Abstract
Objective:
To evaluate and compare the safety and efficacy of spinal manipulation, mobilization, and massage for the management of cervicogenic headache (CGH) using meta-analytic techniques.
Methods:
Comprehensive searches were conducted in Cochrane, Embase, PubMed, and ClinicalTrials.gov to identify studies investigating the effects of manipulation, mobilization, and massage on pain, disability, and physical function in patients with CGH. Key outcomes included pain severity (visual analog scale, VAS), Neck Disability Index (NDI), Flexion-Rotation Test (FRT), and Headache Disability Inventory (HDI) at various follow-up timepoints.
Results:
Fourteen studies totaling 1,297 CGH patients were included. Standard pairwise meta-analysis revealed that sustained natural apophyseal glides (SNAG) mobilization produced significantly greater improvements compared to non-SNAG interventions in VAS (MD = 1.73, 95%CI: 1.05, 2.40), NDI (MD = 8.55, 95%CI: 2.73, 14.37), FRT (MD = −7.22, 95%CI: −9.38, −5.07), and HDI (MD = 9.29, 95%CI: 3.64, 14.95), with benefits maintained over time. Network meta-analysis showed that for VAS improvement, the surface under the cumulative ranking curve (SUCRA) probabilities were: cervical spine manipulation (CSM, 98.9%), mobilization (67.3%), exercise (21.0%), and massage (12.8%). For NDI, the SUCRA scores were: CSM (82.2%), mobilization (57.2%), exercise (6.7%), and massage (53.9%). CSM exhibited significantly greater VAS reductions compared to exercise, massage, and mobilization, while mobilization was superior to exercise and massage for VAS. For NDI, CSM was significantly better than exercise, but no other between-group differences were observed.
Conclusion:
In patients with CGH, SNAG mobilization can significantly improve pain and function, with benefits maintained in the long-term. Additionally, CSM may be the most effective short-term intervention for reducing pain and disability compared to mobilization, massage, and exercise, although clinician expertise appears to be an important factor.
Systematic Review Registration:
1 Introduction
Cervicogenic Headache (CGH) denotes a type of headache syndrome characterized by the transmission of pain sensations from the cervical region to the head (1). Typically arising from issues such as cervical muscle tension, cervical facet joint osteoarthritis, cervical disc protrusion, and other cervical pathologies, CGH commonly manifests alongside symptoms like neck pain, restricted cervical mobility, and cervical-thoracic stiffness (2). These symptoms tend to emerge following sustained neck postures, repetitive cervical movements, or physical exertion, often accompanied by limitations in cervical range of motion. CGH presents as a non-throbbing, unilateral headache originating from the cervical spine and extending to the occipital, temporal, and periorbital regions, representing a predominant headache subtype. The precise pathophysiological mechanisms underlying cervicogenic headache remain elusive but are intricately linked to pathological changes within cervical anatomical structures, encompassing factors such as cervical facet joint dysfunction, myofascial inflammatory or mechanical compression of cervical nerves, and musculoskeletal impairments (3).
Primary management strategies for CGH include physical therapy interventions, comprising manual techniques and therapeutic exercises, which have demonstrated efficacy in alleviating cervicogenic headaches (4). Moderate-quality evidence supports the use of manual therapies (e.g., cervical muscle relaxation techniques, spinal manipulation), targeted exercise modalities (static and dynamic stretching exercises for cervical and scapular joints or upper extremities), and low-load endurance exercise programs to ameliorate headache intensity, pain, disability, as well as frequency and duration (5).
The foundational principles of manual therapy encompass Manipulation, Mobilization, Massage, among other modalities, each distinct yet interconnected in their approaches (6). Manipulation involves high-velocity, low-amplitude maneuvers, whereas Mobilization entails low-velocity, high-amplitude movements. Massage techniques employ varied pressure applications through kneading, stroking, percussion, or other methods to elicit desired muscular responses (7). Owing to diverse anatomical and physiological dysfunctions, manual therapy emerges as a prevalent treatment modality for CGH patients, despite conflicting evidence concerning its effectiveness. “Sustained Natural Apophyseal Glides” (SNAGs), a Mobilization-based therapeutic technique pioneered by Mulligan, posits that subtle joint misalignments following neck trauma or strain contribute to restricted motion and pain, imperceptible through conventional assessments (8). Mulligan believes that they are not visible through palpation or X-rays. However, with the correct joint mobilization, pain-free functional activity can be achieved, and with repeated application, sustained improvement is possible (9). Distinguished from conventional joint mobilizations solely targeting joint structures, Mulligan’s approach integrates joint mobilization with soft tissue release, effectuated by applying pressure to spinal processes in a weight-bearing position (10), inducing synchronous sliding movements in minor joints as part of the SNAGs protocol (11). Meta-analytical findings corroborate the efficacy of SNAGs in alleviating pain, reducing disability, and enhancing quality of life in CGH patients (12), notwithstanding the inconclusive evidence regarding differential efficacy among distinct manual therapy modalities (13).
2 Methods
This study is a meta-analysis of randomized controlled trials (RCTs) conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.1 Search strategy
A literature search was conducted to identify studies on the effects of Manipulation, Mobilization, and Massage in alleviating the frequency, severity, and functionality of patients with Cervicogenic Headaches (CEHs) in Cochrane, Embase, PubMed, and Clinicaltrials.gov. These databases were searched for studies assessing the effects of manipulation, mobilization, and massage on CGH.
The following search terms were used: ((Cervicogenic headaches) OR (Cervicogenic headache)) AND (((((Manipulation) OR (Mobilization)) OR (Massage)) OR (SNAG))). The search deadline was July 1, 2024. The review included studies without any language restrictions, ensuring a more comprehensive search and inclusion of international studies.
2.2 Study selection criteria
Literature inclusion was determined based on the PICOS criteria. P (Patients): studies included had to focus on patients diagnosed with CGH according to accepted diagnostic criteria. This ensures the studies are highly relevant to the topic of interest; I (Intervention): the intervention must involve one or more manual therapies such as manipulation, mobilization, or massage. The use of SNAGs was also included; C (Control): The control could include other manual therapies, sham treatments, exercise interventions, or no intervention. This broad control category allowed for comparison across different interventions. O (Outcome): the study outcomes needed to include pain and functional measures post-intervention, specifically using tools such as the Neck Disability Index (NDI), Headache Disability Inventory (HDI), Numerical Pain Rating Scale (NPRS), and the Flexion-Rotation Test (FRT); S (Study design): Only randomized controlled trials (RCTs) were included to ensure the highest level of evidence. RCTs are considered the gold standard in clinical research for assessing the effectiveness of interventions.
Studies were excluded for the following reasons: (1) headaches diagnosed as migraines or tension-type headaches from other causes, (2) case reports or studies with fewer than 5 participants, (3) studies not published in peer-reviewed journals, and (4) studies not published in English.
Impact of control group variability on comparison: inconsistent sham interventions: different control group settings across studies (e.g., placebo mobilizations vs. minimal interventions) introduce variability, making it hard to determine if observed effects are from the manual therapy (like snag) or the control treatments themselves. Sham groups and placebo effect: if some control groups receive more active treatments (e.g., mild mobilization), it could mask the effects of the manual therapy. This makes it difficult to know if improvements are due to the experimental therapy or the control intervention being unexpectedly effective. Bias in interpretation: the variation in control conditions can lead to biased conclusions. If one study uses a minimal control while another uses a more active placebo, it may make the experimental treatment seem more effective than it actually is.
To improve the validity and comparability of future research on SNAG therapy for CGH, studies should adopt standardized sham interventions (e.g., “non-specific mobilization”) to ensure consistent controls, implement rigorous double-blinding procedures for both participants and assessors to minimize bias, incorporate active comparators like spinal manipulation to better evaluate relative efficacy, and standardize patient cohorts based on clinical characteristics such as headache severity and duration. These methodological refinements would enhance study reliability and facilitate more meaningful comparisons across trials investigating SNAG’s therapeutic effectiveness.
Revised network meta-analysis strategy: subgroup analysis: group studies by control type to see how different controls impact treatment outcomes. This would clarify how snag compares under different conditions. Sensitivity analysis: conduct sensitivity analyses to explore how variations in control conditions affect results. This helps adjust the findings and makes the conclusions more reliable.
2.3 Outcome measures
Headache Disability Inventory (HDI): a self-report questionnaire assessing the impact of headaches on daily activities. Higher scores indicate greater disability caused by headaches.
Neck Disability Index (NDI): a self-report questionnaire measuring limitations in daily activities due to neck pain. Higher scores indicate greater disability.
Numerical Pain Rating Scale (NPRS): a scale quantifying pain intensity using a numerical scale, providing a standardized measure of pain severity. Higher scores indicate greater pain intensity.
Flexion-Rotation Test (FRT): used to assess dysfunction in the C1-C2 motion segment, represented by the angle of rotation in neck flexion position, with a normal value around 45° and reduced angles indicating dysfunction (14).
2.4 Data extraction and quality assessment
Data were extracted into a predefined Excel sheet, including first author, publication date, patient characteristics, sample size, patient age, interventions, intervention duration, outcome measures, etc. Cross-checking was performed on extracted data, and discrepancies were resolved by a third reviewer.
Two authors independently assessed bias risk using the Cochrane risk of bias tool. Bias risk was evaluated across 7 items under 6 domains: selection (including random sequence generation and allocation concealment), performance (blinding of participants and personnel), detection (blinding of outcome assessment), attrition (completeness of outcome data), reporting (selective reporting of results), and other biases. Each item was judged as “low risk of bias,” “high risk of bias,” or “unclear” based on bias assessment criteria.
2.5 Statistical methods
This study compares the efficacy of different manual therapy modalities in CGH. Network meta-analysis is the preferred method, but due to substantial differences in methods and outcomes of sham interventions among studies, there may be considerable heterogeneity that could complicate interpretation and affect conclusions. Therefore, this study is divided into two parts: a conventional meta-analysis comparing the efficacy of SNAGS vs. non-SNAGS, and a network meta-analysis comparing the efficacy of CSM, Mobilization, and Massage.
Conventional meta-analysis was conducted using the R meta package, and figures were generated. Heterogeneity among studies was analyzed using Q and I2 tests. I2 values were interpreted as follows: 0 indicates variation due to sampling error only; <0.25 suggests low heterogeneity; between 0.25 and 0.5 suggests moderate heterogeneity; >0.5 indicates high heterogeneity. Subgroup analyses were conducted for moderate to high heterogeneity, using random-effects models, while fixed-effects models were used for no to low heterogeneity. Funnel plots were used to assess publication bias, with Begg’s test and Egger’s test conducted when including ≥10 studies, and visual inspection for symmetry when fewer than 10 studies. Standardized mean differences (SMD) were used for continuous variables, and risk ratios (RR) for categorical variables. Statistical significance was considered when SMD did not include 0 and RR did not include 1. Stata software was utilized for network meta-analysis, generating network plots, calculating Surface Under The Cumulative Ranking (SUCRA), creating SUCRA plots, and pairwise comparison forest plots. In the network plot, the size of points represents sample sizes, lines indicate direct comparisons, and the thickness of lines represents the number of studies included. Higher SUCRA values indicate better rankings.
3 Results
3.1 Literature screening process
A total of 513 articles were initially retrieved from the databases. After eliminating duplicates using Endnote, 193 articles underwent preliminary screening. Upon reviewing titles and abstracts, 157 articles were excluded for reasons such as not involving clinical studies, lacking manual therapy utilization, or not being RCTs. Following a full-text review of the remaining 36 articles, 22 were further excluded due to various reasons like data extraction challenges, inadequate intervention durations, or data unavailability, resulting in the inclusion of 16 articles. The flowchart illustrating the literature inclusion process is depicted in Figure 1.
Figure 1

Basic information of included literature chart.
3.2 Basic information of included literature
Among the 16 included articles, a total of 769 subjects were involved with an average age range spanning from 21.8 to 48.4 years. Manual therapy methods in the included studies encompassed Manipulation, Mobilization, SNAGs, Massage, among others. Table 1 presents the basic information of the included literature. The quality assessment of the included studies using the Risk of Bias (ROB) tool is illustrated in Figure 2.
Table 1
| Author | Year | Intervention | n | Age | Duration and frequency |
|---|---|---|---|---|---|
| Dunning JR (25) | 2016 | Manipulation | 58 | 34.1 (12.6) | 6–8 sessions over 4 weeks |
| Mobilization and exercise | 52 | 36.4 (10.0) | |||
| Kashif M (26) | 2022 | Mulligan SNAGs | 20 | 22.20 (1.64) | 3 times a week for a total of 20 min per performance for 12 times in 4 weeks |
| Placebo treatment | 20 | 21.80 (1.54) | |||
| Christian N (27) | 2017 | Mulligan SNAGs | 8 | 26.8 (1.5) | Treatment for 1 week |
| Active neck Range of motion exercises | 8 | 31 (2.09) | |||
| Malo-Urriés M (28) | 2017 | Translatoric mobilizations | 41 | 42.49 (15.61) | 30-min treatment consisting of 30-s series of translatoric mobilizations of the upper cervical spine with 10-s rest periods between sets |
| No treatment | 41 | 40.59 (15.10) | |||
| Youssef EF (29) | 2013 | Passive spinal mobilizations mobilization | 18 | 32.4 (6.5) | Two sessions/week for 6 weeks |
| Massage | 18 | 31.0 (3.49) | |||
| Lerner-Lentz A (21) | 2021 | Mobilization | 24 | 47.5 (17.7) | Two sessions, uncertain timing |
| Manipulation | 21 | 48.4 (15.5) | |||
| McDevitt AW (30) | 2022 | Thoracic spine manipulation | 24 | 34.96 (9.38) | 1–2 times weekly for up to 4 weeks |
| Hold | 24 | 33.88 (11.79) | |||
| Nambi G (31) | 2024 | Cervical spine manipulation | 32 | 35.6 (3.8) | 6 sessions over 3 weeks |
| Conventional physiotherapy | 32 | 36.2 (3.7) | |||
| Satpute K (32) | 2024 | Mulligan SNAGs | 33 | 40 (11) | 6 treatment sessions as per group allocation spread over 4 consecutive weeks |
| Exercise | 33 | 40 (11) | |||
| Shin EJ (33) | 2014 | SNAGs | 20 | 48.20 (7.79) | 3times per week, 20 min per performance, a total of 12 times in 4 weeks |
| Placebo SNAGs | 20 | 48.05 (6.81) | |||
| Kirthika V (34) | 2018 | Mulligan SNAGs | 12 | 26.2 (6.8) | 3 times per session/day×5 days/week for 4 weeks’ duration |
| Muscle energy technique | 12 | 25.7 (7.1) | |||
| Khalil M (35) | 2019 | Mulligan SNAGs | 15 | 42.53 (7.15) | 9 sessions every other day for 4 weeks |
| Traditional treatment | 15 | 41.6 (6.62) | |||
| Murtza S (36) | 2024 | Rocabado | 18 | 40.06 (8.93) | 2 treatment sessions per week with a maximum of 16 treatment sessions over 8 weeks |
| SNAGs | 18 | 40.39 (10.59) | |||
| Jin X (37) | 2023 | SNAGs | 20 | 30.05 (6.75) | Once per day, 10 times for one session |
| Health promotion | 20 | 27.19 (4.76) | |||
| Rani M (38) | 2022 | Spinal mobilization | 20 | 41.45 (13.21) | 4 weeks, 4 times a week (16 sessions) and each treatment session lasted for approximately 30 min |
| SNAGs | 20 | 38.55 (9.28) | |||
| Motion exercises | 20 | 38.65 (13.89) | |||
| Hall T (39) | 2007 | Shame SNAGs | 16 | 38 (14) | Daily self-administration for 12 months |
| SNAGs | 16 | 33 (11) |
Characteristics of included studies.
Figure 2
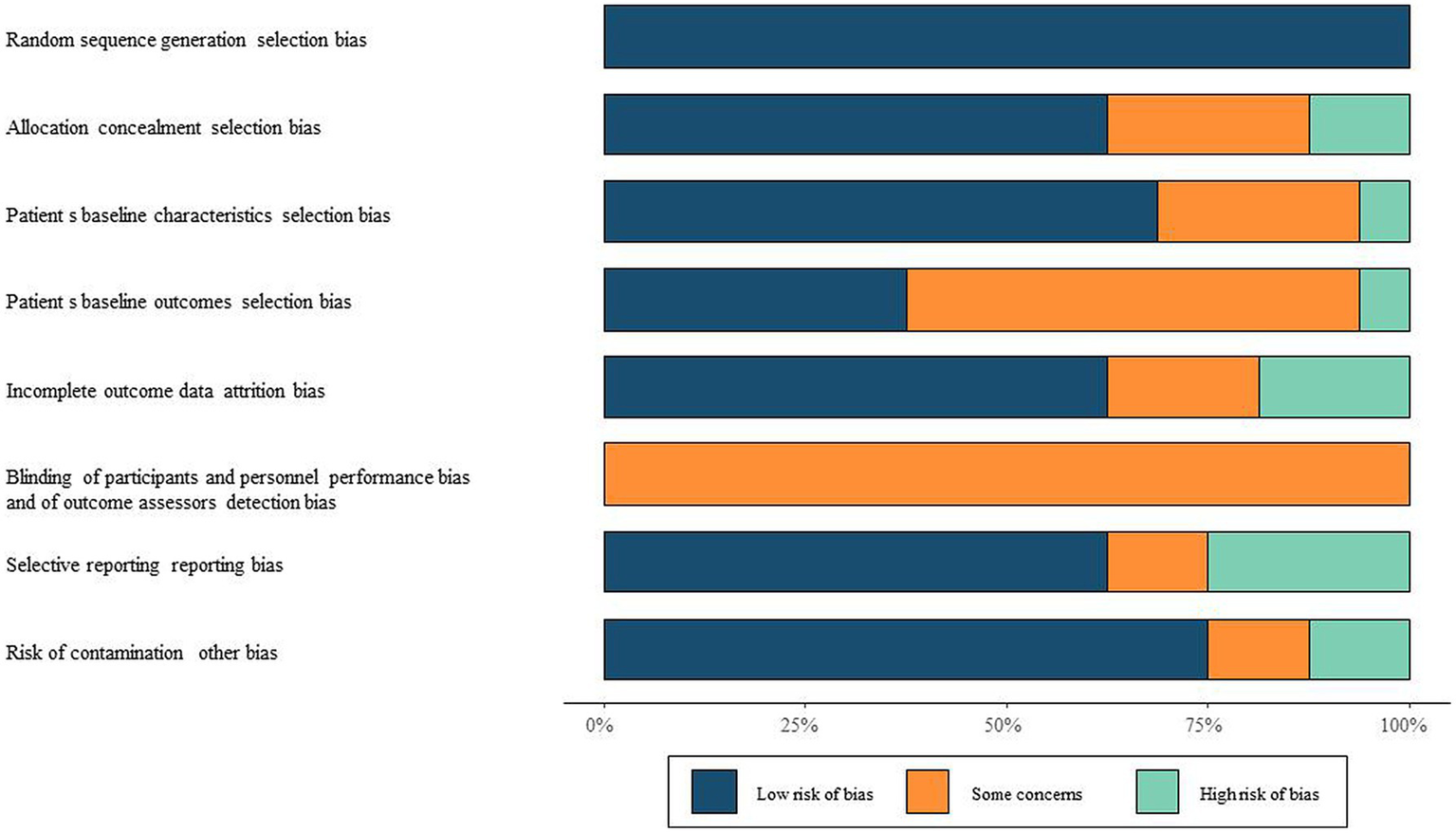
Risk of bias assessment of included literature ROB chart.
3.3 SNAG vs. non-SNAG
Out of the included studies, 10 articles reported the use of SNAG with control groups involving SNAG, exercise, soft tissue massage, Mobilization, etc. Follow-up durations ranged from a minimum of 1 week to a maximum of 12 months. Based on the follow-up time, data were categorized into short-term (≤4 weeks), medium-term (4–24 weeks), and long-term (≥24 months), followed by subgroup analysis.
For the VAS indicator, significant heterogeneity was detected, necessitating the use of a random-effects model to combine effect sizes. The studies affirmed that SNAGs significantly reduced VAS scores, with an overall combined mean difference (MD) of 1.73 (95% CI: 1.05, 2.40). The MDs for short-term, medium-term, and long-term were 1.83 (95% CI: 0.77, 2.90), 1.26 (95% CI: 0.30, 2.23), and 2.14 (95% CI: 1.74, 2.54), respectively. The relationship between intervention duration and VAS scores post-SNAG and non-SNAG interventions is depicted in Figure 3.
Figure 3

Forest plot of VAS after SNAG and non-SNAG interventions.
For the NDI indicator, significant heterogeneity was also observed, and a random-effects model was employed for combining effect sizes. The studies indicated that SNAGs significantly reduced NDI scores, with an overall combined MD of 8.55 (95% CI: 2.73, 14.37). The MDs for short-term and medium-term were 7.49 (95% CI: 1.53, 13.45) and 12.29 (95% CI: −7.04, 31.62), respectively, with no reports on long-term outcomes. The relationship between intervention duration and NDI scores post-SNAG and non-SNAG interventions is shown in Figure 4.
Figure 4

Forest plot of NDI after SNAG and non-SNAG interventions.
For the FRT indicator, significant heterogeneity was noted, and a random-effects model was utilized for combining effect sizes. The studies demonstrated that SNAGs significantly increased FRT scores, with an overall combined MD of −7.22 (95% CI: −9.38, −5.07). The MDs for short-term, medium-term, and long-term were −5.58 (95% CI: −7.97, −3.19), −9.15 (95% CI: −11.38, −6.91), and −11.00 (95% CI: −12.22, −9.78), respectively. The relationship between intervention duration and FRT scores post-SNAG and non-SNAG interventions is illustrated in Figure 5.
Figure 5
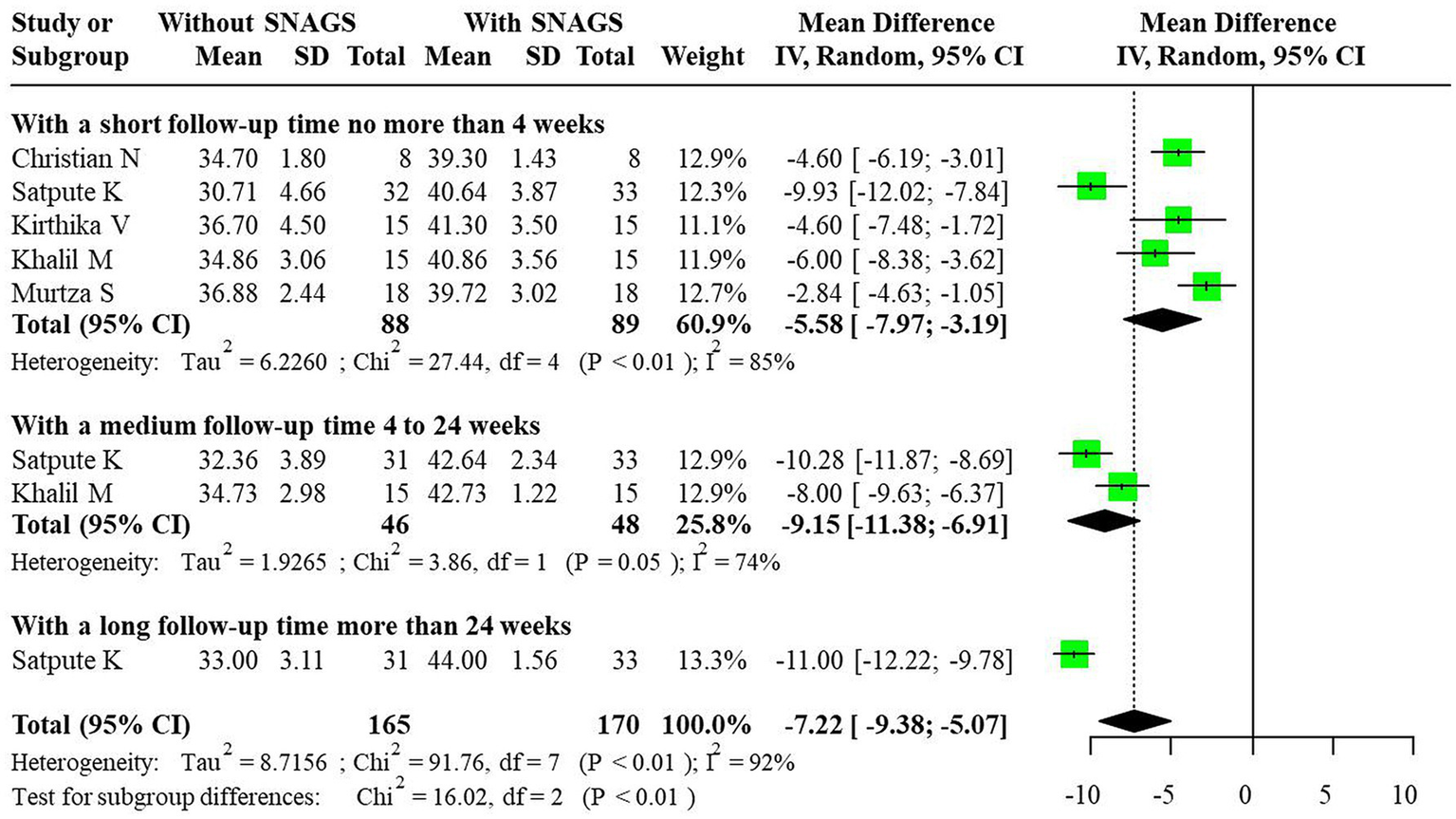
Forest plot of FRT after SNAG and non-SNAG interventions.
Regarding the HDI indicator, significant heterogeneity was observed, prompting the use of a random-effects model to combine effect sizes. The studies revealed that SNAGs significantly reduced HDI scores, with an overall combined MD of 9.29 (95% CI: 3.64, 14.95). The MDs for short-term, medium-term, and long-term were 11.46 (95% CI: 1.89, 21.03), 6.00 (95% CI: 3.96, 8.04), and 7.00 (95% CI: 3.64, 14.95), respectively. The relationship between intervention duration and HDI scores post-SNAG and non-SNAG interventions is shown in Figure 6.
Figure 6
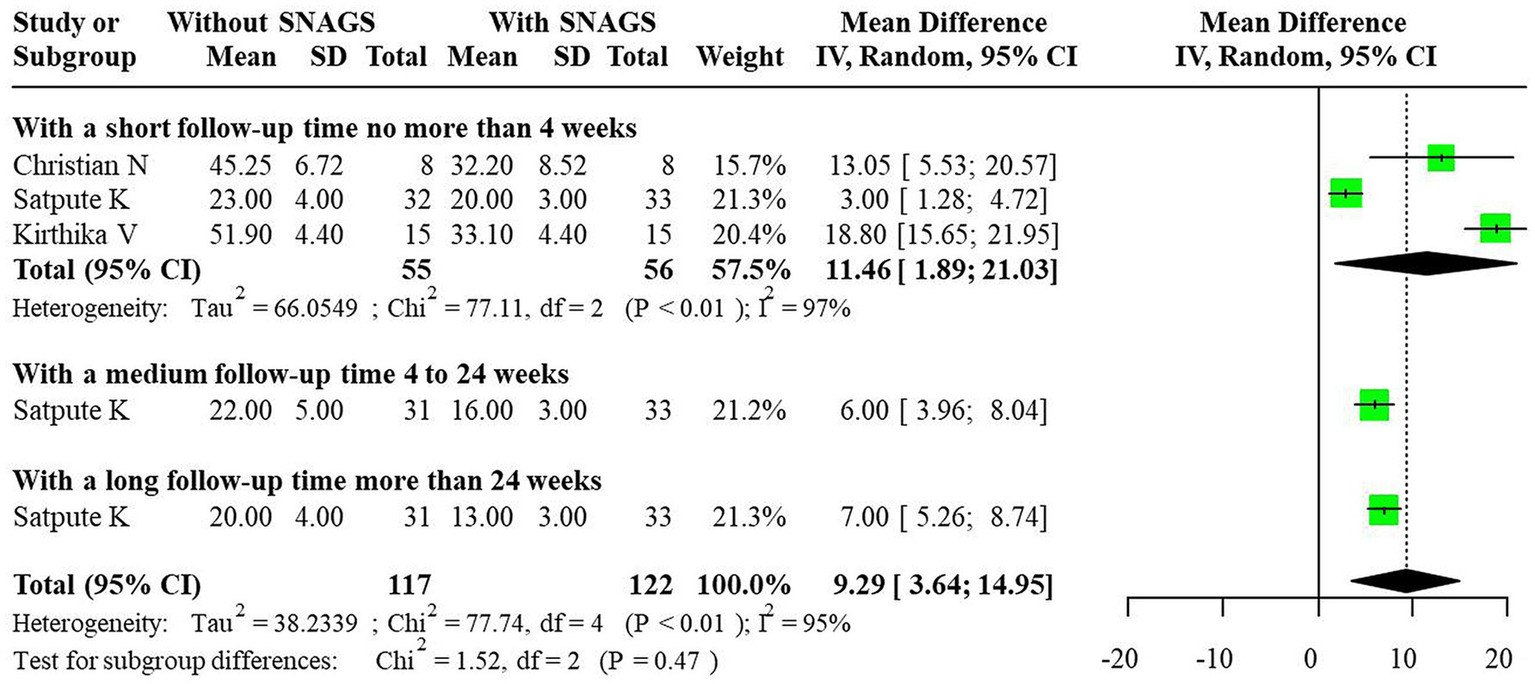
Forest plot of HDI after SNAG and non-SNAG interventions.
A funnel plot was constructed, and visual assessment was employed to evaluate publication bias. The funnel plot for the VAS indicator exhibited symmetry, while those for other indicators displayed some asymmetry, suggesting potential publication bias. The funnel plots for SNAG and non-SNAG indicators are presented in Figure 7.
Figure 7
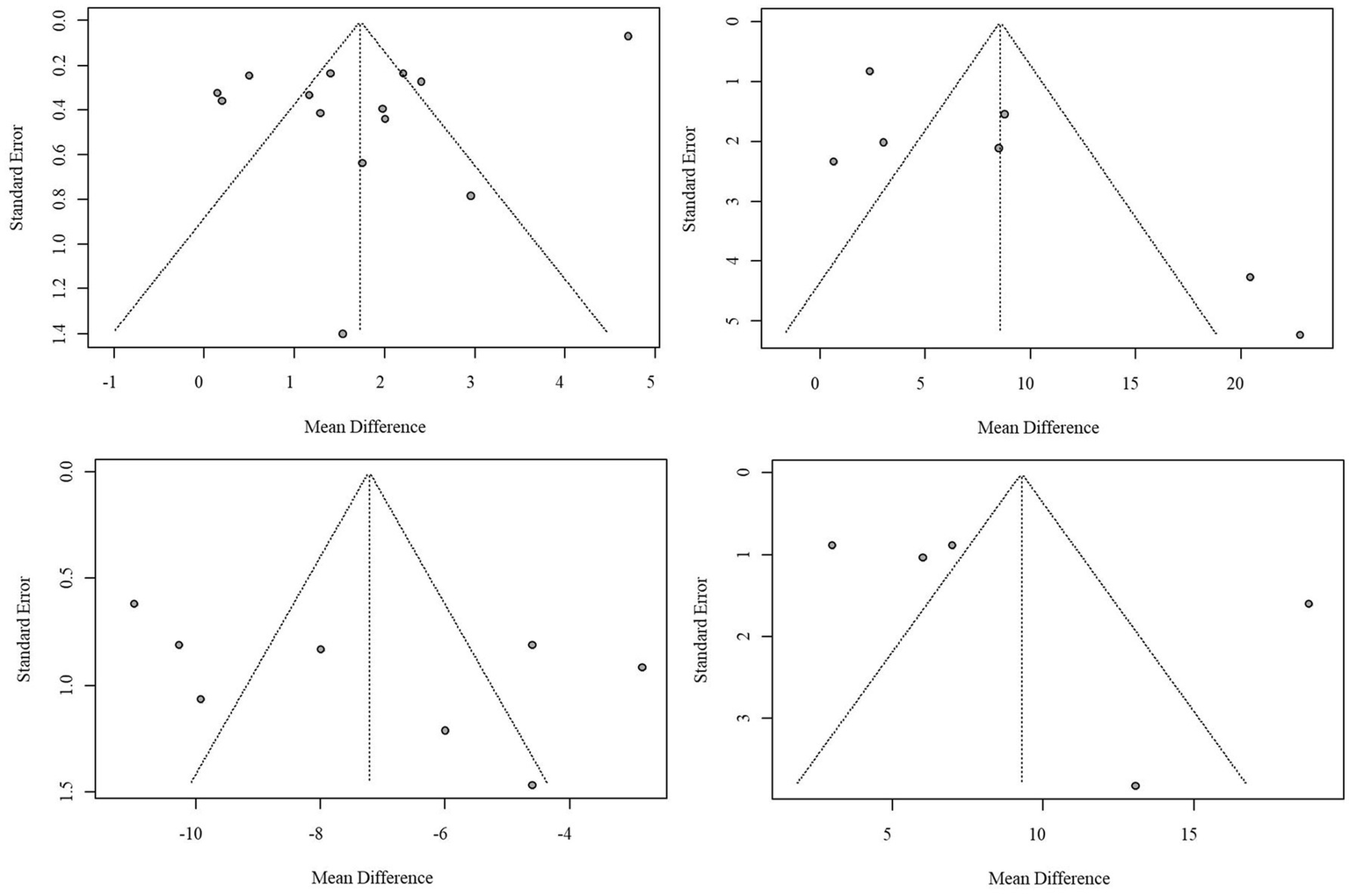
Funnel plot of publication bias in SNAG and non-SNAG indicators.
3.4 Network meta-analysis results of CSM, mobilization, and massage efficacy
Considering VAS and NDI as primary outcome indicators after 4 weeks of intervention, 6 articles reported enhancements in VAS following CSM, Mobilization, and Massage treatments, while 5 articles reported improvements in NDI. Direct comparisons among different intervention methods are summarized in the network relationship diagram for VAS and NDI indicators shown in Figure 8. The thickness of lines in the diagram represents the number of studies, while the size of the nodes indicates the sample size of included studies.
Figure 8

(A) Network plot for VAS outcomes. Direct comparisons of different interventions (CSM: cervical spine manipulation; Mobilization; Massage; Exercise) on visual analog scale (VAS) improvement. Node size represents sample size, and line thickness indicates the number of included studies. (B) Network plot for NDI outcomes. Direct comparisons of different interventions on Neck Disability Index (NDI) improvement. Network structure illustrates pairwise comparisons, with node and line definitions as in (A).
The SUCRA scores for various intervention methods in improving VAS scores were as follows: CSM (98.9%), Mobilization (67.3%), Exercise (21.0%), Massage (12.8%). For improving NDI scores, the SUCRA scores were: CSM (82.2%), Mobilization (57.2%), Exercise (6.7%), Massage (53.9%). CSM demonstrated superior effects in enhancing VAS and NDI. The SUCRA plots for different intervention methods for VAS and NDI indicators are presented in Figure 9.
Figure 9
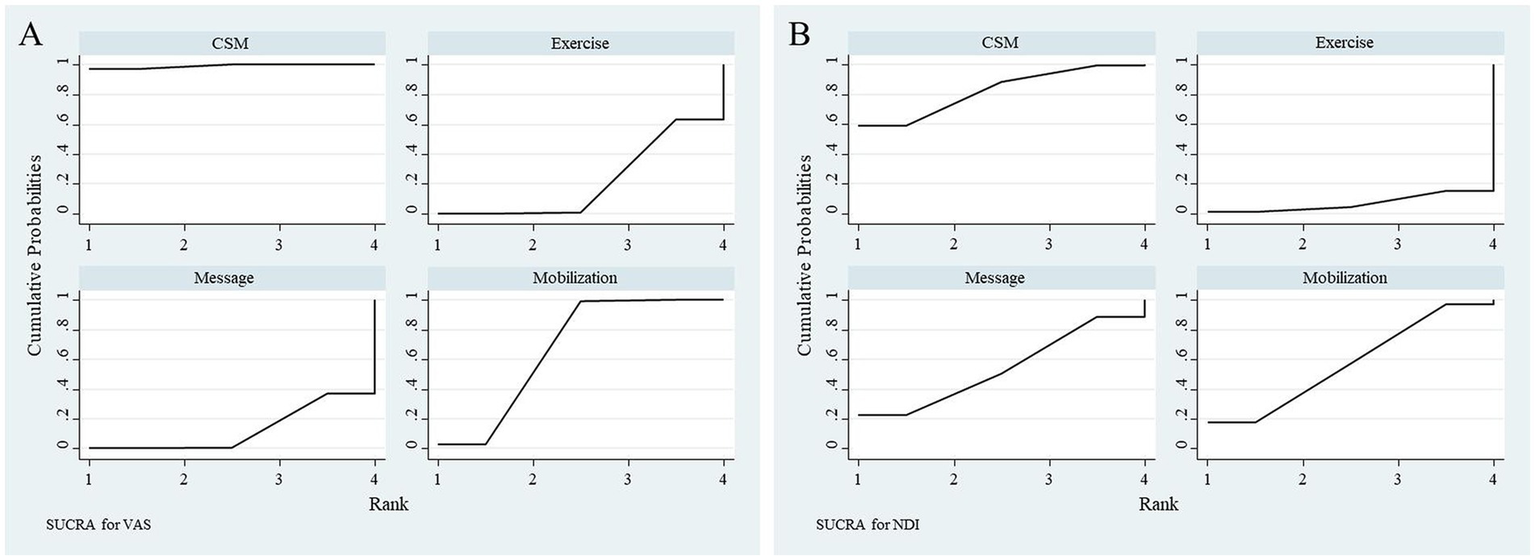
(A) SUCRA ranking for VAS outcomes. Surface Under the Cumulative Ranking (SUCRA) probabilities (0-100%) for interventions, showing cervical spine manipulation (CSM, 98.9%) as the most effective for VAS reduction, followed by mobilization (67.3%). (B) SUCRA ranking for NDI outcomes. SUCRA probabilities rank CSM (82.2%) highest for NDI improvement, with mobilization (57.2%) and massage (53.9%) as secondary options.
CSM significantly outperformed Exercise, Massage, and Mobilization in reducing VAS scores. Compared to Exercise, the MD for VAS scores was 2.29 (95% CI: 1.01, 3.58); compared to Massage, the MD for VAS scores was 2.53 (95% CI: 1.43, 3.64); compared to Mobilization, the MD for VAS scores was 0.90 (95% CI: 0.00, 1.80). Mobilization significantly outperformed Exercise and Massage in reducing VAS scores. Compared to Exercise, the MD for VAS scores was 1.40 (95% CI: 0.26, 2.54); compared to Massage, the MD for VAS scores was 1.63 (95% CI: 0.52, 2.75). The forest plot for VAS scores with different interventions is shown in Figure 10. In reducing NDI scores, CSM significantly outperformed Exercise with an MD of 1.36 (95% CI: 0.08, 2.65), while no significant differences were observed in NDI scores among the other intervention methods. The forest plot for NDI scores with different interventions is shown in Figure 11.
Figure 10
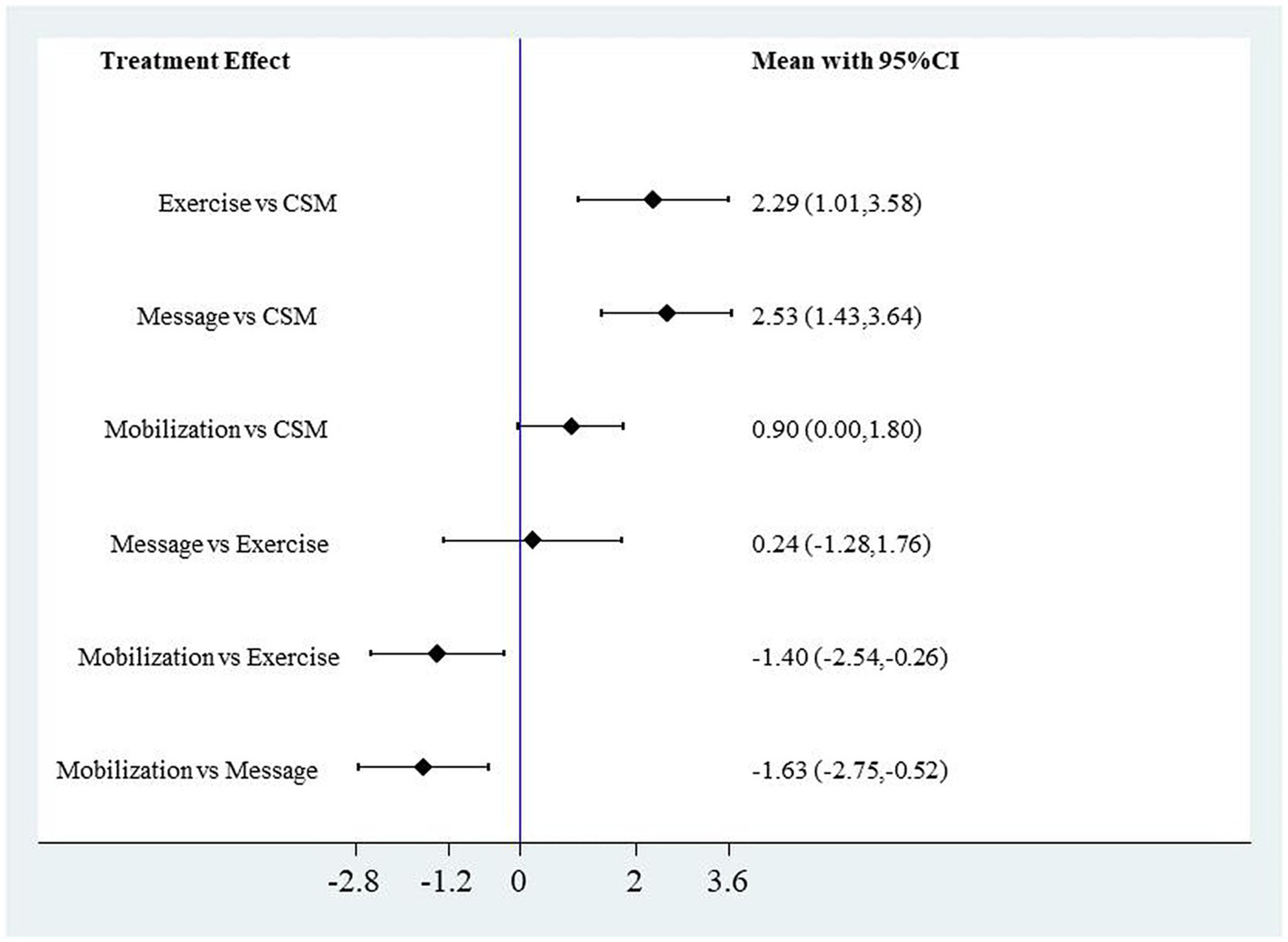
Forest plot of VAS scores for different interventions.
Figure 11

Forest plot of NDI scores for different interventions.
3.5 Comparing safety and effectiveness
3.5.1 Effectiveness
Both cervical and thoracic spinal manipulation, as well as SNAGs, demonstrated strong efficacy in reducing pain, improving cervical range of motion, and decreasing headache frequency. Mobilization, particularly when combined with other therapies such as exercise, also yielded significant positive results. However, spinal manipulation (both cervical and thoracic) tended to provide more pronounced and faster benefits in terms of pain relief and disability reduction.
3.5.2 Safety
Mobilization and SNAGs were among the safest interventions for CGH, with minimal risk of adverse effects. These methods were often preferred for patients who might not tolerate more aggressive manipulation. In contrast, spinal manipulation, particularly in the upper cervical spine, carried slightly higher risks, though these remained generally low and manageable when performed by experienced clinicians.
For patients with CGH, spinal manipulation (cervical and thoracic) and SNAGs proved to be the most effective interventions for pain relief and functional improvement. Mobilization and massage were also effective, especially when integrated with other therapies, but spinal manipulation often delivered faster and more substantial benefits. In terms of safety, mobilization and SNAGs were generally the safer options, with fewer adverse effects, while manipulation remained a highly effective choice when administered by trained professionals (Table 2).
Table 2
| Effectiveness of manipulative interventions for CGH | Study | Findings | Safety concerns |
|---|---|---|---|
| Upper Cervical and Thoracic Manipulation | Dunning JR (25) | The study compared upper cervical and upper thoracic manipulation to mobilization and exercise for CGH. The results showed that manipulation (especially in the cervical and thoracic spine) provided significant improvements in headache frequency and severity compared to mobilization and exercise. This suggests that manipulation might be more effective in reducing CGH symptoms. | Cervical spine manipulation, particularly in the upper segments (C1-C2), can carry a small risk of adverse events, such as vertebral artery dissection or cervical artery damage. However, well-trained practitioners can minimize these risks. The studies generally report low incidence of adverse effects when these techniques are administered by experienced clinicians. |
| Sustained Natural Apophyseal Glides (SNAGs) | Kashif M (26), Shin EJ (33), and several others (21, 27–39) | SNAGs, specifically targeting the upper cervical spine (C1-C2), have been shown to significantly improve both headache intensity and cervical function. The studies demonstrated that SNAGs were effective in reducing the duration of headaches and improving cervical range of motion. SNAGs are particularly beneficial for those with CGH related to restricted cervical mobility. | Mobilization techniques, including SNAGs, are typically associated with fewer risks compared to high-velocity manipulation. These techniques focus on joint mobilization and range of motion rather than high-velocity thrusts. They are generally considered safe and have a low incidence of adverse effects. However, care should still be taken to ensure the appropriate application, particularly for patients with conditions like cervical instability or acute inflammation. Massage therapy is generally considered safe and carries a low risk of adverse effects, particularly when compared to more invasive manual therapies like spinal manipulation. It can be used as an adjunct to other treatments to improve muscle relaxation and alleviate tension in CGH patients. |
| Mobilization vs. Massage Therapy | Youssef EF (29) | The study comparing mobilization and massage therapy found that mobilization was more effective at reducing headache frequency and improving function compared to massage. While massage provided some benefit, mobilization was superior in improving cervical mobility and reducing pain intensity. | |
| Manipulation vs. Mobilization and Exercise | Lerner-Lentz A (21) | This study found that manipulation combined with exercise provided better outcomes in reducing both pain and disability compared to mobilization alone. It highlights the benefit of integrating manipulation with exercise to improve long-term outcomes for CGH. | |
| Thoracic Spine Manipulation | McDevitt AW (30) | Thoracic spine thrust manipulation was found to be effective in alleviating CGH symptoms. The study showed that thoracic manipulation improved headache frequency and severity, supporting the broader role of spinal manipulation techniques beyond just the cervical spine for CGH management. | Thoracic manipulation is considered safer than cervical manipulation in terms of risk to the cervical arteries, and adverse events are rarer. It may also be beneficial for patients who have difficulty tolerating cervical manipulation. |
| Cervical vs. Thoracic Spinal-Thrust Manipulation | Nambi G (31) | This study compared cervical and thoracic spinal thrust manipulation for CGH. It found that both interventions were effective, but cervical manipulation was slightly more effective in reducing headache intensity and improving cervical function. However, thoracic manipulation still showed significant benefits, especially for patients with less cervical mobility. | |
| Mulligan Techniques | Satpute K (32), Kirthika V (34), Khalil M (35) | Mulligan manual therapy techniques, including SNAGs, combined with exercise, significantly reduced headache frequency and intensity. Studies highlighted that Mulligan’s techniques, particularly in combination with exercise, could provide more substantial improvements compared to exercise alone, especially for reducing disability associated with CGH. |
Effectiveness of manipulative interventions for CGH.
4 Discussion
The current investigation represents the first direct comparison of the effects of SNAGS versus non-SNAG interventions on pain, function, and range of motion outcomes in patients with CGH. The results revealed that SNAG mobilization produced statistically significant superior improvements relative to control interventions, including reductions in VAS scores (MD = 1.73, 95%CI: 1.05, 2.40), NDI scores (MD = 8.55, 95%CI: 2.73, 14.37), FRT values (MD = −7.22, 95%CI: −9.38, −5.07), and HDI scores (MD = 9.29, 95%CI: 3.64, 14.95). Notably, these beneficial effects were maintained over time. The heterogeneity in the studies—stemming from variations in manual therapy techniques, treatment protocols (such as frequency and duration), and patient populations—can impact both the reliability and generalizability of the findings. Different therapies and treatment regimens may yield inconsistent results, making it difficult to determine which specific intervention is most effective for CGH. Additionally, the findings from one study may not be applicable to other settings or populations due to differences in patient demographics and the focus of each study. To address this heterogeneity, the article implemented several strategies: standardizing data extraction and outcome measures (such as NDI, VAS, and ROM), assessing bias risk using tools like the Cochrane Risk of Bias Tool, applying the PICOS framework to ensure comparable study features, acknowledging variability in treatment protocols, and possibly using network meta-analysis to synthesize results from different interventions. These measures help improve the consistency and applicability of the findings, despite the differences across studies.
The observed advantages of SNAG mobilization are consistent with Mulligan’s theoretical principles of manual therapy. The SNAG technique involves the application of graded mobilization along the treatment plane of the selected cervical facet joint, from the mid-range to the end-range, with the joint position maintained. This approach is theorized to reduce cervical functional impairment and improve disability by preserving the natural arthrokinematics of the zygapophyseal joints. Additionally, joint mobilization may help decrease adhesions and increase the pain pressure threshold of the paraspinal musculature. The positive effects of SNAG are likely mediated by a reduction in trigeminal cervical nucleus hyperresponsiveness and blockade of A-β fiber stimulation, which can attenuate pain and improve function (15).
The current findings align with a recent meta-analysis of 8 studies (357 participants) demonstrating that SNAG mobilization significantly improved pain, flexion-rotation, and functional outcomes in CGH patients (16). The analgesic and functional benefits of SNAG may be attributed to the stimulation of inhibitory pathways in the spinal cord and activation of descending inhibitory mechanisms in the lateral gray area around the midbrain aqueduct (17, 18).
The network meta-analysis component of this study compared the relative effects of cervical spine manipulation (CSM), mobilization, massage, and exercise on 4-week VAS and NDI outcomes. The rankwise SUCRA scores indicated that CSM had the best effects on improving both VAS (98.9%) and NDI (82.2%), suggesting it may be the most effective intervention for reducing pain and disability in CGH. CSM demonstrated significantly greater reductions in VAS compared to exercise, massage, and mobilization, while mobilization was superior to exercise and massage. For NDI, CSM was significantly better than exercise, but there were no other between-group differences.
CSM, mobilization, and massage represent common manual therapy approaches for CGH, with massage and exercise being established standard treatments (19). The rationale for CSM is that the high-velocity, low-amplitude thrust can significantly improve spinal posture and function by applying corrective forces to dysfunctional joint segments, thereby relieving pain and catalyzing the body’s natural healing processes (20). However, the literature lacks clear guidance on the optimal choice between CSM and mobilization. Interestingly, when clinician decision-making determines the interventions, the effects of CSM and mobilization appear similar, suggesting the experience and skill level of the provider may be a key determinant of outcomes (21, 22).
Several limitations warrant consideration. Both components of this study exhibited substantial heterogeneity, with variability in the frequency, duration, and nature of spinal interventions across studies. This lack of standardization complicates the translation of findings to clinical practice. Additionally, while the network meta-analysis allowed for comparative evaluation of several manual therapy modalities, the large differences between sham/control groups precluded the inclusion of SNAG, thereby limiting the comprehensiveness of the analysis.
The skill level of clinical experts can be quantified through several measures: the number of years a clinician has been practicing or the number of similar cases they have treated can give an indication of their expertise. Experience could be categorized into levels (e.g., novice, intermediate, advanced) and factored into research analysis. Certification and Training: clinicians who have additional certifications or specialized training (e.g., manual therapy certifications, advanced physiotherapy training) could be considered more skilled. Researchers could document and assess the types of training and professional development the clinicians have undergone. Standardized Skill Assessment: tools like the clinical competency examination or performance-based assessments can objectively assess the clinician’s manual therapy skills. These could include assessments of technique precision, patient interaction, and the application of evidence-based practices. Patient outcomes: an indirect measure of skill could be the clinician’s track record in improving patient outcomes, such as pain reduction, mobility improvement, or patient satisfaction. These could be tracked using outcome measures like the NDI or VAS.
To enhance the validity and reliability of future research, several methodological improvements should be considered regarding clinician training, standardization, and skill assessment. Clinician training and standardization: future studies should ensure that all clinicians involved in the study meet a standardized level of competence. This could be achieved by requiring participants to have a minimum number of hours in specific training programs or certifications related to the intervention being tested. Clinician matching across groups: to control for skill variability, studies could match clinicians across the experimental and control groups. For example, clinicians with similar levels of experience and expertise should treat both groups to minimize the impact of skill differences on treatment outcomes. Incorporating clinician skill as a variable: researchers should explicitly assess and report clinician skill level as a variable in their studies. This could involve documenting qualifications, years of experience, and certification levels, and then analyzing how these factors might influence treatment outcomes. Blinding and external review: to ensure consistency, independent external experts could review the treatment techniques and outcomes. This could provide an objective evaluation of whether treatment techniques are being applied as intended and if the clinician’s skill is impacting the results. Randomized assignment of clinicians: by randomly assigning patients to clinicians with different levels of expertise, researchers can analyze how variations in clinician skill affect treatment outcomes. This could also help in identifying the most effective clinical practices for specific techniques.
Studies on the correlation between X-ray findings and head and neck symptoms have important implications for the clinical use of manual therapy, especially in treating conditions like CGH (23, 24). X-ray imaging often reveals structural abnormalities, such as spinal misalignments, degenerative changes, or facet joint dysfunction, which may correlate with symptoms like pain, stiffness, and headaches. If a strong correlation is found between X-ray abnormalities (e.g., disc degeneration or misalignments) and symptoms, clinicians may place more focus on these factors when selecting manual therapy techniques. X-ray results can help clinicians tailor treatment plans based on structural findings. For example, if issues like joint dysfunction or facet joint problems are identified, clinicians may prioritize joint mobilizations or spinal manipulation over techniques like massage. In cases where postural issues are evident, manual therapy combined with posture correction exercises may be emphasized. When X-ray findings show a correlation with persistent or severe symptoms, it suggests that manual therapies such as spinal manipulation or mobilization could be more effective for these patients, potentially improving pain relief and functionality. Conversely, when there’s minimal correlation between X-ray findings and symptoms, soft tissue techniques like massage or muscle energy techniques may be just as beneficial, highlighting the importance of a comprehensive approach to manual therapy. X-ray imaging also helps in identifying contraindications or red flags, such as fractures or tumors, which may require modifications to treatment plans. For example, patients with severe degenerative changes might benefit more from gentle mobilizations rather than high-velocity manipulations, reducing the risk of harm. The integration of X-ray results into the overall diagnostic process can enhance treatment planning. It underscores that manual therapy should not be based solely on symptoms like pain, but should also consider underlying structural contributors. Additionally, X-rays can serve as a monitoring tool, helping clinicians track the progression of structural changes in patients with chronic conditions like CGH. This allows for adjustments in treatment to address any new complications or degeneration over time. In some cases, when X-rays indicate that structural abnormalities do not correlate with symptoms, clinicians may focus on alternative therapies such as exercise, posture correction, or ergonomic adjustments, with manual therapy being used more as an adjunct. Here, the emphasis shifts toward preventive measures to address lifestyle factors that may contribute to poor posture or movement patterns.
The small sample sizes and potential selection biases in these studies significantly limit the ability to generalize their findings to the broader CGH patient population. While the studies provide important insights into the effectiveness of manual therapy interventions, their conclusions should be interpreted cautiously. Larger, more diverse studies with more robust sampling strategies would help improve the external validity and reliability of the findings, allowing for more confident recommendations that can be applied to the wider CGH population in clinical settings.
5 Conclusion
In conclusion, this investigation provides evidence that SNAG mobilization can significantly improve pain, function, and range of motion in patients with CGH, with durable benefits over time. Moreover, the network meta-analysis suggests that CSM may be the most effective short-term intervention for reducing pain and disability in this population, although clinician expertise appears to be an important factor. Future research is needed to establish optimal dosing and standardization of spinal manual therapies for CGH.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XX: Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. YL: Conceptualization, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the study on the correlation between positive signs on X-ray of the upper neck segment and head and neck symptoms, Specialized Project of Traditional Chinese Medicine Research in Sichuan Province, 2024MS192.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer JZ declared a shared parent affiliation with the author YL to the handling editor at the time of review.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Verma S Tripathi M Chandra PS . Cervicogenic headache: current perspectives. Neurol India. (2021) 69:S194–8. doi: 10.4103/0028-3886.315992
2.
Bogduk N Govind J . Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol. (2009) 8:959–68. doi: 10.1016/S1474-4422(09)70209-1
3.
Piovesan EJ Utiumi MAT Grossi DB . Cervicogenic headache - how to recognize and treat. Best Pract Res Clin Rheumatol. (2024) 38:101931. doi: 10.1016/j.berh.2024.101931
4.
Demont A Lafrance S Benaissa L Mawet J . Cervicogenic headache, an easy diagnosis? A systematic review and meta-analysis of diagnostic studies. Musculoskelet Sci Pract. (2022) 62:102640. doi: 10.1016/j.msksp.2022.102640
5.
Garcia JD Arnold S Tetley K Voight K Frank RA . Mobilization and manipulation of the cervical spine in patients with cervicogenic headache: any scientific evidence?Front Neurol. (2016) 7:40. doi: 10.3389/fneur.2016.00040
6.
Chaibi A Knackstedt H Tuchin PJ Russell MB . Chiropractic spinal manipulative therapy for cervicogenic headache: a single-blinded, placebo, randomized controlled trial. BMC Res Notes. (2017) 10:310. doi: 10.1186/s13104-017-2651-4
7.
Demont A Lafrance S Gaska C Kechichian A Bourmaud A Desmeules F . Efficacy of physiotherapy interventions for the management of adults with cervicogenic headache: a systematic review and meta-analyses. PM R. (2023) 15:613–28. doi: 10.1002/pmrj.12856
8.
Hearn A Rivett DA . Cervical SNAGs: a biomechanical analysis. Man Ther. (2002) 7:71–9. doi: 10.1054/math.2002.0440
9.
Fernández-de-las-Peñas C Cuadrado ML . Therapeutic options for cervicogenic headache. Expert Rev Neurother. (2014) 14:39–49. doi: 10.1586/14737175.2014.863710
10.
Anandkumar S . The effect of sustained natural apophyseal glide (SNAG) combined with neurodynamics in the management of a patient with cervical radiculopathy: a case report. Physiother Theory Pract. (2015) 31:140–5. doi: 10.3109/09593985.2014.971922
11.
Reid SA Rivett DA Katekar MG Callister R . Sustained natural apophyseal glides (SNAGs) are an effective treatment for cervicogenic dizziness. Man Ther. (2008) 13:357–66. doi: 10.1016/j.math.2007.03.006
12.
Aslıyüce YÖ Ülger Ö . Mulligan mobilization for cervicogenic headache - a systematic review. Int J Osteopathic Med. (2022) 43:31–8. doi: 10.1016/j.ijosm.2022.03.002
13.
Blumenfeld A Siavoshi S . The challenges of cervicogenic headache. Curr Pain Headache Rep. (2018) 22:47. doi: 10.1007/s11916-018-0699-z
14.
Hall TM Robinson KW Fujinawa O Akasaka K Pyne EA . Intertester reliability and diagnostic validity of the cervical flexion-rotation test. J Manip Physiol Ther. (2008) 31:293–300. doi: 10.1016/j.jmpt.2008.03.012
15.
Andrews DP Odland-Wolf KB May J Baker R Nasypany A Dinkins EM . Immediate and short-term effects of mulligan concept positional sustained natural apophyseal glides on an athletic young-adult population classified with mechanical neck pain: an exploratory investigation. J Man Manip Ther. (2018) 26:203–11. doi: 10.1080/10669817.2018.1460965
16.
Cardoso R Seixas A Rodrigues S Moreira-Silva I Ventura N Azevedo J et al . The effectiveness of sustained natural apophyseal glide on flexion rotation test, pain intensity, and functionality in subjects with cervicogenic headache: a systematic review of randomized trials. Arch Physiother. (2022) 12:20. doi: 10.1186/s40945-022-00144-3
17.
Chu J Allen DD Pawlowsky S Smoot B . Peripheral response to cervical or thoracic spinal manual therapy: an evidence-based review with meta analysis. J Man Manip Ther. (2014) 22:220–9. doi: 10.1179/2042618613Y.0000000062
18.
Mata JZ Azkue JJ Bialosky JE Saez M López ED Arrieta MA et al . Restoration of normal central pain processing following manual therapy in nonspecific chronic neck pain. PLoS One. (2024) 19:e0294100. doi: 10.1371/journal.pone.0294100
19.
Page P . Cervicogenic headaches: an evidence-led approach to clinical management. Int J Sports Phys Ther. (2011) 6:254–66. doi: 10.1186/s13063-021-05690-y PMID:
20.
Fleming R Forsythe S Cook C . Influential variables associated with outcomes in patients with cervicogenic headache. J Man Manip Ther. (2007) 15:155–64. doi: 10.1179/106698107790819846
21.
Lerner-Lentz A O'Halloran B Donaldson M Cleland JA . Pragmatic application of manipulation versus mobilization to the upper segments of the cervical spine plus exercise for treatment of cervicogenic headache: a randomized clinical trial. J Man Manip Ther. (2021) 29:267–75. doi: 10.1080/10669817.2020.1834322
22.
Kent P Marks D Pearson W Keating J . Does clinician treatment choice improve the outcomes of manual therapy for nonspecific low back pain? A metaanalysis. J Manipulative Physiol Ther. (2005) 28:312–22. doi: 10.1016/j.jmpt.2005.04.009
23.
Bini P Hohenschurz-Schmidt D Masullo V Pitt D Draper-Rodi J . The effectiveness of manual and exercise therapy on headache intensity and frequency among patients with cervicogenic headache: a systematic review and meta-analysis. Chiropr Man Therap. (2022) 30:49. doi: 10.1186/s12998-022-00459-9
24.
Núñez-Cabaleiro P Leirós-Rodríguez R . Effectiveness of manual therapy in the treatment of cervicogenic headache: a systematic review. Headache. (2022) 62:271–83. doi: 10.1111/head.14278
25.
Dunning JR Butts R Mourad F Young I Fernandez-de-Las Peñas C Hagins M et al . Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC Musculoskelet Disord. (2016) 17:64. doi: 10.1186/s12891-016-0912-3
26.
Kashif M Manzoor N Safdar R Khan H Farooq M Wassi A . Effectiveness of sustained natural apophyseal glides in females with cervicogenic headache: a randomized controlled trial. J Back Musculoskelet Rehabil. (2022) 35:597–603. doi: 10.3233/BMR-210018
27.
Christian N . Comparative study to find the effect of Mulligan’s snag technique (C1-C2) versus Maitland’s technique (C1-C2) in Cervicogenic headache among information technology professionals. Int J Physiother. (2017) 4:178–83. doi: 10.15621/ijphy/2017/v4i3/149071
28.
Malo-Urriés M Tricás-Moreno JM Estébanez-de-Miguel E Hidalgo-García C Carrasco-Uribarren A Cabanillas-Barea S . Immediate effects of upper cervical translatoric mobilization on cervical mobility and pressure pain threshold in patients with cervicogenic headache: a randomized controlled trial. J Manip Physiol Ther. (2017) 40:649–58. doi: 10.1016/j.jmpt.2017.07.007
29.
Youssef EF Shanb AS . Mobilization versus massage therapy in the treatment of cervicogenic headache: a clinical study. J Back Musculoskelet Rehabil. (2013) 26:17–24. doi: 10.3233/BMR-2012-0344
30.
McDevitt AW Cleland JA Rhon DI Altic RAK Courtney DJ Glynn PE et al . Thoracic spine thrust manipulation for individuals with cervicogenic headache: a crossover randomized clinical trial. J Man Manip Ther. (2022) 30:78–95. doi: 10.1080/10669817.2021.1947663
31.
Nambi G Alghadier M Eltayeb MM Aldhafian OR Saleh AK Alsanousi N et al . Comparative effectiveness of cervical vs thoracic spinal-thrust manipulation for care of cervicogenic headache: a randomized controlled trial. PLoS One. (2024) 19:e0300737. doi: 10.1371/journal.pone.0300737
32.
Satpute K Bedekar N Hall T . Mulligan manual therapy added to exercise improves headache frequency, intensity and disability more than exercise alone in people with cervicogenic headache: a randomised trial. J Physiother. (2024) 70:224–33. doi: 10.1016/j.jphys.2024.06.002
33.
Shin EJ Lee BH . The effect of sustained natural apophyseal glides on headache, duration and cervical function in women with cervicogenic headache. J Exerc Rehabil. (2014) 10:131–5. doi: 10.12965/jer.140098
34.
Kirthika VS Kumar V Kuppuswamy P . Is mulligan’s sustained natural apophyseal glides (Snags) or muscle energy technique is effective in the non-surgical management of cervicogenic headache? A two-group pretest-posttest randomized controlled trial. Asian J Pharm Clin Res. (2018) 11:230. doi: 10.22159/ajpcr.2018.v11i9.26808
35.
Khalil M Alkhozamy H Fadle S Hefny A Ismail M . Effect of mulligan upper cervical manual traction in the treatment of cervicogenic headache: a randomized controlled trial. Physiother Q. (2019) 27:13–20. doi: 10.5114/pq.2019.87738
36.
Murtza S Noor R Bashir MS Ikram M . Effects of sustained natural apophyseal glides versus rocabado 6 × 6 program in subjects with cervicogenic headache. BMC Musculoskelet Disord. (2024) 25:169. doi: 10.1186/s12891-024-07290-8
37.
Jin X Du HG Kong N Shen JL Chen WJ . Clinical efficacy of the mulligan maneuver for cervicogenic headache: a randomized controlled trial. Sci Rep. (2023) 13:22034. doi: 10.1038/s41598-023-48864-1
38.
Rani M Kaur J . Effectiveness of different physiotherapy interventions in the management of cervicogenic headache: a pilot randomized controlled trial. J Man Manip Ther. (2022) 30:96–104. doi: 10.1080/10669817.2021.1962687
39.
Hall T Chan HT Christensen L Odenthal B Wells C Robinson K . Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. J Orthop Sports Phys Ther. (2007) 37:100–7. doi: 10.2519/jospt.2007.2379
Summary
Keywords
cervicogenic headache, Neck Disability Index, Flexion-Rotation Test, manual therapy, meta-analysis
Citation
Xu X and Ling Y (2025) Comparative safety and efficacy of manual therapy interventions for cervicogenic headache: a systematic review and network meta-analysis. Front. Neurol. 16:1566764. doi: 10.3389/fneur.2025.1566764
Received
25 January 2025
Accepted
22 April 2025
Published
16 May 2025
Volume
16 - 2025
Edited by
Jun Zhong, Shanghai Jiao Tong University, China
Reviewed by
Jun Zhu, Chengdu University of Traditional Chinese Medicine, China
Youkang Dong, Yunnan University of Traditional Chinese Medicine, China
Updates
Copyright
© 2025 Xu and Ling.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Ling, 13881816924@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.