Abstract
Background:
Clinical practice guidelines (CPGs) have an indispensable role in guiding the selection of various non-pharmaceutical interventions (NPIs) for post-stroke emotional disorders (PSED). However, little is known about their quality and recommendations. This study aims to critically appraise the quality of existing NPIs for PSED CPGs and extract relevant recommendations, present the research distribution of various NPIs in an evidence map, and assist clinicians in making decisions.
Methods:
A systematic search was undertaken in PubMed, Embase, CINAHL, Web of Science, China National Knowledge Infrastructure, Wanfang, VIP, SinoMed, and international guideline developing institutions from origin to November 20, 2024, to identify the CPGs on NPIs for PSED. The CPGs finally selected were blindly evaluated by two reviewers using the Appraisal of Guidelines Research & Evaluation (AGREE) II instrument and the reporting quality was evaluated using the RIGHT statement. The overall agreement among reviewers was analyzed using intraclass correlation coefficient (ICC).
Results:
Nine guidelines were included and evaluated. Two CPGs were grade A (recommended) and seven CPGs were grade B (recommended with modification). The reporting rate of RIGHT ranged from 40.00 to 80.00%. Nine NPIs were extracted, and there were similarities and differences between the recommendations.
Conclusion:
This study provides specific direction for improving the quality of CPGs for NPIs for PSED, and provides useful information for clinicians and stakeholders, and provides a basis for clinical decision-making.
1 Introduction
Cerebral stroke is the second largest cause of death worldwide, accounting for 11.6% of the total number of deaths (1). It is characterized by a high incidence, high recurrence rate, high disability rate and high mortality rate, leading to an increased burden of disease around the world (1). Post-stroke emotional disorder (PSED) is one of the most common and serious complications, commonly occurring at all stages of the disease and its pathogenesis is still unclear (2). It includes post stroke depression (PSD), post-stroke anxiety (PSA), post-stroke comorbid anxiety and depression (PSCAD), post-stroke emotional imbalance (PSEI) and post-stroke anger proneness (PSAP) (3). Approximately one-third of stroke survivors develop some form of emotional disorder (2–4). Studies have shown (5, 6) that emotional disorders are closely related to patients’ prognosis. If patients are not treated in time, it will affect the recovery of neurological function and the ability to return to society, and even lead to increased mortality. There is no universally effective method for the treatment of PSED, and although drug therapy has a certain effect, there are many side effects (7). Some systematic reviews and meta-analyses have shown that non-pharmaceutical interventions (NPIs) can effectively reduce emotional symptoms and improve patient’s quality of life (7–9). Many authoritative organizations have issued a number of CPGs related to the treatment and rehabilitation of Stroke, which contain NPIs to help health care workers and patients to make local health care decisions (10).
The purpose of this study is to evaluate the quality of guidelines related to NPIs for PSED, to make relevant recommendations for NPIs use in PSED, to provide information for standardized practice and management, to identify potential directions that CPGs should focus on in the future, and to provide a reference for relevant policy development and clinical practice.
2 Materials and methods
2.1 Search strategy
We systematically searched the following databases: PubMed, Web of Science, Embase, CINAHL, China National Knowledge Infrastructure (CNKI), Wanfang, VIP, SinoMed, YiMaiTong. We also hand-searched 6 databases of international guideline developing institutions: Guideline International Network (GIN), Registered Nurses’ Association of Ontario (RNAO), Scottish Intercollegate Guidelines Network (SIGN), National Institute for Health and Care Excellence (NICE), National Guideline Clearinghouse (NGC), and New Zealand Guidelines Group (NZGG). Articles were retrieved by combining subject terms and free terms, from origin to November 20, 2024. The full search strategies are shown in Supplementary material 1.
2.2 Study selection
In our study, the inclusion criteria were: guidelines which provided recommendations regarding NPIs for PSED and included access to the full text. Both evidence-based clinical practice guidelines and consensus-based clinical practice guidelines (EB-CPGs and CB-CPGs) were included, and the guidelines had to at least contain details of evidence retrieval and literature evaluation. We have described both consensus statements and expert opinions as CB-CPGs (11). The CPGs had to include NPIs for PSED. The most commonly included NPIs were: psychotherapy, social support therapy, traditional Chinese medicine non-pharmacological therapies, and physical therapy (12). If guidelines were available in multiple languages (such as English and Chinese), only the version in the original language was eligible for inclusion. In cases of updated guidelines, only the most recent version was considered. Exclusion criteria were editorial or correspondence articles that summarized organizational clinical practice guidelines.
2.3 Data extraction
Two reviewers (LY and ZJ) screened all references independently, and any ambiguities were resolved by a third reviewer (LJJ). The two reviewers developed a purpose-designed data extraction sheet covering the basic characteristics, which included the following: title, guideline development institution, publication year, development country, guideline type, journal, target population, number of references and funding support. This was used to record extracted NPIs for PSED both where there was a clear level of evidence or recommendation and also where suggested or conclusive intervention methods were concealed within the paragraphs of guidelines written in flowing text format.
2.4 Guideline quality assessment
The methodological quality of the guidelines was evaluated by two experienced reviewers (LY and ZJ) using the Application of Guidelines for Research and Evaluation (second version) (AGREE II) (10), which consists of 23 items organized into the six domains. In case of disagreement, the decision was made after discussion with a third reviewer (ZD). The standardized scores for each of the individual AGREE domains were calculated: a higher score indicates a higher quality of the domain.1 According to the standardized score of each field in the guide, the recommendations were divided into three levels: ≥60% of 6 domains were rated as Grade A (recommended); more than three domains with≥30%, but less than< 60% domains were rated as Grade B (recommended with modifications); more than three domains with <30% were rated as Grade C (not recommended) (13–15).
Two reviewers (LY and ZJ) were trained to independently assess the reporting quality appraisals of CPGs using the Reporting Items for practice Guidelines in Healthcare (RIGHT) checklist (16), which consists of 35 sub-items grouped into seven domains and the criteria for assessing the items are “Yes” (guideline reported majority information), “No” (relevant information on the item was not reported), and “NA” (not applicable, the item did not need to be evaluated due to certain characteristics of the guideline). Any inconsistency was resolved by a third reviewer (ZD) after a thorough discussion by the two reviewers. We calculated the domain reporting rate for each included guideline, and calculated the mean reporting rate of each domain for all included guidelines (17–19).
2.5 Data synthesis and analysis
The reviewers thoroughly read, carefully understood, and accurately interpreted the implications of the recommendations regarding NPIs for PSED, and then classified them into different themes based on their characteristics. Both the evidence quality and the recommendation strength of the same NPIs were compared and analyzed. We used visual clinical pathways to display NPIs related to different emotional states and utilized Intraclass Correlation Coefficients (ICCs) to evaluate the level of consistency and reliability between the two researchers (20). The degree of agreement could be classified into poor (<0.40), moderate (0.40–0.75), good (≥0.75) (21, 22). Data were entered using an excel form and data analysis was performed using the “SPSSAU Data Analysis Platform.”2 A bubble plot was designed to comprehensively display the overall quality of each eligible CPG, the X-axis denoted the average reporting rate of the RIGHT checklist, and the Y-axis listed the AGREE II total score. An evidence map was used to summarize the strength distribution of the guideline recommendations.
3 Results
3.1 Search results
A total of 276 records were retrieved through the literature search. There were 166 duplicates, and 33 irrelevant records: nine CPGs (23–31) proved eligible (Figure 1). Five of these were EB-CPGs (23, 24, 27, 28, 30) and four were CB-CPGs (25, 26, 29, 31). Table 1 presents the characteristics of the eligible CPGs.
Figure 1

Flow diagram of literature screening.
Table 1
| Developer and Guideline, year | Journal | Country | Guideline type | Target user | Number of References | Funding source |
|---|---|---|---|---|---|---|
| UWHMC, 2012 (26) | Journal of general internal medicine | United States | EB-CPGs | Healthcare providers | 67 | None |
| AHA/ASA, 2017 (27) | Stroke | United States | EB-CPGs | Healthcare providers | 102 | None |
| CSPM, 2018 (28) | Brazilian Journal of Psychiatry | China | CB-CPGs | Stroke clinicians and related workers | 126 | Jiangsu Provincial Special Program of Medical Science |
| CGHCMRA, 2019 (29) | Chinese Journal of Geriatric Care | China | CB-CPGs | Rehabilitation physician | 43 | None |
| CSC, 2020 (30) | International Journal of Stroke | Canada | EB-CPGs | Healthcare professionals and system leaders | 106 | Heart and Stroke Foundation, Canada |
| CSA, 2020 (31) | Stroke and Vascular Neurology | China | EB-CPGs | Healthcare professionals | 46 | Chinese Stroke Association Guidelines Writing Committee |
| HMHA, 2020 (34) | Journal of Clinical Psychosomatic Diseases | China | CB-CPGs | Stroke clinicians | 34 | None |
| CBNIRC, 2022 (33) | Indian Journal of Psychiatry | India | EB-CPGs | Psychiatry | 110 | None |
| BCPA, 2023 (36) | Chinese Journal of Stroke | China | CB-CPGs | Stroke clinicians | 6 | National Key Research and Development Program of China |
Characteristics of eligible guidelines.
UWHMC, University of Washington Harborview Medical Center; AHA/ASA, Heart Association/American Stroke Association; CSPM, Chinese Society of Psychosomatic Medicine; CGHCMRA, Chinese Geriatric Health Care and Medical Research Association; CSC, Canadian Stroke Consortium; CSA, Chinese Stroke. Association; CHMHA, Chinese Henan Mental Health Association; CBNIRC, Clinical Brain Neuropsychiatric Institute and Research Center; BCPA, Beijing Cerebrovascular disease Prevention Association.
3.2 Quality of CPGs
The overall quality of the included guidelines was acceptable, two of which were rated as grade A, and seven were rated as grade B. The results of the AGREE II score are shown in Table 2. The details of the AGREE II scores are reported in Supplementary material 2. Since there were no uniform criteria according to AGREE II instrument and other previous studies had defined a uniform criterion for overall quality (23, 32). We defined domains with scores <50% as lower scores, 50–70% as moderate, and >70% as high scores. Among the six domains of AGREE II, Domain 1 (Scope and Purpose), Domain four (Clarity of Presentation) and Domain six (Editorial Independence) scores were relatively high. Scores were moderate in Domain two (Stakeholder Involvement), 44.44% of CPGs scores <60%, mainly due to “The views and preferences of the target population (patients, public, etc.) have been sought” had low scores, indicating that these CPGs did not adequately take into account the values and preferences of the patients in their development. Domain five (Applicability) domain scores have been scored relatively low, because the CPGs did not adequately describe the advantages and disadvantages in the application process or specify implementation strategies, etc. Domain three (Rigor of Development) had the lowest score compared with other domains. In this domain, 66.67% of the guidelines scored < 60%. This was mainly due to poor rigor in the formulation of the guidelines. There was a lack of detailed description of the methods for forming recommendations, the strength of recommendations, the level of supporting evidence, the external review process before publication of the guidelines, and the steps for updating the guidelines. The ICC statistics for the assessment between the two reviewers regarding the AGREE II domains varied from 0.61 to 0.98 (p < 0.001), reflecting that inter-rater reliability was good to excellent.
Table 2
| Guideline, year | Scope and purpose | Stakeholder involvement | Rigor of development | Clarity of presentation | Applicability | Editorial independence | The number of domains with standardized scores ≥ 60% | ICC | p | Strength of recommendation |
|---|---|---|---|---|---|---|---|---|---|---|
| UWHMC, 2012 (26) | 88.89 | 47.22 | 43.75 | 88.89 | 22.92 | 87.50 | 3 | 0.79 | <0.001 | B |
| AHA/ASA, 2017 (27) | 97.22 | 61.11 | 65.63 | 88.89 | 52.08 | 87.50 | 5 | 0.83 | <0.001 | B |
| CSPM, 2018 (28) | 91.67 | 41.67 | 19.79 | 80.56 | 33.33 | 91.67 | 3 | 0.52 | <0.001 | B |
| CGHCMRA, 2019 (29) | 91.67 | 66.67 | 29.17 | 88.89 | 50.00 | 87.50 | 4 | 0.77 | <0.001 | B |
| CSC, 2020 (30) | 100.00 | 72.22 | 97.92 | 100.00 | 81.25 | 95.83 | 6 | 0.98 | <0.001 | A |
| CSA, 2020 (31) | 91.67 | 77.78 | 66.67 | 91.67 | 60.41 | 91.67 | 6 | 0.97 | <0.001 | A |
| HMHA, 2020 (34) | 91.67 | 52.78 | 9.38 | 91.67 | 37.50 | 79.17 | 3 | 0.79 | <0.001 | B |
| CBNIRC, 2022 (33) | 100.00 | 52.78 | 38.54 | 80.56 | 43.75 | 87.50 | 3 | 0.79 | <0.001 | B |
| BCPA, 2023 (36) | 86.11 | 77.78 | 20.83 | 91.67 | 41.67 | 79.17 | 4 | 0.61 | <0.001 | B |
| Mean ± SD | 93.21 ± 4.83 | 61.11 ± 13.32 | 43.52 ± 28.41 | 89.20 ± 5.96 | 46.99 ± 16.90 | 87.50 ± 5.51 | - | - | - | - |
Standardized scores of guidelines as measured by AGREE II instrument.
The overall RIGHT reporting rate of the nine guidelines ranged from 40.00% to 80.00%, with an average reporting rate of 56.51%. Among the seven domains, the “basic information” domain had the highest reporting rate (98.15%), followed by “background” domain (79.17%), and the “Review and Quality Assurance” domain got the lowest reporting rate (27.78%). Items with serial reporting defects included item 10b (Indicate how the outputs were selected and sorted), item14a (values and preferences of the target population), item14b (other cost and resource applications), item14c (other factors taken into consolidation), item16 (while the draft guideline undertook independent review), item17 (while the guideline was subject to a quality assurance process). The report quality assessment for all domains is shown in Figure 2. A bubble plot showed the overall quality of each guideline (Figure 3), the two blue spheres represented relatively high-quality CPGs, namely CSC (27) and CSA (28), and the seven CPGs with yellow spheres were relatively low-quality.
Figure 2

Reporting of RIGHT items in CPGs and Supplementary material 3.
Figure 3

Grading and analysis of reporting and methodological quality of CPGs.
3.3 Recommendations on NPIs for PSED
We summarized nine NPIs from the eligible CPGs (23–31), and only four CPGs (23, 27, 28, 30) identified the level of evidence and/or strength of recommendation. Details regarding the level of evidence and the strength of the recommendations in the different grading systems are described in Supplementary material 4, and the evidence quality and recommendation strength are reported in Supplementary material 5. The main types of PSED are PSD and PSA in the eligible CPGs. There were similarities and differences in recommendations for NPIs, and differences in recommendation strength (Figure 4). The visual clinical pathways of NPIs for PSD and PSA are shown in Figure 5.
Figure 4

Evidence map of CPG recommendations on NPIs for PSED.
Figure 5
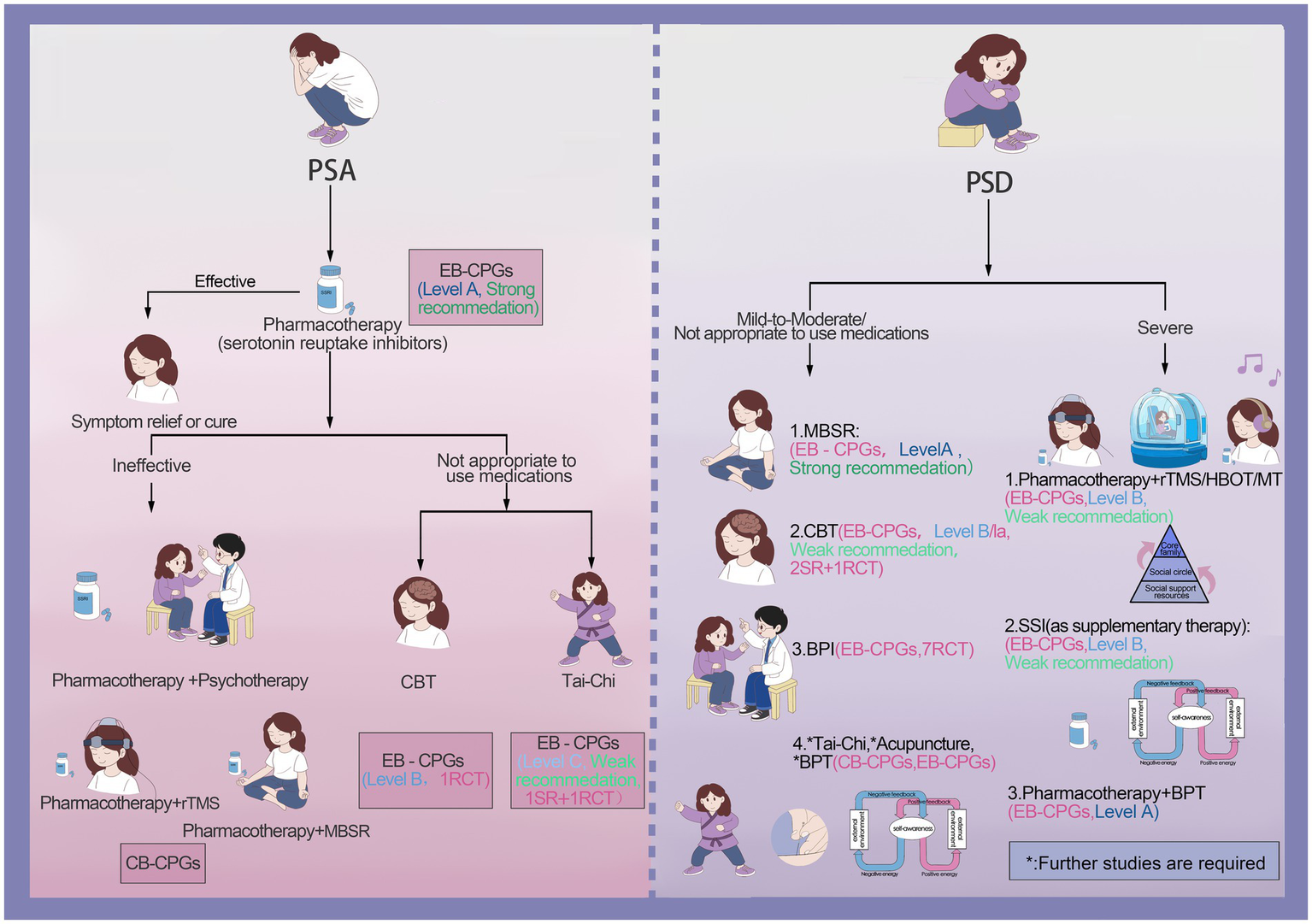
Clinical pathway map of NPIs.
With regard to the use of psychotherapy for PSD, three CPGs (28, 29, 31) recommended using mindfulness-based stress reduction (MBSR) to improve symptoms, one EB-CPG (28) gave this a strong recommendation, while two CB-CPGs gave no recommendation strength. Seven CPGs (23, 25–27, 29–31) recommended cognitive behavioral interventions (CBT) to improve symptoms of PSD, but only one EB-CPG (30) recommended CBT to improve mild PSD and this gave a weak recommendation. There were four CPGs (26–29) that recommended that music therapy (MT) in combination with drug therapy was more effective for severe PSD, and only one guideline (28) gave this a weak recommendation. Balancing Psychotherapy (BPT) integrated treatment modalities from diverse psychological schools to help eliminate the cause of PSD. Specifically, two CPGs (25, 27) had put forward the suggestion that BPT could be utilized as an auxiliary treatment modality for PSD. However, they failed to offer precise recommendations. The guidelines suggested that psychotherapy can be the primary treatment option for patients suffering from mild to moderate PSD, and also for those who had poor medication compliance or experienced adverse drug reactions (25, 29). However, for patients with severe PSD or those with complications, it was recommended that psychotherapy be used as an adjunctive treatment to pharmacotherapy (27, 29).
In terms of social intervention treatment, social support interventions (SSI) were recommended as a supplementary treatment for PSD (25, 26, 28, 29). It was recommended that family members, friends, and colleagues encourage patients to participate in social activities, and one EB-CPG (28) gave this a weak recommendation. Additionally, another EB-CPG (24) recommended the utilization of brief psychosocial interventions (BPI). The supporting evidence was derived from seven RCTs (n = 775) and showed the effectiveness of BPI. However, since the designs of these studies were not rigorous, it was uncertain whether antidepressants played an auxiliary role, so no specific recommendation strength was provided.
Some NPIs suggested that traditional Chinese medicine had potential effects in treating PSD. Two CB-CPGs (25, 29) recommended the application of acupuncture and Tai-Chi to alleviate the symptoms of PSD. Another EB-CPG (27) pointed out that compared with drug therapy, acupuncture was regarded as effective in the treatment of PSD. Nevertheless, acupuncture has not been extensively used in the healthcare systems of different countries. Its clinical effectiveness needs further study. Hence, no recommendation strength was given.
Another type of NPI for PSD was physical therapy. A weak recommendation was given for the combined application of repetitive transcranial magnetic stimulation (rTMS) and drugs in the treatment of severe PSD (31, 33). Hyperbaric oxygen therapy (HBOT) has also been shown to improve the metabolism of brain tissue and promote brain function recovery (31, 34). One EB-CPG (31) recommended using HBOT combined with drug treatment for severe PSD and gave it a weak recommendation.
For the NPIs for PSA, the CPGs recommended drug therapy as the first choice (23, 27, 28, 31). One CB-CPG (31) recommended that when the efficacy of drug therapy was not satisfactory, a combination approach could be adopted. Specifically, drug therapy could be paired with psychotherapy such as CBT, or joined with rTMS, or integrated with MBSR, all with the aim of enhancing the therapeutic outcome. When patients were unable to take medication, Tai-Chi was recommended for the treatment of PSA, and was given a weak recommendation (30), nevertheless, further validation of the effect is necessary. In addition, one CPG (27) recommended CBT for the treatment of PSA. However, the evidence was derived from one RCT and the strength of recommendation was not provided.
4 Discussion
NPIs possess the advantages of high safety, a broad applicable population, as well as the enhancement of patients’ self-management capabilities (34). The majority of stroke patients were the elderly, who are likely to have multiple underlying co-morbidities, such as diabetes, hypertension and so on (35). Typically, these patients need to take a long term drug therapy to control their conditions, with resultant liver and kidney damage (33, 36). The use of NPIs could reduce the side effects of drugs. They focus on the cultivation of patients’ psychological adjustment ability and a positive attitude toward life, thereby facilitating the overall rehabilitation process (23, 32).
The overall quality of the nine CPGs in this study still needs improvement. Stakeholder Involvement, Rigor of Development and Applicability were underrepresented in all CPGs. All the guidelines had elaborated on the target populations (23–31). However, the viewpoints and preferences of these people (patients, the public, etc.) had not been taken into account. Future guideline developers could adopt methods such as questionnaires and interviews (35, 37) to understand the viewpoints and choices of the target populations, consider their actual feelings and needs, provide treatment options that meet their expectations, improve treatment compliance, and at the same time reflect the humanization of medical care.
In the rigor of the development, most of the guidelines did not describe in detail the strength of the recommendations and the level of evidence. The methods for formulating the recommendations (23–26, 29–31), the review of CPGs by external experts, their publication (23, 25, 26, 28–31), and the procedures for updating the CPGs were also inadequately reported (23–26, 29–31). The applicability score was the lowest among all CPGs. Only two CPGs considered the facilitator and barrier factors in the application process (24, 27), and six CPGs provided suggestions for applying the recommendations to practice, but lacked detailed implementation strategies (23–27, 29), Similarly, only two CPGs stated the potential resource impact of applying these recommendations (27, 28), but did not report the potential costs. Thus, the deficiency in the clinical applicability of the guidelines implied that, throughout the development process, insufficient attention was paid to transforming the recommendations into clinical applications. The assessment results of the RIGHT list indicated that the domain with the lowest score was Review and Quality Assurance. Similar to AGREE II, there were also deficiencies in such aspects as “the views and preferences of the target population,” “cost and resource impact,” “independent review” and “quality assurance.” Consequently, the future development of CPGs covering NPIs for PSED needs to center on the aspects of those low-scoring items, with the aim of enhancing the overall guideline quality.
The latest systematic reviews and a meta-analysis indicate that NPIs are effective in improving mood and quality of life for stroke survivors (12, 38). So far, the CPGs relating to NPIs for PSED only cover the two different types of emotional disorders: namely PSD and PSA, with PSD being the predominant focus. The recommendations of the guidelines are inconsistent and most of the guidelines did not give a clear recommendation (23–27, 29, 31), while some provided merely the level of evidence (23, 27, 28, 30). This indicates a lack of uniformity in the evidence related to NPIs for PSD and PSA, as well as varying degrees of research depth in this area.
Our research found that the NPIs strongly recommended by the guideline were MBSR (Level A) which (28) was developed by a multidisciplinary team in China, and the patient group it targeted was Chinese adult stroke patients. However, since the guideline was not specifically designed for PSD, it did not mention the specific implementation methods of MBSR and so lacks clinical applicability. Relevant studies have suggested that MBSR can be one-time or multi-stage, using techniques such as diaphragmatic breathing, mind–body scan and mindful imaging (39). The subtypes of the intervention include mindful cognitive therapy, mindful stress reduction therapy and mindful self-care (40). Nevertheless, there are several obstacles to the clinical application of MBSR. For instance, there is a scarcity of professionals well-versed in both the theory and practice of MBSR. Additionally, patients’ cultural backgrounds and religious beliefs could pose challenges, which might potentially explain why other CPGs did not provide relevant recommendations.
The CPGs made weak recommendations for NPIs including Tai Chi and CBT. The evidence was derived from systematic reviews and RCTs (26, 30, 33, 36). SSI as an adjuvant therapy has also been given a weak recommendation (Level B), and the evidence level for the combination of drugs with rTMS, HBOT or MT was Level B. Due to the lack of high-quality evidence in the studies of these NPIs, CPGs made weak recommendations, which have also been verified by other research (38, 41). In addition, since Tai Chi research was influenced by Chinese data, the promotion and application of Tai Chi in other countries or regions may be restricted. Therefore, when using Tai Chi as an intervention, its localization should be fully considered, and the quality of original research should be improved. A recent systematic review and meta-analysis have shown that acupuncture was the most effective non-pharmacological intervention for improving patients’ emotions (38). In addition, acupuncture had a positive impact on other stroke-related symptoms, such as physical function, speech, and cognition (42, 43), further enhancing the overall treatment efficacy for improving emotions. This was consistent with the viewpoints expressed in the CPGs included in our study (25, 27, 29). However, due to acupuncture’s extensive theoretical system, complex mechanism of action, and high operational requirements, it had not been widely applied globally and further in-depth research was still needed.
Our results indicate that the CPGs included in this study only recommend different NPIs, but detailed clinical implementation plans for NPIs are still lacking. Most of the existing CPGs were focused on PSD. In contrast, other CPGs incorporate the treatment and management of PSED as a segment of their content. However, the recommendations regarding PSED tend to be neither sufficiently clear nor comprehensive. Stroke patients frequently suffer from multiple emotional problems (44). However, there were few studies on emotional states such as PSA, PSCAD, PSEI, PSAP, and extremely few studies on the comorbidity of different emotional states (45). Future research should explore the efficacy of NPIs for different emotional states. By integrating the preferences and demands of patients as well as other stakeholders, and utilizing a variety of tools and resources, personalized intervention programs need to be formulated to further enhance the evidence quality of NPIs for PSED. Subsequently, this will provide high-quality evidence support for the formulation of NPIs guidelines for PSED, and facilitate clinicians making more scientific and feasible clinical decisions.
To our knowledge, this is the first comprehensive systematic study on the existing CPGs for NPIs for PSED. We have used the most common and comprehensive assessment tools, namely AGREE II and RIGHT, to evaluate the methodological quality and reporting quality of the CPGs. We have comprehensively extracted the recommendations, including the recommended content hidden in paragraph style texts. Additionally, we have also used an evidence map to clearly display the strength distribution of the recommendations, and visualized the clinical intervention pathways in different emotional states to assist in clinical decision-making. However, there are several limitations in our study. First, although we used systematic and standardized methods for retrieval, only English and Chinese CPGs were eventually included, and this might result in potential biases. Only two reviewers evaluated the included guidelines, but the consistency between the reviewers was relatively good.
5 Conclusion
The overall quality of the included guidelines still needs to be enhanced, especially in aspects such as stakeholder involvement, rigor of development and clinical applicability. The existing CPGs have provided recommendations on various NPIs for the treatment of PSD and PSA. When applying them to clinical practice, comprehensive considerations should be made by integrating patients’ wishes and the medical environmental factors. In the future, when formulating guidelines for NPIs for PSED, the differences in the emotional stages of patients, the clinical applicability of the guidelines, as well as potential resource and implementation barriers should be taken into account, and timely updates and specific recommendations should be provided. Our research findings can help clinicians choose the most suitable guidelines and recommendations based on the actual situation and accessible resources, promote the standardized application of NPIs in patients with PSED, and improve the quality of the development of clinical practice guidelines for NPIs for PSED. At the same time, they also provide a reference for future guideline formulation and research.
Statements
Author contributions
YL: Visualization, Writing – original draft, Writing – review & editing. JZ: Formal analysis, Writing – original draft. J-jL: Formal analysis, Writing – original draft. DZ: Formal analysis, Visualization, Writing – original draft. LT: Methodology, Writing – review & editing. Y-HJ: Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by National High Level Chinese Medicine Hospital Clinical Research Funding (no. DFRCGC-2024QHTS-CC007).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1580799/full#supplementary-material
References
1.
Feigin VL Stark BA Johnson CO Roth GA Bisignano C Abady GG et al . Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
2.
Medeiros GC Roy D Kontos N Beach SR . Post-stroke depression: a 2020 updated review. Gen Hosp Psychiatry. (2020) 66:70–80. doi: 10.1016/j.genhosppsych.2020.06.011
3.
Broomfield NM Blake J Gracey F Steverson T . Post-stroke emotionalism: diagnosis, pathophysiology, and treatment. Int J Stroke. (2024) 19:857–66. doi: 10.1177/17474930241242952
4.
Guo J Wang J Sun W Liu X . The advances of post-stroke depression: 2021 update. J Neurol. (2021) 269:1236–49. doi: 10.1007/s00415-021-10597-4
5.
Fan X-W Yang Y Wang S Zhang Y-J Wang A-X Liao X-L et al . Impact of persistent poor sleep quality on post-stroke anxiety and depression: a National Prospective Clinical Registry Study. Nat Sci Sleep. (2022) 14:1125–35. doi: 10.2147/NSS.S357536
6.
Ni H Liu Y Yang J Qin H Hu Y Deng H et al . The association between caregiver burden, social capital, and family functioning among caregivers of older adults with PSD-A cross-sectional study. Psychol Health Med. (2024) 30:1–13. doi: 10.1080/13548506.2024.2411064
7.
Zhang J Zhao Y Li H Yang Y Tang Q . Effectiveness of acupuncture plus music therapy for post-stroke depression: systematic review and meta-analysis. Medicine. (2024) 103:e39681. doi: 10.1097/MD.0000000000039681
8.
Waller A Fakes K Carey M Dizon J Parrey K Coad M et al . Quality of life and mood disorders of mild to moderate stroke survivors in the early post-hospital discharge phase: a cross-sectional survey study. BMC Psychol. (2023) 11:32. doi: 10.1186/s40359-023-01068-8
9.
Frank D Gruenbaum BF Zlotnik A Semyonov M Frenkel A Boyko M . Pathophysiology and current drug treatments for post-stroke depression: a review. Int J Mol Sci. (2022) 23:15114. doi: 10.3390/ijms232315114
10.
Eapen BC Tran J Ballard-Hernandez J Buelt A Hoppes CW Matthews C et al . Stroke rehabilitation: synopsis of the 2024 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guidelines. Ann Intern Med. (2025) 178:249–68. doi: 10.7326/ANNALS-24-02205
11.
Zhong K An X Kong Y . The effectiveness of five-element music therapy for post-stroke depression: a systematic review and meta-analysis. Heliyon. (2024) 10:e26603. doi: 10.1016/j.heliyon.2024.e26603
12.
Ahrens J Shao R Blackport D Macaluso S Viana R Teasell R et al . Cognitive -behavioral therapy for managing depressive and anxiety symptoms after stroke: a systematic review and meta-analysis. Top Stroke Rehabil. (2022) 30:368–83. doi: 10.1080/10749357.2022.2049505
13.
Zhang R Yan S-y Wang Y-y Huang Q Ren X-y Tan R et al . Analysis of the status and trends of Chinese clinical practice guideline development between 2010 and 2020: a systematic review. Front Med. (2021) 8:758617. doi: 10.3389/fmed.2021.758617
14.
Gao C Li X Li F Li J Zhang J . Non-pharmacological interventions on quality of life in stroke survivors: a systematic review and meta-analysis. Worldviews Evid-Based Nurs. (2024) 21:158–82. doi: 10.1111/wvn.12714
15.
Brouwers MC Kho ME Browman GP Burgers JS Cluzeau F Feder G et al . AGREE II: advancing guideline development, reporting, and evaluation in health care. Prev Med. (2010) 51:421–4. doi: 10.1016/j.ypmed.2010.08.005
16.
Gavriilidis P Askari A Roberts KJ Sutcliffe RP . Appraisal of the current guidelines for management of cholangiocarcinoma—using the appraisal of guidelines research and evaluation II (AGREE II) instrument. Hepatobil Surg Nutr. (2020) 9:126–35. doi: 10.21037/hbsn.2019.09.06
17.
Linn DD Beckett RD Faust AC . Use of the AGREE II instrument to evaluate critical care practice guidelines addressing pharmacotherapy. J Eval Clin Pract. (2022) 28:1061–71. doi: 10.1111/jep.13687
18.
Zhou X Yang Y Li C Gu S Hou W Lai X et al . What information can we gain from the quality appraisal of guidelines with physical activity recommendations for cancer patients? A systematic review using the AGREE II and AGREE-REX tools. Support Care Cancer. (2023) 31:97. doi: 10.1007/s00520-022-07567-5
19.
Chen Y Yang K Marušic A Qaseem A Meerpohl JJ Flottorp S et al . A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med. (2016) 166:128–32. doi: 10.7326/M16-1565
20.
Khattab M Howard B Al-Rifai S Torgerson T Vassar M . Adherence to the RIGHT statement in Society of Interventional Radiology guidelines. J Osteopath Med. (2021) 121:11–24. doi: 10.1515/jom-2020-0024
21.
Zhao Y Li Y Li J Song W Zhao J Xu Y et al . Reporting quality of chronic kidney disease practice guidelines according to the RIGHT statement: a systematic analysis. Ther Adv Chronic Dis. (2020) 11:17. doi: 10.1177/2040622320922017
22.
Wayant C Cooper C Turner DA Vassar M . Evaluation of the NCCN guidelines using the RIGHT statement and AGREE-II instrument: a cross-sectional review. BMJ Evid Based Med. (2019) 24:219–26. doi: 10.1136/bmjebm-2018-111153
23.
Andrade R Pereira R van Cingel R Staal JB Espregueira-Mendes J . How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II). Br J Sports Med. (2020) 54:512–9. doi: 10.1136/bjsports-2018-100310
24.
Vasil K Lewis J Ray C Baxter J Bernstein C Brewer D et al . Assessment of reliability and validity of the Cochlear implant skills review: a new measure to evaluate Cochlear implant users' device skills and knowledge. Am J Audiol. (2021) 30:105–27. doi: 10.1044/2020_AJA-20-00038
25.
Youdan GA Chihuri ST Wong CK . Preliminary analysis of reliability and validity of the life space questionnaire as a real-world mobility measure for people with lower limb loss: a technical note. Prosth Orthot Int. (2022) 46:491–5. doi: 10.1097/PXR.0000000000000148
26.
Creutzfeldt CJ Holloway RG Walker M . Symptomatic and palliative care for stroke survivors. J Gen Intern Med. (2012) 27:853–60. doi: 10.1007/s11606-011-1966-4
27.
Towfighi A Ovbiagele B El Husseini N Hackett ML Jorge RE Kissela BM et al . Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2017) 48:e30–43. doi: 10.1161/STR.0000000000000113
28.
Zhao FY Yue YY Li L Lang SY Wang MW Du XD et al . Clinical practice guidelines for post-stroke depression in China. Rev Bras Psiquiatr. (2018) 40:325–34. doi: 10.1590/1516-4446-2017-2343
29.
Wu L Dong J-G Huang L-P Song G-Q Song L-P Xie Y et al . Expert consensus on rehabilitation treatment techniques for elderly stroke patients in China. Chin J Geriatr Care. (2019) 17:3–16. doi: 10.3969/j.issn.1672-2671.2019.01.001
30.
Lanctôt KL Lindsay MP Smith EE Sahlas DJ Foley N Gubitz G et al . Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke, 6th edition update 2019. Int J Stroke. (2019) 15:668–88. doi: 10.1177/1747493019847334
31.
Zhang T Zhao J Li X Bai Y Wang B Qu Y et al . Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. (2020) 5:250–9. doi: 10.1136/svn-2019-000321
32.
Li X Yu X Xie Y Feng Z Ma Y Li J . Critical appraisal of the quality of clinical practice guidelines for idiopathic pulmonary fibrosis. Ann Transl Med. (2020) 8:1405. doi: 10.21037/atm-20-3200
33.
Saha GCK Pattojoshi A . Management of psychiatric disorders in patients with stroke and traumatic brain injury. Indian J Psychiatry. (2022) 64:S344–54.
34.
Song JG Wang CH Lv LX Li W-Q Zhang Z-H Han S-K et al . Clinical diagnosis and treatment guidelines for post-stroke depression. J Clin Psychosom Dis. (2020) 26:1–5. doi: 10.3969/j.issn.1672-187X.2020.03.054
35.
Chen MQ Shi WR Wang HY Sun YX . Sex differences of combined effects between hypertension and general or central obesity on ischemic stroke in a middle-aged and elderly population. Clin Epidemiol. (2021) 13:197–206. doi: 10.2147/CLEP.S295989
36.
Zhao X-Q Wang C-X Du Y-F Fu J-H Fu Y Huang X-S et al . Expert consensus on multidisciplinary management of stroke-related non-motor symptoms. Chin J Stroke. (2023) 18:315–34. doi: 10.3969/j.issn.1673-5765.2023.03.011
37.
Liu L Jin Q Chen Y Yin P . Perioperative non-pharmaceutical therapies for insomnia in cancer survivors: a systematic review and network meta-analysis protocol. BMJ Open. (2024) 14:140. doi: 10.1136/bmjopen-2023-080140
38.
Bhatia K Ladd LM Carr KH Di Napoli M Saver JL McCullough LD et al . Contemporary antiplatelet and anticoagulant therapies for secondary stroke prevention: a narrative review of current literature and guidelines. Curr Neurol Neurosci Rep. (2023) 23:235–62. doi: 10.1007/s11910-023-01266-2
39.
Reilly A Sharif A Bhagra O Dominari A Katsos K Nathani KR et al . Evaluation of mindfulness-based interventions for pain, anxiety, and depression in spinal cord injury patients: a systematic review and meta-analysis. Clin Neurol Neurosurg. (2025) 251:108839. doi: 10.1016/j.clineuro.2025.108839
40.
Stöllberger C Schneider B Finsterer J . Drug-drug interactions with direct oral anticoagulants for the prevention of ischemic stroke and embolism in atrial fibrillation: a narrative review of adverse events. Expert Rev Clin Pharmacol. (2023) 16:313–28. doi: 10.1080/17512433.2023.2187376
41.
Monroy-Fraustro D Maldonado-Castellanos I Aboites-Molina M Rodríguez S Sueiras P Altamirano-Bustamante NF et al . Bibliotherapy as a non-pharmaceutical intervention to enhance mental health in response to the COVID-19 pandemic: a mixed-methods systematic review and bioethical meta-analysis. Front Public Health. (2021) 9:629872. doi: 10.3389/fpubh.2021.629872
42.
Tanner L Sowden S Still M Thomson K Bambra C Wildman J . Which non-pharmaceutical primary care interventions reduce inequalities in common mental health disorders? A protocol for a systematic review of quantitative and qualitative studies. Int J Environ Res Public Health. (2021) 18:978. doi: 10.3390/ijerph182412978
43.
Buhr RG Huynh A Lee C Nair VP Romero R Wisk LE . Health professional vs layperson values and preferences on scarce resource allocation. JAMA Netw Open. (2024) 7:e241958. doi: 10.1001/jamanetworkopen.2024.1958
44.
Ferro JM Santos AC . Emotions after stroke: a narrative update. Int J Stroke. (2020) 15:256–67. doi: 10.1177/1747493019879662
45.
Kutlubaev MA Akhmetova AI Ozerova AI . Emotional disorders after stroke. Zh Nevrol Psikhiatr Im S S Korsakova. (2023) 123:30–5. doi: 10.17116/jnevro202312312230
Summary
Keywords
cerebral stroke, emotional disorder, non-pharmacological intervention, clinical practice guidelines, evidence-based medicine
Citation
Li Y, Zhang J, Li J-j, Zhao D, Tang L and Jin Y-H (2025) An evidence map of clinical practice guideline recommendations and quality of non-pharmaceutical interventions for post-stroke emotional disorders. Front. Neurol. 16:1580799. doi: 10.3389/fneur.2025.1580799
Received
28 February 2025
Accepted
26 May 2025
Published
09 June 2025
Volume
16 - 2025
Edited by
Nicola Smania, University of Verona, Italy
Reviewed by
Valentina Varalta, University of Verona, Italy
Daniela Burguêz, Hospital São Lucas da PUCRS, Brazil
Updates
Copyright
© 2025 Li, Zhang, Li, Zhao, Tang and Jin.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Tang, tangling@zxyjhhl.org.cn; Ying-Hui Jin, jinyinghuiebm@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.