Abstract
The human body exhibits remarkable adaptability to diverse environments. Astronauts in microgravity experience physiological changes like those observed in stroke patients due to inactivity. This shared challenge inspires the exploration of rehabilitation methods, bridging the gap between space medicine and physical therapy. This perspective examines the physiological similarities between microgravity and stroke, focusing on proprioceptive deficits. We then introduce the axial loading suit astronauts use to counteract these deficits and its potential application in stroke rehabilitation. We propose the TheraSuit Method®, a suit utilizing similar principles, as a promising tool to enhance whole-body proprioception and facilitate muscle activation against gravity, thereby promoting strength and functional recovery in stroke patients.
Introduction
One of the brain’s primary functions is to receive sensory input from the environment and produce an appropriate motor response, i.e., body movement. The brain depends on blood flowing freely to deliver oxygen to the different areas to function correctly. A vascular interruption, like a stroke, can compromise parts of the brain that can get damaged without oxygen and lose important function (1). Every year, it is estimated that nearly 800,000 people are affected by a stroke in the United States (2), i.e., one roughly every 40 s.
Strokes disrupt communication between neurons (3), and can present with a wide range of symptoms, varying from altered cognition, paresis, muscle atrophy, absence of movement, vestibular disturbances, and difficulty standing and maintaining balance. This reduces overall independence and function and deteriorates the quality of life (4, 5).
Rehabilitation is a necessary intervention post-stroke to improve strength, balance and gait, and diminish sedentarism that can occur after hospitalization (4, 6). Different rehabilitation strategies have been applied to facilitate healing, such as mobilization, resistive exercises, neuromuscular electric stimulation, transfers from bed to sitting on a chair, and ambulation when possible (7–9). However, there is a lack of consensus on universally established rehabilitative strategies, including frequency and duration (10). During the first few weeks post stroke, an intensive intervention (i.e., carried out daily for at least an hour) may be applied to preserve motor maps and take advantage of enhanced neuroplasticity (10), which could increase sensory responses and encourage motor engagement (11). Maintaining strength can help preserve muscle mass, additionally helping speed recovery (12).
Stroke causes impairments of proprioception that translate into an altered sensory system (13). Proprioception is part of the sensory system that is necessary for premotor activation. Proprioception is codependent on muscle contraction to send signals to the receptors in the joints, Golgi tendon organs, and muscle spindles to activate somatic responses to adjust muscle tone (13). One common consequence of impaired proprioception after a stroke is the neglect of the affected side of the body. This neglect can manifest in various ways, with one notable impact on weight-bearing activities. Individuals may unintentionally favor their unaffected side, leading to an uneven weight distribution during activities like standing or walking. This asymmetrical weight-bearing affects the affected limb and can contribute to difficulties in maintaining balance and stability (4, 13). While Apriliyasari et al. (14) provide an excellent recent review of the effect of proprioceptive training in stroke rehabilitation, it is apparent that most of the interventions discussed do not target improving proprioception of the whole-body segments (13). Stroke patients may benefit from simulated axial loading that can be experienced by the sensory-motor system (6). Similar axial loading is also successfully used by astronauts who experience similar neuro-musculoskeletal changes in space, like that after a stroke.
Similarities in physiological changes due to a stroke and exposure to microgravity
The human body in space experiences microgravity and adapts to a less demanding environment. As a result, astronauts often lack the strength, stamina, and cardiovascular endurance required to meet the demands of Earth’s gravitational forces immediately upon their return from spaceflight (13, 15). Astronauts come back with various physiological adaptations like muscle atrophy, gait disturbances, altered proprioceptive function, vestibular disturbances, cardiovascular deconditioning, fluid shifts to the upper body, loss of bone density, and low vision (15–21). These adaptations are observed more frequently during longer-duration spaceflight missions, spanning over weeks or months (6, 22–24).
These changes can resemble the physiological adaptations observed in patients who have undergone prolonged bed rest following a stroke (4, 6). In fact, researchers use bed-rest as one of the spaceflight analogs to force the inactivity of different parts of the human body, test out various countermeasures, and understand the physiological adaptations at the fundamental level (24). The inability to move independently and safely quickly leads to muscle atrophy, loss of strength, and cardiovascular deconditioning in stroke patients (25). The affected side post-stroke can also lead to decreased bone density and compromised bone integrity (4). Alteration of the sensorimotor and vestibular system can make it challenging to maintain an orthostatic position (26). There is also a migration of fluids from the lower extremities to the chest and head, increasing intracranial pressure, which can increase dizziness, lack of balance and low vision, making the patient prone to falls (26).
These similarities between astronauts and stroke patients, who both have experienced a period of limited mobility or/and bed rest, have increased the medical community’s interest in seeking alternative and effective rehabilitation techniques (24). Space missions have significantly contributed to our understanding of rehabilitation programs designed to counteract the detrimental physiological effects of reduced gravitational activation (6, 18, 27). Astronauts undergo intensive rehabilitation interventions to accelerate recovery (15). They also employ various exercise techniques or other countermeasures, like body suits while in space, to reduce the debilitating physiological effects on their bodies.
Countermeasure loading suits for astronauts
To mitigate the harmful somatosensory and musculoskeletal deficits, the “Pingvin” (also sometimes called “Penguin”) suit was developed by Soviet scientists to be used by their cosmonauts during spaceflight (28). The suit featured an intricate system of elastic bands anchored at the waistband, generating vertical tension between the shoulders and waist and horizontally between the waist and feet. This axial loading challenged the cosmonaut’s muscles and core stability. While the suit was routinely used during Soviet spaceflights in the 1970s, 1980s, it was prone to overheating and discomfort and thus replaced by newer variants, like the Penguin-3 suit (29).
NASA has been funding the development of in-flight countermeasure suits for many years; for example, the Gravity Loading Countermeasure Suit (or the MIT Skinsuit) (30, 31) is a passive axial loading suit concept, but so far, we have only seen some pilot data from parabolic flights about its effectiveness or from a handful of spaceflights where it was used more as a technology demonstration. Similarly, a Torso Compression Harness to prevent spinal deconditioning (32) and a Variable Vector Countermeasure Suit (or V2 suit) (33) to provide “viscous resistance” against a selected “down” direction during movements are proposed and supported to some extent by NASA for initial feasibility. However, we have not seen quantitative data from experimental tests, especially in microgravity. An ESA-funded study proposed the concept of the ‘Dynasuit’ (34) in 2012 as an active, intelligent suit with bio-sensors and actuators in a biofeedback loop that included movement resistance and foot sole stimulation. However, we have yet to see this idea realized in the public domain.
The TheraSuit Method®
History of the TheraSuit Method®
Inspired by the early success of axial loading suits such as the Pingvin suit during spaceflight and recognizing that children with conditions like Cerebral Palsy (CP) experience similar movement difficulties as astronauts, the Pediatric Institute of the Russian Academy of Sciences developed and modified the Pingvin suit into various versions of the Adeli suit (e.g., Adeli-92, Adeli-94). These modified suits have been utilized to treat children with CP and other neuromuscular disorders. In 2000, a trained Polish physical therapist couple, Richard and Izabela Koscielny, whose daughter has Cerebral Palsy (CP), explored various rehabilitation strategies for her. They developed a variant of the Russian Adeli suit known as the TheraSuit® garment, along with the use of Universal Exercise Unit (UEU) and an intensive training program. This marked the first implementation of such a program in the United States, and they were awarded a patent for their invention under the name “TheraSuit.” The TheraSuit® garment is made of a soft dynamic orthosis, capable of providing significant sensory input of proprioception to increase functional movement in synergy (35). The development of the TheraSuit® garment is the facilitation of functional movement in all planes: sagittal, frontal, and transverse. The Therasuit Method® (that combines the garment, the UEU, and the intensive program) can be tailored to the individual needs of each patient with a neurological disorder. It is based on training principles for strength gains, respecting the peak physiological response of each patient. Care plans can be designed depending on the type of energy production, muscle fibers, and level of functioning. While there are other suits in the market in the US, like the Pediasuit, the Adeli suit, and the Neurosuit, to the best of our knowledge, TheraSuit® is the only method FDA certified in the United States. It has been used actively in various clinics around the world, mainly as part of a rehabilitation program for children with CP. While there are a few clinical trials done with the pediatric population with CP, and they have been successful in increasing gross motor skills, gait quality, and body alignment (36, 37), The TheraSuit Method® has not yet been applied in adult populations, particularly in the context of stroke rehabilitation; however, its principles hold potential for enhancing post-stroke rehabilitation outcomes.
Pillars of the TheraSuit Method®
The TheraSuit Method® has several pillars that define its principles. This technique is not limited to TheraSuit® garment use only; it is based on intensive therapies using strength training principles and task-specific exercises involving repetitive movements and work against gravity employing the UEU.
Preparation
The body’s preparation includes hot packs and massages using neurological mobilization, traction, compressions, and vibration. This helps bring body awareness while stimulating sensory receptors in the skin, muscles, and joints (38).
Heat
The heat promotes vasodilation, helps eliminate lactic acid, and increases muscle oxygen (39). It also relaxes muscles and trigger points and decreases muscle tone (40).
Massage
Increases circulation and improve oxygenation, promoting muscle relaxation (40). The friction of the massage stimulates sensory receptors, relaxing painful muscles, and increasing blood flow (40). The massage also helps to break down connective tissue and promotes myofascial release.
Mobilization
Joint compressions, traction, and mobilization can be done to prepare the limb for resistive exercises in the pulley system. Mobilizations can shorten and elongate muscles, exposing nerves to tension and stretches and increasing the range of motion to facilitate exercises. Ranging and mobilizing the limbs can improve mobility and neuromuscular function (38).
Universal exercise unit
The Universal Exercise Unit (UEU) or “Cage” is heavy equipment made from metal with a grid wall designed and open in the front. It has a cubic or box shape measuring two meters by two meters by two meters. This equipment uses a system of cables, pulleys, weights, harnesses, and bungees. It can be used in various ways, such as pulleys for resistive exercises or the “spider” system for body suspension.
The Pulley system
The pulley allows the limbs to be suspended in gravity elimination to facilitate movement and help with complex movement patterns. This equipment utilizes weights to create resistance or facilitate movement. The goal is for the movement to be done actively. While working in the pulley system, sandbags are specially prepared to be used as an extra set of hands; they help hold a limb down or align the body. The UEU allows for the isolation of muscle groups and targets specific movements. Strength training promotes increased function, improving the quality of gait, balance, and coordination. Figure 1 is an example of the use of the pulley system.
Figure 1

Pulley system.
The “Spider” suspension
The “spider” system allows the patient to be suspended by a belt connected to four or more bungees that attach to the cage, eliminating gravity and facilitating the standing position (41, 42). Bungees can also be attached lower on the cage and add weight and resistance to the moment in standing. The “spider” system supports safely shifting body weight, jumping, kneeling, half-kneeling, and standing. The “spider” cage is an effective tool to be able to stand a patient who is having balance and strength difficulties. Figure 2 shows an example of exercises in the UEU spider system.
Figure 2
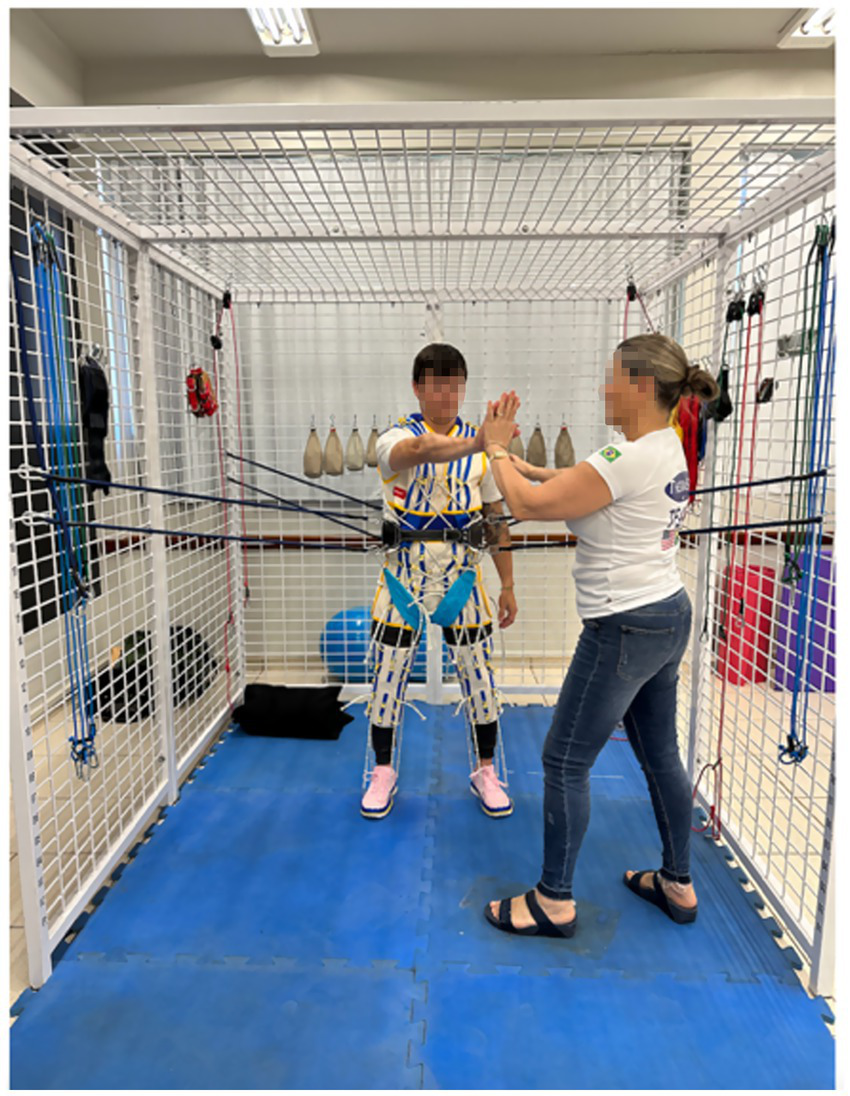
Example of exercise in the Universal Exercise Unit spider system.
TheraSuit® garment
The TheraSuit® garment is a soft, dynamic orthotic consisting of a hat, vest, shorts, knee pads, and shoes with rubber bands that attach to specifically placed hooks on the body in order to inhibit or facilitate movements (42). These rubber bands provide support through facilitation, resistance, inhibition, postural correction, and body alignment. It also offers dynamic feedback and deep proprioceptive input to the muscles, joints, and nervous system (36, 37). The TheraSuit® garment stabilizes the trunk and corrects posture, thus facilitating specific strength and functional tasks (35, 36).
The garment used, and the intensive intervention of resistive exercises represent the TheraSuit Method® (41). It is important to emphasize that the TheraSuit Method® is composed of pillars that include several components to promote strength and functional gains. These pillars include the preparation of the body to be worked on with massage, heat, vibration, and mobilization. This is followed by resistive exercises on the pulley system, facilitating activation against gravity. The following action is fitting the TheraSuit® garment to work on motor function on the floor, gait training, and other tasks. The treatment concludes with vestibular training and strengthening performed on the spider or pulley.
The TheraSuit® garment is one of the components of the TheraSuit Method®. It is used when there is a need to align the body, correct the posture, stabilize the trunk, and provide strong proprioceptive input (36, 37). In some instances, the TheraSuit® garment will not be used when applying the TheraSuit® Method®. The use of the TheraSuit® garment is contra-indicated in the presence of scoliosis, progressive metabolic disorders, joint degenerations, severe osteoporosis, severe subluxation, and fixed contractures (41, 42).
Benefits of the TheraSuit Method®
Participation in more intensive therapies and resistive exercises offers benefits that may maintain strength (36, 37, 41). The use of the TheraSuit® garment is meant to increase the loading and proprioception in the joints and muscles of the affected side of the body. The elastic components used in the TheraSuit® garment provide resistance, compression, and axial loading to the body, generating stimulation of the Golgi tendon and creating a reflex response (43).
The TheraSuit Method® can retrain the central nervous system, helping to normalize muscle tone, correct gait pattern, improve balance, increase strength, and maintain bone density through impact and weight training (35, 36, 41, 42). Elastic bands can be used to correctly align the body, support weak muscles, and provide external stabilization (35, 36, 41, 42). The bands can be adjusted for each patient to provide support or resistance.
The TheraSuit Method® uses training principles with increased frequency and has demonstrated significant gains in gait patterns in children with CP (44, 45). Research studies have shown measurable strength gains by the third week of intensive treatment (36, 37). However, it is essential to emphasize that to maintain muscle strength, it is necessary to continue resistance exercises during intervals between one intervention and another (37).
Intensive therapy using the TheraSuit Method® has demonstrated results in increasing gross motor function to a greater extent than traditional therapies have shown promoting postutal correction (45–48). It has shown consistent improvement and positive effects on speed, cadence, and step length (44) In conclusion, despite the limited number of studies, there is evidence of this method’s effectiveness in treating children with neurological disorders.
Discussion
Astronauts have been using countermeasures for many decades to reduce the physiological changes during spaceflight. One such focused countermeasure includes the stimulation of proprioception through axial loading suits in combination with strength training (15). The TheraSuit Method® has the potential to offer significant advantages in the recovery of patients with neurological disorders, such as stroke, here on Earth. This approach may enhance strength, increase resistance, improve balance, and overall patient functionality. Furthermore, the proprioceptive input delivered through this method can lead to notable improvements in trunk control, balance performance, gait, and mobility in post-stroke patients. By integrating these benefits, the TheraSuit Method® could play a pivotal role in facilitating more effective rehabilitation outcomes (14).
There is a limited number of peer-reviewed studies on the TheraSuit Method®, all focused on children (45, 48–50). To date, no studies have been conducted on the use of the TheraSuit Method® specifically within the context of post-stroke rehabilitation. This presents a significant gap in the literature, as understanding the application of the TheraSuit Method® in this area could offer valuable insights into its potential benefits.
It is crucial to explore these strengthening programs, as they have the potential to enhance functional gains for patients recovering from strokes. By investigating how the TheraSuit Method® can facilitate improvements in muscle strength, mobility, and overall functional ability, we may uncover effective strategies for rehabilitation that can significantly impact patient outcomes.
Conducting research in this domain will not only contribute to the evidence base for the TheraSuit Method® but also aid clinicians in developing comprehensive rehabilitation plans tailored to the unique needs of post-stroke patients. Ultimately, future research could lead to improved recovery trajectories and quality of life for individuals affected by stroke.
Statements
Author contributions
RL: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. RG: Writing – review & editing. JO: Writing – review & editing. DM: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
RL is an instructor of the TheraSuit Method®.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Carr JH Shepherd RB . Neurological rehabilitation: Optimizing motor performance. 2nd ed. Edinburgh: Churchill Livingstone (2010).
2.
CDC . (2024). Stroke facts. Available online at: https://www.cdc.gov/stroke/facts.htm [Accessed Febrauy 5, 2024]
3.
Tsao CW Aday AW Almarzooq ZI Anderson CAM Arora P Avery CL et al . Heart disease and stroke Statistics-2023 update: a report from the American Heart Association. Circulation. (2023) 147:e93–e621. doi: 10.1161/CIR.0000000000001123
4.
Ostrowska PM Studnicki R Rykaczewski M Spychała D Hansdorfer-Korzon R . Evaluation of the effect of SPIDER system therapy on weight shifting symmetry in chronic stroke patients-a randomized controlled trial. Int J Environ Res Public Health. (2022) 19:6214. doi: 10.3390/ijerph192316214
5.
Saber Tehrani AS Kattah JC Kerber KA Gold DR Zee DS Urrutia VC et al . Diagnosing stroke in acute dizziness and Vertigo: pitfalls and pearls. Stroke. (2018) 49:788–95. doi: 10.1161/STROKEAHA.117.016979
6.
Motanova E Bekreneva M Rukavishnikov I Shigueva TA Saveko AA Tomilovskaya ES . Application of space technologies aimed at proprioceptive correction in terrestrial medicine in Russia. Front Physiol. (2022) 13:921862. doi: 10.3389/fphys.2022.921862
7.
Brewer L Horgan F Hickey A Williams D . Stroke rehabilitation: recent advances and future therapies. QJM. (2013) 106:11–25. doi: 10.1093/qjmed/hcs174
8.
Brower RG . Consequences of bed rest. Crit Care Med. (2009) 37:S422–8. doi: 10.1097/CCM.0b013e3181b6e30a
9.
Vikne H Strøm V Pripp AH Gjøvaag T . Human skeletal muscle fiber type percentage and area after reduced muscle use: a systematic review and meta-analysis. Scand J Med Sci Sports. (2020) 30:1298–317. doi: 10.1111/sms.13675
10.
Coleman ER Moudgal R Lang K Hyacinth HI Awosika OO Kissela BM et al . Early rehabilitation after stroke: a narrative review. Curr Atheroscler Rep. (2017) 19:59. doi: 10.1007/s11883-017-0686-6
11.
Scrivener K Dorsch S McCluskey A Schurr K Graham PL Cao Z et al . Bobath therapy is inferior to task-specific training and not superior to other interventions in improving lower limb activities after stroke: a systematic review. J Physiother. (2020) 66:225–35. doi: 10.1016/j.jphys.2020.09.008
12.
Di Girolamo FG Fiotti N Milanović Z Situlin R Mearelli F . The aging muscle in experimental bed rest: a systematic review and Meta-analysis. Front Nutr. (2021) 8:633987. doi: 10.3389/fnut.2021.633987
13.
Yu Y Chen Y Lou T Shen X . Correlation between proprioceptive impairment and motor deficits after stroke: a meta-analysis review. Front Neurol. (2022) 12:688616. doi: 10.3389/fneur.2021.688616
14.
Apriliyasari RW Van Truong P Tsai PS . Effects of proprioceptive training for people with stroke: a meta-analysis of randomized controlled trials. Clin Rehabil. (2022) 36:431–48. doi: 10.1177/02692155211057656
15.
Krittanawong C Singh NK Scheuring RA Urquieta E Bershad EM Macaulay TR et al . Human health during space travel: state-of-the-art review. Cells. (2023) 12:40. doi: 10.3390/cells12010040
16.
Carriot J Mackrous I Cullen KE . Challenges to the vestibular system in space: how the brain responds and adapts to microgravity. Front Neural Circ. (2021) 15:760313. doi: 10.3389/fncir.2021.760313
17.
Chuang TT . Interplanetary regenerative medicine for mission Mars of SpaceX and NASA. Regen Med. (2016) 11:427–9. doi: 10.2217/rme-2016-0061
18.
Grimm D . Microgravity and space medicine 2.0. Int J Mol Sci. (2022) 23:4456. doi: 10.3390/ijms23084456
19.
Ozdemir RA Goel R Reschke MF Wood SJ Paloski WH . Critical role of Somatosensation in postural control following spaceflight: Vestibularly deficient astronauts are not able to maintain upright stance during compromised Somatosensation. Front Physiol. (2018) 9:1680. doi: 10.3389/fphys.2018.01680
20.
Proske U Weber BM . Proprioceptive disturbances in weightlessness revisited. NPJ Microgravity. (2023) 9:64. doi: 10.1038/s41526-023-00318-8
21.
Roberts DR Asemani D Nietert PJ Eckert MA Inglesby DC Bloomberg JJ et al . Prolonged microgravity affects human brain structure and function. AJNR Am J Neuroradiol. (2019) 40:1878–85. doi: 10.3174/ajnr.A6249
22.
Grimm D Hemmersbach R . Translation from microgravity research to earth application. Int J Mol Sci. (2022) 23:995. doi: 10.3390/ijms231910995
23.
Macias BR Patel NB Gibson CR Samuels BC Laurie SS Otto C et al . Association of Long-Duration Spaceflight with Anterior and Posterior Ocular Structure Changes in astronauts and their recovery. JAMA Ophthalmol. (2020) 138:553–9. doi: 10.1001/jamaophthalmol.2020.0673
24.
Scott JPR Kramer A Petersen N Green DA . The role of long-term head-down bed rest in understanding inter-individual variation in response to the spaceflight environment: a perspective review. Front Physiol. (2021) 12:614619. doi: 10.3389/fphys.2021.614619
25.
Patsaki I Dimitriadi N Despoti A Tzoumi D Leventakis N Roussou G et al . The effectiveness of immersive virtual reality in physical recovery of stroke patients: a systematic review. Front Syst Neurosci. (2022) 16:880447. doi: 10.3389/fnsys.2022.880447
26.
Winkelman C . Bed rest in health and critical illness: a body systems approach. AACN Adv Crit Care. (2009) 20:254–66. doi: 10.1097/NCI.0b013e3181ac838d
27.
Hupfeld KE McGregor HR Reuter-Lorenz PA Seidler RD . Microgravity effects on the human brain and behavior: dysfunction and adaptive plasticity. Neurosci Biobehav Rev. (2021) 122:176–89. doi: 10.1016/j.neubiorev.2020.11.017
28.
Kozlovskaya IB Girgoriev AI Stephantzov VI . Countermeasures of the negative effects of weightlessness on physical systems in long-term space flights. Acta Astronaut. (1995) 36:661–8.
29.
Yarmanova EN Kozlovskaya IB Khimoroda NN Fomina EV . Evolution of Russian microgravity countermeasures. Aerosp Med Hum Perform. (2015) 86:A32–7. doi: 10.3357/AMHP.EC05.2015
30.
Bellisle R.F. Newman D.J. (2020). “Countermeasure suits for spaceflight,” in 50th International Conference on Environmental Systems: Lisbon, Portugal.
31.
Waldie JM Newman DJ . A gravity loading countermeasure skinsuit. Acta Astronaut. (2011) 68:722–30. doi: 10.1016/j.actaastro.2010.07.022
32.
Sayson JV Lotz J Parazynski S Hargens AR . Back pain in space and post-flight spine injury: mechanisms and countermeasure development. Acta Astronaut. (2013) 86:24–38. doi: 10.1016/j.actaastro.2012.05.016
33.
Duda KR Vasquez RA Middleton AJ Hansberry ML Newman DJ Jacobs SE et al . The variable vector countermeasure suit (V2Suit) for space habitation and exploration. Front Syst Neurosci. (2015) 9:55. doi: 10.3389/fnsys.2015.00055
34.
Letier P Motard E Luchsinger R Kovacs G Stauffer Y Bertschi M . (2012). “Dynasuit, intelligent space countermeasure suit concept based on new artificial muscles technologies and biofeedback,” in International Symposium on Artificial Intelligence, Robotics and Automation in Space. Paris, France.
35.
Koscielny I . Treatment method therasuit(TM) In: Cerebral palsy magazine (2004). 8–13.
36.
Karadag-Saygi E Giray E . The clinical aspects and effectiveness of suit therapies for cerebral palsy: a systematic review. Turk J Phys Med Rehabil. (2019) 65:93–110. doi: 10.5606/tftrd.2019.3431
37.
Kaushik K Kumar K . Effect of cage therapy using advanced spider suit compared to traditional physical therapy on gross motor function in children with cerebral palsy – an Indian experience. Int J Neurorehabilit. (2016) 03:193. doi: 10.4172/2376-0281.1000193
38.
Bravo C Skjaerven LH Guitard Sein-Echaluce L Catalan-Matamoros D . Experiences from group basic body awareness therapy by patients suffering from fibromyalgia: a qualitative study. Physiother Theory Pract. (2020) 36:933–45. doi: 10.1080/09593985.2018.1517286
39.
Szekeres M MacDermid JC Grewal R Birmingham T . The short-term effects of hot packs vs therapeutic whirlpool on active wrist range of motion for patients with distal radius fracture: a randomized controlled trial. J Hand Ther. (2018) 31:276–81. doi: 10.1016/j.jht.2017.08.003
40.
Gui-Demase M Silva K Teixeira G . Manual therapy associated with topical heat reduces pain and self-medication in patients with tension-type headache. Fisioter Pesqui. (2021) 28:244–51. doi: 10.1590/1809-2950/17019328032021
41.
Bailes AF Greve K Schmitt LC . Changes in two children with cerebral palsy after intensive suit therapy: a case report. Pediatr Phys Ther. (2010) 22:76–85. doi: 10.1097/PEP.0b013e3181cbf224
42.
Koscielny I. Koscielny R. (2024). Therasuit® Method: Basic course.
43.
Prokopenko SV Rudnev VA Arakchaa ÉM Derevtsova SN . Use of the principle of proprioceptive correction in the restoration of voluntary movements in the paralyzed arm in patients in the late recovery and residual post-stroke periods. Neurosci Behav Physiol. (2008) 38:627–31. doi: 10.1007/s11055-008-9015-4
44.
Belizón-Bravo N Romero-Galisteo RP Cano-Bravo F Gonzalez-Medina G Pinero-Pinto E Luque-Moreno C . Effects of dynamic suit orthoses on the Spatio-temporal gait parameters in children with cerebral palsy: a systematic review. Children (Basel). (2021) 8:1016. doi: 10.3390/children8111016
45.
Martins E Cordovil R Oliveira R Pinho J Vaz JR . The immediate effects of Therasuit® on the gait pattern of a child with unilateral spastic cerebral palsy. J Pediatr Neurol Dis. (2017) 1:S1011. doi: 10.4172/2572-4983.1000S1011
46.
Lee SH Shim JS Kim K Moon J Kim MY . Gross motor function outcome after intensive rehabilitation in children with bilateral spastic cerebral palsy. Ann Rehabil Med. (2015) 39:624–9. doi: 10.5535/arm.2015.39.4.624
47.
Mélo TR Yamaguchi B Chiarello CR Costin ACS Erthal V Israel VL et al . Intensive neuromotor therapy with suit improves motor gross function in cerebral palsy: a Brazilian study. Motricidade. (2018) 13:54. doi: 10.6063/motricidade.13669
48.
Azab ASR Hamed SA . Effect of suit therapy on back geometry in spastic diplegic cerebral palsied children. J Am Sci. (2014) 10:245–51.
49.
Baptista PPA Furtado ACA Fernandes TG Freire Júnior RC Lima CFM Mendonça ASGB . Positive impact of the Therasuit method on gross motor function of children with autism spectrum disorder: case series. Front Neurol. (2023) 14:1254867. doi: 10.3389/fneur.2023.1254867
50.
Norian S Rajaby R Daneshmandi H Fayazi A . Evaluation of the effect and durability of a 12-week exercise program with Therasuit on balance and gait kinematics in children with cerebral palsy spastic diplegia. Sci J Rehabil Med. (2023). 13:612–25. doi: 10.32598/SJRM.13.3.3121
Summary
Keywords
stroke, proprioception, rehabilitation, microgravity, bed rest, TheraSuit Method®, axial-loading suit
Citation
Lampert R, Goel R, Oblanca JV and Martins DF (2025) From astronauts to stroke survivors: how the TheraSuit Method® can boost balance and recovery. Front. Neurol. 16:1581256. doi: 10.3389/fneur.2025.1581256
Received
28 February 2025
Accepted
25 June 2025
Published
13 August 2025
Volume
16 - 2025
Edited by
Elena S. Tomilovskaya, Russian Academy of Sciences (RAS), Russia
Reviewed by
Satoshi Iwase, Aichi Medical University, Japan
Updates
Copyright
© 2025 Lampert, Goel, Oblanca and Martins.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rose Lampert, roselampert@mac.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.