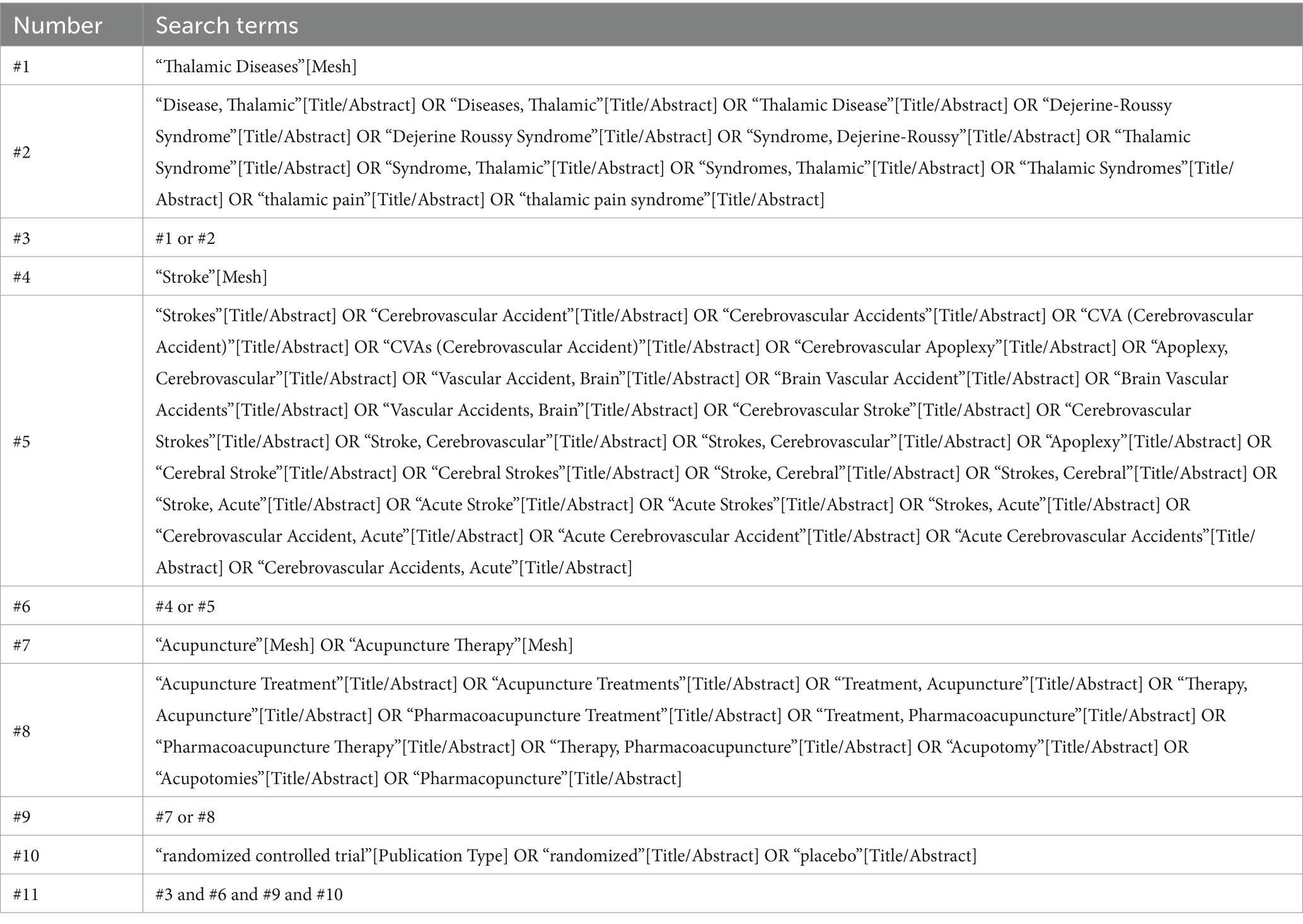
In addition to two clinical trial registries, ClinicalTrials.gov and the Chinese Clinical Trial Registry, we also searched eight English and Chinese databases: PubMed, MEDLINE (via Embase), Cochrane Library, Embase, China National Knowledge Infrastructure (CNKI), China Biomedical Literature Database (CBM), VIP Database, and Wanfang Data. This search covered randomized controlled trials (RCTs) published from the inception of these databases up to February 2024. Different combinations of Medical Subject Headings (MeSH) and non-MeSH phrases were used in the search, including “thalamic Diseases,” “thalamic pain,” “thalami syndromes,” “stroke,” “cerebrovascular accident,” “acupuncture,” “acupuncture therapy,” “pharmacopuncture,” “pharmacoacupuncture,” “acupuncture treatment,” “randomized” and “randomized controlled trial.” No restrictions were placed on language, study population, or country. Table 1 provides specific search technique details.
2.1.2 Inclusion criteria
(1) All RCTs published in Chinese or English that had an eligible intervention and/or outcome for PS-TP were included. The included RCTs should adhere carefully to the randomization principle; nevertheless, there were no stringent restrictions because blinding and placebo control in acupuncture therapy are challenging to adhere to.
(2) The subjects that were included had to fulfill the PS-TP diagnostic requirements.
(3) Acupuncture was administered to the experimental groups either in addition to or instead of medication, and pharmaceuticals were used as the control group. Body acupuncture, scalp acupuncture, plum-blossom acupuncture, three-edged acupuncture, electro-acupuncture, wrist-ankle acupuncture were all included.
(4) Outcome indicators: At least one obvious indicator such as the total efficacy rate, visual analogue scale (VAS), present pain intensity score (PPI), pain rating index (PRI), β-endorphin (β-EP), substance P (SP) and adverse reactions was included.
2.1.3 Exclusion criteria
(1) Studies that did not account for the type of study.
(2) Research that used non-drug treatment in the control group or non-acupuncture treatment in the treatment group were rejected.
(3) Studies were excluded if repeated attempts to contact the authors failed to retrieve the full text or accessible data.
(4) Repeated publications.
2.2 Studies selection process
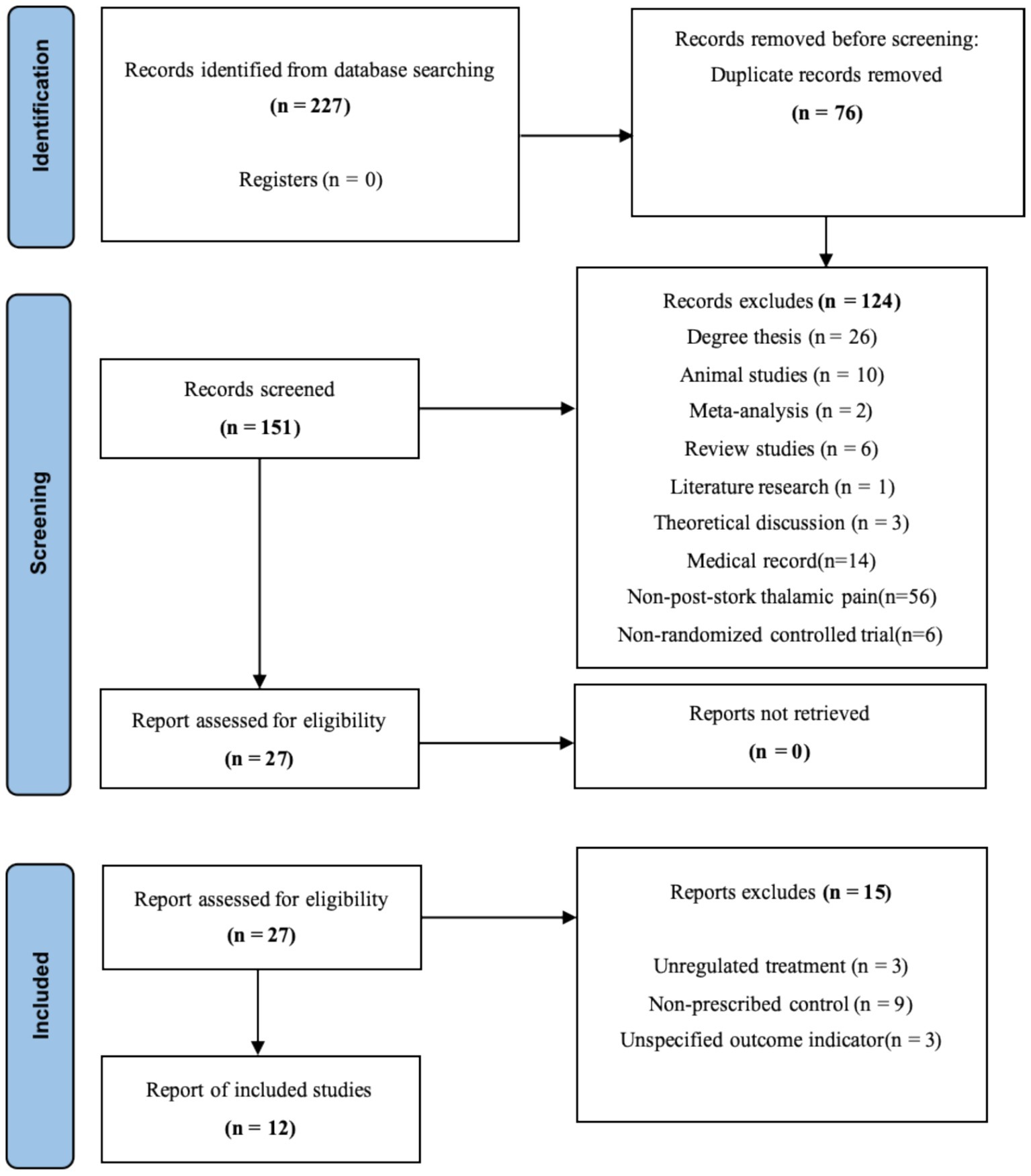
Figure 1 illustrates the selection procedure for research. First, duplicate articles were eliminated from the obtained literature by using EndNote X9 was automatic review feature. Second, unidentified duplicates, such as reports on different facets of the same research as well as duplicates from several journals and multilingual publications, were sorted out by two independent investigators (TZ and LC). After that, these two researchers looked through the article titles and abstracts to choose relevant research studies according to the kind of study, the interventions/comparators, and the results. Thirdly, two investigators (TZ and LC) conducted a full-text assessment in order to omit publications based on the specified exclusion criteria. Any disagreements were settled by consensus or after speaking with DXL, a third investigator.
2.3 Risk of bias assessment
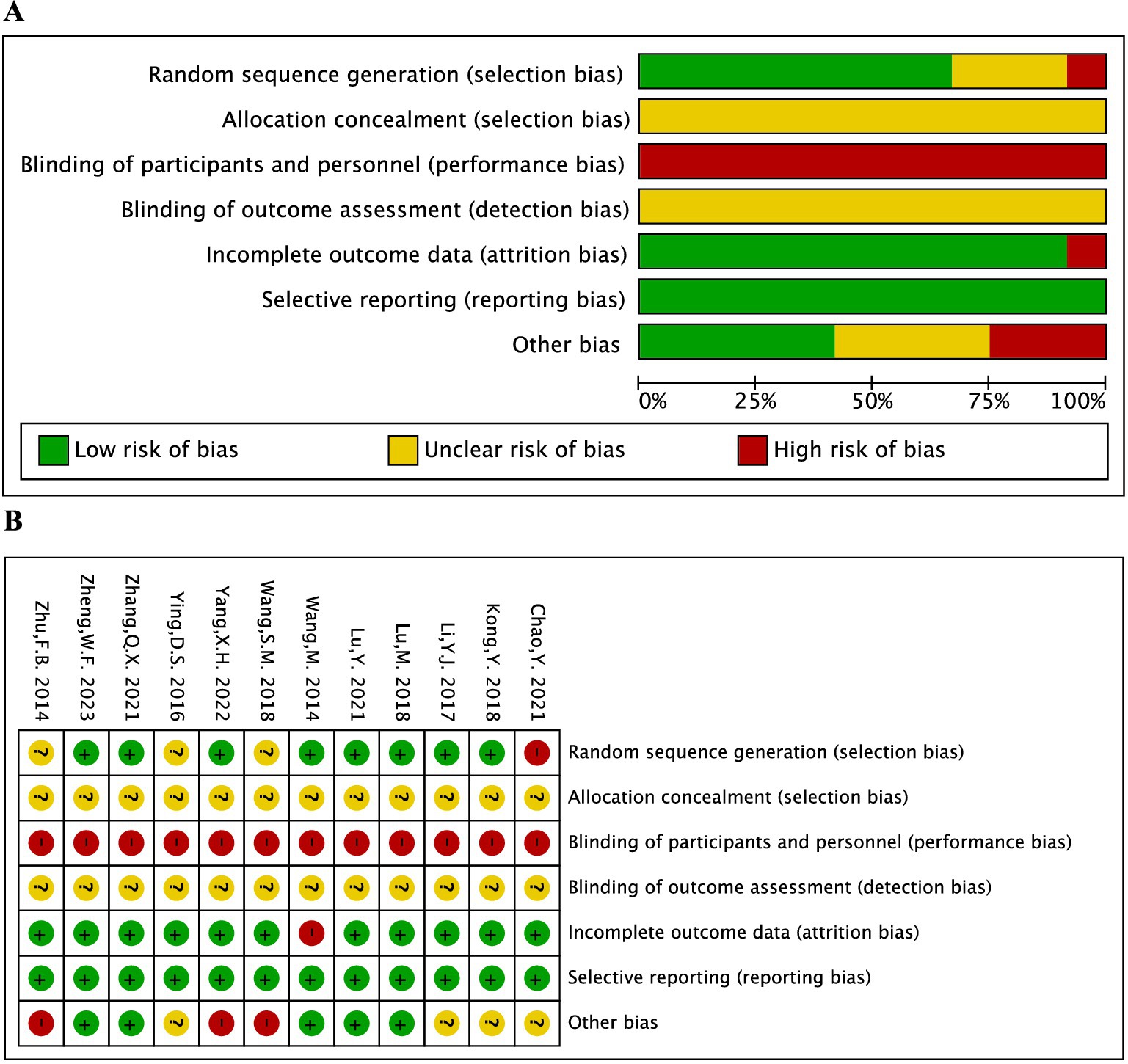
The Cochrane scoring system was used to gauge the methodological quality of trials that satisfied eligibility criteria (11). Based on seven criteria, including random sequence generation methodology, treatment allocation concealment, participant, healthcare provider, data collector, outcome assessor, and data analyst blinding, infrequently missing outcome data, and absence of selective outcome reporting, each included study was assessed by two independent researchers (TZ and KJ). One of the three categories—low risk, high risk, or unclear risk of bias—was assigned to the evaluation. After the study assessment was cross-checked, a third investigator (XD) determined any disagreements with the protocols.
2.4 Data extraction
Two researchers (KJ and JZ) independently retrieved data from studies that qualified. Data about the study (authors, publication year, design, follow-up period, etc.); participant characteristics (age, gender, duration, diagnosis, etc.); intervention/control method (number of treatments, frequency, etc.); and outcomes (types of primary and secondary outcome measures, the total efficacy rate, mean and standard deviation (SD) of VAS scores, PPI scores, PRI scores, adverse event, etc.) were all entered into an electronic data-extraction form.
2.5 Data synthesis and statistical analysis
We conducted all analyses using Review Manager (version 5.4), Stata (version 14.0), and TSA 0.9.5.10 Beta. Specifically, meta-analyses were performed with Review Manager, trial sequential analyses were conducted using TSA software, and publication bias was assessed through Stata. Heterogeneity was investigated in the involved publications. A fixed-effects model was employed when p ≥ 0.05 or I2 < 50% indicated that the heterogeneity among the studies was deemed to be minimal; however, when p < 0.05 or I2 ≥ 50% suggested that there was heterogeneity between studies, a random-effects model was employed. When appropriate, sensitivity analyses could be performed to examine the sources of heterogeneity. For the measurement data, the relative risk (RR) was utilized, and for the count data, the mean difference (MD). There was a 95% confidence interval (CI) attached to both. The difference was statistically significant when p ≤ 0.05. The quality of evidence was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) rating system approach. The evidence quality was categorized into four levels: high, moderate, low, and very low. Two reviewers (TZ and HS) independently assessed the certainty of evidence using GRADE criteria. Discrepancies were resolved by consensus.
3 Results
3.1 Study selection
Initial database searching identified 227 distinct records, as seen in Figure 1. Seventy-six of these studies were disqualified for being duplicated. The following criteria led to the exclusion of an additional 139 studies: degree thesis (n = 26), animal studies (n = 10), meta-analyses (n = 2), review studies (n = 6), literature research (n = 1), theoretical discussions (n = 3), medical records (n = 14), non-PS-TP (n = 56), non-RCTs (n = 6), unregulated treatments (n = 3), non-prescribed controls (n = 9), and unspecified outcome indicators (n = 3). Ultimately, 12 studies were included in the analysis.
3.2 Characteristics of the included studies
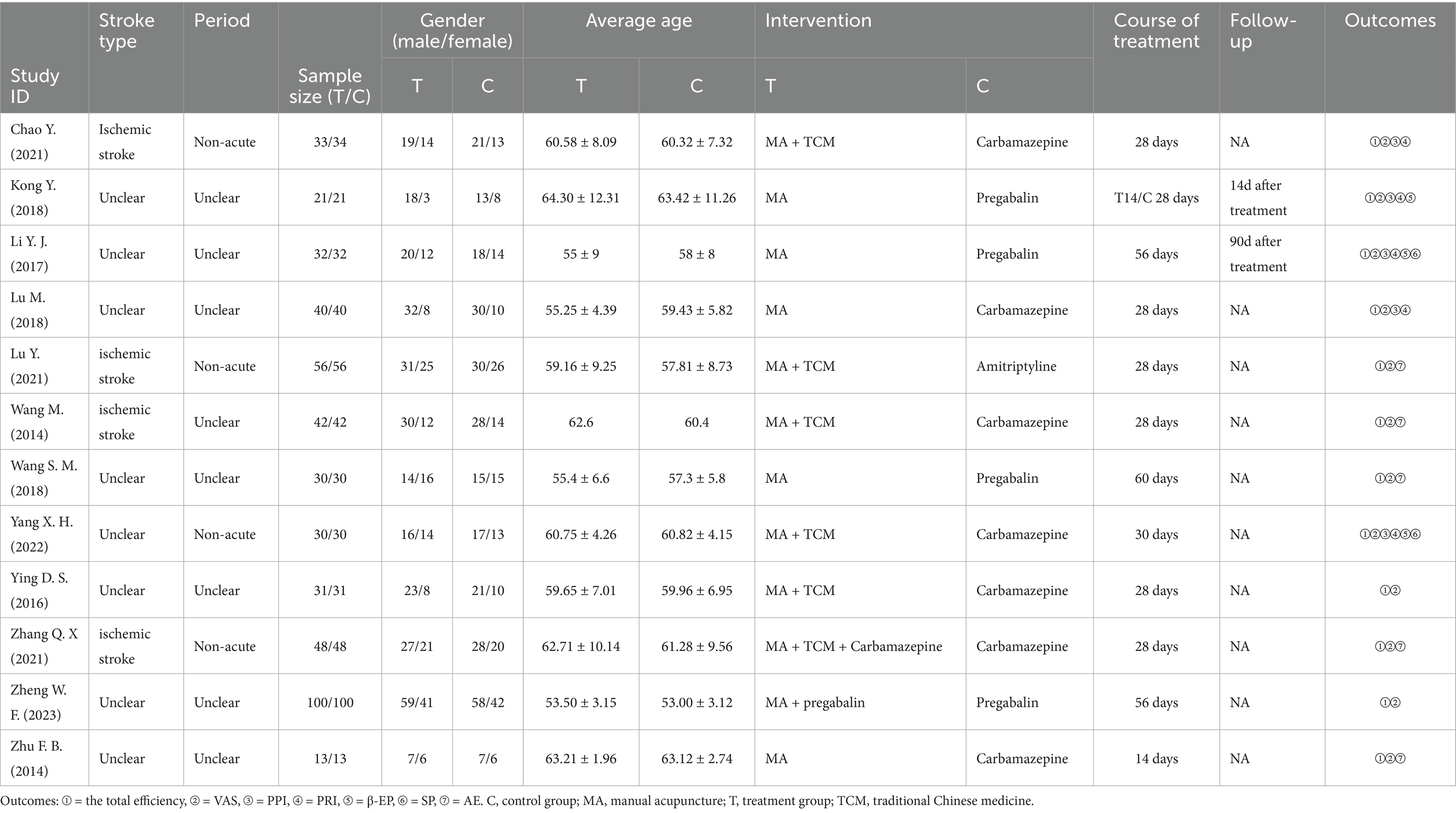
The characteristics of the 12 included studies (12–23) with 953 subjects are detailed in Table 2. All studies were conducted in China and published between 2014 and 2023. Sample sizes ranged from 26 to 200, with treatment duration varying from 14 to 60 days. All participants were diagnosed with PS-TP. Four studies included patients with ischemic stroke, while eight studies did not specify the stroke type, encompassing both ischemic and hemorrhagic strokes. Four studies included period with non-acute, while eight studies did not specify the period. Gender and average age data showed no statistically significant differences, ensuring comparability. Of the included studies, five compared manual acupuncture (MA) to Western medicine (WM), five compared MA plus TCM with WM, one compared MA plus WM with WM, and one compared MA plus TCM plus WM with WM. The most frequently used MA was Xingnao Kaiqiao acupuncture, and the most common WM was Carbamazepine. The 12 studies provided data on 12 comparisons for the total efficacy rate, 12 comparisons for VAS, five comparisons for PPI and PRI, three comparisons for β-EP, two comparisons for SP, two comparisons for aftereffects, and five comparisons for adverse event rates.
3.3 Risk of bias
The risk of bias evaluation for each study is shown in Figure 2. The results indicated that only one study, which used incorrect methods for random sequence generation, was identified as high risk. Additionally, three studies did not specify the randomization methods. None of the 12 studies reported allocation concealment or blinded participants, personnel, or outcome assessors. One study had 12 participants lost to follow-up or excluded, while the remaining 11 studies had complete data. All 12 studies provided detailed reports on all outcome indicators. Three studies had only one author each, and four did not adequately describe other potential risk factors.
3.4 Meta-analysis results
3.4.1 VAS
The VAS score was evaluated in 12 included studies and covered 953 patients (12–23). Following heterogeneity testing (I2 = 63%, p = 0.002), it suggested statistically significant heterogeneity among the selected literature in this study, requiring exploration of heterogeneity (Figure 3A).
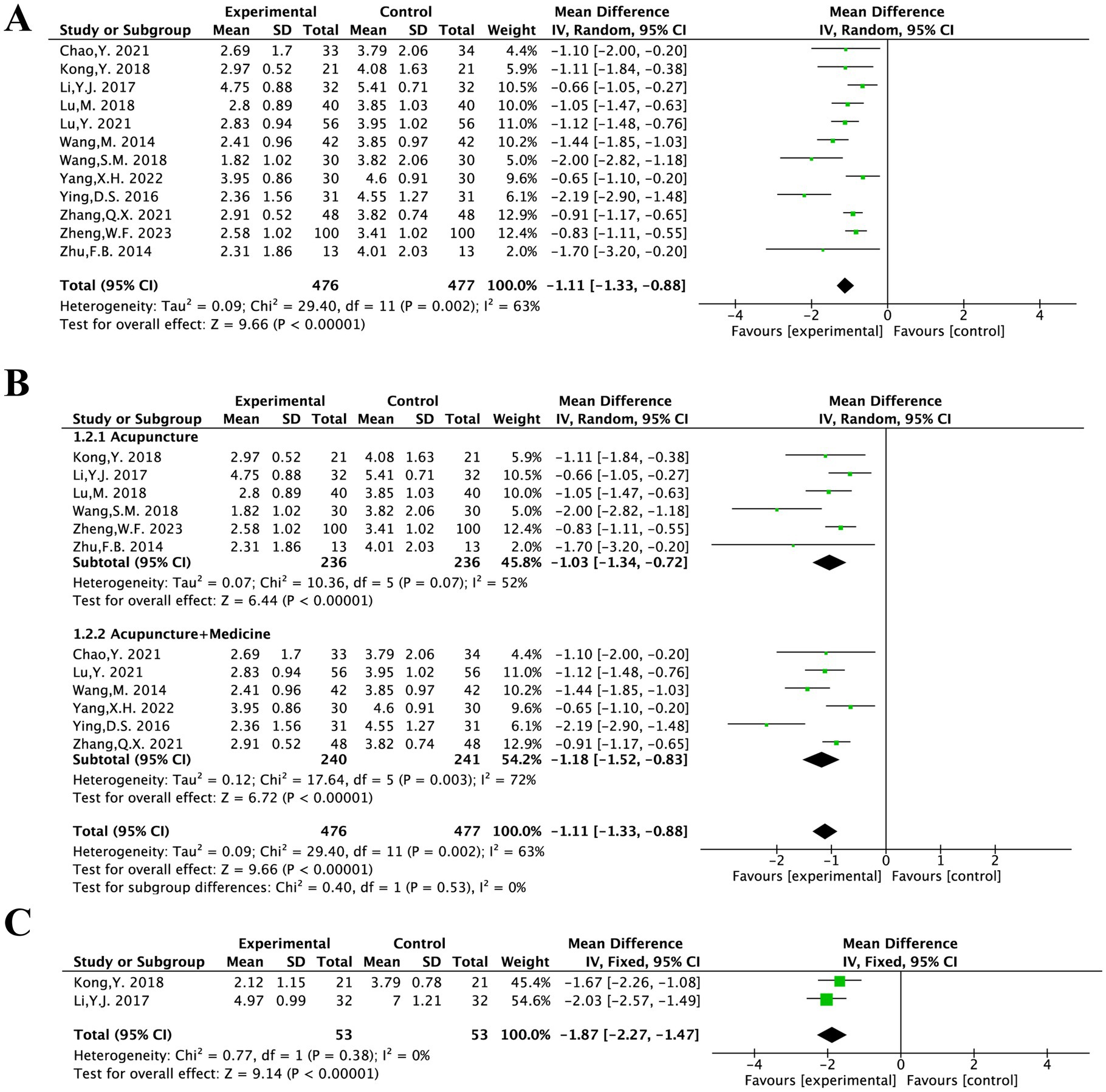
Figure 3. The forest plot of the VAS score (A) based on the difference in intervention methods (B) and aftereffect (C).
Sensitivity analysis to find sources of heterogeneity: In the sensitivity analysis of the 12 included studies, it was found that the survey by Ying D. S. 2016 had a significant impact on heterogeneity (13). This study was a single-centre RCT and the findings may be attributed to the relatively significant efficacy observed in the study combined with its small sample size. Therefore, a random-effects model was employed for the meta-analysis of 12 studies.
This finding suggested that acupuncture treatment for PS-TP reduces VAS scores more effectively than the conventional medical treatment [MD = −1.11, 95% CI (−1.33, −0.88), p = 0.002].
Based on the intervention methods, the 12 articles were categorized into “MA” and “MA + TCM” groups for subgroup analysis.
Heterogeneity testing was performed on the MA group; results showed that there was significant and statistically meaningful heterogeneity among the included studies (I2 = 52%, p = 0.07). A random-effects model was therefore used. It was statistically significant [MD = −1.03, 95% CI (−1.34, −0.72), p < 0.00001] and showed that acupuncture treatment was more effective than the conventional medical treatment in improving VAS scores for PS-TP.
The MA + TCM group was heterogeneity testing (I2 = 72%, p = 0.003), indicating a large degree of statistically significant heterogeneity among the chosen studies. Differences in the kinds of Chinese herbal formulations utilized in addition to acupuncture could be the cause of the notable variation. A random-effects model was therefore used. The results showed that acupuncture in conjunction with TCM was more effective than the conventional medical treatment in improving VAS scores for PS-TP. It was statistically significant [MD = −1.18, 95% CI (−1.52, −0.83), p < 0.00001] (Figure 3B).
Two literatures included in this study conducted aftereffect evaluations of VAS (14, 17). There was no substantial heterogeneity among the chosen literatures, according to the results of the heterogeneity test (I2 = 0%, p = 0.38). For meta-analysis, a fixed-effects model could therefore be applied.
This difference was statistically significant, suggesting that acupuncture treatment was more effective than the conventional medical treatment in reducing VAS scores aftereffect for PS-TP [MD = −1.87, 95% CI (−2.27, −1.47), p < 0.00001] (Figure 3C).
3.4.2 PPI
The PPI was evaluated in five included studies and covered 313 patients (14, 15, 17, 20, 21). After heterogeneity testing (I2 = 95%, p < 0.00001), showing a considerable degree of heterogeneity in the chosen literature. Thus, for the meta-analysis, a random-effects model was employed.
It was statistically significant, suggesting that acupuncture treatment was more effective than the conventional medical treatment in reducing PPI scores for PS-TP [MD = −0.65, 95% CI (−1.13, −0.16), p = 0.009] (Figure 4A).
Two studies included in this study conducted aftereffect evaluations of PPI (14, 17). There was no substantial heterogeneity among the chosen literature, according to the results of the heterogeneity test (I2 = 0%, p = 0.76). For meta-analysis, a fixed-effects model could therefore be applied.
It was statistically significant, suggesting that acupuncture treatment was more effective than the conventional medical treatment in reducing PPI scores for PS-TP [MD = −1.19, 95% CI (−1.48, −0.91), p < 0.00001] (Figure 4B).
3.4.3 PRI
The PRI was evaluated in five included studies and covered 953 patients (14, 15, 17, 20, 21). The heterogeneity testing (I2 = 76%, p = 0.002) showed a considerable degree of heterogeneity in the chosen literature. Based on the intervention methods, the five articles were categorized into “MA” and “MA + TCM” groups for subgroup analysis.
The MA group was tested for heterogeneity (I2 = 0%, p = 0.39) showing no significant heterogeneity among the included studies. It was statistically significant [MD = −1.02, 95% CI (−1.41, −0.63), p < 0.00001]. The MA + TCM group showed significant heterogeneity (I2 = 91%, p = 0.0006). Analysis results indicated that acupuncture therapy for PS-TP was superior to the conventional medical treatment in reducing PRI scores (Figure 5).
Two articles evaluated PRI for aftereffect (14, 17). The heterogeneity testing (I2 = 98%, p < 0.00001) showed a considerable degree of heterogeneity in the chosen literature and considered that the acupuncture frequency and duration were different in the two studies: twice daily for 2 weeks and 6 days per week for 8 weeks. The high heterogeneity might be attributable to the differing frequencies and durations. Given the non-overlapping confidence intervals between the two studies and substantial heterogeneity (I2 > 75%), a meta-analysis was deemed inappropriate. The results of each study were therefore presented separately with a narrative synthesis.
The MD of Li Y. J. 2017 was −4.66 with a 95% CI of (−5.29, −4.03). The MD of Kong Y. 2018 was −1.54 with a 95% CI of (−1.98, −1.10). Both studies suggested that acupuncture was superior to standard pharmacotherapy in alleviating PS-TP. Both studies reported that acupuncture treatment was more effective than the conventional medical treatment in reducing PRI scores for PS-TP.
3.4.4 β-EP
The β-EP was evaluated in three included studies and covered 166 patients (14, 17, 21). Following heterogeneity testing (I2 = 70%, p = 0.04), it indicated that there was statistically significant variation in the chosen literature. For the meta-analysis, a random-effects model was thus selected.
The findings suggested that acupuncture treatment for PS-TP was superior to the conventional medical treatment in increasing plasma β-EP levels [MD = 8.83, 95% CI (5.42, 12.25), p < 0.00001] (Figure 6).
3.4.5 SP
The SP was evaluated in two included studies and covered 124 patients (14, 21). The heterogeneity testing (I2 = 0%, p = 0.96) showed no significant heterogeneity among the included studies. Therefore, a fixed-effects model could be used for meta-analysis.
The results implied that the conventional medical treatment’s SP levels were not as effectively reduced by acupuncture treatment [MD = −4.75, 95% CI (−7.11, −2.40), p < 0.0001] (Figure 7).
3.4.6 The total efficacy rate
The 12 articles included in this study underwent testing for heterogeneity (I2 = 32%, p = 0.14). It suggested that there was no statistically significant heterogeneity across the chosen literature. Thus, a fixed-effects model was chosen for the meta-analysis.
The result indicated that acupuncture was superior to the conventional medical treatment in treating PS-TP [RR = 1.24, 95% CI (1.17, 1.31), p < 0.00001] (Figure 8).
3.4.7 Safety evaluation
The rate of AE was evaluated in five included studies and covered 378 patients (12, 16, 18, 19, 23). Following heterogeneity testing (I2 = 62%, p = 0.03), it indicated statistically significant heterogeneity between the chosen literature in this study, requiring exploration of heterogeneity.
Sensitivity analysis to locate sources of heterogeneity: In a sensitivity analysis of the five included studies, Zhang Q. X. 2021 was found to exert a significant influence on heterogeneity (18). It was considered that the heterogeneity might be due to this study recording adverse reactions such as dizziness, dry mouth, and bruising after acupuncture, which differed from the adverse reaction contents recorded in other studies. A random-effects model was therefore employed.
The results suggested that acupuncture treatment for PT-SP was safer than the conventional medical treatment [RR = 0.43, 95% CI (0.14, 1.32), p = 0.03] (Figure 9).
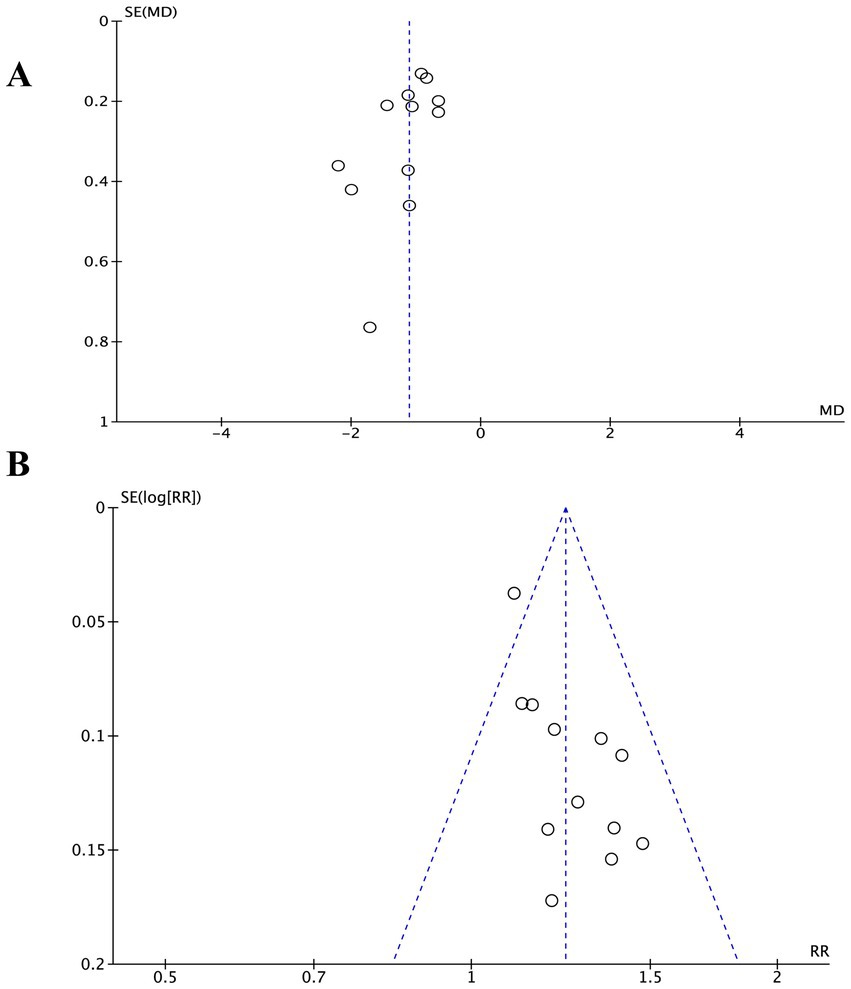
3.5 Publication bias detection
Investigating publication bias using funnel plots of VAS scores and the total efficacy rate, both showed mild asymmetry. Egger’s test results for VAS scores (p = 0.075) and for the total efficacy rate (p = 0.532) suggested no publication bias (Figure 10).
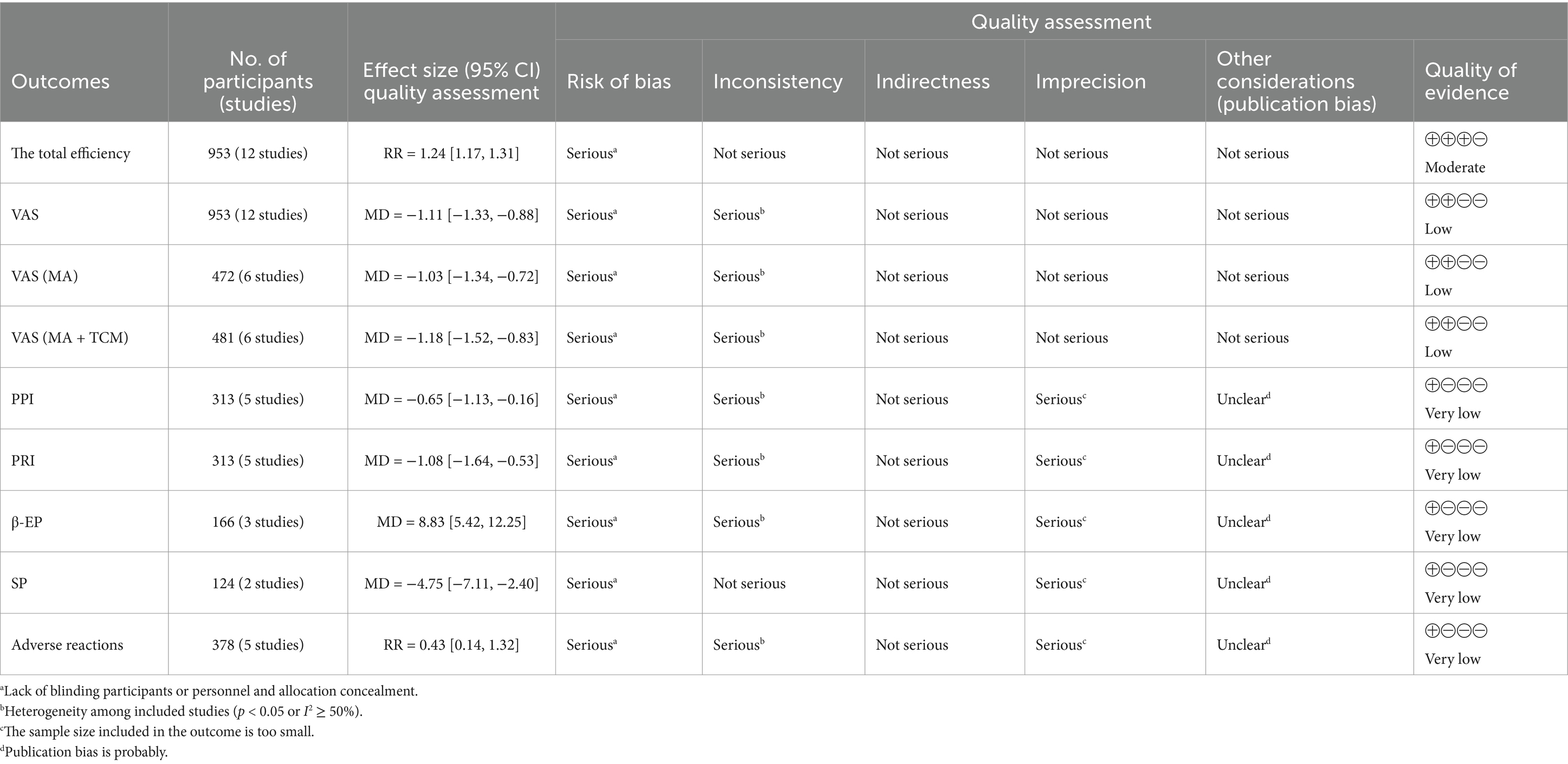
3.6 GRADE assessment
The GRADE system was utilized to evaluate the overall quality of the evidence. For all outcome measures, the evidence quality ranged from moderate to very low. The primary factor contributing to this decline in quality was the lack of blinding. Additional concerns included high heterogeneity among the studies, small sample sizes, and unclear allocation concealment (Table 3).
3.7 TSA
To estimate the required sample size for the meta-analysis and reduce the risk of false-positive results owing to random error, TSA was conducted for VAS scores, PPI scores, PRI scores, β-EP, SP, total efficacy rates, and adverse reactions. The Z-value curves (solid blue lines) for VAS scores, PPI scores, PRI scores, β-EP, SP, and total efficacy rates exceed both the traditional threshold (black dashed line) and the TSA threshold (solid red line). Except for PPI, the cumulative sample sizes for these outcomes had reached the required information size (RIS), allowing for definitive conclusions. Although the cumulative sample size for PPI had not yet reached the RIS, additional trials were not deemed necessary, permitting early definitive conclusions. For adverse reactions, the Z-value curves exceed the traditional threshold but did not meet the TSA threshold. The cumulative data had also not reached the expected amount, suggesting that conventional meta-analysis might lead to false-positive results. Therefore, additional trials were needed to confirm these findings (24) (Figure 11).
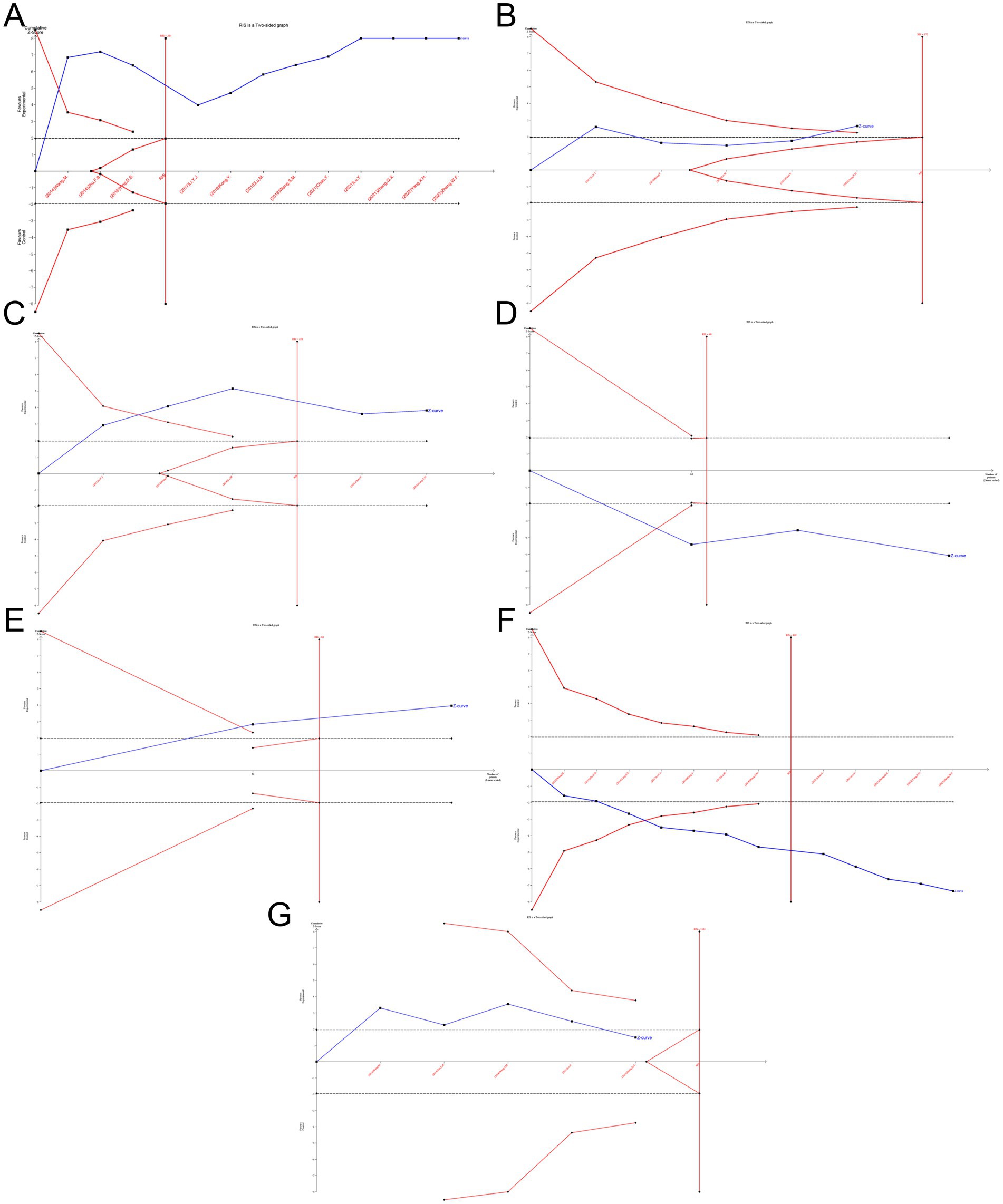
Figure 11. TSA for the VAS (A), PPI (B), PRI (C), β-EP (D), SP (E), total efficacy rate (F) and adverse reactions (G).
4 Discussion
4.1 Main findings
4.1.1 Pain scores
There was significant heterogeneity among pain indicators and subgroups, likely due to the diverse geographical locations and varying acupuncture techniques used in the studies. All 12 clinical trials included in this analysis reported positive outcomes, indicating that acupuncture was more effective than Western medication in reducing VAS, PPI, and PRI scores for PS-TP. Additionally, the combination of acupuncture with medication also showed notable efficacy in reducing VAS scores. VAS, PPI, and PRI together constitute the Short-Form McGill Pain Questionnaire (SF-MPQ), which assesses multiple dimensions of pain, including severity, type, and emotional aspects (25). Future research could further refine these assessments to better understand acupuncture is effectiveness across different pain types. Several studies have explored the mechanisms of acupuncture in treating PS-TP generally attributing its effects to the promotion of functional recovery following nerve damage (26–30). Monitoring relevant indicators and exploring the correlation between pain scores and these indicators could further elucidate the efficacy and mechanisms of acupuncture.
Recent advancements in studying the aftereffects of acupuncture highlight that these effects change over time, differing from the immediate effects targeting the spinal cord (31, 32). These aftereffects might influence the extrapyramidal system or neural circuits in the brain (33). As the cumulative aftereffects increase with more sessions, acupuncture tolerance may develop, leading to reduced analgesic effects. Thus, optimizing the frequency and duration of acupuncture sessions is crucial to balancing aftereffects, tolerance, and pain relief (34, 35). Follow-up studies showed that SF-MPQ of the treatment group remained lower than those of the control group, suggesting sustained benefits of acupuncture. However, variations in sample sizes, follow-up durations, acupoint selection, and techniques might affect the accuracy of these findings.
The minimal clinically important difference (MCID), a critical metric for evaluating the clinical significance of therapeutic effects, plays a pivotal role in both clinical research and medical practice. Currently, there is no established MCID threshold for the VAS in central neuropathic pain. Therefore, we referenced an MCID of 1.5 derived from chronic pain studies involving fibromyalgia and knee osteoarthritis (36). Compared to these conditions, PS-TP involves central nervous system damage with distinct pathophysiological mechanisms, which may result in more limited treatment-related improvements. This suggested that the MCID for PS-TP could be smaller than 1.5. Furthermore, based on the post-intervention analysis of VAS scores in this study MD was −1.87, the observed improvement did not reach the hypothesized MCID within the current treatment duration. Future studies should prioritize defining MCID thresholds specific to PS-TP and extending follow-up periods to investigate the optimal acupuncture treatment duration for this condition.
4.1.2 Analgesic mechanism
Acupuncture is analgesic mechanisms include the gate control theory of pain, diffuse noxious inhibitory control theory, reduction of central nervous system excitability, and modulation of neurotransmitters and immune functions. Recent studies have linked variations in blood-related indicators with pain-related disease processes (37–41). Acupuncture is analgesic effects involve bidirectional modulation of central neurotransmitters to suppress pain transmission. Acupuncture stimulates neural impulses that involve various chemicals, cytokines, and antagonistic factors (42). Enhancing acupuncture analgesia are substances such as β-EP, serotonin (5-HT), endogenous morphine-like substances, and acetylcholine, while substances like SP, cholecystokinin octapeptide, and GABA may oppose its effects. Three studies reported changes in β-EP and SP levels (43), indicating that acupuncture may reduce β-EP levels and increase SP levels, thus alleviating PS-TP.
4.1.3 Safety evaluation
Pharmacological treatments for PS-TP often have various adverse reactions, and non-pharmacological interventions lack standardized safety profiles (44, 45). Literature suggests that that acupuncture has a far lower rate of adverse events than Western treatment (46). Five studies reported adverse events, with four only detailing names and incidence rates. Two studies (Wang S. M. 2018 and Zhang, Q. X. 2021) noted the incidence and resolution time of acupuncture-induced bruising. One study (Wang M. 2014) also detailed measures taken and outcomes for adverse events. Overall, adverse events were lower in the treatment groups than the control groups, and acupuncture alone had fewer adverse events than combined acupuncture and medication treatments. This implies that acupuncture has a safety benefit for PS-TP. However, due to small sample sizes and various confounding factors, larger-scale real-world studies are needed to further investigate safety.
4.1.4 Mechanisms of pain emotion
Neuroscientific research confirms that pain-related emotions are integral to the pain experience, originating from thalamic pain signals and affecting pain perception (47). Acupuncture therapy has shown effectiveness in the regulation of pain-related emotions, not only alleviating pain but also modulating negative emotions (48, 49). This dual benefit highlights a significant advantage of acupuncture in pain management.
4.1.5 GRADE assessment and TSA
TSA was performed for all outcome indicators. Except for safety, the analyses were conclusive, suggesting no need for additional trials. GRADE assessment rated only total efficacy rate as moderate quality and the VAS score as low quality, while other indicators were rated very low. This rating is attributed to lack of blinding, small sample sizes, and publication bias. Future clinical studies should adhere to rigorous design and implementation standards to enhance research quality.
4.2 Strengths and limitations
4.2.1 Strengths
The strengths of this study include: (1) Incorporation of recent, high-quality studies with larger sample sizes, allowing a more comprehensive analysis. Previous reviews lacked detailed meta-analyses on post-effects, safety, and neuropeptide levels. (2) Evaluation of acupuncture is therapeutic effects across multiple indicators, reflecting its multi-mechanism and multi-target nature. (3) Use of subgroup and sensitivity analyses to address heterogeneity. (4) Applying qualitative and quantitative methods to assess publication bias, enhancing credibility. (5) Innovative use of TSA to adjust for random errors, ensuring reliable meta-analysis results.
4.2.2 Limitations
This study has limitations: (1) Variability in acupuncture protocols, including location, technique, and patient factors, affects efficacy and data accuracy (35, 50–53). (2) Given the lack of positive control drugs with established therapeutic efficacy for this disease, heterogeneous control group interventions may increase inter-study heterogeneity. (3) There is considerable variation in how side effects are reported across different studies, some studies do not provide detailed reports of adverse reactions, which impacts the comprehensive assessment of the safety of acupuncture treatment. (3) Non-standardized randomization and the lack of blinding in included studies could lead to bias. (4) Because all research was done in China, generalizability may be limited. (5) Low quality of evidence for some indicators, as assessed by GRADE, may impact result accuracy.
4.3 Implications for further research
This study provides a comprehensive analysis of the efficacy and safety of acupuncture for PS-TP, evaluating multiple indicators, including overall efficacy rates, scale scores, blood test results, and adverse reaction rates. To address the limitations of studies and enhance future research, several areas for improvement are suggested: (1) Sample size: Increasing sample sizes in future studies can enhance statistical power, reduce random errors, and improve the reliability of conclusions. (2) Study design: Adhering to Cochrane Handbook guidelines is crucial. Future studies should provide detailed reports on random sequence generation, allocation concealment, and blinding implementation. While blinding researchers is challenging in acupuncture studies, using sham acupuncture for the control group can blind participants. Incorporating a placebo-controlled design (acupuncture + placebo vs. sham acupuncture + medication) can help meet blinding and ethical requirements. As the field advances, it is imperative to establish standardized control protocols specifically tailored for PS-TP research. Such standardization will enhance the comparability and reliability of findings across studies, ultimately facilitating evidence-based clinical decision-making. (3) Safety evaluation: More focus is needed on safety aspects. Future research should more thoroughly document and report adverse reactions to comprehensively assess the safety of acupuncture. (4) Long-term effects: Current studies lack sufficient attention to the long-term effects of acupuncture. Future research should include multiple follow-up time points post-treatment to better understand the enduring effects and patterns of acupuncture for PS-TP. (5) Objective assessment methods: Investigate mechanisms using objective assessment tools such as blood tests, functional magnetic resonance imaging, and electroencephalography. These methods can provide deeper insights into the mechanisms of acupuncture. (6) Pain emotion assessment: There should be an increased emphasis on evaluating pain emotion indicators to more accurately assess the comprehensive efficacy of acupuncture therapy.
Addressing these areas will contribute to a more thorough understanding of acupuncture’s effectiveness and safety for PS-TP.
5 Conclusion
This study demonstrates that acupuncture is effective in improving clinical outcomes and reducing pain scores for PS-TP, with the added benefit of reducing β-EP levels and increasing SP levels. It offers certain advantages in reducing pain scores long-term, without significant adverse reactions observed. While the evidence supports acupuncture as an effective treatment for PS-TP, the small sample size and variability in study designs call for further research. Continued exploration through RCTs is necessary to provide more substantial evidence for clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
TZ: Data curation, Formal analysis, Project administration, Software, Visualization, Writing – original draft, Writing – review & editing. JZ: Data curation, Project administration, Writing – original draft, Writing – review & editing. LC: Data curation, Visualization, Writing – original draft, Writing – review & editing. KJ: Data curation, Writing – original draft. DW: Software, Writing – review & editing. HS: Writing – original draft, Writing – review & editing. BW: Writing – review & editing. XC: Writing – review & editing. XD: Conceptualization, Methodology, Supervision, validation, Writing – original draft, Writing – review & editing. LZ: Conceptualization, Methodology, Supervision, validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the High-Level Traditional Chinese Medicine Hospital SMI Project (DZMG-LJRC0010) and China Medical Association of Minorities (2023MY174-50).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ri, S. The management of poststroke thalamic pain: update in clinical practice. Diagnostics. (2022) 12:1439. doi: 10.3390/diagnostics12061439
2. Liu, S. New perspective of acupuncture analgesia: reward of chronic pain relief and related brain reward circuits. Zhen Ci Yan Jiu. (2022) 47:268–73. doi: 10.13702/j.1000-0607.20210176
3. Mohanan, AT, Nithya, S, Nomier, Y, Hassan, DA, Jali, AM, Qadri, M, et al. Stroke-induced central pain: overview of the mechanisms, management, and emerging targets of central post-stroke pain. Pharmaceuticals. (2023) 16:1103. doi: 10.3390/ph16081103
4. He, C, Liu, R, Fan, Z, Li, Y, Yang, M, Wugang, H, et al. Microglia in the pathophysiology of hemorrhagic stroke and the relationship between microglia and pain after stroke: a narrative review. Pain Ther. (2021) 10:927–39. doi: 10.1007/s40122-021-00288-3
5. Song, S, Sun, C, Pei, L, Xu, W, and Huang, Y. Progress in diagnosis and treatment of central post-stroke pain. Med J Peking Union Med Coll Hosp. (2024) 15:265–71. doi: 10.12290/xhyxzz.2023-0591
6. Tao, Y, Lei, J, and You, H. Pathophysiological mechanism and treatment of central pain after stroke. Chin J Pain Med. (2023) 29:371–5. doi: 10.3969/j.issn.1006-9852.2023.05.009
7. Liqun, Z, Jing, L, and Haojun, Y. Progress of clinical research on acupuncture in the treatment of central pain after stroke. J External Ther Tradit Chin Med. (2021) 30:90–2. doi: 10.3969/j.issn.1006-978X.2021.03.042
8. Jinyu, Y, and Xiyuan, X. Research progress on traditional Chinese medicine in the treatment of thalamic pain after stroke. Chin Med Mod Distance Educ China. (2022) 20:206–8. doi: 10.3969/j.issn.1672-2779.2022.05.076
9. Yue, L, Ruoyu, W, Shenwei, L, Xixiao, H, Yating, X, Yiyan, W, et al. Advances in the treatment of post-stroke thalamic pain with acupuncture. J Emerg Tradit Chin Med. (2022) 31:2057. doi: 10.3969/j.issn.1004-745X.2022.11.048
10. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
11. Higgins, JPT, Altman, DG, Gotzsche, PC, Juni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
12. Min, W, Shuhong, G, Boru, Z, and Ming, L. The clinical observation of acupuncture combined with herbs to treat thalamic pain after ischemic stroke. Tian Jing Tradit Chin Med. (2014) 31:269–71. doi: 10.11656/j.issn.1672-1519.2014.05.05
13. Dansong, Y, Liang, Z, and Ming, Y. Clinical observation on 31 cases of post-stroke thalamic pain treated by Yanghe tang plus flavor combined with acupuncture. Zhejiang J Tradit Chin Med. (2016) 51:349–50. doi: 10.13633/j.cnki.zjtcm.2016.05.021
14. Yajie, L, Hao, T, Li, A, and Xuemin, S. Resuscitation acupuncture for thalamic pain: a randomized controlled trial. Chin Acupunct Moxibust. (2017) 37:14–8. doi: 10.13703/j.0255-2930.2017.01.003
15. Ming, L, Linzhi, L, and Lu, M. Clinical observation on restoring consciousness and opening the orifices needling combined with scalp acupuncture electrical stimulation in treating 40 cases of thalamic pain after stroke. J Tradit Chin Med. (2018) 59:861–5. doi: 10.13288/j.11-2166/r.2018.10.012
16. Shumin, W. Clinical observation of row/dot needling cutaneous region of Meridian sinew combined with needling stellate ganglion treating post-stroke thalamic pain. Acta Chin Med Pharmacol. (2018) 46:81–4. doi: 10.19664/j.cnki.1002-2392.180122
17. Ying, K, Yumenxin, W, Di, W, and Hongchao, D. Clinical observation on the treatment of post-stroke thalamic pain by the “Dragon and Tiger Fighting” acupuncture method. Guiding J Tradit Chin Med Pharm. (2018) 24:52–4. doi: 10.13862/j.cnki.cn43-1446/r.2018.14.016
18. Qixin, Z, and Yin, L. Clinical observation on treatment of thalamic pain in convalescent stage of ischemic stroke with acupuncture and medicine. World J Integr Tradit Western Med. (2021) 16:1119. doi: 10.13935/j.cnki.sjzx.210627
19. Ying, L, Jingmian, Y, Yanxia, Y, and Qixin, Z. Clinical effect of acupuncture and medicine in the treatment of thalamic pain in the recovery period of ischemic stroke. World J Integr Tradit Western Med. (2021) 16:1353. doi: 10.13935/j.cnki.sjzx.210736
20. Yu, C, and Min, W. The efficacy of acupuncture and medicine in treating thalamic pain in 33 cases of recovery after ischemic stroke. Hunan J Tradit Chinese Med. (2021) 37:72–4. doi: 10.16808/j.cnki.issn1003-7705.2021.03.025
21. Xiaohong, Y. Effect of acupuncture combined with Shentong Zhuyu decoction on the degree of thalamus pain and hemorheology index in stroke recovery period. J Med Inform. (2022) 35:177–9. doi: 10.3969/j.issn.1006-1959.2022.11.047
22. Weifeng, Z, and YingLin, C. Clinical observation on 100 cases of post stroke thalamic pain treated with consciousness-restoring resuscitation acupuncture combined with Pregabalin. J Gansu Univ Chin Med. (2023) 40:68–72. doi: 10.16841/j.issn1003-8450.2023.02.15
23. Fengbin, Z. Clinical research on mind-regulating analgesic acupuncture for thalamic pain. Med Inf. (2014) 27:69–70. doi: 10.3969/j.issn.1006-1959.2014.24.067
24. Yun, X, Yin, S, Zhaolan, L, and Jianping, L. Estimation of sample size in systematic review and meta-analysis: trial sequential analysis. Mod Chin Clin Med. (2013) 20:31–3. doi: 10.3969/j.issn.1672-2205.2013.05.009
25. Melzack, R. The Short-Form Mcgill Pain Questionnaire. Pain. (1987) 30:191–7. doi: 10.1016/0304-3959(87)91074-8
26. He, GH, Ruan, JW, Zeng, YS, Zhou, X, Ding, Y, and Zhou, GH. Improvement in acupoint selection for acupuncture of nerves surrounding the injury site: electro-acupuncture with governor vessel with local Meridian acupoints. Neural Regen Res. (2015) 10:128–35. doi: 10.4103/1673-5374.150720
27. Caifang, T. Clinical efficacy observation of head-needle plexus method for the treatment of thalamic pain in the recovery period of stroke. [Master’s thesis]. Heilongjiang: Heilongjiang University of Chinese Medicine (2018).
28. Xirui, Y. Clinical observation on the effect of Sun’s abdominal acupuncture on improving thalamic pain after apoplexy. [Master’s thesis]. Heilongjiang: Heilongjiang University of Chinese Medicine (2018).
29. Shinong, G, Yujia, L, and Zhenjie, W. Effect of Tongdu Tiaoshen acupuncture on nerve function and Beclin-1 protein expression in Cir rats based on autophagy. JCAM. (2020) 36:64–8. doi: 10.3969/j.issn.1005-0779.2020.10.017
30. Tyrtyshnaia, A, and Manzhulo, I. Neuropathic pain causes memory deficits and dendrite tree morphology changes in mouse hippocampus. J Pain Res. (2020) 13:345–54. doi: 10.2147/jpr.s238458
31. Shaozong, C. Clinical significance of the study of the chronotropic relationship of the action of acupuncture. J Clin Acupunct and Moxibust. (2008) 6:1–3. doi: 10.3969/j.issn.1005-0779.2008.06.001
32. Yunfan, X, Yiyi, W, Rongrong, L, Ning, L, Xiaofen, H, Yongliang, J, et al. Progress in the study of the central mechanism of the cumulative effect of acupuncture analgesia. Zhejiang J Integr Tradit Chin Western Med. (2022) 32:585–8. doi: 10.3969/j.issn.1005-4561.2022.06.027
33. Yu, Z, Xiaofei, J, Jiani, L, Li, R, Zuoyao, M, Jinpen, C, et al. Analysis of low frequency amplitude on acupuncture antagonist muscles in patients with acupuncture stroke by resting state functional MRI. Ningxia Med. (2020) 42:601–4. doi: 10.13621/j.1001-5949.2020.07.0601
34. Shirong, H. Aftereffects of acupuncture analgesia, acupuncture tolerance and frequency of needling. China J Pain Med. (2006) 6:360–2. doi: 10.3969/j.issn.1006-9852.2006.06.016
35. Lulu, L, Liqiong, W, Jingwen, Y, Jianfeng, T, Tianqi, W, Xuan, Z, et al. Researches status on time-effect of acupuncture. Chin Acupunct Moxibust. (2019) 39:565–70. doi: 10.13703/j.0255-2930.2019.05.029
36. Antonioni, A, Baroni, A, Fregna, G, Ahmed, I, and Straudi, S. The effectiveness of home-based transcranial direct current stimulation on chronic pain: a systematic review and meta-analysis. Digit Health. (2024) 10:20552076241292677. doi: 10.1177/20552076241292677
37. Vickers, AJ, Vertosick, EA, Lewith, G, Macpherson, H, Foster, NE, Sherman, KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
38. Takenaka, S, Sukenaga, N, Ohmuraya, M, Matsuki, Y, Maeda, L, Takao, Y, et al. Association between neuropathic pain characteristics and DNA methylation of transient receptor potential ankyrin 1 in human peripheral blood. Medicine. (2020) 99:e19325. doi: 10.1097/md.0000000000019325
39. Islam, B, Stephenson, J, Young, B, Manca, M, Buckley, DA, Radford, H, et al. The identification of blood biomarkers of chronic neuropathic pain by comparative transcriptomics. NeuroMolecular Med. (2021) 24:320–38. doi: 10.1007/s12017-021-08694-8
40. Ko, JH, and Kim, S-N. Effect of acupuncture on pain and substance P levels in middle-aged women with chronic neck pain. Front Neurol. (2023) 14:1267952. doi: 10.3389/fneur.2023.1267952
41. Yevgi, R, Laloğlu, E, and Bilge, N. High plasma calcitonin gene-related peptide and serum pituitary adenylate cyclase-activating polypeptide levels in patients with neuropathic pain. Rev Neurol. (2023) 179:289–96. doi: 10.1016/j.neurol.2022.10.005
42. Zheng, X, Lin, J, Wang, Z, Zeng, Z, and Chen, H. Research of the analgesic effects and central nervous system impact of electroacupuncture therapy in rats with knee osteoarthritis. Heliyon. (2024) 10:e21825. doi: 10.1016/j.heliyon.2023.e21825
43. Qian, W, and Yongxin, B. Analysis on the principle of acupuncture analgesia. China J Tradit Chin Med Pharm. (2019) 34:4911–3.
44. Kim, JS, Bashford, G, Murphy, KT, Martin, A, Dror, V, and Cheung, R. Safety and efficacy of pregabalin in patients with central post-stroke pain. Pain. (2011) 152:1018–23. doi: 10.1016/j.pain.2010.12.023
45. Liampas, A, Velidakis, N, Georgiou, T, Vadalouca, A, Varrassi, G, Hadjigeorgiou, GM, et al. Prevalence and management challenges in central post-stroke neuropathic pain: a systematic review and meta-analysis. Adv Ther. (2020) 37:3278–91. doi: 10.1007/s12325-020-01388-w
46. Yijun, Z, Qinhui, F, Jun, W, and Jian, P. Recent research progress on the treatment of thalamic pain after stroke with acupuncture and moxibustion. Chin J Acupunct Moxibust. (2017) 6:166–70. doi: 10.3877/cma.j.issn.2095-3240.2017.04.012
47. Jianqiao, F. Acupuncture analgesia-panorama multi-dimensional treatment of pain. Acupunct Res. (2018) 43:459–66. doi: 10.13702/j.1000-0607.180380
48. X-m, S, Shen, Z, Sun, J, Fang, F, J-f, F, Wu, Y-y, et al. Strong manual acupuncture stimulation of “Huantiao” (Gb 30) reduces pain-induced anxiety and P-Erk in the anterior cingulate cortex in a rat model of neuropathic pain. Evid Based Complement Alternat Med. (2015) 2015:235491. doi: 10.1155/2015/235491
49. Wu, Y-y, Jiang, Y-l, He, X-f, Zhao, X-y, Shao, X-m, Du, J-y, et al. Effects of electroacupuncture with dominant frequency at SP 6 and ST 36 based on Meridian theory on pain-depression dyad in rats. Evid Based Complement Alternat Med. (2015) 2015:732845. doi: 10.1155/2015/732845
50. Leung, A, Zhao, Y, and Shukla, S. The effect of acupuncture needle combination on central pain processing-an fMRI study. Mol Pain. (2014) 10:1744–8069. doi: 10.1186/1744-8069-10-23
51. Laiju, Z, Yajun, W, and Kai, S. The impact of course on the therapeutic effect of acupuncture and moxibustion. Clin J Tradit Chinese Med. (2018) 30:754–7. doi: 10.16448/j.cjtcm.2018.0228
52. Hui, W, Changzhen, G, Haihe, T, Yinmin, W, and Baoyan, L. From experience to evidence in clinical acupuncture medicine—a discussion of modern acupuncture efficacy research methods. Guiding J Tradit Chin Med Pharm. (2021) 27:1–8. doi: 10.13862/j.cnki.cn43-1446/r.20200806.007
Keywords: acupuncture, stroke, thalamic pain, systematic review, meta-analysis
Citation: Zhang T, Zhai J, Cheng L, Jiang K, Wang D, Shi H, Wang B, Chen X, Dong X and Zhou L (2025) Acupuncture effects of post-stroke thalamic pain: a systematic review and meta-analysis of randomized controlled trials. Front. Neurol. 16:1528956. doi: 10.3389/fneur.2025.1528956
Edited by:
Hongxuan Wang, Sun Yat-sen Memorial Hospital, ChinaReviewed by:
Eric Chun-Pu Chu, EC Healthcare, Hong Kong SAR, ChinaAnnibale Antonioni, University of Ferrara, Italy
Han Wang, First Affiliated Hospital of Anhui University of Traditional Chinese Medicine, China
Guido Knapp, Technical University Dortmund, Germany
Copyright © 2025 Zhang, Zhai, Cheng, Jiang, Wang, Shi, Wang, Chen, Dong and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinglu Dong, YXJ0aGFzZHhsQDE2My5jb20=; Li Zhou, emhvdWxqazcyMTFAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Tianwei Zhang
Tianwei Zhang Junying Zhai
Junying Zhai Ling Cheng1,2
Ling Cheng1,2 Kaixin Jiang
Kaixin Jiang Dayang Wang
Dayang Wang Xing Chen
Xing Chen Xinglu Dong
Xinglu Dong