Abstract
Objective:
Hand dysfunction is one of the main causes of disability in stroke. This systematic review and meta-analysis aimed to evaluate the efficacy of different types of acupuncture therapy in improving hand dysfunction among post-stroke patients.
Methods:
A comprehensive search was conducted across eight databases (PubMed, Cochrane Library, Embase, Web of Science, China National Knowledge Infrastructure [CNKI], Chongqing VIP Chinese Scientific Journals Database [VIP], China Biology Medicine [CBM], and Wan Fang) to identify randomized controlled trials (RCTs). Forty-two RCTs involving 2,766 participants were included. Primary outcomes were the Brunnstrom Recovery Stage (BRS), Fugl-Meyer Assessment (FMA), and Lindmark scores; secondary outcomes included the Modified Ashworth Scale (MAS), Range of Motion (ROM), Manual Muscle Testing (MMT), and Modified Barthel Index (MBI).
Results:
Meta-analyses demonstrated significant improvements in hand function across multiple outcomes: BRS (mean difference [MD] = 0.56, 95% confidence interval [CI]: 0.43–0.69), FMA (MD = 1.24, 95% CI: 0.96–1.53), MAS (MD = −0.48, 95% CI: −0.59 to −0.38), ROM (MD = 0.95, 95% CI: 0.64–1.26), and MBI (MD = 6.70, 95% CI: 4.85–8.55). Subgroup analyses revealed that electroacupuncture (EA) outperformed traditional acupuncture (TA) in improving BRS (p = 0.008). Heterogeneity was partially attributed to acupuncture modalities, with EA exhibiting lower variability compared to traditional methods.
Conclusion:
This meta-analysis supports the use of acupuncture, particularly EA, for enhancing hand function in post-stroke patients. EA demonstrates superior efficacy and consistency, suggesting its prioritization in clinical practice.
1 Introduction
Stroke is an acute cerebrovascular disease caused by cerebral vascular occlusion or rupture, leading to brain function disorder. It can be classified into ischemic stroke (1) or hemorrhagic stroke (2). Common sequalae of stroke include cognitive impairment, hemiplegia, aphasia, and other neurological deficits. Stroke is a prevalent condition, with 15 million cases occurring globally each year, ranking second in global mortality and third in disability rates (3). Hand dysfunction is a frequent complication of stroke and one of the main contributors to disability. Clinical manifestations include motor impairment, swelling, pain, and numbness in the affected hand, severely impacting activities of daily living. Additionally, it imposes significant psychological burdens (4). Moreover, the negative impact of hand dysfunction extends to increased caregiving costs for families and society (5, 6). Thus, identifying effective treatments for post-stroke hand dysfunction is imperative.
As a core component of traditional Chinese medicine, acupuncture is widely utilized in stroke rehabilitation. Its efficacy and cost-effectiveness have been demonstrated in multiple clinical trials. Substantial studies have confirmed the utility of acupuncture in improving various functional impairments in stroke patients (7, 8). Research further corroborated the definitive therapeutic effects on shoulder-hand syndrome (9) and hand spasticity in stroke patients (10). In recent years, the heightened awareness of rehabilitation in China has led to an increasing number of studies employing systematic rehabilitation assessments to evaluate acupuncture outcomes. This trend enables the execution of the present study. Building on prior research, we conducted a meta-analysis of clinical trials to assess the efficacy of acupuncture in treating post-stroke hand dysfunction, with subgroup analyses to identify factors contributing to variability in outcomes. Our objective is to evaluate the therapeutic effects of various acupuncture techniques on post-stroke hand function through the lens of modern rehabilitation theories, thereby providing higher-quality evidence for the significance of acupuncture in stroke rehabilitation. Additionally, we aim to offer novel insights into the selection of acupuncture modalities for patients with post-stroke hand dysfunction.
2 Data and methods
2.1 Search strategy
Two researchers independently reviewed randomized controlled trials (RCTs) published from January 1, 2005, to December 31, 2024. The search encompassed eight databases, including four English-language databases (Cochrane Library, PubMed, Embase, and Web of Science) and four Chinese-language databases (China National Knowledge Infrastructure [CNKI], Chongqing VIP Chinese Scientific Journals Database [VIP], China Biology Medicine [CBM], and Wan Fang Database). For PubMed, the search strategy employed the following:
MeSH terms and keywords: (((((“Stroke”[MeSH Terms]) OR (stroke[Title/Abstract])) OR (cerebrovascular accident[Title/Abstract])) OR (cerebral stroke[Title/Abstract])) OR (CVA[Title/Abstract])) AND (((“Acupuncture Therapy”[MeSH Terms]) OR (“Therapy, Acupuncture”[MeSH Terms])) OR (Acupuncture[Title/Abstract])) AND ((“Hand”[MeSH Terms]) OR (hand[Title/Abstract])).
Analogous search strategies were adapted for other databases. The complete search strategies for all databases are provided in Supplementary File 1.
2.2 Eligibility criteria
2.2.1 Inclusion criteria
The inclusion criteria were as follows: (1) only RCTs investigating acupuncture for stroke treatment, published between January 1, 2005, and December 31, 2024, were included. (2) Participants exhibited hand dysfunction (regardless of age, sex, disease duration, stroke type, or treatment duration). (3) RCTs evaluating various acupuncture modalities for stroke were included. The distinction between experimental and healthy groups was that the experimental group received one additional acupuncture therapy compared to the healthy group. (4) Studies must report at least one primary outcome measure. Outcome Measures: Primary outcomes: Brunnstrom Recovery Staging (BRS) for hand, Fugl-Meyer Assessment (FMA) Upper Extremity wrist/hand items, Lindmark Hand Assessment. Secondary outcomes: Modified Ashworth Scale (MAS) for hand joints, Range of motion (ROM) of hand joints, Manual Muscle Testing (MMT) for hand musculature, and Modified Barthel Index (MBI).
2.2.2 Exclusion criteria
The exclusion criteria were as follows: (1) including animal studies, observational studies, meta-analyses, reviews, and systematic reviews. (2) Studies with unclear or undefined diagnostic criteria. (3) Patients diagnosed with other condition/complication that affects hand function (e.g., shoulder-hand syndrome). (4) Studies lacking assessment methods for any primary outcome measures. (5) Studies where additional non-acupuncture therapies were introduced to the experimental group beyond the healthy group’s baseline treatment. (6) Duplicate publications of the same study across multiple language databases. (7) Studies with inaccessible full texts or insufficient data.
2.3 Data extraction and analysis
2.3.1 Data extraction
Two researchers first excluded duplicate records using the deduplication function in EndNote X9, followed by screening titles and abstracts to remove irrelevant studies or duplicates that did not meet the inclusion criteria. Subsequently, full texts of the remaining studies were retrieved and independently assessed for eligibility based on the predefined inclusion and exclusion criteria. The researchers then checked their judgments. Any disagreement was resolved through discussion with a third researcher. A data extraction form was designed in Microsoft Excel to systematically extract the following information: publication year, country, first author, diagnostic criteria source, sample sizes of the experimental and healthy groups, demographic data (sex, age, disease duration), intervention methods for both groups, duration and frequency of interventions, outcome measures (primary and secondary), and adverse events.
2.3.2 Quality assessment
The methodological quality of included studies was evaluated using the risk-of-bias tool integrated in RevMan 5.4 (Cochrane Collaboration), covering the following domains: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessors; (5) completeness of outcome data; (6) selective reporting; and (7) other potential biases. Each domain was classified as having a high risk, low risk, or unclear risk of bias (ROB). Any disagreements in assessment were resolved through discussion with a third investigator.
2.3.3 Statistical analysis
Statistical analyses were conducted using RevMan 5.4. Outcome measures were converted to continuous data, and results were expressed as mean difference (MD) with 95% confidence intervals (CI). Heterogeneity was evaluated using the p-value and I2 statistic. A p-value ≥0.05 combined with I2 ≤ 50% indicated low statistical heterogeneity, whereas a p-value <0.05 and I2 > 50% suggested substantial heterogeneity. Subgroup analyses were subsequently performed to identify potential sources of heterogeneity. Forest plots and funnel plots were generated to assess the heterogeneity of meta-analysis results and publication bias, respectively. Publication bias was considered absent if the funnel plot exhibited symmetry; asymmetry indicated potential publication bias. RevMan 5.4 and Excel were utilized for the creation of graphs and tables.
3 Results
3.1 Study characteristics
A total of 13,107 articles were identified through the search strategy: 100 from PubMed, 155 from Cochrane Library, 168 from Embase, 141 from Web of Science, 2,045 from CNKI, 4,062 from Wan fang, 4,276 from VIP, and 2,160 from CBM. After removing 7,496 duplicates, 4,199 articles were excluded based on title or abstract screening. The remaining 1,412 full-text articles underwent further review, and 42 studies were ultimately included. The detailed selection process is illustrated in Figure 1.
Figure 1

Flow diagram.
Table 1 summarizes the baseline characteristics of the included studies, detailing sample size, gender distribution, age and disease duration at baseline, intervention methods in experimental and healthy groups, stroke types, diagnostic criteria, outcome measures, and adverse events. A total of 42 studies involving 2,766 patients (1,380 in the experimental group and 1,386 in the healthy group) were included. Individual study sample sizes ranged from 22 to 120. Most studies reported gender distribution, with male participants predominating. The mean age of participants was reported separately for experimental and healthy groups in all studies except one, which provided combined data (11). Mean ages across studies ranged from 50 to 65 years. Disease duration was reported separately in 37 studies and combined in one study (11); five studies did not report disease duration. The mean disease duration varied widely, from 6 days to 32 months, meanwhile most studies reported durations between 2 weeks and 4 months. Twenty-four studies (12–35) included both ischemic and hemorrhagic stroke; 8 studies (36–43) enrolled ischemic stroke only, 10 studies (11, 44–52) did not specify stroke type.
Table 1
| Trial Name | Sample size | Sex (male/female) | Age (years) | Disease course (months) | Methods of intervention | Extra acupuncture location | Therapy duration (weeks) | Type of stroke | Source of diagnostic criteria | Outcome measures | Adverse reactions | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | T | C | T | C | |||||||
| Huang Xinyun 2024 (12) | 32 | 32 | 26/6 | 22/10 | 58.56 ± 11.85 | 60.25 ± 12.17 | 5.00 (3.25, 12.00) | 6.00 (2.00, 11.00) | Traditional acupuncture | Acupuncture | Hand, arm, head and body | 4 | Ischemic or hemorrhage stroke | Not specified in detail | BRS, MAS, MMT, MBI | Not reported |
| Zhang Miao 2024 (36) | 30 | 30 | 23/7 | 20/10 | 66.4 ± 8.4 | 69.4 ± 11.6 | 1.6 ± 1.1 | 1.7 ± 1.5 | Traditional acupuncture | Acupuncture | Hand | 4 | Ischemic stroke | CT or MRI, Chinese expert consensus standards and guidelines | BRS, FMA, MAS, ROM | Not reported |
| Xie Qing 2024 (13) | 30 | 30 | 23/7 | 19/11 | 60.27 ± 14.04 | 57.9 ± 8.91 | Not reported | Not reported | Electroacupuncture | Rehabilitation + Functional electrical stimulation therapy | Hand, arm and head | 4 | Ischemic or hemorrhage stroke | Chinese expert consensus standards | BRS, FMA, MBI | Not reported |
| Liu Hong 2024 (14) | 50 | 50 | 24/26 | 27/23 | 56 ± 5 | 57 ± 4 | 2.51 ± 0.98 | 2.15 ± 0.75 | Warm Needling | Rehabilitation + Extracorporeal shock wave therapy | Hand, Arm, Head and Body | 6 | Ischemic or hemorrhage stroke | Chinese expert consensus standards | FMA | Not reported |
| Guo Bao 2024 (15) | 51 | 51 | 27/24 | 29/22 | 56.17 ± 5.38 | 56.81 ± 5.41 | 2.83 ± 0.52 | 2.76 ± 0.51 | Traditional acupuncture | Rehabilitation | Hand, arm and head | 4 | Ischemic or hemorrhage stroke | Chinese guidelines | BRS | Not reported |
| Wang Peixin 2023 (16) | 30 | 30 | 17/13 | 18/12 | 52.30 ± 7.86 | 53.83 ± 13.05 | 0.842 ± 0.268 | 0.821 ± 0.277 | Traditional acupuncture | Rehabilitation | Arm | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese guidelines and instructional books | BRS, FMA, MBI | Not reported |
| Fan Sujin 2023 (44) | 35 | 35 | 16/19 | 18/17 | 58.60 ± 7.23 | 58.77 ± 6.08 | 1.830 ± 0.345 | 1.801 ± 0.348 | Traditional acupuncture | Acupuncture | Hand | 4 | Stroke | CT/MRI, Chinese guidelines | FMA, MAS | Not reported |
| Fan Dongqing 2023 (17) | 30 | 33 | 16/14 | 17/16 | 56.90 ± 9.40 | 58.58 ± 10.56 | 3.07 ± 1.50 | 3.41 ± 1.80 | Traditional acupuncture | Acupuncture | Hand | 2 | Ischemic or hemorrhage stroke | CT/MRI, Chinese guidelines | BRS, FMA, MAS, MBI | T: 1 case felt pain. |
| Zhao Fengfan 2022 (18) | 30 | 30 | 18/12 | 14/16 | 62.9 ± 8.74 | 65.27 ± 9.51 | 3.24 ± 1.64 | 3.26 ± 1.35 | Warm Needling | Rehabilitation | Hand | 4 | Ischemic or hemorrhage stroke | CT/MRI Chinese guidelines and instructional books | BRS, FMA | Not reported |
| Zhang Xinzhi 2022 (45) | 25 | 25 | 11/14 | 12/13 | 65.16 ± 9.20 | 65.96 ± 8.98 | 3.34 ± 1.07 | 3.42 ± 1.04 | Electroacupuncture | Rehabilitation | Hand and arm | 3 | Stroke | CT or MRI, Chinese expert consensus standards and guidelines | FMA, MAS, MBI | Not reported |
| Xu Weiyan 2022 (19) | 30 | 30 | 18/12 | 16/14 | 60.47 ± 7.86 | 60.80 ± 8.56 | 2.73 ± 1.47 | 3.12 ± 1.50 | Traditional acupuncture | Rehabilitation + Acupuncture | Hand | 4 | Ischemic or hemorrhage stroke | CT, Chinese guidelines | BRS, Lindmark, ROM, MBI | Not reported |
| Shao Yinjin 2022 (20) | 42 | 43 | 24/18 | 20/23 | 54.14 ± 4.59 | 54.40 ± 7.28 | 2.16 ± 0.64 | 2.04 ± 0.69 | Fire Needling | Rehabilitation | Arm | 6 | Ischemic or hemorrhage stroke | Chinese guidelines | FMA, MAS | Not reported |
| Long Xiaona 2022 (21) | 30 | 31 | 18/12 | 17/14 | 63 ± 12 | 65 ± 9 | 0.733 ± 0.583 | 0.727 ± 0.522 | Electroacupuncture | Rehabilitation + Rehabilitation Robot | Hand | 6 | Ischemic or hemorrhage stroke | Chinese guidelines | BRS, FMA, ROM | Not reported |
| Chen Ying 2022 (37) | 32 | 32 | 17/15 | 18/14 | 57.25 ± 8.199 | 56.00 ± 8.436 | 2.85 ± 1.28 | 2.92 ± 1.08 | Traditional acupuncture | Rehabilitation + Acupuncture | Hand | 4 | Ischemic stroke | Chinese guidelines | FMA, MAS | Not reported |
| Ma Nanda 2021 (38) | 30 | 30 | 21/9 | 18/12 | 51.67 ± 12.430 | 55.23 ± 10.258 | Not reported | Not reported | Traditional acupuncture | Rehabilitation | Hand, arm and head | 4 | Ischemic stroke | CT/MRI | BRS, MBI | Not reported |
| Jia Yanfei 2021 (46) | 49 | 48 | 28/21 | 29/19 | 53.45 ± 6.60 | 52.65 ± 5.49 | 10.2 ± 1.92 | 9.96 ± 1.56 | Electroacupuncture | Acupuncture | Arm | 4 | Stroke | Chinese expert consensus standards and guidelines | BRS, Lindmark | Not reported |
| Huang Linying 2021 (22) | 30 | 30 | 15/15 | 18/12 | 60.63 | 58.87 | Not reported | Not reported | Traditional acupuncture | Acupuncture | Hand + arm | 5 | Ischemic or hemorrhage stroke | Chinese guidelines | BRS, FMA, MAS | Not reported |
| Duan Yifei 2021 (39) | 30 | 30 | 17/13 | 16/14 | 56.2 ± 9.4 | 55.3 ± 10.0 | 1.04 ± 0.32 | 1.09 ± 0.29 | Traditional acupuncture | Rehabilitation | Hand + arm | 8 | Ischemic stroke | Chinese expert consensus standards | FMA, MAS, MBI | Not reported |
| Dou Jie 2021 (40) | 47 | 47 | 29/18 | 27/20 | 58.53 ± 12.66 | 56.74 ± 14.90 | 31.38 ± 24.79 | 32.61 ± 19.46 | Electroacupuncture | Rehabilitation + Acupuncture | Hand + arm | 4 | Ischemic stroke | CT/MRI, Chinese guidelines | BRS, MBI | Not reported |
| Wang Xiaochun 2020 (47) | 33 | 34 | 18/15 | 16/18 | 51 ± 9 | 53 ± 10 | 2.16 ± 1.27 | 2.06 ± 1.09 | Traditional acupuncture | Rehabilitation | Hand + arm | 4 | Stroke | CT/MRI, Chinese guidelines | FMA, MAS, MBI | T: 1 case felt pain. |
| Yuan Qin 2020 (23) | 30 | 30 | 18/12 | 15/15 | 64.65 ± 2.51 | 65.34 ± 2.68 | Not reported | Not reported | Traditional acupuncture | Rehabilitation + Acupuncture | Hand | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese guidelines | FMA, MBI | Not reported |
| Ma Lifei 2020 (48) | 20 | 20 | 12/8 | 11/9 | 61.85 ± 8. 28 | 60.45 ± 7. 08 | 1.45 ± 0. 68 | 1. 50 ± 0. 68 | Traditional acupuncture | Rehabilitation | Hand and arm | 4 | Stroke | Chinese guidelines | BRS, MBI | Not reported |
| Liu Juan 2020 (24) | 30 | 30 | 16/14 | 13/17 | 60.35 ± 6.20 | 61.67 ± 7.20 | 0.553 ± 0.253 | 0.549 ± 0.243 | Fire needling | Acupuncture | Hand, arm and head | 2 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | BRS, MBI | Not reported |
| Zhang Xuan 2019 (25) | 20 | 20 | 14/6 | 11/9 | 54.13 ± 12.73 | 55.21 ± 12.09 | 3.82 ± 2.16 | 3.78 ± 2.69 | Traditional acupuncture | Rehabilitation | Hand and arm | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | FMA, MBI | Not reported |
| Xian Zuxin 2019 (41) | 43 | 43 | 23/20 | 26/17 | 65.27 ± 6.56 | 64.79 ± 6.48 | 2.79 ± 0. 54 | 2.83 ± 0.56 | Electroacupuncture | Rehabilitation + Functional electrical stimulation therapy | Hand | 6 | Ischemic stroke | CT/MRI, Chinese guidelines | Lindmark, MBI | Not reported |
| Liu Jun’e 2019 (26) | 60 | 60 | 33/17 | 35/25 | 60.60 ± 10.86 | 60.83 ± 9.62 | 2.77 ± 0.95 | 2.47 ± 0.94 | Electroacupuncture | Rehabilitation | Hand and arm | 10 | Ischemic or hemorrhage stroke | Chinese expert consensus standards | FMA, MAS | Not reported |
| Ling Shanshan 2019 (42) | 22 | 22 | 17/5 | 13/9 | 63.18 ± 9.93 | 57.77 ± 14.26 | 1.81 ± 1.57 | 2.197 ± 1.43 | Traditional acupuncture | Rehabilitation | Body | 4 | Ischemic stroke | CT/MRI, Chinese instructional books | BRS, MBI | Not reported |
| Fan Hongyang 2019 (27) | 30 | 30 | 19/11 | 19/11 | 61.3 ± 9.3 | 61.6 ± 9.6 | 3.7 ± 2.5 | 3.6 ± 2.4 | Traditional acupuncture | Acupuncture | Hand | 2 | Ischemic or hemorrhage stroke | CT/MRI, Chinese guidelines and instructional books | BRS, FMA, MAS | Not reported |
| Chen Siqi 2018 (28) | 30 | 31 | 16/14 | 17/14 | 59 ± 7 | 58 ± 6 | 3.91 ± 1.44 | 3.31 ± 1.17 | Traditional acupuncture | Rehabilitation | Hand | 9 | Ischemic or hemorrhage stroke | Chinese expert consensus standards | FMA, MAS | T: 4 cases felt pain. |
| Weng Yilin 2018 (29) | 29 | 27 | 18/11 | 15/12 | 56.90 ± 10.88 | 55.67 ± 10.57 | 0.97 ± 0.27 | 1.05 ± 0.19 | Electroacupuncture | Rehabilitation | Arm | 4 | Ischemic or hemorrhage stroke | American and Chinese guidelines | FMA, MBI | Not reported |
| Sun Dingjiong 2018 (49) | 25 | 25 | 11/9 | 8/12 | 63.27 ± 8.12 | 62.09 ± 7.89 | 0.41 ± 0.18 | 0.47 ± 0.17 | Traditional acupuncture | Rehabilitation | Hand, arm and head | 6 | Stroke | CT/MRI, Chinese guidelines | FMA, MBI | Not reported |
| Tian Meng 2017 (30) | 30 | 30 | 16/14 | 17/13 | 50.2 ± 4.6 | 49.9 ± 4.0 | 0.67 ± 0.14 | 0.63 ± 0.11 | Electroacupuncture | Rehabilitation + Acupuncture | Hand | 12 | Ischemic or hemorrhage stroke | Chinese expert consensus standards | FMA, MAS, MBI | Not reported |
| Zhang Rui 2017 (31) | 20 | 20 | 16/4 | 18/2 | 55.15 ± 10.97 | 54.90 ± 11.29 | 0.71 ± 0.72 | 1.11 ± 1.03 | Traditional acupuncture | Rehabilitation+Mirror Therapy | Head | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | BRS | Not reported |
| Wang Jie 2016 (50) | 43 | 43 | 26/17 | 23/20 | 50.55 ± 12.99 | 51.45 ± 10.48 | 0.18 ± 0.11 | 0.16 ± 0.14 | Traditional acupuncture | Rehabilitation | Hand | 4 | Stroke | CT/MRI, Chinese expert consensus standards | FMA, MBI | Not reported |
| Tulunayi Wanli 2016 (32) | 45 | 45 | 22/23 | 13/21 | 56.7 ± 4.5 | 56.2 ± 4.1 | 1.58 ± 0.39 | 1.55 ± 0.35 | Traditional acupuncture | Rehabilitation | Hand, arm and head | 6 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | FMA, MBI | Not reported |
| Yang Jiangxia 2015 (51) | 40 | 40 | 27/13 | 25/15 | 60 ± 9 | 61 ± 9 | 2.52 ± 0.77 | 2.49 ± 0.71 | Floating Needle Technique | Rehabilitation | Arm | 8 | Cerebrovascular disease | Chinese instructional books | FMA, MAS, MBI | Not reported |
| Jin Yisi 2015 (52) | 18 | 18 | 9/9 | 10/8 | 57.81 ± 2.12 | 58.72 ± 3.14 | 0.261 ± 0.020 | 0.257 ± 0.017 | Electroacupuncture | Rehabilitation | Arm | 3 | Stroke | Chinese guidelines | BRS | Not reported |
| Cui Shaoyang 2015 (33) | 32 | 32 | 19/13 | 18/14 | 51.19 ± 7.89 | 52.28 ± 7.39 | 0.91 ± 0.19 | 0.94 ± 0.21 | Traditional acupuncture | Rehabilitation + Mirror therapy | Hand, arm and head | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | BRS, MBI | Not reported |
| Jiang Zaiyi 2014 (34) | 11 | 11 | Not reported | Not reported | 55.55 ± 8.98 | 52.73 ± 14.55 | 1.70 ± 3.21 | 0.715 ± 1.01 | Electroacupuncture | Rehabilitation | Hand, arm and head | 2 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | FMA | Not reported |
| Zhou Yu 2013 (35) | 32 | 35 | 19/13 | 21/14 | 55.67 ± 8.75 | 57.09 ± 9.02 | 0.205 ± 0.048 | 0.197 ± 0.052 | Traditional acupuncture | Rehabilitation | Head and hand | 4 | Ischemic or hemorrhage stroke | CT/MRI, Chinese expert consensus standards | FMA, MBI | Not reported |
| Zhuang Lixing 2011 (43) | 44 | 43 | 23/21 | 24/19 | 65.47 ± 6.33 | 63.53 ± 7.35 | 1.45 ± 0.21 | 1.31 ± 0.24 | Traditional Acupuncture | Rehabilitation | Hand, arm and head | 5 | Ischemic stroke | CT/MRI, Chinese expert consensus standards | BRS | C: 1 case was hematoma. |
| Chen Anliang 2008 (11) | 30 | 30 | Not reported | Not reported | Not specified in detail | Not specified in detail | Not specified in detail | Not specified in detail | Traditional Acupuncture | Rehabilitation | Hand and arm | 4 | Stroke | CT/MRI, Chinese expert consensus standards | Lindmark, MBI | Not reported |
Characteristics of all included RCTs.
BRS, Brunnstrom Recovery stage (hand); FMA, Fugl-Meyer assessment (hand); Lindmark, Lindmark assessment (hand); MAS, Modified Ashworth Scale Assessment; ROM, range of motion; MBI, Modified Barthel Index. C, control group; T, test group.
In this study, the healthy groups of 8 studies (12, 17, 22, 24, 27, 36, 44, 46) utilized acupuncture therapy, while 23 studies (11, 15, 16, 18, 20, 25, 26, 28, 29, 32, 34, 35, 38, 39, 42, 43, 45, 47–52) employed conventional rehabilitation therapy in their healthy groups. The healthy groups of 5 studies (19, 23, 30, 37, 40) adopted acupuncture combined with conventional rehabilitation therapy, and 6 studies (13, 14, 21, 31, 33, 41) implemented conventional rehabilitation therapy integrated with novel rehabilitation methods. One study (42) administered sham acupuncture combined with rehabilitation therapy in the healthy group. Building upon the healthy group interventions, 26 studies (11, 12, 15–17, 19, 22, 23, 25, 27, 28, 31–33, 35–39, 42–44, 47–50) incorporated traditional acupuncture (TA) as an additional intervention, 11 studies (13, 21, 26, 29, 30, 34, 40, 41, 45, 46, 52) utilized EA, 2 studies (14, 18) applied warm acupuncture, 2 studies (20, 24) implemented fire acupuncture, and 1 study (51) adopted floating acupuncture. Adverse events were reported in 4 studies: two studies (17, 47) documented one case of pain in the experimental group, one study (28) reported four cases of pain in the experimental group, and one study (43) observed one case of subcutaneous hematoma in the healthy group.
3.2 Risk of bias
3.2.1 Random sequence generation
Random sequence generation was described in 39 studies, among which 32 studies were assessed as low ROB. Specifically, 25 studies (13–17, 20, 24, 25, 27, 30, 31, 33, 34, 36, 39, 41, 42, 44–46, 48–52) utilized random number tables for sequence generation, while 7 studies (12, 22, 28, 29, 37, 43, 47) employed computer-generated randomization. Seven studies (11, 18, 21, 23, 26, 32, 38) were classified as unclear ROB due to insufficient methodological details, as they mentioned randomization without specifying the generation method. Three studies (19, 35, 40) were deemed high ROB because they assigned participants based on chronological order of enrollment.
3.2.2 Allocation concealment
Three studies (12, 43, 47) implemented allocation concealment using sealed envelopes, and one study (30) mentioned allocation concealment without specifying the methodology. These studies were evaluated as low ROB. The remaining 38 studies (11, 13–29, 31–42, 44–46, 48–52) ignored the description of allocation concealment and were thus classified as unclear ROB.
3.2.3 Blinding of participants and personnel
One study (12) adopted a double-blind design, and five studies (16, 17, 29, 36, 47) utilized a single-blind design; these were assessed as low ROB. The remaining 36 studies (11, 13–15, 18–28, 30–35, 37–46, 48–52) did not report the application of blinding for participants or personnel, resulting in an unclear ROB classification.
3.2.4 Blinding of outcome assessment
Two studies (12, 29) applied blinding to outcome assessment and were therefore rated as low ROB. The remaining 40 studies did not describe the implementation of blinding for outcome assessment and were consequently deemed unclear ROB.
3.2.5 Completeness of outcome data
Nine studies (12, 17, 20, 25, 28, 29, 37, 44, 47) explicitly reported dropouts and provided reasons for attrition or described methods for handling missing data. Thirty studies (11, 13–15, 18, 19, 21–24, 26, 27, 30–35, 38–43, 46, 48–52) documented no participant withdrawals during the trial. These studies were assessed as low ROB. Two studies (16, 45) reported dropouts but failed to clarify the reasons or data management strategies, and one study (36) exhibited significant data entry errors in one outcome measure; these were classified as high ROB.
3.2.6 Selective reporting
All included studies reported all predefined outcome measures. Five studies (11, 13, 22, 23, 38) were deemed high ROB due to failure to separately report the disease course across intervention groups. The remaining 37 studies (12, 14–21, 24–37, 39–52) were evaluated as low ROB.
3.2.7 Other risks of bias
No studies reported information related to other sources of bias, resulting in an unclear ROB classification. Potential language bias may exist as only studies published in Chinese or English were included. Additionally, the predominance of studies conducted in China introduces potential geographical bias. ROB graph results are shown in Figure 2.
Figure 2
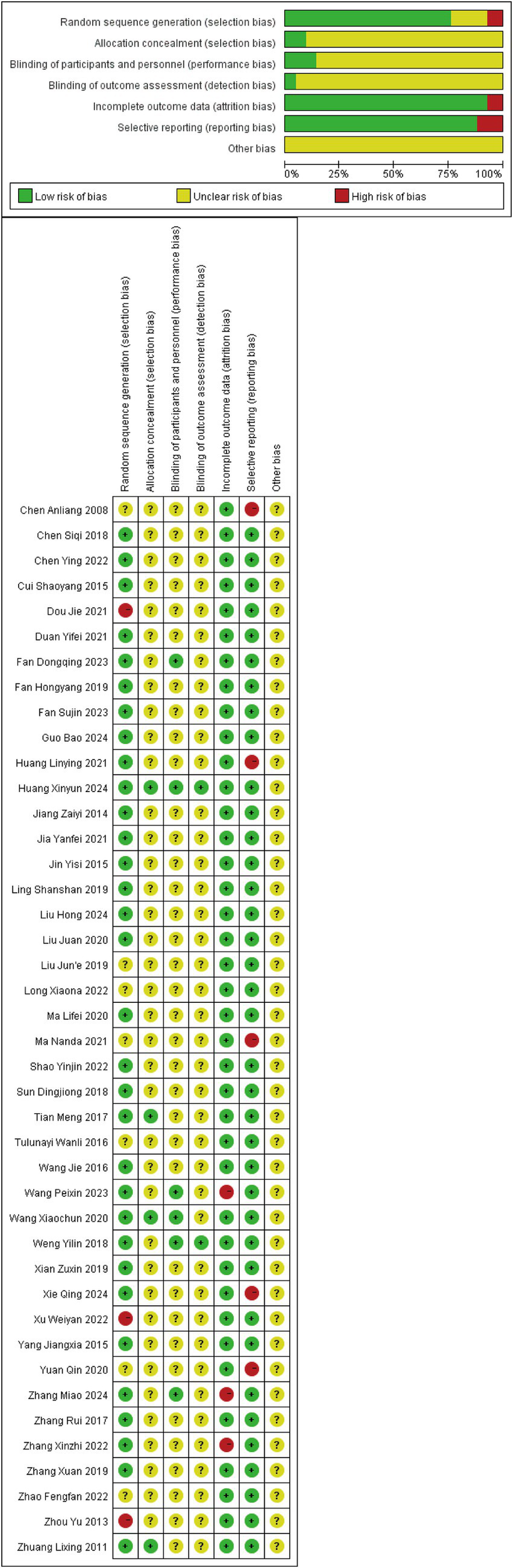
Risk of bias graph.
3.3 Meta-analysis of results
3.3.1 Brunnstrom recovery stage (BRS)
A total of 21 studies (12, 13, 15–19, 21, 22, 24, 27, 31, 33, 36, 38, 40, 42, 43, 46, 48, 52) reported BRS as an outcome measure, involving 1,329 patients (664 in the experimental group and 665 in the healthy group). The random-effects meta-analysis demonstrated a significant improvement in hand BRS with acupuncture (MD = 0.56, 95% CI = 0.43–0.69, Chi2 = 45.12, p = 0.001, I2 = 56%), indicating that acupuncture effectively improves the BRS of the hand in stroke patients.
Analysis of 14 studies employing TA showed low within-subgroup heterogeneity (MD = 0.45, 95% CI = 0.32–0.59; p = 0.08, I2 = 37%). Similarly, the EA subgroup exhibited low heterogeneity (MD = 0.77, 95% CI = 0.58–0.96; p = 0.23, I2 = 28%). Subgroup analysis of two studies utilizing other acupuncture methods demonstrated high heterogeneity (MD = 0.75, 95% CI = 0.11–1.38; p = 0.09, I2 = 65%). These findings suggest that the choice of different acupuncture methods contributed to the heterogeneity. Details are presented in Figure 3.
Figure 3
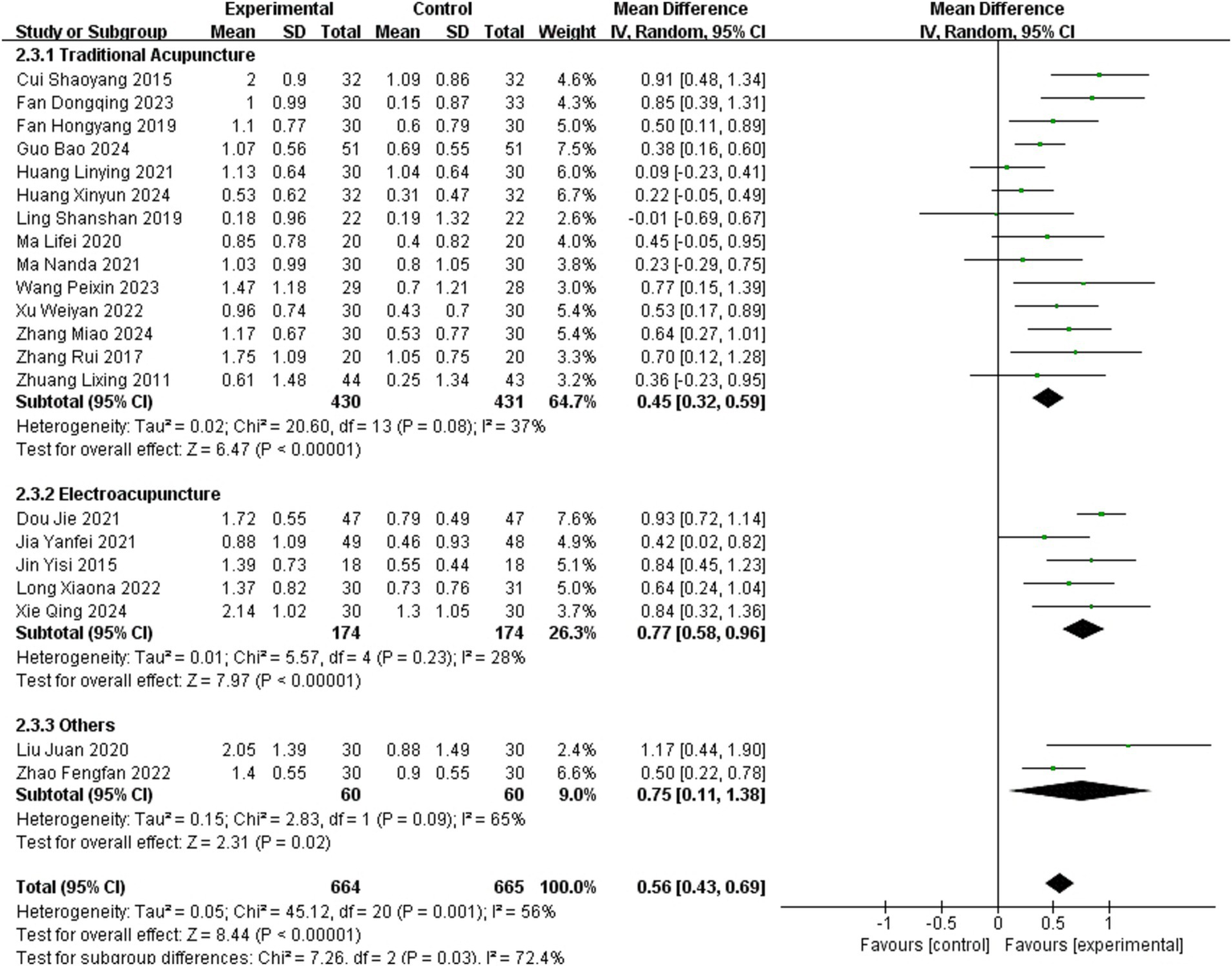
Meta-analysis of the effects of different acupuncture methods on BRS.
The subgroup analysis explained heterogeneity in BRS. Significant differences in effect sizes were observed between subgroups (Chi2 = 7.26, p = 0.03, I2 = 72.4%), whereas within-subgroup heterogeneity was negligible. Pairwise comparisons identified statistically significant differences between TA and EA subgroups (Chi2 = 6.95, p = 0.008 [<0.0167], I2 = 85.6%), with no significant differences in other comparisons. This suggests distinct effects of TA and EA on BRS. Bonferroni correction is shown in Supplementary File 2.
3.3.2 Fugl-Meyer assessment (FMA)
A total of 27 studies (13, 14, 16–18, 20–23, 25–30, 32, 34–37, 39, 44, 45, 47, 49–51) reported FMA as an outcome measure, involving 1,769 patients (881 in the experimental group and 888 in the healthy group). The random-effects meta-analysis revealed a large effect size favoring acupuncture (SMD = 1.24, 95% CI = 0.96–1.53, Chi2 = 189.71, p < 0.001, I2 = 86%).
Subgroup analysis of 16 studies employing TA demonstrated significant within-subgroup heterogeneity (SMD = 1.50, 95% CI = 1.02–1.98; p < 0.001, I2 = 91%). In contrast, subgroup analysis of 7 studies using EA exhibited low heterogeneity (SMD = 1.14, 95% CI = 0.88–1.40; p = 0.16, I2 = 36%). Subgroup analysis of 4 studies utilizing other acupuncture methods also showed low heterogeneity (SMD = 0.81, 95% CI = 0.58–1.04; p = 0.75, I2 = 0%). It suggested that heterogeneity differences between subgroups may be associated with acupuncture methods. Details are presented in Figure 4.
Figure 4
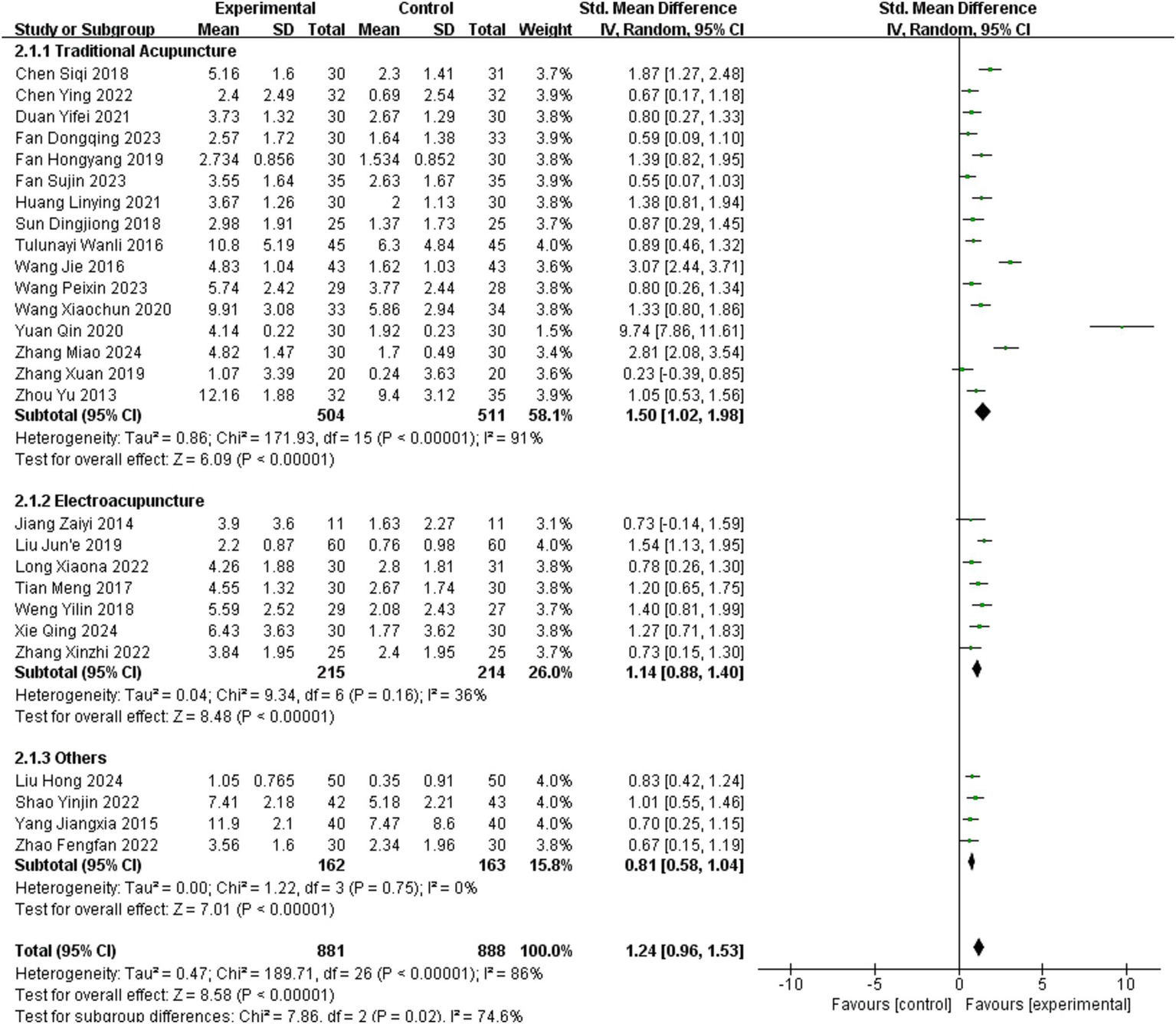
Meta-analysis of the effects of different acupuncture methods on FMA.
The subgroup analysis partially explained the heterogeneity in FMA. Significant differences in effect sizes were observed between subgroups (Chi2 = 7.86, p = 0.02, I2 = 74.6%). Pairwise comparisons indicated potential statistical differences primarily between the TA and other acupuncture methods subgroups. However, due to the diversity of techniques categorized under “others” and the study’s primary focus on comparing TA with EA, no further analyses were conducted. After excluding a study in which potential data – entry errors might have occurred (36), the research findings of this part remained unaffected.
3.3.3 Lindmark
Four studies (11, 19, 41, 46) reported the Lindmark as an outcome measure, involving 303 patients (152 in the experimental group and 151 in the healthy group). A random-effects model showed that acupuncture was equally effective in improving Lindmark scores (SMD = 1.34, 95 %CI = 0.38–2.30, Chi2 = 41.43, p < 0.001, I2 = 93%).
Analysis of 2 studies employing TA showed a significant improvement in hand Lindmark scores (SMD = 1.21, 95% CI = 0.09–2.33; p = 0.005, I2 = 87%). In contrast, subgroup analysis of 2 studies using EA revealed inconclusive effects on Lindmark scores (SMD = 1.48, 95% CI = −0.50–3.46; p < 0.001, I2 = 97%).
Differences in effect sizes between subgroups were not statistically significant (Chi2 = 0.05, p = 0.82, I2 = 0%). However, due to the limited number of included studies and substantial variability among them, these findings should be interpreted with caution. Details are presented in Figure 5.
Figure 5
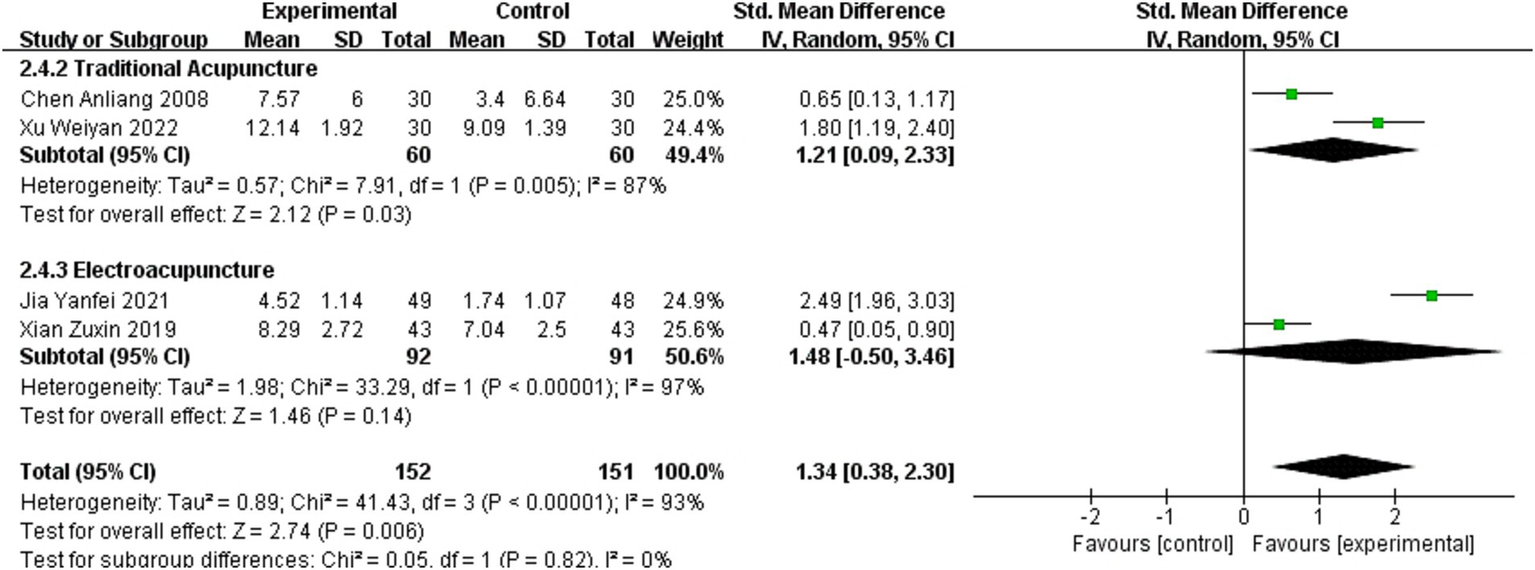
Meta-analysis of the effects of different acupuncture methods on Lindmark scores.
3.3.4 Modified Ashworth Scale (MAS)
Fifteen studies (12, 17, 20, 22, 26–28, 30, 36, 37, 39, 44, 45, 47, 51) reported MAS as an outcome measure, involving 1,024 patients (509 in the experimental group and 515 in the healthy group). The fixed – effect model indicates that acupuncture was effective in improving MAS scores in stroke patients, showing excellent consistency (MD = −0.48, 95% CI = −0.59–0.38, Chi2 = 16.13, p = 0.31, I2 = 13%).
Analysis of 10 studies using TA showed low within-subgroup heterogeneity (MD = −0.50, 95% CI = −0.63–0.37; p = 0.17, I2 = 30%). Subgroup analysis of 3 studies applying EA demonstrated negligible heterogeneity (MD = −0.60, 95% CI = −0.83–0.37; p = 0.98, I2 = 0%). Subgroup analysis of 2 studies utilizing other acupuncture methods suggested high heterogeneity (MD = −0.31, 95% CI = −0.55–0.07; p = 0.58, I2 = 65%).
No significant differences in effect sizes were observed between subgroups (Chi2 = 2.98, p = 0.22, I2 = 33.0%), implying comparable efficacy among different acupuncture regimens in improving hand MAS grades in stroke patients. Details are presented in Figure 6.
Figure 6
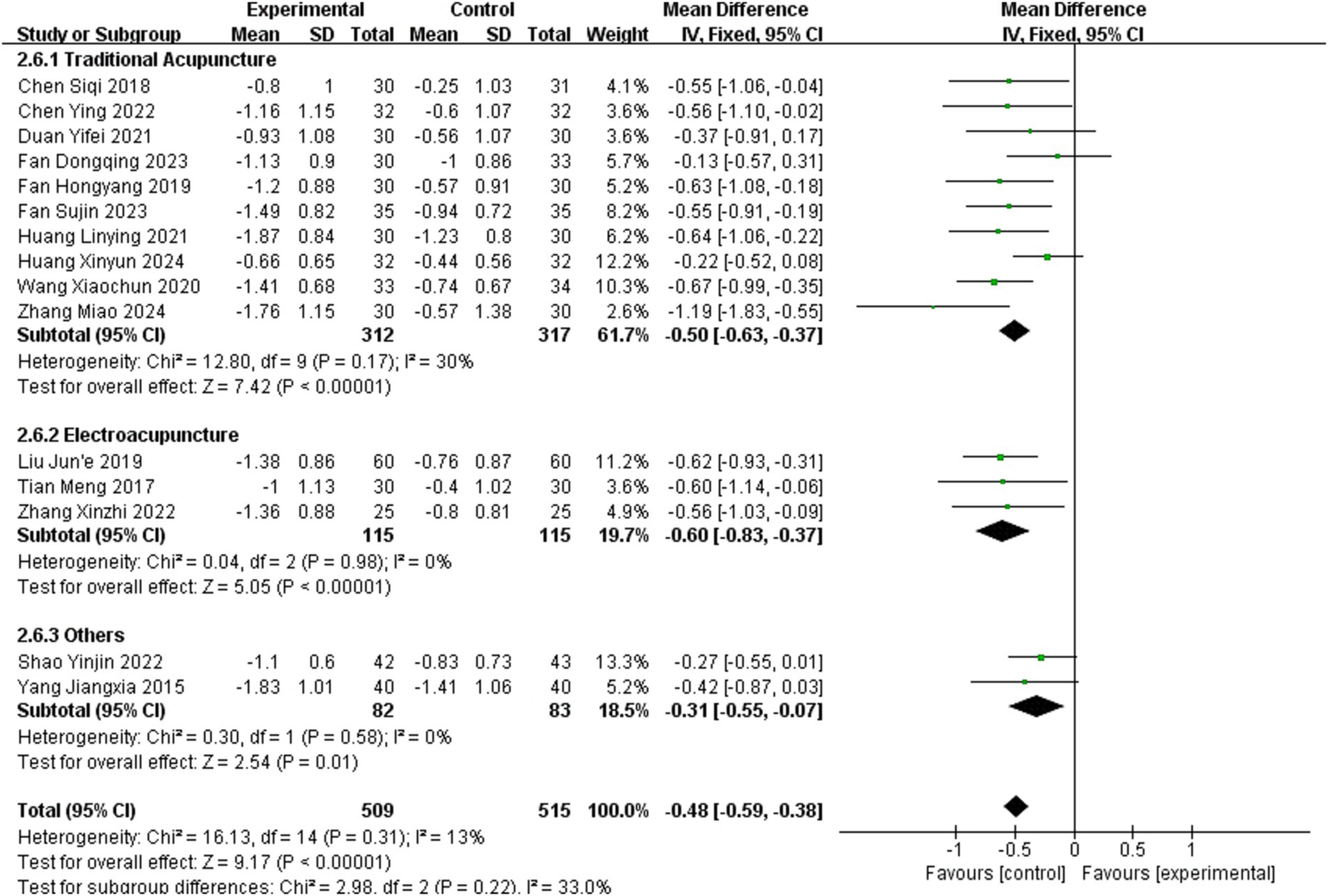
Meta-analysis of the effects of different acupuncture methods on MAS.
3.3.5 Range of motion (ROM)
Three studies (19, 21, 36) reported ROM as an outcome measure, involving 181 patients (90 in the experimental group and 91 in the healthy group). Pooled data from the meta-analysis demonstrated that acupuncture improved hand ROM in stroke patients (SMD = 0.95, 95% CI = 0.64–1.26; p = 0.71, I2 = 0%).
Subgroup analysis was not performed due to the limited number of studies and the unambiguous effect size. Details are presented in Figure 7.
Figure 7
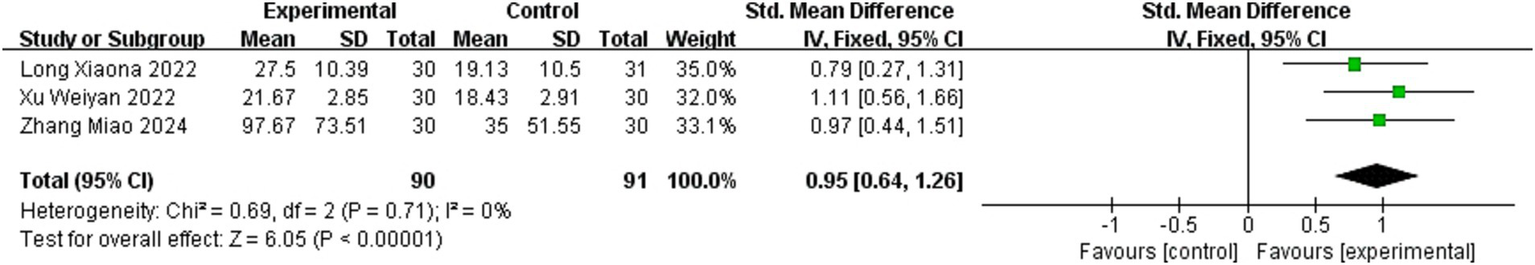
Meta-analysis of the effects of different acupuncture methods on ROM.
3.3.6 Modified Barthel Index (MBI)
Twenty-five studies (11–13, 16, 17, 19, 23–25, 29, 30, 32, 33, 35, 38–42, 45, 47–51) reported MBI as an outcome measure, involving 1,578 patients (787 in the experimental group and 791 in the healthy group). The random – effects model demonstrated the effectiveness of acupuncture, accompanied by substantial heterogeneity (MD = 6.70, 95% CI = 4.85–8.55, Chi2 = 256.23, p < 0.001, I2 = 91%).
Subgroup analysis based on acupuncture methods was performed using a random-effects model. The analysis showed high heterogeneity within the TA subgroup (MD = 6.21, 95% CI = 3.80–8.63; p < 0.001, I2 = 88%). Similarly, EA subgroup exhibited substantial heterogeneity (MD = 7.32, 95% CI = 3.33–11.30; p < 0.001, I2 = 89%). The two studies employing other acupuncture methods also demonstrated high heterogeneity (MD = 9.02, 95% CI = 3.32–14.71; p = 0.03, I2 = 78%). Further details are provided in Figure 8.
Figure 8
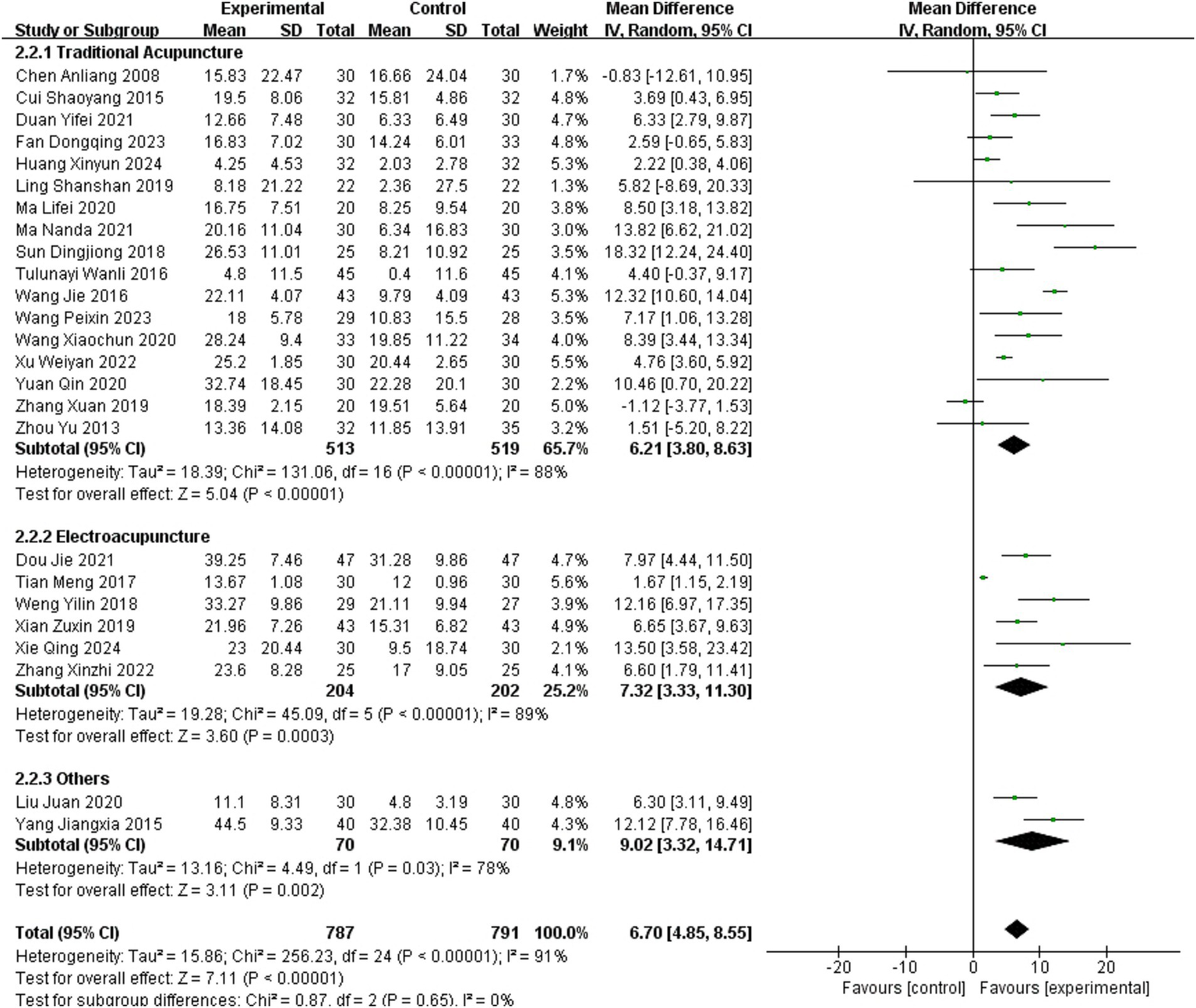
Meta-analysis of the effects of different acupuncture methods on MBI.
As subgroup analyses stratified by acupuncture methods failed to account for the heterogeneity in the Modified Barthel Index (MBI), a secondary subgroup analysis was performed by categorizing studies into two groups using a baseline MBI score of 50 as the threshold. For studies involving patients with baseline MBI scores ≥50, the subgroup exhibited low heterogeneity (MD = 4.24, 95% confidence interval CI = 2.30–6.19; p = 0.19, I2 = 32%). In contrast, significant heterogeneity persisted in the subgroup with baseline MBI scores <50 (MD = 7.39, 95% CI = 5.04–9.74; p < 0.001, I2 = 93%). Subgroup analysis based on MBI scores partially explained the heterogeneity in acupuncture’s effects on MBI outcomes among stroke patients. Compared with patients with high MBI scores, acupuncture might have a more significant effect on patients with low MBI scores (Chi2 = 4.09, p = 0.04 [>0.025], I2 = 75.6%). Further details are available in Figure 9.
Figure 9
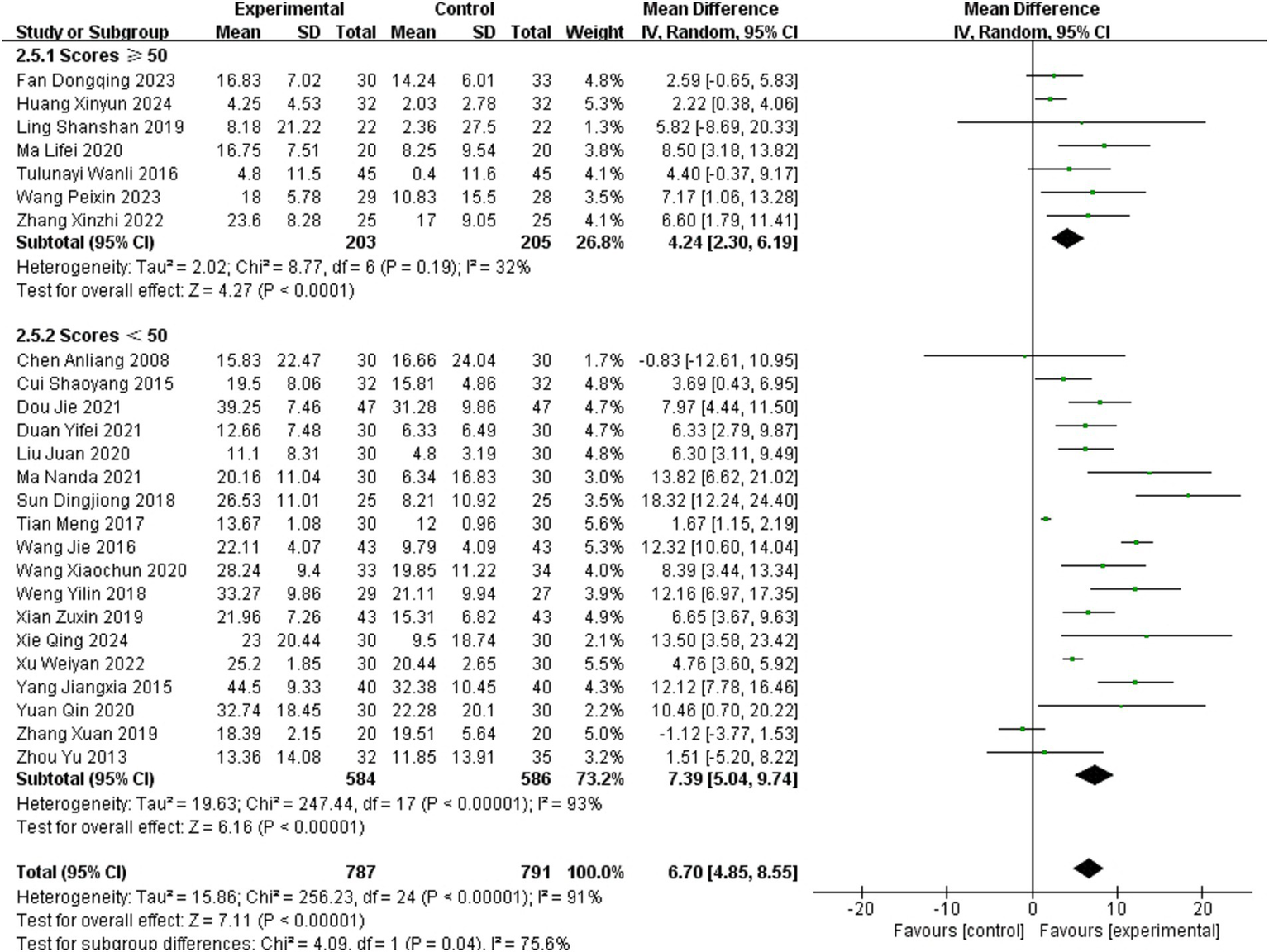
Meta-analysis of acupuncture effects on the MBI stratified by baseline scores.
3.3.7 Manual Muscle Testing (MMT)
Only one study (12) compared the MMT scores between the experimental and healthy groups, reporting no statistically significant effect (p = 0.311). Consequently, subgroup analysis was not performed due to insufficient data.
3.3.8 Sensitivity analysis
Sensitivity analysis was conducted using RevMan 5.4. Funnel plots for all outcome measures were generated, with symmetrical distributions suggesting low publication bias (Figure 10). To evaluate the stability of the results, sensitivity analyses were performed by sequentially excluding individual studies. The pooled effect sizes exhibited minimal fluctuation, confirming the robustness of the findings. GRADEpro was used to assess the certainty in the body of evidence for each outcome evaluated. The results indicated that the overall confidence level of the evidence was moderate (Figure 11).
Figure 10
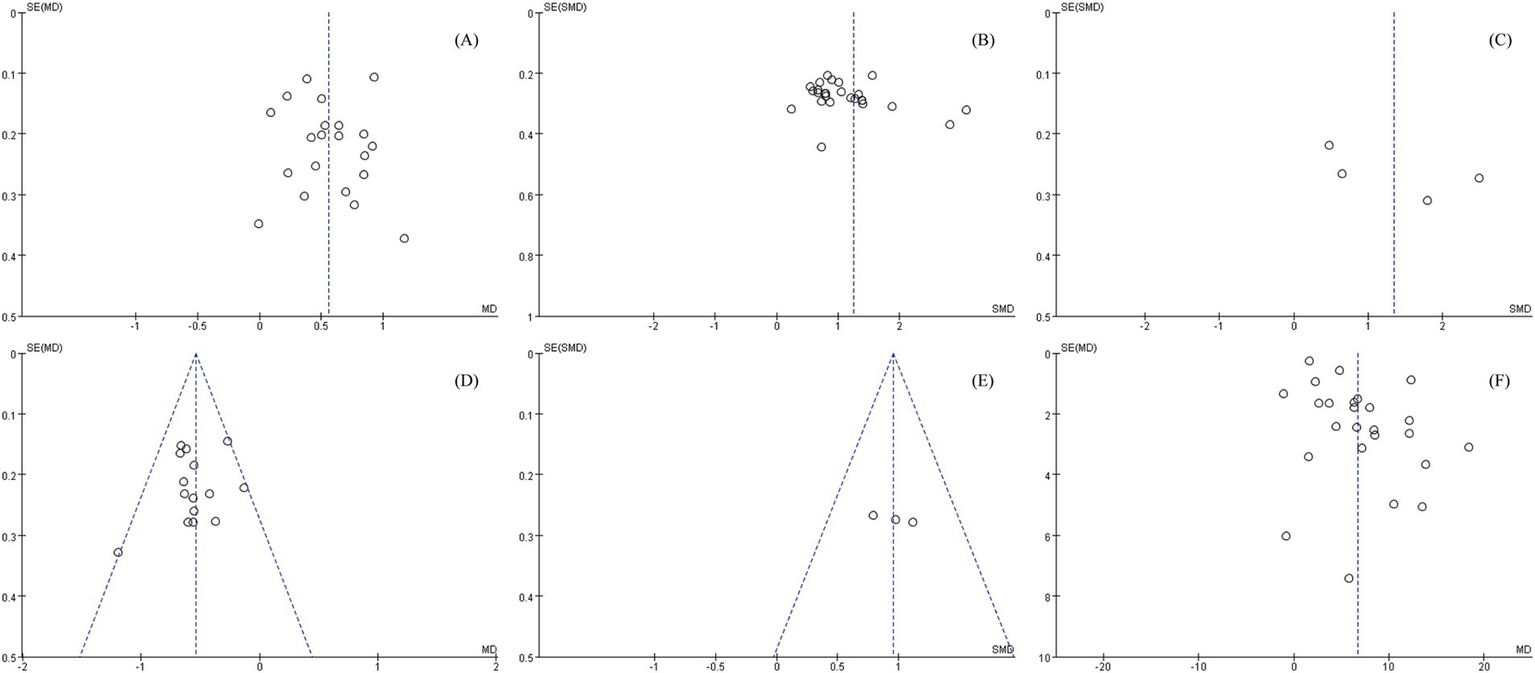
Sensitivity analyses of various outcome indicators, (A) BRS, (B) FMA, (C) Lindmark, (D) MAS, (E) ROM, (F) MBI.
Figure 11

Robustness of the synthesized results.
4 Discussion
In this study, we enhanced the credibility and quality of the research by implementing rigorous experimental controls, including standardized protocols and strict adherence to pre-defined inclusion/exclusion criteria. These measures minimized potential confounding variables, ensuring that the observed therapeutic effects could be attributed specifically to acupuncture. To our knowledge, this is the first investigation to evaluate the efficacy of acupuncture for post-stroke hand dysfunction using a comprehensive rehabilitation assessment framework to quantify functional outcomes. This study systematically evaluated the safety and efficacy of acupuncture in improving hand function in stroke patients through a meta-analysis of 42 trials. The results demonstrated that acupuncture significantly improved hand muscle tone, ROM, and functional performance, while also enhancing activities of daily living. Moreover, acupuncture exhibited favorable tolerability, high compliance, and a low incidence of adverse events, with no severe complications reported. We compared TA methods with EA. Notably, EA demonstrated superior efficacy to TA in enhancing BRS stages, with lower heterogeneity observed in improving FMA scores.
It is noteworthy that blinding implementation in acupuncture research remains a critical methodological challenge. Our meta-analysis indicates that most studies fail to rigorously adhere to blinding standards, a limitation rooted in two intrinsic characteristics of these therapies. First, successful acupuncture requires inducing deqi (a characteristic compound sensation including pain, numbness, or swelling through precise acupoint stimulation), which inherently conflicts with blinding. Since deqi is both a prerequisite for therapeutic efficacy and a subjective patient experience, patients often recognize treatment authenticity during the intervention, thereby compromising outcome objectivity. Second, an inherent paradox exists in operator blinding: while using the same practitioner for real and sham interventions ensures procedural consistency, it risks unblinding, as practitioners may infer group allocation based on acupoint selection or manipulation techniques. Conversely, employing different practitioners introduces variability in manipulation skills, potentially biasing treatment effects. Notably, omitting sham acupuncture controls further increases unblinding risks. These dual challenges—patient-perceived deqi and operator-dependent efficacy—suggest that overemphasizing blinding as the sole criterion for assessing methodological quality in acupuncture research may be inappropriate.
As an indispensable part of traditional Chinese medicine, acupuncture exerts multimodal therapeutic effects in stroke rehabilitation through molecular and neurophysiological mechanisms. At the molecular level, EA inhibits cellular pyroptosis in cerebral ischemia/reperfusion injury models via PI3K/AKT/mTOR signaling (53), while concurrently mitigating neuroinflammation through cytokine regulation (54, 55). These neuroprotective effects synergize with angiogenesis promotion via miR-7 suppression (56) preserving peri-infarct neuronal viability. Functionally, acupuncture-induced neuroplasticity manifests as large-scale activation of sensorimotor networks and thalamic regions (57), with contralateral stimulation further modulating regional homogeneity in critical brain areas (58). Such plasticity facilitates neural circuit rewiring through enhanced neurogenesis and synaptic sprouting (59), directly supporting recovery of fine motor control—a prerequisite for hand function rehabilitation requiring precise cortical mapping.
Clinically, the therapeutic superiority of EA over TA may originate from three interlinked mechanistic advantages: first, electrical stimulation ensures the activation of corticospinal pathway (60), promoting synaptic remodeling and facilitating compensatory neural response generation post nerve injury; second, enhanced functional connectivity provides sustained neuromodulator effects (61, 62) particularly advantageous for patients with sensorimotor integration deficits; finally, through quantifiable parameters (e.g., frequency, intensity) reproducibly, EA avoids the dependence of manual acupuncture techniques on the operator, thus achieving personalized and precise solutions that are difficult to achieve with TA.
Neuroplasticity mechanisms and our findings clarify the significant heterogeneity in TA efficacy. This variability primarily stems from operator-dependent factors, including (1) acupoint selection criteria (e.g., anatomy-guided vs. meridian-based approaches) and (2) manipulation techniques (e.g., needle depth, angular dynamics). In resource-limited clinical settings where operator skill levels vary, EA demonstrates superior reproducibility through its parameter-driven approach. Healthcare systems in underserved areas (such as rural regions or primary care facilities in developing countries) are often confronted with multifaceted challenges, including shortages of medical equipment and insufficient healthcare professionals. As a combination of TA and electrical stimulation, EA provides a simple, safe and effective rehabilitation method due to its standardized scheme, cost-effectiveness and evidence-based treatment benefits, which is worth popularizing.
This study has several limitations. First, while we intentionally avoided overemphasizing blinding procedures for doctors and patients, most included studies failed to report whether outcome assessors or statistical analysts were blinded, nor did they describe allocation concealment methods. These reporting gaps may introduce bias risks, particularly for outcomes involving subjective measurements. Second, in the TA group, variability in acupoint selection criteria and acupuncture techniques resulted in high heterogeneity, preventing subgroup analyses to assess the specific effects of different acupuncture methods or acupoint choices on post-stroke hand dysfunction. Future trials should adopt standardized protocols and incorporate studies from diverse countries/regions to better compare and evaluate the efficacy of distinct acupuncture approaches.
5 Conclusion
Our study confirms the efficacy of acupuncture in alleviating post-stroke hand dysfunction, with electroacupuncture demonstrating comparative advantages over traditional methods in enhancing motor function recovery. Despite consistent reports of positive outcomes across existing studies, critical methodological limitations—particularly the inadequate implementation of allocation concealment and blinding—raise concerns about the validity of current evidence. To strengthen clinical applicability, future research must prioritize rigorous trial designs, standardized efficacy assessments, and systematic exploration of optimal acupoint combinations and stimulation parameters. These efforts will facilitate the development of evidence-based protocols for post-stroke rehabilitation.
Statements
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found: all data were extracted from published studies cited in the manuscript. Summarized results are presented in the text, and raw data can be obtained by contacting the corresponding authors of the original publications.
Author contributions
YL: Visualization, Writing – original draft, Conceptualization, Investigation, Software. JZho: Investigation, Resources, Writing – review & editing. JZhe: Investigation, Writing – review & editing. JC: Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Innovation Fund for Integrating Chinese and Western Medicine (ZS22XTCX02) at the Third Affiliated Hospital of Zhejiang University of Traditional Chinese Medicine.
Acknowledgments
The authors would like to express their sincere gratitude to Jing Chen for the financial support, which greatly facilitated this research. Special thanks are extended to Biao Ru for their invaluable guidance and insightful critiques throughout the development of this review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1589874/full#supplementary-material
SUPPLEMENTARY FILE 1The complete search strategies for all databases.
SUPPLEMENTARY FILE 2Bonferroni correction of BRS.
SUPPLEMENTARY FILE 3List of abbreviations.
References
1.
Jiang H Zhang C Lin M Yin Y Deng S Liu W et al . Deciphering the mechanistic impact of acupuncture on the neurovascular unit in acute ischemic stroke: insights from basic research in a narrative review. Ageing Res Rev. (2024) 101:102536. doi: 10.1016/j.arr.2024.102536
2.
Magid-Bernstein J Girard R Polster S Srinath A Romanos S Awad IA et al . Cerebral hemorrhage: pathophysiology, treatment, and future directions. Circ Res. (2022) 130:1204–29. doi: 10.1161/CIRCRESAHA.121.319949
3.
Feigin VL Owolabi MO . Pragmatic solutions to reduce the global burden of stroke: a world stroke organization-lancet neurology commission. Lancet Neurol. (2023) 22:1160–206. doi: 10.1016/S1474-4422(23)00277-6
4.
Hu Z Sun W Cui E Chen B Zhang M . Association between psychiatric disorders and the risk of stroke: a meta-analysis of cohort studies. Front Neurol. (2024) 15:1444862. doi: 10.3389/fneur.2024.1444862
5.
Shahid J Kashif A Shahid MK . A comprehensive review of physical therapy interventions for stroke rehabilitation: impairment-based approaches and functional goals. Brain Sci. (2023) 13:717. doi: 10.3390/brainsci13050717
6.
Wu S Wu B Liu M Chen Z Wang W Anderson CS et al . Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/S1474-4422(18)30500-3
7.
Yang A Wu HM Tang JL Xu L Yang M Liu GJ . Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev. (2016) 2016. doi: 10.1002/14651858.CD004131.pub3
8.
Zhang J Wu M Li X Yu D Jia H Wang B et al . Effect of acupuncture on dysphagia after stroke: a Meta-analysis and trial sequential analysis of randomized controlled trials. Cerebrovasc Dis. (2025) 1-25:1–25. doi: 10.1159/000544743
9.
Gittler M Davis AM . Guidelines for adult stroke rehabilitation and recovery. JAMA. (2018) 319:820–1. doi: 10.1001/jama.2017.22036
10.
Tian Y Yan X Wang H Dang C Sun Y . Efficacy of acupuncture therapy for spastic paralysis in post-stroke patients: a systematic review and meta-analysis. Int J Neurosci. (2025) 135:180–7. doi: 10.1080/00207454.2023.2292955
11.
Anliang C Xueping L Junlong Y Wenhong S Jun Z Wei W et al . Effect of acupuncture on nerve trunks and rehabilitation training on hand function of stroke patients. Chin J Rehabilit. (2008) 23:416. doi: 10.3870/zgkf.2008.06.019
12.
Huang XY Liao OP Jiang SY Tao JM Li Y Lu XY et al . Three-dimensional kinematic analysis can improve the efficacy of acupoint selection for post-stroke patients with upper limb spastic paresis: a randomized controlled trial. J Integr Med. (2024) 23:15–24. doi: 10.1016/j.joim.2024.12.004
13.
Qing X Huihui W Xuejiao L . Clinical study of acupuncture combined with functional electrical stimulation on hand dysfunction after stroke. Syst Med. (2024) 9:9–13. doi: 10.19368/j.cnki.2096-1782.2024.04.009
14.
Hong L Yingxuan A Xue S Xin M Weiping C . The influence of warm – needling Moxibustion combined with shock wave on hand function and cognitive function after stroke. Shanghai J Acupunct Moxibust. (2024) 43:1307–12. doi: 10.13460/j.issn.1005-0957.2024.12.1307
15.
Bao G Xing S Xuezhi R Xiaodong Y Ru W . The influence of traditional Chinese medicine brain-awakening acupuncture on the recovery of limb function during the rehabilitation phase in patients with post-stroke hemiplegia. J Clin Res. (2024) 41:58–61. doi: 10.3969/j.issn.1671-7171.2024.01.016
16.
Peixin W . Clinical observation on acupuncture at “complementary acupuncture points” for intervention of hand dysfunction after stroke. [Master’s thesis]. Chengde (HB), China: Chengde Medical University (2023). Available from: https://link.cnki.net/doi/10.27691/d.cnki.gcdyx.2023.000308
17.
Dongqing F . Clinical observation on the treatment of hand spasm after stroke by Ying – sui Xie Hegu (LI4) combined with needling Sifeng (EX – UE10). [Master’s thesis]. Harbin (HL), China: Heilongjiang University of Chinese Medicine (2023). Available from: https://link.cnki.net/doi/10.27127/d.cnki.ghlzu.2023.000157
18.
Fengfan Z . Clinical observation on the treatment of finger spasm after stroke by He – gu puncture at Hegu (LI4) point combined with warm – needling Moxibustion. [Master’s thesis]. Shenyang (LN), China: Liaoning University of Traditional Chinese Medicine (2022). Available from: https://link.cnki.net/doi/10.27213/d.cnki.glnzc.2022.000087
19.
Weiyan X . Observation on the curative effect of guan acupuncture at Zhongquan point on flexion and extension dysfunction of wrist and finger joints during stroke recovery period. [Master’s thesis]. Nanchang (JX), China: Jiangxi University of Traditional Chinese Medicine (2022). Available from: https://link.cnki.net/doi/10.27180/d.cnki.gjxzc.2022.000091
20.
Yinjin S Shuiping X Xiaochun W Guihua W Wenjuan D . Effects of fire-needle acupuncture Jingjin node combined with rehabilitation training on hand spasm and hemorheology after stroke. J Jiangxi Univ Chin Med. (2022) 34:60–3.
21.
Xiaona L Peiyang S Yugang W Lingling Z Haoran C . Effect of electroaccupuncture combined with rehabilitation manipulator on hand function in post-stroke hemiplegia. Shanghai J Acupunct Moxibust. (2022) 41:330–4. doi: 10.13460/j.issn.1005-0957.2022.04.0330
22.
Linying H . Clinical observation on the therapeutic efficacy of the hand five – needle penetrating acupuncture method in treating finger spasm of sequelae of stroke. [Master’s thesis]. Shenyang (LN), China: Liaoning University of Traditional Chinese Medicine (2021). Available from: https://link.cnki.net/doi/10.27213/d.cnki.glnzc.2021.000512
23.
Qin Y Ying W . Study on the effect of Acupoint stimulation combined with rehabilitation training onFinger fine movement after stroke. World Latest Med Informat. (2020) 20:115. doi: 10.3969/j.issn.1671-3141.2020.89.047
24.
Juan L . Mill fire-needle pricking at connecting meridians for hand dysfunction after stroke. Tradit Chin Med Rehabilit. (2020) 11:19–21. doi: 10.19787/j.issn.1008-1879.2020.22.005
25.
Xuan Z Zhifeng L . Research on the repetitive transeranial magnetic stimulation combined with acupuncture on rehabilitation of hand function after stroke. Guangming J Chin Med. (2019) 34:762–4. doi: 10.3969/j.issn.1003-8914.2019.05.045
26.
Jun'e L Lianjia L Hongze R . Acupuncture antagonistic muscle combined with spastic muscle Thera-peutic apparatus clinical observation on the treatment of finger Spasmafter apoplexy. Biped Health. (2019) 28:15–7. doi: 10.19589/j.cnki.issn1004-6569.2019.09.015
27.
Hongyang F . Clinical observation on the treatment of spasmodic palsy of fingers after apoplexy with articular needling Sifeng (EX-UE 10). [Master’s thesis]. Harbin (HL), China: Heilongjiang University of Chinese Medicine (2019). Available from: https://link.cnki.net/doi/10.27127/d.cnki.ghlzu.2019.000285
28.
Chen S He L Gao X Wang Y Kang G Feng L . Clinical observation on plum-blossom needle combined with rehabilitation training for hand spasm after stroke. Zhongguo Zhen Jiu. (2018) 38:799–802. doi: 10.13703/j.0255-2930.2018.08.001
29.
Yilin W . Electromyographic biofeedback assessment of wrist dorsiflexion dysfunction rehabilitation by electroacupuncture after stroke. [Master’s thesis]. Fuzhou (FJ), China: Fujian University of Traditional Chinese Medicine (2018). Available from: https://kns.cnki.net/kcms2/article/abstract?v=vFI3APHTe50cXF8QHkhiPNuc0iIt9xXK-W_E_YAN-m5rhbCdrgTXVmPbXdt9sUp4vn4YObhA0Q0Q68dfjAdWbTEJ34D4IsD1W4eoDcS_bqwT03IHV-e-DfADy9jFbNTX0ZaRN2kqd4gffqtQVTxHGt_l_p8U7NOVF7c9D8SEaqvPSPda5T2ZnQ-3m_LfzrWtfYN-ai477CE=&uniplatform=NZKPT&language=CHS
30.
Tian M Lou T Leng J . Clinical observation of acupuncture plus electroacupuncture for hand spasm in stroke patients. Zhongguo Zhen Jiu. (2017) 37:932–5. doi: 10.13703/j.0255-2930.2017.09.005
31.
Rui Z Meilan Z Ying Y Bangliang L Lianhua W . Effects of mirror therapy combined with Tongdu Xingshen acupuncture on upper extremity function in post-stroke patients. Chin J Phys Med Rehabilit. (2017) 39:588–93. doi: 10.3760/cma.j.issn.0254-1424.2017.08.006
32.
Wanli T Ae A . The impact of acupuncture therapy on motor function and sleep quality of stroke patients in the convalescent stage. Shaanxi J Tradit Chin Med. (2016) 3:357–8.
33.
Shaoyang C Mingzhu X Shenghui Z Xinsheng L Chunzhi T Shuhui W et al . Effect of Jin's three – needle therapy combined with Mirror therapy on upper limb and hand dysfunction in hemiplegic patients. Chin J Phys Med Rehabilit. (2015) 37:550–1. doi: 10.3760/cma.j.issn.0254-1424.2015.07.022
34.
Zaiyi J Guodong H Quan Z Muyuan C Shenyi L Jie Z . Clinical observation on 20 cases stroke hand dysfunction by selected Acupoint stimulation combined with motor imagery therapy. Guiding J Tradit Chin Med Phar. (2014) 11:20–2. doi: 10.13862/j.cnki.cn43-1446/r.2014.11.007
35.
Yu Z Haibin M Xiangtao C Xiaoyan Y Jingpeng C Weixing Z . Impact of scalp acupuncture combined with acupuncture at hand Acupoints on the affected side and functional training on early hand function in hemiplegic stroke patients. Ningxia Med J. (2013) 35:749–50. doi: 10.13621/j.1001-5949.2013.08.003
36.
Miao Z Wenxun X Lu L Peng C Shaosong W Yuanbo F et al . Clinical study on the treatment of hand dysfunction on ischemic stroke decubation by acupuncture “hand fourteen acupuncture”. J Liaoning Univ Tradit Chin Med. (2024) 26:65–9. doi: 10.13194/j.issn.1673-842X.2024.11.013
37.
Ying C . A clinical study on hand dysfunction after cerebral infarction treated by penetrating from acupuncture points named Baxie (extra 28) to Laogong (P8). Master’s thesis]. Guangzhou (GD), China: Guangzhou University of Chinese Medicine (2022). Available from: https://link.cnki.net/doi/10.27044/d.cnki.ggzzu.2022.000873
38.
Manandhar M . Clinical study of acupuncture and occupational therapy in the treatment of upper limb dysfunction after stroke [Master’s thesis]. Tongliao (NM), China: Inner Mongolia University for Nationalities (2021). Available from: https://d.wanfangdata.com.cn/thesis/ChhUaGVzaXNOZXdTMjAyNDA5MjAxNTE3MjUSCUQwMjQ3Njc0NRoIYXBpNmZrcmc%3D
39.
Yifei D Yanhong L Wenjuan S Yan L Runrun Y Siqi C et al . Observation on therapeutic effect of yuan-source points and collateral -points combination with rehabilitation training on hand spasm after stroke. Modern J Integr Tradit Chin Western Med. (2021) 30:497–501. doi: 10.3969/j.issn.1008-8849.2021.05.009
40.
Jie D Yong Z Xinying S Rui J . Efficacy of electroacupuncture at yuan-primary and Luo-connecting acupoints of three yang meridians of hands in treating patients with cerebral infarction at convalescence. J Clin Med Pract. (2021) 25:91–4. doi: 10.7619/jcmp.20212431
41.
Zuxin X Xiaohua W Li L Lijuan D Yuanzhong C . Effect of scalp Acupoint twirling reinforcing method combined with functional electrical stimulation on the rehabilitation of fine hand movements and limb muscle strength in stroke hemiplegic patients. Modern J Integr Tradit Chin Western Med. (2019) 28:2909–11. doi: 10.3969/i.issn.1008-8849.2019.26.014
42.
Shanshan L . The effects of abdominal acupuncture treatment on motor dysfunction of upper limb in patients with stroke[Master’s thesis]. Guangzhou (GD), China: Guangzhou University of Chinese Medicine (2019). Available from: https://link.cnki.net/doi/10.27044/d.cnki.ggzzu.2019.000766
43.
Lixing Z Shifen X Xun Z . Effect of JIN's 3-needle technique and motor function training on upper extremities motor recovery of cerebral apoplexy induced hemiplegia In: The 11th academic symposium of Guangdong provincial acupuncture association. Guangzhou (GD), China. Beijing (BJ), China: Chinese Acupuncture and Moxibustion Society (2010) 15–18.
44.
Sujin F Sheng W Guiqin Z Mengwei L Jia H . Clinical observation on the treatment of hand spasm after stroke by the acupuncture method of reinforcing Yang and Reducing Yin. China Naturopathy. (2023) 31:73–6. doi: 10.19621/j.cnki.11-3555/r.2023.1321
45.
Xinzhi X . Clinical observation on the efficacy of electro – acupuncture at Waiguan (SJ5) and Wailaogong (EX – UE8) points combined with rehabilitation training in the treatment of finger flexion spasm after ischemic stroke. Chin J Integr Med Cardio Cerebr Dis. (2022) 20:3232–4.
46.
Yanfei J Pengmu S Yuelai C . Efficacy of acupuncture at Waiguan-Yangxi and Neiguan-Ximen matching acupoints on hand function in stroke patients with hand grasping disorder. Clin J Chin Med. (2021) 13:80–2. doi: 10.3969/j.issn.1674-7860.2021.14.024
47.
Wang XC Liu T Wang JH Zhang JJ . Post-stroke hand spasm treated with penetrating acupuncture combined with kinesiotherapy: a randomized controlled trial. Zhongguo Zhen Jiu. (2020) 40:21–5. doi: 10.13703/j.0255-2930.20190106-k0003
48.
Lifei M Ying Z Chunfang W Changcheng S Kuan L Xia X . Effects of acupuncture on upper limb motor function after stroke based on brain electrophysiology. Chin J Rehabilit. (2020) 35:135–8. doi: 10.3870/zgkf.2020.03.005
49.
Dingjiong S . The influence of Xingnao Kaiqiao acupuncture method combined with Brunnstrom staging on hand dysfunction after stroke. Lishizhen Med Materia Med. (2018) 29:1656–7. doi: 10.3969/j.issn.1008-0805.2018.07.039
50.
Jie W Ying W Liushun J Ronglin C . Effect of early rehabilitation training combined with penetration needling Hegu (LI4) and Houxi (SI3) on finger function of stroke patients with hemiplegia. J Zhejiang Chin Med Univ. (2016) 40:851–4.
51.
Yang J Xiao H . The effect of floating-needle therapy combined with rehabilitation training for the hand function recovery of post-stroke patients. Zhongguo Zhen Jiu. (2015) 35:758–62. doi: 10.13703/j.0255-2930.2015.08.002 PMID:
52.
Yisi J Bo Y Guizhen Z . The clinical research on shoulder acupuncture combined with upper limb function training to improve upper limb motor functions in patients with hemiplegia after stroke. Henan Tradit Chin Med. (2015) 35:142–4. doi: 10.16367/j.issn.1003-5028.2015.01.0062
53.
Qiu Z Ma J Zhang X Jiao M Zhi L . Electroacupuncture combined with trigonel line inhibits pyroptosis in cerebral ischemia-reperfusion by suppressing autophagy via the PI3K/AKT/mTOR signaling pathway. Brain Res Bull. (2025) 221:111200. doi: 10.1016/j.brainresbull.2025.111200
54.
Sun X Cai J Zhang A Pang B Cheng C Cha Q et al . Electroacupuncture pretreatment alleviates post-stroke spasticity in rats by inhibiting NF-κB/NLRP3 signaling pathway-mediated inflammation and neuronal apoptosis. Nan Fang Yi Ke Da Xue Xue Bao. (2024) 44:2102–9. doi: 10.12122/j.issn.1673-4254.2024.11.06
55.
Yu YY Yang Y Jiang J . Moxibustion preconditioning reduces inflammatory response in rats with cerebral ischemia-reperfusion injury by regulating PI3K/AKT/mTOR signaling pathway. Zhen Ci Yan Jiu. (2024) 49:238–46. doi: 10.13702/j.1000-0607.20230267
56.
Yu Q Shu S Ju XY Peng W Ren XQ Si SH et al . Electroacupuncture promotes angiogenesis in mice with cerebral ischemia by inhibiting miR-7. Chin J Integr Med. (2024) 30:543–50. doi: 10.1007/s11655-023-3715-z
57.
Qian X Zhang H Peng J Song L Lv Q Jia W et al . Acupuncture modulates group neural activity in patients with post stroke sensory impairment: an fMRI study based on inter-subject correlation and inter-subject functional connectivity. Brain Res Bull. (2025) 222:111259. doi: 10.1016/j.brainresbull.2025.111259
58.
Chen SQ Cai DC Chen JX Yang H Liu LS . Altered brain regional homogeneity following contralateral acupuncture at Quchi (LI 11) and Zusanli (ST 36) in ischemic stroke patients with left hemiplegia: an fMRI study. Chin J Integr Med. (2020) 26:20–5. doi: 10.1007/s11655-019-3079-6
59.
Zhang J Lu C Wu X Nie D Yu H . Neuroplasticity of acupuncture for stroke: an evidence-based review of MRI. Neural Plast. (2021) 2021:1–14. doi: 10.1155/2021/2662585
60.
Winstein CJ Stein J Arena R Bates B Cherney LR Cramer SC et al . Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2016) 47:e98–e169. doi: 10.1161/STR.0000000000000098
61.
Li M Zou F Zheng T Zou W Li H Lin Y et al . Electroacupuncture alters brain network functional connectivity in subacute stroke: a randomised crossover trial. Medicine. (2024) 103:e37686. doi: 10.1097/MD.0000000000037686
62.
Li SS Xing XX Hua XY Zhang YW Wu JJ Shan CL et al . Electroacupuncture modulates abnormal brain connectivity after ischemia reperfusion injury in rats: a graph theory-based approach. Brain Behav. (2024) 14:e3504. doi: 10.1002/brb3.3504
Summary
Keywords
acupuncture, electroacupuncture, hand dysfunction, stroke, meta-analysis
Citation
Liu Y, Zhou J, Zheng J and Chen J (2025) Efficacy of different acupuncture therapies on hand dysfunction in post-stroke patients: a systematic review and meta-analysis. Front. Neurol. 16:1589874. doi: 10.3389/fneur.2025.1589874
Received
08 March 2025
Accepted
02 May 2025
Published
22 May 2025
Volume
16 - 2025
Edited by
Lorie Gage Richards, The University of Utah, United States
Reviewed by
Aylin Akçalı, University of Gaziantep, Türkiye
Xun Luo, Kerry Rehabilitation Medicine Research Institute, China
Updates
Copyright
© 2025 Liu, Zhou, Zheng and Chen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Chen, doctorchen1975@163.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.